What is Reproduction All living things reproduce Reproduction
- Slides: 33
What is Reproduction? All living things reproduce. Reproduction — the process by which organisms make more organisms like themselves sets living things apart from nonliving things. the reproductive system is essential to keeping a species alive, unlike other body systems it's not essential to keeping an individual alive.
Human Reproductive Process 2 kinds of sex cells are involved: 1. Male- sperm 2. Female - the egg or ovum meet in the female's reproductive system to create a new individual. Sperm + Egg = ****Both the male and female reproductive systems are essential for reproduction. ****
Genes Humans, like other organisms, pass certain characteristics of themselves to the next generation through their GENES the special carriers of human traits. Genes come from the males sperm and the females egg The genes males and females pass along to their offspring are what make kids similar to others in their family and also what make each child unique.
The Male Reproductive System
Function of the MRS The purpose of the organs of the MRS is to perform the following functions: To produce, maintain, and transport sperm (the male reproductive cells) and protective fluid (semen) To discharge sperm within the female reproductive tract during sex To produce and secrete male sex hormones responsible for maintaining the male reproductive system, which help a boy develop into a sexually mature man during puberty.
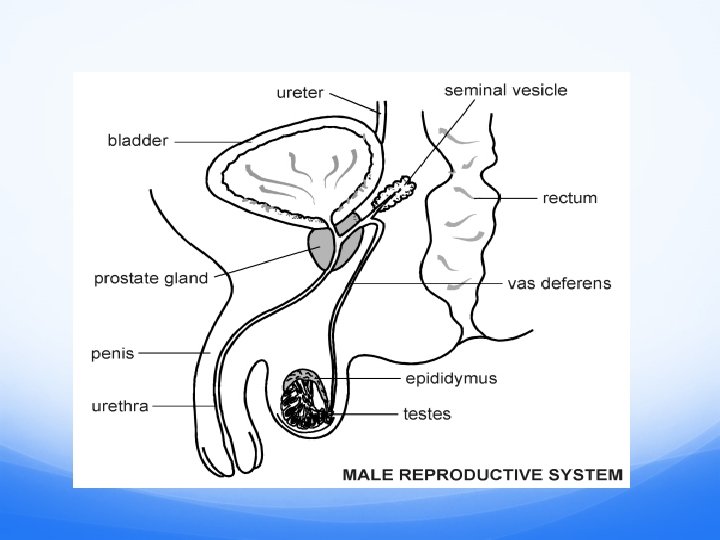
Male Genitals Unlike the female, whose sex organs are located entirely within the pelvis, the male has reproductive organs, or genitals, that are both inside and outside the pelvis. The male genitals include: the testicles the duct system which is made up of: epididymis and the vas deferens the accessory glands, which include: the seminal vesicles and prostate gland the penis
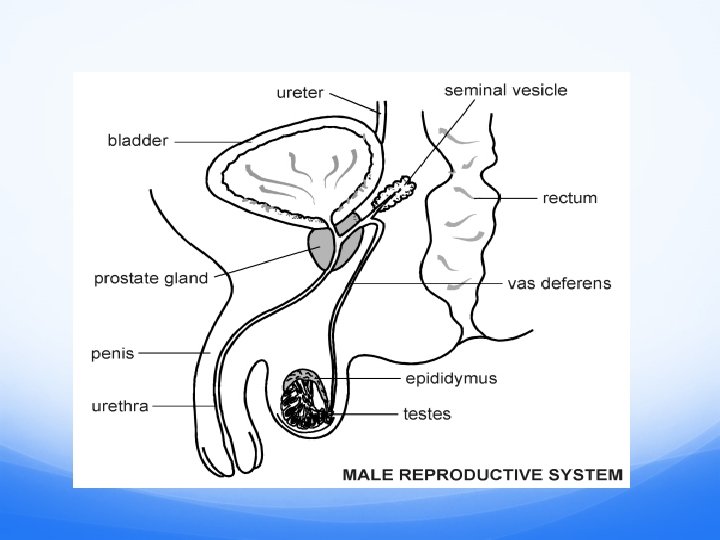
Testicles Oval-shaped and grow to be about 2 inches in length and 1 inch in diameter. Function: Produce main male hormone = testosterone. Generate sperm The testicles descend during the 7 th month of fetal life. Cryptorchidism: condition if the testes do not descend. Hormone therapy or surgery may be required to relocate the testes to the scrotum. The surgery should be done by the time the boy is 4 or 5 years old.
