What Pediatric Primary Care Providers Need to Know



- Slides: 56
What Pediatric Primary Care Providers Need to Know About Medication Assisted Therapy for Adolescent Opioid Addiction • Diana Deister, MS, MD • Child and Adolescent Psychiatrist • Adolescent Substance Use and Addictions Program • Division of Developmental Medicine Boston Children’s Hospital • October 24 th, 2017 1
Disclosure Diana Deister, MS, MD has no relationships with commercial companies to disclose. 2
Learning outcomes • Review the neurobiology of opioids • Review the epidemiology of opioid use in adolescents and opioid related deaths in MA • Review the evidence for appropriate use of medicationassisted therapy (MAT) for opioid use disorders in adolescents • Understand how to monitor patients on MAT even if they are receiving MAT elsewhere 3
4
Opiates Oxy co d 20 m one g Opioids 5
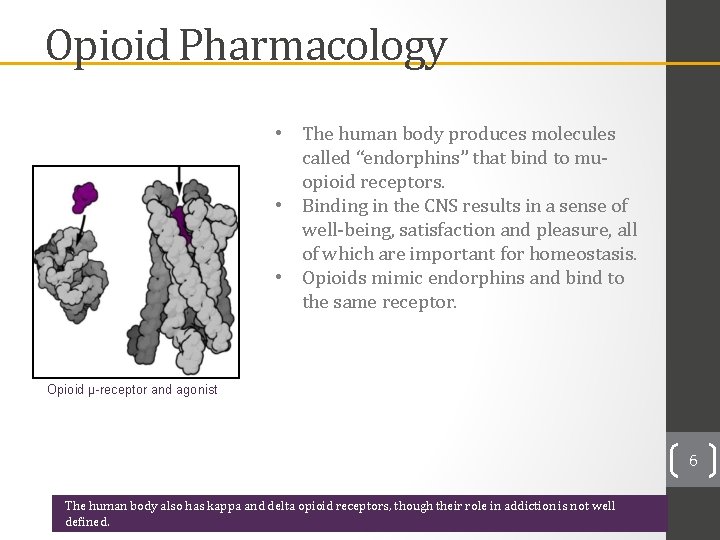
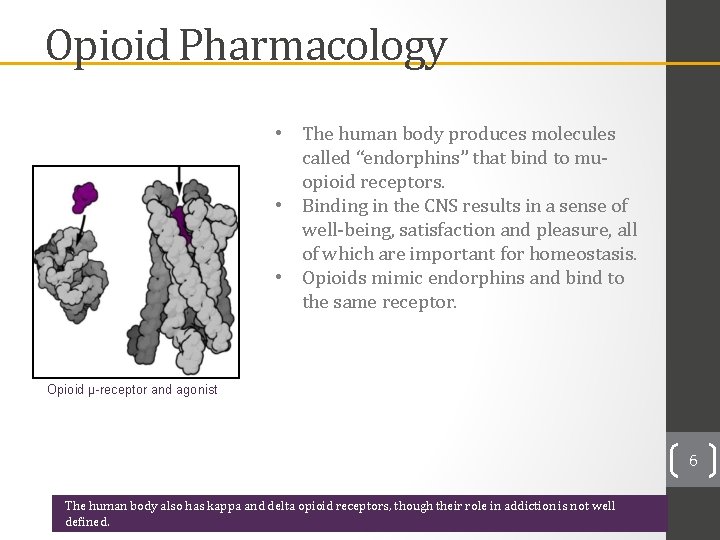
Opioid Pharmacology • The human body produces molecules called “endorphins” that bind to muopioid receptors. • Binding in the CNS results in a sense of well-being, satisfaction and pleasure, all of which are important for homeostasis. • Opioids mimic endorphins and bind to the same receptor. Opioid µ-receptor and agonist 6 The human body also has kappa and delta opioid receptors, though their role in addiction is not well defined.
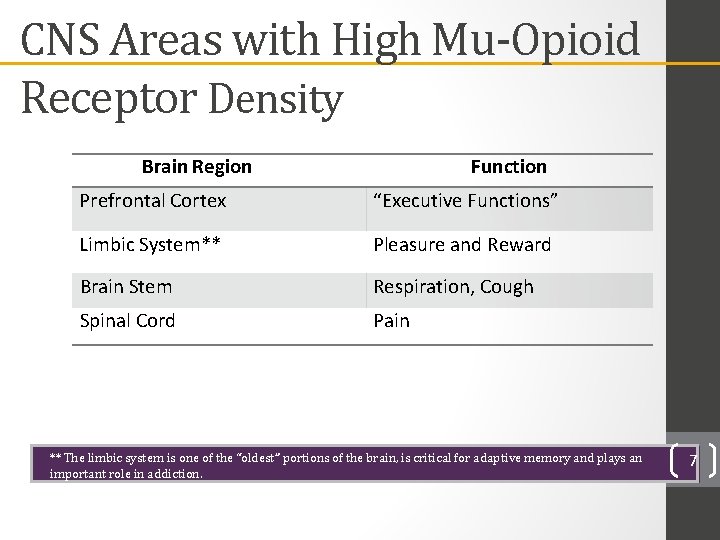
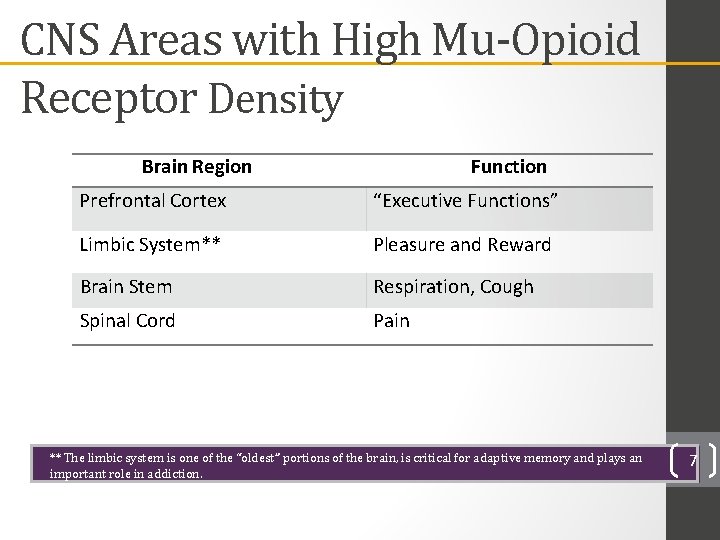
CNS Areas with High Mu-Opioid Receptor Density Brain Region Function Prefrontal Cortex “Executive Functions” Limbic System** Pleasure and Reward Brain Stem Respiration, Cough Spinal Cord Pain ** The limbic system is one of the “oldest” portions of the brain, is critical for adaptive memory and plays an important role in addiction. 7
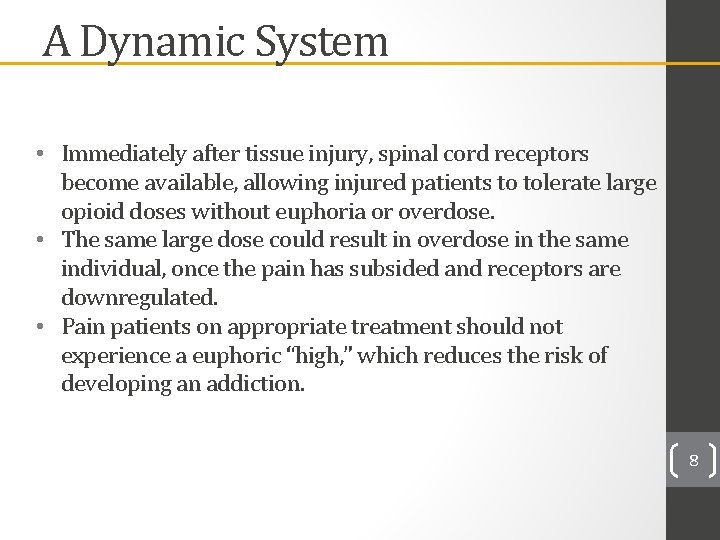
A Dynamic System • Immediately after tissue injury, spinal cord receptors become available, allowing injured patients to tolerate large opioid doses without euphoria or overdose. • The same large dose could result in overdose in the same individual, once the pain has subsided and receptors are downregulated. • Pain patients on appropriate treatment should not experience a euphoric “high, ” which reduces the risk of developing an addiction. 8
