What is EBP The Iowa Model Debra Mark
What is EBP & The Iowa Model Debra Mark, Ph. D, RN Assistant Professor, debramar@hawaii. edu
Objectives �Discuss the rationale for EBP �Differentiate EBP from research �Describe the Iowa Model �Discuss the importance of translation science to EBP
History of EBP � 1972: Publication by the Nuffield Provincial Hospitals Trust of his book, Effectiveness and Efficiency Random Reflections on Health Services. “Because resources would always be limited, they should be used to provide equitably those forms of health care which had been shown in properly designed evaluations to be effective. ” � 1980 s: Oxford Database of Perinatal Trials. � Cochrane Library Archie L. Cochrane, 1909 - 1988
So, where are we after 40 years?

National & International Centers � Australia � Cochrane Library (www. thecochranelibrary. com) � Joanna Briggs Institute � England � Keele University � United States � Agency for Healthcare Research & Quality (www. ahrq. gov) � Arizona State University � Department of Health & Human Services � Indiana (Joanna Briggs Collaborative) � Michigan – National Nurse Practice Network � Quality & Safety Education for Nurses (www. qsen. org) - EBP competencies � University of Texas
Rationale for EBP Why Do We Need it? Quality Healthcar e Cost Access
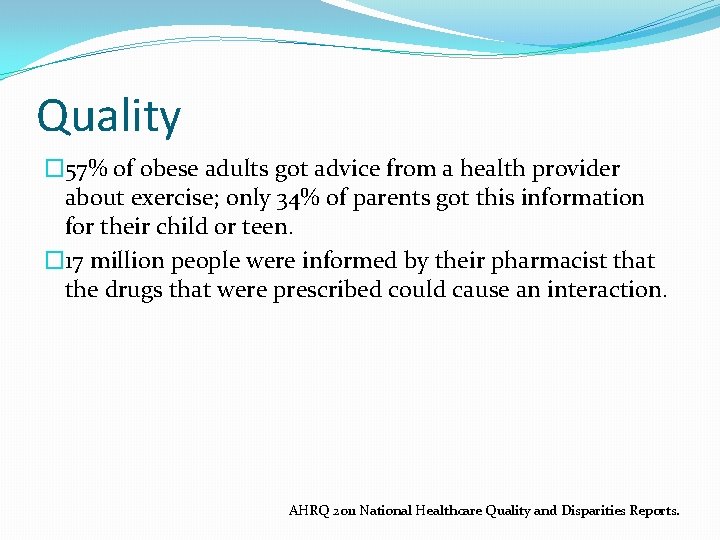
Quality � 57% of obese adults got advice from a health provider about exercise; only 34% of parents got this information for their child or teen. � 17 million people were informed by their pharmacist that the drugs that were prescribed could cause an interaction. AHRQ 2011 National Healthcare Quality and Disparities Reports.
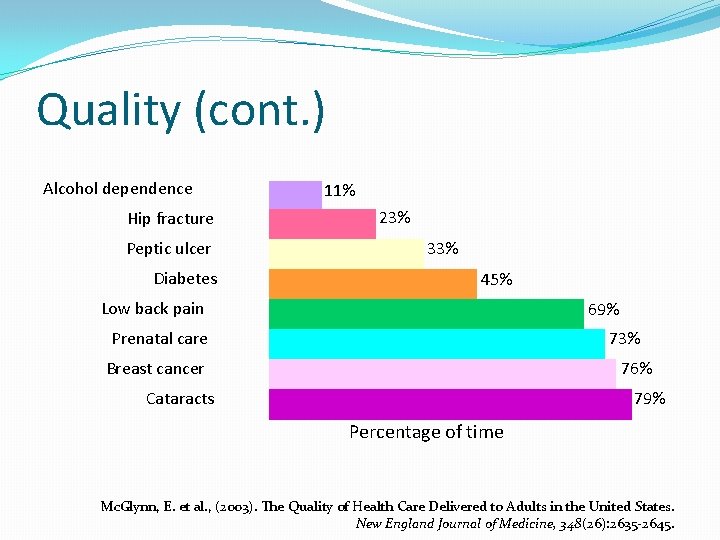
Quality (cont. ) Alcohol dependence Hip fracture Peptic ulcer Diabetes 11% 23% 33% 45% Low back pain 69% Prenatal care 73% Breast cancer 76% Cataracts 79% Percentage of time Mc. Glynn, E. et al. , (2003). The Quality of Health Care Delivered to Adults in the United States. New England Journal of Medicine, 348(26): 2635 -2645.