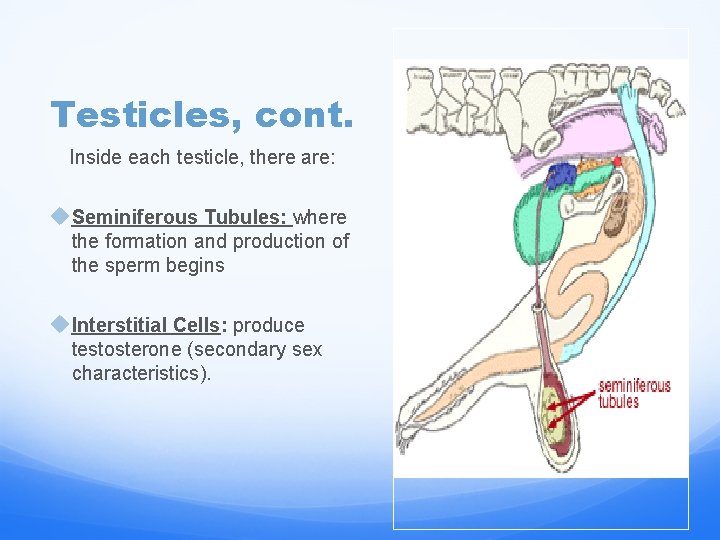
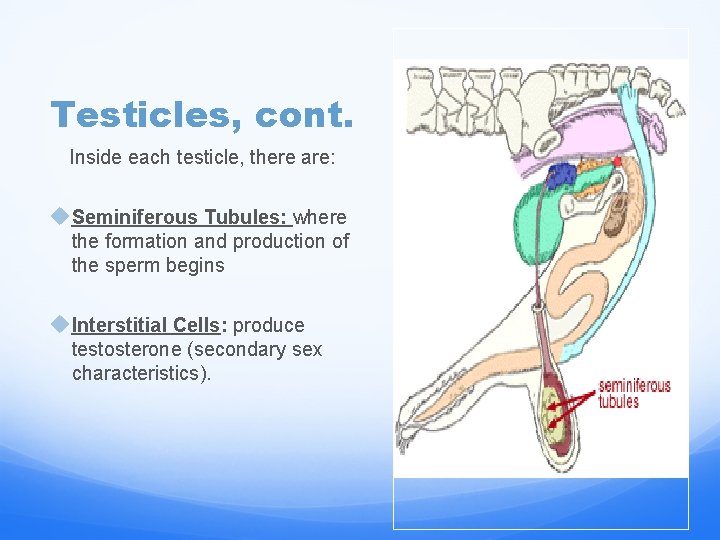
Testicles, cont. Inside each testicle, there are: u. Seminiferous Tubules: where the formation and production of the sperm begins u. Interstitial Cells: produce testosterone (secondary sex characteristics).
HORMONES Hormones: special chemicals that start, speed up, slow down, or stop activities inside the body. The testes produce sperm cells and the hormone testosterone. Testosterone controls male sexual development as well as the development of male secondary sex characteristics during puberty. Secondary Sex Characteristics: Physical changes that accompany the onset of puberty. Testicles enlarge Penis enlarges Pubic hair Height spurt Ejaculation Axillary hair (facial and body hair)
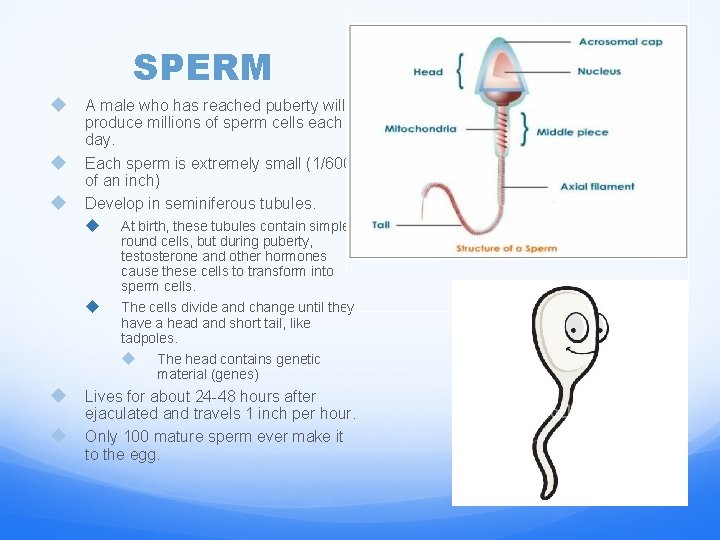
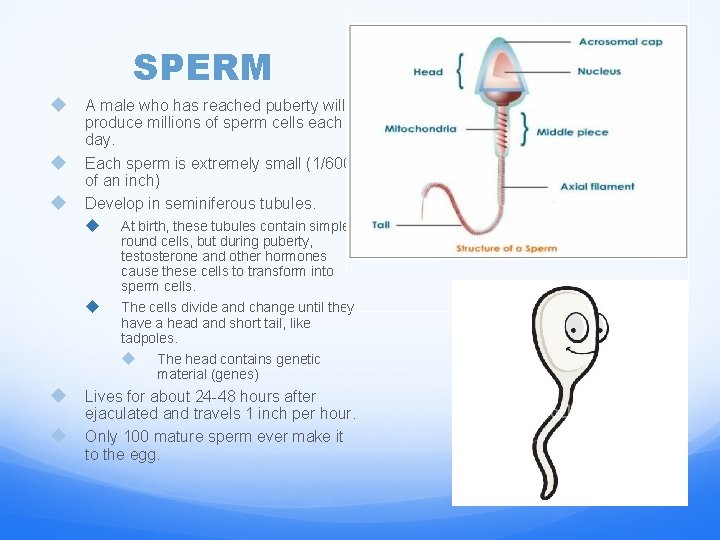
SPERM u u u A male who has reached puberty will produce millions of sperm cells each day. Each sperm is extremely small (1/600 of an inch) Develop in seminiferous tubules. u At birth, these tubules contain simple round cells, but during puberty, testosterone and other hormones cause these cells to transform into sperm cells. u The cells divide and change until they have a head and short tail, like tadpoles. u u u The head contains genetic material (genes) Lives for about 24 -48 hours after ejaculated and travels 1 inch per hour. Only 100 mature sperm ever make it to the egg.
