What do these pictures have in common Status














- Slides: 43

What do these pictures have in common?


Status Asthmaticus in Children by Tonya J. Billips Pediatric Nursing Rounds Old Dominion University Spring, 2011
Objectives Ø Discuss Client History and Assessment Ø Identify and correlate Nursing Problems and plan of care as related to patient Ø Discuss Status Asthmaticus Ø Identify common medications/peak flow meter Ø Discuss research relevant to the identified patient
Client History & Assessment 8 year old African American male • Hx: Asthma, Attention deficit hyperactivity disorder (ADHD), Attention deficit disorder (ADD), Gastroesophageal Reflux Disease (GERD) • Noncompliant medication therapy • Allergies: treenuts, seafood, grass, cats, dogs
Client History & Assessment: Family and Psychosocial History § § Stress r/t frequent asthma attacks, ADD/ADHD Transportation/socioeconomic issues One parent unemployed Noncompliant with treatments or medical recommendations § Support for other siblings
Client History & Assessment: Cultural Considerations Patient and family stem from a Christian background. Because of the family’s religious views, they are unreceptive to the doctor’s prognosis in regard to recovery. Other broad scope cultural considerations identified includes: low-income, minority (AA), lack of resources, and lack of education related to disease process
Client History & Assessment: Chief Reason for Admission § Patient presented with increased wheezing and SOB § Parents administered albuterol per asthma action plan § Symptoms worsened - changes seen in mental status and severe difficulty in breathing taken to CHKD § Upon arrival patient suffered respiratory failure, altered mental status sedated w/ ketamine, intubated § Developed decreased HR cardiac arrest. CPR performed w/ chest compressions and administered epinephrine § Anoxia led to neurological impairment/brain damage

Client History & Assessment: Primary Medical Diagnosis § Status Asthmaticus § Respiratory Failure § Cardiac Arrest
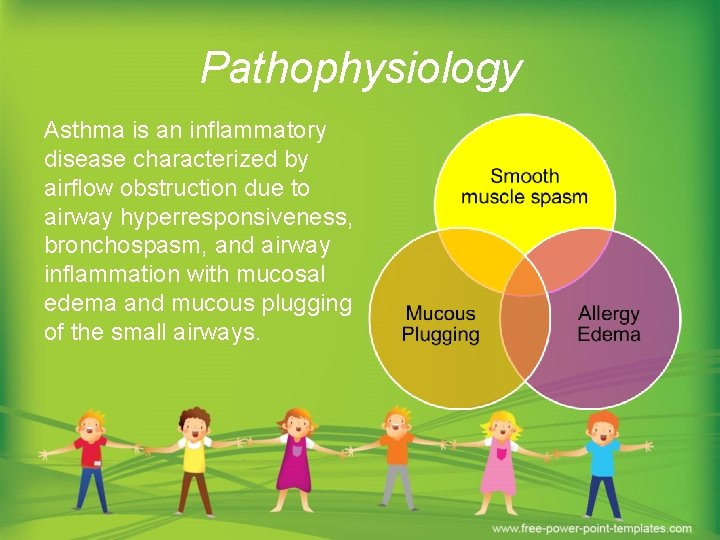
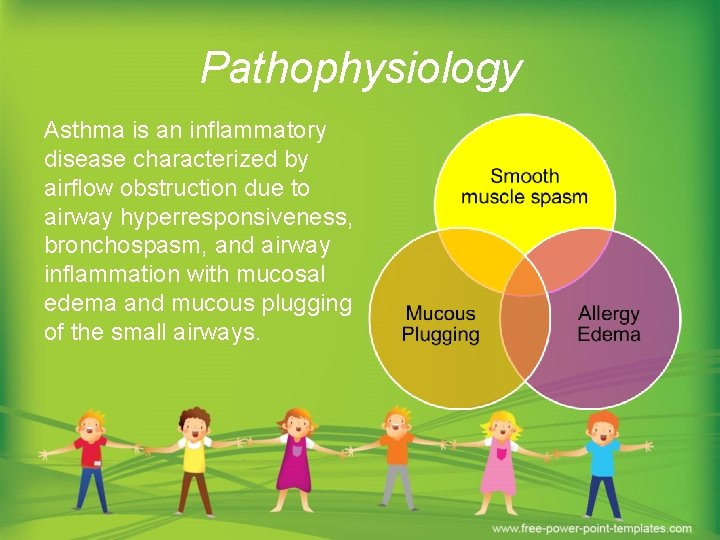
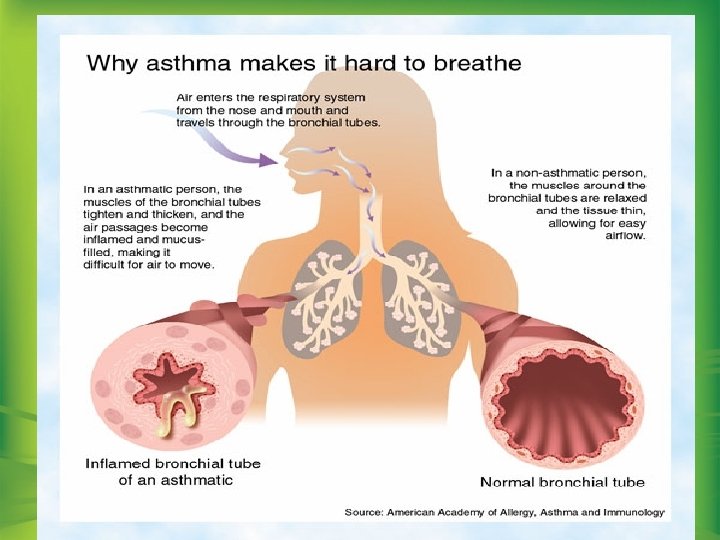
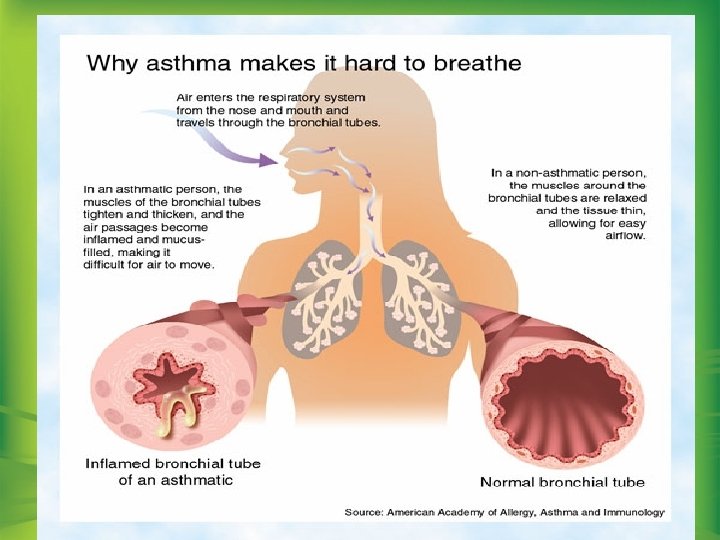
Pathophysiology Asthma is an inflammatory disease characterized by airflow obstruction due to airway hyperresponsiveness, bronchospasm, and airway inflammation with mucosal edema and mucous plugging of the small airways.