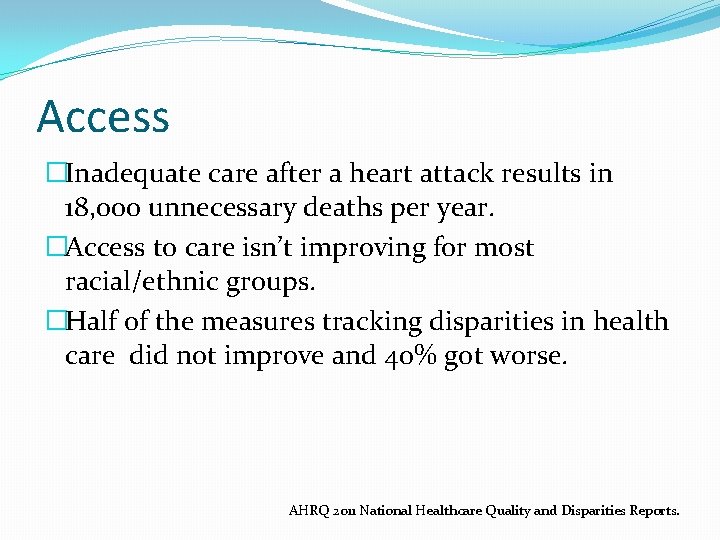
Access �Inadequate care after a heart attack results in 18, 000 unnecessary deaths per year. �Access to care isn’t improving for most racial/ethnic groups. �Half of the measures tracking disparities in health care did not improve and 40% got worse. AHRQ 2011 National Healthcare Quality and Disparities Reports.
Cost �Healthcare in the U. S. = 15. 2% of GDP (2008) � 25% (2025) �$100 billion on health-related research (Dorsey et al. , 2010)
And yet… �It takes 17 years to get 14% of scientific findings into practice (Balas & Boren, 2000). �An evidence-based policy or procedure does not a practice change make.
Bottom Line: �EBP is no longer a luxury �But a necessity �Possible litigation �Use evidence in day-to-day decision-making �Administrators �Clinicians �Educators �Researchers

Advantages �Improves patient outcomes �Documents quality improvement efforts �Identifies performance issues/practice inconsistencies/variances �Empowers staff �Builds skills �Increases satisfaction for patients, staff, families �Increases efficiency �Decreases costs Demands �EBP-receptive culture �Strong leadership support �Decentralized administration �Shared governance �Vision/Mission committed to quality � Integration into practice standards & CIS �Resources � Skill development � Money/time � Researchers & Librarians
EBP vs QI vs Research How are they different?
Quality Improvement Is: �An activity to evaluate existing local practices with a goal of documenting and correcting deficiencies.
QI Models �PDCA �Most common �Plan Do Check Act (PDCA) �Six Sigma �Variation �Define Measure Analyze Improve Control (DMAIC) �Root Cause Analysis (RCA) �Retrospective analysis �Example: Cardiac Arrest
Research Is: �Systematic investigation to validate existing knowledge and generate new knowledge �Description �Explanation �Prediction �Control
Research Methods �Quantitative �Experimental (Randomized Controlled Trials) �Quasi-Experimental �Non-Experimental (Descriptive) � Example: Nursing Experience & Critical Care Patient Outcomes �Qualitative �Ethnography �Grounded Theory �Phenomenology
EBP Is �Integration of best research evidence with clinical expertise and patient values (Sackett et al, 2000). �Synthesis and use of evidence from scientific investigations (e. g. observational studies) and other types of knowledge (e. g. case reports; expert opinion) (Cook, 1998).
