What Matters To You Matters To Us Challenges












- Slides: 71
What Matters To You, Matters To Us Challenges in supporting patient-centred interdisciplinary care. Northland’s e-shared care experience
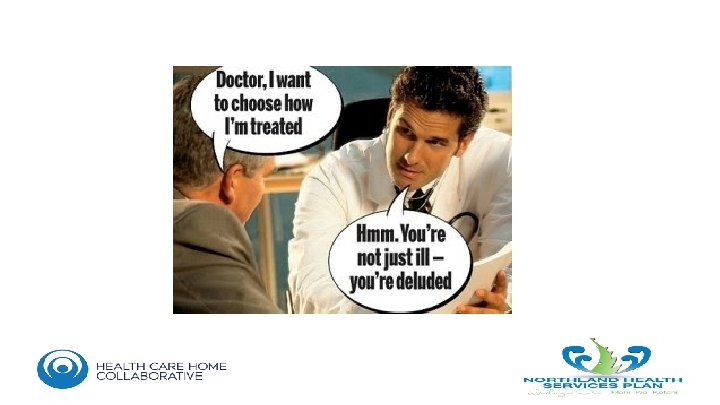




HCH Practices want to be: • Person centred (not disease centred) • Continuous relationships over time • Coordinating access to other services • Comprehensive – most of the care most people need most of the time
HCH is an Ethos • • • Problem Solving Learning to Learn Capability to make intelligent choices It’s not really about being different but doing things better We do have control of our own systems and performance • Exercising Personal Responsibility – TAKE THE PATIENT TEST
Pass the Patient Test • • Take a room full of your patients Explain how you currently deliver them “care” Ask them if they think that’s reasonable and defensible Likely then apologise and consider actually “caring for them” • TAKE THE PATIENT TEST with patient portals, telephone triage, HCH model ……. . ? Shared Care
I can plan my care with people who understand me and my carer(s), allow me control, and bring together services to achieve the outcomes important to me. ‘Narrative for person-centred coordinated care: summary statement’, National Voices and Think Local Act Personal 2013
What Matters to You, Matters to Us The Challenges Patient Centred vs. Provider Buy-in Funding/Investment Landscape IT Limitations Matters in Northland
What Matters to You, Should Matter to Us The Challenges Patient Centred vs. Provider Buy-in Funding/Investment Landscape IT Limitations Matters in Northland
What Matters to You, Should Matter to Us The Challenges Patient Centred vs. Provider Buy-in Funding/Investment Landscape IT Limitations Matters in Northland
The Wise Words of Don Berwick ‘There needs to be a radical redesign to move the focus of health from a quality improvement health focus to a courageous pursuit of wellbeing’
None of us are as smart as all of us.
