What Should be the Lipid Targets in Patients
What Should be the Lipid Targets in Patients with Diabetes and the Metabolic Syndrome? Michael Davidson M. D. FACC, Diplomate of the American Board of Lipidology Clinical Professor, Director of Preventive Cardiology The University of Chicago Pritzker School of Medicine 1

DISCLOSURES Michael H. Davidson, MD Consulting Fees – Abbott Vascular, Astra. Zeneca, Glaxo. Smith. Kline Honoraria – Abbott Vascular, Astra. Zeneca, Glaxo. Smith. Kline, Schering-Plough Corp. / Merck & Co. , Inc. Grants/Contracted Research – Abbott Vascular, Astra. Zeneca
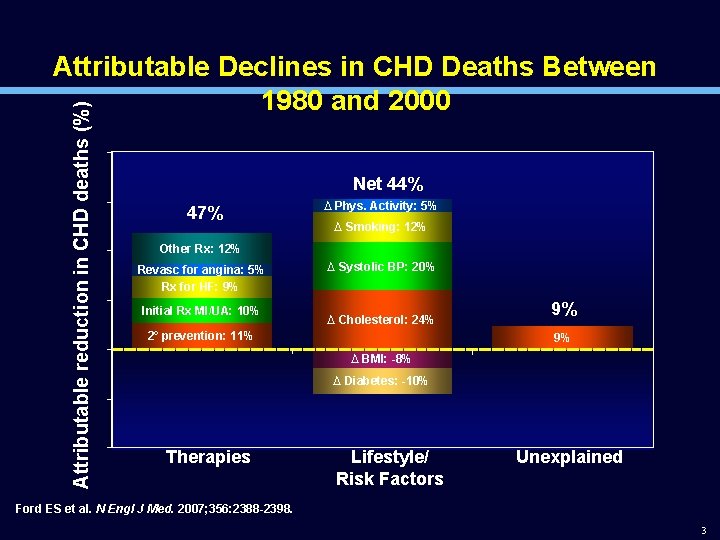
Attributable reduction in CHD deaths (%) Attributable Declines in CHD Deaths Between 1980 and 2000 Net 44% 47% ∆ Phys. Activity: 5% ∆ Smoking: 12% Other Rx: 12% Revasc for angina: 5% Rx for HF: 9% Initial Rx MI/UA: 10% ∆ Systolic BP: 20% ∆ Cholesterol: 24% 2˚ prevention: 11% 9% 9% ∆ BMI: -8% ∆ Diabetes: -10% Therapies Lifestyle/ Risk Factors Unexplained Ford ES et al. N Engl J Med. 2007; 356: 2388 -2398. 3
4
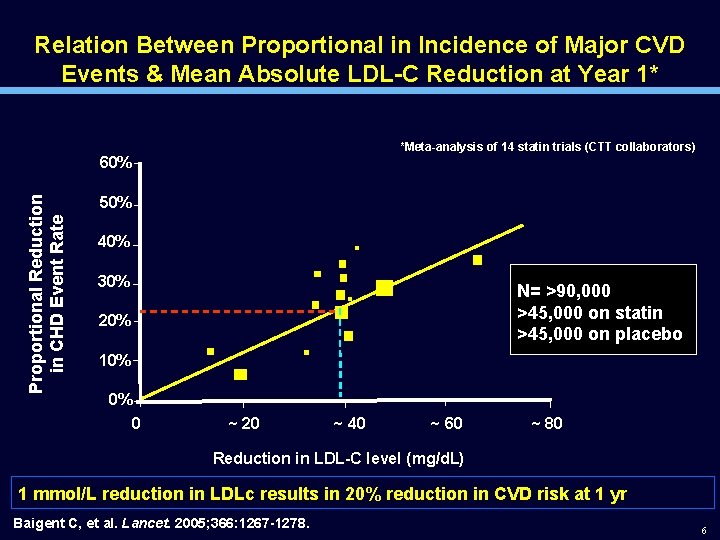
Relation Between Proportional in Incidence of Major CVD Events & Mean Absolute LDL-C Reduction at Year 1* *Meta-analysis of 14 statin trials (CTT collaborators) Proportional Reduction in CHD Event Rate 60% 50% 40% 30% N= >90, 000 >45, 000 on statin >45, 000 on placebo 20% 10% 0% 0 ~ 20 ~ 40 ~ 60 ~ 80 Reduction in LDL-C level (mg/d. L) 1 mmol/L reduction in LDLc results in 20% reduction in CVD risk at 1 yr Baigent C, et al. Lancet. 2005; 366: 1267 -1278. 6
