What are the Unmet Needs of DES that






- Slides: 20

What are the Unmet Needs of DES that can be Justified by Development of BRS? Alan C. Yeung, MD Li Ka Shing Professor of Medicine Chief, Division of Cardiovascular Medicine Medical Director, Cardiovascular Health

Disclosure Statement of Financial Interest Within the past 12 months, I or my spouse/partner have had a financial interest/arrangement or affiliation with the organization(s) listed below. Affiliation/Financial Relationship • • • Grant/Research Support Scientific Advisory Board Executive Physician Council Company • • • Abbott Vascular, Medtronic, Abbott Vascular Boston Scientific Corp
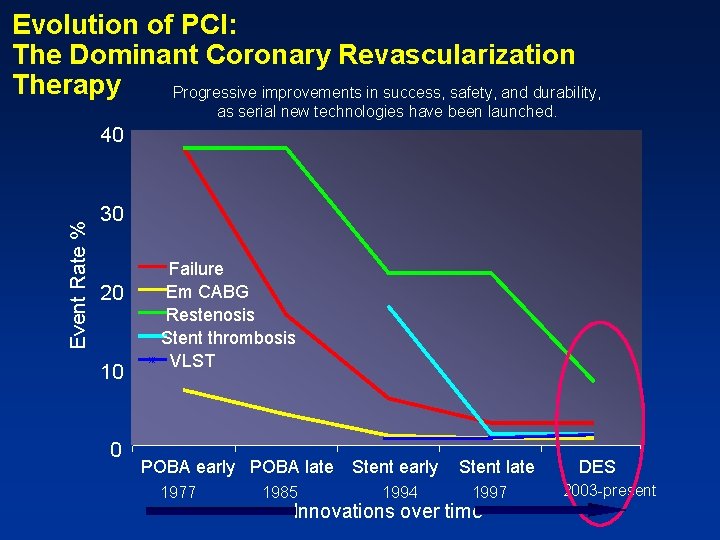
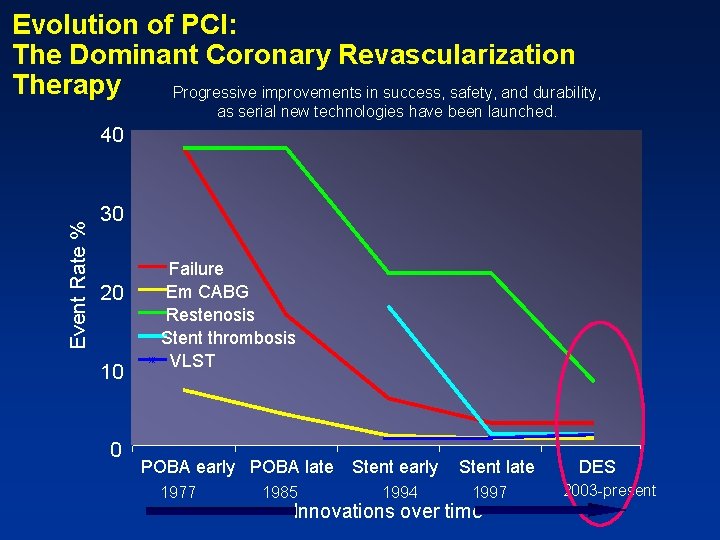
Evolution of PCI: The Dominant Coronary Revascularization Therapy Progressive improvements in success, safety, and durability, as serial new technologies have been launched. Event Rate % 40 30 20 10 0 Failure Em CABG Restenosis Stent thrombosis VLST POBA early POBA late 1977 1985 Stent early 1994 Stent late 1997 Innovations over time DES 2003 -present
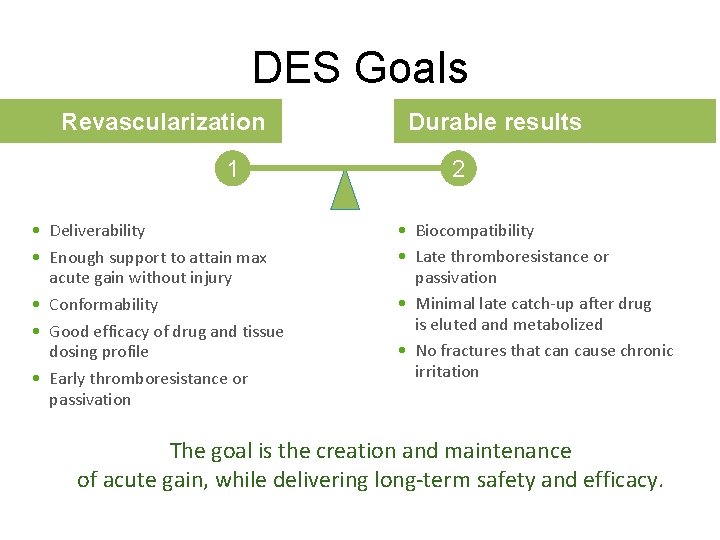
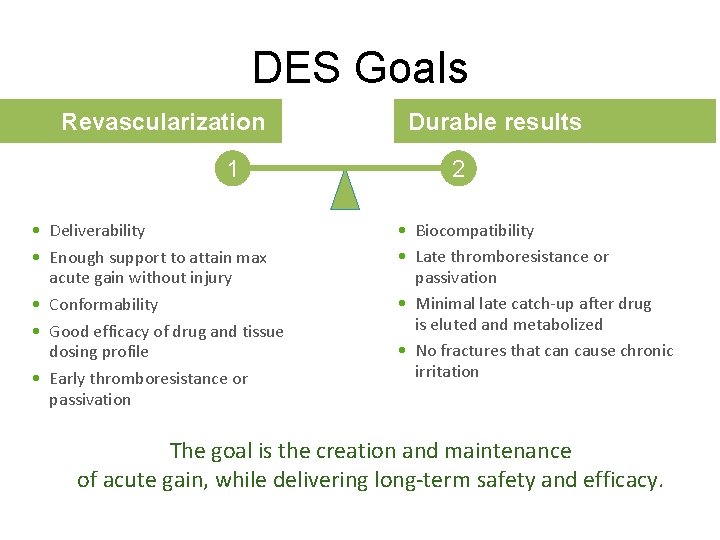
DES Goals Revascularization 1 • Deliverability • Enough support to attain max acute gain without injury • Conformability • Good efficacy of drug and tissue dosing profile • Early thromboresistance or passivation Durable results 2 • Biocompatibility • Late thromboresistance or passivation • Minimal late catch-up after drug is eluted and metabolized • No fractures that can cause chronic irritation The goal is the creation and maintenance of acute gain, while delivering long-term safety and efficacy.