Treatment Plan § § § Cardiorespiratory monitoring Monitor for decreasing neurological status Provide adequate nutrition via GT Provide humidified O 2, PEEP, FIO 2, VT for V/Q mismatching Administer IV fluids (NS 0. 9%) to rehydrate to achieve euvolemia β-agonists to mediate bronchodilatation for smooth-muscle relaxation (epinephrine, albuterol) Ketamine to potentiate catecholamines Anticholinergics – Ipratropium to prevent wheezing, difficulty breathing Steroids – IV methylprednisolone Lidocaine Antibiotics – Ancef to protect against respiratory tract infections Provide family support and teaching
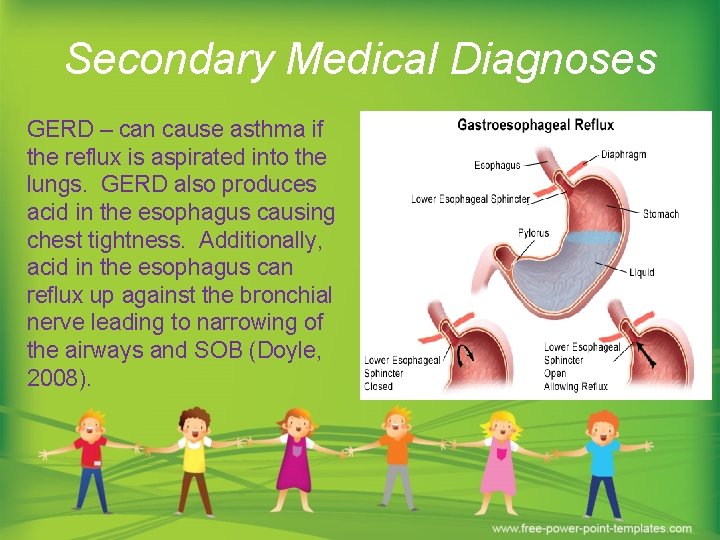
Secondary Medical Diagnoses GERD – can cause asthma if the reflux is aspirated into the lungs. GERD also produces acid in the esophagus causing chest tightness. Additionally, acid in the esophagus can reflux up against the bronchial nerve leading to narrowing of the airways and SOB (Doyle, 2008).
Secondary Medical Diagnoses ADD/ADHD – behavioral disorder can lead to hyperactivity causing h wheezing and WOB Allergies – produces asthmatic triggers related to seasonal changes (pollen, grass, animals, etc. )
Expected Developmental Stage: Psychosocial According to Erickson the patient is in the Industry vs. Inferiority stage: “UNMET” d/t neurological impairment § The child wants to work and produce, accomplishing and achieving tasks § The child may display negative attributes of inadequacy and inferiority if too much is expected of him or if he feels unable to measure up to set standards Note: child “MET” the developmental stage prior to asthma attack
Application of Psychosocial Development The patient was neurologically impaired and was unable to achieve tasks independently. With this in mind I provided assistance with ADLs such as changing his diaper, providing oral care, bathing, and repositioning him. As the patient recovers, he will require positive feedback/encouragement when accomplishing tasks independently. “Children with physical or mental limitations are sometimes at a disadvantage for acquisition of certain skills. When the reward structure is based on evidence of mastery, children who are incapable of developing these skills are at risk for feeling inadequate and inferior” (Hockenberry & Wilson, 2011, p. 647).

