Wheeze and Asthma Mark Minor M D Section





- Slides: 41
Wheeze and Asthma Mark Minor, M. D. Section of Pulmonary Medicine Dayton Children’s Hospital
Conflicts of Interest / Disclaimers • None
Question 1 • What is the timeframe for onset of action of systemic prednisone (orapred)? A. 30 minutes B. 1 -2 hours C. 4 -6 hours D. 12 hours
Question 2 • Which 2 year old child has a positive asthma predictive index? A. B. C. D. 3 episodes of wheezing/year and allergic rhinitis 3 episodes of wheezing/year and 7% blood eosinophils 3 episodes of wheezing/year and eczema 3 episodes of wheezing/year and wheezing outside of colds
Objectives • Overview of causes of wheezing • Define natural course of wheezing in infants • Review risk factors for asthma • Review step method for asthma treatment • Review alternatives for uncontrolled persistent asthma
Case • 9 year old with recurrent wheeze and persistent dry cough o Cough present for about two years, day and night o Multiple visits to PCP, ED, Urgent Care with complaint of cough • Documentation of wheeze and use of Albuterol and/or systemic steroids on separate occasions o Multiple courses of systemic steroids for wheeze / cough with subjective improvement • Usually accompanied with URI symptoms • Minimal improvement with use of Albuterol o On exam: Dry cough, mild inspiratory and expiratory wheeze
Causes of wheezing • Asthma • Vascular rings or slings • Tracheomalacia, Bronchomalacia • Viruses • Chronic aspiration • Cystic Fibrosis • Foreign body • Mediastinal or airway mass
Wheezing in infancy • Common problem • Approximately 1/3 of infants (Kuehni et al. Eur Resp Journal; 2000 16(1): 81 -5) • Recurrent wheeze in about 1: 5 infants (Alvarez et al. Aller Immun; 2018, 209 -310)
Risk factors for recurrent wheeze • Viral respiratory tract infections (RSV, rhinovirus etc. ) • Atopic sensitization • Family history of asthma • Pre-natal and Post-natal exposure to maternal smoking • Gastroesophageal reflux/Aspiration • Exposure to environmental pollution • Prematurity (BPD), Male gender • Structural airway anomalies
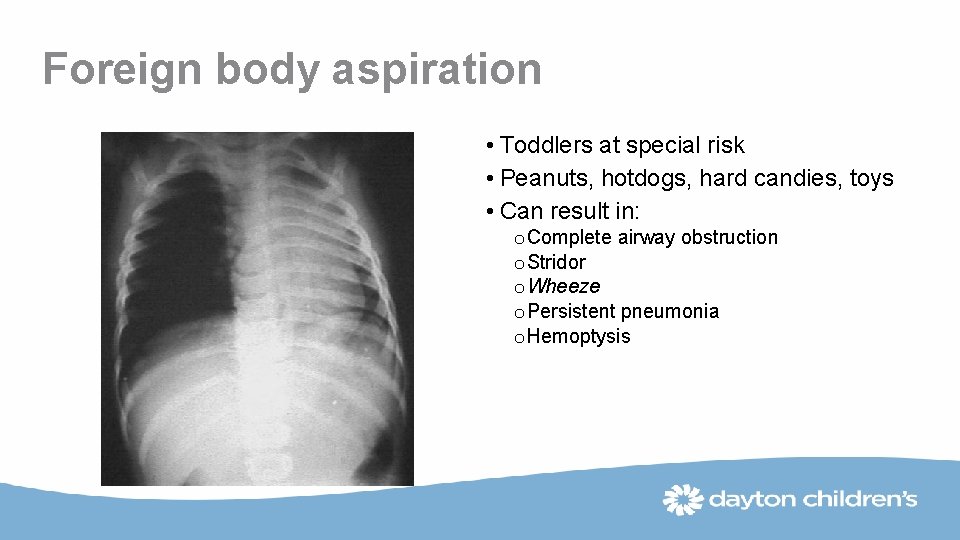
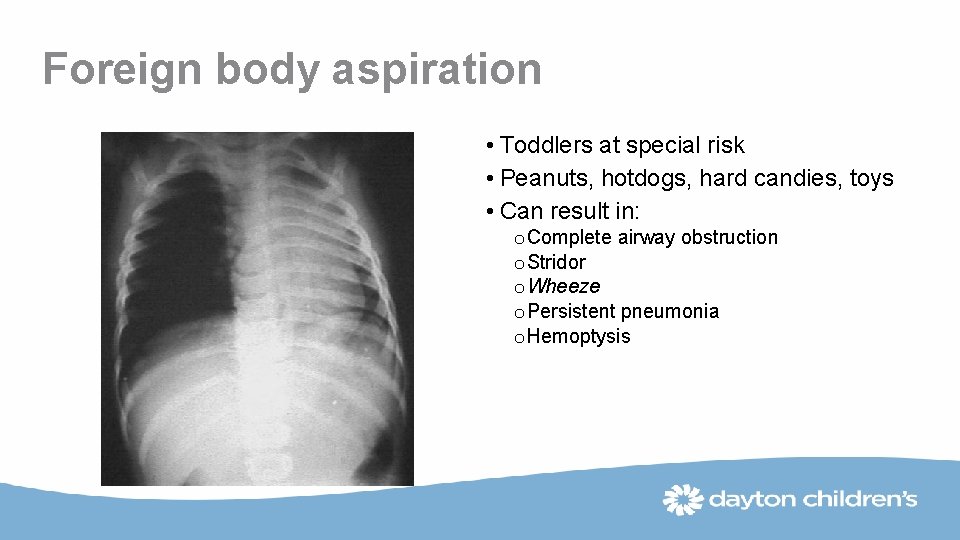