Shared Care and SDH • Healthcare isn’t about medicine/treatment and procedures • Health is about well-being and care is about “what matters to you” • Without a paradigm shift to “what matters to patients”, collaboration and a fit for purpose workforce we are just going to frustrate patients and burn out providers • It’s the 10% we aren’t doing that will make 90% of the well-being gain • Don’t do screening if you don’t have treatment options
Burnout Matters

Understanding the Relationship Between Social Determinants of Health and Physician Burnout: the US Context New Zealand HCH Webinar November 2018 J. Nwando Olayiwola, MD, MPH, FAAFP CEO, Inspire Health Solutions, LLC Chief Clinical Transformation Officer, Rubicon. MD Associate Physician & Clinical Instructor, University of California, San Francisco Clinical Instructor, Columbia University Center for Family & Community Medicine Twitter and IG: @Dr. Nwando
Background: Burnout in US PCPs
SDH and PCPs/GPs Leading causes of workplace stress for safety net clinicians in US were insufficient resources for patients and within their health Few resources exist to address SDH systematically and comprehensively in underserved settings Dimensions of burnout may be pronounced for GPs working with vulnerable populations, organisational resources are low; emotional and material needs of patients are high Sources: 1. Gottlieb, L. , Sandel, M. , & Adler, N. E. (2013). Collecting and applying data on social determinants of health in health care settings. JAMA Intern Med, 173(11), 1017 -1020. doi: 10. 1001/jamainternmed. 2013. 560 2. Hayashi, A. S. , Selia, E. , & Mc. Donnell, K. (2009). Stress and provider retention in underserved communities. J Health Care Poor Underserved, 20(3), 597 -604.
Objective • To understand relationships between clinician perceptions of capacity to address SDH and clinician burnout
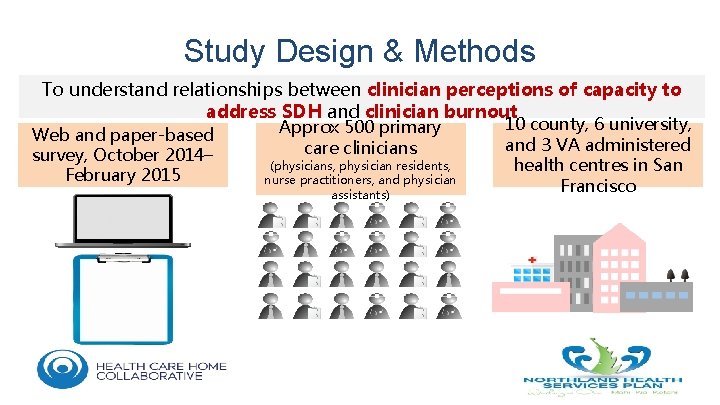