Scrotum Loose pouch-like sac of skin that hangs behind and below the penis. contains the testicles (also called testes), as well as many nerves and blood vessels. The scrotum acts as a "climate control system" for the testes. Cremaster muscles: the muscles that elevate the testes and are located at the base of the scrotal sac. • • • Assist in keeping the testes temperature normal. When hot, muscles relax and the scrotal sac hangs away from the body. When cool, muscles contract and pull together to keep the testes warm. Testes must be kept 3 -5 degrees cooler then the body or they will not be able to produce sperm. A 2 -3 degree increase in temperature does occasionally result in temporary sterility in men, but fertility returns after a short time. a. Sterility: the inability to produce offspring. b. Fertility: the state of being capable of producing offspring.
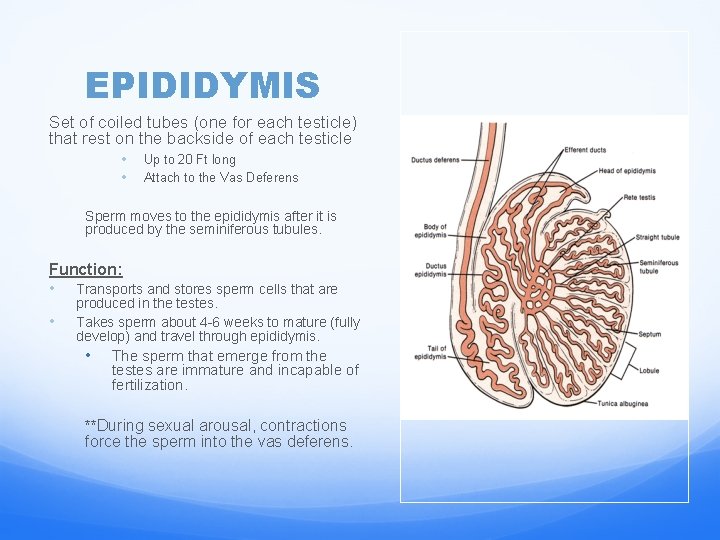
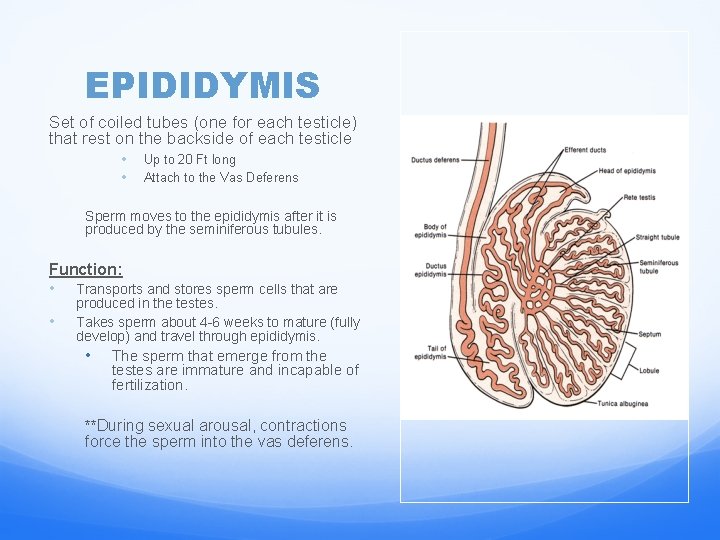
EPIDIDYMIS Set of coiled tubes (one for each testicle) that rest on the backside of each testicle • • Up to 20 Ft long Attach to the Vas Deferens Sperm moves to the epididymis after it is produced by the seminiferous tubules. Function: • Transports and stores sperm cells that are • produced in the testes. Takes sperm about 4 -6 weeks to mature (fully develop) and travel through epididymis. • The sperm that emerge from the testes are immature and incapable of fertilization. **During sexual arousal, contractions force the sperm into the vas deferens.