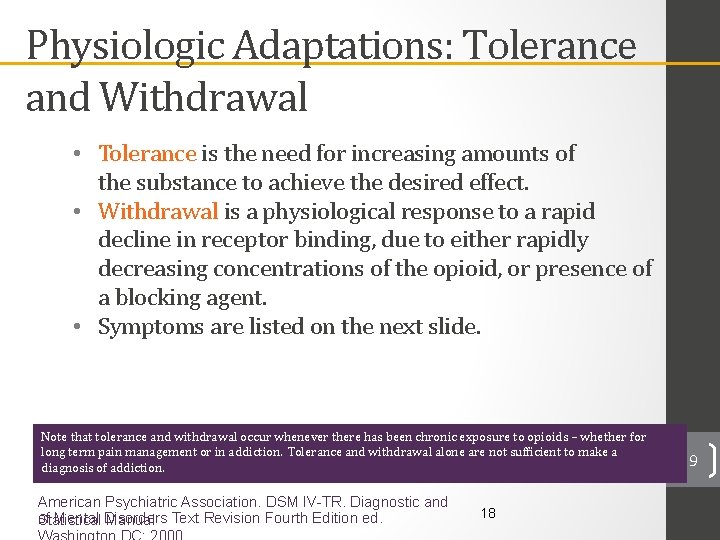
Physiologic Adaptations: Tolerance and Withdrawal • Tolerance is the need for increasing amounts of the substance to achieve the desired effect. • Withdrawal is a physiological response to a rapid decline in receptor binding, due to either rapidly decreasing concentrations of the opioid, or presence of a blocking agent. • Symptoms are listed on the next slide. Note that tolerance and withdrawal occur whenever there has been chronic exposure to opioids – whether for long term pain management or in addiction. Tolerance and withdrawal alone are not sufficient to make a diagnosis of addiction. . American Psychiatric Association. DSM IV-TR. Diagnostic and of Mental Disorders Statistical Manual Text Revision Fourth Edition ed. 18 9
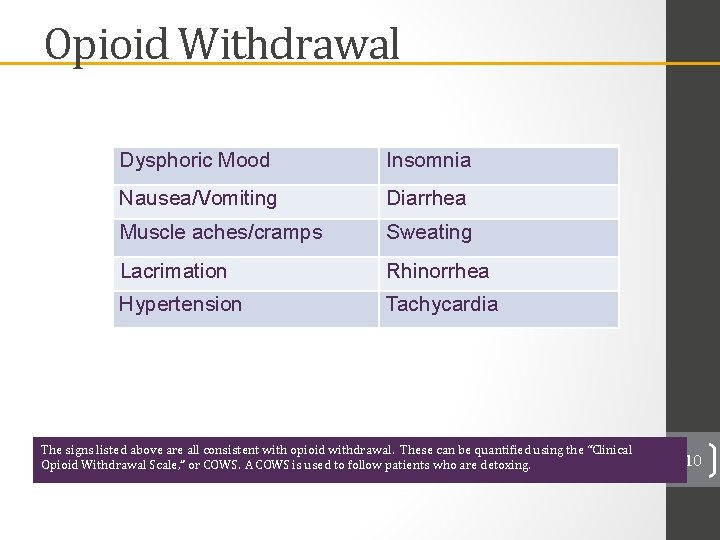
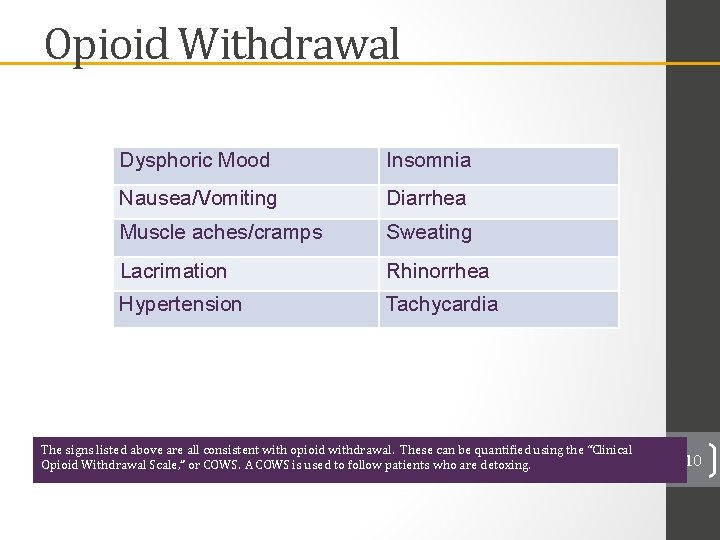
Opioid Withdrawal Dysphoric Mood Insomnia Nausea/Vomiting Diarrhea Muscle aches/cramps Sweating Lacrimation Rhinorrhea Hypertension Tachycardia The signs listed above are all consistent with opioid withdrawal. These can be quantified using the “Clinical Opioid Withdrawal Scale, ” or COWS. A COWS is used to follow patients who are detoxing. 10
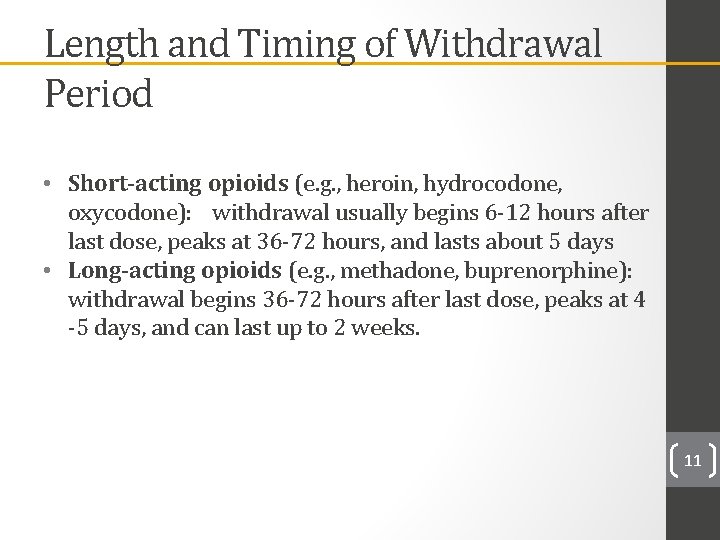
Length and Timing of Withdrawal Period • Short-acting opioids (e. g. , heroin, hydrocodone, oxycodone): withdrawal usually begins 6 -12 hours after last dose, peaks at 36 -72 hours, and lasts about 5 days • Long-acting opioids (e. g. , methadone, buprenorphine): withdrawal begins 36 -72 hours after last dose, peaks at 4 -5 days, and can last up to 2 weeks. 11
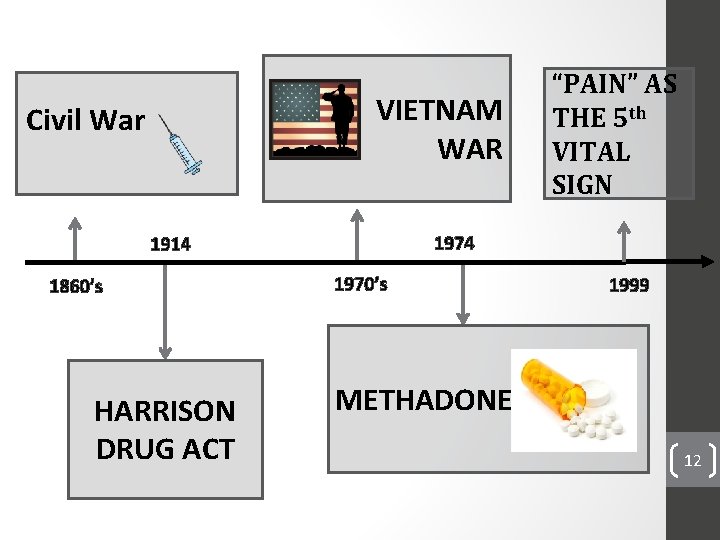
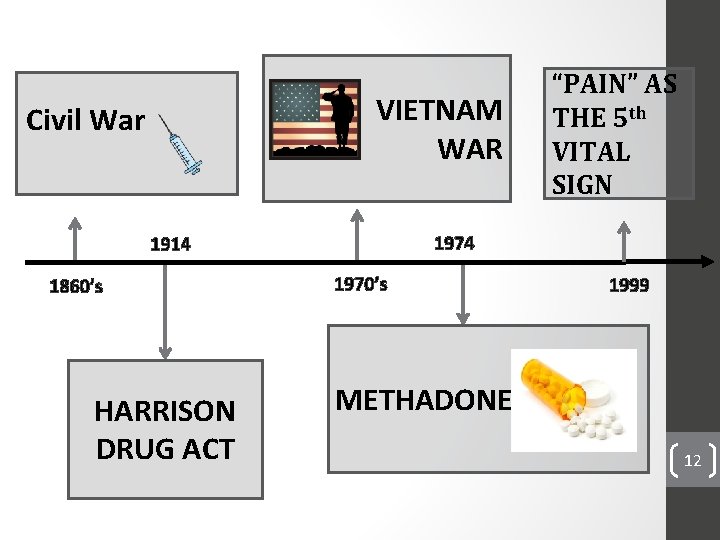
VIETNAM WAR Civil War 1974 1914 1860’s HARRISON DRUG ACT “PAIN” AS THE 5 th VITAL SIGN 1970’s 1999 METHADONE 12
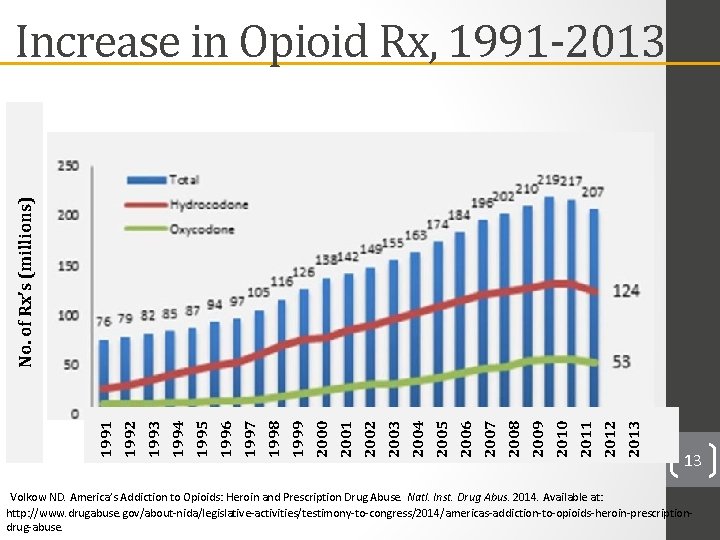
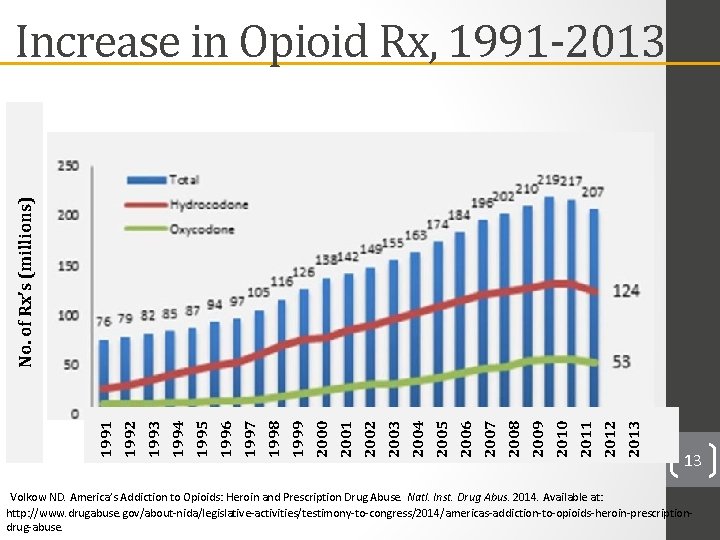
2001 2002 2003 2004 2005 2006 2007 2008 2009 2010 2011 2012 2013 1994 1995 1996 1997 1998 1999 2000 1992 1991 No. of Rx’s (millions) Increase in Opioid Rx, 1991 -2013 Volkow ND. America’s Addiction to Opioids: Heroin and Prescription Drug Abuse. Natl. Inst. Drug Abus. 2014. Available at: 13 http: //www. drugabuse. gov/about-nida/legislative-activities/testimony-to-congress/2014/americas-addiction-to-opioids-heroin-prescriptiondrug-abuse.