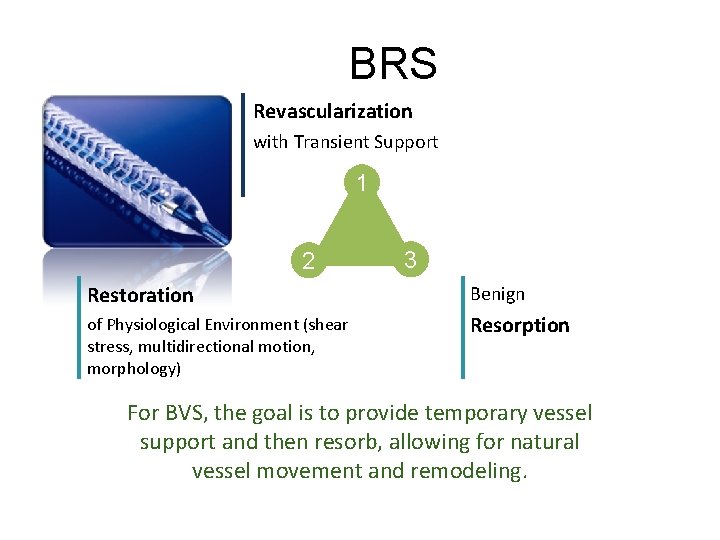
BRS Revascularization with Transient Support 1 2 3 Restoration Benign of Physiological Environment (shear stress, multidirectional motion, morphology) Resorption For BVS, the goal is to provide temporary vessel support and then resorb, allowing for natural vessel movement and remodeling.

DES UNMET NEEDS n Continue TLF creep after one year n Side branch jailing n Permanent presence of incomplete opposition n Diffuse disease stenting leading to full metal jacket n Lack of Vulnerable plaque treatment strategy n Permanent absence of vasomotion n Permanent implant

DES UNMET NEEDS n Continue TLF creep after one year n Side branch jailing n Permanent presence of incomplete apposition n Diffuse disease stenting leading to full metal jacket n Lack of Vulnerable plaque treatment strategy n Permanent absence of vasomotion n Permanent implant
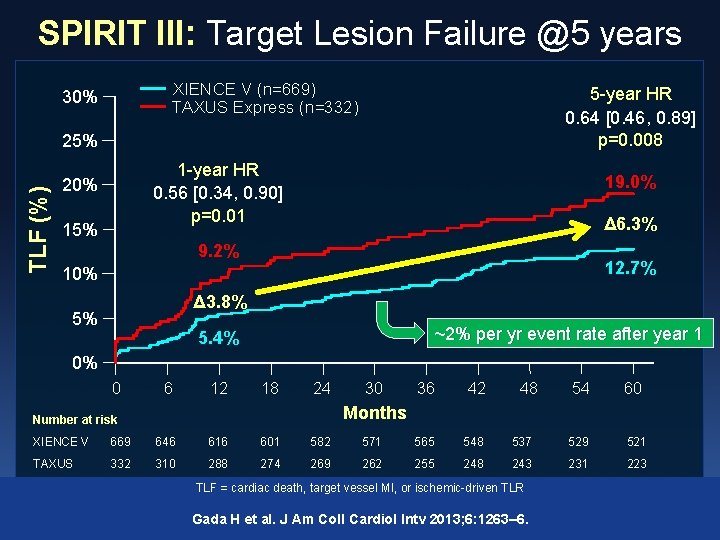
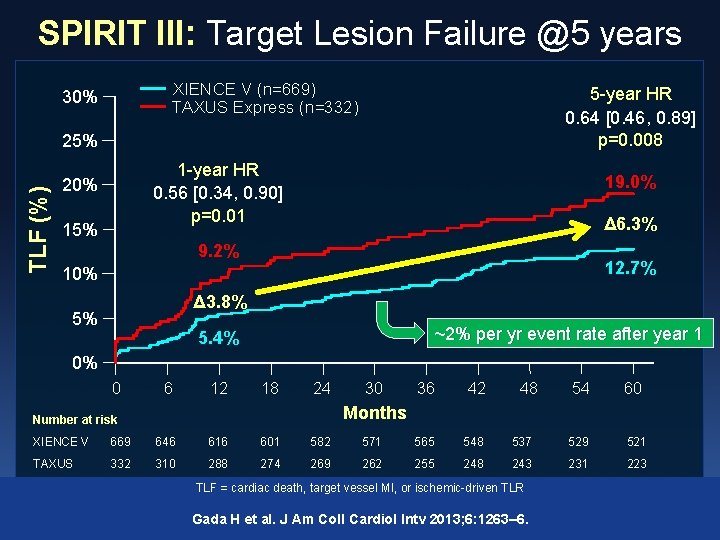
SPIRIT III: Target Lesion Failure @5 years XIENCE V (n=669) TAXUS Express (n=332) 30% 5 -year HR 0. 64 [0. 46, 0. 89] p=0. 008 TLF (%) 25% 1 -year HR 0. 56 [0. 34, 0. 90] p=0. 01 20% 15% 19. 0% Δ 6. 3% 9. 2% 12. 7% 10% Δ 3. 8% 5% ~2% per yr event rate after year 1 5. 4% 0% 0 6 12 18 24 30 36 42 48 54 60 Months Number at risk XIENCE V 669 646 616 601 582 571 565 548 537 529 521 TAXUS 332 310 288 274 269 262 255 248 243 231 223 TLF = cardiac death, target vessel MI, or ischemic-driven TLR Gada H et al. J Am Coll Cardiol Intv 2013; 6: 1263– 6.
