What PARIHS is about Introducing the PARIHS Group
What PARIHS is about
Introducing the PARIHS Group Brendan Mc. Cormack Jo Rycroft-Malone Alison Kitson Angie Titchen Kate Seers Gill Harvey
Despite growing acknowledgement within the research community that the implementation of research into practice is a complex and messy task, conceptual models describing the process still tend to be uni-dimensional, suggesting some linearity and logic. (Kitson, Harvey & Mc. Cormack, 1998)
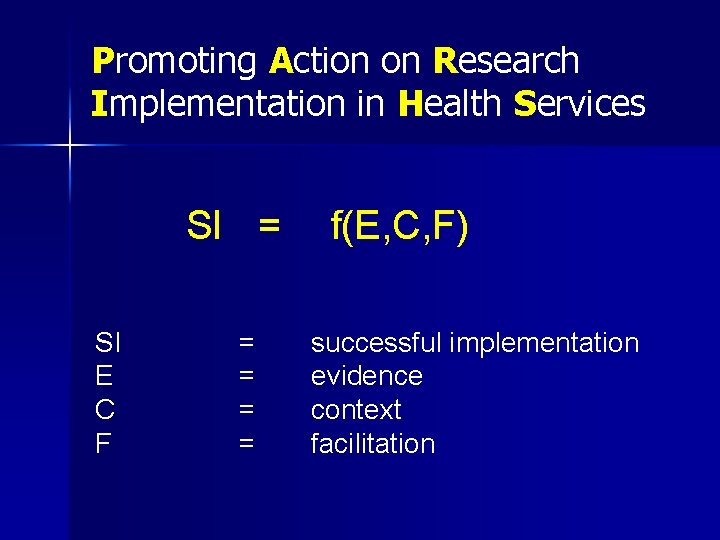
Promoting Action on Research Implementation in Health Services SI = SI E C F = = f(E, C, F) successful implementation evidence context facilitation
Successful implementation is a function of the relation between: - the nature of the evidence the context or environment in which the proposed change is to be implemented and the way or method by which the change is facilitated
Framework Development n Practical experience from: – Research projects – Quality Improvement initiatives – Practice Development programme Theoretical - concept development n Empirical inquiry - content validity n Developing & testing interventions n Tool and ‘toolkit’ development n
Checking out the framework n Numerous conference presentations Workshop/Group exercises n 1998 publication in Quality in Health Care n n n n Establishing a level of face validity Concept analysis of evidence, context and facilitation – published in Journal of Advanced Nursing 2002 publication in Quality in Health Care Focus groups Case study 2004 publication in Journal of Clinical Nursing 2008 publication in Implementation Science
‘Hypothesis’ The successful implementation of evidence into practice is more likely to occur in situations where the research evidence is strong (‘high’), there is consensus about it and it matches patients’ preferences, the context is conducive to change/the new practice (‘high’), and appropriate approaches and mechanisms of facilitation are in place (‘high’).