Monitoring the Future 2015 survey
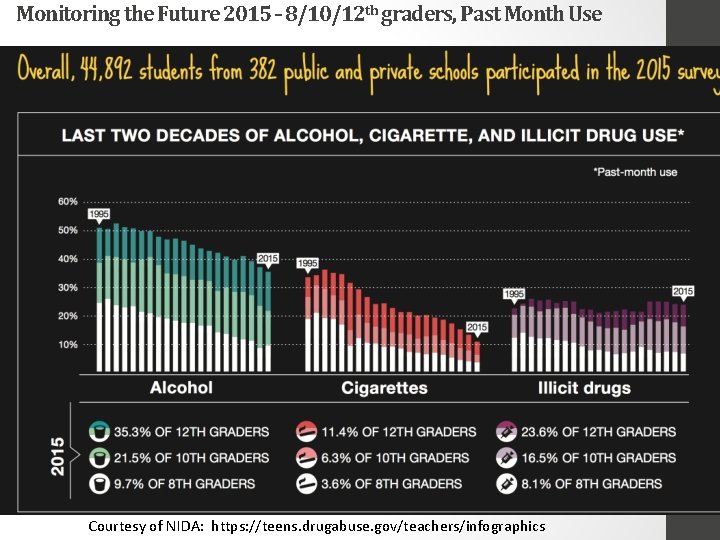
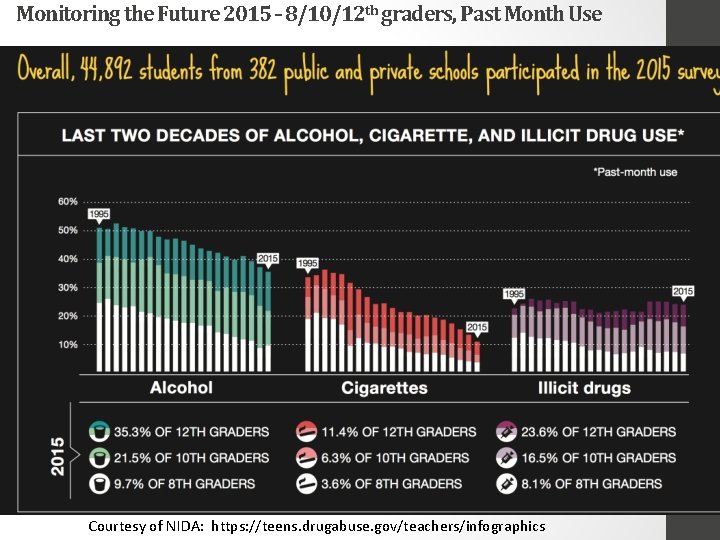
Monitoring the Future 2015 – 8/10/12 th graders, Past Month Use Courtesy of NIDA: https: //teens. drugabuse. gov/teachers/infographics
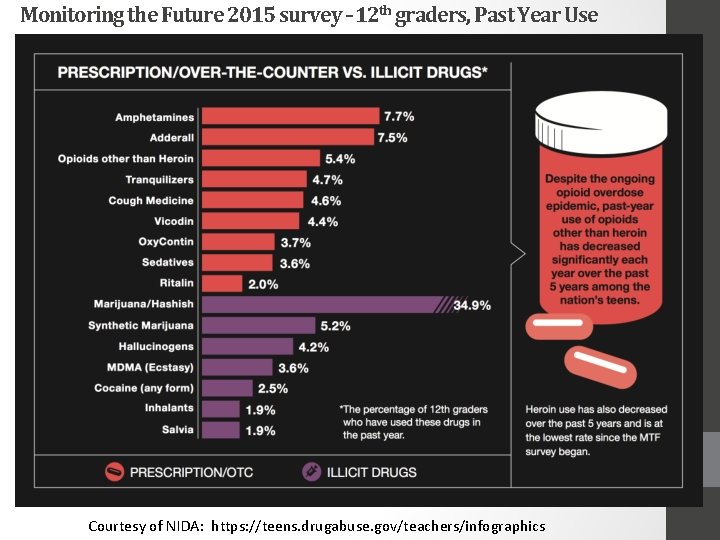
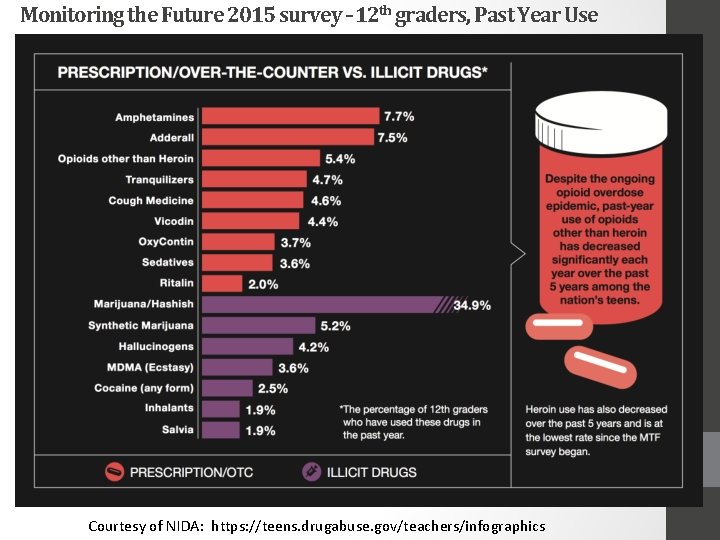
Monitoring the Future 2015 survey – 12 th graders, Past Year Use Courtesy of NIDA: https: //teens. drugabuse. gov/teachers/infographics
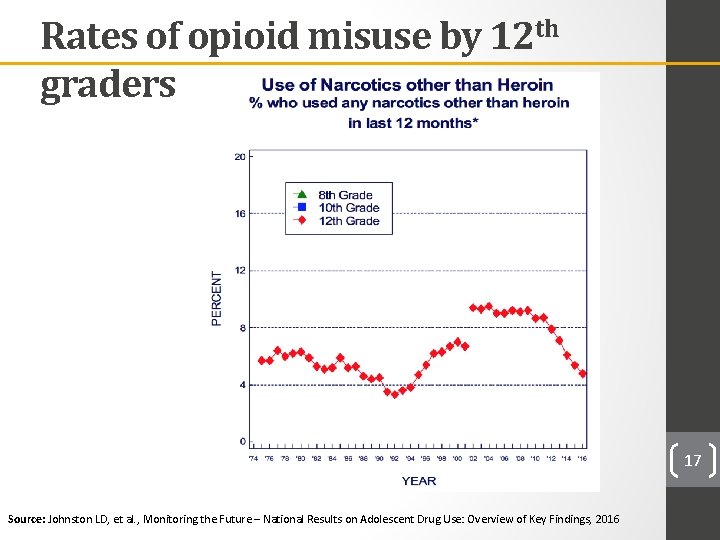
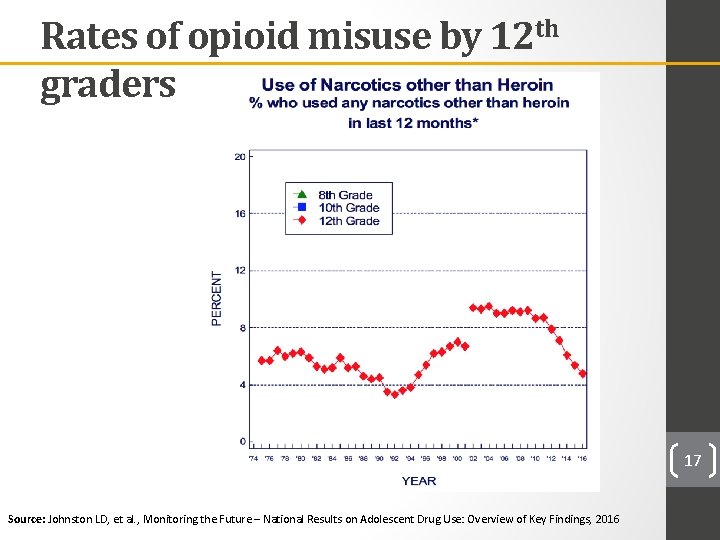
Rates of opioid misuse by 12 th graders 17 Source: Johnston LD, et al. , Monitoring the Future – National Results on Adolescent Drug Use: Overview of Key Findings, 2016

Mass Opioid Death Rate

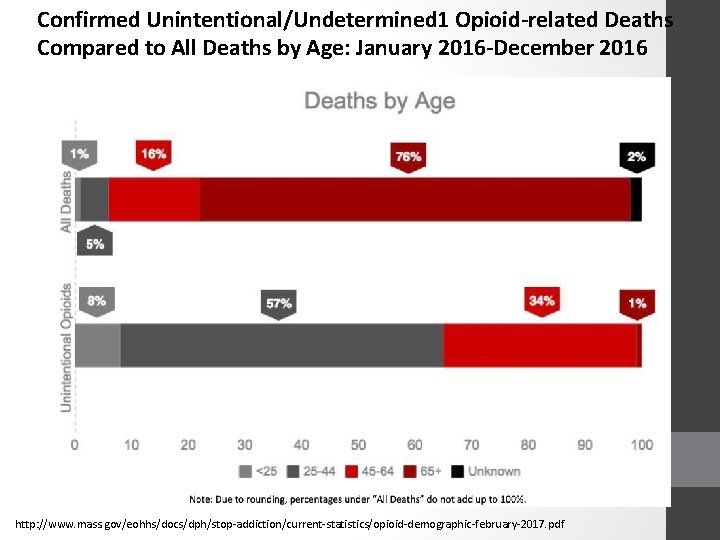
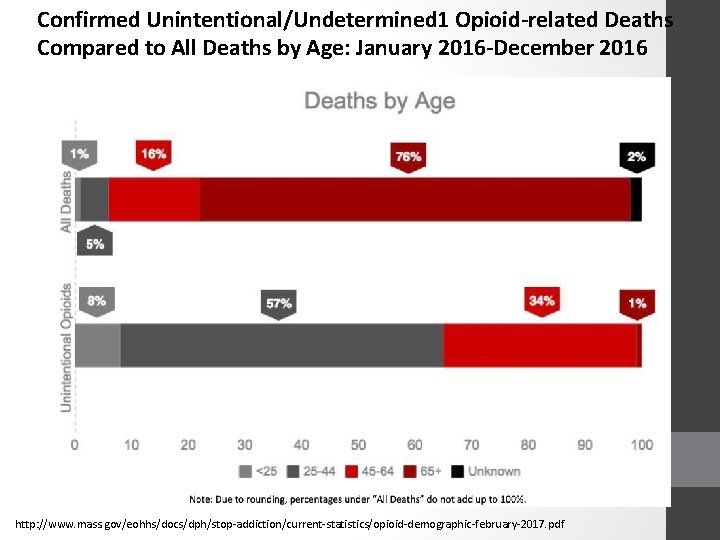
Confirmed Unintentional/Undetermined 1 Opioid-related Deaths Compared to All Deaths by Age: January 2016 -December 2016 http: //www. mass. gov/eohhs/docs/dph/stop-addiction/current-statistics/opioid-demographic-february-2017. pdf
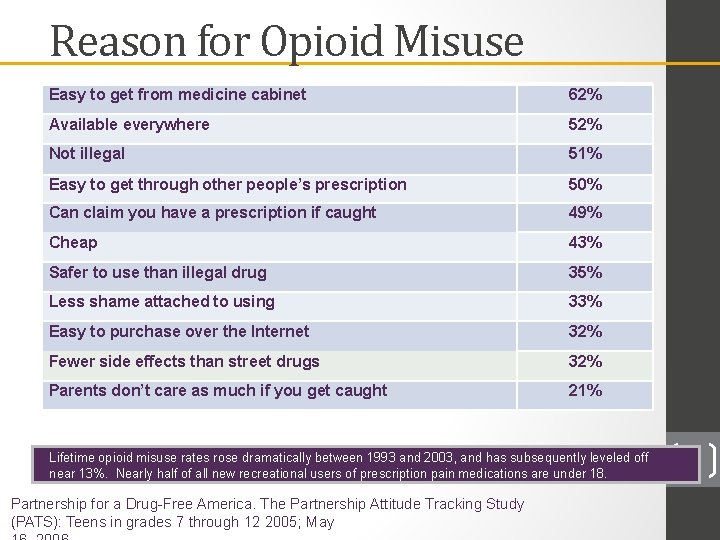
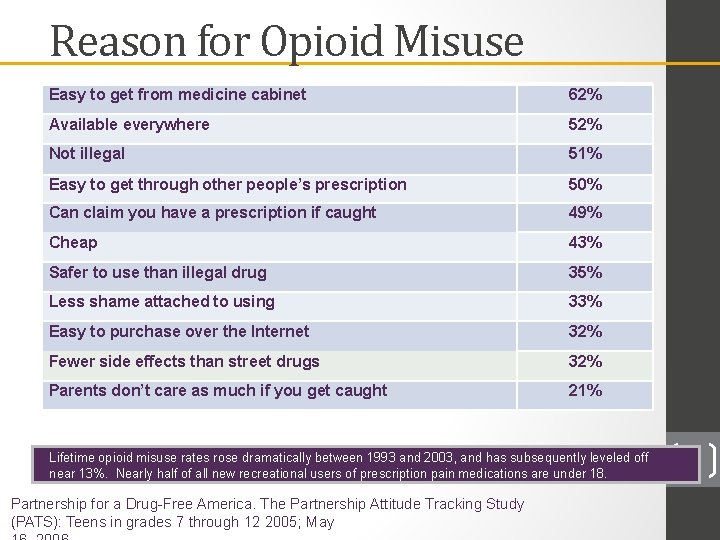
Reason for Opioid Misuse Easy to get from medicine cabinet 62% Available everywhere 52% Not illegal 51% Easy to get through other people’s prescription 50% Can claim you have a prescription if caught 49% Cheap 43% Safer to use than illegal drug 35% Less shame attached to using 33% Easy to purchase over the Internet 32% Fewer side effects than