Is it statins or LDL-c? 7

Linking Cholesterol to Atherosclerosis The young Nikolai N. Anitschkow ca. 1904, at the time a student at the Military Medical Academy in St. Petersburg. His drawing of a typical foam cellrich lesion in a rabbit 8
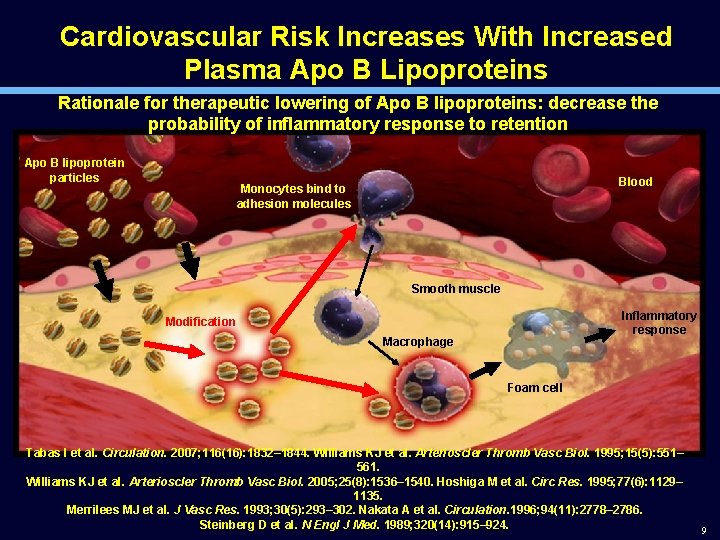
Cardiovascular Risk Increases With Increased Plasma Apo B Lipoproteins Rationale for therapeutic lowering of Apo B lipoproteins: decrease the probability of inflammatory response to retention Apo B lipoprotein particles Blood Monocytes bind to adhesion molecules Smooth muscle Inflammatory response Modification Macrophage Foam cell Tabas I et al. Circulation. 2007; 116(16): 1832– 1844. Williams KJ et al. Arterioscler Thromb Vasc Biol. 1995; 15(5): 551– 561. Williams KJ et al. Arterioscler Thromb Vasc Biol. 2005; 25(8): 1536– 1540. Hoshiga M et al. Circ Res. 1995; 77(6): 1129– 1135. Merrilees MJ et al. J Vasc Res. 1993; 30(5): 293– 302. Nakata A et al. Circulation. 1996; 94(11): 2778– 2786. Steinberg D et al. N Engl J Med. 1989; 320(14): 915– 924. 9

A. Non-Human Mammals B. Humans - US 700 FH Homozygotes 300 200 - 100 50 - Lion 150 Rat Guinea Pig Sheep Cow Rabbit Dog Cat Camel Pig LDL Levels FH Heterozygotes Normal Adults Newborns 0 10
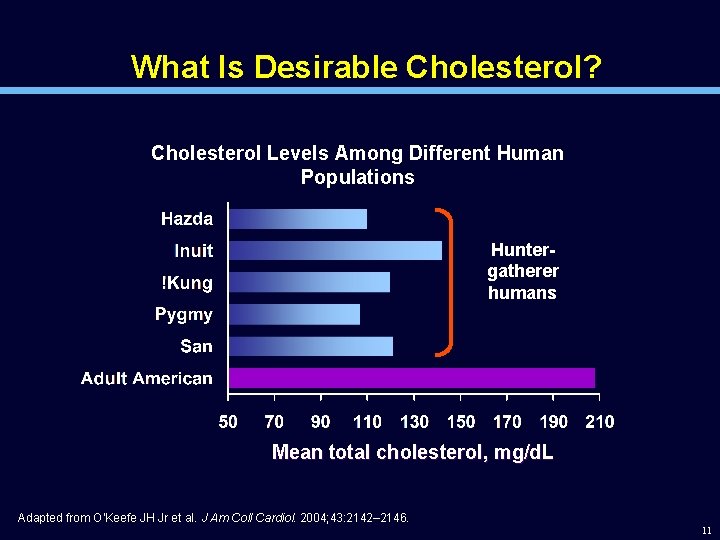
What Is Desirable Cholesterol? Cholesterol Levels Among Different Human Populations Huntergatherer humans Mean total cholesterol, mg/d. L Adapted from O’Keefe JH Jr et al. J Am Coll Cardiol. 2004; 43: 2142– 2146. 11
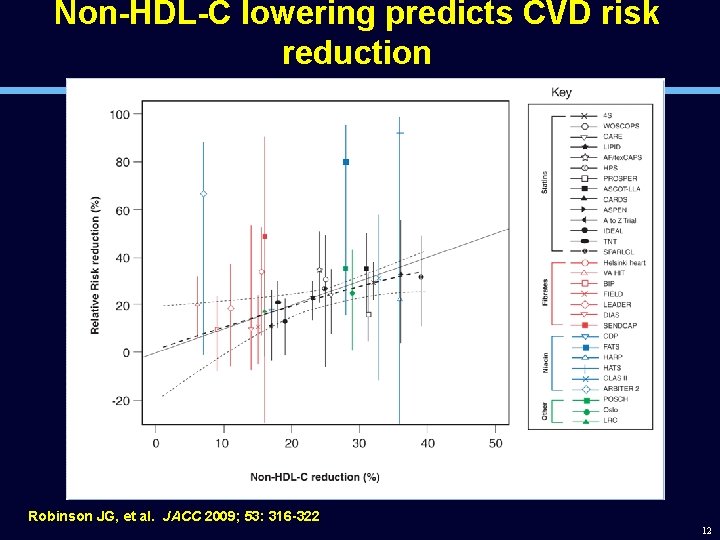
