What Neglect Looks Like Dr Marianne Cochrane Consultant

- Slides: 52
What Neglect Looks Like Dr Marianne Cochrane Consultant Paediatrician Lead for Child Protection
Contents n Definitions and Concept n. Risk factors and Indicators n. How Does Neglect Present n. The Effects of Neglect n. What More Can we Do?
What is Neglect? n Neglect is the persistent failure to meet a child’s basic physical and/or psychological needs, likely to result in the serious impairment of the child’s health or development. Neglect may occur during pregnancy as a result of maternal substance abuse
Types of Neglect § Medical neglect § Nutritional neglect § Emotional neglect § Educational neglect § Physical neglect § Lack of supervision and guidance n (Horwath 2007)
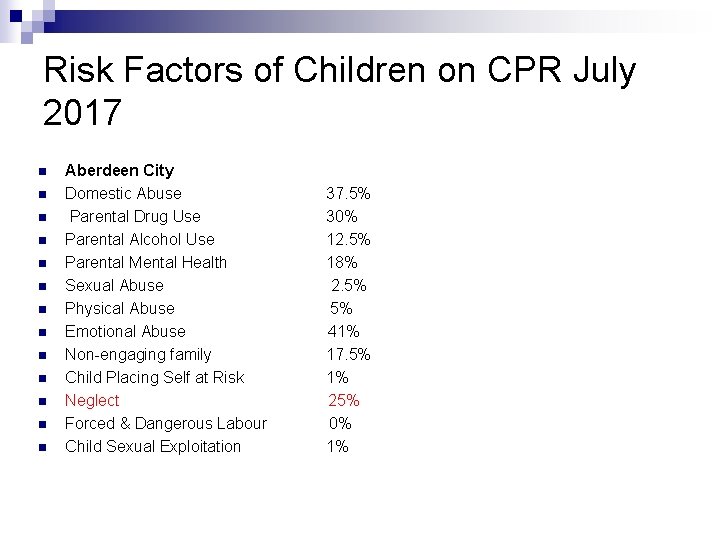
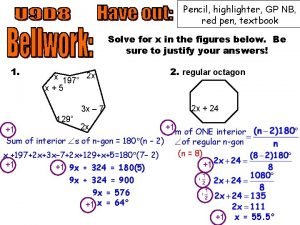
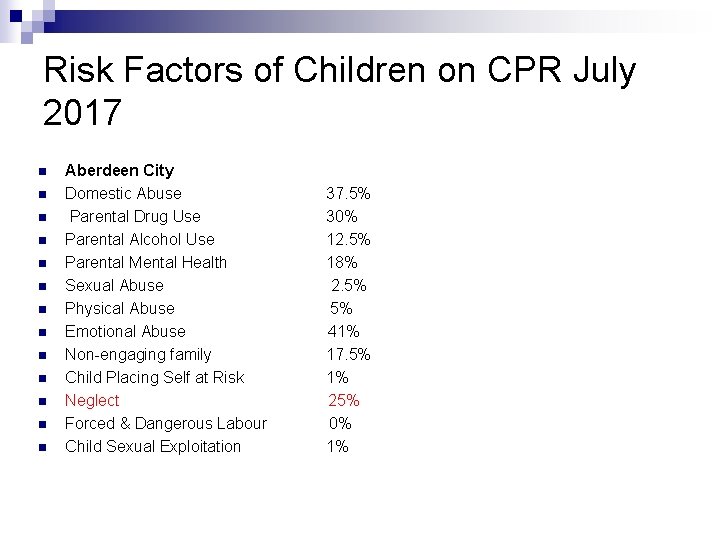
Risk Factors of Children on CPR July 2017 n n n n Aberdeen City Domestic Abuse 37. 5% Parental Drug Use 30% Parental Alcohol Use 12. 5% Parental Mental Health 18% Sexual Abuse 2. 5% Physical Abuse 5% Emotional Abuse 41% Non-engaging family 17. 5% Child Placing Self at Risk 1% Neglect 25% Forced & Dangerous Labour 0% Child Sexual Exploitation 1%
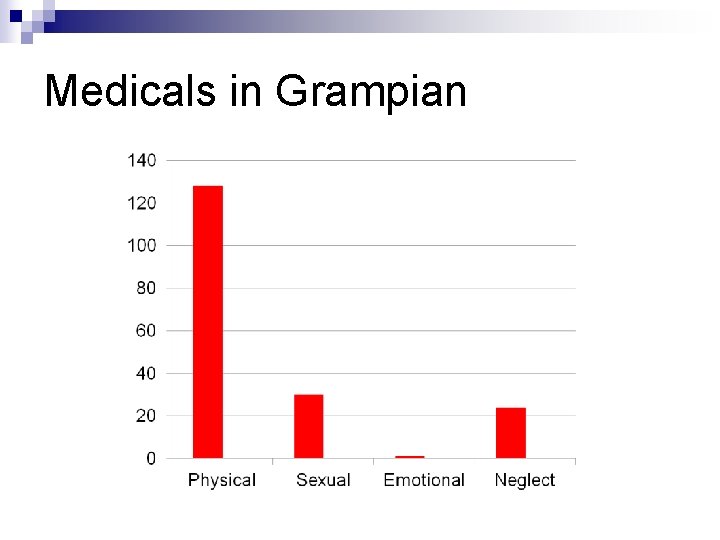
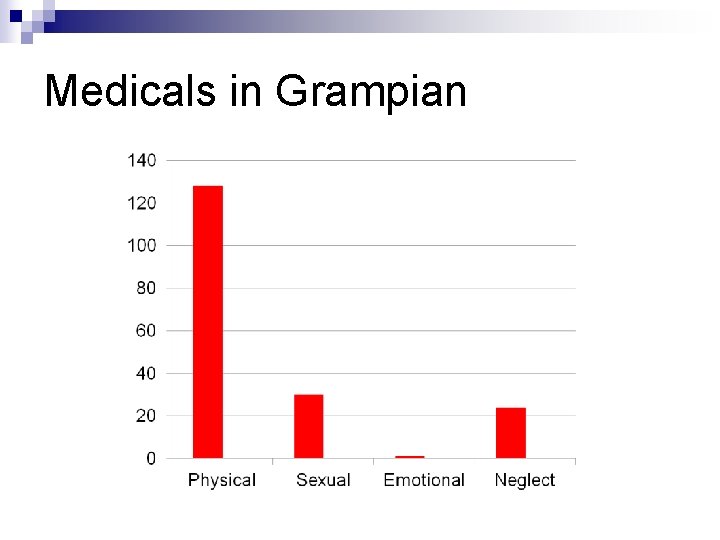
Medicals in Grampian
The Concept of Neglect § In some ways it is relatively simple to identify a child whose needs are not being met § But ‘neglect’ as a basis for intervention is a complex phenomenon that is difficult to define § In the face of a range of views of what constitutes adequate care, defining children’s needs and determining what constitutes neglect has been problematic n (NSPCC 2007)