EBP Is Not �Conduct of research �“Best practice” �What others are doing to decrease length of stay (LOS) �Quality improvement – only �Synthesis of research – only
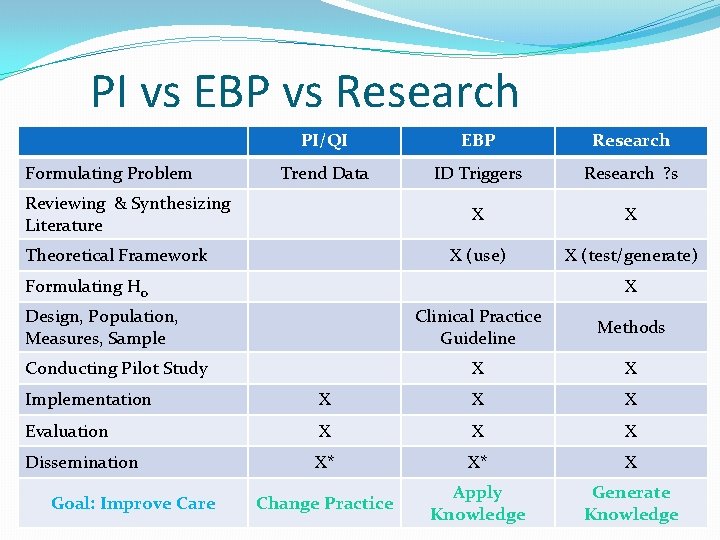
PI vs EBP vs Research Formulating Problem PI/QI EBP Research Trend Data ID Triggers Research ? s X X X (use) X (test/generate) Reviewing & Synthesizing Literature Theoretical Framework Formulating Ho X Design, Population, Measures, Sample Conducting Pilot Study Clinical Practice Guideline Methods X X Implementation X X X Evaluation X X X Dissemination X* X* X Change Practice Apply Knowledge Generate Knowledge Goal: Improve Care
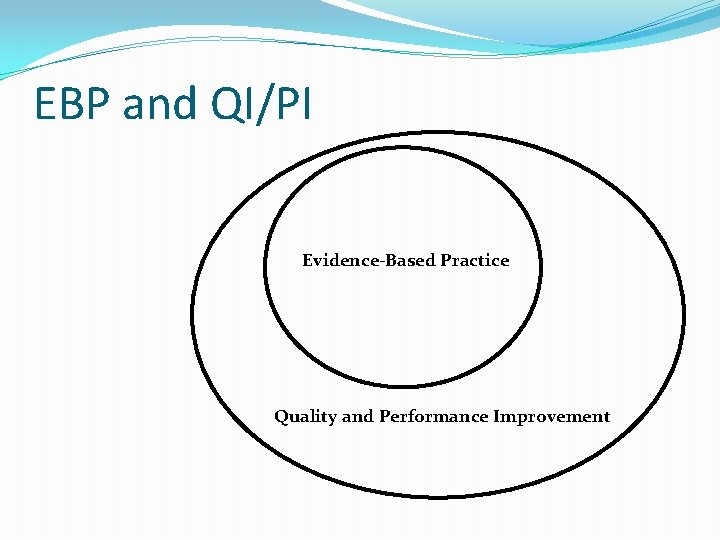
EBP and QI/PI Evidence-Based Practice Quality and Performance Improvement
Differentiate EBP from Research �Read the three scenarios �Determine which one is: �Process Improvement/Quality Improvement �Evidence-based Practice �Research
QI, EBP, or Research? Scenario 1 �Fever in patients with head injuries results in increased intracranial pressure and secondary brain injury. However, it was noted that management of fever in patients with traumatic brain injury varied widely in one neuroscience intensive care unit. �A multidisciplinary team was formed who found, critiqued, and synthesized the literature. The project resulted in delineated interventions for low, medium, and high fevers that progressed from noninvasive to invasive temperature management practices; care for shivering patients became an additional product. �Evaluation of the project resulted in a three-fold improvement in temperature management practices; monitoring of compliance is ongoing.