Non-HDL-C lowering predicts CVD risk reduction Robinson JG, et al. JACC 2009; 53: 316 -322 12
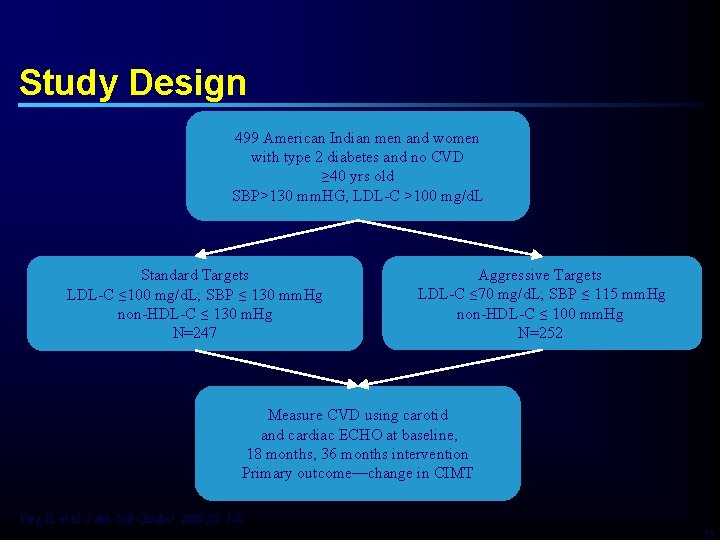
Study Design 499 American Indian men and women with type 2 diabetes and no CVD ≥ 40 yrs old SBP>130 mm. HG, LDL-C >100 mg/d. L Standard Targets LDL-C ≤ 100 mg/d. L; SBP ≤ 130 mm. Hg non-HDL-C ≤ 130 m. Hg N=247 Aggressive Targets LDL-C ≤ 70 mg/d. L; SBP ≤ 115 mm. Hg non-HDL-C ≤ 100 mm. Hg N=252 Measure CVD using carotid and cardiac ECHO at baseline, 18 months, 36 months intervention Primary outcome—change in CIMT Fleg JL et al. J Am Coll Cardiol. 2008; 52: 1 -8. 13
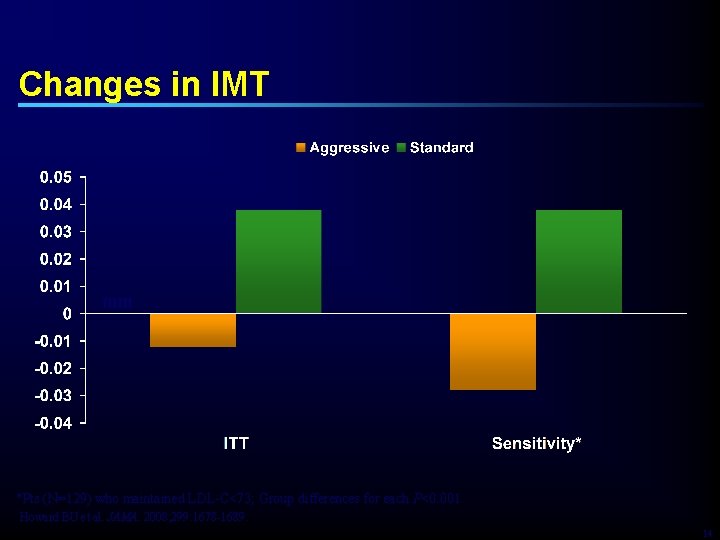
Changes in IMT mm *Pts (N=129) who maintained LDL-C<73; Group differences for each P<0. 001 Howard BU et al. JAMA. 2008; 299: 1678 -1689. 14
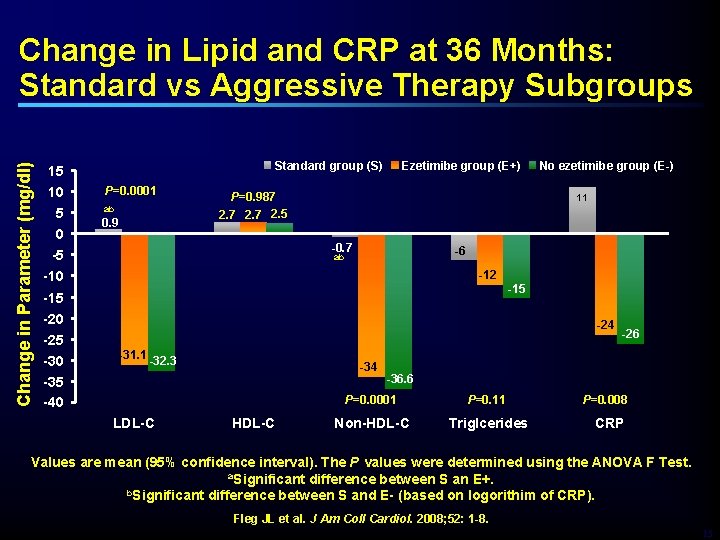
Change in Parameter (mg/dl) Change in Lipid and CRP at 36 Months: Standard vs Aggressive Therapy Subgroups 15 10 5 0 -5 -10 -15 -20 -25 -30 -35 -40 Standard group (S) P=0. 0001 ab 0. 9 Ezetimibe group (E+) P=0. 987 2. 5 No ezetimibe group (E-) 11 -0. 7 -6 ab -12 -15 -24 -31. 1 -32. 3 LDL-C -34 HDL-C -26 -36. 6 P=0. 0001 P=0. 11 Non-HDL-C Triglcerides P=0. 008 CRP Values are mean (95% confidence interval). The P values were determined using the ANOVA F Test. a. Significant difference between S an E+. b. Significant difference between S and E- (based on logorithim of CRP). Fleg JL et al. J Am Coll Cardiol. 2008; 52: 1 -8. 15
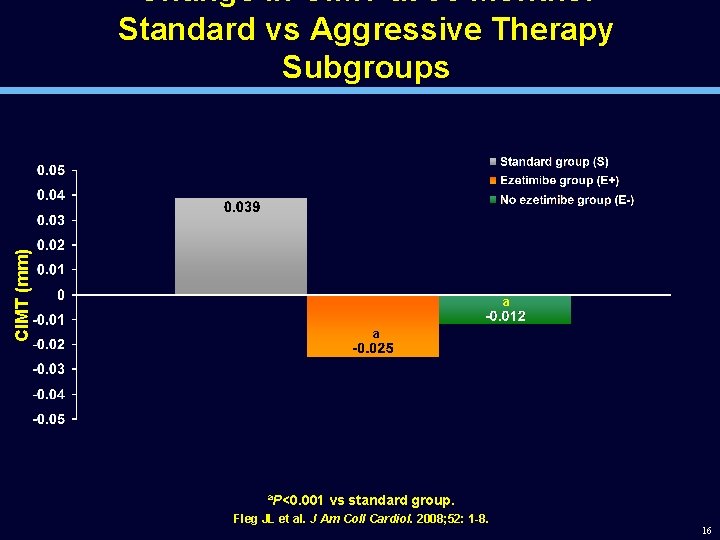