Foreign body aspiration • Toddlers at special risk • Peanuts, hotdogs, hard candies, toys • Can result in: o Complete airway obstruction o Stridor o Wheeze o Persistent pneumonia o Hemoptysis
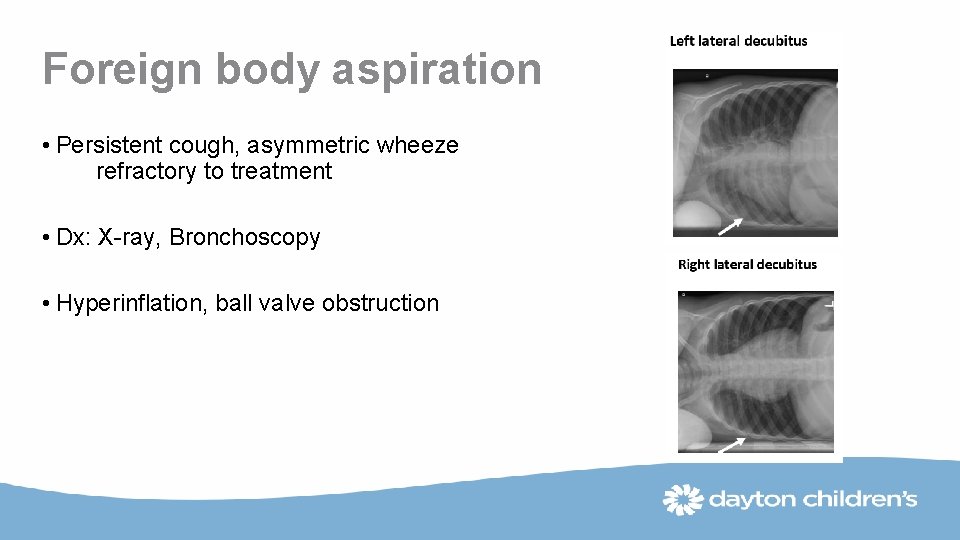
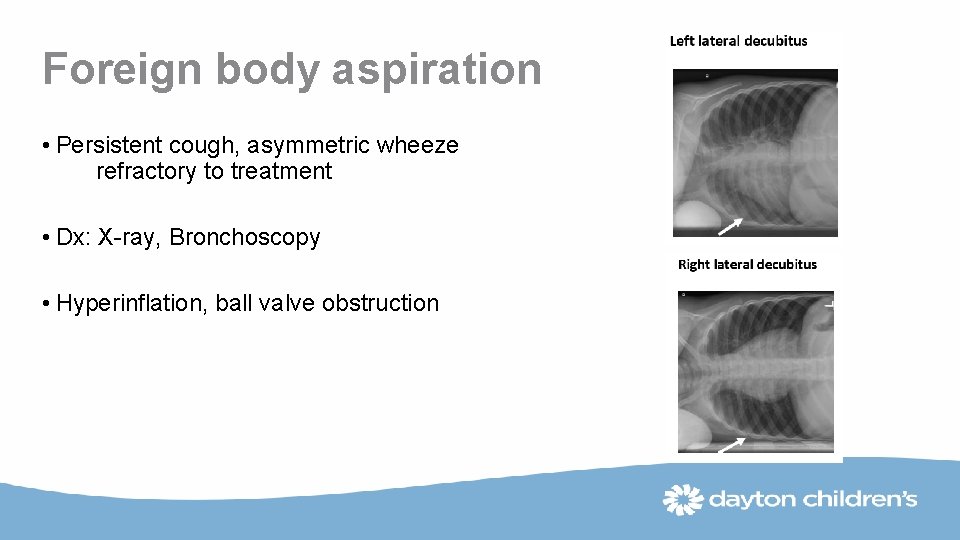
Foreign body aspiration • Persistent cough, asymmetric wheeze refractory to treatment • Dx: X-ray, Bronchoscopy • Hyperinflation, ball valve obstruction

Peanut in Right Mainstem Bronchus
Virus induced wheezing • Strong association between viral bronchiolitis and recurrent wheezing during infancy • Infants in daycare have more wheezing episodes than infants who are not in daycare due to increased exposure to viruses
Virus induced wheezing • 20% of all children have at least one episode of lower respiratory illness associated with wheezing in the first year of life • Rhino Virus infection leading to hospitalization during infancy is an early predictor of the subsequent development of asthma K otaneimi-syrjanen A. et al. JACI 2003, 111: 66 • Risk of asthma after viral bronchiolitis is increased in the presence of allergic sensitization in early life and if the infection is more severe