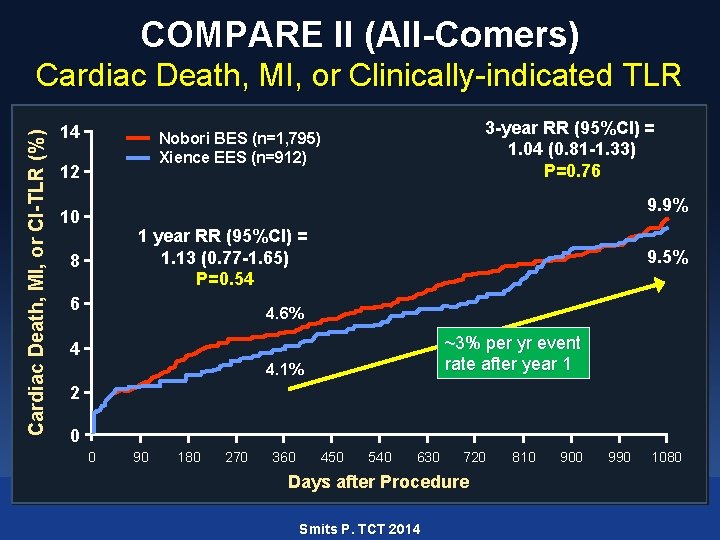
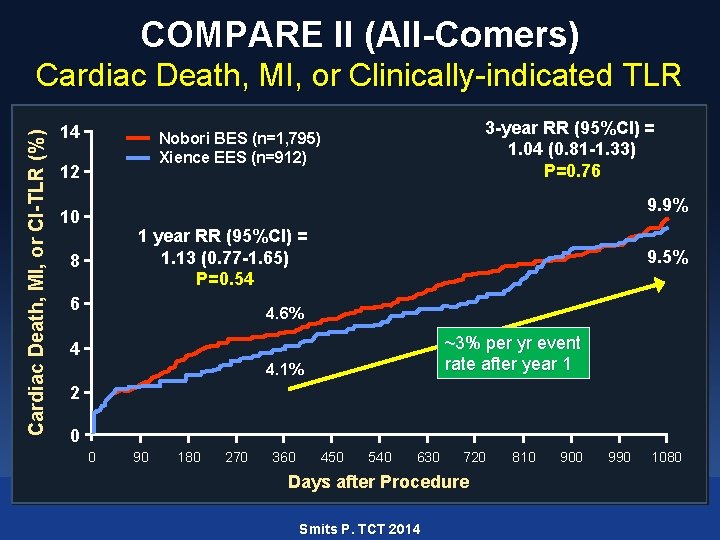
COMPARE II (All-Comers) Cardiac Death, MI, or CI-TLR (%) Cardiac Death, MI, or Clinically-indicated TLR 14 3 -year RR (95%CI) = 1. 04 (0. 81 -1. 33) P=0. 76 Nobori BES (n=1, 795) Xience EES (n=912) 12 9. 9% 10 1 year RR (95%CI) = 1. 13 (0. 77 -1. 65) P=0. 54 8 6 9. 5% 4. 6% ~3% per yr event rate after year 1 4 4. 1% 2 0 0 90 180 270 360 450 540 630 720 Days after Procedure Smits P. TCT 2014 810 900 990 1080
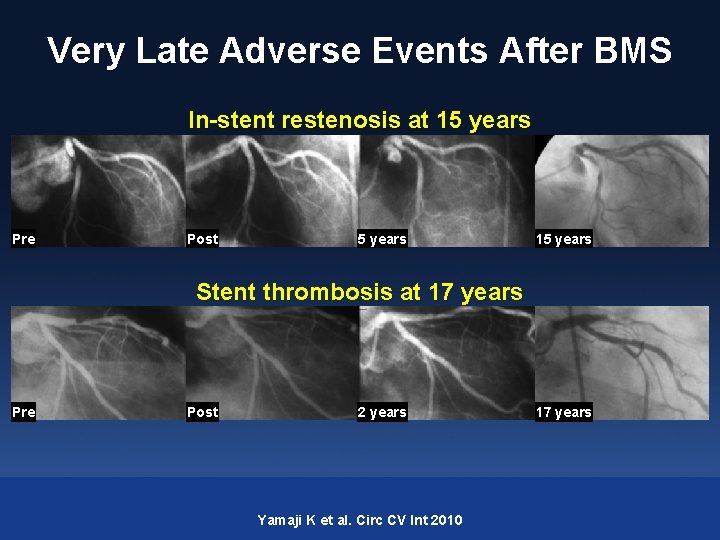
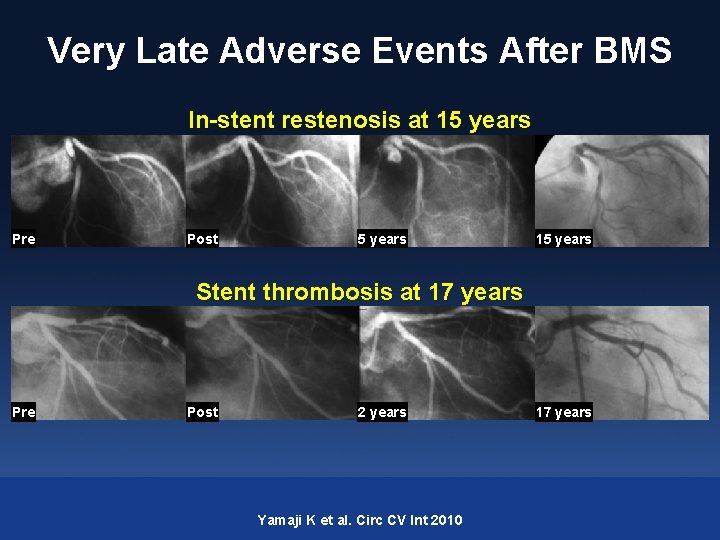
Very Late Adverse Events After BMS In-stent restenosis at 15 years Pre Post 5 years 15 years Stent thrombosis at 17 years Pre Post 2 years Yamaji K et al. Circ CV Int 2010 17 years
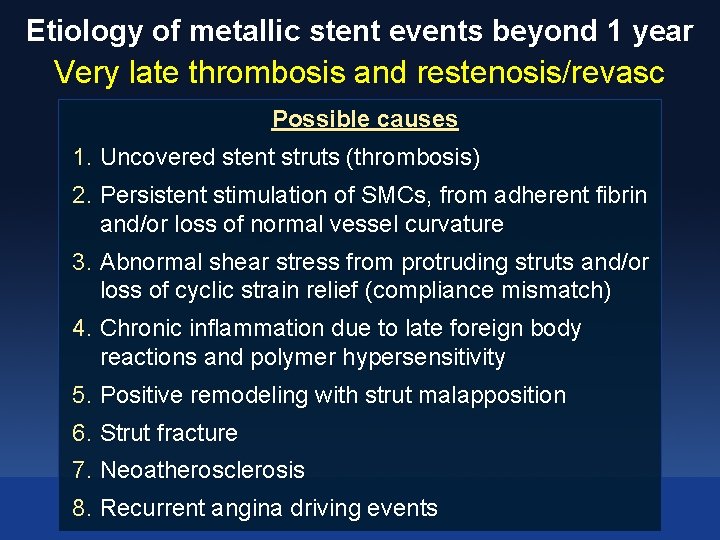
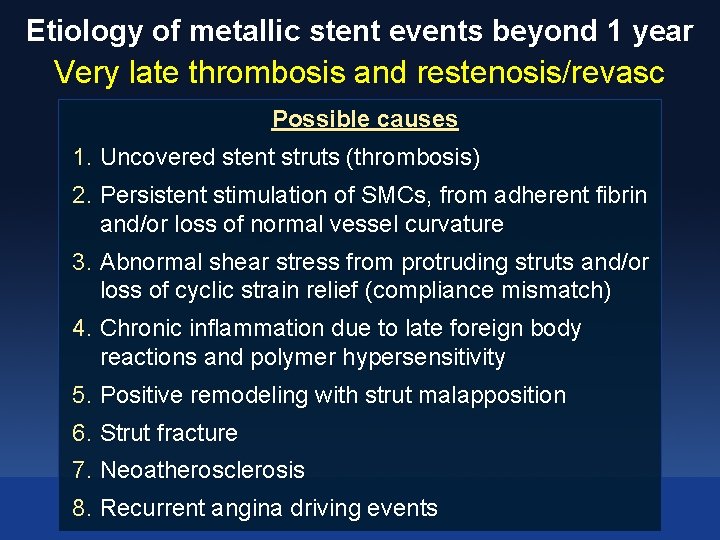
Etiology of metallic stent events beyond 1 year Very late thrombosis and restenosis/revasc Possible causes 1. Uncovered stent struts (thrombosis) 2. Persistent stimulation of SMCs, from adherent fibrin and/or loss