CIMT (mm) Change in CIMT at 36 Months: Standard vs Aggressive Therapy Subgroups a a a. P<0. 001 vs standard group. Fleg JL et al. J Am Coll Cardiol. 2008; 52: 1 -8. 16
Is LDL-c or LDL-p/Apo. B/non-HDL? 17
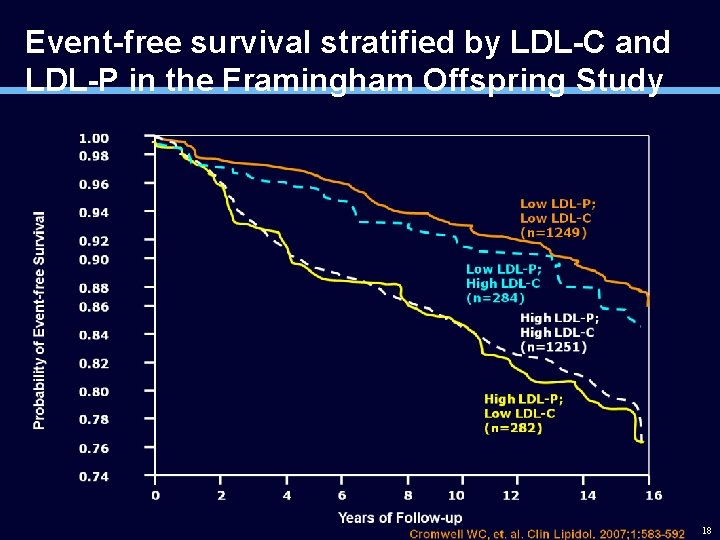
Event-free survival stratified by LDL-C and LDL-P in the Framingham Offspring Study 18
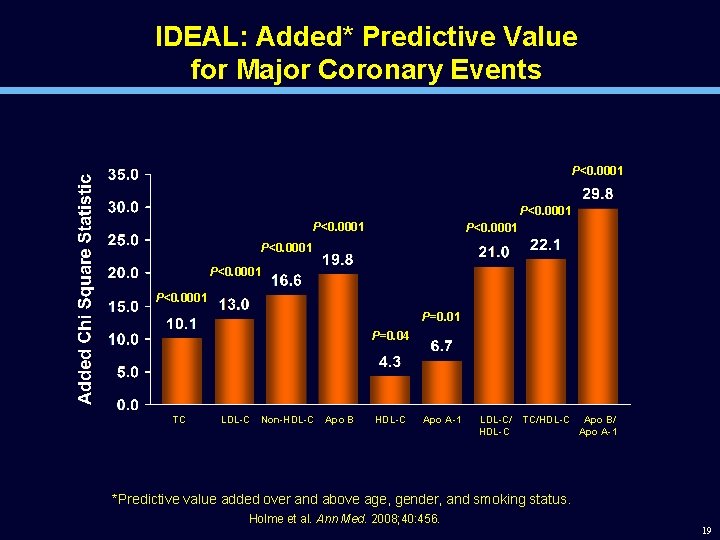
IDEAL: Added* Predictive Value for Major Coronary Events P<0. 0001 P<0. 0001 P=0. 04 TC LDL-C Non-HDL-C Apo B HDL-C Apo A-1 LDL-C/ HDL-C TC/HDL-C Apo B/ Apo A-1 *Predictive value added over and above age, gender, and smoking status. Holme et al. Ann Med. 2008; 40: 456. 19
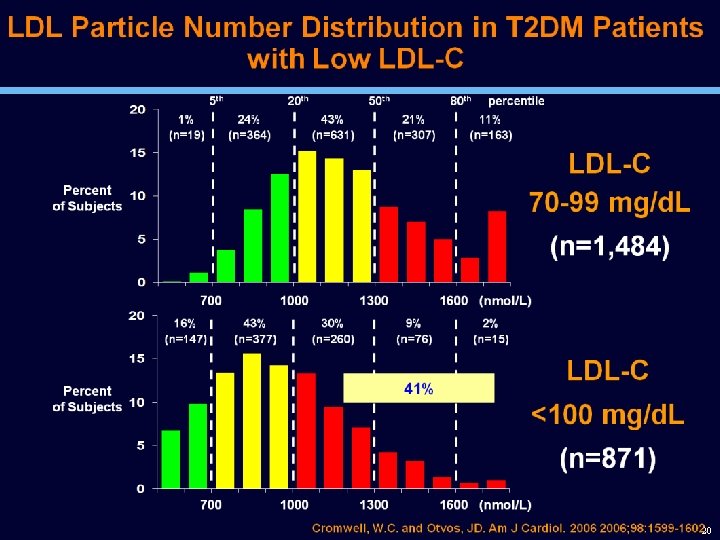
20
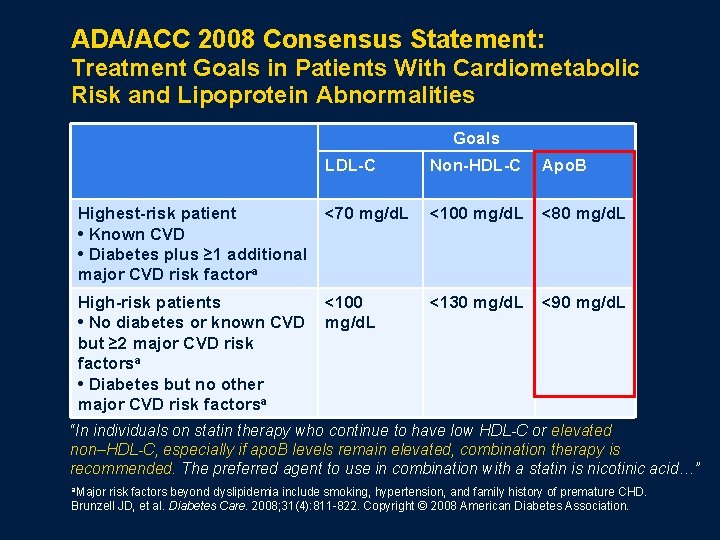
ADA/ACC 2008 Consensus Statement: Treatment Goals in Patients With Cardiometabolic Risk and Lipoprotein Abnormalities Goals LDL-C Non-HDL-C Apo. B Highest-risk patient • Known CVD • Diabetes plus ≥ 1 additional major CVD risk factora <70 mg/d. L <100 mg/d. L <80 mg/d. L High-risk patients • No diabetes or known CVD but ≥ 2 major CVD risk factorsa • Diabetes but no other major CVD risk factorsa <100 mg/d. L <130 mg/d. L <90 mg/d. L “In individuals on statin therapy who continue to have low HDL-C or elevated non–HDL-C, especially if apo. B levels remain elevated, combination therapy is recommended. The preferred agent to use in combination with a statin is nicotinic acid…” a. Major risk factors beyond dyslipidemia include smoking, hypertension, and family history of premature CHD. Brunzell JD, et al. Diabetes Care. 2008; 31(4): 811 -822. Copyright © 2008 American Diabetes Association.