Study Design & Methods To understand relationships between clinician perceptions of capacity to address SDH and clinician burnout Web and paper-based survey, October 2014– February 2015 Approx 500 primary care clinicians (physicians, physician residents, nurse practitioners, and physician assistants) 10 county, 6 university, and 3 VA administered health centres in San Francisco
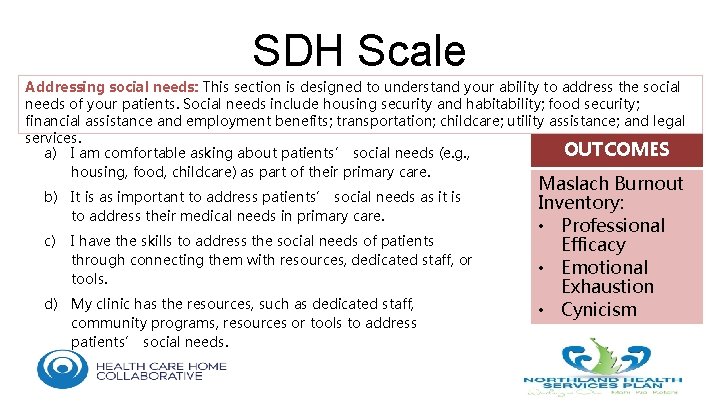
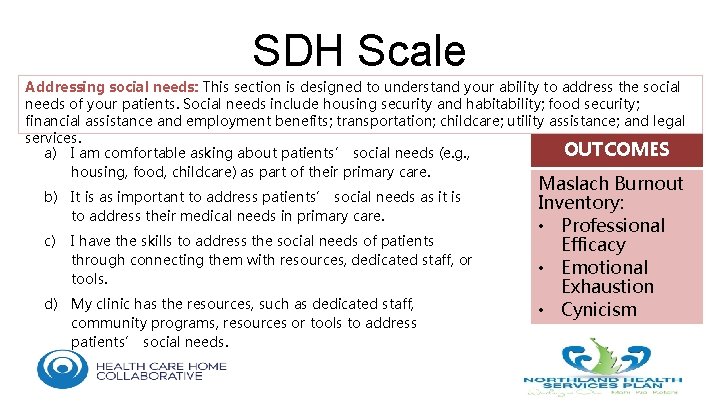
SDH Scale Addressing social needs: This section is designed to understand your ability to address the social needs of your patients. Social needs include housing security and habitability; food security; financial assistance and employment benefits; transportation; childcare; utility assistance; and legal services. OUTCOMES a) I am comfortable asking about patients’ social needs (e. g. , housing, food, childcare) as part of their primary care. b) It is as important to address patients’ social needs as it is to address their medical needs in primary care. c) I have the skills to address the social needs of patients through connecting them with resources, dedicated staff, or tools. d) My clinic has the resources, such as dedicated staff, community programs, resources or tools to address patients’ social needs. Maslach Burnout Inventory: • Professional Efficacy • Emotional Exhaustion • Cynicism
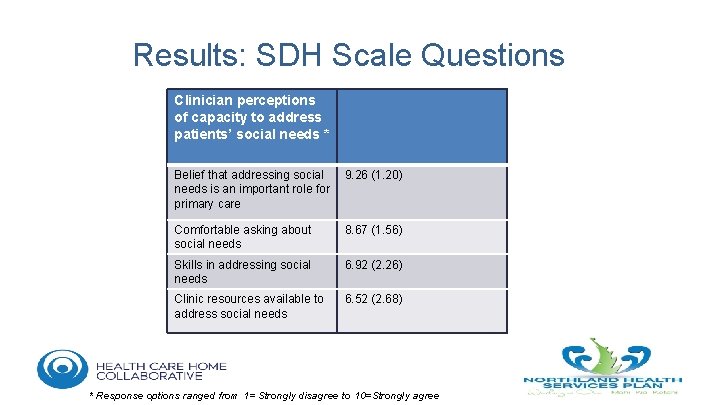
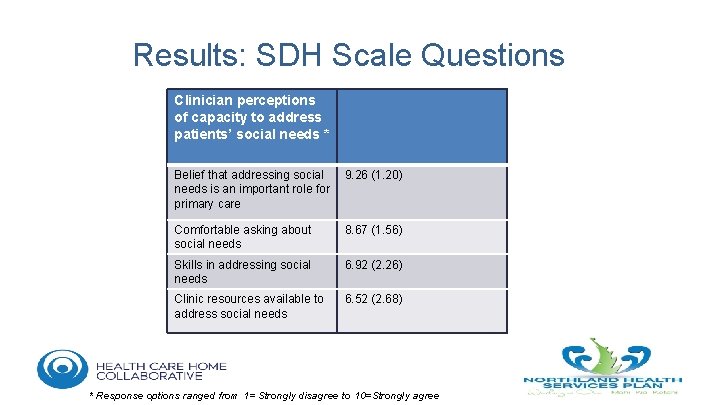
Results: SDH Scale Questions Clinician perceptions of capacity to address patients’ social needs * Belief that addressing social needs is an important role for primary care 9. 26 (1. 20) Comfortable asking about social needs 8. 67 (1. 56) Skills in addressing social needs 6. 92 (2. 26) Clinic resources available to address social needs 6. 52 (2. 68) * Response options ranged from 1= Strongly disagree to 10=Strongly agree
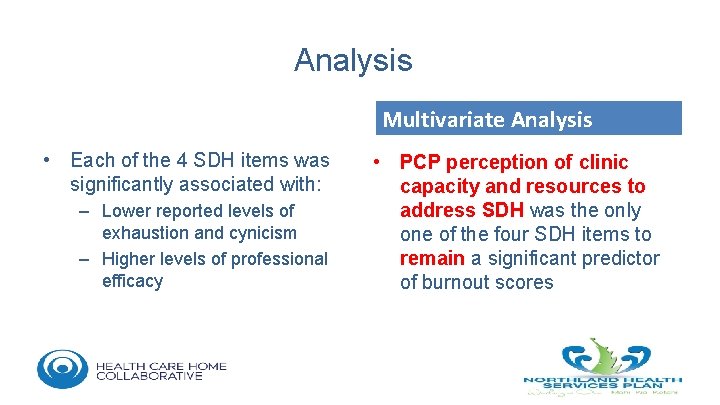
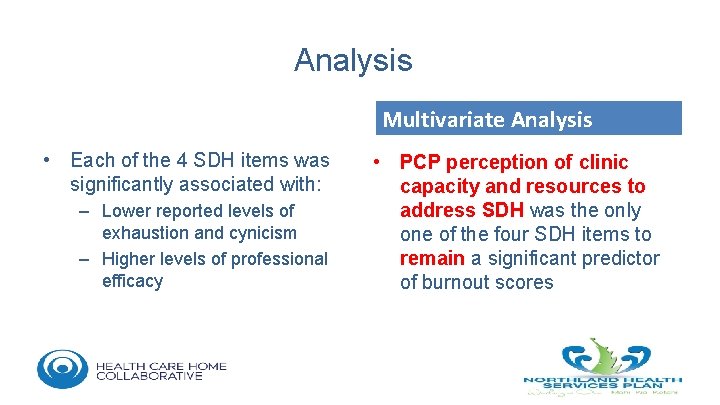