Barriers to Action Professionals struggle to identify and act on indicators of neglect (Laming 2003; Gilbert et al 2009) • Neglect rarely produces a crisis which requires proactive authoritative action • Evidencing Harm •
Mind Sets n Fears about being considered judgemental n A focus on parent rather than the child n Failure to consider/understand child’s lived experience n A fixed view of the family n Parents’ superficial or false compliance n Not my area of expertise n Reluctance to refer
Risk Factors: Social and Environmental Poverty (Sedlak 2010; Connell-Carricks 2003), Social Isolation (Connell-Carricks 2003), Poor living conditions (Slack et al 2003).
Risk Factors: Parents • Maternal mental ill-health • learning disabilities • drug and alcohol misuse • domestic violence, especially in combination (Schumacher et al 2001). • Men – risk or resource? lack of research evidence (Zanoni 2013)
Risk Factors: Children • Pre-term/low birth weight babies • complex health needs (Strathearn et al 2001). • Age of child (pre-school and adolescents most at risk). • Disabled children (Stalker and Mc. Arthur 2012)
Risk Factors (Sidebotham 2003) Risk of neglect occurring - Risk factors are not predictors of neglect - Risk factors for neglect are also risks for other adverse outcomes not connected with maltreatment (so what causes the harm? ) - Families with risk factors for neglect often do not neglect their children (prospective studies) But risk factors help us to understand the child’s experience and help agencies to work out priorities for support.
Indicators of Neglect Evidence that the child may be experiencing actual neglect (Sidebotham 2003) • Behavioural and developmental indicators • Physical Appearance • Poor Health • Faltering Growth/Obesity • Cognitive Skills • Harm due to lack of Supervision
