What is EvidenceBased Practice EvidenceBased Practice from a
What is Evidence-Based Practice? Evidence-Based Practice from a Nursing Perspective Cynthia Padula, Ph. D, RN Nurse Researcher, The Miriam Hospital Master’s Program Director, Rhode Island College

Objectives w Describe evidence based practice from a nursing perspective w Identify challenges to using evidence based practice in nursing w Compare and contrast evidence based nursing and medicine w Recognize the impact of the Magnet movement on evidence based nursing practice w Identify resources relevant to nursing
Definition “Process by which nurses make clinical decisions using best available evidence, clinical expertise, & patient preferences in the context of available resources” (Di. Censo, 1998)
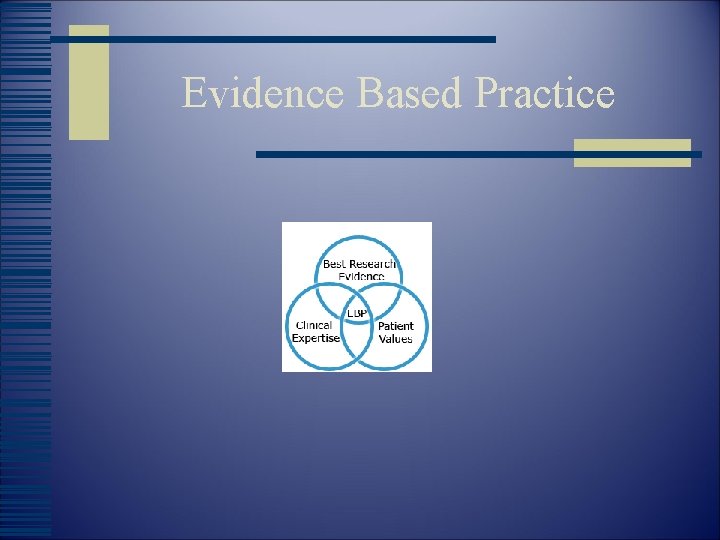
Evidence Based Practice

What is Evidence-Based Nursing Practice w Builds on process of research use, but more encompassing w More specific than term ‘best practices’ w Does not foster rigid adherence to standardized guidelines w Recognizes the role of clinical expertise w EB nursing practice is a state of mind!
Why Evidence-Based Practice in Nursing w Fueled by accrediting bodies, professional organizations, third party payers w Potential to improve quality, reduce variations in care w Focus on practices that result in best possible outcomes at possibly lower cost w Provides a way to keep pace with advances
Why Evidence-Based Practice in Nursing w Potential to narrow the ‘research-practice gap’: adoption of research findings into practice can take as long as 17 years (Balas & Boren) w Impacted by perception that published research is not w relevant to practice w Provides a means to answer problematic clinical w practice issues w Potential to improve individual bedside practice; w supports/improves clinical decision-making skills w Bedside nurse as conduit!!
Traditional Basis for Nursing Practice (Stetler) w Rituals, unverified rules w Anecdotes, isolated experiences w Customs, opinions, unit cultures w Physicians’ authority
Bases for Practice in Nursing (Stetler, 1998) w Philosophical/conceptual basis: mission; values; professional practice models; conceptual frameworks; professional codes w Regulatory basis: state practice act; JCAHO; regulatory agencies w Traditional basis w *Evidence-based practice
Alternative Approach w Clinical expertise as necessary but not sufficient to provide best possible care w Emphasis is on systematic, reproducible, unbiased evidence w Focus on evidence authority *in combination with clinical expertise
Core Competencies w Ask: why are we doing this. . what is the evidence? w Think critically! w Think out of the box!
Core Competencies (cont. ) w Prioritize and clearly articulate answerable clinical questions with a focus on outcomes w Appreciate role of quality improvement activities w Evaluate practice outcomes w *Work effectively with others

Core Competencies (cont. ) w Search for evidence • Evaluate the evidence
Core Competencies (cont. ) w Read and understand research

Levels of Evidence Hierarchy (Stetler et al. )* w w w w Level I: Meta-analysis of multiple RCTs (‘gold standard’) Level II: Individual RCTs Level III: Quasi-experimental Level IV: Non-experimental; qualitative Level V: Program evaluation; QI; RU; case reports Level VI: Opinion of respected authorities *modified slightly by Padula

Levels of Evidence Pyramid

Evidence Based Practice Process w w Identify a practice issue Formulate an answerable question Search for best evidence Critically evaluate the evidence and clinical relevance w Make recommendations w Apply to clinical practice w Evaluate impact/effectiveness/ outcomes