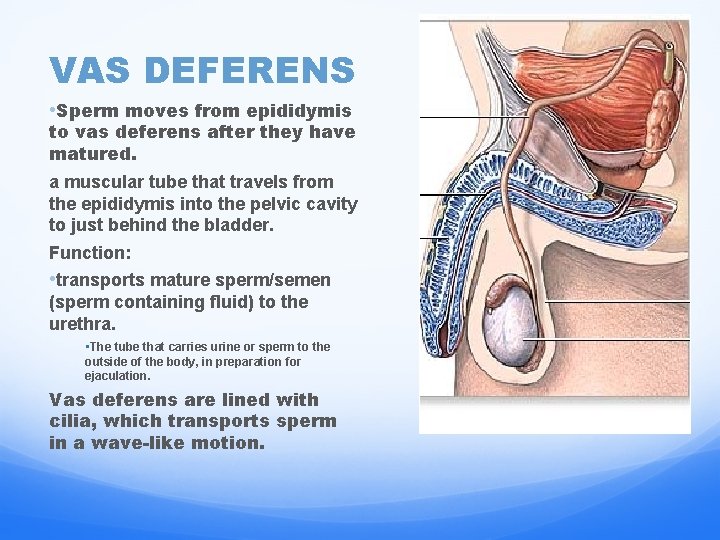
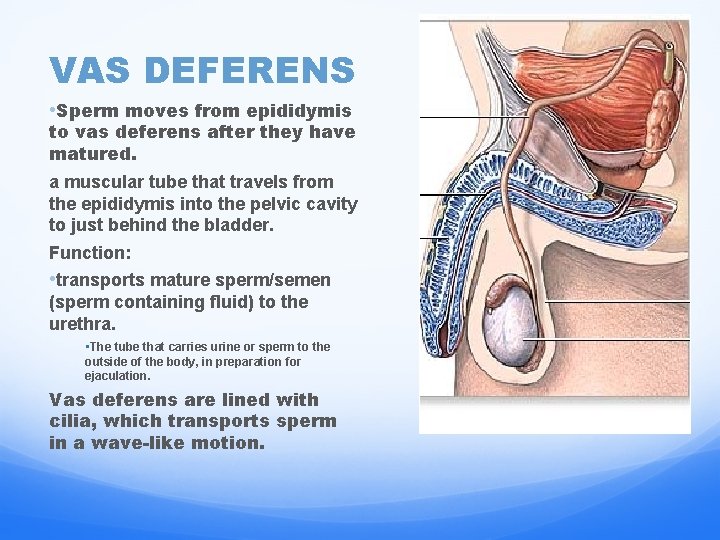
VAS DEFERENS • Sperm moves from epididymis to vas deferens after they have matured. a muscular tube that travels from the epididymis into the pelvic cavity to just behind the bladder. Function: • transports mature sperm/semen (sperm containing fluid) to the urethra. • The tube that carries urine or sperm to the outside of the body, in preparation for ejaculation. Vas deferens are lined with cilia, which transports sperm in a wave-like motion.