Expected Developmental Stage: Cognitive According to Piaget this patient is in the “concrete-operational” period: UNMET d/t neurological impairment § Magical thinking diminishes, and the child has a much better understanding of cause and effect § The child begins to accept rules by may not necessarily understand them § The child is ready for basic reading, writing, and arithmetic § Abstract thinking begins to develop during the middle elementary school years § Parents remain very important and adult reassurance of the child’s competence and basic self-worth is essential Note: child “MET” the developmental stage prior to asthma attack

Application of Cognitive Development The degree of brain damage has not yet been identified. Currently, the patient is unable to develop or understand ideas based on perceptual thinking. As the patient recovers he may or may not regain part of this ability. With this in mind, caregivers should understand the patient may not possess a level of intelligence appropriate for his age or that of a younger child. Introduction of new skills should be approached slowly to alleviate frustration and inadequacy.

Physical Assessment
Physical Assessment Exceptions § Neuro – neurological assessment every hour; responds to pain; assess for progressive dilated pupils § Respiratory – Bivona trach in place; mechanical ventilation with PEEP of 5, VT 330; pulse ox monitoring, and suctioning PRN § GI – GT in place on R abdomen § M/S - decorticate posturing; ROM to prevent contractures
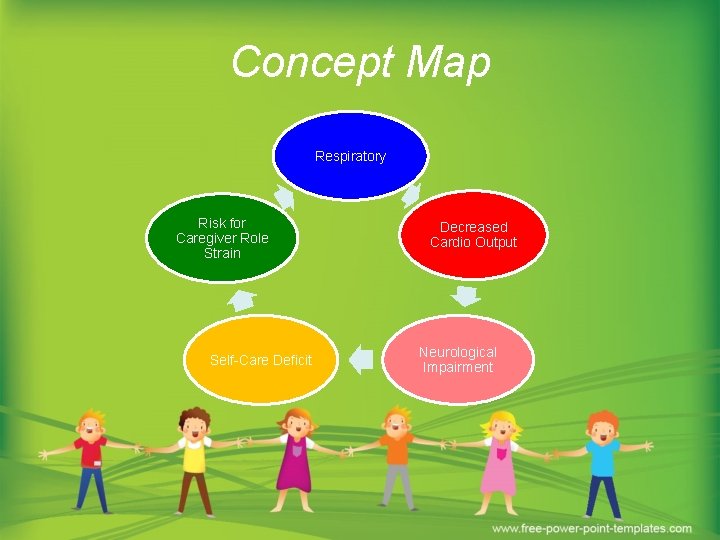
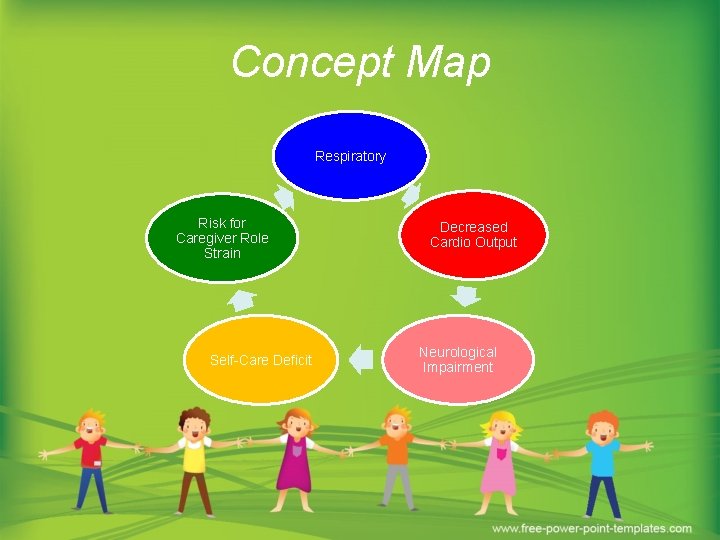
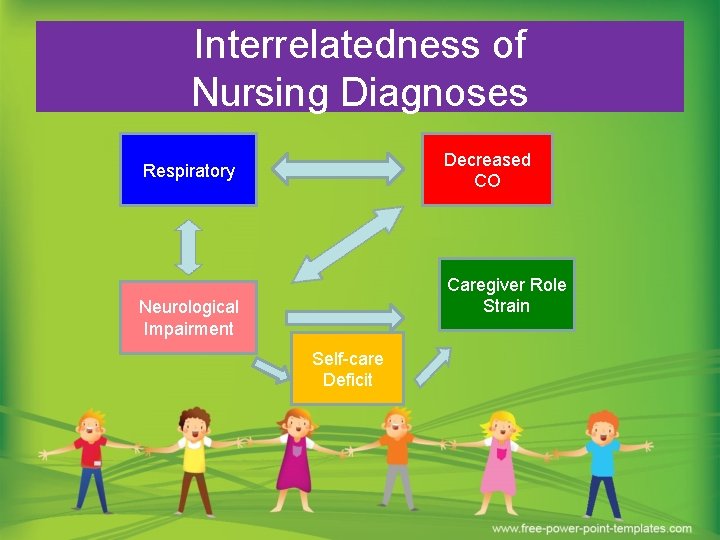
Concept Map Respiratory Risk for Caregiver Role Strain Self-Care Deficit Decreased Cardio Output Neurological Impairment