street drugs 32% Parents don’t care as much if you get caught 21% Lifetime opioid misuse rates rose dramatically between 1993 and 2003, and has subsequently leveled off near 13%. Nearly half of all new recreational users of prescription pain medications are under 18. Partnership for a Drug-Free America. The Partnership Attitude Tracking Study (PATS): Teens in grades 7 through 12 2005; May 22
Heroin • Heroin (di-acetyl morphine) rapidly crosses the blood brain barrier, where it is metabolized to morphine, resulting in very rapid delivery of morphine to the central nervous system. • Because it is potent and relatively inexpensive, individuals who have become addicted to opioids may switch to heroin to combat tolerance • Increased purity of heroin since the 1990 s has made snorting or smoking practical alternatives to injecting, thus lowering the barrier to initiate use. 23
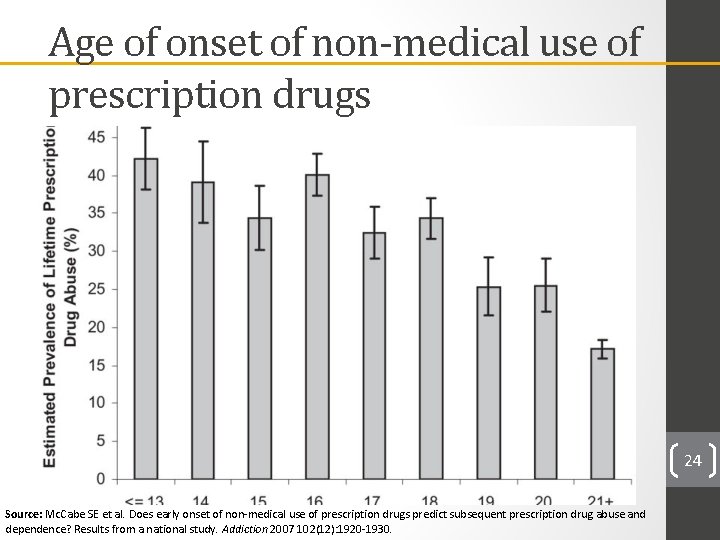
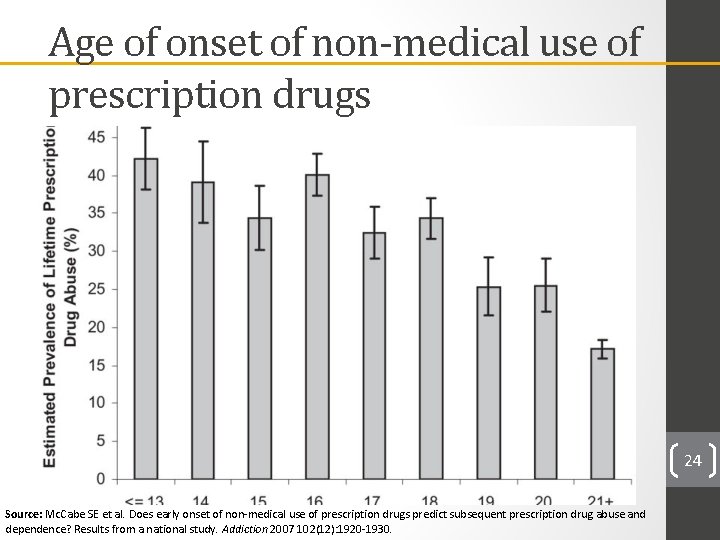
Age of onset of non-medical use of prescription drugs 24 Source: Mc. Cabe SE et al. Does early onset of non-medical use of prescription drugs predict subsequent prescription drug abuse and dependence? Results from a national study. Addiction 2007 102(12): 1920 -1930.
Prescribed opioid use Opioid misuse
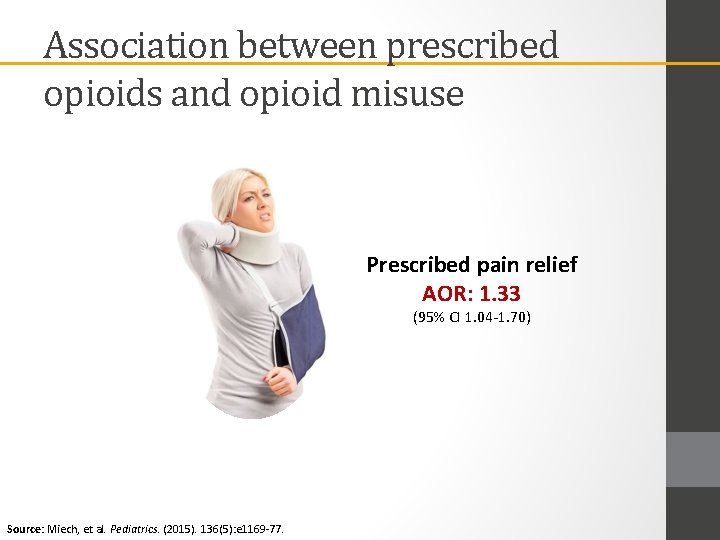
Association between prescribed opioids and opioid misuse Prescribed pain relief AOR: 1. 33 (95% CI 1. 04 -1. 70) Source: Miech, et al. Pediatrics. (2015). 136(5): e 1169 -77.