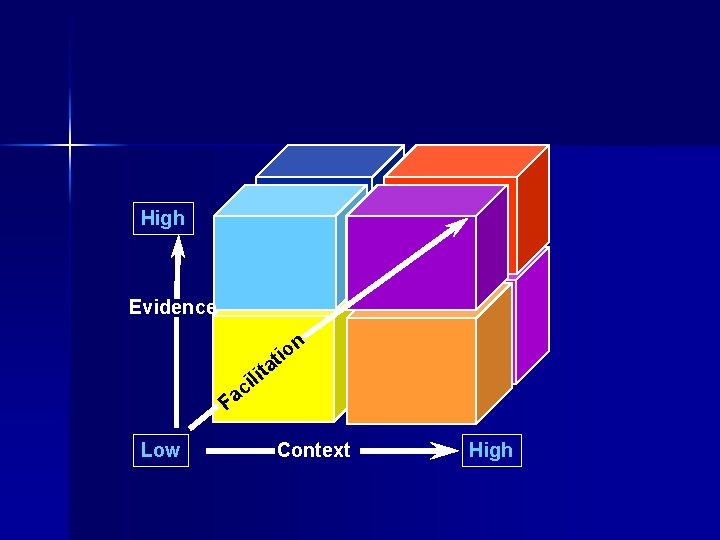
High Evidence n lit i c tio a Fa Low Context High

The Nature of Evidence Information and knowledge upon which decisions about care based: 1. 2. 3. 4. Research Clinical Experience Patient Experience Local Information/Data
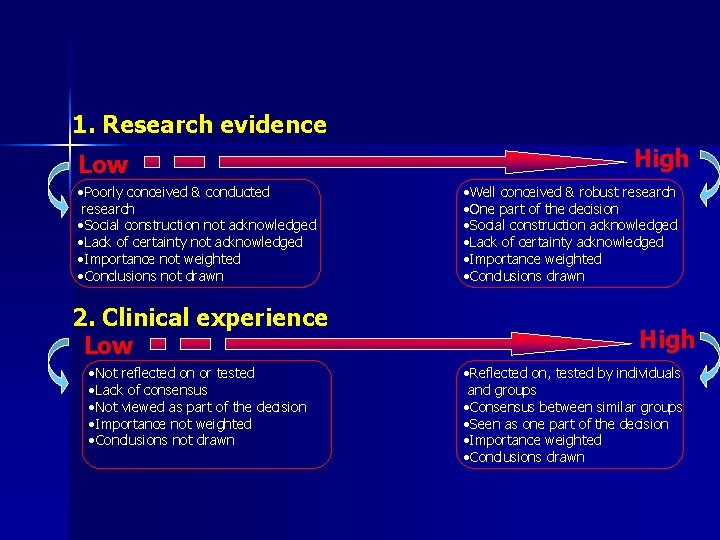
1. Research evidence Low • Poorly conceived & conducted research • Social construction not acknowledged • Lack of certainty not acknowledged • Importance not weighted • Conclusions not drawn 2. Clinical experience Low • Not reflected on or tested • Lack of consensus • Not viewed as part of the decision • Importance not weighted • Conclusions not drawn High • Well conceived & robust research • One part of the decision • Social construction acknowledged • Lack of certainty acknowledged • Importance weighted • Conclusions drawn High • Reflected on, tested by individuals and groups • Consensus between similar groups • Seen as one part of the decision • Importance weighted • Conclusions drawn
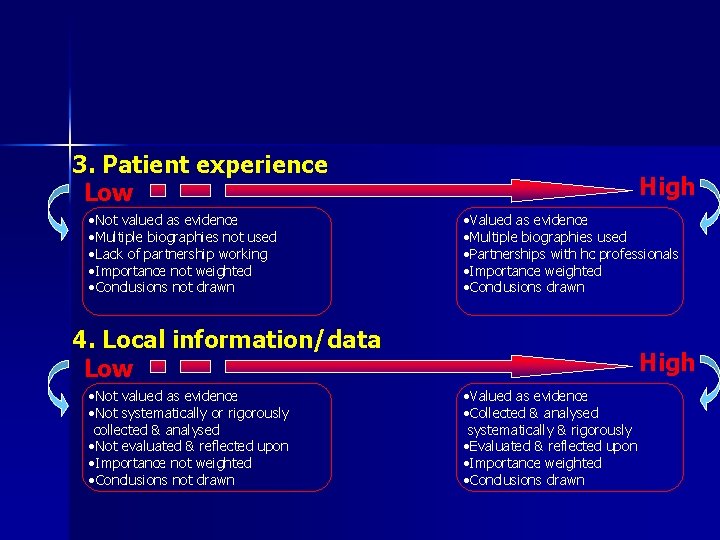
3. Patient experience Low • Not valued as evidence • Multiple biographies not used • Lack of partnership working • Importance not weighted • Conclusions not drawn High • Valued as evidence • Multiple biographies used • Partnerships with hc professionals • Importance weighted • Conclusions drawn 4. Local information/data Low • Not valued as evidence • Not systematically or rigorously collected & analysed • Not evaluated & reflected upon • Importance not weighted • Conclusions not drawn High • Valued as evidence • Collected & analysed systematically & rigorously • Evaluated & reflected upon • Importance weighted • Conclusions drawn
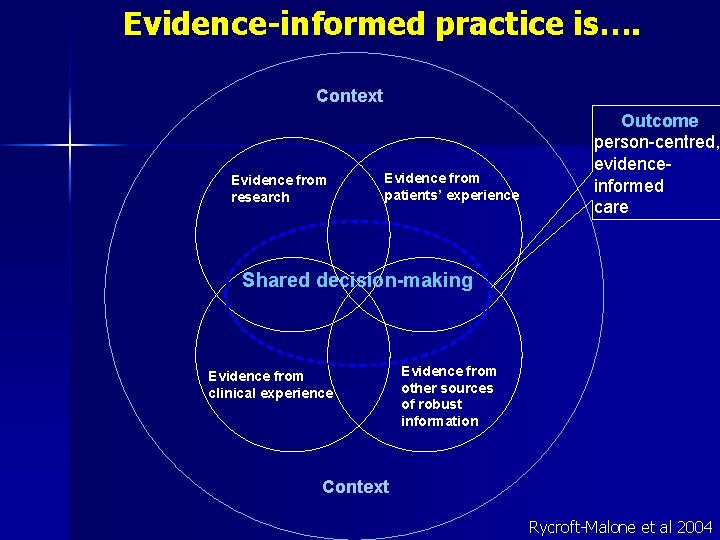