of normal vessel curvature 3. Abnormal shear stress from protruding struts and/or loss of cyclic strain relief (compliance mismatch) 4. Chronic inflammation due to late foreign body reactions and polymer hypersensitivity 5. Positive remodeling with strut malapposition 6. Strut fracture 7. Neoatherosclerosis 8. Recurrent angina driving events
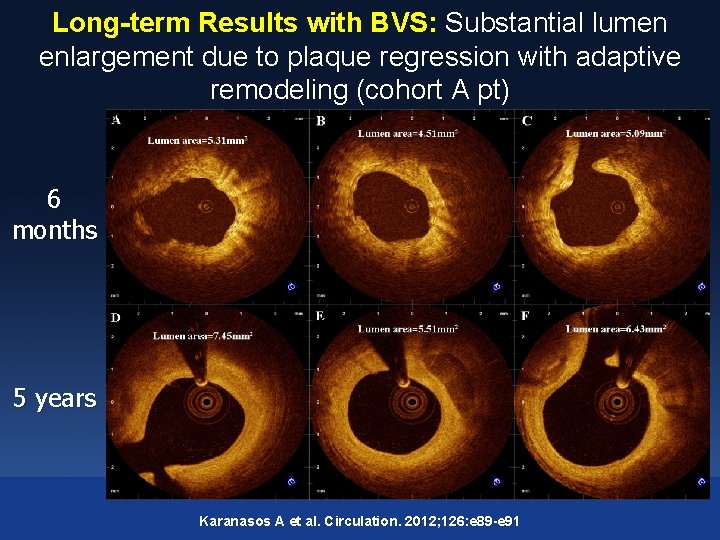
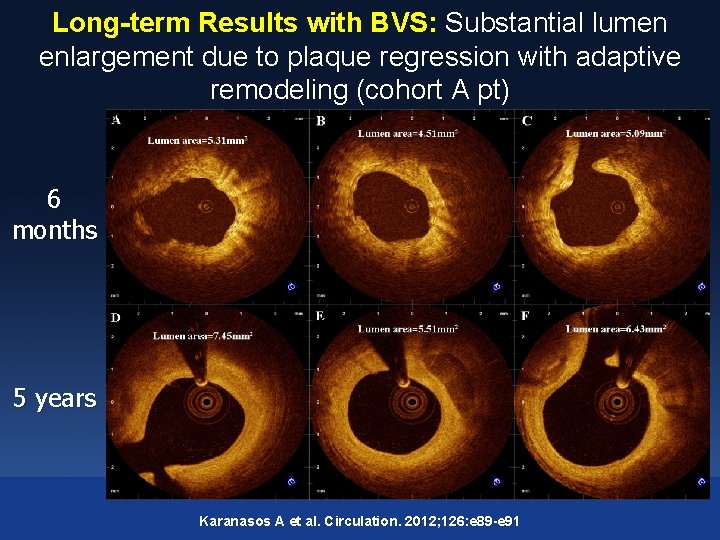
Long-term Results with BVS: Substantial lumen enlargement due to plaque regression with adaptive remodeling (cohort A pt) 6 months 5 years Karanasos A et al. Circulation. 2012; 126: e 89 -e 91

From TAXUS to XIENCE to ABSORB 30% Absorb BVS (theoretical) XIENCE EES (n=669) TAXUS PES (n=332) TLF (%) 25% 19. 0% 20% 15% 9. 2% 10% 12. 7% 5% 7. 2% 5. 4% 0% 0 6 12 18 24 30 36 42 48 54 60 Months Number at risk XIENCE V 669 646 616 601 582 571 565 548 537 529 521 TAXUS 332 310 288 274 269 262 255 248 243 231 223 TLF = cardiac death, target vessel MI, or ischemic-driven TLR Spirit III: Gada H et al. J Am Coll Cardiol Intv 2013; 6: 1263– 6