QI, EBP, or Research? Scenario 2 �Research findings discussed at a unit journal club indicated that applying heat to the extremity facilitated IV catheter insertion. Nurses participating in the journal club questioned whether moist or dry heat was more effective. No literature was found addressing this question. �The project was designed to test which form of heat was more efficacious before IV cannulation. A proposal was developed, IRB approval was obtained, and funding was obtained to conduct the project in the oncology infusion center. �It was found that dry heat was the best type of heat with respect to time to cannulation, number of cannulation attempts, and patient satisfaction. The results were presented at a local conference and published in the Oncology Nurses Forum.
QI, EBP, or Research? Scenario 3 �Routine lab audits revealed that the ED had a high blood culture contamination rate. The ED nurse manager shared this data with the staff and a clinical nurse volunteered to lead the effort to reduce the contamination rate. �The clinical nurse identified sources of variation in practice, standardized a blood culture draw procedure, developed educational materials for the nurses and techs, and verified competency for all staff on the new procedure. �Repeat audits demonstrated that the contamination rate decreased from 6. 38% to 2. 7%, which was below the national benchmark.
The Iowa Model Why do we need one? How would you describe it?
Models for EBP �Guide our planning, thinking, writing, etc. �Several EBP models � Logical sequence � Organizationally & culturally sensitive � Utilize all or most evidence �Ace Star �Arizona State University �Iowa
Iowa Model �Seven Steps 1. 2. 3. 4. 5. 6. 7. Identify & Prioritize Topics Form a Team Assemble Relevant Research & Related Literature Critique & Synthesize Research for Use in Practice Pilot the Change in Practice Institute the Change in Practice Monitor & Analyze Structure, Process, and Outcome Data
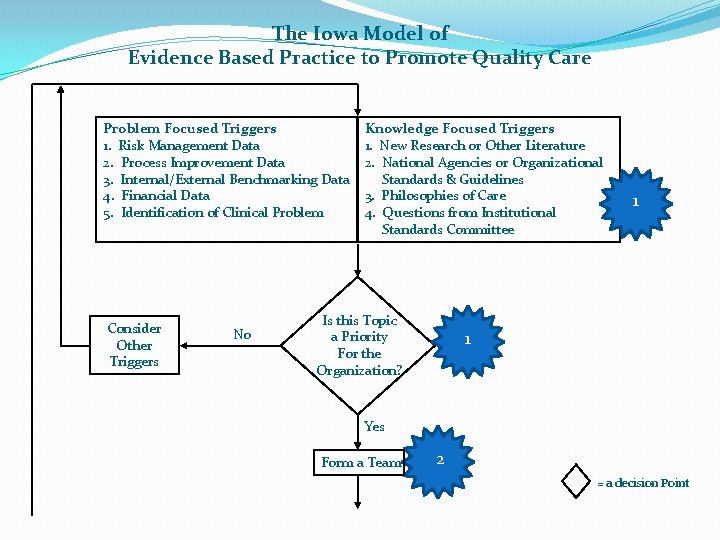