Indicators of Neglect But not all indicators are distinctive characteristics of neglect alone – may signal other or parallel problems (eg post natal depression [mother or father] or inherent conditions in the child) n Cumulative, persistent, chronic n
Medical Neglect Failure to comply with medication n Failure to attend essential appointments n Failure to seek medical attention appropriately. . . . n Compromising the health and wellbeing of the child
Case 1: 3 year old boy referred by GP with squint n Attends first appointment at Eye Clinic and Optometrist n Patching recommended n Not brought to 2 follow up appointments n Discharged and re-referred n Not brought again. . n
Case 1 n Outcome for child: n PERMANENT LOSS OF VISION IN EYE DUE TO NON COMPLIANCE WITH PATCHING AND NON ATTENDANCE AT APPOINTMENTS
Nutritional Neglect Faltering growth through lack of understanding of dietary needs or a failure or inability to provide an appropriate diet. n Obesity through inadequate attention to the child’s diet and/or life style or the persistent failure to take medical advice about diet and lifestyle modification. n
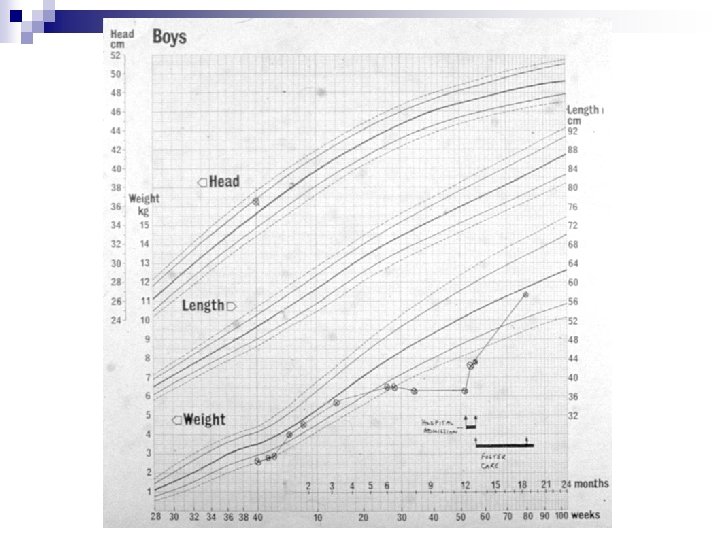
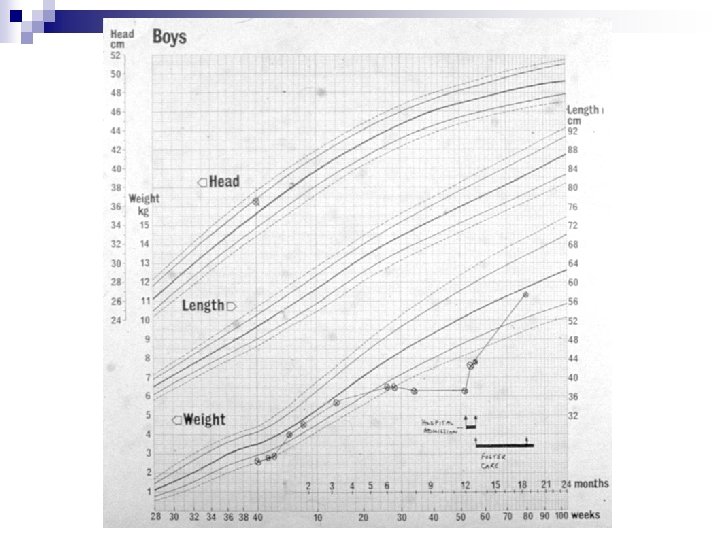
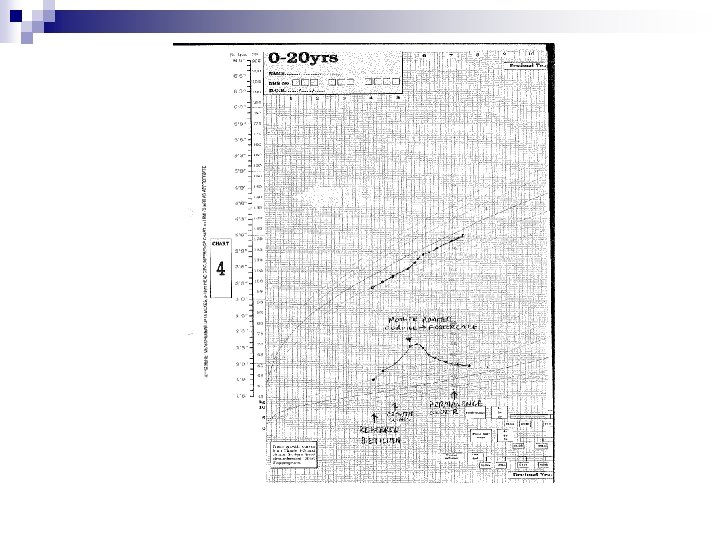
Growth Faltering n Important feature of neglect n Simple test : height, weight, chart n Complex evaluation – Non Organic but why? n Medico-legal value

Obesity n NICE Guidelines: Public Health Problem n Child Protection Companion 2013: ¨ Fulfils 3 categories: ¨ All other options been exhausted/no other options ¨ Statutory measures likely to make a difference ¨ Imminent harm