Analysis Multivariate Analysis • Each of the 4 SDH items was significantly associated with: – Lower reported levels of exhaustion and cynicism – Higher levels of professional efficacy • PCP perception of clinic capacity and resources to address SDH was the only one of the four SDH items to remain a significant predictor of burnout scores
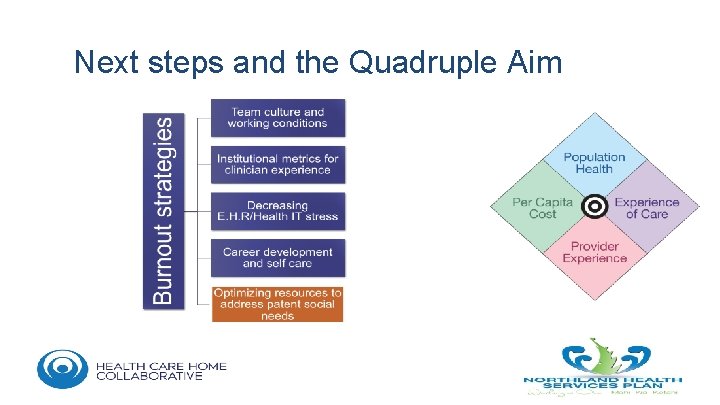
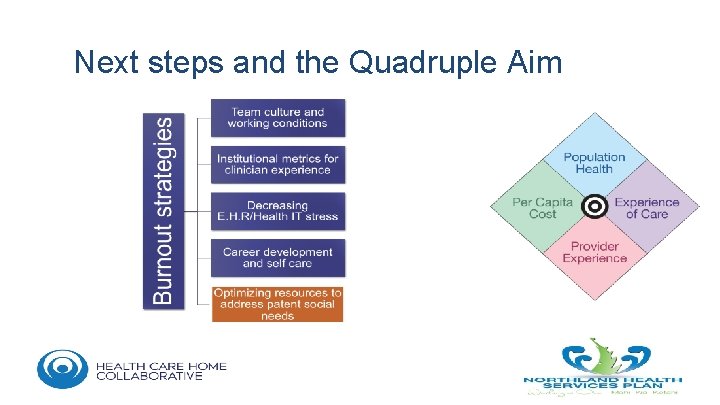
Next steps and the Quadruple Aim

What Matters to You, Should Matter to Us The Challenges Patient Centred vs. Provider Buy-in Funding/Investment Landscape IT Limitations Matters in Northland


Northern Region Long Term Investment Plan Combined Board Workshop 7 August 2017 34
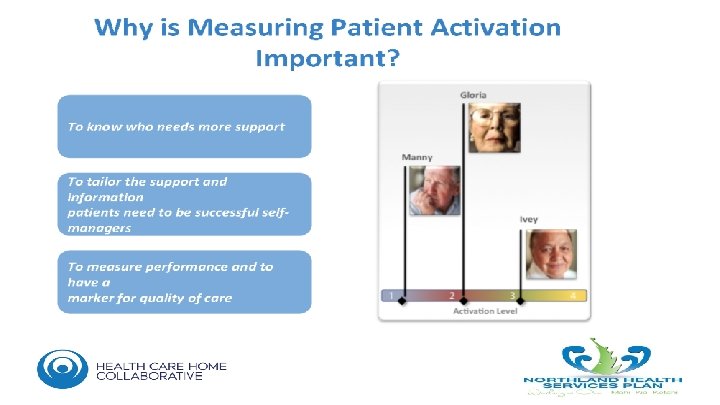
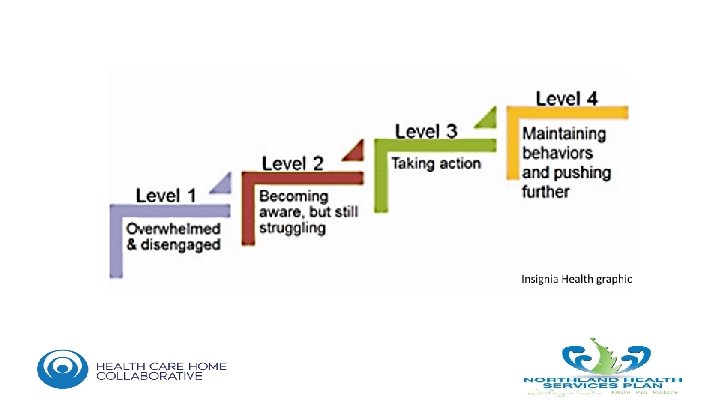
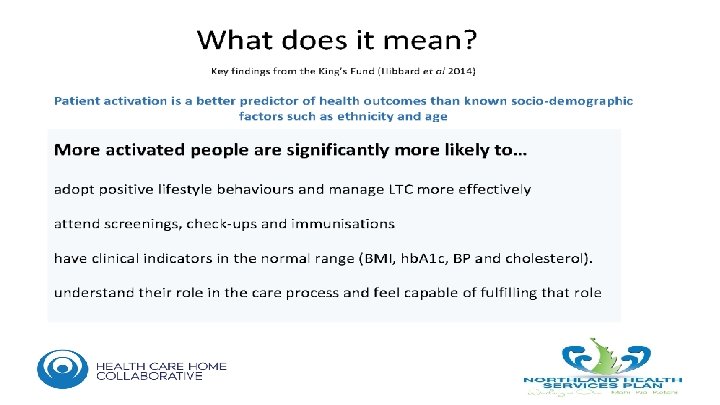
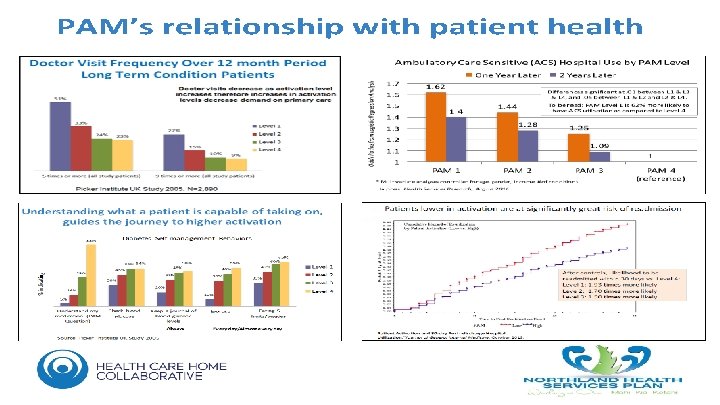
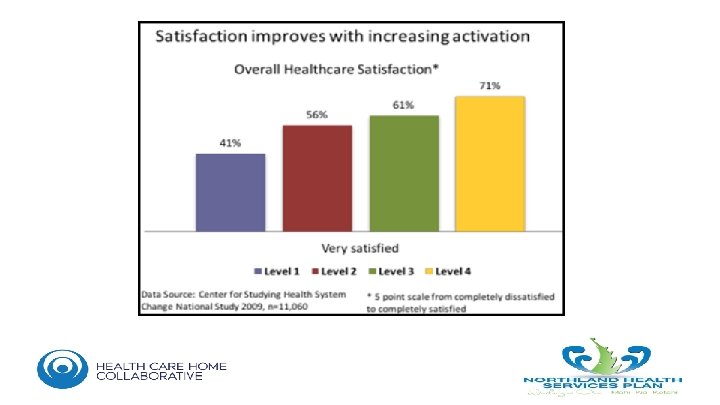
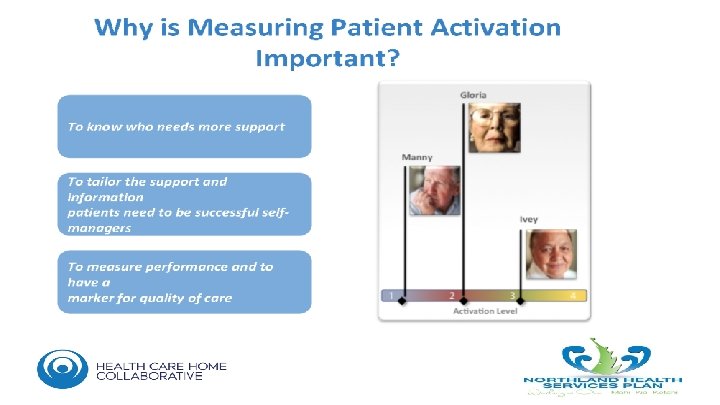
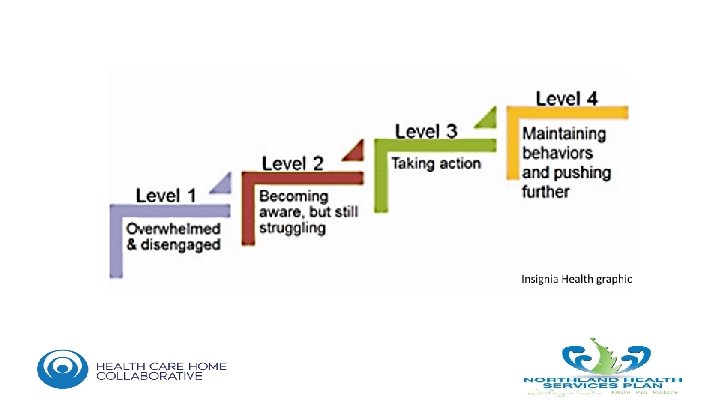
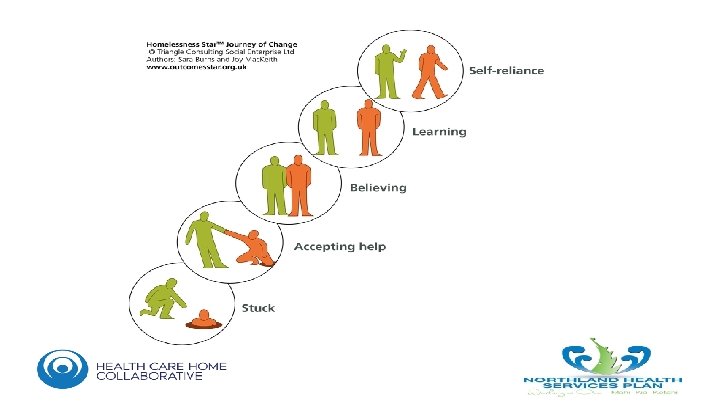
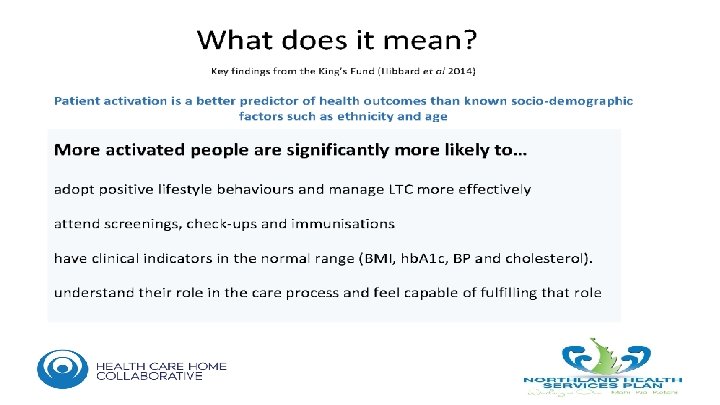
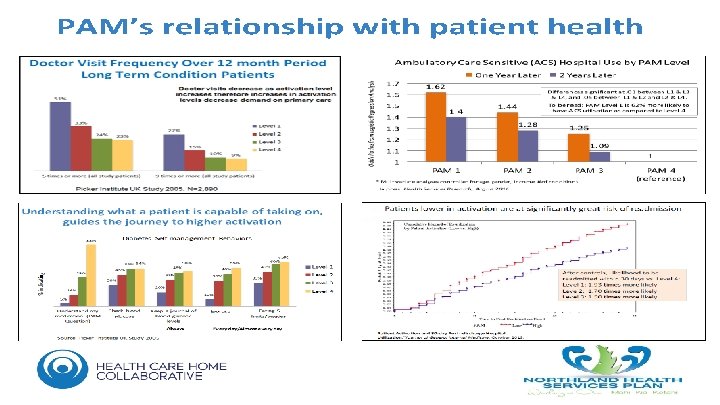
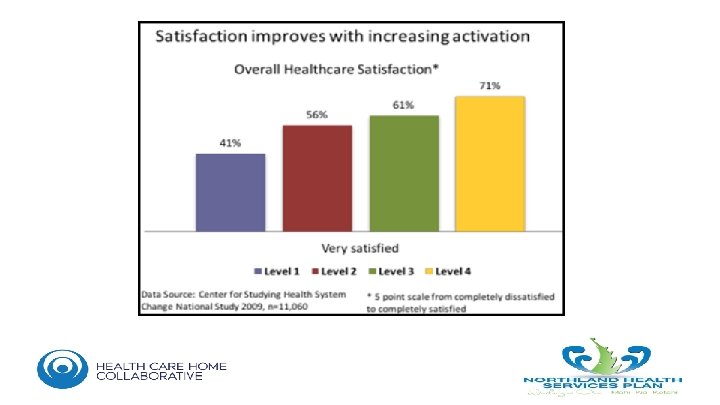
Doing Things Differently and Working Together The report from the Nuffield Trust signals we need to focus on model of care changes, and increased health sector integration and collaboration across the Northern Region • The Nuffield Report provided a high level overview of the evidence to guide future health system planning. • The consistent message was the need for a shift in the balance of care from the hospital into the community, both to improve health outcomes in our population and avoid the need for hospital care. • They see a model of care shift towards a proactive, networked model which activates patients to be more involved in their own health and care. • Their evidence is arranged along the care journey, suggesting improvements across the system: − Patient activation initiatives to engage our population in keeping themselves healthy; − Proactive care to keep our population out of hospitals, and; − Networked models of care to