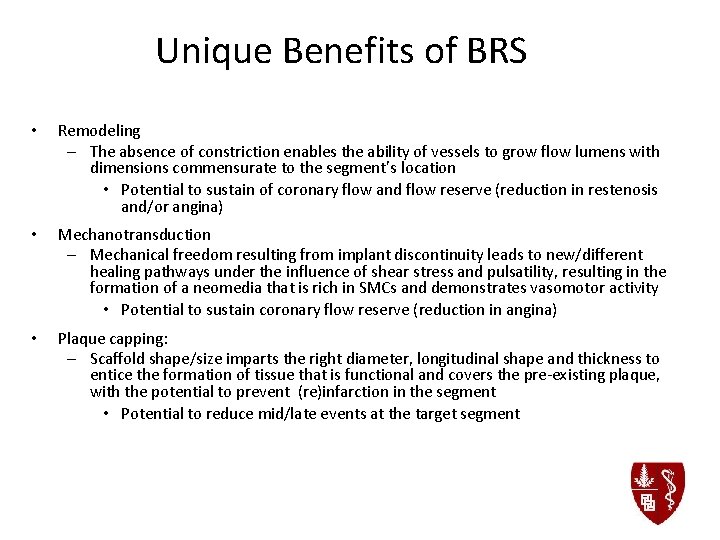
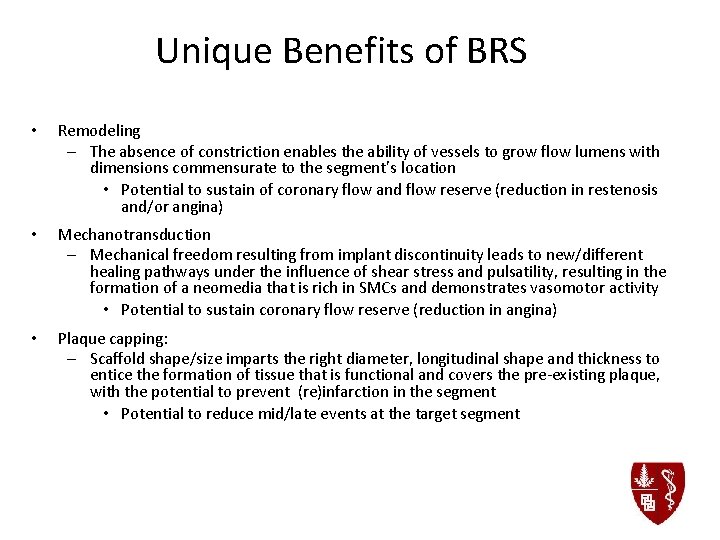
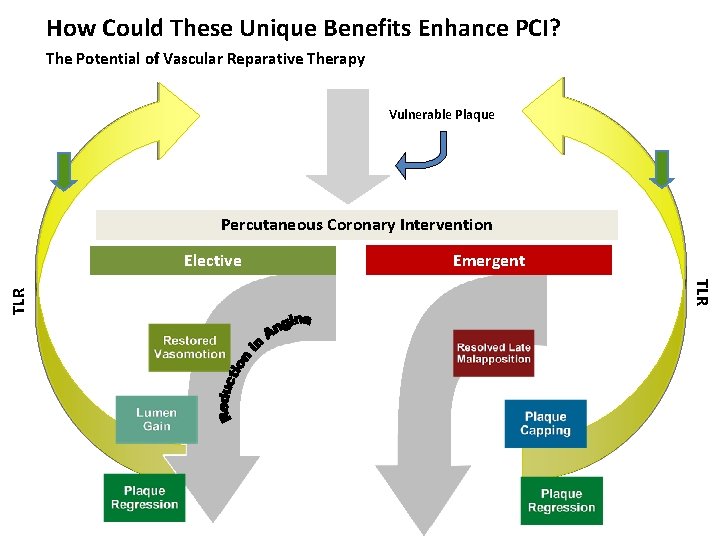
Unique Benefits of BRS • Remodeling – The absence of constriction enables the ability of vessels to grow flow lumens with dimensions commensurate to the segment’s location • Potential to sustain of coronary flow and flow reserve (reduction in restenosis and/or angina) • Mechanotransduction – Mechanical freedom resulting from implant discontinuity leads to new/different healing pathways under the influence of shear stress and pulsatility, resulting in the formation of a neomedia that is rich in SMCs and demonstrates vasomotor activity • Potential to sustain coronary flow reserve (reduction in angina) • Plaque capping: – Scaffold shape/size imparts the right diameter, longitudinal shape and thickness to entice the formation of tissue that is functional and covers the pre-existing plaque, with the potential to prevent (re)infarction in the segment • Potential to reduce mid/late events at the target segment