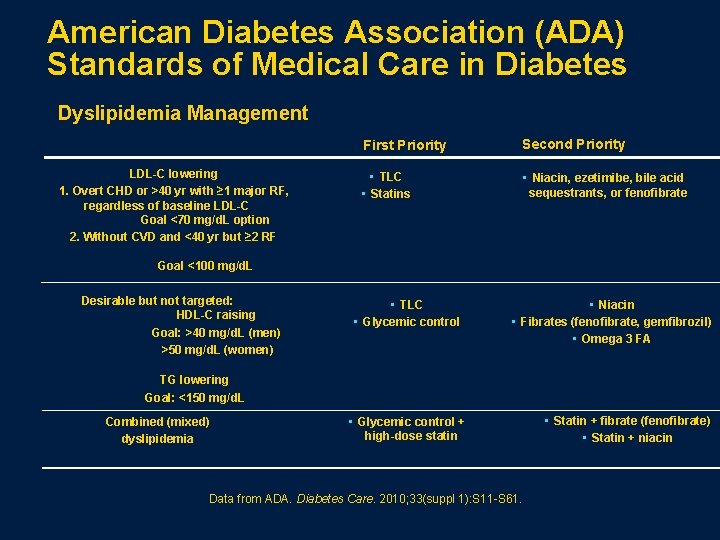
American Diabetes Association (ADA) Standards of Medical Care in Diabetes Dyslipidemia Management LDL-C lowering 1. Overt CHD or >40 yr with ≥ 1 major RF, regardless of baseline LDL-C Goal <70 mg/d. L option 2. Without CVD and <40 yr but ≥ 2 RF First Priority Second Priority • TLC • Statins • Niacin, ezetimibe, bile acid sequestrants, or fenofibrate Goal <100 mg/d. L Desirable but not targeted: HDL-C raising Goal: >40 mg/d. L (men) >50 mg/d. L (women) • TLC • Glycemic control • Niacin • Fibrates (fenofibrate, gemfibrozil) • Omega 3 FA TG lowering Goal: <150 mg/d. L Combined (mixed) dyslipidemia • Glycemic control + high-dose statin Data from ADA. Diabetes Care. 2010; 33(suppl 1): S 11 -S 61. • Statin + fibrate (fenofibrate) • Statin + niacin
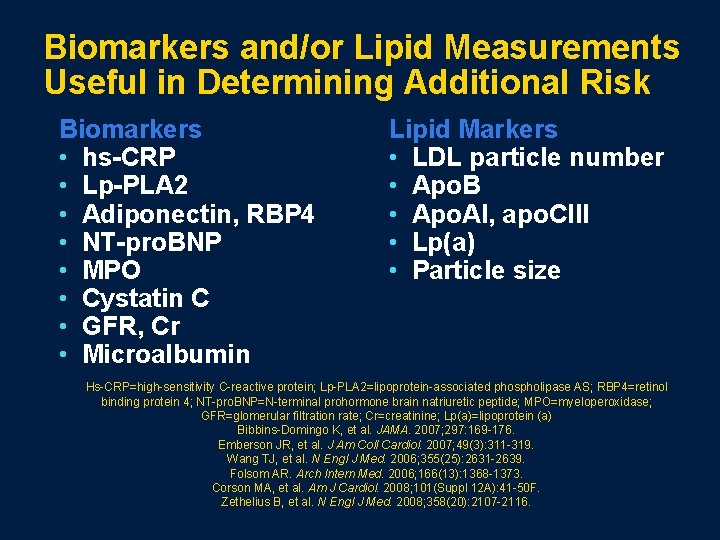
Biomarkers and/or Lipid Measurements Useful in Determining Additional Risk Biomarkers • hs-CRP • Lp-PLA 2 • Adiponectin, RBP 4 • NT-pro. BNP • MPO • Cystatin C • GFR, Cr • Microalbumin Lipid Markers • LDL particle number • Apo. B • Apo. AI, apo. CIII • Lp(a) • Particle size Hs-CRP=high-sensitivity C-reactive protein; Lp-PLA 2=lipoprotein-associated phospholipase AS; RBP 4=retinol binding protein 4; NT-pro. BNP=N-terminal prohormone brain natriuretic peptide; MPO=myeloperoxidase; GFR=glomerular filtration rate; Cr=creatinine; Lp(a)=lipoprotein (a) Bibbins-Domingo K, et al. JAMA. 2007; 297: 169 -176. Emberson JR, et al. J Am Coll Cardiol. 2007; 49(3): 311 -319. Wang TJ, et al. N Engl J Med. 2006; 355(25): 2631 -2639. Folsom AR. Arch Intern Med. 2006; 166(13): 1368 -1373. Corson MA, et al. Am J Cardiol. 2008; 101(Suppl 12 A): 41 -50 F. Zethelius B, et al. N Engl J Med. 2008; 358(20): 2107 -2116.