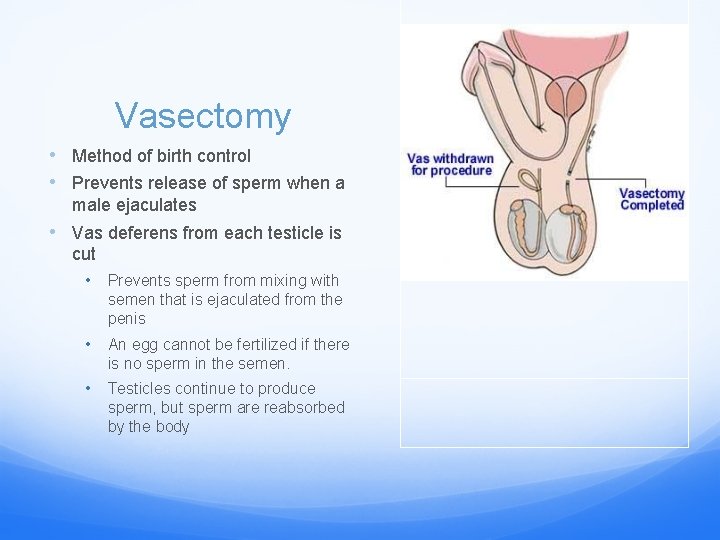
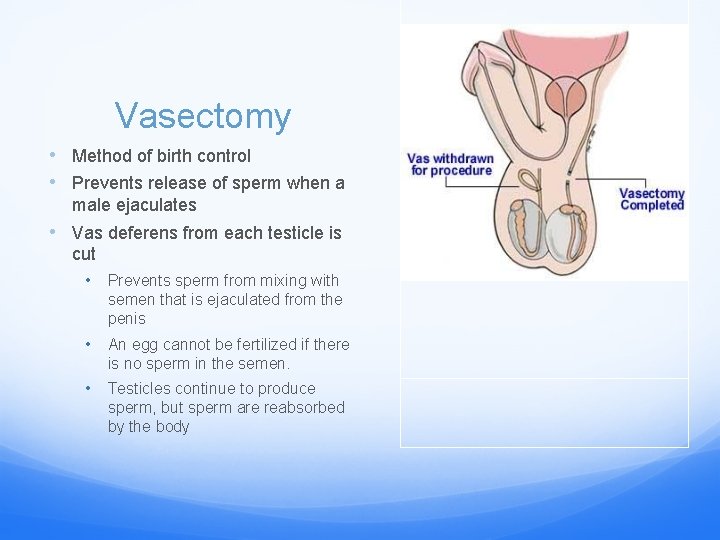
Vasectomy • Method of birth control • Prevents release of sperm when a male ejaculates • Vas deferens from each testicle is cut • Prevents sperm from mixing with semen that is ejaculated from the penis • An egg cannot be fertilized if there is no sperm in the semen. • Testicles continue to produce sperm, but sperm are reabsorbed by the body
Accessory Glands 1. Seminal Vesicle 2. Prostate Gland provide fluids that lubricate the duct system and nourish the sperm.
SEMINAL VESICLE u sac-like structures attached to the vas deferens to the side of the bladder. u Produce a sugar rich fluid that contains several chemicals, which is called FRUCTOSE. u Fructose is produced so that the sperm will live. u Provides them with a source of energy to help them move. u The fluid of the seminal vesicles: u makes up most of the volume of a man's ejaculatory fluid, or ejaculate. u flows into the vas deferens and mixes with the sperm.
PROSTATE GLAND § The prostate gland is a walnut-sized structure, surrounding the ejaculatory ducts at the base of the urethra, just below the urinary bladder in front of the rectum. § Contributes a highly alkaline, thin, milky fluid to the ejaculate, that contains proteins, calcium, citric acid, cholesterol, and various enzymes which help to nourish the sperm. § The alkalinity of the secretion allows sperm to move quickly through the highly acidic environment of the female vagina. The urethra, which carries the ejaculate to be expelled during orgasm, runs through the center of the prostate gland. • Contains muscle fibers in which contract to help eject the semen from the penis.
Bulbourethral Glands Also called COWPERS GLAND pea-sized structures located on the sides of the urethra just below the prostate gland. Function: produce a clear, slippery fluid that empties directly into the urethra. This fluid serves to lubricate the urethra and to neutralize any acidity that may be present due to residual drops of urine in the urethra.
Semen is made up of…. 1. Sperm 2. Fructose from the seminal vesicle. 3. Nourishing fluids from prostate gland 4. Lubricating fluid from Bulbourethral/Cowpers’ gland.