Respiratory *Priority* § Related to respiratory failure, course breath sounds, long term ventilation therapy (PEEP, VT, FIO 2), brain damage, decreasing O 2 sats, pulse ox monitoring § Trach dependent § Hx of Asthma § Tenacious secretions, course BS § Labs – ABGs (acidosis/alkalosis) Rx: Advair, Singulair, Proair, Ancef, Nasonex, Albuterol, Ipratropium, Methylprednisolone, Humidified O 2 Collaborative and traditional interventions: RT: CPT BID, heated trach collar, suctioning PRN, continuous pulse monitoring

Respiratory: Interventions and Outcomes Nursing Interventions § § § Monitor respiratory status; rate and depth of breaths; chest expansion; adventitious breath sounds; auscultate breath sounds qh. Monitor LOC Maintain O 2 Sat >90% Record I&O qh to monitor fluid balance – report signs of fluid overload or dehydration Monitor effectiveness of PEEP, FIO 2, and VT Desired Outcome Patient will maintain adequate gas exchange as evidenced by clear breath sounds, RR WNL for age (30 -60 bpm), oxygen saturations >90% and absence of retractions, and use of accessory muscles
Decreased Cardiac Output § Related to cardiac arrest, decreased HR and rhythm, administration of CPR, respiratory failure Rx: Epinephrine, Ketamine Collaborative Interventions: Radiology for EKGs, cardiac telemetry, monitor fluid status, daily weights
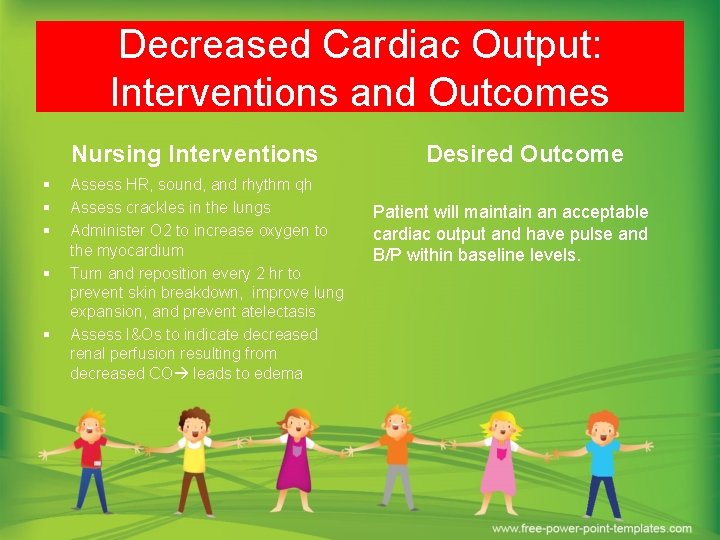
Decreased Cardiac Output: Interventions and Outcomes Nursing Interventions § § § Assess HR, sound, and rhythm qh Assess crackles in the lungs Administer O 2 to increase oxygen to the myocardium Turn and reposition every 2 hr to prevent skin breakdown, improve lung expansion, and prevent atelectasis Assess I&Os to indicate decreased renal perfusion resulting from decreased CO leads to edema Desired Outcome Patient will maintain an acceptable cardiac output and have pulse and B/P within baseline levels.