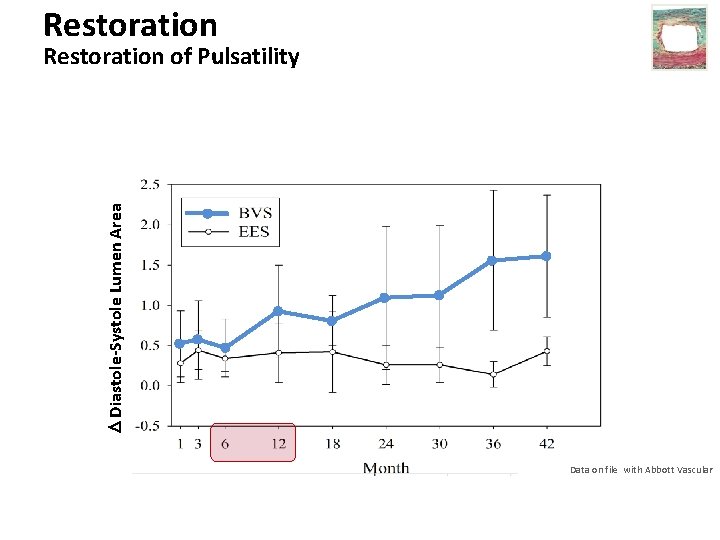
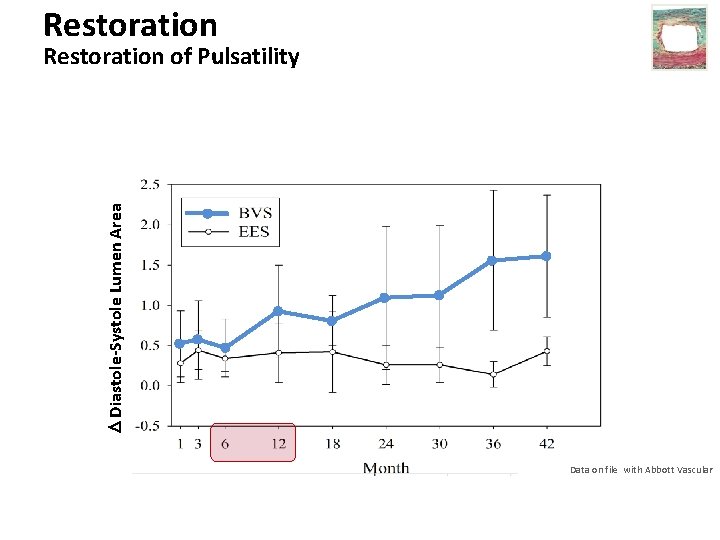
Restoration Diastole-Systole Lumen Area Restoration of Pulsatility Data on file with Abbott Vascular
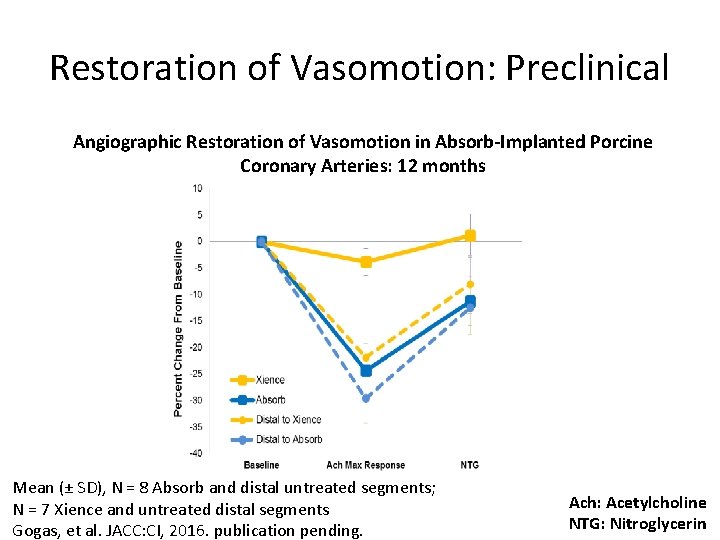
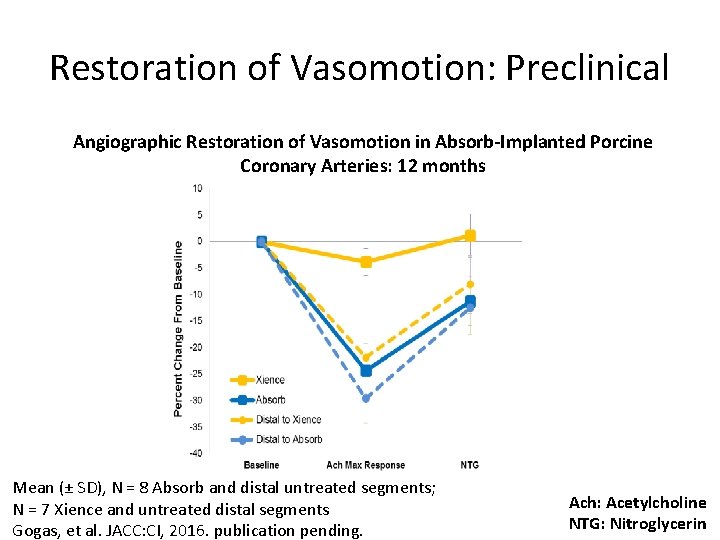
Restoration of Vasomotion: Preclinical Angiographic Restoration of Vasomotion in Absorb-Implanted Porcine Coronary Arteries: 12 months Mean (± SD), N = 8 Absorb and distal untreated segments; N = 7 Xience and untreated distal segments Gogas, et al. JACC: CI, 2016. publication pending. Ach: Acetylcholine NTG: Nitroglycerin

Why BRS may extend the scope of PCI using DES ? Diffuse LAD disease (vs. LIMA) Precision PCI By sealing high risk plaques Bioresorbable reservoir for specific indications (e. g. STEMI, ISR)
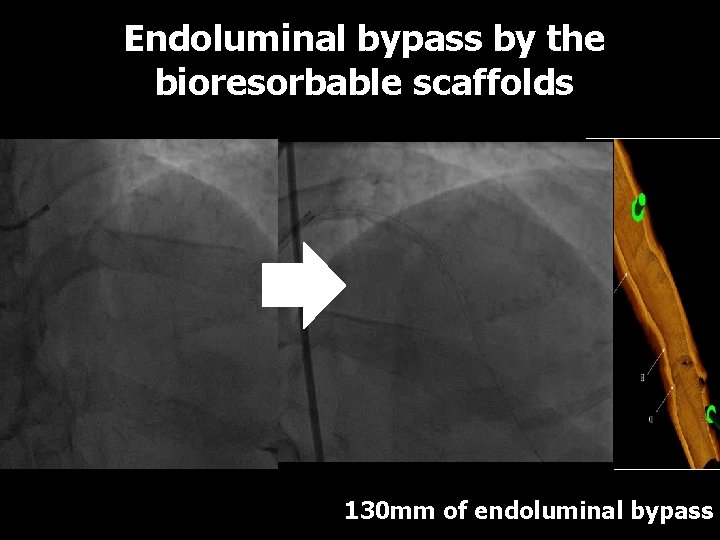
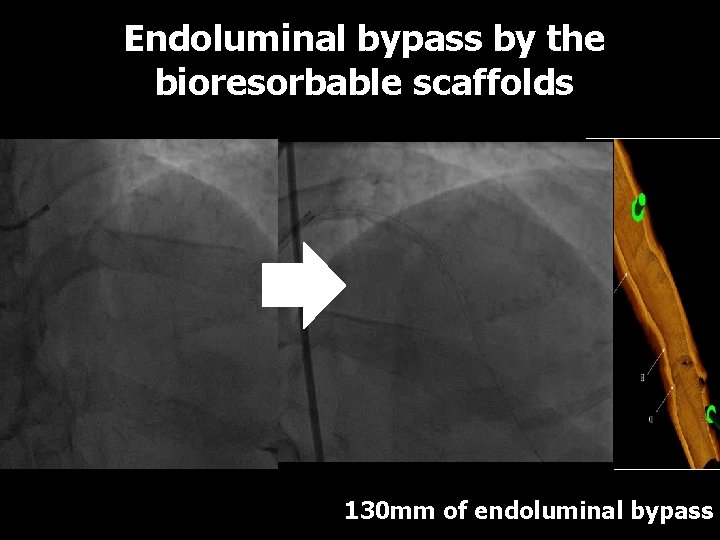
Endoluminal bypass by the bioresorbable scaffolds LCx Absorb 2. 5 x 28 mm Absorb 3. 5× 28 mm Absorb 3. 0× 28 mm Absorb 2. 5× 18 mm SYNTAX score 36 130 mm of endoluminal bypass
