What is EBP and an Overview of the
What is EBP and an Overview of the Iowa Model Marita G. Titler, Ph. D, RN, FAAN Professor and Dumas Endowed Chair University of Michigan School of Nursing and UMHS Ann Arbor, Michigan
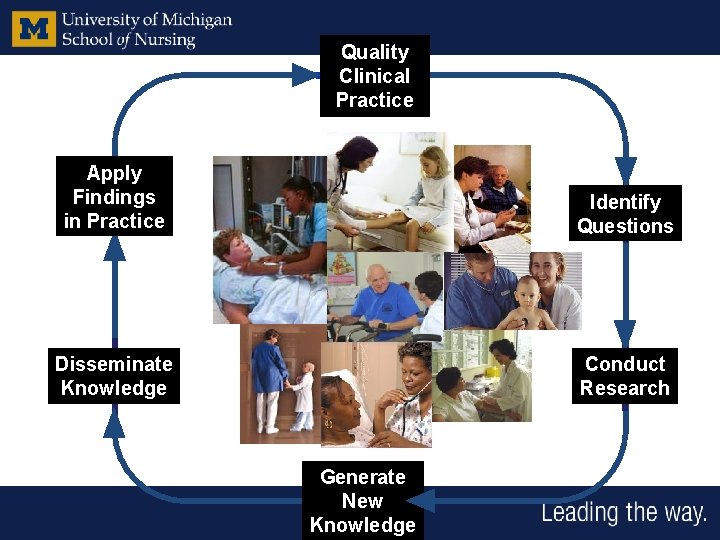
Quality Clinical Practice Apply Findings in Practice Identify Questions Disseminate Knowledge Conduct Research Generate New Knowledge
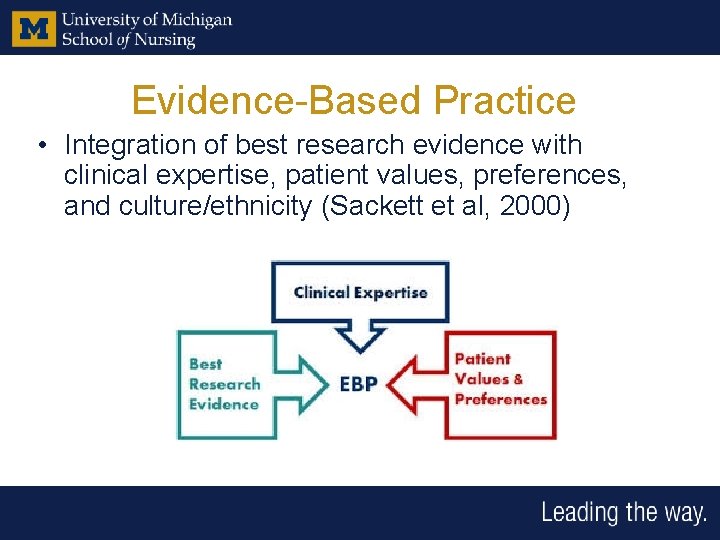
Evidence-Based Practice • Integration of best research evidence with clinical expertise, patient values, preferences, and culture/ethnicity (Sackett et al, 2000)
What it (EBP) is not • Conduct of research – generation of knowledge • “Best practice” – what are other centers doing to decease LOS • Quality Assessment • Synthesis of research – only
Conduct of Nursing Research Conduct of Research and Evidence-Based Practice are Different
Conduct of Research • Systematic study of a phenomenon such as testing an intervention to improve selfcare of individuals with heart failure.