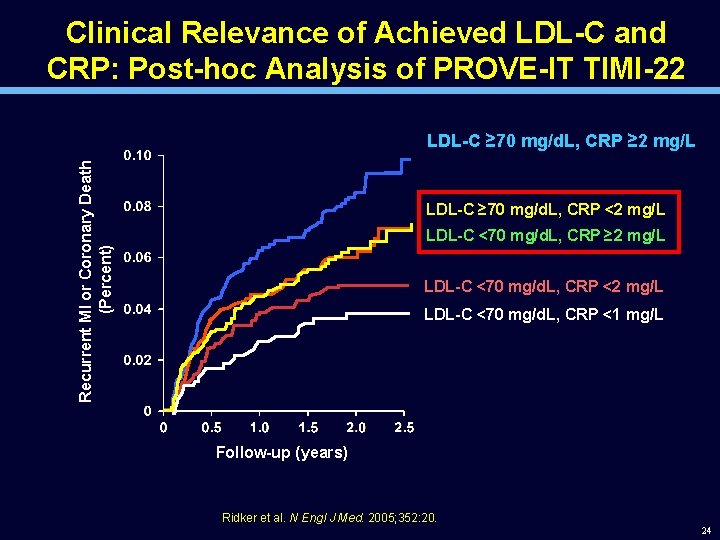
Clinical Relevance of Achieved LDL-C and CRP: Post-hoc Analysis of PROVE-IT TIMI-22 Recurrent MI or Coronary Death (Percent) LDL-C ≥ 70 mg/d. L, CRP ≥ 2 mg/L LDL-C ≥ 70 mg/d. L, CRP <2 mg/L LDL-C <70 mg/d. L, CRP ≥ 2 mg/L LDL-C <70 mg/d. L, CRP <1 mg/L Follow-up (years) Ridker et al. N Engl J Med. 2005; 352: 20. 24
Should LDL be lowered regardless of the baseline in high risk patients? 25
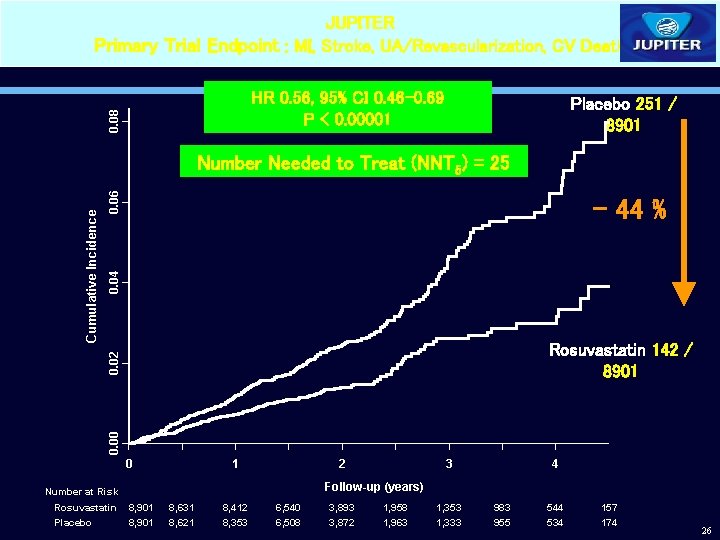
JUPITER Primary Trial Endpoint : MI, Stroke, UA/Revascularization, CV Death 0. 08 HR 0. 56, 95% CI 0. 46 -0. 69 P < 0. 00001 Placebo 251 / 8901 0. 06 0. 04 - 44 % Rosuvastatin 142 / 8901 0. 00 0. 02 Cumulative Incidence Number Needed to Treat (NNT 5) = 25 0 1 2 4 Follow-up (years) Number at Risk Rosuvastatin Placebo 3 8, 901 8, 631 8, 621 8, 412 8, 353 6, 540 6, 508 3, 893 3, 872 1, 958 1, 963 1, 353 1, 333 983 955 544 534 157 174 26
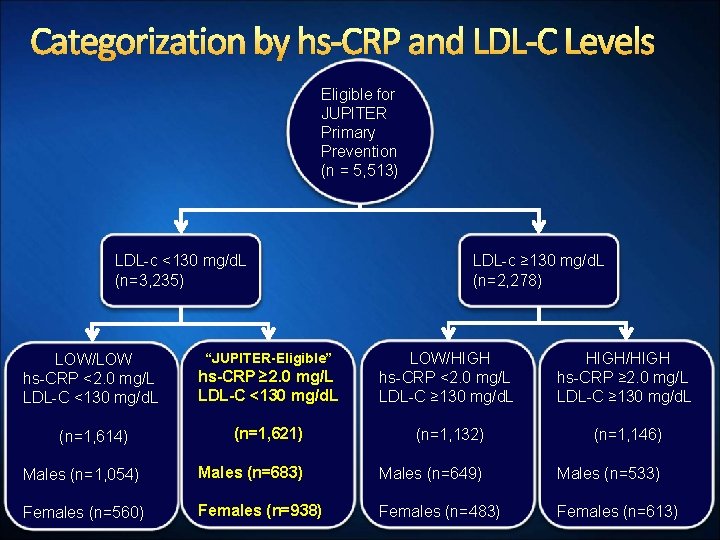
Categorization by hs-CRP and LDL-C Levels Eligible for JUPITER Primary Prevention (n = 5, 513) LDL-c <130 mg/d. L (n=3, 235) LDL-c ≥ 130 mg/d. L (n=2, 278) hs-CRP ≥ 2. 0 mg/L LDL-C <130 mg/d. L LOW/HIGH hs-CRP <2. 0 mg/L LDL-C ≥ 130 mg/d. L HIGH/HIGH hs-CRP ≥ 2. 0 mg/L LDL-C ≥ 130 mg/d. L (n=1, 621) (n=1, 132) (n=1, 146) Males (n=1, 054) Males (n=683) Males (n=649) Males (n=533) Females (n=560) Females (n=938) Females (n=483) Females (n=613) LOW/LOW hs-CRP <2. 0 mg/L LDL-C <130 mg/d. L (n=1, 614) “JUPITER-Eligible”
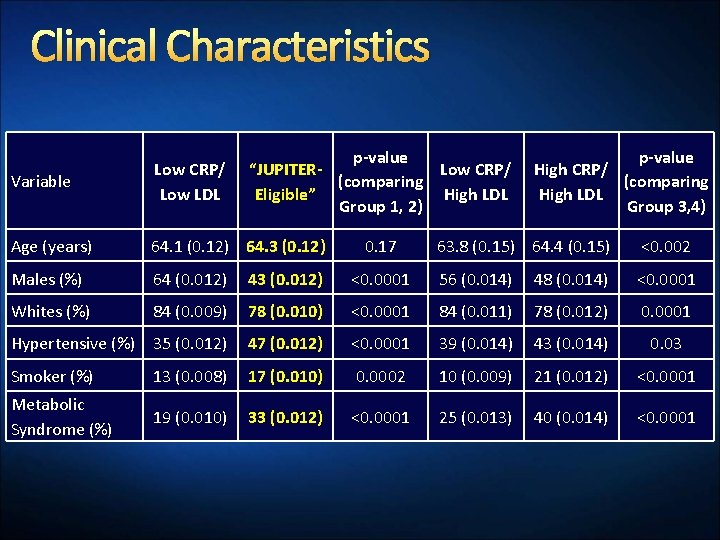