Childhood asthma
Epidemiology of Childhood Asthma • Most important chronic respiratory disorder in childhood • Affects approximately 5 -15% of all children o Boys > Girls in young children o Girls > Boys in adolescents • Adverse outcomes significantly determined by race and ethnicity Akinbami L. Centers for Disease Control 2006; 381: 1

Evaluation and Treatment of Atopy in Childhood Asthma • Atopy is present in > 75% of children with persistent asthma • Role in exacerbations based on age: o < 3 years: viral respiratory infections o > 3 years: viral infections + allergen exposure • Sensitization pattern based on age: o < 1 year: eczema/milk, soy, egg, wheat, peanut o > 3 years: dust mite, molds, pollen, ragweed Heymann et al, J Allergy Clin Immunol 2004; 114: 239
Diagnosing asthma in infancy • Infants and toddlers who present with frequent early wheeze is a challenge • Almost 80% of asthma starts before 5 years of age
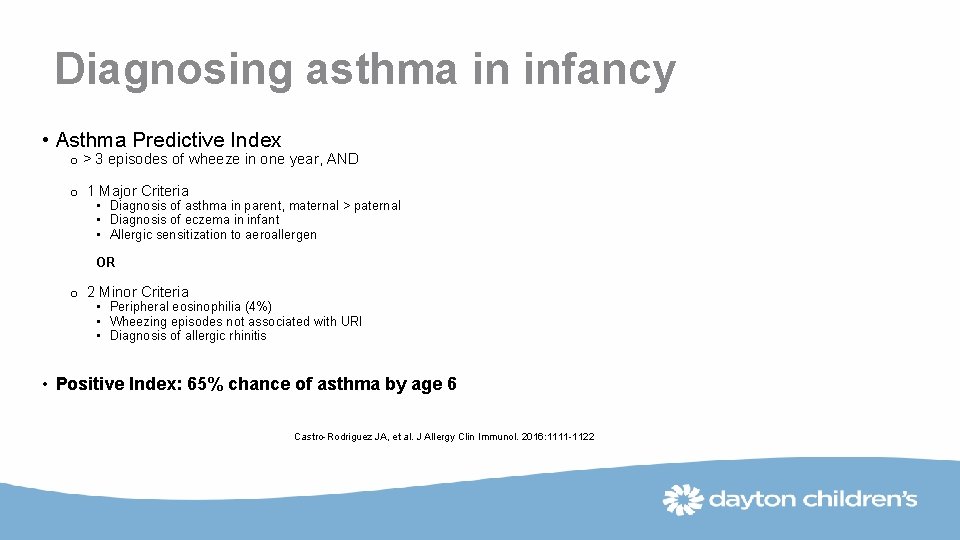