Evidence-informed practice is…. Context Evidence from research Evidence from patients’ experience Outcome person-centred, evidenceinformed care Shared decision-making Evidence from clinical experience Evidence from other sources of robust information Context Rycroft-Malone et al 2004
Context of Implementation The environment or setting in which the proposed changes is to be implemented: n Culture n Leadership n Evaluation
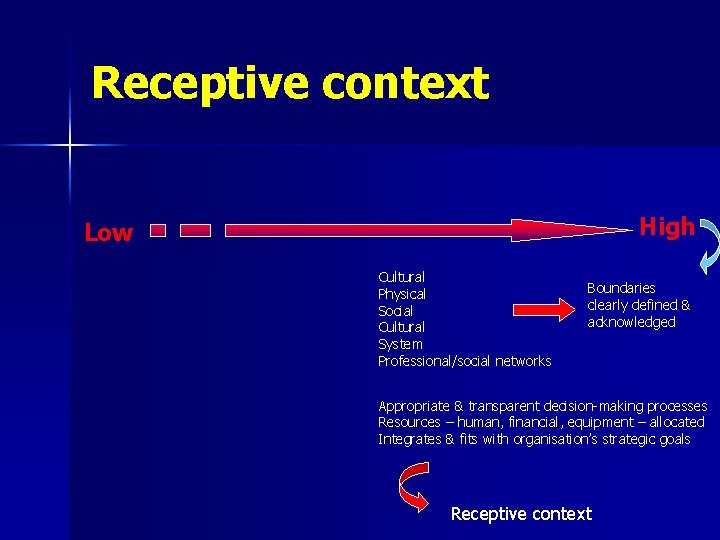
Receptive context High Low Cultural Physical Social Cultural System Professional/social networks Boundaries clearly defined & acknowledged Appropriate & transparent decision-making processes Resources – human, financial, equipment – allocated Integrates & fits with organisation’s strategic goals Receptive context
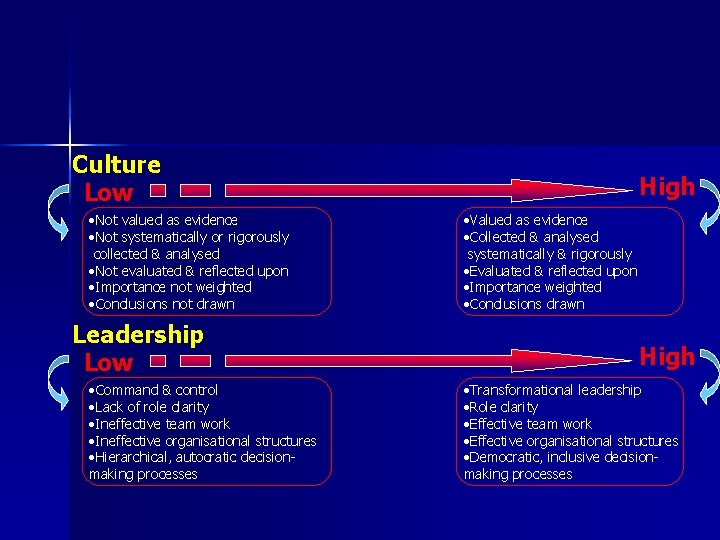
Culture Low • Not valued as evidence • Not systematically or rigorously collected & analysed • Not evaluated & reflected upon • Importance not weighted • Conclusions not drawn Leadership Low • Command & control • Lack of role clarity • Ineffective team work • Ineffective organisational structures • Hierarchical, autocratic decisionmaking processes High • Valued as evidence • Collected & analysed systematically & rigorously • Evaluated & reflected upon • Importance weighted • Conclusions drawn High • Transformational leadership • Role clarity • Effective team work • Effective organisational structures • Democratic, inclusive decisionmaking processes
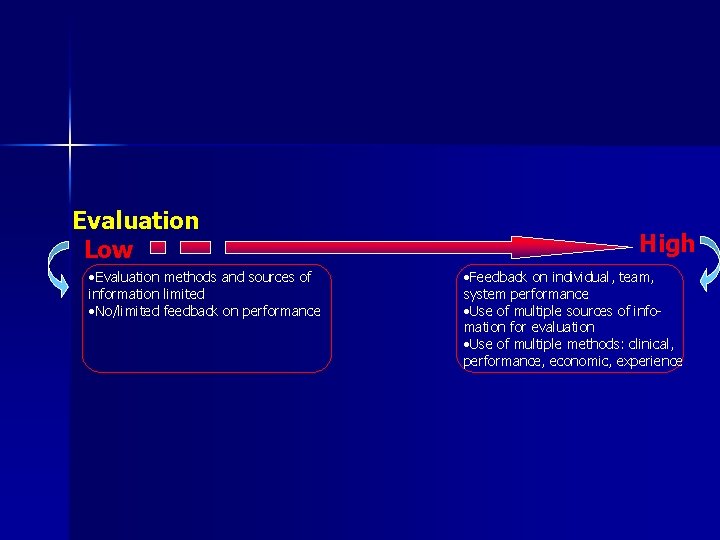
Evaluation Low • Evaluation methods and sources of information limited • No/limited feedback on performance High • Feedback on individual, team, system performance • Use of multiple sources of infomation for evaluation • Use of multiple methods: clinical, performance, economic, experience
Facilitation The process of enabling or making things easier n n Appropriate Purpose Role Skills