Quality Improvement • Processes used to improve care delivery • Consider structure, processes, and outcomes of care. • System approach • PDSA/rapid cycle change
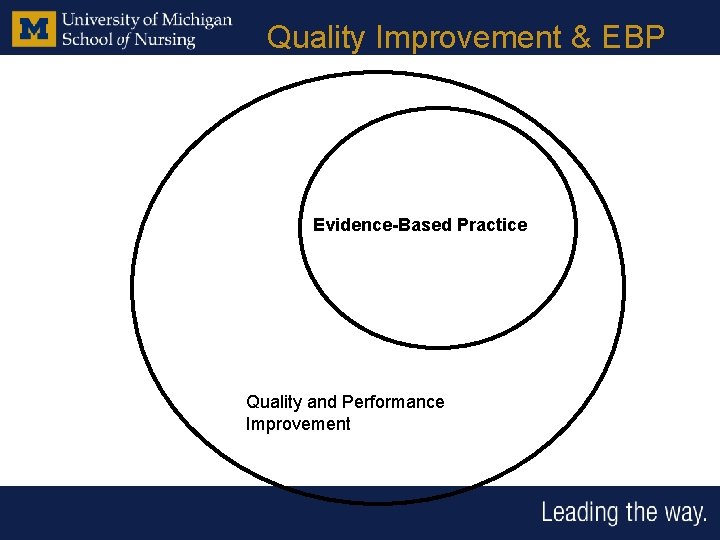
Quality Improvement & EBP Evidence-Based Practice Quality and Performance Improvement
Why EBP • Failures to use evidence from research to make informed decisions in healthcare abound. • Findings from science do not automatically transfer into practice.
Why Listen to Bowel Sounds? Diane Madsen, RN (see December 2005 AJN)
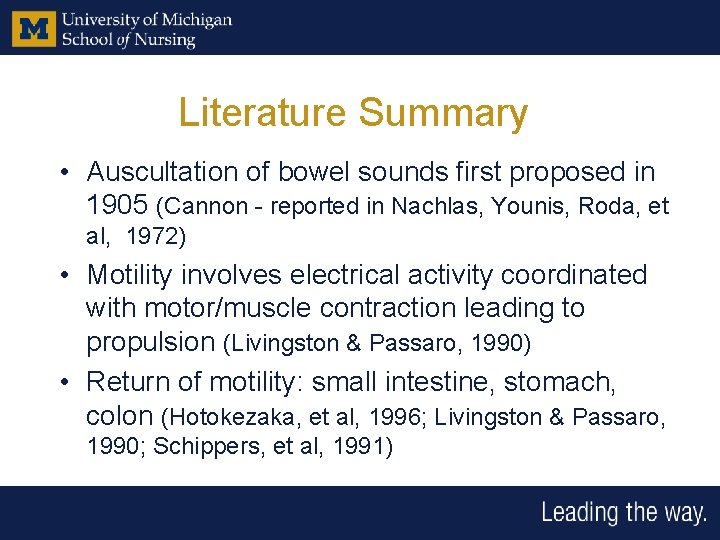
Literature Summary • Auscultation of bowel sounds first proposed in 1905 (Cannon - reported in Nachlas, Younis, Roda, et al, 1972) • Motility involves electrical activity coordinated with motor/muscle contraction leading to propulsion (Livingston & Passaro, 1990) • Return of motility: small intestine, stomach, colon (Hotokezaka, et al, 1996; Livingston & Passaro, 1990; Schippers, et al, 1991)
Literature Summary • Return of bowel sounds likely represents early uncoordinated motor activity in small intestine and not coordinated propulsion in colon (Boghaert, et al, 1987; Nachlas, et al 1972 ; Rothnie, et al, 1963; Benson, et al, 1994; Morris, et al, 1983) • Ability to tolerate feeding is limited by stomach and colonic motility (Cali, et al, 2000; Hotokezaka, et al, 1996; Nachlas, et al, 1972) • Monitoring bowel sounds does not serve to indicate recovery of motility s/p abdominal surgery patients (Huge, et al, 2000)
Why Listen to Bowel Sounds? TRADITION