Clinical Characteristics p-value “JUPITERLow CRP/ (comparing Eligible” High LDL Group 1, 2) Variable Low CRP/ Low LDL Age (years) 64. 1 (0. 12) 64. 3 (0. 12) Males (%) 64 (0. 012) 43 (0. 012) Whites (%) 84 (0. 009) 0. 17 p-value High CRP/ (comparing High LDL Group 3, 4) 63. 8 (0. 15) 64. 4 (0. 15) <0. 002 <0. 0001 56 (0. 014) 48 (0. 014) <0. 0001 78 (0. 010) <0. 0001 84 (0. 011) 78 (0. 012) 0. 0001 Hypertensive (%) 35 (0. 012) 47 (0. 012) <0. 0001 39 (0. 014) 43 (0. 014) 0. 03 Smoker (%) 13 (0. 008) 17 (0. 010) 0. 0002 10 (0. 009) 21 (0. 012) <0. 0001 Metabolic Syndrome (%) 19 (0. 010) 33 (0. 012) <0. 0001 25 (0. 013) 40 (0. 014) <0. 0001
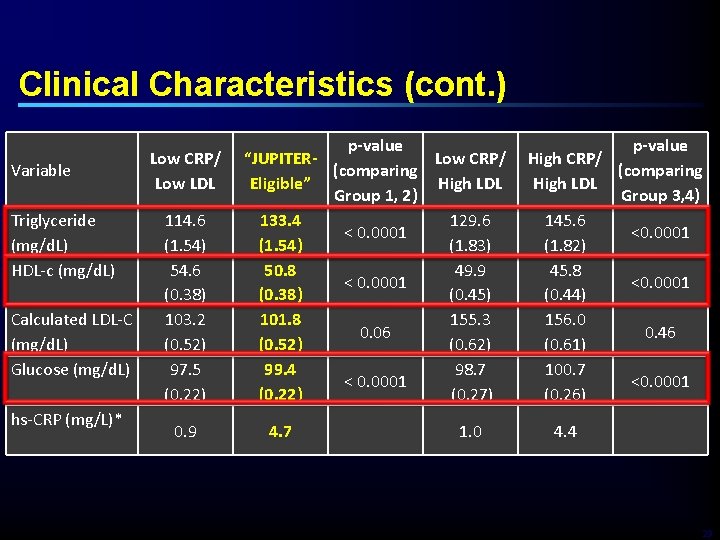
Clinical Characteristics (cont. ) Variable Triglyceride (mg/d. L) HDL-c (mg/d. L) Calculated LDL-C (mg/d. L) Glucose (mg/d. L) hs-CRP (mg/L)* Low CRP/ Low LDL 114. 6 (1. 54) 54. 6 (0. 38) 103. 2 (0. 52) 97. 5 (0. 22) 0. 9 p-value “JUPITERLow CRP/ (comparing Eligible” High LDL Group 1, 2) 133. 4 129. 6 < 0. 0001 (1. 54) (1. 83) 50. 8 49. 9 < 0. 0001 (0. 38) (0. 45) 101. 8 155. 3 0. 06 (0. 52) (0. 62) 99. 4 98. 7 < 0. 0001 (0. 22) (0. 27) 4. 7 1. 0 p-value High CRP/ (comparing High LDL Group 3, 4) 145. 6 <0. 0001 (1. 82) 45. 8 <0. 0001 (0. 44) 156. 0 0. 46 (0. 61) 100. 7 <0. 0001 (0. 26) 4. 4 29
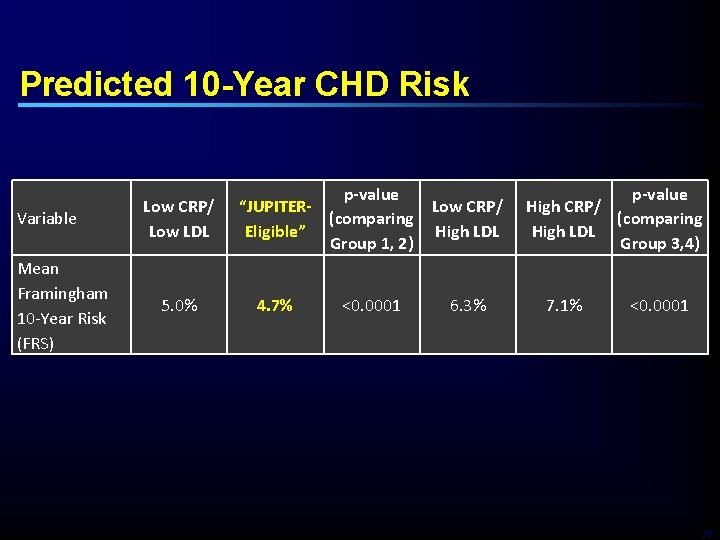
Predicted 10 -Year CHD Risk Variable Mean Framingham 10 -Year Risk (FRS) Low CRP/ Low LDL 5. 0% p-value “JUPITERLow CRP/ (comparing Eligible” High LDL Group 1, 2) 4. 7% <0. 0001 6. 3% p-value High CRP/ (comparing High LDL Group 3, 4) 7. 1% <0. 0001 30