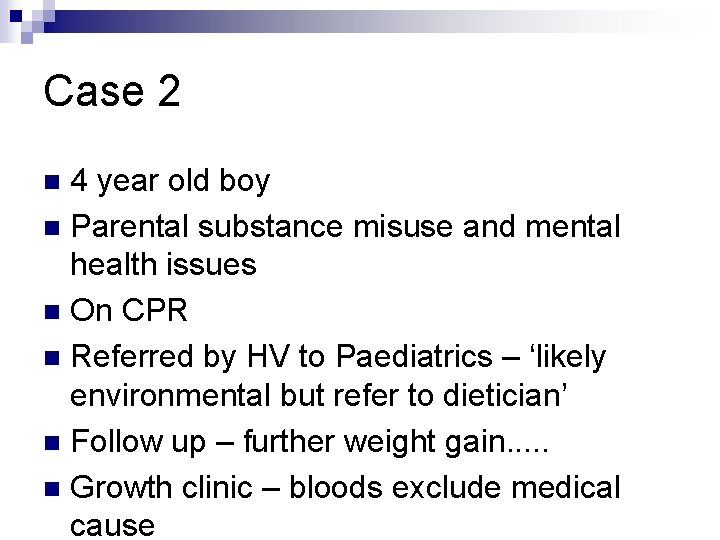
Case 2 4 year old boy n Parental substance misuse and mental health issues n On CPR n Referred by HV to Paediatrics – ‘likely environmental but refer to dietician’ n Follow up – further weight gain. . . n Growth clinic – bloods exclude medical cause n
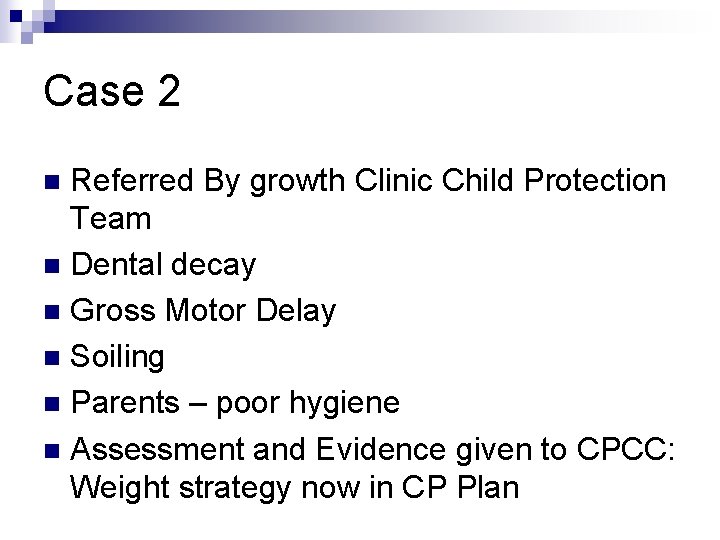
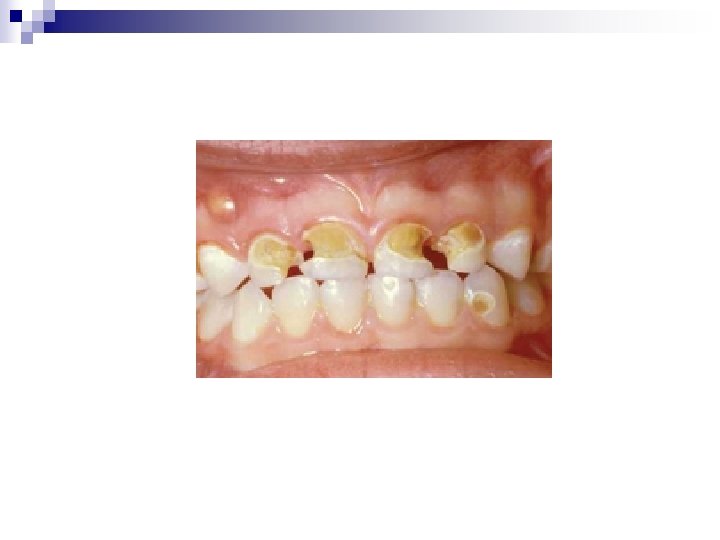
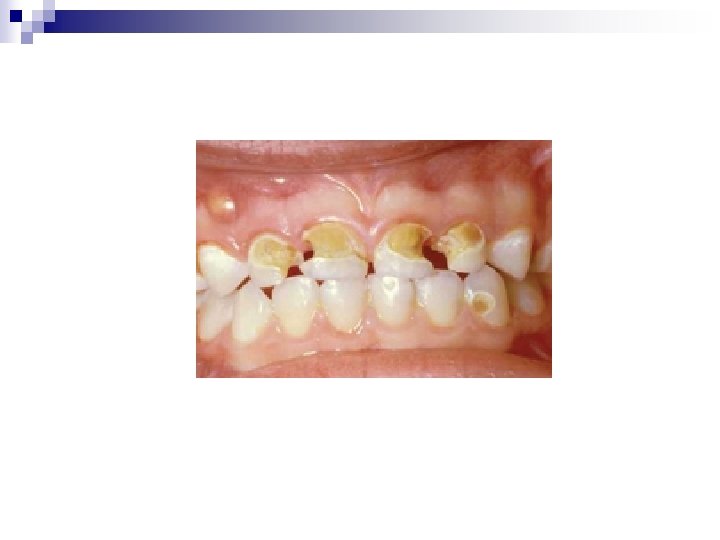
Case 2 Referred By growth Clinic Child Protection Team n Dental decay n Gross Motor Delay n Soiling n Parents – poor hygiene n Assessment and Evidence given to CPCC: Weight strategy now in CP Plan n
Developmental Delay and Neglect n Speech/ motor delay/social interaction n Recovery in foster care: review n Evidence – Standardised assessment used in Children’s Hearing System And Court
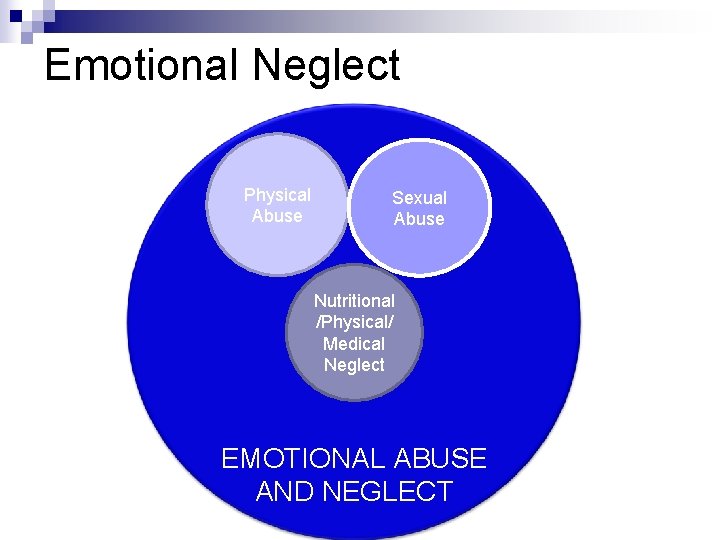
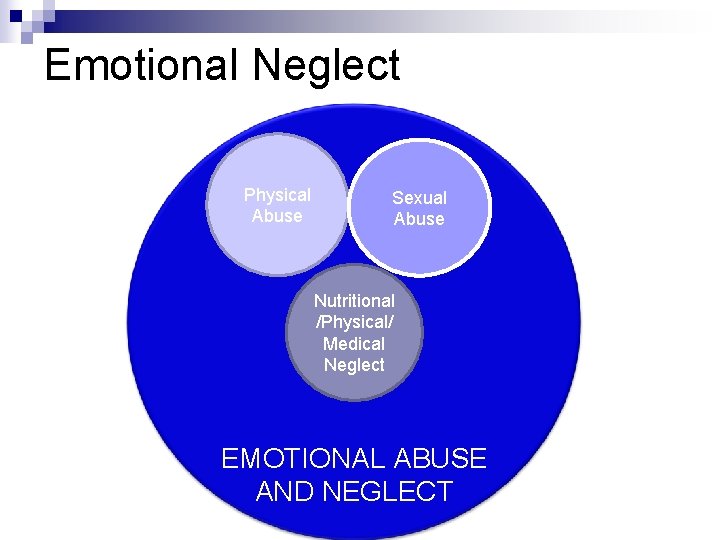
Emotional Neglect Physical Abuse Sexual Abuse Nutritional /Physical/ Medical Neglect EMOTIONAL ABUSE AND NEGLECT
Emotional Neglect Emotional unavailability, unresponsiveness n Extremely little or no emotional or psychological interaction n Developmentally inappropriate or inconsistent interactions with the child n Failing to promote the child’s social adaptation n Across all ages of children n
Emotional Development n 1 – 1. 5 years ¨ Sense of basic trust n 1. 5 – 3 years ¨ Sense of autonomy n 3 - 6 years ¨ Sense of initiative
Case 3 8 year old girl n Disclosure of sexual abuse n Further history of violence in home n Parental substance and alcohol misuse n Parents separated – living with mother in Central Belt; contact with father in holidays n Been to 5 schools since starting n