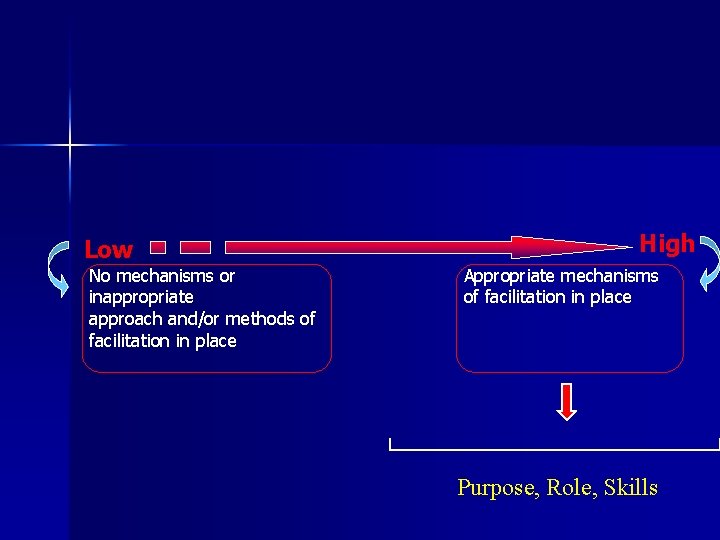
Low No mechanisms or inappropriate approach and/or methods of facilitation in place High Appropriate mechanisms of facilitation in place Purpose, Role, Skills
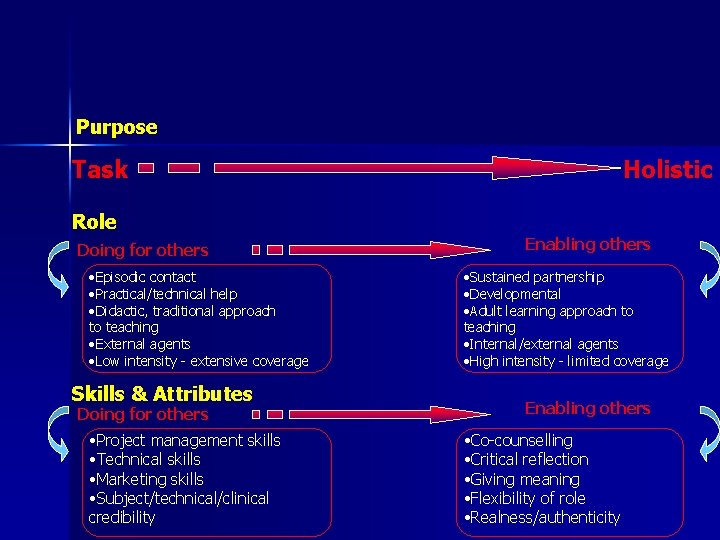
Purpose Task Holistic Role Doing for others • Episodic contact • Practical/technical help • Didactic, traditional approach to teaching • External agents • Low intensity - extensive coverage Skills & Attributes Doing for others • Project management skills • Technical skills • Marketing skills • Subject/technical/clinical credibility Enabling others • Sustained partnership • Developmental • Adult learning approach to teaching • Internal/external agents • High intensity - limited coverage Enabling others • Co-counselling • Critical reflection • Giving meaning • Flexibility of role • Realness/authenticity
Working hypotheses n n Most successful implementation will occur when evidence is ‘high’, practitioners agree about it, the context is developed, and where there is appropriate facilitation Least successful implementation occurs when context and facilitation are inadequate Poor contexts can be overcome by appropriate facilitation Chances of successful implementation are still weak, even in an adequate context, but where there’s inappropriate facilitation
How is/has it been used? As a conceptual framework n As an evaluative framework n As a map n As a set of hypotheses n See the world map for examples!
Questions/challenges Is it greater than the sum of its parts? n How do the elements interact? n What factors are more important – weighting? n Dynamics of high to low – do they work? Is it comprehensive (enough)? n How does the individual fit into the framework? n
Next steps PARIHS collaboration n Tool development n – Measuring/evaluating evidence, context, facilitation n Intervention research – e. g. FIRE – EU grant n Capability building through education & training opportunities