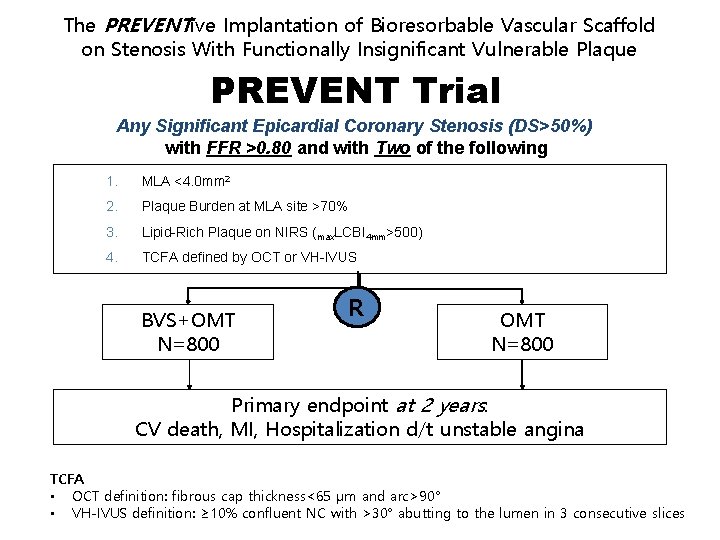
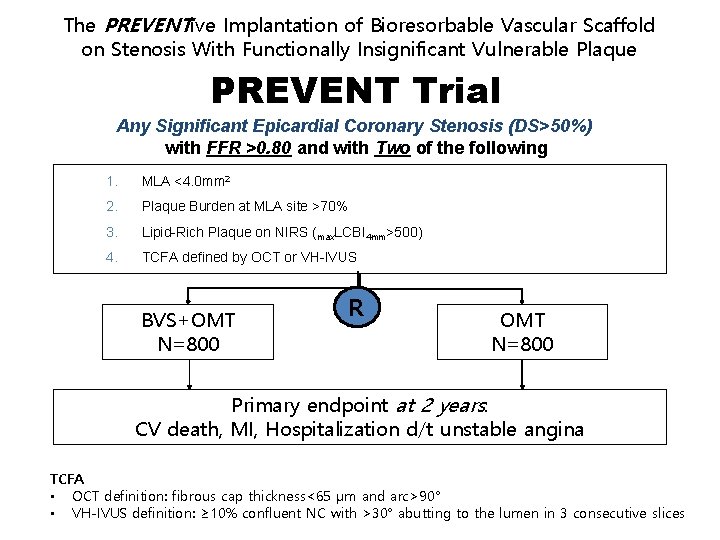
The PREVENTive Implantation of Bioresorbable Vascular Scaffold on Stenosis With Functionally Insignificant Vulnerable Plaque PREVENT Trial Any Significant Epicardial Coronary Stenosis (DS>50%) with FFR >0. 80 and with Two of the following 1. MLA <4. 0 mm 2 2. Plaque Burden at MLA site >70% 3. Lipid-Rich Plaque on NIRS (max. LCBI 4 mm>500) 4. TCFA defined by OCT or VH-IVUS BVS+OMT N=800 R OMT N=800 Primary endpoint at 2 years: CV death, MI, Hospitalization d/t unstable angina TCFA • OCT definition: fibrous cap thickness<65 μm and arc>90° • VH-IVUS definition: ≥ 10% confluent NC with >30° abutting to the lumen in 3 consecutive slices
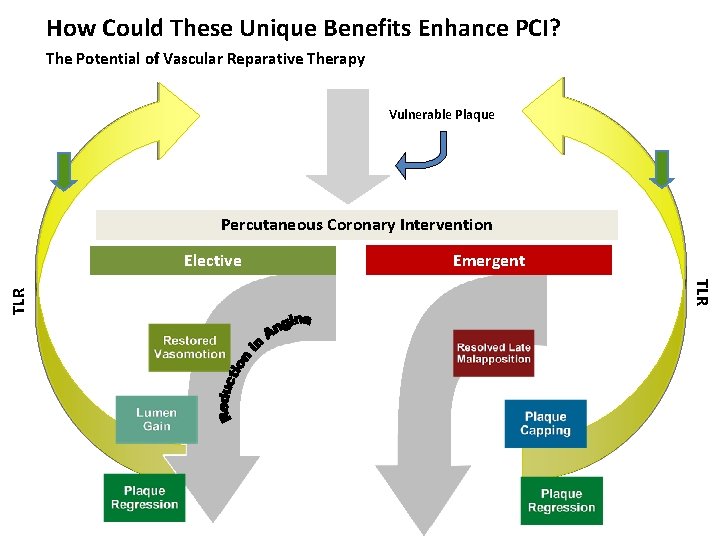
How Could These Unique Benefits Enhance PCI? The Potential of Vascular Reparative Therapy Vulnerable Plaque Percutaneous Coronary Intervention Emergent TLR Elective
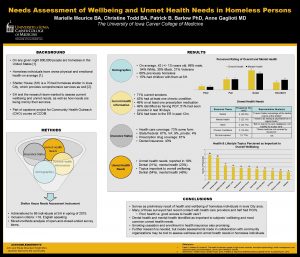
 Unmet needs in severe asthma
Unmet needs in severe asthma Insidan region jh