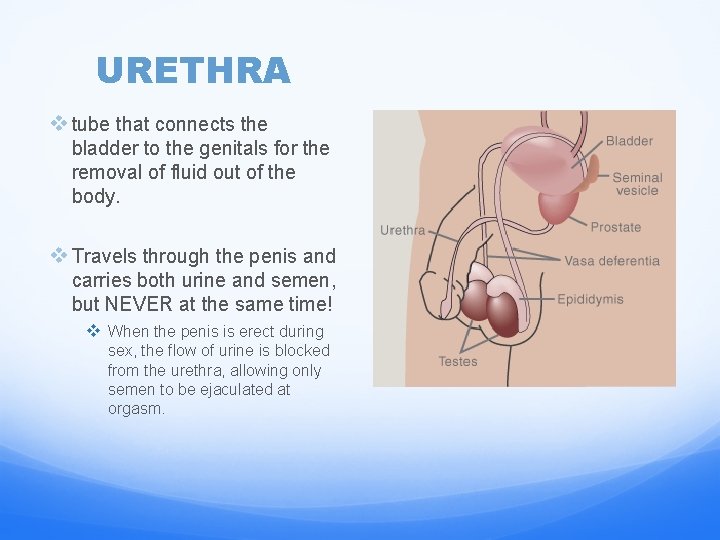
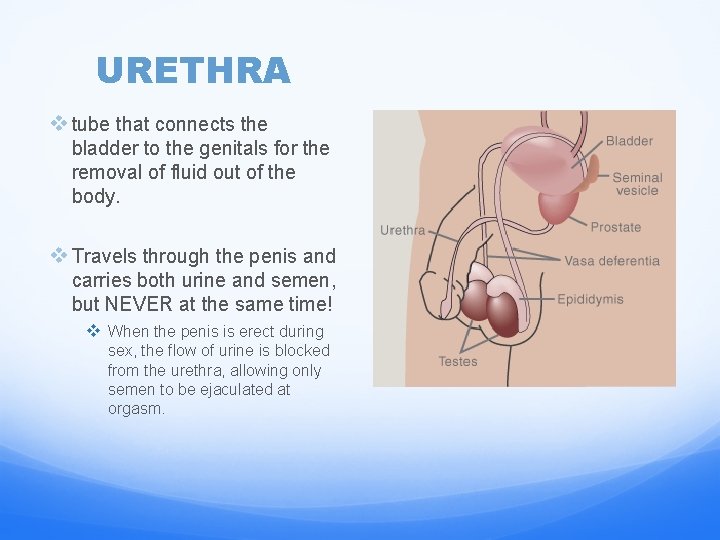
URETHRA v tube that connects the bladder to the genitals for the removal of fluid out of the body. v Travels through the penis and carries both urine and semen, but NEVER at the same time! v When the penis is erect during sex, the flow of urine is blocked from the urethra, allowing only semen to be ejaculated at orgasm.
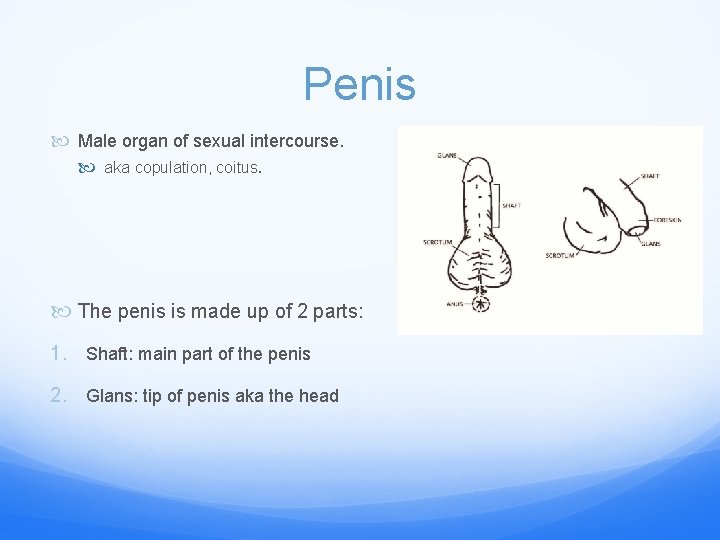
Penis Male organ of sexual intercourse. aka copulation, coitus. The penis is made up of 2 parts: 1. Shaft: main part of the penis 2. Glans: tip of penis aka the head
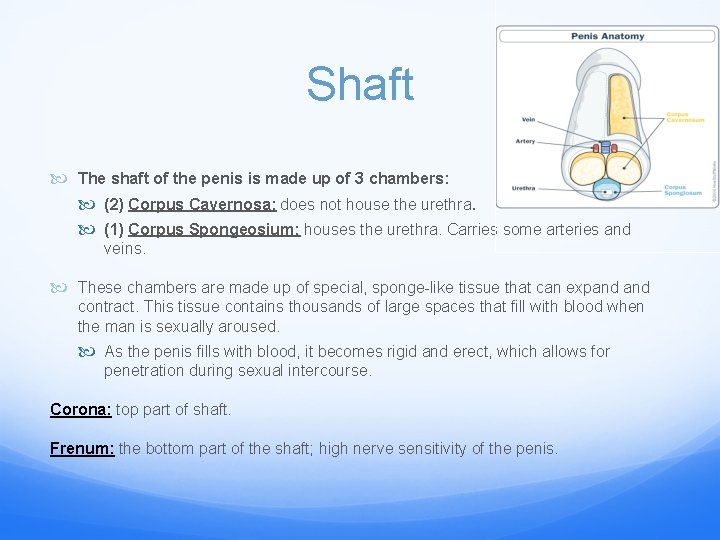
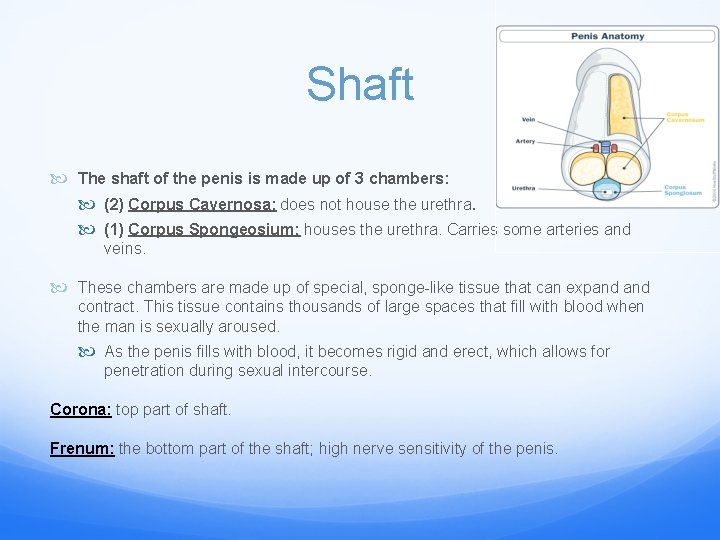
Shaft The shaft of the penis is made up of 3 chambers: (2) Corpus Cavernosa: does not house the urethra. (1) Corpus Spongeosium: houses the urethra. Carries some arteries and veins. These chambers are