Prescribed opioid use Opioid misuse Alc/MJ/tobacco use
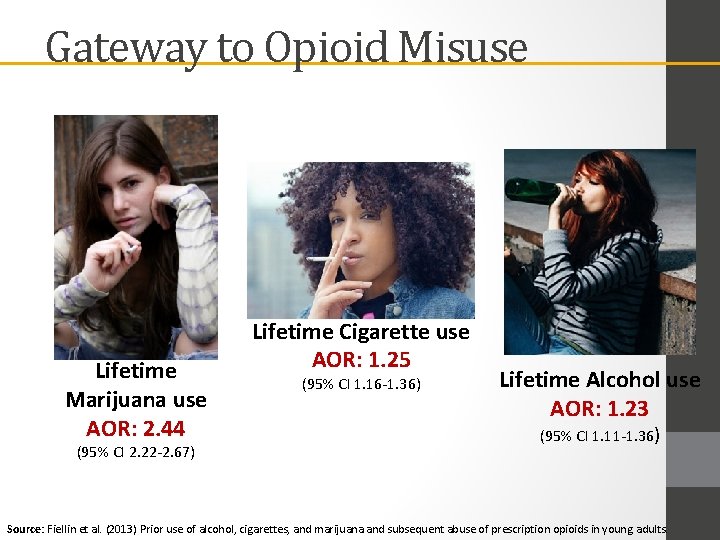
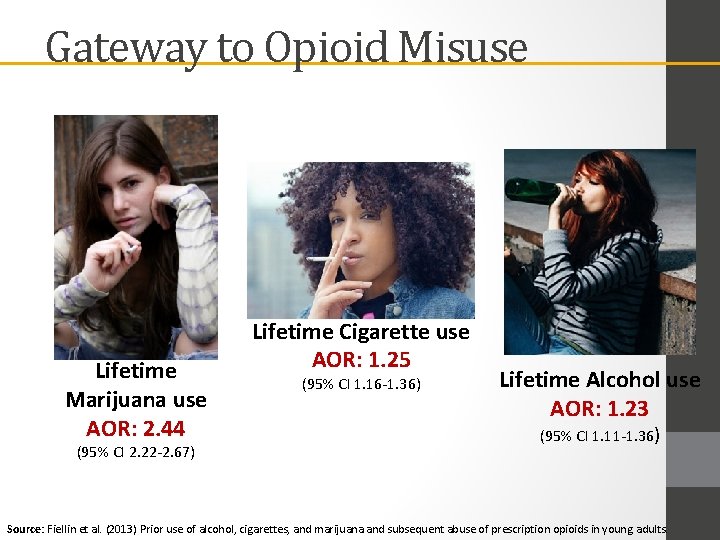
Gateway to Opioid Misuse Lifetime Marijuana use AOR: 2. 44 (95% CI 2. 22 -2. 67) Lifetime Cigarette use AOR: 1. 25 (95% CI 1. 16 -1. 36) Lifetime Alcohol use AOR: 1. 23 (95% CI 1. 11 -1. 36) Source: Fiellin et al. (2013) Prior use of alcohol, cigarettes, and marijuana and subsequent abuse of prescription opioids in young adults.
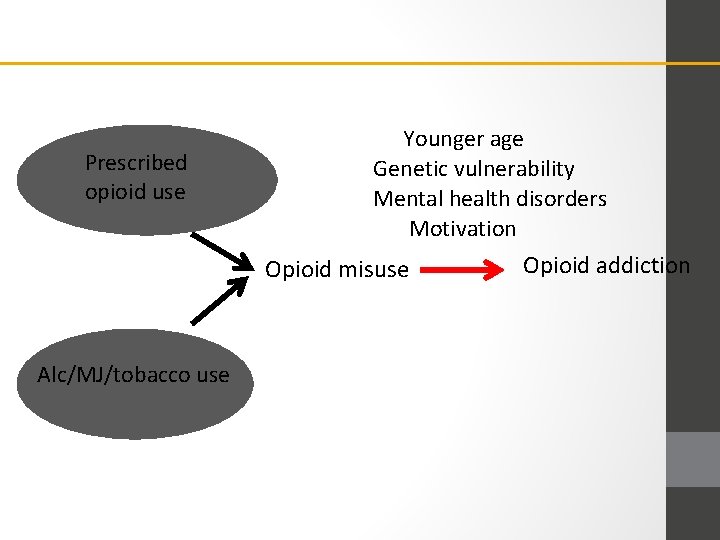
Prescribed opioid use Younger age Genetic vulnerability Mental health disorders Motivation Opioid misuse Alc/MJ/tobacco use Opioid addiction
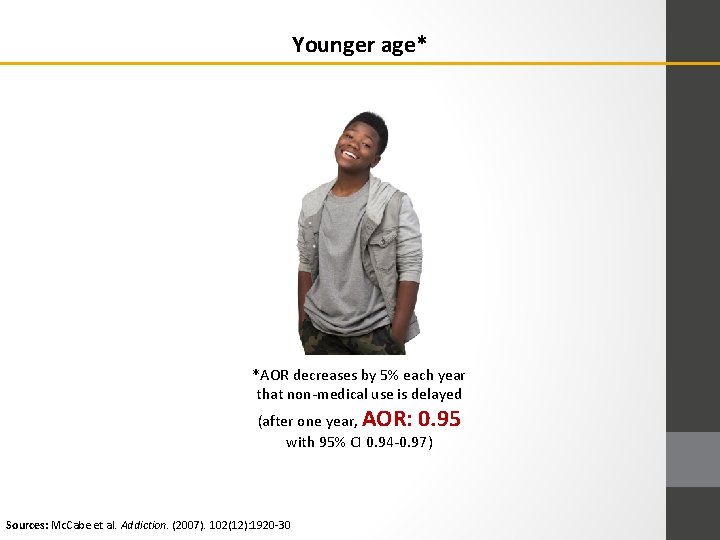
Younger age* *AOR decreases by 5% each year that non-medical use is delayed (after one year, AOR: 0. 95 with 95% CI 0. 94 -0. 97) Sources: Mc. Cabe et al. Addiction. (2007). 102(12): 1920 -30
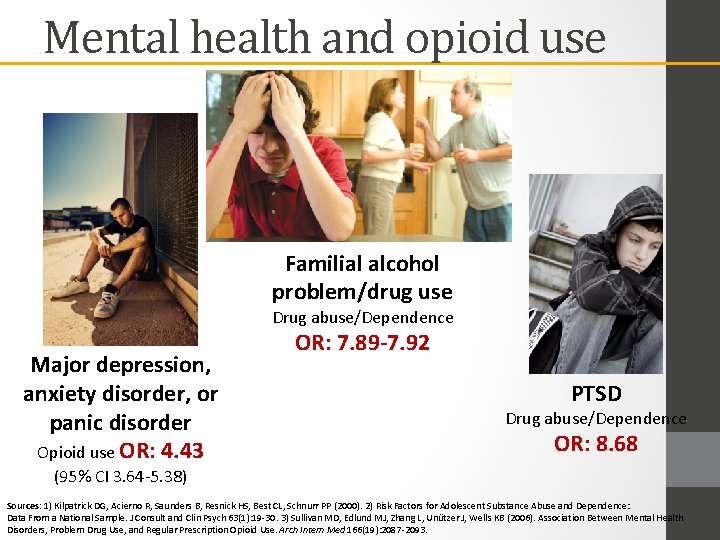
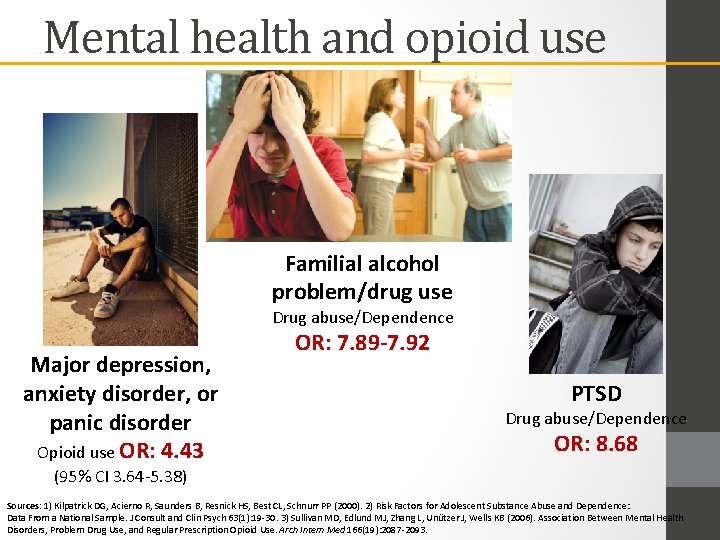
Mental health and opioid use Familial alcohol problem/drug use Drug abuse/Dependence Major depression, anxiety disorder, or panic disorder Opioid use OR: 4. 43 OR: 7. 89 -7. 92 PTSD Drug abuse/Dependence OR: 8. 68 (95% CI 3. 64 -5. 38) Sources: 1) Kilpatrick DG, Acierno R, Saunders B, Resnick HS, Best CL, Schnurr PP (2000). 2) Risk Factors for Adolescent Substance Abuse and Dependence: Data From a National Sample. J Consult and Clin Psych 63(1): 19 -30. 3) Sullivan MD, Edlund MJ, Zhang L, Unützer J, Wells KB (2006). Association Between Mental Health Disorders, Problem Drug Use, and Regular Prescription Opioid Use. Arch Intern Med 166(19): 2087 -2093.