deliver an integrated, collaborative service once the patient is in the system. • This should be supported by investments balanced across public health, primary and community care, and hospital based services, with a focus on: − Cost-effective public health interventions. − Community based alternatives to admission − Different types of hospital based services − Increased productivity across the whole system 35
Doing Things Differently and Working Together The report from the Nuffield Trust signals we need to focus on model of care changes, and increased health sector integration and collaboration across the Northern Region • The Nuffield Report provided a high level overview of the evidence to guide future health system planning. • The consistent message was the need for a shift in the balance of care from the hospital into the community, both to improve health outcomes in our population and avoid the need for hospital care. • They see a model of care shift towards a proactive, networked model which activates patients to be more involved in their own health and care. • Their evidence is arranged along the care journey, suggesting improvements across the system: − Patient activation initiatives to engage our population in keeping themselves healthy; − Proactive care to keep our population out of hospitals, and; − Networked models of care to deliver an integrated, collaborative service once the patient is in the system. • This should be supported by investments balanced across public health, primary and community care, and hospital based services, with a focus on: − Cost-effective public health interventions. − Community based alternatives to admission − Different types of hospital based services − Increased productivity across the whole system 36
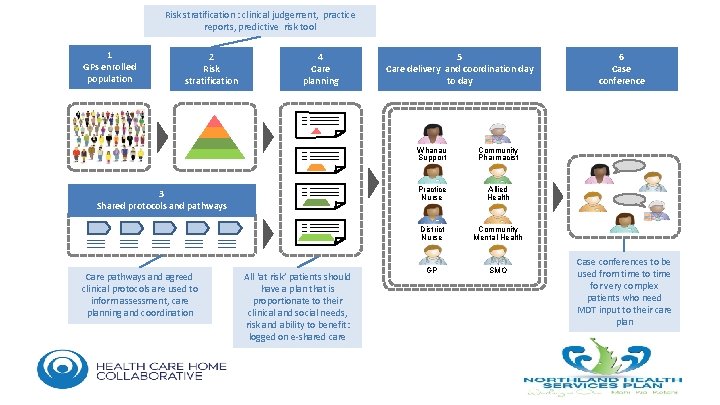
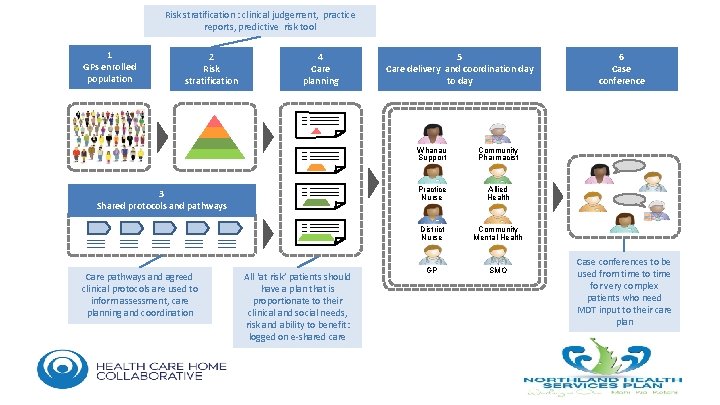
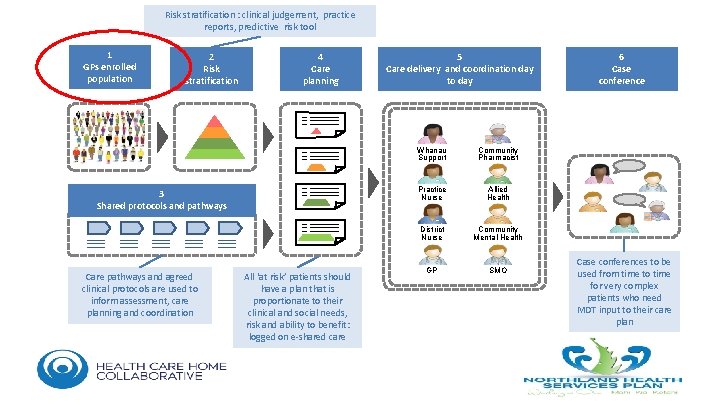
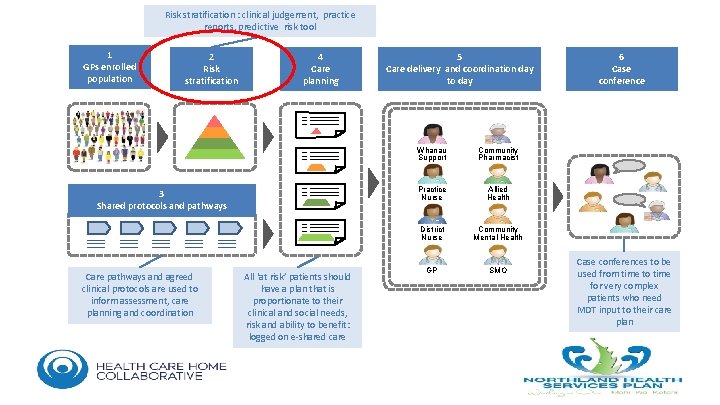
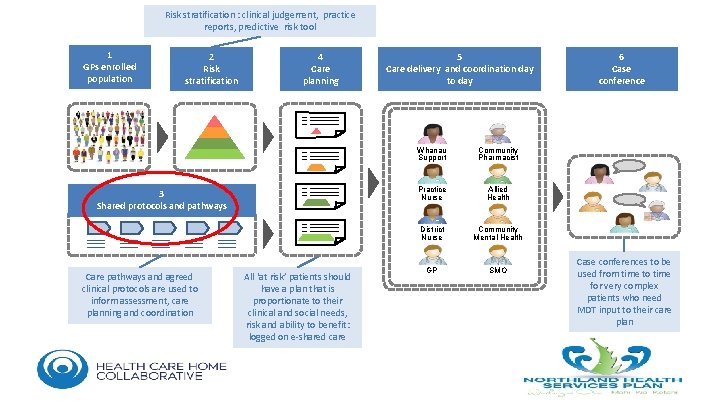