The Iowa Model of Evidence Based Practice to Promote Quality Care Problem Focused Triggers 1. Risk Management Data 2. Process Improvement Data 3. Internal/External Benchmarking Data 4. Financial Data 5. Identification of Clinical Problem Consider Other Triggers No Knowledge Focused Triggers 1. New Research or Other Literature 2. National Agencies or Organizational Standards & Guidelines 3. Philosophies of Care 4. Questions from Institutional Standards Committee Is this Topic a Priority For the Organization? 1 1 Yes Form a Team 2 = a decision Point
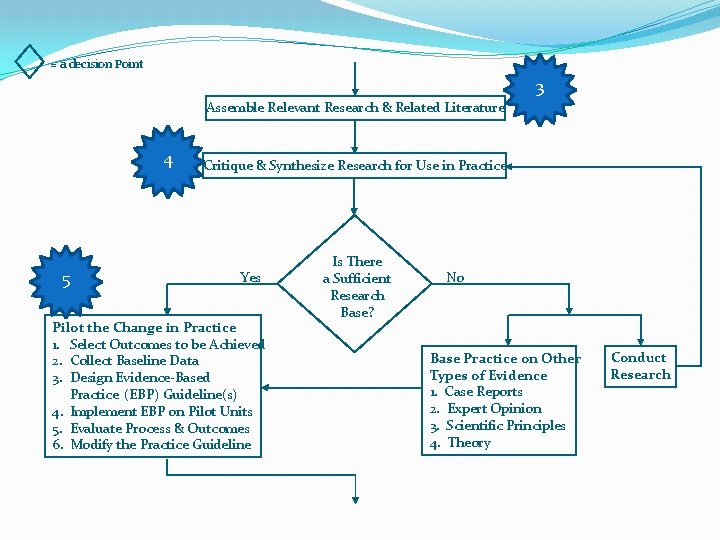
= a decision Point 3 Assemble Relevant Research & Related Literature 4 5 Critique & Synthesize Research for Use in Practice Yes Pilot the Change in Practice 1. Select Outcomes to be Achieved 2. Collect Baseline Data 3. Design Evidence-Based Practice (EBP) Guideline(s) 4. Implement EBP on Pilot Units 5. Evaluate Process & Outcomes 6. Modify the Practice Guideline Is There a Sufficient Research Base? No Base Practice on Other Types of Evidence 1. Case Reports 2. Expert Opinion 3. Scientific Principles 4. Theory Conduct Research
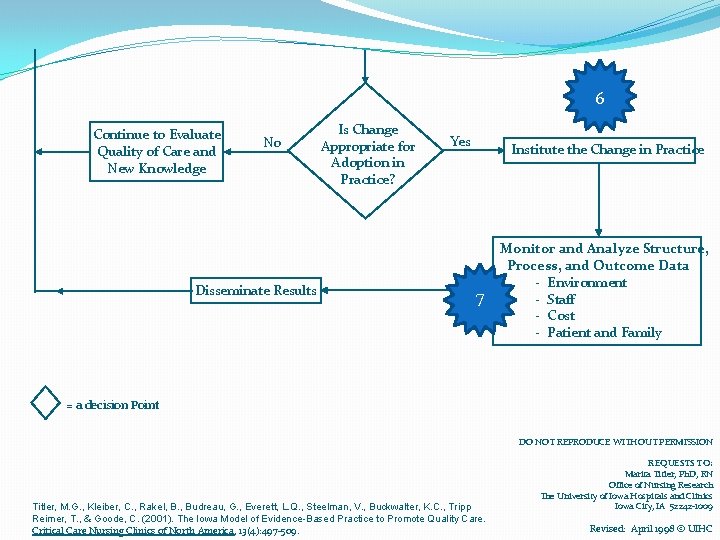
6 Continue to Evaluate Quality of Care and New Knowledge No Disseminate Results Is Change Appropriate for Adoption in Practice? Yes Institute the Change in Practice 7 Monitor and Analyze Structure, Process, and Outcome Data - Environment - Staff - Cost - Patient and Family = a decision Point DO NOT REPRODUCE WITHOUT PERMISSION Titler, M. G. , Kleiber, C. , Rakel, B. , Budreau, G. , Everett, L. Q. , Steelman, V. , Buckwalter, K. C. , Tripp Reimer, T. , & Goode, C. (2001). The Iowa Model of Evidence-Based Practice to Promote Quality Care. Critical Care Nursing Clinics of North America, 13(4): 497 -509. REQUESTS TO: Marita Titler, Ph. D, RN Office of Nursing Research The University of Iowa Hospitals and Clinics Iowa City, IA 52242 -1009 Revised: April 1998 © UIHC
Translation Science Why is it so important?