made up of special, sponge-like tissue that can expand contract. This tissue contains thousands of large spaces that fill with blood when the man is sexually aroused. As the penis fills with blood, it becomes rigid and erect, which allows for penetration during sexual intercourse. Corona: top part of shaft. Frenum: the bottom part of the shaft; high nerve sensitivity of the penis.
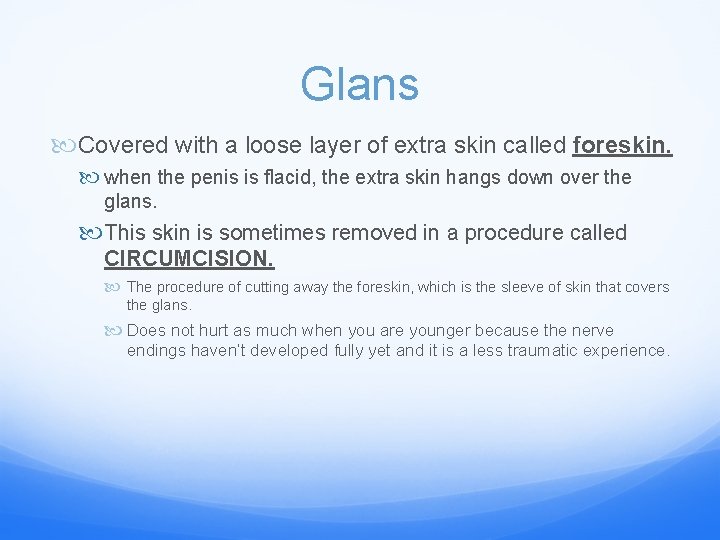
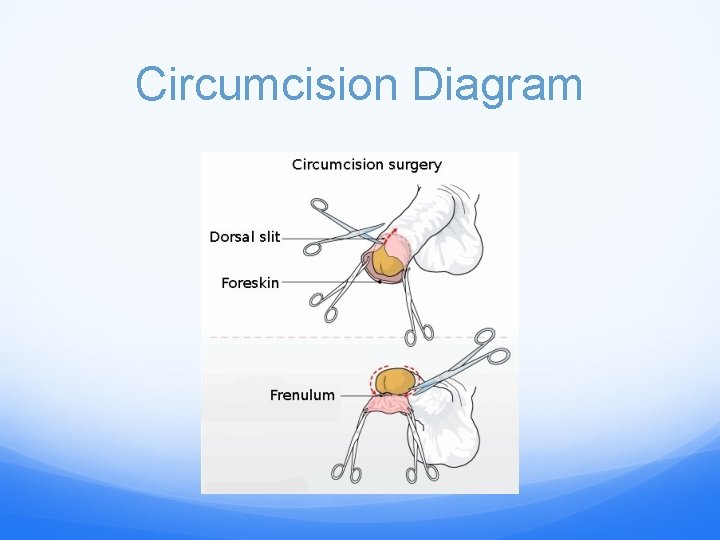
Glans Covered with a loose layer of extra skin called foreskin. when the penis is flacid, the extra skin hangs down over the glans. This skin is sometimes removed in a procedure called CIRCUMCISION. The procedure of cutting away the foreskin, which is the sleeve of skin that covers the glans. Does not hurt as much when you are younger because the nerve endings haven’t developed fully yet and it is a less traumatic experience.