Diagnosing asthma in infancy • Asthma Predictive Index o > 3 episodes of wheeze in one year, AND o 1 Major Criteria • Diagnosis of asthma in parent, maternal > paternal • Diagnosis of eczema in infant • Allergic sensitization to aeroallergen OR o 2 Minor Criteria • Peripheral eosinophilia (4%) • Wheezing episodes not associated with URI • Diagnosis of allergic rhinitis • Positive Index: 65% chance of asthma by age 6 Castro-Rodriguez JA, et al. J Allergy Clin Immunol. 2016: 1111 -1122
Other predictors increasing risk of asthma • Maternal overweight or obesity during pregnancy • Prenatal maternal smoking • Postnatal maternal smoking, < 5 years of age • Other household smoking • Preterm birth and low birth weight • RSV infection • Household mold • BMI > 95 th %
Approach to acute asthma exacerbation, or status asthmaticus • Administer treatment of inhaled SABA, repeat times three, and promptly give oral corticosteroids if needed o Addition of Ipratropium Bromide (Atrovent) is effective o Prednisone 2 mg/kg/day up to 40 -60 mg for 3 -7 days, or o Dexamethasone 0. 6 mg/kg (maximum 12 mg), repeat x 1 in 24 hours • Prednisone has onset of action: 4 to 6 hours • IV Fluids if dehydrated, watch for SIADH, hypokalemia • Keep Oxygen saturation > 95%