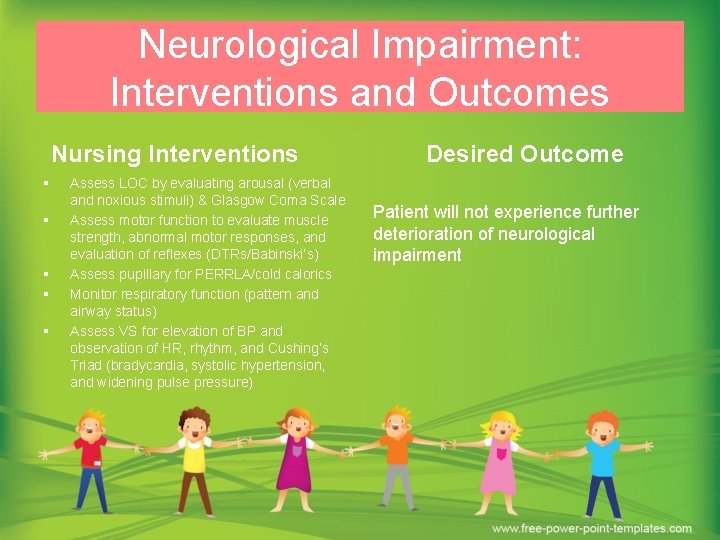
Neurological Impairment § Related to obtunded level of consciousness, right pupil non-reactive to light, no response to voice – only painful stimuli, decorticate posturing, characteristics similar to persistent vegetative state. § Rx/Treatment: O 2, mechanical ventilation Collaborative intervention: neurological assessments, changes in posturing from decorticate to decerebrate, RT for adequate ventilation settings (PEEP/VT) Complementary intervention: talking to the patient/singing songs. Traditional intervention: Provide quiet low stimulated environment
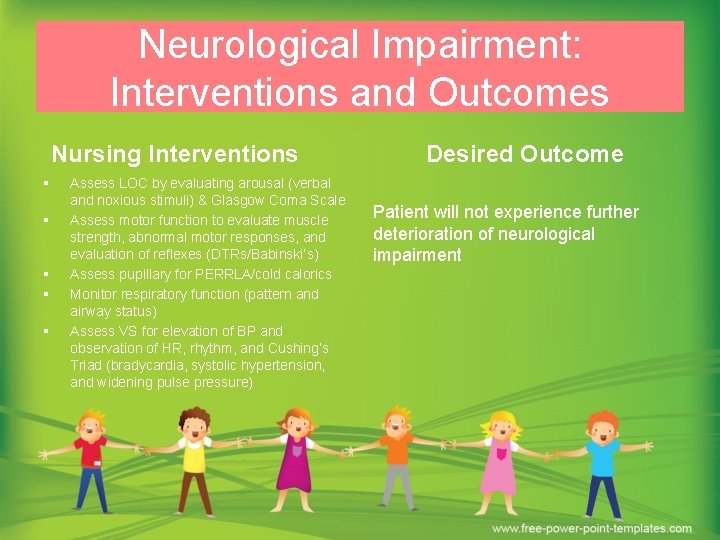
Neurological Impairment: Interventions and Outcomes Nursing Interventions § § § Assess LOC by evaluating arousal (verbal and noxious stimuli) & Glasgow Coma Scale Assess motor function to evaluate muscle strength, abnormal motor responses, and evaluation of reflexes (DTRs/Babinski’s) Assess pupillary for PERRLA/cold calorics Monitor respiratory function (pattern and airway status) Assess VS for elevation of BP and observation of HR, rhythm, and Cushing’s Triad (bradycardia, systolic hypertension, and widening pulse pressure) Desired Outcome Patient will not experience further deterioration of neurological impairment

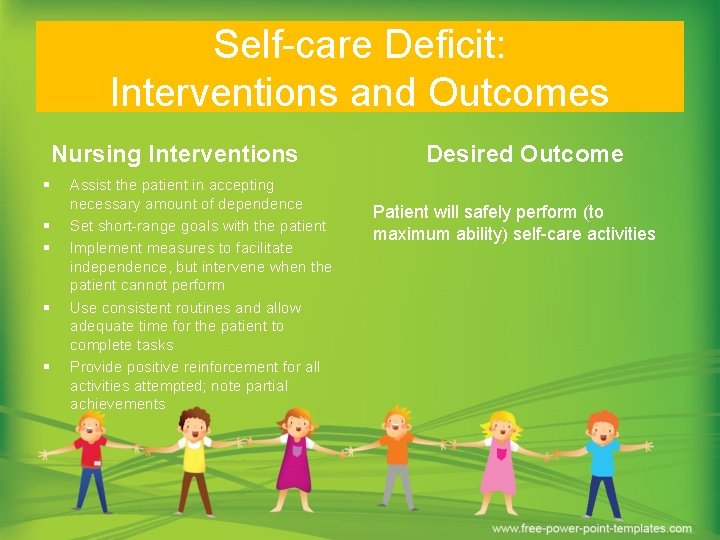
Self-care Deficit § Physical impairment – loss of mobility/inability to perform ADLs § Impaired neurological functioning persistent vegetative state § Cognitive impairment Collaborative interventions: Clinician to provide daily care, PT/OT for ROM exercises, Dietician to provide adequate feedings Traditional intervention: provide empathetic support/encouragement
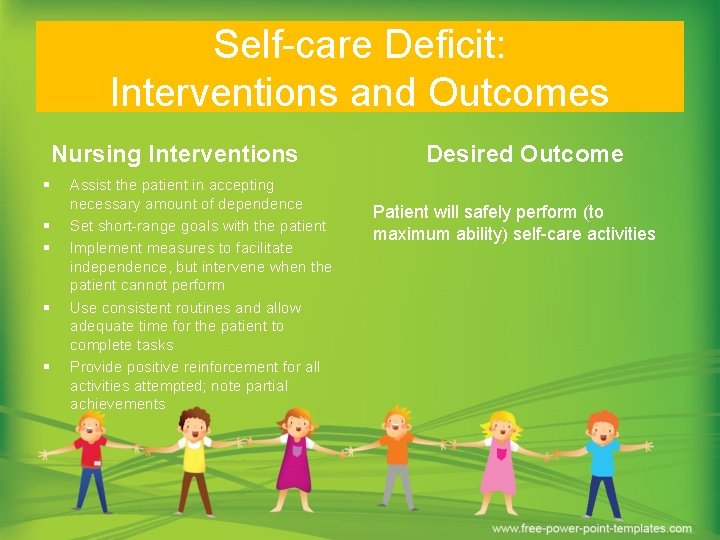
Self-care Deficit: Interventions and Outcomes Nursing Interventions § § § Assist the patient in accepting necessary amount of dependence Set short-range goals with the patient Implement measures to facilitate independence, but intervene when the patient cannot perform Use consistent routines and allow adequate time for the patient to complete tasks Provide positive reinforcement for all activities attempted; note partial achievements Desired Outcome Patient will safely perform (to maximum ability) self-care activities