Case 3 –First Examination n n n Overweight Poor Hygiene Allowed general examination Cried when genital examination approached – high level of distress. Not undertaken Report “very distressed child made a clear allegation of child sexual abuse” Recommends: SPECIFIC POST ABUSE PSYCHOLOGICAL SUPPORT
Case 3 n NOW IN CARE OF FATHER n 2 further appointments to attempt examination – DNA n 3 rd appointment attended – refused examination n NO FURTHER FOLLOW UP
Case 3 2007 n Assault by father n n Disclosure made to school n Bruising to back seen consistent with disclosure
Case 3 - CARE HISTORY 2007 Father Temporary foster care n March 2010 Permanent Care n October 2010 t Temporary foster care n December 2010 Temporary foster care n October 2011 Residential Home n
Case 3 - referral Adolescent Psychiatry n Depression and low self esteem n Comforts eats n n FAILED TO ATTEND APPOINTMENT
LAC Health Assessment n n n n November 2011 Consent from child (age 15) Admission to hospital with alcohol related haematemesis /Pancreatitis Smokes cigarettes and cannabis Sexually active Poor school attendance Immunisations up to date
LAC Health Assessment Vision normal n Examination normal n Overweight n Referral to Family Planning n
Case 3 Outcome Pregnant age 15 1 st child n Pregnant age 17 2 nd child (father unknown) n Living with Domestic Violence n Personality Disorder – seeing Psychiatry n Child Protection Concerns about both children – Medicals: taken into foster care n
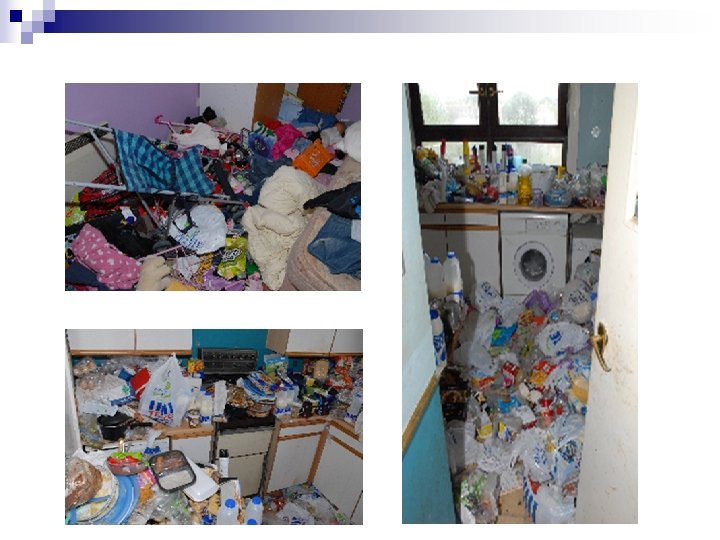
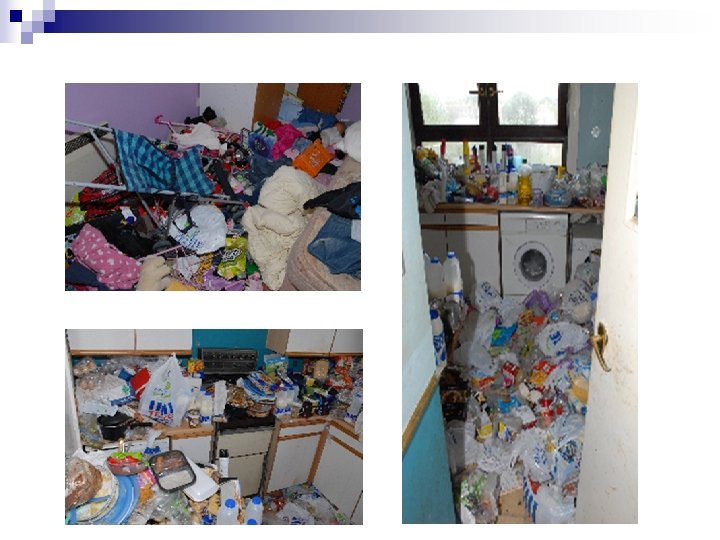
Physical Neglect Inappropriate clothing and/or footwear for the weather or child’s size n Persistent poor hygiene (smelly and dirty) n Severe and persistent infestations n Hypothermia or red, swollen and cold hands and feet from cold damage n