Circumcision is not medically necessary, parents who choose to have their children circumcised often do so based on: 1. Religious beliefs 2. Concerns about hygiene Smegma: an oil that is produced underneath the foreskin. If the foreskin is not circumcised and the smegma isn’t cleaned, a build up of bacteria will occur which can result in adhesions and the adult male will not be able to have an erection. 3. Cultural or social reasons Boys who have circumcised penises and those who don't aren’t any different. Penises work and feel the same, regardless of whether the foreskin has been removed.
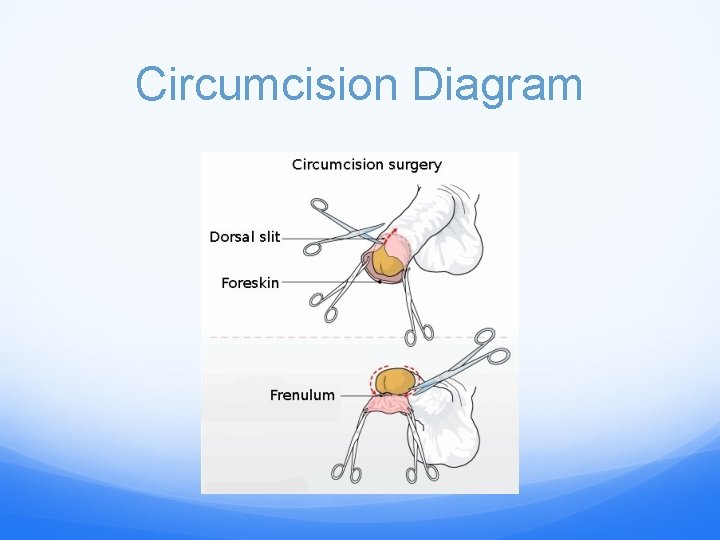
Circumcision Diagram
ERECTION The lengthening, thickening, and hardening of the penis of the male upon sexual arousal. Controlled by nerves in the spinal cord. A man has very limited voluntary control. All erections are not always due to sexual stimulation. “Morning erections” are caused by bladder tension. Periodic erections for no known reasons are common and not indicative of any abnormal functioning. Newborn babies and young boys experience erections, most likely caused by nerve irritability. Every erection does not result in an orgasm.
Erection Cont. Impotence: the inability to attain and/or maintain and erection. Caused by psychological problems. Caused by nerve damage of lower spine; physiological Drugs used for high blood pressure Nocturnal Emission: “Wet Dreams” When a male is sleeping, his penis may become erect and ejaculation may occur. Normal and occur in most males during adolescence.
EJACULATION The expulsion of semen out of a males body through the urethra. 300 million to 600 million sperm cells are ejaculated each time. When the male ejaculates during intercourse, semen is deposited into the female's vagina. From the vagina the sperm make their way up through the cervix and move through the uterus with help from uterine contractions. If a mature egg is in one of the female's fallopian tubes, a single sperm may penetrate it, and fertilization, or conception, occurs.
The Pathway of Sperm through the MRS http: //www. youtube. com/watch? v=HPH 4 b. VKa. U 4 Y
Problems that may occur in the MRS Disorders of the Scrotum, Testicles, or Epididymis 1. Testicular trauma: mild injury to the testicles can cause severe pain, bruising, or swelling. Most testicular injuries occur when the testicles are struck, hit, kicked, or crushed, usually during sports or due to other trauma. 2. Varicocele: This is a varicose vein (an abnormally swollen vein) in the network of veins that run from the testicles. Varicoceles commonly develop while a boy is going through puberty. A varicocele is usually not harmful, although it can damage the testicle or decrease sperm production. 3. Testicular cancer: This is one of the most common cancers in men younger than 40. It occurs when cells in the testicle divide abnormally and form a tumor. Testicular cancer can spread to other parts of the body, but if it's detected early, the cure rate is excellent. Teen boys should be encouraged to learn to perform testicular self examinations.
Continued… 4. Epididymitis: is inflammation of the epididymis, the coiled tubes that connect the testes with the vas deferens. It is usually caused by an infection, such as the sexually transmitted disease chlamydia, and results in pain and swelling next to one of the testicles. 5. Hydrocele: A hydrocele occurs when fluid collects in the membranes surrounding the testes. Hydroceles may cause swelling in the scrotum around the testicle but are generally painless. In some cases, surgery may be needed to correct the condition. 6. Inguinal hernia: When a portion of the intestines pushes through an abnormal opening or weakening of the abdominal wall and into the groin or scrotum, it is known as an inguinal hernia. The hernia may look like a bulge or swelling in the groin area. It can be corrected with surgery.
What is the reproductive system? Put away your packets… Take out a paper and pen/pencil Write down 5 pieces of information that you remember/learned about the Male Reproductive System Write down any questions that you may still have about the Male Reproductive System