Publications n Kitson A, Rycroft-Malone J, Harvey G, Mc. Cormack B, Seers K, Titchen A (2008) Evaluating the successful implementation of evidence into practice using the PARIHS framework: Theoretical and practical challenges, Implementation Science, 3(1), 7 th January 2008 n Rycroft-Malone J, Harvey G, Seers K, Kitson A. Mc. Cormack B, & Titchen A. (2004) An exploration of the factors that influence the implementation of evidence into practice. Journal of Clinical Nursing , 13, 913 -924 n Rycroft-Malone J, Seers K, Titchen A, Harvey G, Kitson A, Mc. Cormack B (2004) What counts as evidence in evidence-based practice? Journal of Advanced Nursing , 47(1): 81 -90. n Rycroft-Malone J. (2004) The PARIHS framework – A framework for guiding the implementation of evidence -based practice. Journal of Nursing Care Quality , 19(4), 297 -304. n Harvey G, Loftus-Hills A, Rycroft-Malone J, Titchen A, Kitson A, Mc. Cormack B, Seers K (2002) Getting evidence into practice: the role and function of facilitation. Journal of Advanced Nursing , 37(6): 577 -588. n Mc. Cormack B, Kitson A, Harvey G, Rycroft-Malone J, Titchen A, Seers K (2002) Getting evidence into practice: the meaning of context. Journal of Advanced Nursing , 38(1): 94 -104. n Rycroft-Malone J, Kitson A, Harvey G, Mc. Cormack B, Seers K, Titchen A, Estabrooks C (2002) Ingredients for change: revisiting a conceptual framework. Quality in Healthcare, 11(2): 174 -180. n Rycroft-Malone J, Harvey G, Kitson A, Mc. Cormack B, Seers K, Titchen A (2002) Getting evidence into practice: ingredients for change. Nursing Standard, 16(37): 38 -43. n Kitson A, Harvey G, Mc. Cormack B (1998) Enabling the implementation of evidence based practice: a conceptual framework. Quality in Health Care , 7, 3: 149 -158.
- Slides: 25