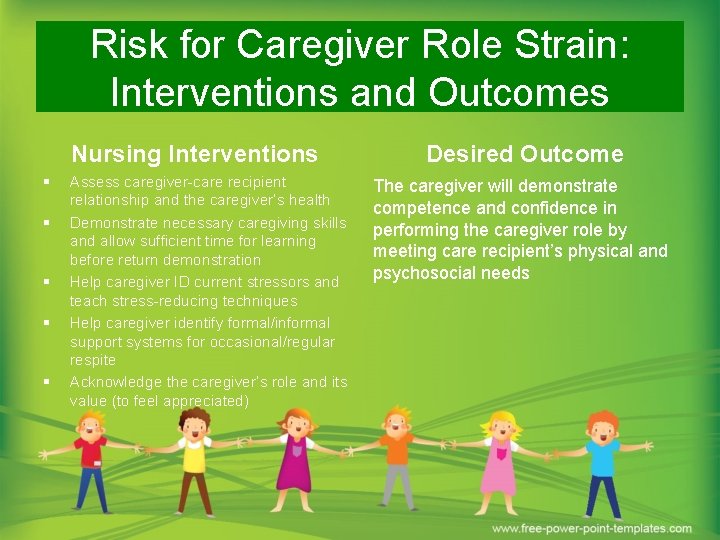
Risk for Caregiver Role Strain § § Codependency Not developmentally ready for caregiver role § Economic hardship/employment issues § Continuous medical attention § Lack of education r/t care and therapy § Providing care for other children § New disability Collaborative Intervention: Discharge planner, chaplain, OT/PT, community support groups, supplemental resources Traditional: provide empathetic support
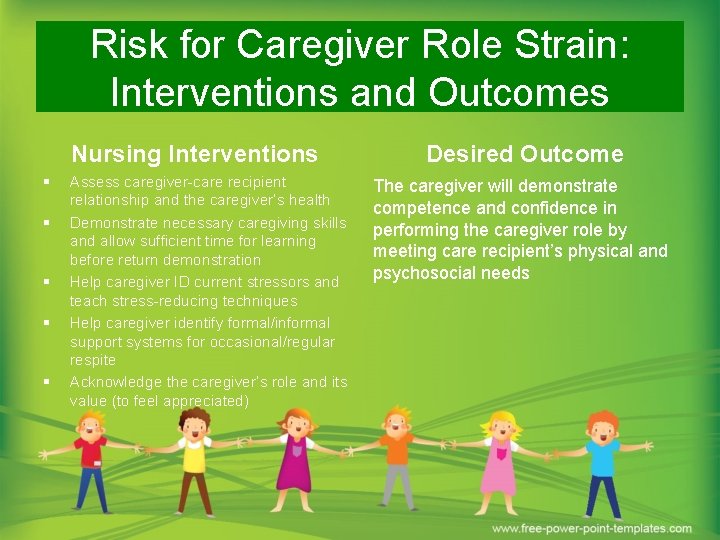
Risk for Caregiver Role Strain: Interventions and Outcomes Nursing Interventions § § § Assess caregiver-care recipient relationship and the caregiver’s health Demonstrate necessary caregiving skills and allow sufficient time for learning before return demonstration Help caregiver ID current stressors and teach stress-reducing techniques Help caregiver identify formal/informal support systems for occasional/regular respite Acknowledge the caregiver’s role and its value (to feel appreciated) Desired Outcome The caregiver will demonstrate competence and confidence in performing the caregiver role by meeting care recipient’s physical and psychosocial needs
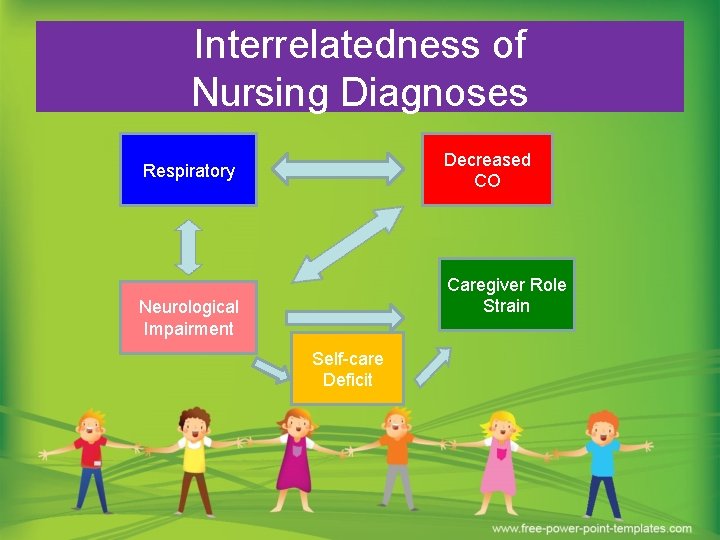
Interrelatedness of Nursing Diagnoses Decreased CO Respiratory Caregiver Role Strain Neurological Impairment Self-care Deficit
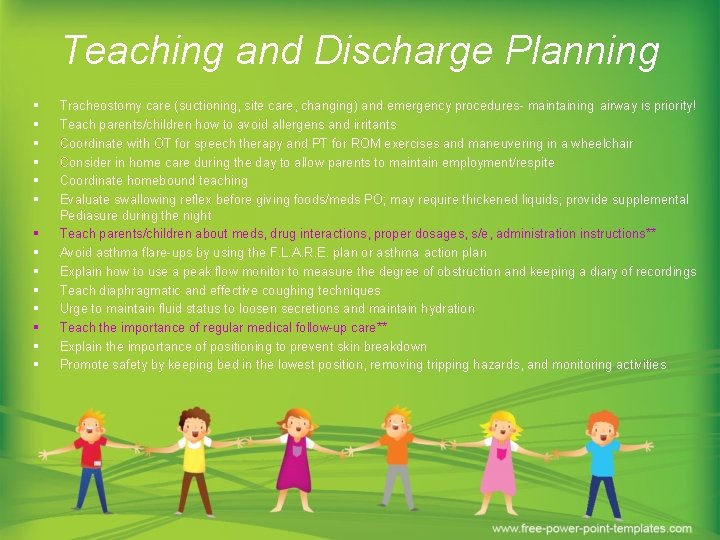
Teaching and Discharge Planning § § § § Tracheostomy care (suctioning, site care, changing) and emergency procedures- maintaining airway is priority! Teach parents/children how to avoid allergens and irritants Coordinate with OT for speech therapy and PT for ROM exercises and maneuvering in a wheelchair Consider in home care during the day to allow parents to maintain employment/respite Coordinate homebound teaching Evaluate swallowing reflex before giving foods/meds PO; may require thickened liquids; provide supplemental Pediasure during the night Teach parents/children about meds, drug interactions, proper dosages, s/e, administration instructions** Avoid asthma flare-ups by using the F. L. A. R. E. plan or asthma action plan Explain how