EBP in Nursing
Readiness of US Nurses for EBP (Pravikoff et al. , 2005) w Purpose: to examine nurses’ perceptions of their skills in obtaining evidence and their access to tools with which to do so. w Sample: stratified random sample of 3, 000 RNs across the US; 1, 097 responded w Measurement: 93 item measure; content validity established; varying response format
Sample Characteristics (Pravikoff et al. ) w 91% female w 79% between >40 years of age w Educational preparation: Diploma 17% AD 34% BSN 39% MS 9% w Employment: 60% in hospitals
Subscale: Information Need/Seeking w How often do you need w information to support nursing role? 61%: once or twice a week w How do you find the information w needed? 67% always or freq sought a colleague 58% didn’t use research reports at all 82% had never used a hospital library
Subscale: Resource Availability and Use w 83%: at least somewhat successful when searching the Internet w 19% somewhat confident in ability to search CINAHL; 76% never search CINAHL w 36% somewhat confident in ability to search MEDLINE w 83% rarely or never sought librarian assistance; 82% didn’t use hospital library
Resource Use/Availability (cont. ) w 77% had never received instruction re: electronic resources w 36% reported had access to electronic databases; 29% did not know if access was available w 26% had access to electronic databases on nursing units w 49% had access to the Internet on units
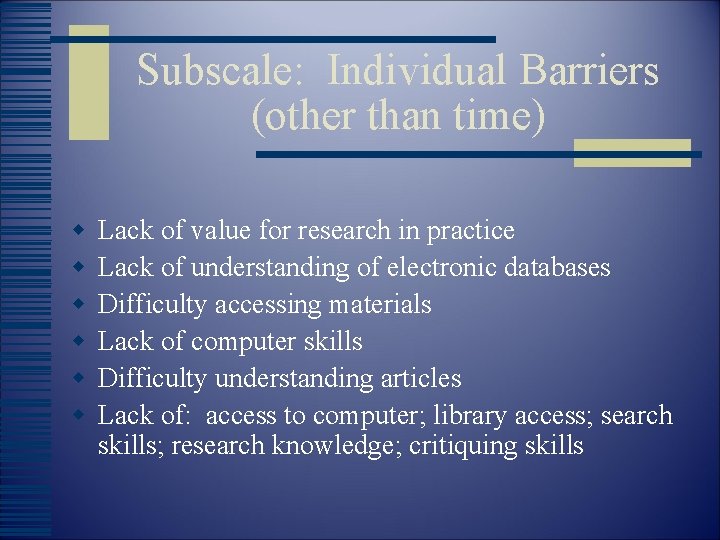
Subscale: Individual Barriers (other than time) w w w Lack of value for research in practice Lack of understanding of electronic databases Difficulty accessing materials Lack of computer skills Difficulty understanding articles Lack of: access to computer; library access; search skills; research knowledge; critiquing skills
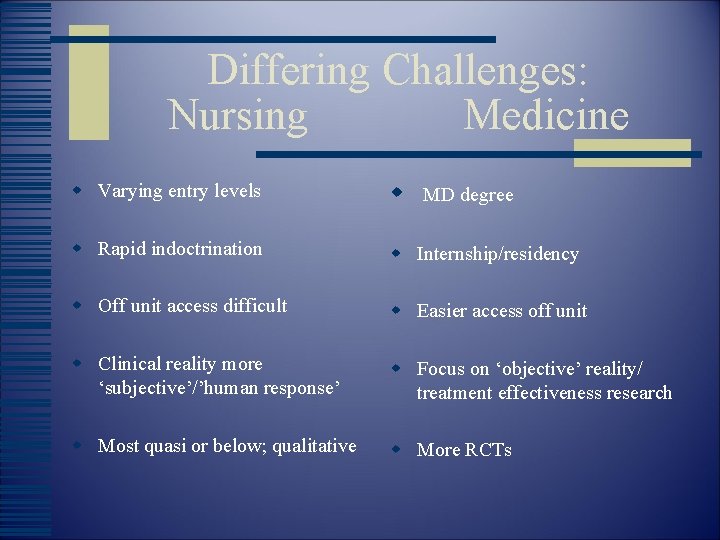
Differing Challenges: Nursing Medicine w Varying entry levels w MD degree w Rapid indoctrination w Internship/residency w Off unit access difficult w Easier access off unit w Clinical reality more ‘subjective’/’human response’ w Focus on ‘objective’ reality/ treatment effectiveness research w Most quasi or below; qualitative w More RCTs