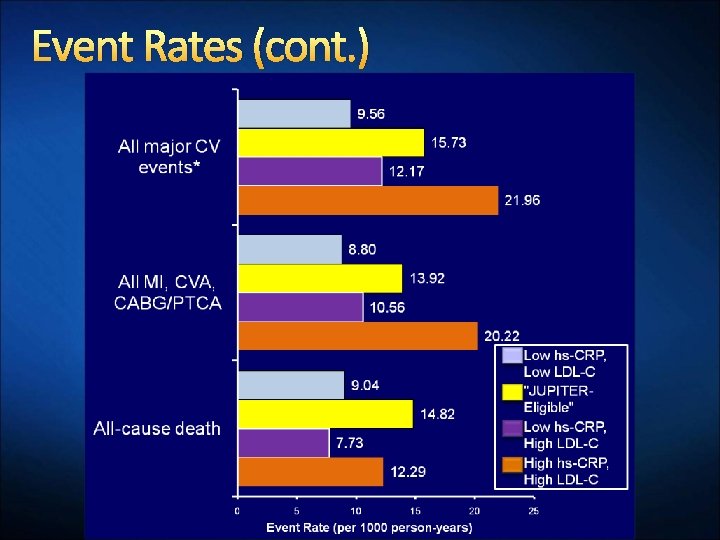
Event Rates (cont. )
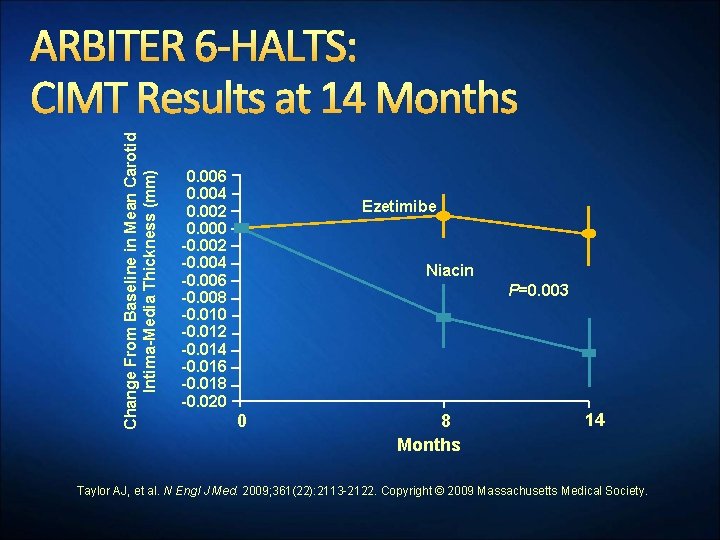
Change From Baseline in Mean Carotid Intima-Media Thickness (mm) ARBITER 6 -HALTS: CIMT Results at 14 Months 0. 006 0. 004 0. 002 0. 000 -0. 002 -0. 004 -0. 006 -0. 008 -0. 010 -0. 012 -0. 014 -0. 016 -0. 018 -0. 020 Ezetimibe Niacin P=0. 003 0 8 Months 14 Taylor AJ, et al. N Engl J Med. 2009; 361(22): 2113 -2122. Copyright © 2009 Massachusetts Medical Society.

Evolution of Lipid Guidelines Current and Future- Targets TARGET Statin monotherapy LDL-C HDL-C The Lower The Better TG TARGET ATP I, ATP III Comprehensive is the Best ATP IV ? ? (FIELD, JUPITER ACCORD, etc…. . ) LIKELY TO: ØConfirm Top Priority: LDL-C HDL-C - Combination therapy TG ATP III update, IDF ESC, EASD, ADA, NICE intensive LDL-C reduction to achieve goals ØReinforce: HDL and TG as secondary therapeutic targets (i. e. in T 2 DM, Met. S) Ø New Markers of High CV Risk: Apo B? Hs-CRP? . . .
Conclusions · Achievement of LDL-C and Non-HDL-C should be the primary goal of lipid therapy for patients with diabetes and metabolic syndrome and the lower the better · Lifetime low LDL levels are associated with a marked reduction of CVD events · In the US population with a growing prevalence of metabolic syndrome and obesity, non-HDL/Apo. B is more predictive of CVD than LDL-c · In patients at high risk (CVD, diabetes, elevated CRP), LDL reduction with statins has proven outome benefits regardless of baseline LDL-c levels 34
- Slides: 33