to use a peak flow monitor to measure the degree of obstruction and keeping a diary of recordings Teach diaphragmatic and effective coughing techniques Urge to maintain fluid status to loosen secretions and maintain hydration Teach the importance of regular medical follow-up care** Explain the importance of positioning to prevent skin breakdown Promote safety by keeping bed in the lowest position, removing tripping hazards, and monitoring activities
F. L. A. R. E. Action Plan • • • Follow-up with your physician Learn your medications Asthma is a chronic disease Respond to warning signs Emergency care
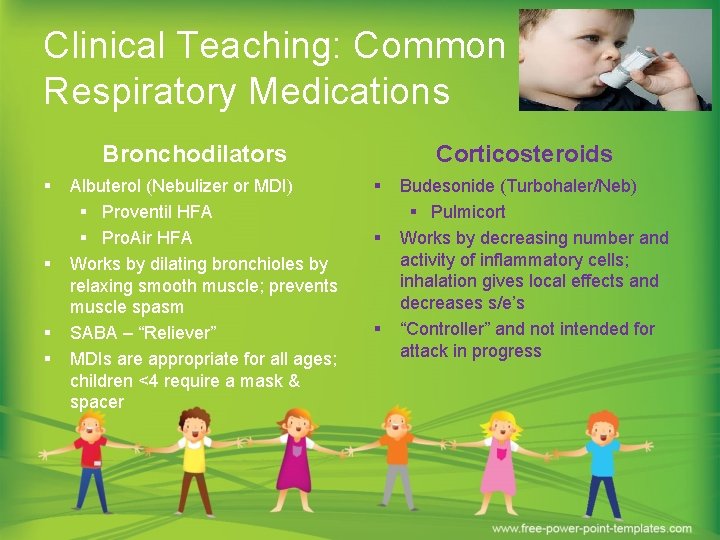
Clinical Teaching: Common Respiratory Medications Bronchodilators § § Albuterol (Nebulizer or MDI) § Proventil HFA § Pro. Air HFA Works by dilating bronchioles by relaxing smooth muscle; prevents muscle spasm SABA – “Reliever” MDIs are appropriate for all ages; children <4 require a mask & spacer Corticosteroids § § § Budesonide (Turbohaler/Neb) § Pulmicort Works by decreasing number and activity of inflammatory cells; inhalation gives local effects and decreases s/e’s “Controller” and not intended for attack in progress
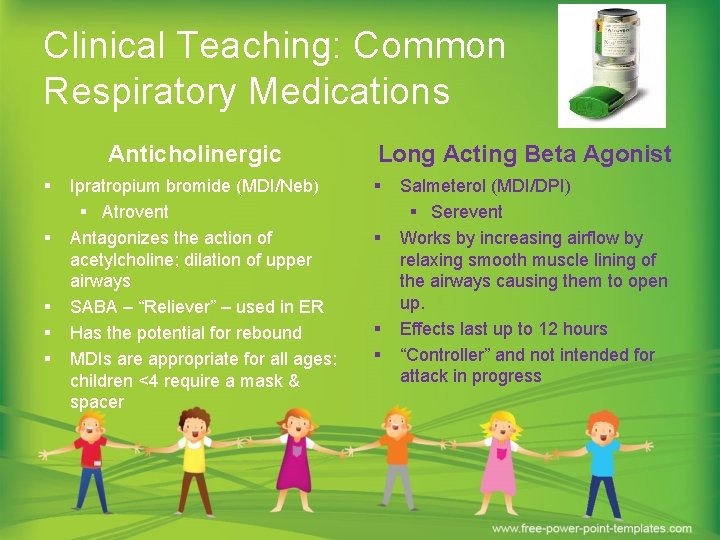
Clinical Teaching: Common Respiratory Medications Anticholinergic § § § Ipratropium bromide (MDI/Neb) § Atrovent Antagonizes the action of acetylcholine; dilation of upper airways SABA – “Reliever” – used in ER Has the potential for rebound MDIs are appropriate for all ages; children <4 require a mask & spacer Long Acting Beta Agonist § § Salmeterol (MDI/DPI) § Serevent Works by increasing airflow by relaxing smooth muscle lining of the airways causing them to open up. Effects last up to 12 hours “Controller” and not intended for attack in progress
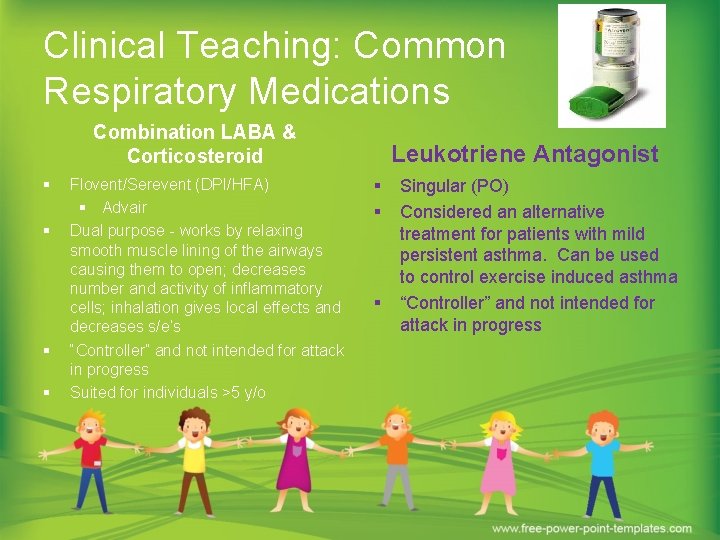
Clinical Teaching: Common Respiratory Medications Combination LABA & Corticosteroid § § Flovent/Serevent (DPI/HFA) § Advair Dual purpose - works by relaxing smooth muscle lining of the airways causing them to open; decreases number and activity of inflammatory cells; inhalation gives local effects and decreases s/e’s “Controller” and not intended for attack in progress Suited for individuals >5 y/o Leukotriene Antagonist § § § Singular (PO) Considered an alternative treatment for patients with mild persistent asthma. Can be used to control exercise induced asthma “Controller” and not intended for attack in progress