EBP Standard • Primary markers of return of GI motility (Bauer et al, 1985): – First flatus – First BM • Additional markers of return of GI motility: – Return of appetite – Benign abdomen or absence of other symptoms • Monitoring for complications
Improvement in Care Based On Evidence • Clinical Exemplars: – Falls – Mobility – Pressure ulcer prevention – B/P monitoring • Operational Exemplars: – Nursing Retention – Ergonomics/staff injuries – Staffing
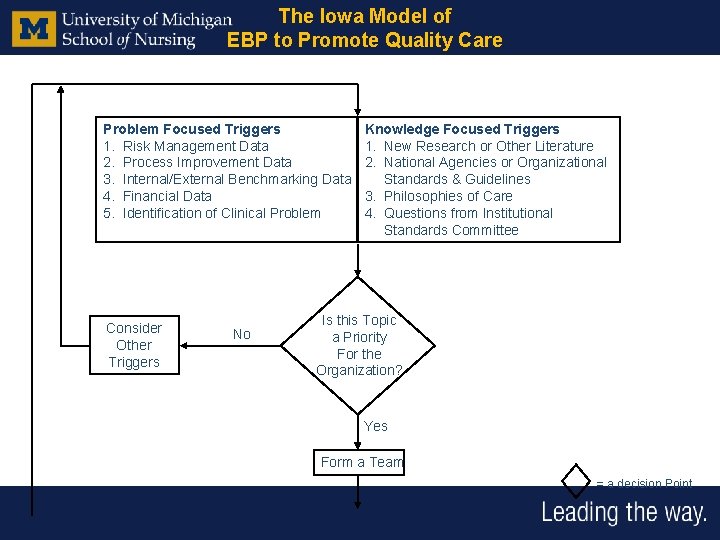
The Iowa Model of EBP to Promote Quality Care Problem Focused Triggers 1. Risk Management Data 2. Process Improvement Data 3. Internal/External Benchmarking Data 4. Financial Data 5. Identification of Clinical Problem Consider Other Triggers No Knowledge Focused Triggers 1. New Research or Other Literature 2. National Agencies or Organizational Standards & Guidelines 3. Philosophies of Care 4. Questions from Institutional Standards Committee Is this Topic a Priority For the Organization? Yes Form a Team = a decision Point
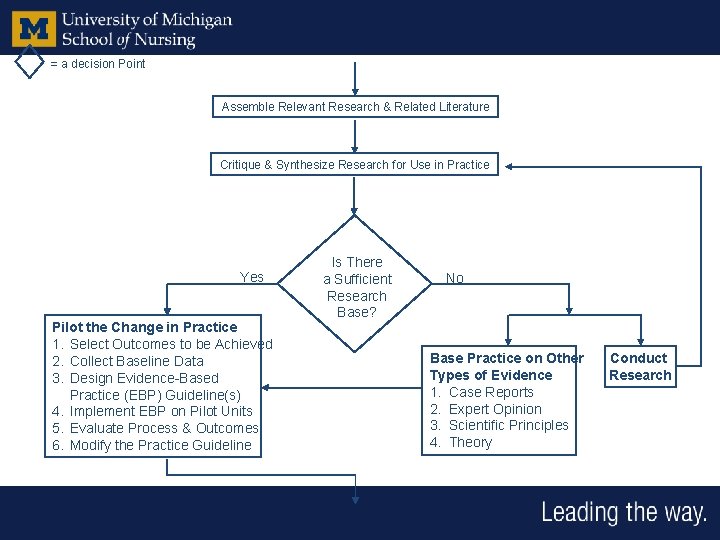
= a decision Point Assemble Relevant Research & Related Literature Critique & Synthesize Research for Use in Practice Yes Pilot the Change in Practice 1. Select Outcomes to be Achieved 2. Collect Baseline Data 3. Design Evidence-Based Practice (EBP) Guideline(s) 4. Implement EBP on Pilot Units 5. Evaluate Process & Outcomes 6. Modify the Practice Guideline Is There a Sufficient Research Base? No Base Practice on Other Types of Evidence 1. Case Reports 2. Expert Opinion 3. Scientific Principles 4. Theory Conduct Research