Insidan region jh Unmet financial need
Unmet financial need Des des des
Des des des Walmart thất bại ở nhật
Walmart thất bại ở nhật Gây tê cơ vuông thắt lưng
Gây tê cơ vuông thắt lưng Premature atrial contraction
Premature atrial contraction Tìm vết của mặt phẳng
Tìm vết của mặt phẳng Sau thất bại ở hồ điển triệt
Sau thất bại ở hồ điển triệt Thể thơ truyền thống
Thể thơ truyền thống Con hãy đưa tay khi thấy người vấp ngã
Con hãy đưa tay khi thấy người vấp ngã Thơ thất ngôn tứ tuyệt đường luật
Thơ thất ngôn tứ tuyệt đường luật Tôn thất thuyết là ai
Tôn thất thuyết là ai Ngoại tâm thu thất chùm đôi
Ngoại tâm thu thất chùm đôi Strategic gender needs and practical gender needs
Strategic gender needs and practical gender needs Learning situation analysis
Learning situation analysis Satisfaction
Satisfaction Primary needs and secondary needs
Primary needs and secondary needs Simple claustral complex
Simple claustral complex Je t'offrirai des fleurs et des nappes en couleurs
Je t'offrirai des fleurs et des nappes en couleurs Budget des ventes
Budget des ventes