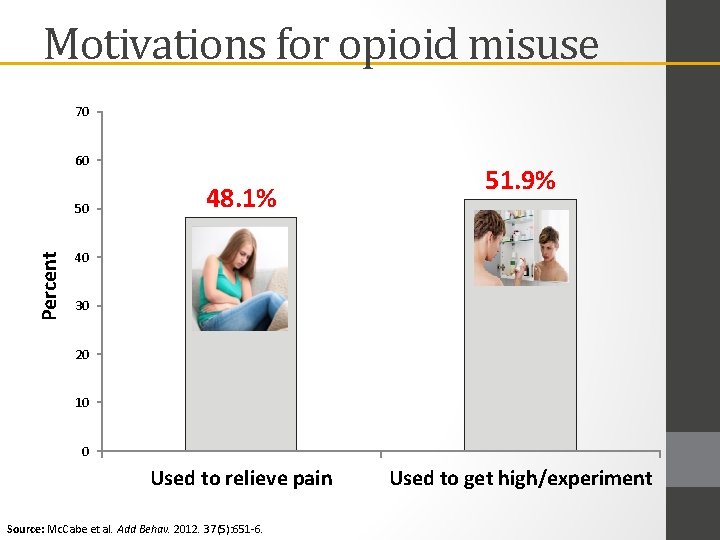
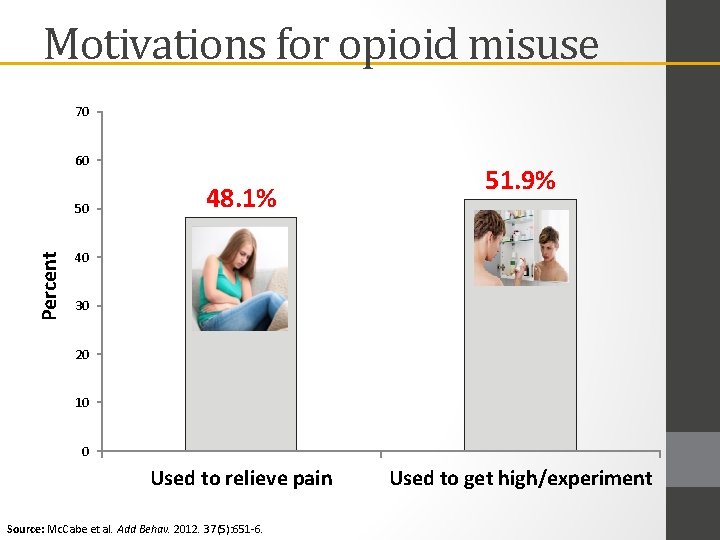
Motivations for opioid misuse 70 60 Percent 50 48. 1% 51. 9% 40 30 20 10 0 Used to relieve pain Source: Mc. Cabe et al. Add Behav. 2012. 37(5): 651 -6. Used to get high/experiment
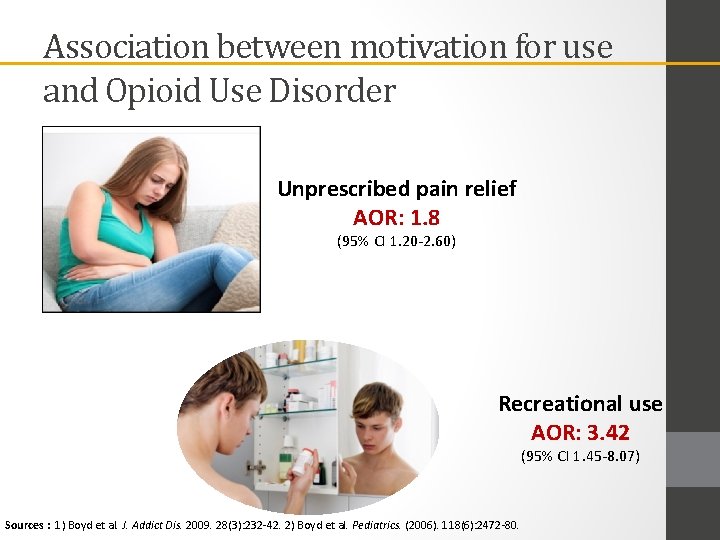
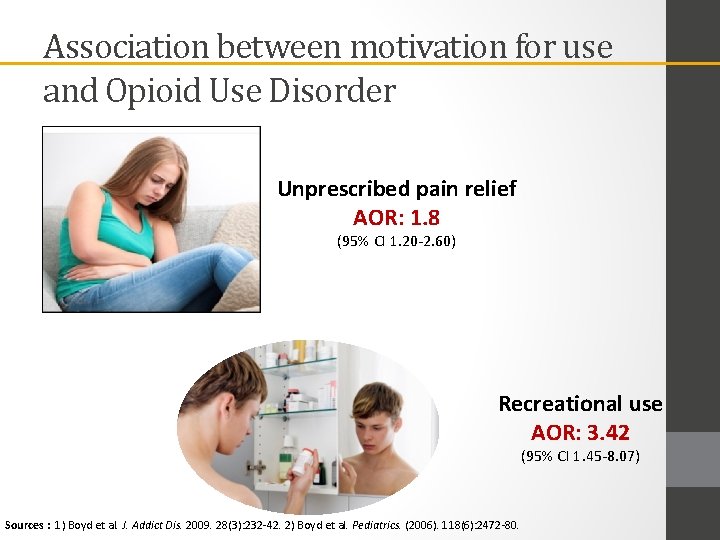
Association between motivation for use and Opioid Use Disorder Unprescribed pain relief AOR: 1. 8 (95% CI 1. 20 -2. 60) Recreational use AOR: 3. 42 (95% CI 1. 45 -8. 07) Sources : 1) Boyd et al. J. Addict Dis. 2009. 28(3): 232 -42. 2) Boyd et al. Pediatrics. (2006). 118(6): 2472 -80.
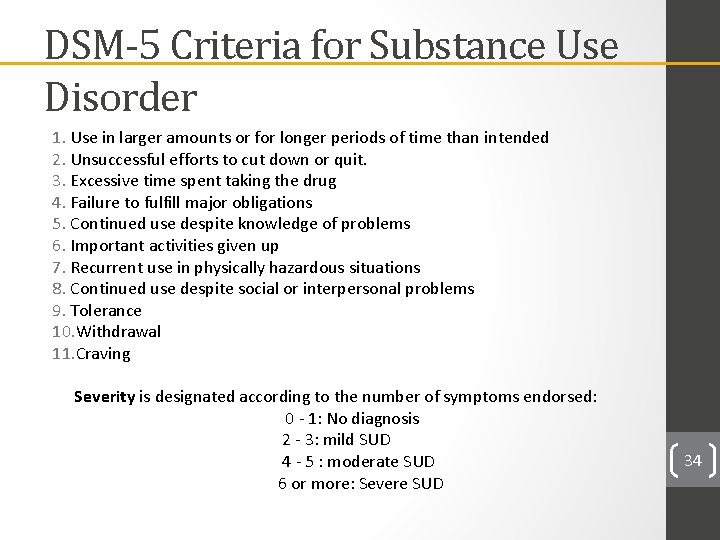
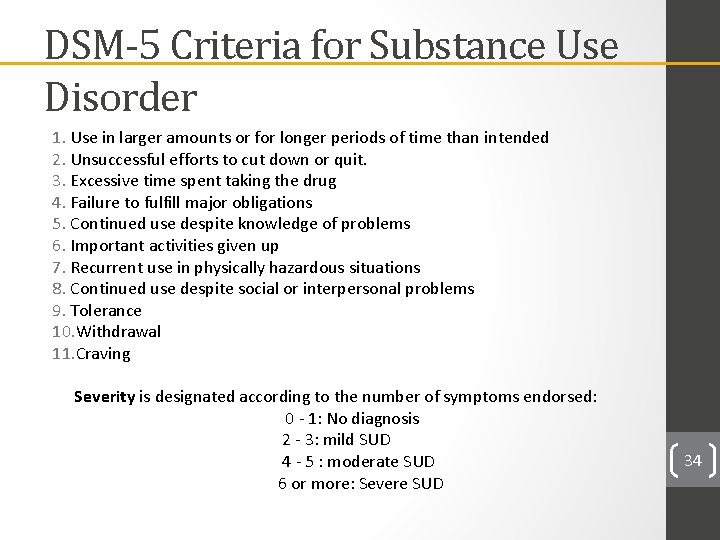
DSM-5 Criteria for Substance Use Disorder 1. Use in larger amounts or for longer periods of time than intended 2. Unsuccessful efforts to cut down or quit. 3. Excessive time spent taking the drug 4. Failure to fulfill major obligations 5. Continued use despite knowledge of problems 6. Important activities given up 7. Recurrent use in physically hazardous situations 8. Continued use despite social or interpersonal problems 9. Tolerance 10. Withdrawal 11. Craving Severity is designated according to the number of symptoms endorsed: 0 - 1: No diagnosis 2 - 3: mild SUD 4 - 5 : moderate SUD 6 or more: Severe SUD 34
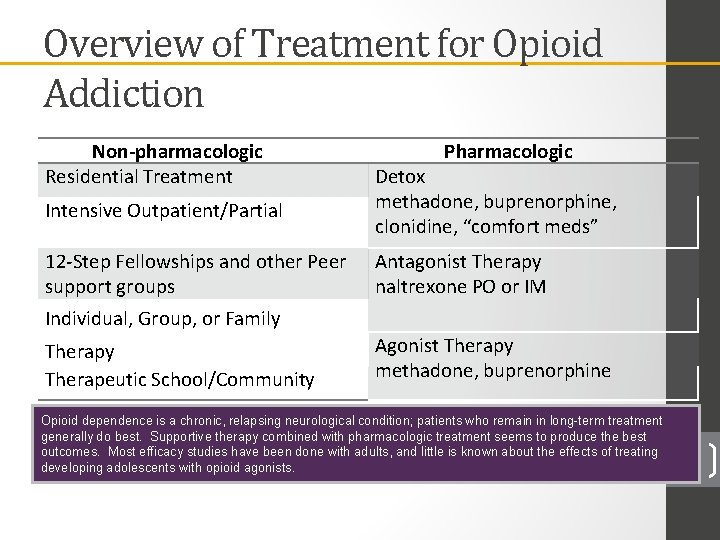
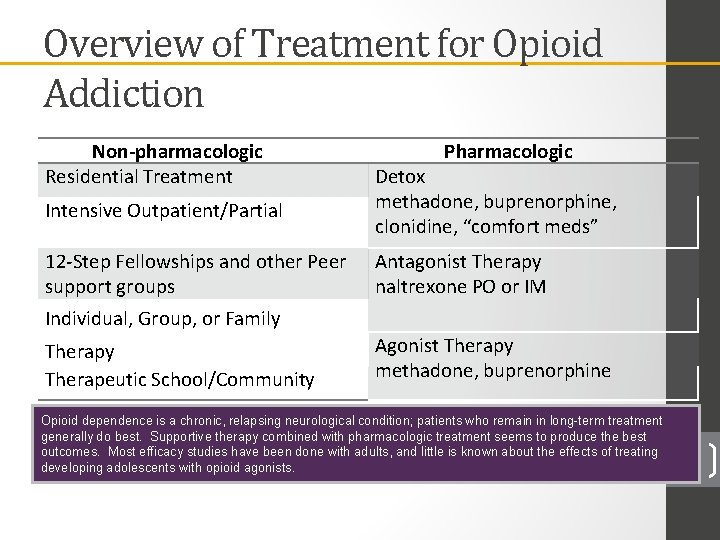
Overview of Treatment for Opioid Addiction Non-pharmacologic Residential Treatment Intensive Outpatient/Partial Pharmacologic Detox methadone, buprenorphine, clonidine, “comfort meds” 12 -Step Fellowships and other Peer support groups Individual, Group, or Family Antagonist Therapy naltrexone PO or IM Therapy Therapeutic School/Community Agonist Therapy methadone, buprenorphine Opioid dependence is a chronic, relapsing neurological condition; patients who remain in long-term treatment generally do best. Supportive therapy combined with pharmacologic treatment seems to produce the best outcomes. Most efficacy studies have been done with adults, and little is known about the effects of treating developing adolescents with opioid agonists. 35
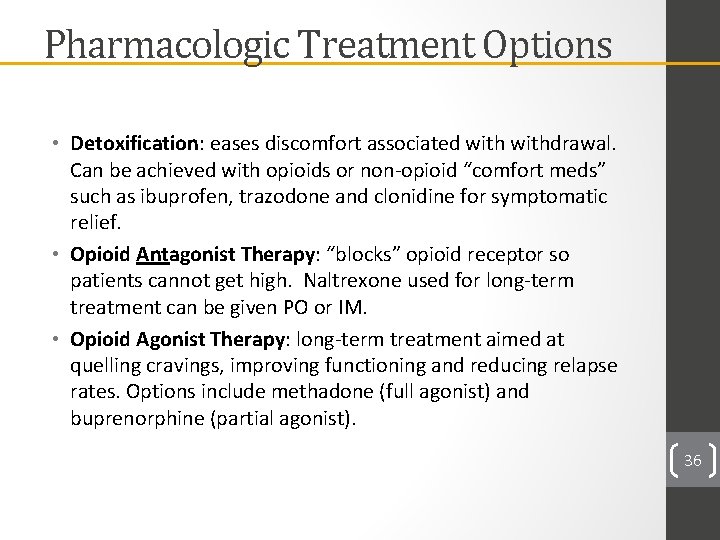
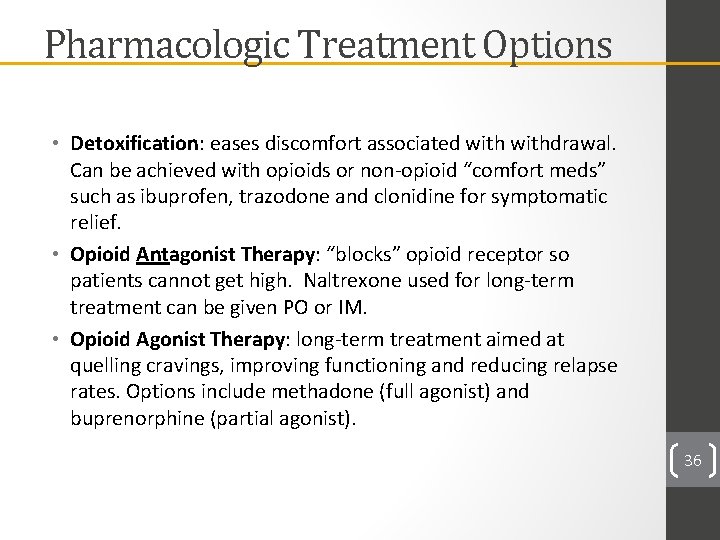
Pharmacologic Treatment Options • Detoxification: eases discomfort associated withdrawal. Can be achieved with opioids or non-opioid “comfort meds” such as ibuprofen, trazodone and clonidine for symptomatic relief. • Opioid Antagonist Therapy: “blocks” opioid receptor so patients cannot get high. Naltrexone used for long-term treatment can be given PO or IM. • Opioid Agonist Therapy: long-term treatment aimed at quelling cravings, improving functioning and reducing relapse rates. Options include methadone (full agonist) and buprenorphine (partial agonist). 36
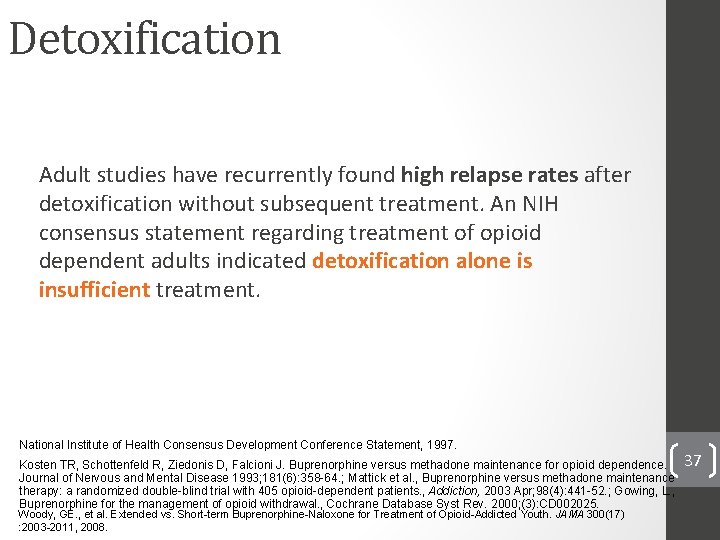
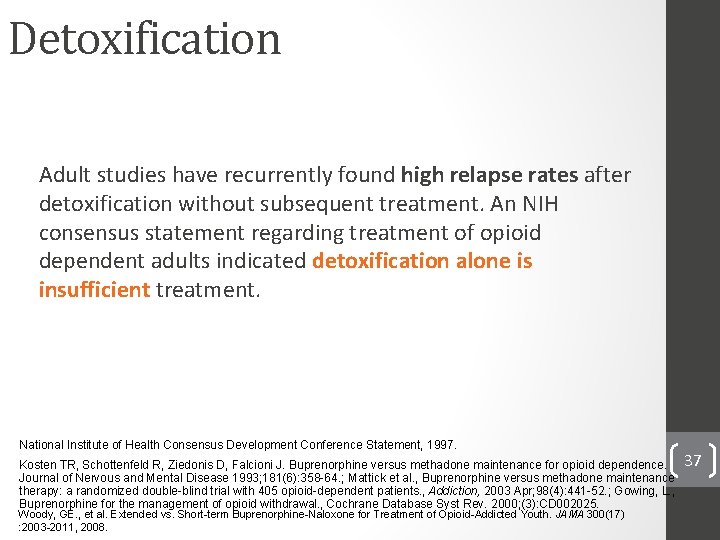
Detoxification Adult studies have recurrently found high relapse rates after detoxification without subsequent treatment. An NIH consensus statement regarding treatment of opioid dependent adults indicated detoxification alone is insufficient treatment. National Institute of Health Consensus Development Conference Statement, 1997. Kosten TR, Schottenfeld R, Ziedonis D, Falcioni J. Buprenorphine versus methadone maintenance for opioid dependence. Journal of Nervous and Mental Disease 1993; 181(6): 358 -64. ; Mattick et al. , Buprenorphine versus methadone maintenance therapy: a randomized double-blind trial with 405 opioid-dependent patients. , Addiction, 2003 Apr; 98(4): 441 -52. ; Gowing, L. , Buprenorphine for the management of opioid withdrawal. , Cochrane Database Syst Rev. 2000; (3): CD 002025. Woody, GE. , et al. Extended vs. Short-term Buprenorphine-Naloxone for Treatment of Opioid-Addicted Youth. JAMA 300(17) : 2003 -2011, 2008. 37