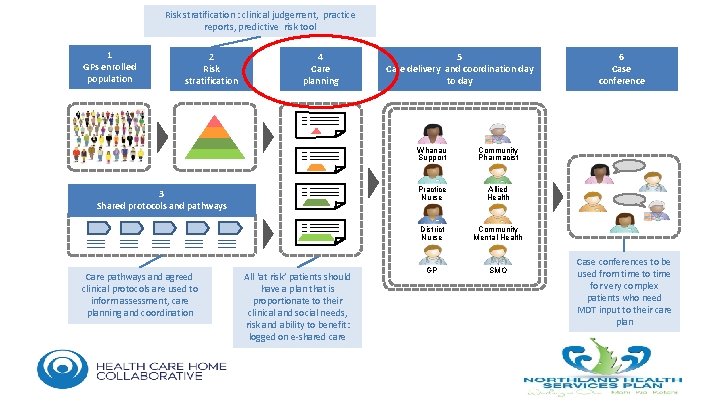
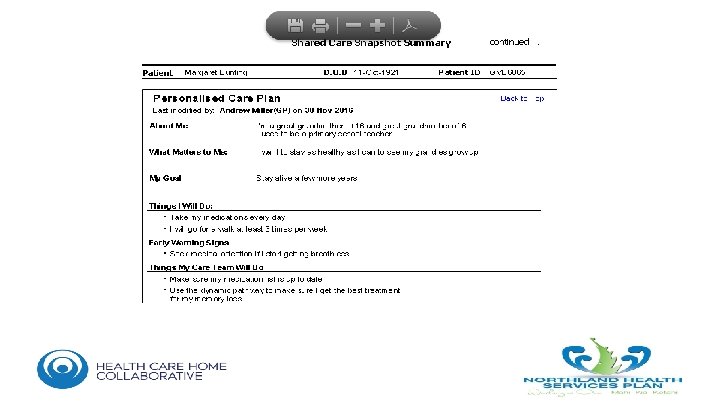
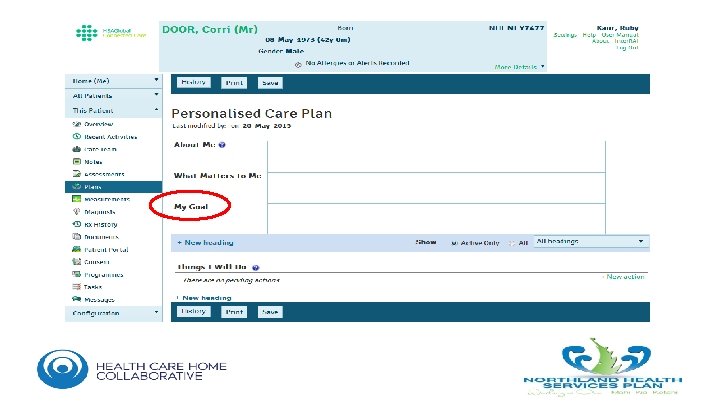
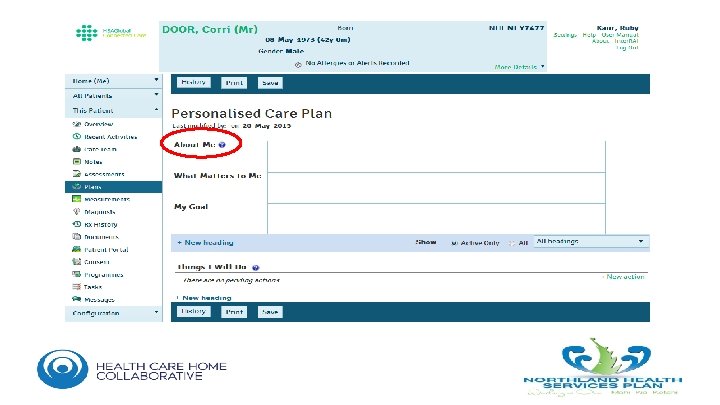
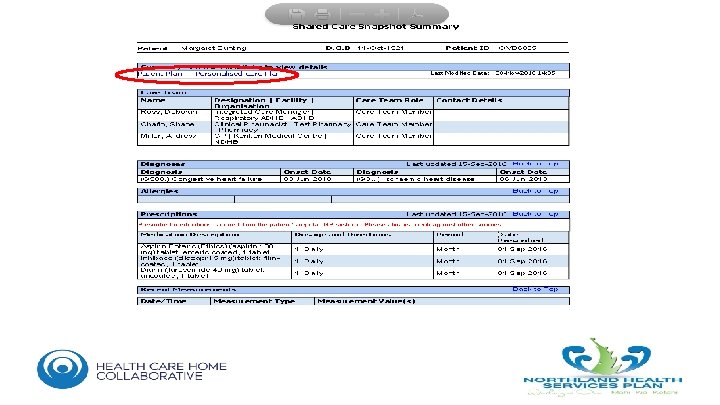
Risk stratification : clinical judgement, practice reports, predictive risk tool 1 GPs enrolled population 2 Risk stratification 4 Care planning 3 Shared protocols and pathways Care pathways and agreed clinical protocols are used to inform assessment, care planning and coordination All ‘at risk’ patients should have a plan that is proportionate to their clinical and social needs, risk and ability to benefit: logged on e-shared care 5 Care delivery and coordination day to day Whanau Support Community Pharmacist Practice Nurse Allied Health District Nurse Community Mental Health GP SMO 6 Case conferences to be used from time to time for very complex patients who need MDT input to their care plan
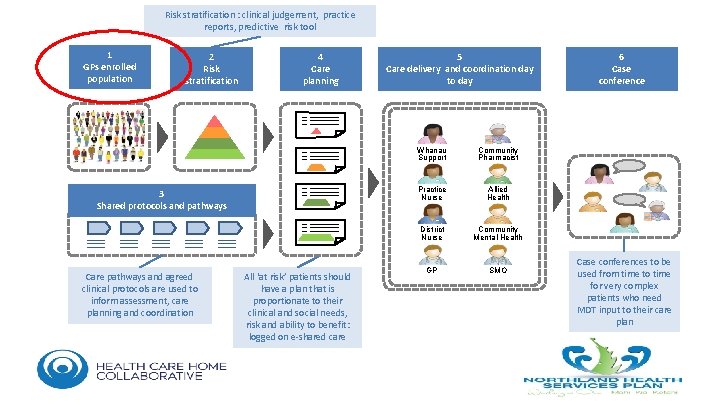
Risk stratification : clinical judgement, practice reports, predictive risk tool 1 GPs enrolled population 2 Risk stratification 4 Care planning 3 Shared protocols and pathways Care pathways and agreed clinical protocols are used to inform assessment, care planning and coordination All ‘at risk’ patients should have a plan that is proportionate to their clinical and social needs, risk and ability to benefit: logged on e-shared care 5 Care delivery and coordination day to day Whanau Support Community Pharmacist Practice Nurse Allied Health District Nurse Community Mental Health GP SMO 6 Case conferences to be used from time to time for very complex patients who need MDT input to their care plan
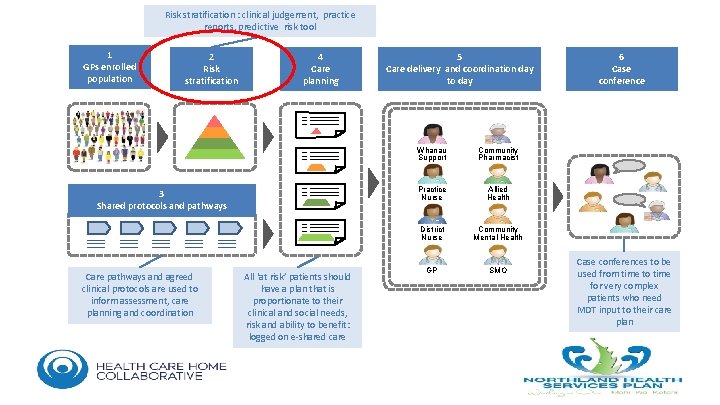
Risk stratification : clinical judgement, practice reports, predictive risk tool 1 GPs enrolled population 2 Risk stratification 4 Care planning 3 Shared protocols and pathways Care pathways and agreed clinical protocols are used to inform assessment, care planning and coordination All ‘at risk’ patients should