Clinical Teaching: How to use a Peak Flow Meter
Research The purpose of this study was to examine the relationship between self-efficacy beliefs and asthma self-management in urban African American (AA) youth. Research focused on 81 AA youth between the ages of 7 and 12 years old. Participants were given a survey to see 1) how often they experienced attacks, 2) how often they visited a physician, 3) the amount of medications required, and 4) individuals who were more likely to respond during an attack. Results showed that the children required 1 -2 doctor visits every 4 months (40%), 2 -3 medications (40% and 27%, respectively), had symptoms <2 per week but >2 per month (21%), and had assistance from their mothers (50. 6%) (Kaul, 2011). This research is applicable to the patient because it shows that self-management is instrumental in reducing the amounts of asthmatic attacks. Because the patient and his parents were noncompliant with medications, he experienced frequent attacks. By teaching children how to properly manage their symptoms, they can reduce asthma symptoms and morbidities related to severe asthma attacks.
Recap Ø Discussed Client History and Assessment Ø Identified and correlate Nursing Problems and plan of care as related to patient Ø Discussed Status Asthmaticus Ø Identified common medications/peak flow meter Ø Discussed research relevant to the identified patient
References Doyle, Jessica. (2008). Asthma, acid reflux: what’s the connection? . Retrieved from http: //www. foxnews. com/story/0, 2933, 396842, 00. html? s. Page=fnc/health/acidreflux Hockenberry, M. J. , & Wilson, D. (2011). Wong's nursing care of infants and children (9 th ed. ). St. Louis, Mo. : Mosby/Elsevier. Kaul, T. (2011). Helping African American children self-manage asthma: the importance of self-efficacy. Journal of School Health, 81(1), 29 -33. doi: 10. 1111/j. 17461561. 2010. 00554. x

Questions