Case 4 16 year old girl n Moderate learning difficulties n Autism n n Returns from School after Christmas Holidays – foul smelling, ? Skin condition, dirty hair skin and clothes,
Case 4 Showered at school – wearing same dirty pants as before holidays, n Took 4 attempts at showering for water to run clear n No bra n Menstruating – no sanitary product n Skin excoriated and raw n Lice n
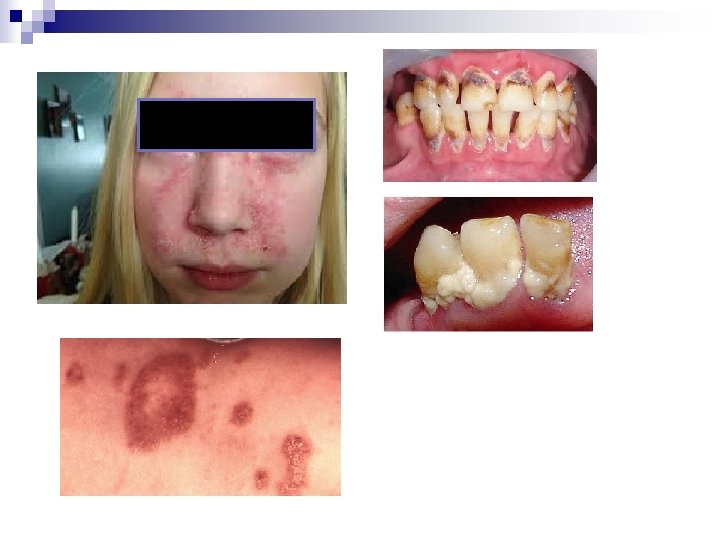
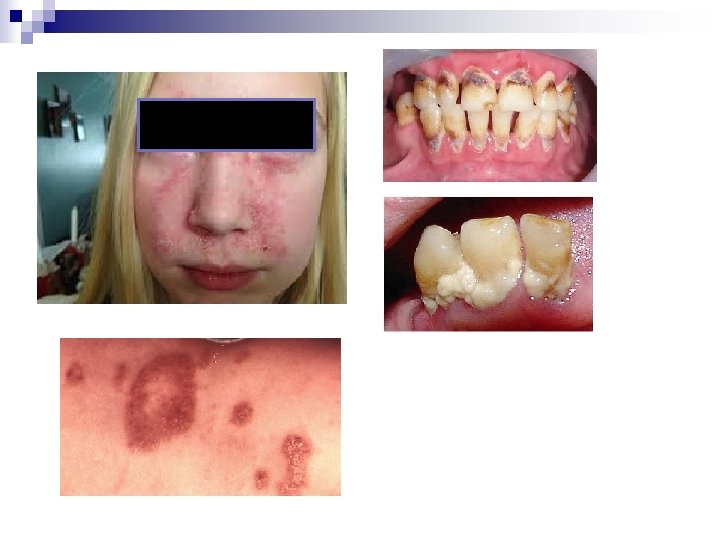
Case 4 – medical assessment BMI 40 n Fungal infection under breasts n Extensive seborrhoeic dermatitis face and scalp n Menstrual blood staining clothes n Extreme odour n Nails long and dirty, smell overwhelming n Extensive dental decay n
Case 4 Parent – “difficult to clean teeth doesn’t like it, Refuses to eat anything but junk, hates getting washes and nails cut” n But. . . . n Know to social work • Seen at Child Development Team • Seen at Epilepsy Clinic • Seen at School •
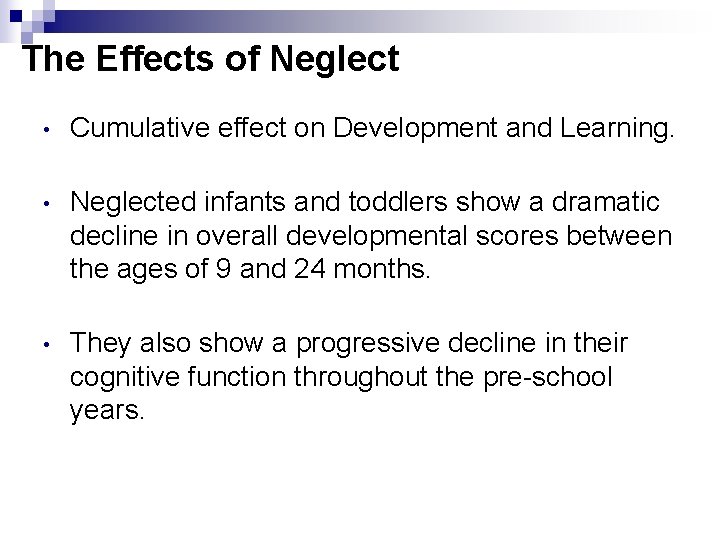
The Effects of Neglect • Cumulative effect on Development and Learning. • Neglected infants and toddlers show a dramatic decline in overall developmental scores between the ages of 9 and 24 months. • They also show a progressive decline in their cognitive function throughout the pre-school years.
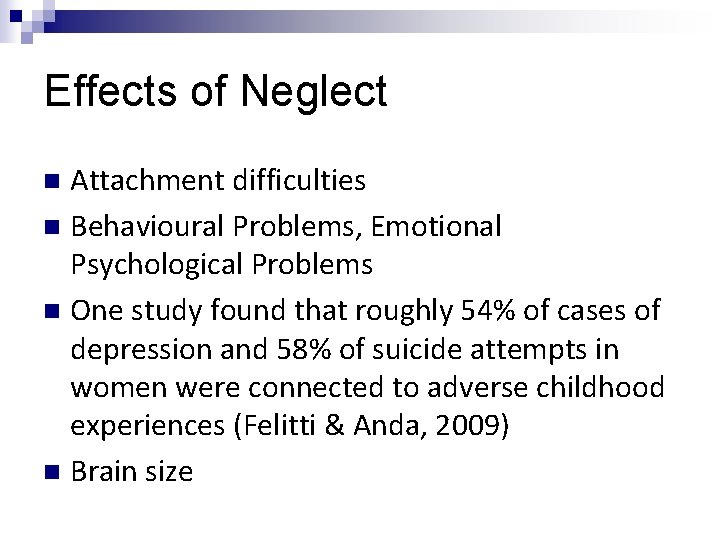
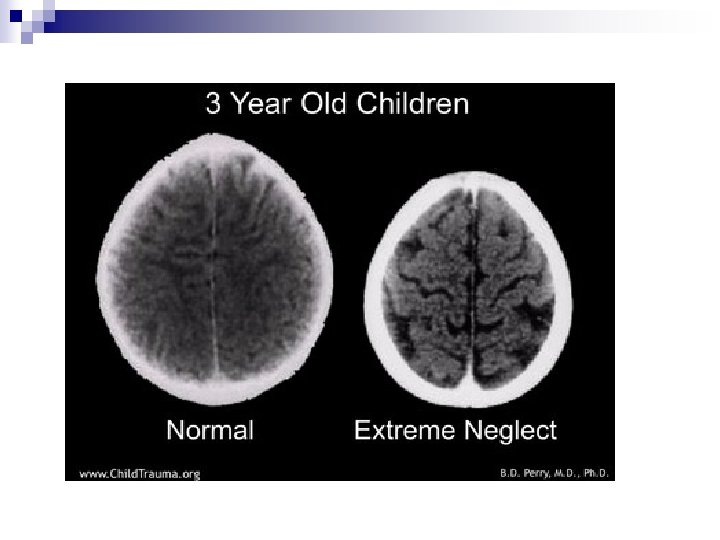
Effects of Neglect Attachment difficulties n Behavioural Problems, Emotional Psychological Problems n One study found that roughly 54% of cases of depression and 58% of suicide attempts in women were connected to adverse childhood experiences (Felitti & Anda, 2009) n Brain size n
