Western Australian Multidisciplinary Post Fall Management Guidelines Physiotherapy
- Slides: 16
Western Australian Multidisciplinary Post Fall Management Guidelines: Physiotherapy 2018
Information about this Power. Point • It provides a summary of the updated Post Fall Multidisciplinary Management Guidelines for Western Australian Health Care Settings 2018. • It is designed to assist in the education of all health professionals involved in the care of a patient post fall. • All health professionals involved in the care of a patient post fall should receive this information. • It is a basic outline and contains only essential information. • It can be adapted to suit your local area and staff. • Refer to the complete guidelines. • Supplementary notes are given below the slides. • The application of local policy may indicate alternative actions or other policies to meet requirements. Please contact Falls. Management. WA@health. wa. gov. au if you have any questions/comments or feedback 2
Role of Physiotherapist The role of Physiotherapy is integral to the multidisciplinary management and care of patients who are at risk of falling, or who have fallen. Local Policy May Apply to Some of These Actions 3
4 main components for Physiotherapy review of a patient following a fall 1. Assessment 2. Intervention 3. Documentation 4. Discharge Planning 4
Note: • Important to involve carers throughout the process where possible. • Physiotherapists are well placed to monitor for any behavioural or thinking changes in their patients. • Escalating any concerns to the Medical Team. 5
Assessment • Once notified patient should be reviewed within 2 working days. • Review details, and results. • Ensure patient has been cleared to mobilise by the Medical Officer. • If verbal consent document this and their name and contact details. Local Policy May Apply to Some of These Actions 6
Assessments include: • • Mobility Strength Balance Other assessments deemed appropriate and necessary It is important to note that if the patient is unable to participate in the assessment due to pain, difficulty in weight-bearing or acute confusion, the physiotherapist should refer back to the MO for further review / investigations. 7
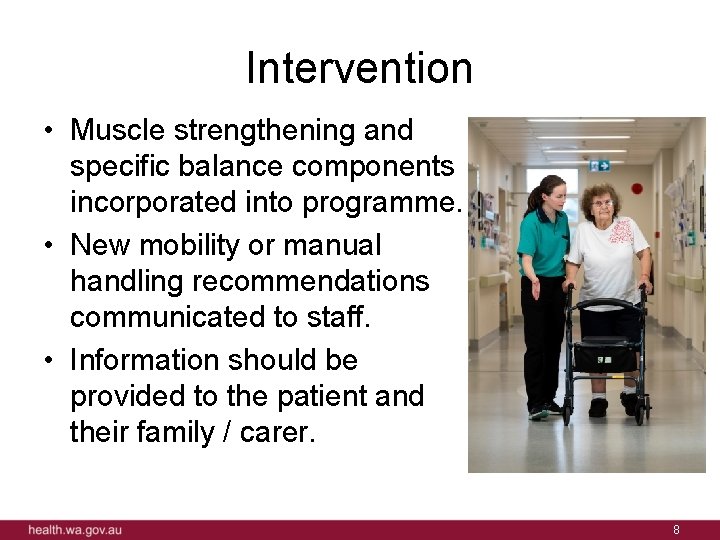
Intervention • Muscle strengthening and specific balance components incorporated into programme. • New mobility or manual handling recommendations communicated to staff. • Information should be provided to the patient and their family / carer. 8
Documentation • Clinical assessment findings. • Recommendations and strategies. • Documented to ensure safety when mobilising for patient and staff. • Update FRAMP and any site specific communication tool. Local Policy May Apply to Some of These Actions 9
Discharge • Start plans early, involving the patients and their carers in the process. • Post-discharge rehabilitation and falls prevention needs should be identified. • Referrals and handovers to appropriate local community services. • Utilise the local service discharge log. Local Policy May Apply to Some of These Actions 10
Resources (refer to Appendices 3. 1 and 3. 2 in the Guidelines) Post Fall Lanyard 11
Post Fall Assessment Proforma Sample 12
Summary • The role of Physiotherapy is integral to the multidisciplinary management and care of patients who are at risk of falling, or who have fallen. • The guidelines have developed by the Physiotherapists within the Western Australian Multidisciplinary Post Fall Guideline Working Party 2018 as evidenced based care for the patient post fall. • State-wide consultation of consumers, health professionals including aboriginal and untrained health care staff has occurred during the guideline development. • The guidelines are to be utilised in conjunction with the Post Fall Management Guidelines in Western Australian Healthcare Settings 2018. Contact Falls. Management@health. wa. gov. au for more information 13
Quiz questions • The following are quiz questions that can be utilised in conjunction with education on the Physiotherapy Post Fall Guidelines 14
Questions • In the absence of documented clearance to mobilise following an inpatient fall, is verbal approval to mobilise a patient sufficient? – No – Yes from the patients nurse – Yes from a DR with their name and contact details documented. • If a patient is unable to participate in the Physiotherapy assessment due to pain, difficulty weight-bearing or acute confusion, what is recommended: – Keep going - no pain no gain! – Press the medical emergency alarm – Stop the assessment and inform the medical officer for further review • What should physiotherapists monitor for during their interactions with patients? – Changes in the patients thinking or behaviour that could indicate a delirium – Signs of clinical deterioration – Environmental Hazards – All of the above 15
Questions Continued… • Where would physiotherapists document patient education provided? – – The FRAMP Patient medical record • Where would the Physiotherapist document their assessment findings and recommendations'? – The FRAMP – Patient Care Plan – Mobility Chart – Any other site specific tool or document, as per local policy – All of the above • Who would they inform of these recommendations? – The staff – The Patient – The Family / carer of the patient – All of the above • When would the Physiotherapist involve the patient and their carer? – Only when asked by the patient and carer – Only for patients with cognitive impairment – At each stage of the patients journey 16