“Invention is hard, but implementation is much more difficult. ” Berwick, 2003
Change, Change… Faced with the choice between Changing one’s mind & Proving that there is no need to do so, Michael-Chain-of-Fools Almost everybody gets busy on the proof J. K. Galbraith American Economist
Diffusion of Innovations �Study of how best to move evidence to the bedside �(& change behavior!) Everett Rogers 1931 – 2004
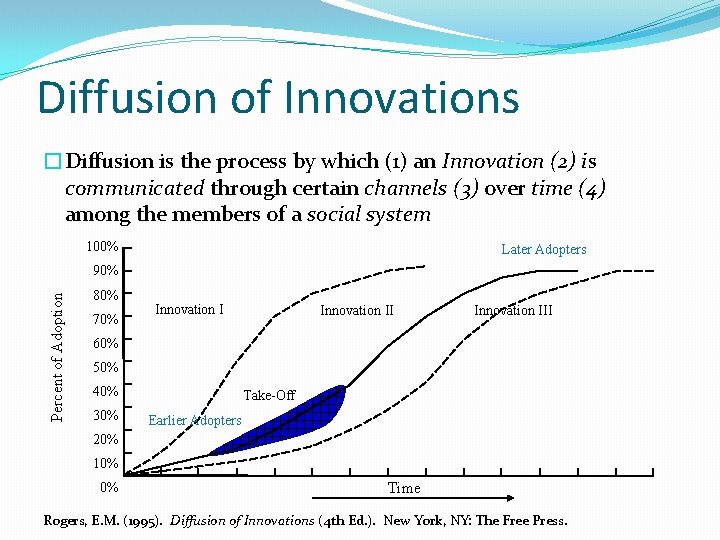
Diffusion of Innovations �Diffusion is the process by which (1) an Innovation (2) is communicated through certain channels (3) over time (4) among the members of a social system 100% Later Adopters Percent of Adoption 90% 80% 70% Innovation III 60% 50% 40% 30% Take-Off Earlier Adopters 20% 10% 0% Time Rogers, E. M. (1995). Diffusion of Innovations (4 th Ed. ). New York, NY: The Free Press.
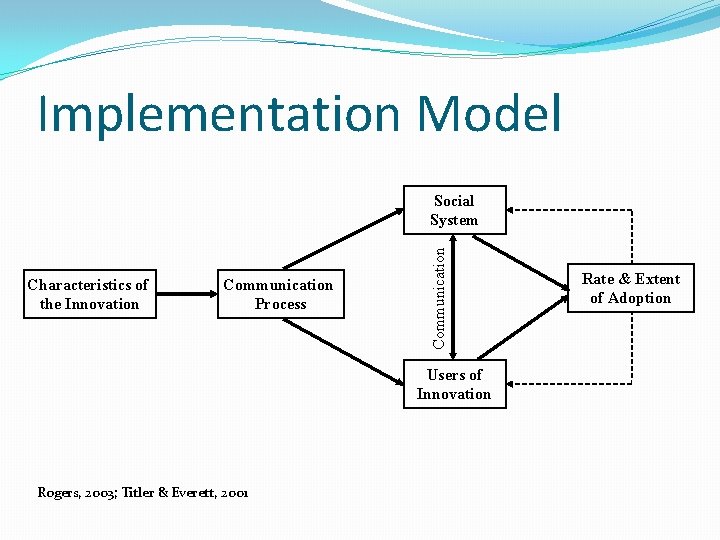
Implementation Model Characteristics of the Innovation Communication Process Communication Social System Users of Innovation Rogers, 2003; Titler & Everett, 2001 Rate & Extent of Adoption
And Neither is EBP!
“No matter what measures are taken, healthcare workers will sometimes falter, and it isn’t reasonable to ask that we achieve perfection. What is reasonable is to ask that we never cease to aim for it. ” Gawande, 2002
Conclusion �Discuss the rationale for EBP �Differentiate EBP from research �Describe the Iowa Model �Discuss the importance of translation science to EBP
- Slides: 41