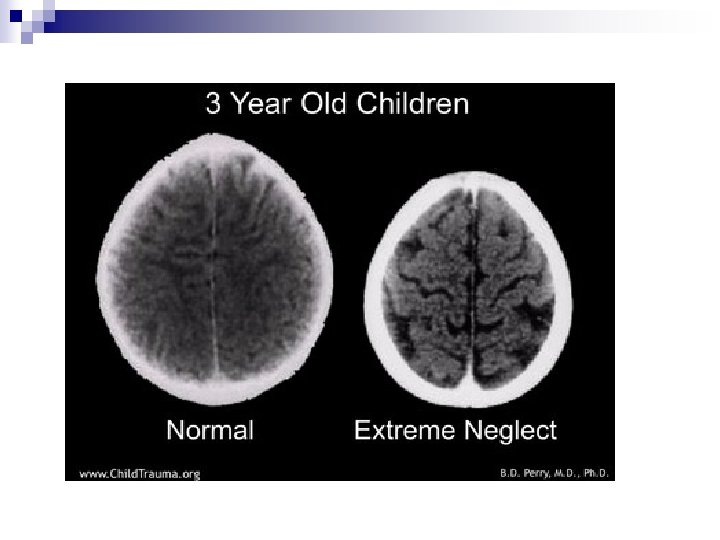
The Effects of Neglect n Neglect is at least as damaging, if not more so, than other forms of maltreatment because its impact is the most far-reaching and difficult to overcome. n Neglect is particularly damaging in the first two to three years of life - a formative period for social, emotional and neurobiological development – it can compromise later development. Can be fatal n
What Can we Do? Recognition of the CUMULATIVE effects n Thinking about the IMPACT on the Child n Robust multi-agency assessments n Communication with families about concerns n n A paediatrician should contribute to a multiagency assessment with a history, examination and relevant clinical investigations. (Child Protection Companion 2013 RCPCH)
 What does he look like
What does he look like What does he look like
What does he look like Marianne cochrane
Marianne cochrane Spice riddles
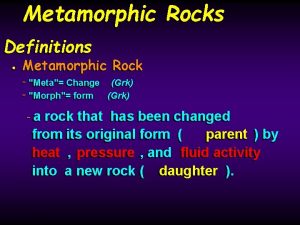
Spice riddles Foliated texture that looks like blackboard
Foliated texture that looks like blackboard Interrupted medulla
Interrupted medulla Dean leventopoulos
Dean leventopoulos Conic sections
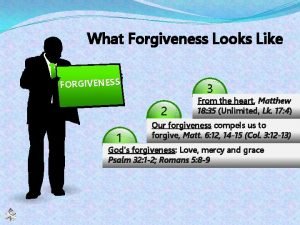
Conic sections What forgiveness looks like
What forgiveness looks like Which organelle looks like a stack of fluffy pancakes
Which organelle looks like a stack of fluffy pancakes How to write in text citations apa
How to write in text citations apa Language that looks like english
Language that looks like english What is the like weather
What is the like weather Chapter 7 a view of the cell
Chapter 7 a view of the cell Literal language examples
Literal language examples Ridge counting
Ridge counting Types of trapezium