Medication Assisted Treatment 38
39
Opioid Function at Receptors • Different exogenous molecules have varying levels of “fit” at the opioid receptor, resulting in different levels of receptor activity with binding • Substances are divided into three groups: full agonists, partial agonists and antagonists. • In general, antagonists have the highest receptor affinity and full agonists the lowest. 40
Methadone – very limited options for patients under age 18 Schedule II Highly regulated Can only be prescribed through “methadone clinics”; very few can take patients under 18 years old. • Methadone programs are highly structured, which offers an advantage for patients, especially with limited social support • Some patients who are not successful with the partial agonist buprenorphine can be successful with methadone. • • 41 Studies in adults comparing methadone to buprenorphine have found nearly identical treatment retention and outcomes
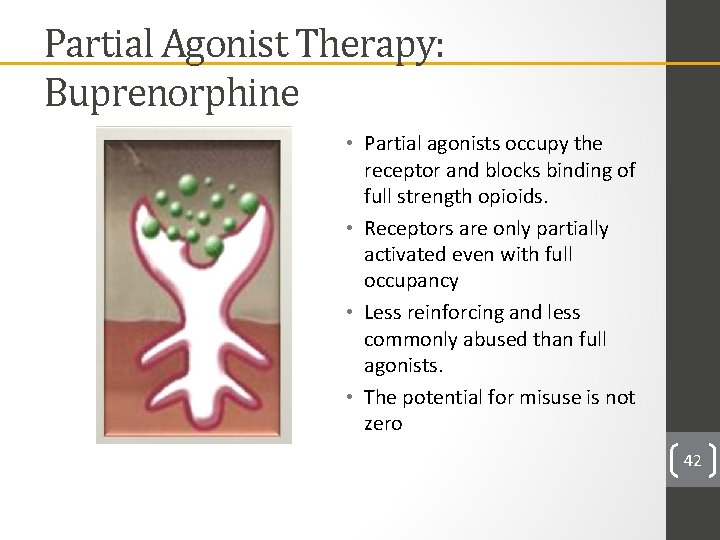
Partial Agonist Therapy: Buprenorphine • Partial agonists occupy the receptor and blocks binding of full strength opioids. • Receptors are only partially activated even with full occupancy • Less reinforcing and less commonly abused than full agonists. • The potential for misuse is not zero 42
Buprenorphine • Buprenorphine – FDA indication for treating patients > 16 years • Schedule III • Can be prescribed from physician offices • Combination product (with naloxone) limits misuse potential • Antagonist properties may be therapeutically useful • Safer than methadone in overdose • Mildly reinforcing which may support medication adherence 43 Studies in adults comparing methadone to buprenorphine have found nearly identical treatment retention and outcomes
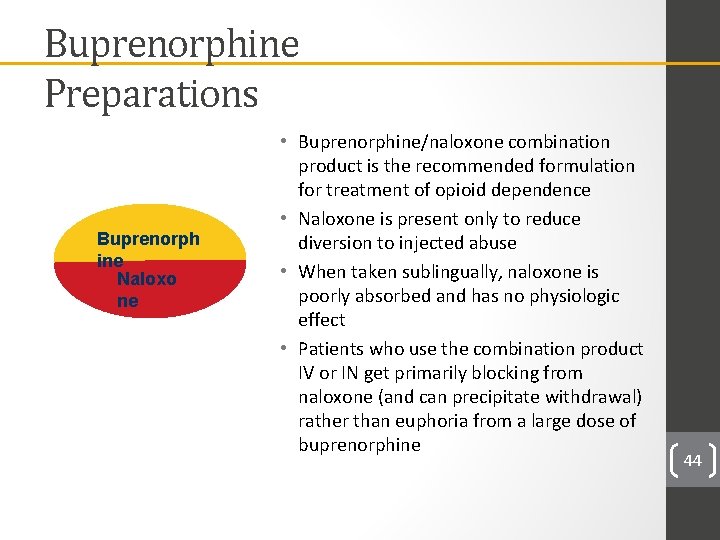
Buprenorphine Preparations Buprenorph ine Naloxo ne • Buprenorphine/naloxone combination product is the recommended formulation for treatment of opioid dependence • Naloxone is present only to reduce diversion to injected abuse • When taken sublingually, naloxone is poorly absorbed and has no physiologic effect • Patients who use the combination product IV or IN get primarily blocking from naloxone (and can precipitate withdrawal) rather than euphoria from a large dose of buprenorphine 44
Research Trials with Adolescents Extended vs. Short-term Buprenorphine-Naloxone for Treatment of Opioid-Addicted Youth: A Randomized Trial Study design • Participants 15 -21 years old with opioid dependence via DSM-IV, N=152 • Randomly assigned to 1 of 2 groups: • 2 -week detox w/ max dose of 14 mg/day buprenorphine (n=78) • 12 -week treatment buprenorphine-naloxone w/ max dose of 24 mg/day for 5 -7 days/ week for 12 weeks (n=74) • All participants received group and individual counseling each week for 12 weeks 45 Woody, GE. , et al. JAMA 300(17) : 2003 -11, 2008
Research Trials with Adolescents Extended vs. Short-term Buprenorphine-Naloxone for Treatment of Opioid-Addicted Youth: A Randomized Trial Summary of Findings • Fewer Opioid positive urine screens in 12 -week-treatment group • Higher retention rates in 12 -week-treatment group 46 Woody, GE. , et al. JAMA 300(17) : 2003 -11, 2008
Buprenorphine Waiver Training: The Half and Half Course – specifically for Pediatricians and Family Physicians in addressing adolescent specific issues http: //www. cvent. com/d/l 4 q 2 mj 47