have a plan that is proportionate to their clinical and social needs, risk and ability to benefit: logged on e-shared care 5 Care delivery and coordination day to day Whanau Support Community Pharmacist Practice Nurse Allied Health District Nurse Community Mental Health GP SMO 6 Case conferences to be used from time to time for very complex patients who need MDT input to their care plan
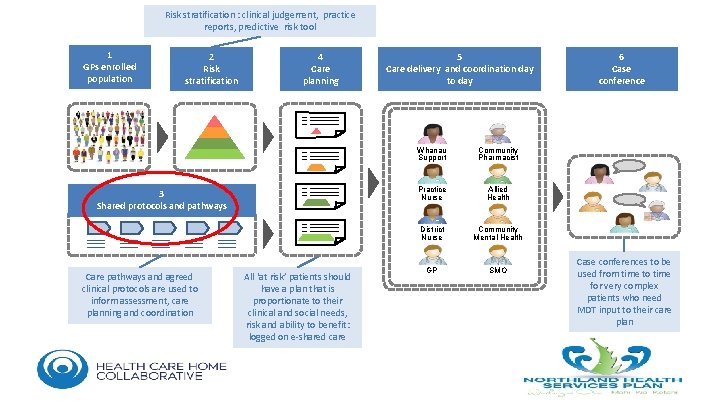
Risk stratification : clinical judgement, practice reports, predictive risk tool 1 GPs enrolled population 2 Risk stratification 4 Care planning 3 Shared protocols and pathways Care pathways and agreed clinical protocols are used to inform assessment, care planning and coordination All ‘at risk’ patients should have a plan that is proportionate to their clinical and social needs, risk and ability to benefit: logged on e-shared care 5 Care delivery and coordination day to day Whanau Support Community Pharmacist Practice Nurse Allied Health District Nurse Community Mental Health GP SMO 6 Case conferences to be used from time to time for very complex patients who need MDT input to their care plan
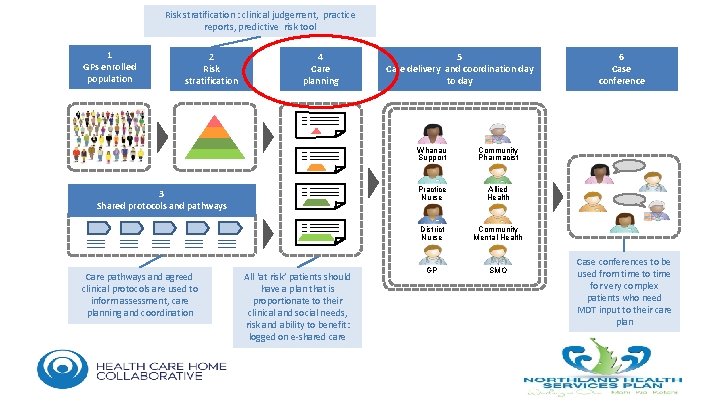
Risk stratification : clinical judgement, practice reports, predictive risk tool 1 GPs enrolled population 2 Risk stratification 4 Care planning 3 Shared protocols and pathways Care pathways and agreed clinical protocols are used to inform assessment, care planning and coordination All ‘at risk’ patients should have a plan that is proportionate to their clinical and social needs, risk and ability to benefit: logged on e-shared care 5 Care delivery and coordination day to day Whanau Support Community Pharmacist Practice Nurse Allied Health District Nurse Community Mental Health GP SMO 6 Case conferences to be used from time to time for very complex patients who need MDT input to their care plan

Hit the target but miss the mark