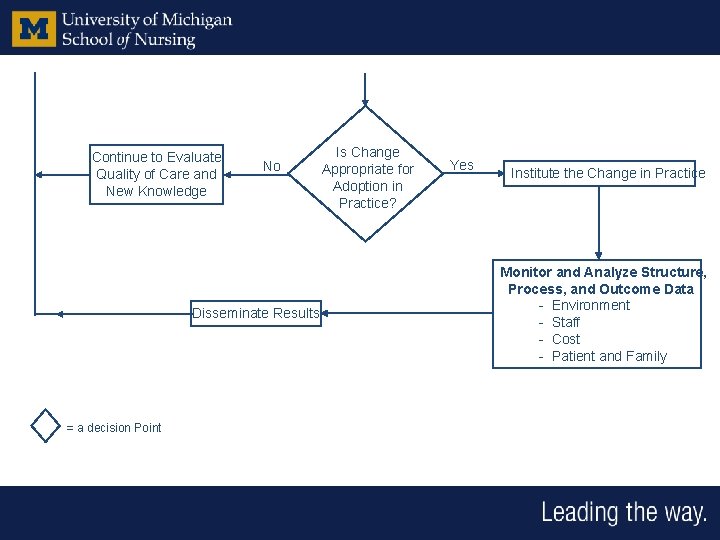
Continue to Evaluate Quality of Care and New Knowledge No Disseminate Results = a decision Point Is Change Appropriate for Adoption in Practice? Yes Institute the Change in Practice Monitor and Analyze Structure, Process, and Outcome Data - Environment - Staff - Cost - Patient and Family
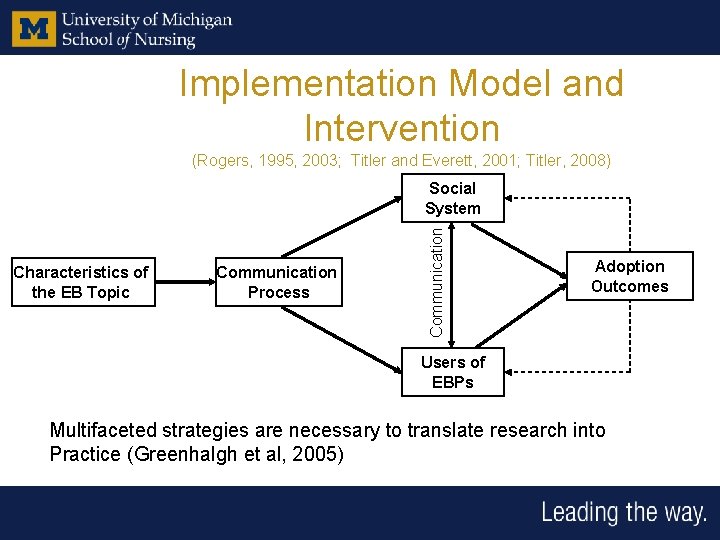
Implementation Model and Intervention (Rogers, 1995, 2003; Titler and Everett, 2001; Titler, 2008) Characteristics of the EB Topic Communication Process Communication Social System Adoption Outcomes Users of EBPs Multifaceted strategies are necessary to translate research into Practice (Greenhalgh et al, 2005)
Change Faced with the choice between changing one’s mind and proving that there is no need to do so, almost everybody gets busy on the proof. J. K. Galbraith American Economist
“You don’t have to see the whole staircase, just take the first step. ” --Martin Luther King, Jr.
Discussion Points • The manager of an inpatient medical unit is addressing wait times for admission from the ED. She is examining discharge times and ED wait times. • The staff in an ambulatory clinic is looking at scheduling system to shorten clinic wait times. • The staff on a surgical unit is wanting to decrease fall rates on the unit. • The nurse is interviewing patients following discharge to understand what information they perceive being given about reducing falls at home.
- Slides: 25