Approach to acute asthma exacerbation, or status asthmaticus • Chest xray? o Severe respiratory distress o Unilateral wheeze o Focally diminished breath sounds • No antibiotics unless reasonable evidence of an acute bacterial infection
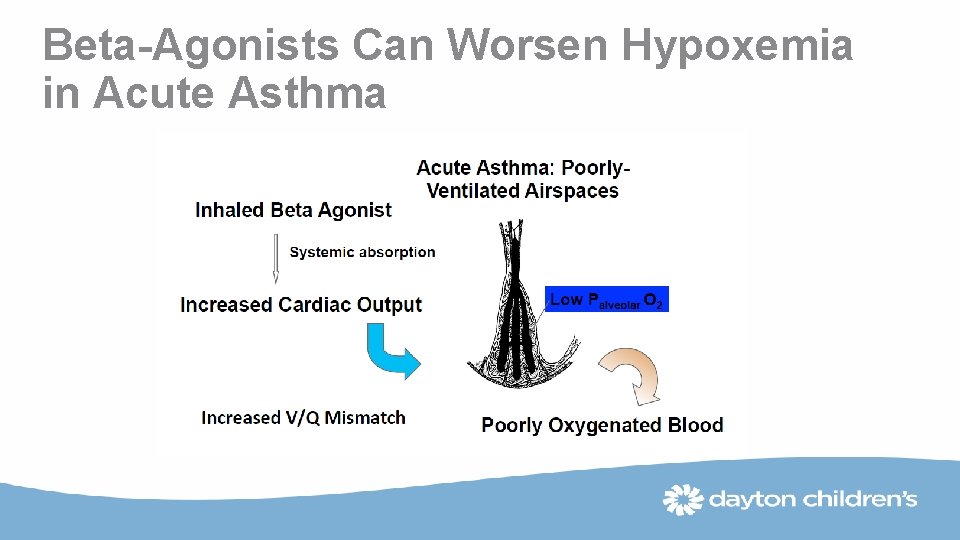
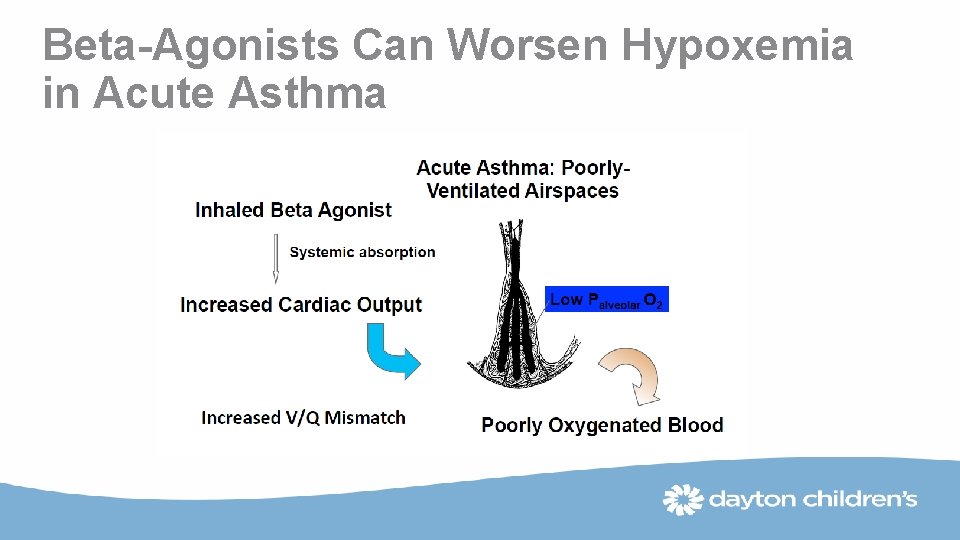
Beta-Agonists Can Worsen Hypoxemia in Acute Asthma
Nebulizer vs MDI with Spacer

Changes/Updated in 2018 to GINA Guidelines • Step 1 o It is explained that the reason ICS should be considered for patients with mild asthma (rather than prescribing SABA alone) is to reduce their risk of serious exacerbations (Pauwels, Lancet 2003; O’Byrne AJRCCM 2001; Reddel Lancet 2017) • Steps 3 -4 o From the large FDA LABA safety studies: adding LABA to ICS in a combination inhaler reduces risk of exacerbations and improves symptoms and lung function, compared with the same dose of ICS alone, but with only a small reduction in reliever use (Stempel NEJM 2016, Peters NEJM 2016) • Step 5 management of severe asthma o Subcutaneous benralizumab (monoclonal anti-IL 5 receptor α antibody) is another add-on treatment for patients aged ≥ 12 years with severe eosinophilic asthma