What Matters to You, Should Matter to Us The Challenges Patient Centred vs. Provider Buy-in Funding/Investment Landscape IT Limitations Matters in Northland
What Matters to You, Matters to Us The Challenges Patient Centred vs. Provider Buy-in Funding/Investment Landscape IT Limitations Matters in Northland
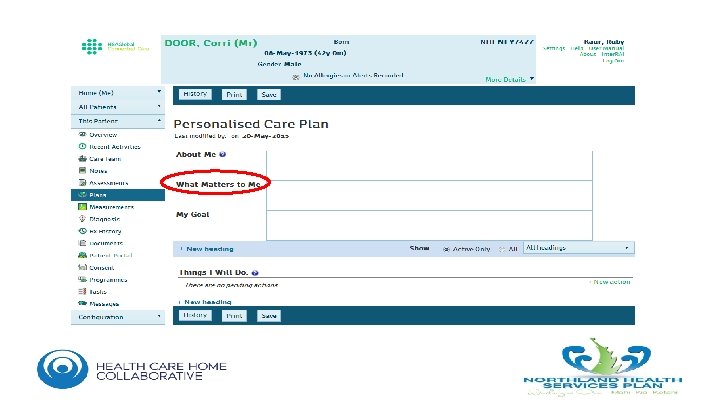
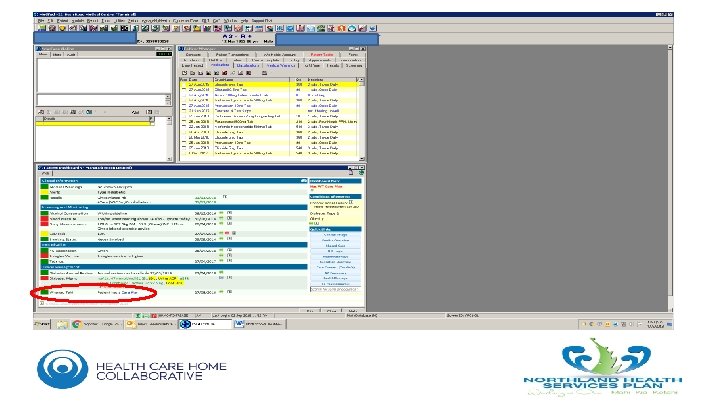
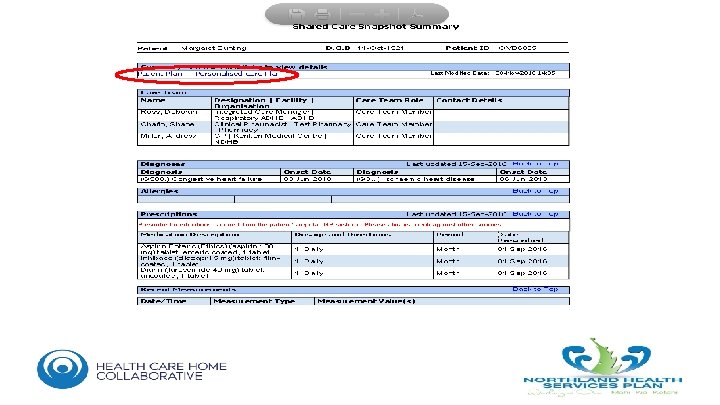
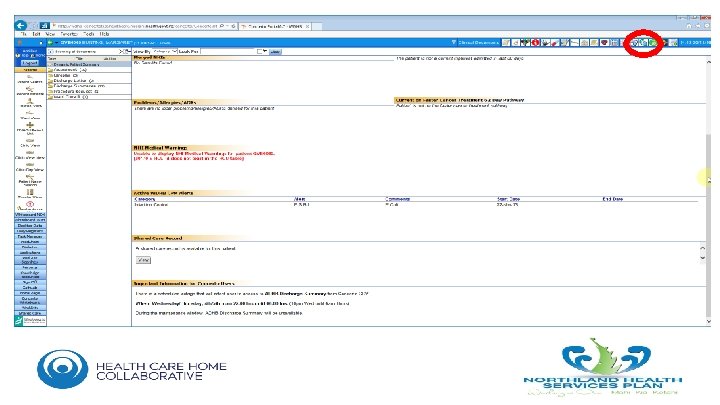
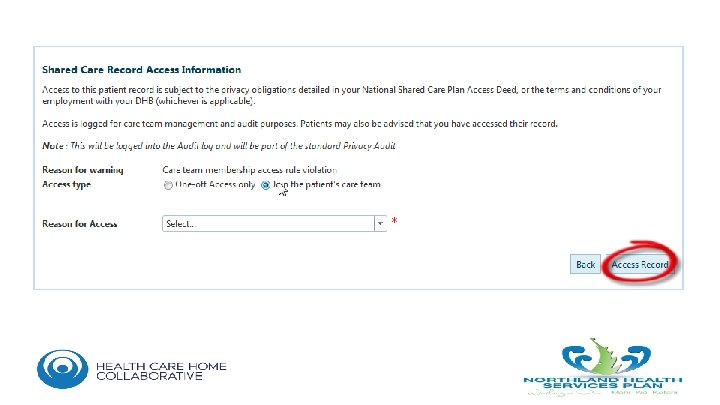
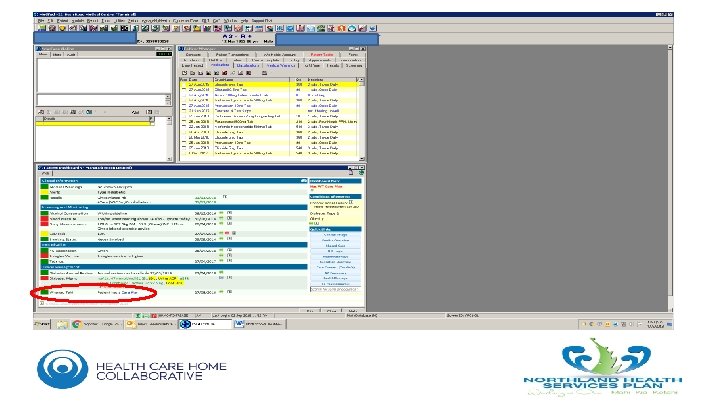
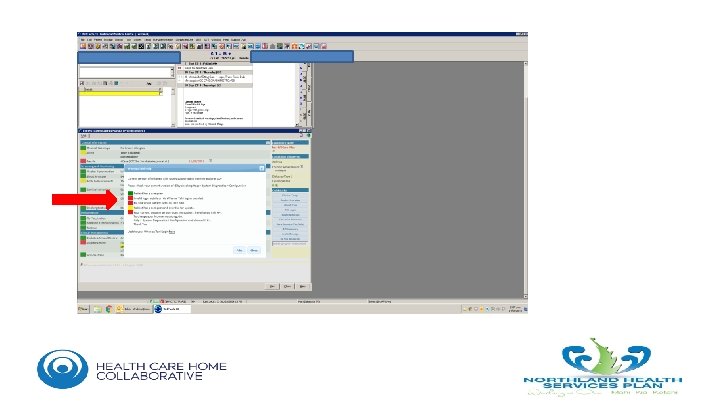
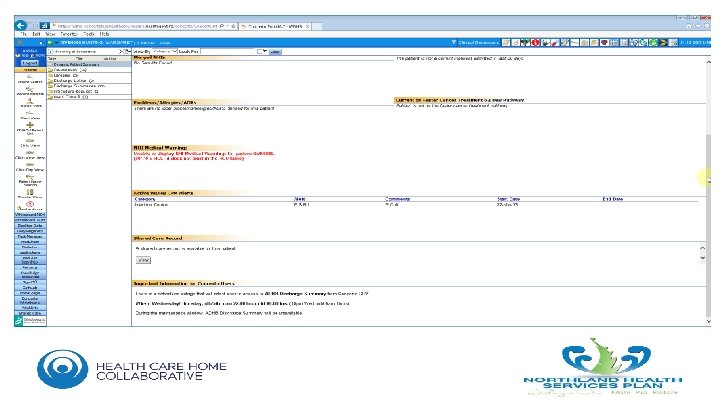
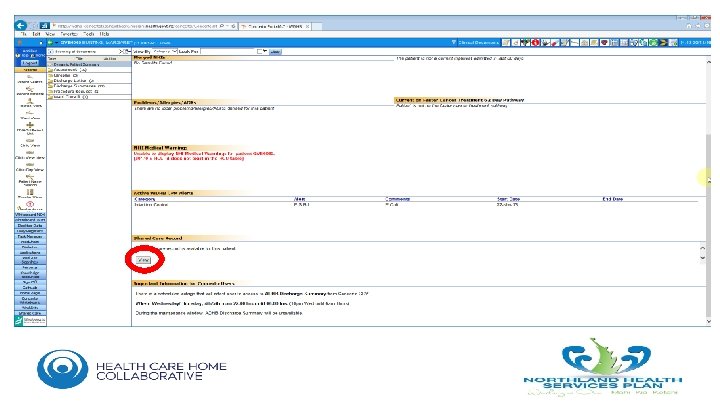
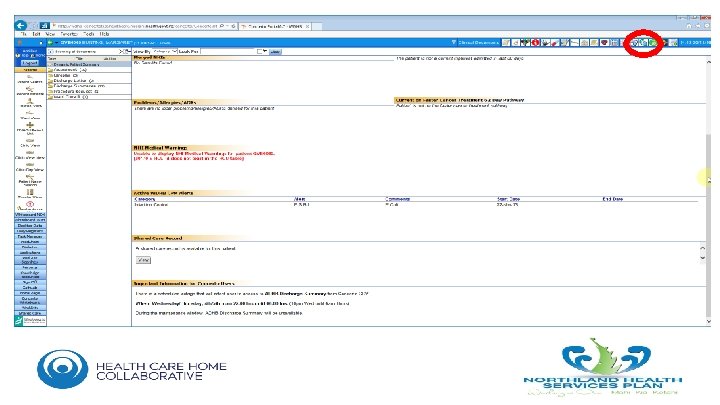
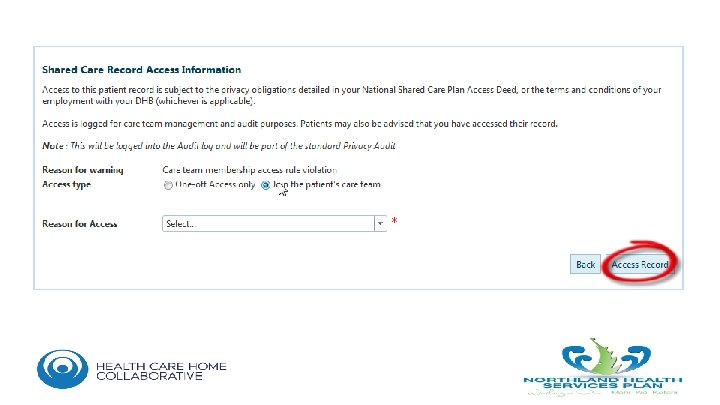
Whanau Tahi • All Northland 160, 000 population now uploaded • All GP, community pharmacy and Maori Health providers have access • Rolling out DHB early adopters- 220 users • Dealing with interoperability problems
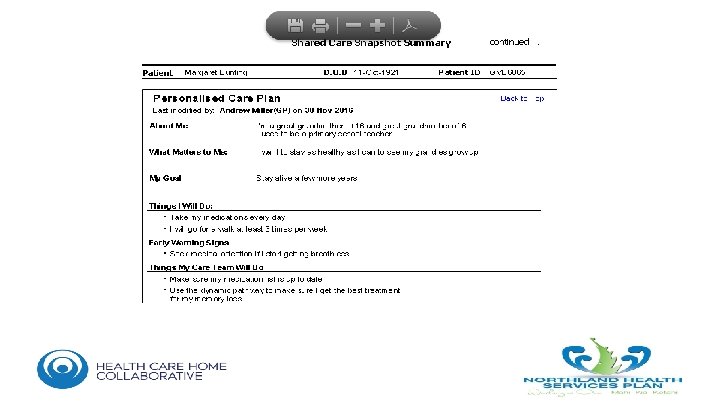

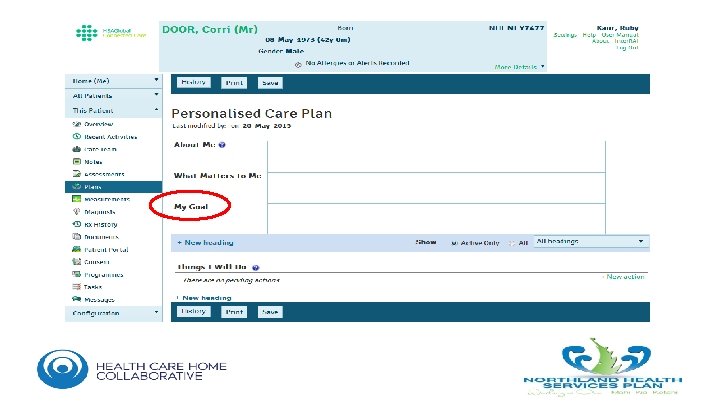
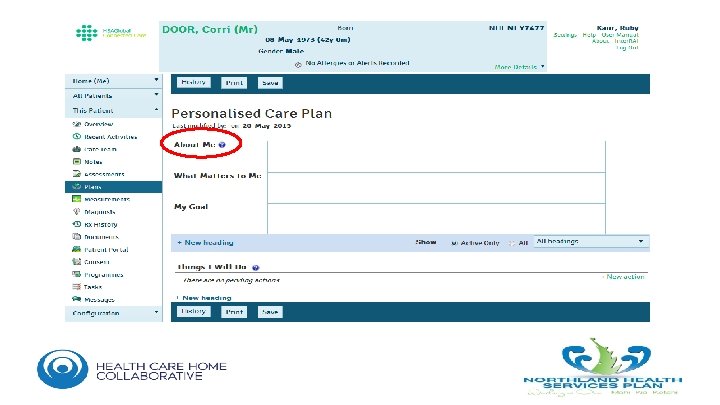
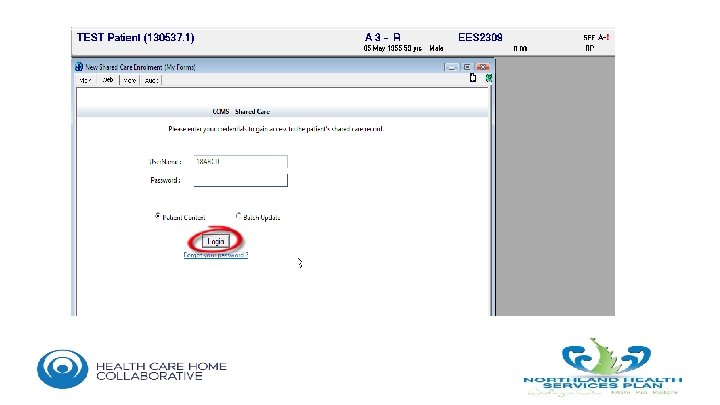
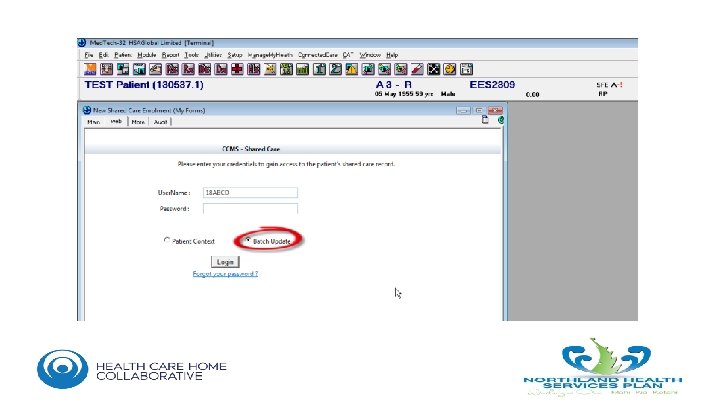
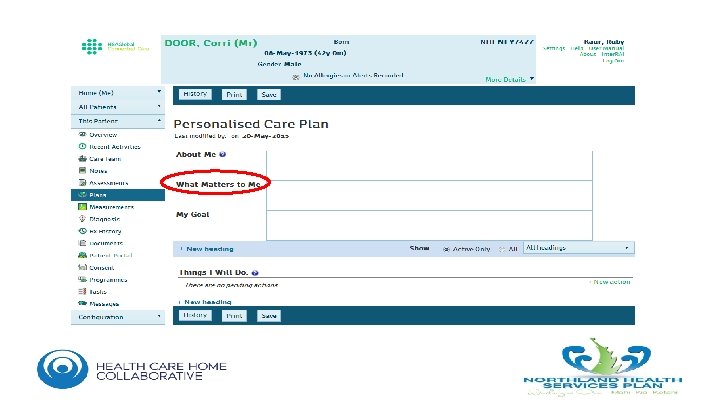
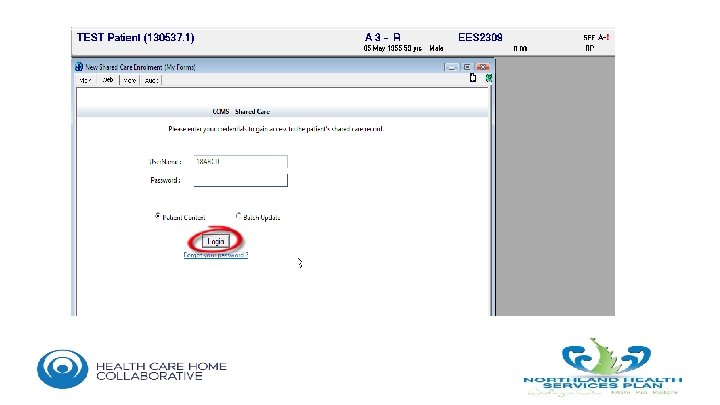
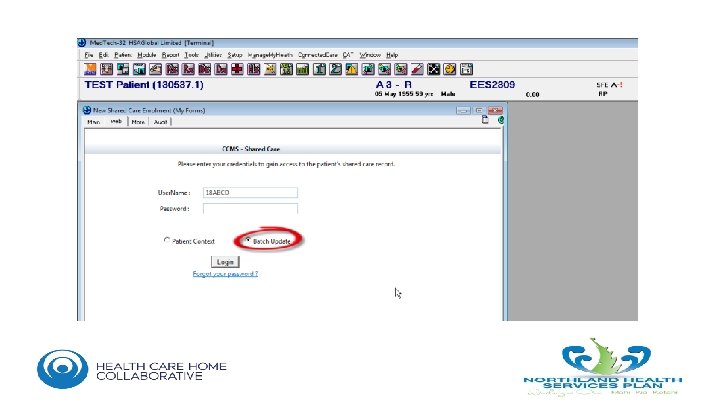
What Matters to You, Matters to Me • • Complete Single Sign On and Batch Update work. Patient Portal for e-Shared Care and ACPs Interoperable Portals HISO open API standards for e-SCPs/ACP- interoperability Investigate Patient Activation Measure tool implementation Recognise that “burn out” is an important disabler Accept failure if necessary (but not yet)
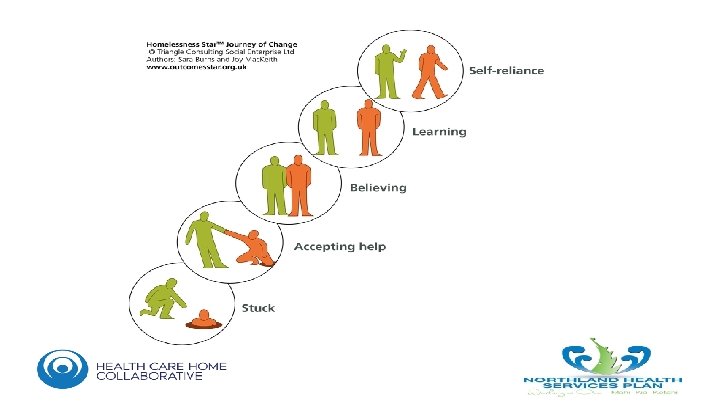
Resources for good Shared Care • • • A named care co-ordinator/key person An e-Shared Care Plan so we’re all “on the same page” Plans are pro-active and person driven, so we can plan ahead Provide flexible funding to the person and the provider Use Navigators, Peer Support, Health Coaches and the Community – to douse the “burn out”
What Matters to You, Matters to Us