Using the Magnet Influence w Administered by the American w Nurses Credentialing Center http: //nursingworld. org. ancc w Magnet designation recognized w and rewards nursing excellence w Forces of Magnetism (14) identified via a landmark study (Mc. Clure & Hindshaw)
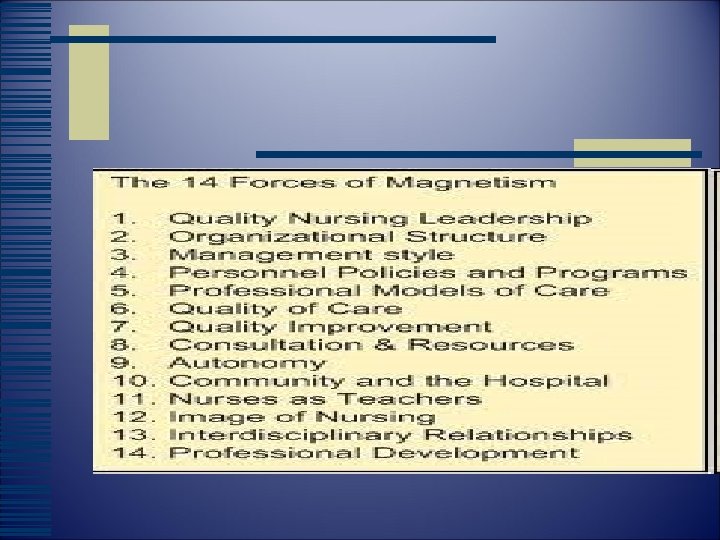
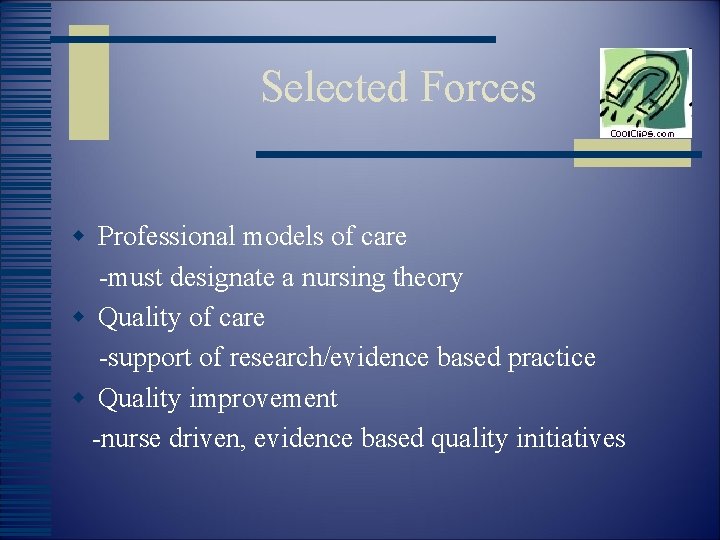
Selected Forces w Professional models of care -must designate a nursing theory w Quality of care -support of research/evidence based practice w Quality improvement -nurse driven, evidence based quality initiatives

Selected Forces (cont. ) w Professional development -training, mentoring w Interdisciplinary relationships -opportunities for collaboration; consultation
Collaboration is Key w Library can serve as archive for nursing publications/Magnet applications (Rourke) w Committee participation w Heightened visibility w Facilitation is key w Write library services and w librarians into grants
Take the Magnet Journey!!
Resources w Evidence Based Nursing Journal w Online Journal of Knowledge Synthesis for Nursing, Sigma Theta Tau http: //www. nursingsociety. org w US Preventive Services Task Force http: //www. ahrq. gov/clinic/uspsfact. htm
Selected Lifespan Resources w Direct links to Pub. Med and Ovid w Micromedex w > 3000 journals w DXplain w MD consult
References w w w w w Baras, E. , & Boren, S. (2000). Managing clinical knowledge for healthcare improvement (pp. 65 -70). Germany: Schattauer Publishing. Dee, C. , & Stanley, e. (2005). Nurses’ information needs: nurses’ and hospital librarians’ perspective. J Hosp Librar, 5(2), 1 -13. Hallyburton, A. , & St. John, B. (2009). Partnering with your library to strengthen nursing research. J Nsg Educ, 49(3), 164 -167. Mc. Clure, M. , & Hinshaw, A. (2002). Magnet hospital revisited. Washington DC: ANA. w Pravikoff, D. , Tanner, A. , & Pierce, S. (2005). Readiness of US nurses w for evidence-based practice. AJN, 105(9), 40 -51.
References (cont. ) w Rourke, D. (2007). The hospital library as a “Magnet Force”…Med Ref w Svcs Quar, 26(3), 47 -54. Sherwill-Navarro, P. , & Roth, K. (2007). Magnet hospital/magnetic w libraries. J Hosp Librar, 7(3), 21 -31 w Stetler C. et al. (1998). Evidence-based practice and the role of nursing w leadership. JONA, 28(7/8), 45 -53. w Stetler, C. et al. (1998). Utilization-focused integrative reviews. Appl w Nurs Res, 11(4).
- Slides: 35