Treatment with Naltrexone: Overview • FDA indication for • Naltrexone is a long-acting, high affinity, competitive opioid receptor antagonist with an active metabolite (6 -β-naltrexol) • Naltrexone blocks the euphoric effects of opioid use. • A study with adults aged 18 and over found that compared to placebo, patients who received naltrexone had less opioid use, better treatment retention and fewer cravings. • There are no data regarding the efficacy or adverse effects profile in children. 48 Krupitsky et al. ,
Naltrexone: Pharmacology • 5 -40% bioavailability when administered orally • Metabolized in the liver, renal excretion • Effective opioid blockade lasts from 1 -3 days depending on dose • Recommended adult dose is 50 mg daily or 380 mg IM monthly • Naltrexone can precipitate opioid withdrawal; start after the withdrawal period is completed – generally 7 days, longer if patient had been using long acting opioid such as methadone 49
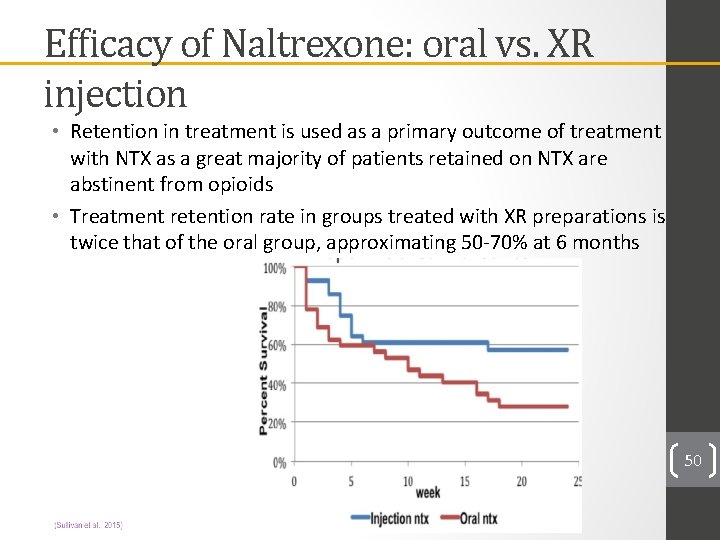
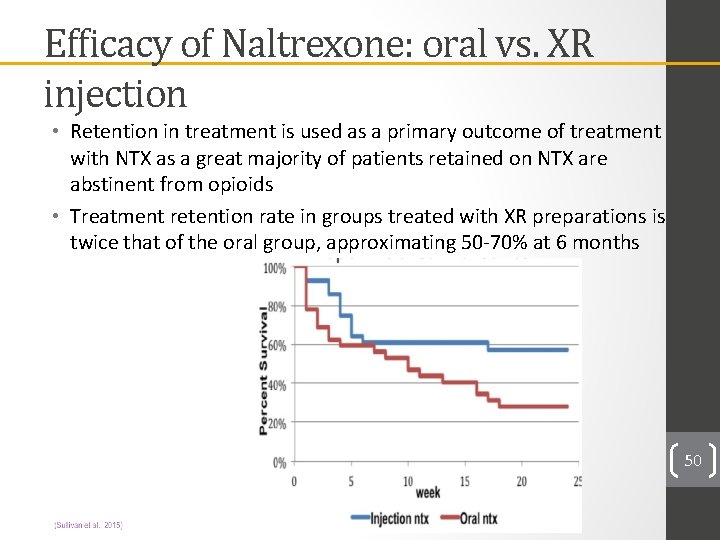
Efficacy of Naltrexone: oral vs. XR injection • Retention in treatment is used as a primary outcome of treatment with NTX as a great majority of patients retained on NTX are abstinent from opioids • Treatment retention rate in groups treated with XR preparations is twice that of the oral group, approximating 50 -70% at 6 months 50
How long will my patient be on MAT? • SUD’s are like any chronic illness requiring maintenance treatment. • • Early sobriety Longer sobriety Relapse Early Sobriety, etc • Patient response to treatment is individual, but should be multi-modal • Changes to lifestyle / diet / exercise help • Psychosocial support should start with MAT and continue after its discontinuation • Individual medication needs vary in short term and long term
Monitor 52
MAT with outside provider • Get a release to speak with the provider that specifically states substance abuse treatment is part of the information being communicated • Notify external provider about critical medical updates • Monitoring patients who get MAT somewhere else • Drug tests – you can order them! • Buprenorphine/norbuprenorphine should be in the sample if patient is taking this medication
Conclusions • Opioid use among adolescents and young adults is a serious problem with potentially life-threatening consequences • Pediatric health care providers can have a significant impact on this problem by: • Recognizing that adolescents can develop opioid use disorders • Using caution in prescribing opioids • Counseling patients and parents about prescription drug misuse • Supporting medication-assisted treatment for patients with severe opioid use disorders 54
Acknowledgements Adolescent Substance Abuse Program (ASAP) Clinicians • Diana Deister, MD, MS • Leslie Green, MSW, LICSW • Scott Hadland, MD, MPH • Sharon Levy, MD, MPH • Shannon Mountain-Ray, MSW, LICSW • Patricia Schram, MD • Jesse Schram, LICSW • Nicholas Chadi, MD Research Assistants • Dylan Kaye, BA • Lily Rabinow, MS • Parissa Salimian, BA • Meghana Vijaysimha, MPH • Rosemary Ziemnik, BS Teaching Collaborators • Pamela Burke, Ph. D, RN, FNP, PNP, FSAHM, FAAN • Linda Malone, DNP, RN, CPNP • Sarah Pitts, MD • Marianne Pugatch, MSW, LICSW • Jennifer Putney, Ph. D, LICSW Research Collaborators • Co-principal investigators: Elissa Weitzman, Sc. D, Msc & Sharon Levy, MD, MPH • Elizabeth Harstad, MD, MPH • Lauren Wisk, Ph. D Research Project Management • Julie Lunstead, MPH, Program Manager • Erin Huang, MPH, Data Manager PCSS MAT Training Providers' Clinical Support System for Medication Assisted Treatment 55
Questions? 56