Uncontrolled asthma • Co-morbidities (GERD, rhinitis, etc) • Poor adherence • Ineffective delivery of treatment, ie poor inhaler technique • Severe therapy-resistant disease • Ongoing exacerbating triggers (smoke, allergens, pollutants) • Misdiagnosis • Inadequate treatment
Persistent asthma • Consider Biologic Therapy (injection therapy) if appropriate o. Xolair o. Nucala o. Dupixent – newest for certain types
Biologic targeting Ig. E • Omalizumab (Xolair) o Binds to free Ig. E o Approved for above age 6 years o Shown to decrease: symptoms, exacerbations, ICS dose o Shown to increase: FEV 1, quality of life
Biologic targeting eosinophils • Mepolizumab (Nucala) o IL-5 binding to eosinophils o Approved for age 12 years and above o Decreases exacerbations, symptoms, ICS dose o Increases FEV 1 and quality of life
Biologic targeting IL-4 and IL-13 • Dupilumab (Dupixent) o. Recently approved for asthma control o. For treatment of atopic dermatitis, eczema, and persistent asthma o. Approved for ages 12 years and above
Summary of key points • Asthma is a complex disease with significant phenotypic heterogeneity • Control of exacerbating factors can improve symptoms • Treatment of asthma is based on severity-based guidelines • New therapies are available to treat severe/uncontrolled asthma

Case continued
Case continued • 9 year old with recurrent wheeze and persistent dry cough
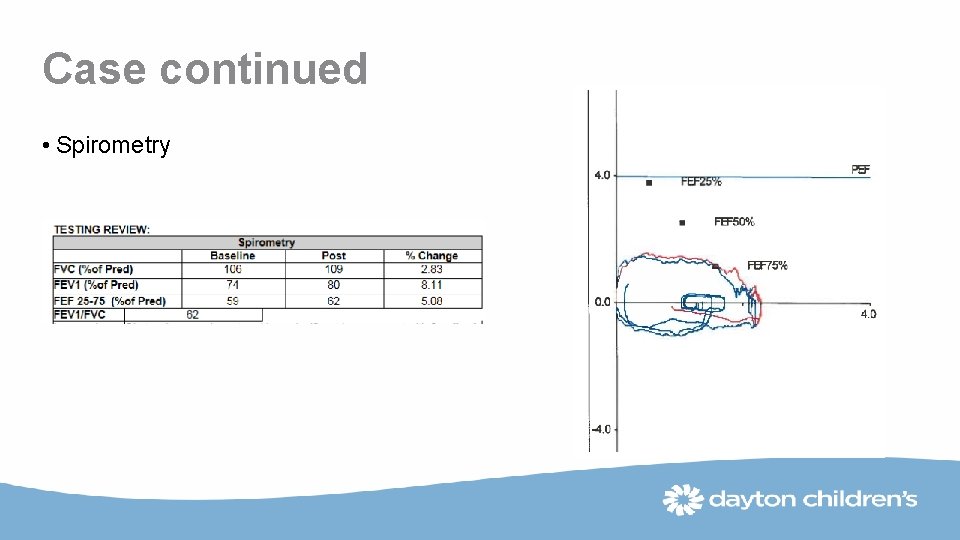
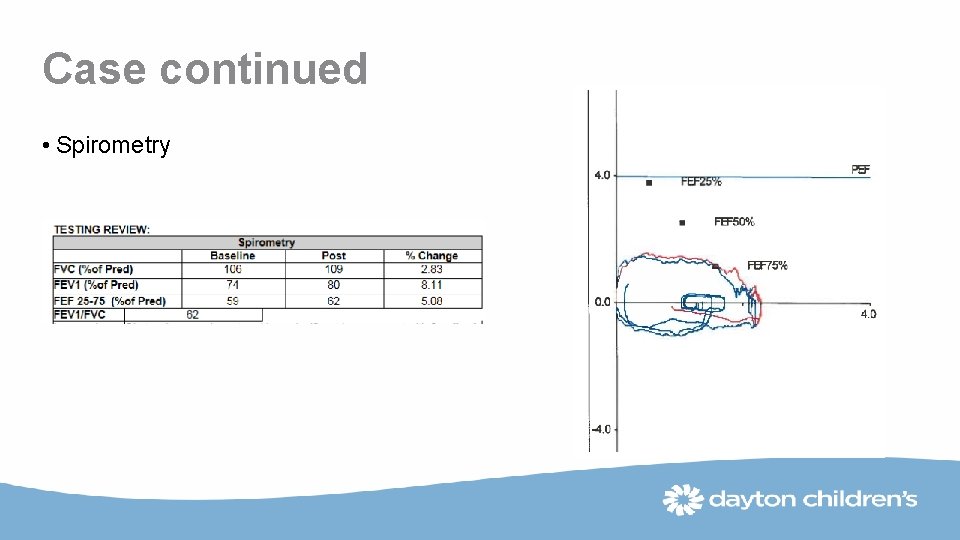
Case continued • Spirometry
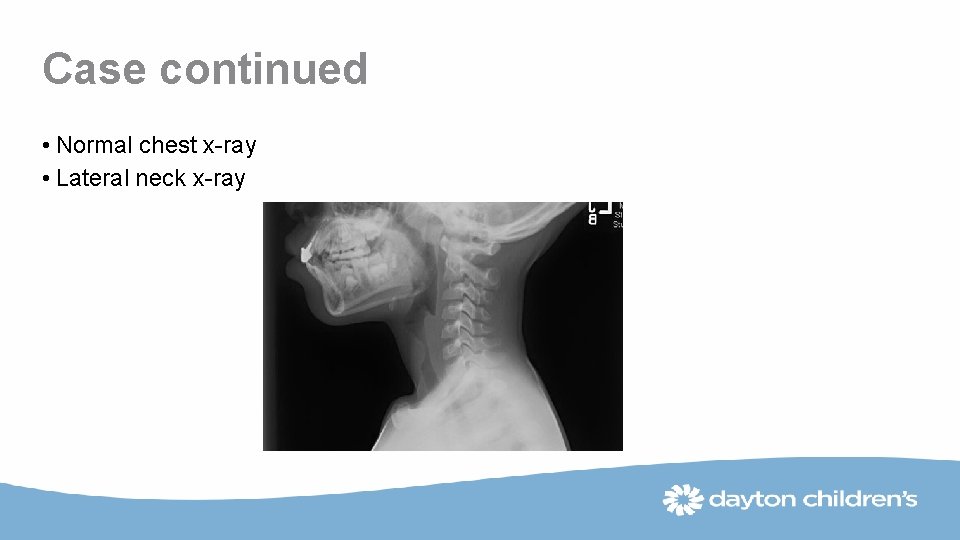
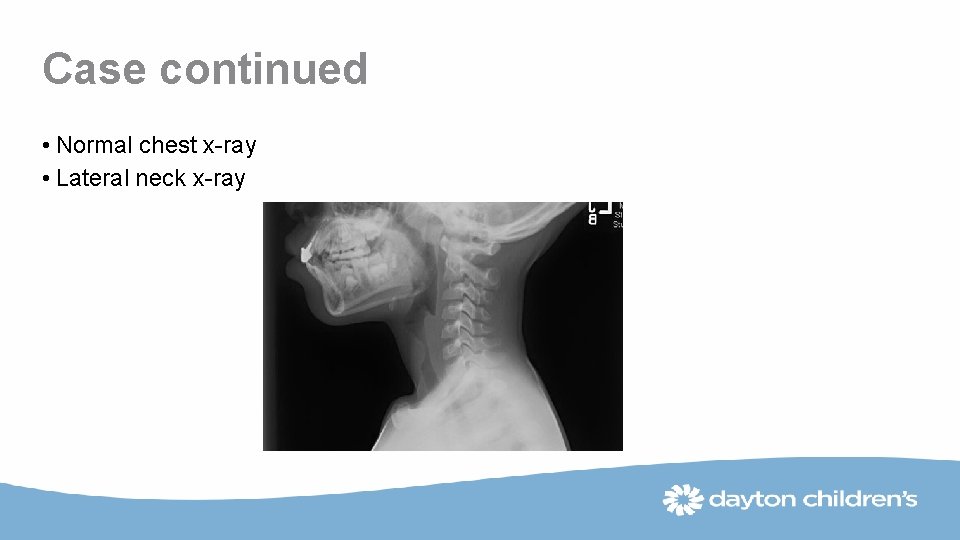
Case continued • Normal chest x-ray • Lateral neck x-ray
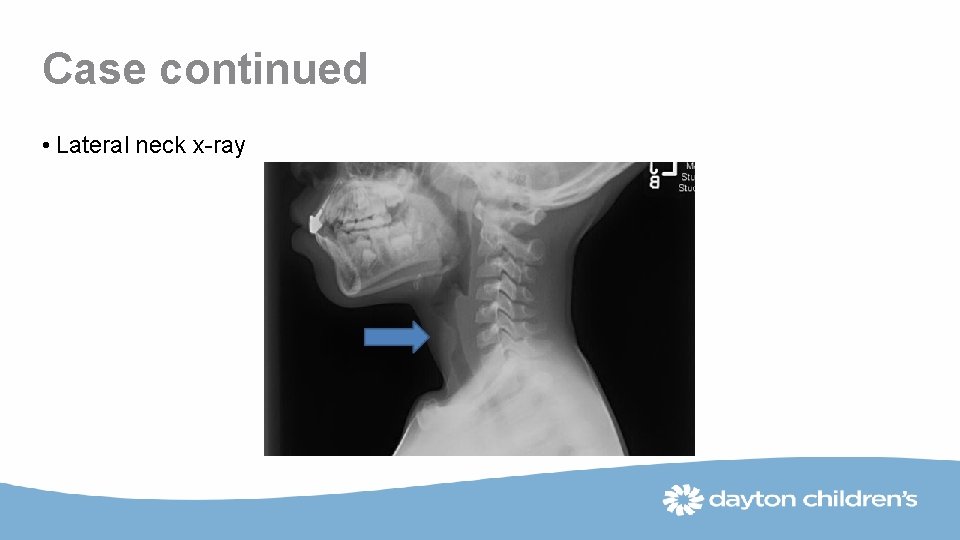
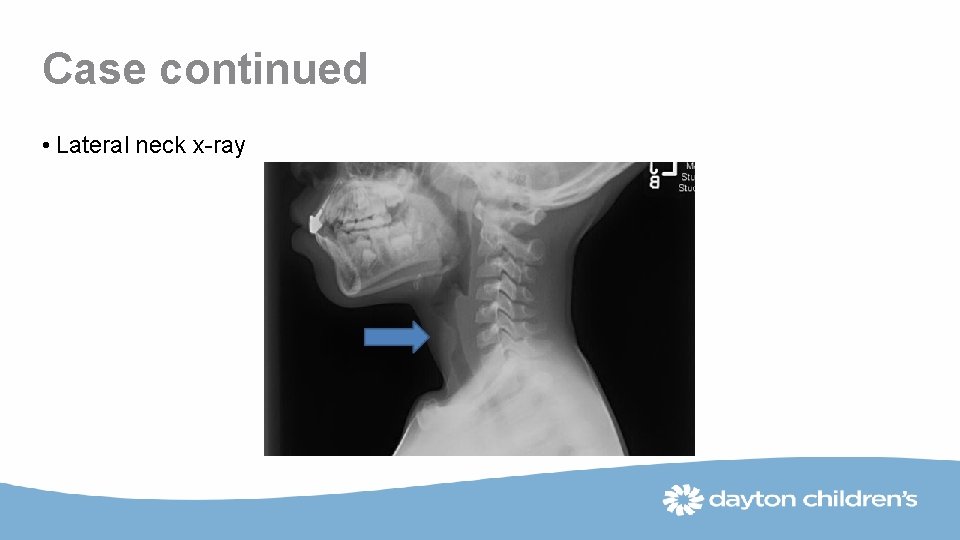
Case continued • Lateral neck x-ray
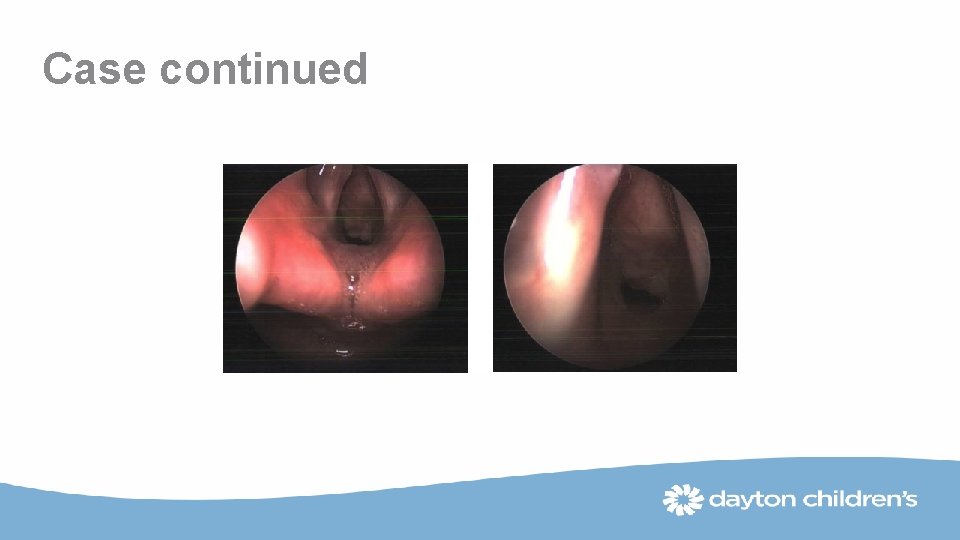
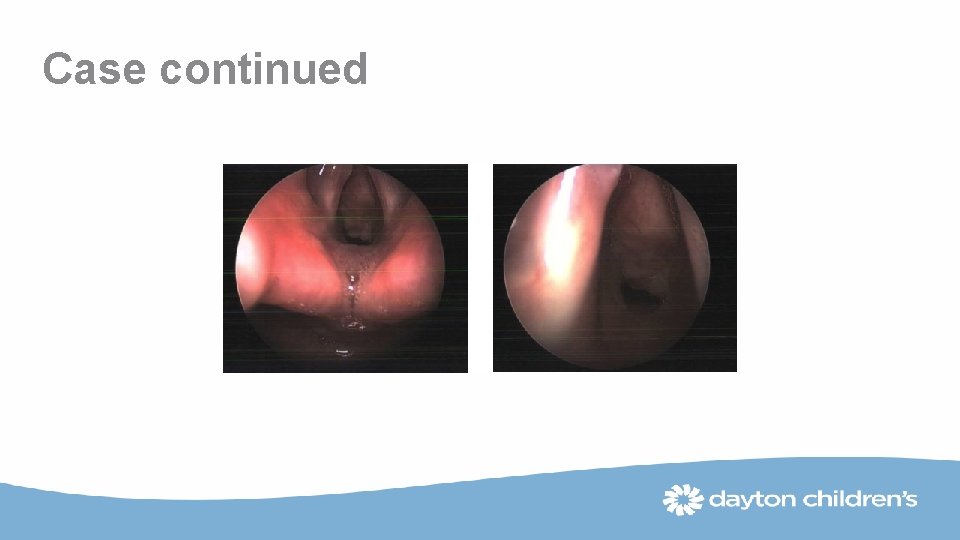
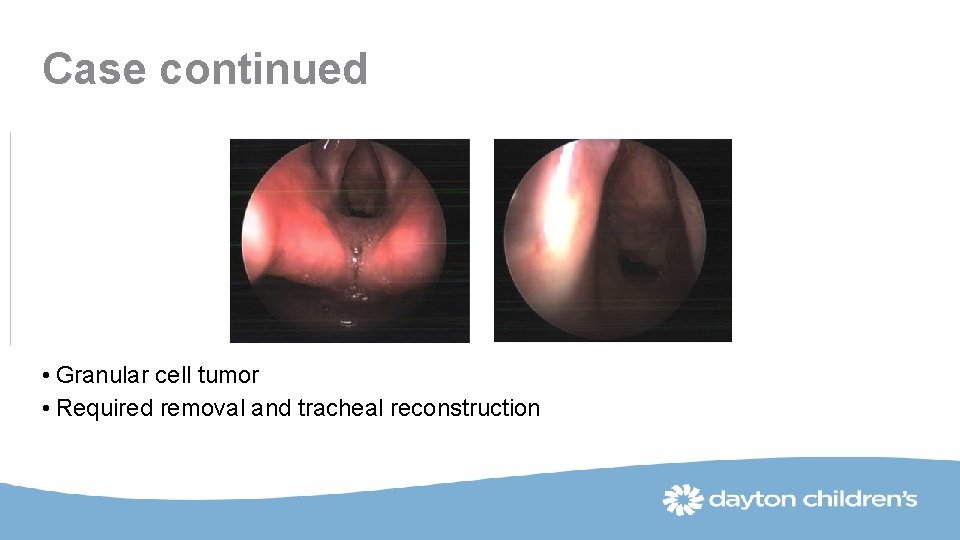
Case continued
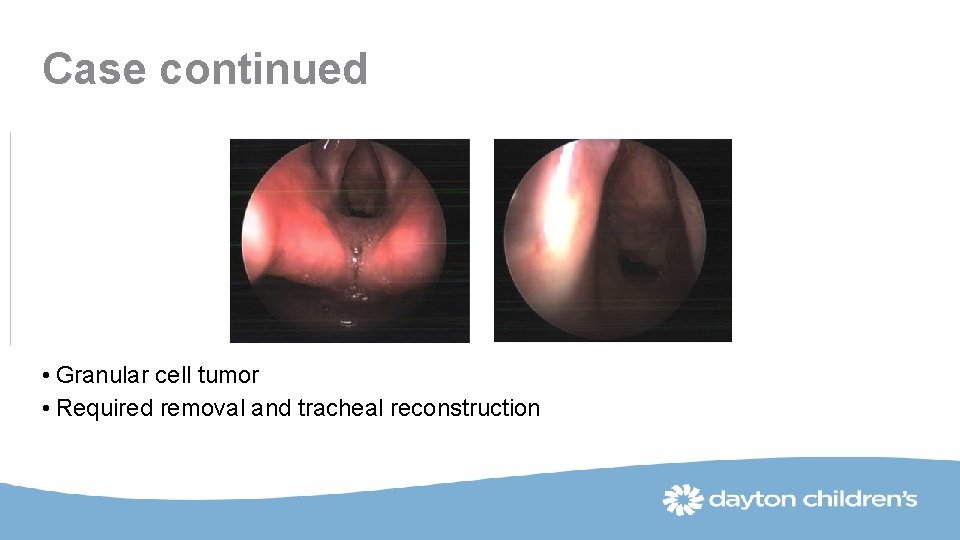
Case continued • Granular cell tumor • Required removal and tracheal reconstruction

Thank You! Mark Minor, MD Section of Pulmonary Medicine Dayton Children’s Hospital