Types of trapezium Nicotine look like
Nicotine look like What is book
What is book Country that looks like a turkey
Country that looks like a turkey What the world looks like
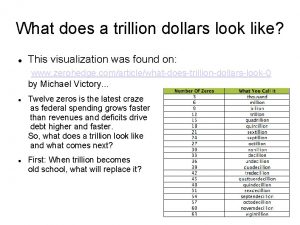
What the world looks like How much does 1 million look like
How much does 1 million look like What organelle looks like a stack of pancakes
What organelle looks like a stack of pancakes Human hair pattern
Human hair pattern Foliated texture that looks like blackboard
Foliated texture that looks like blackboard Commas in a sentence
Commas in a sentence Hyperbola
Hyperbola Guided transmission media
Guided transmission media What does 2 oz of meat look like
What does 2 oz of meat look like Sesgo de performance
Sesgo de performance Cochrane risk of bias table template
Cochrane risk of bias table template Cochrane rapid review
Cochrane rapid review Cochrane
Cochrane Euan cochrane
Euan cochrane Sesgo de desgaste
Sesgo de desgaste Metanalise o que é
Metanalise o que é 5 stappen ebp
5 stappen ebp Cochrane musculoskeletal group
Cochrane musculoskeletal group 027731
027731 Mecir cochrane
Mecir cochrane Cochrane lions football
Cochrane lions football Cochrane metaanalyse
Cochrane metaanalyse Manual cochrane
Manual cochrane Fotos de la guerra del pacifico
Fotos de la guerra del pacifico Mark wilson cochrane
Mark wilson cochrane Cochrane wiley
Cochrane wiley Cochrane training
Cochrane training Emotional neglect examples
Emotional neglect examples Sibling neglect
Sibling neglect Neglect
Neglect Bryce often acts overly confident and daring
Bryce often acts overly confident and daring Whats salutary neglect
Whats salutary neglect Egregious neglect definition
Egregious neglect definition