West Suffolk Community Pain Management Service Christine Waters




- Slides: 36
West Suffolk Community Pain Management Service Christine Waters Senior CNS: Professional Development RN (Non Medical Prescriber) MSc Pain Management Christine. waters 4@nhs. net December 2015
Outline 1. Overview of West Suffolk Community Pain Management Service 2. Reducing the risks of opioid management: national and local initiatives 3. Signposting patients to self management resources 4. CPD resources for HCPs – now and the future 5. Discussion 2
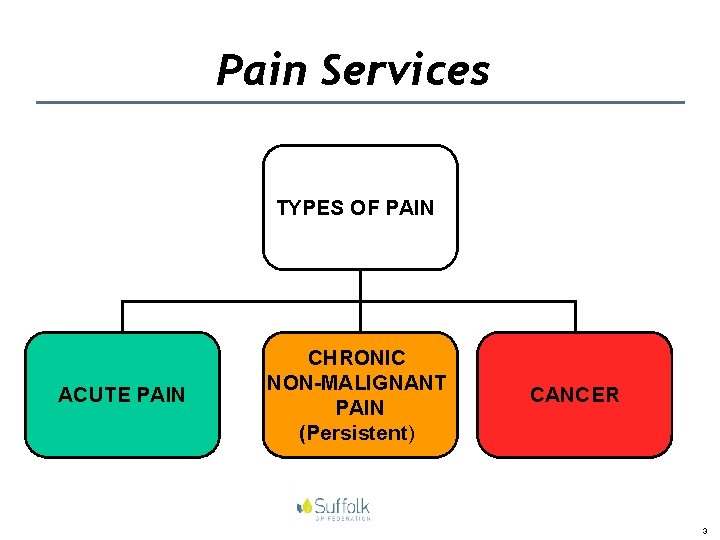
Pain Services TYPES OF PAIN ACUTE PAIN CHRONIC NON-MALIGNANT PAIN (Persistent) CANCER 3
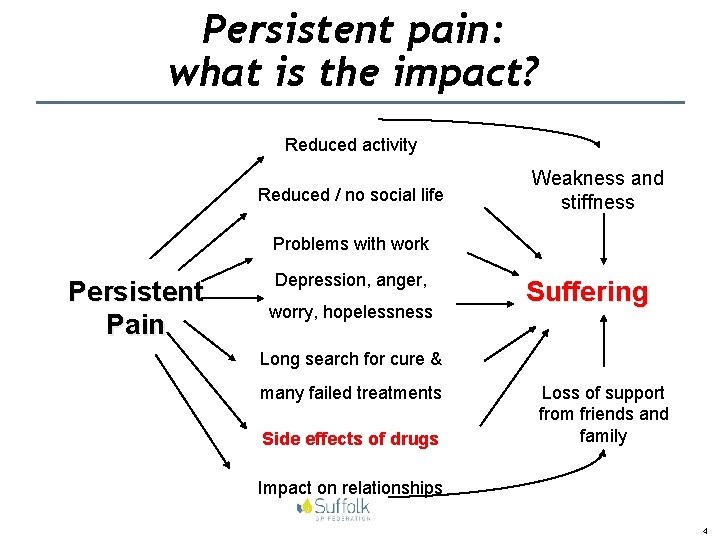
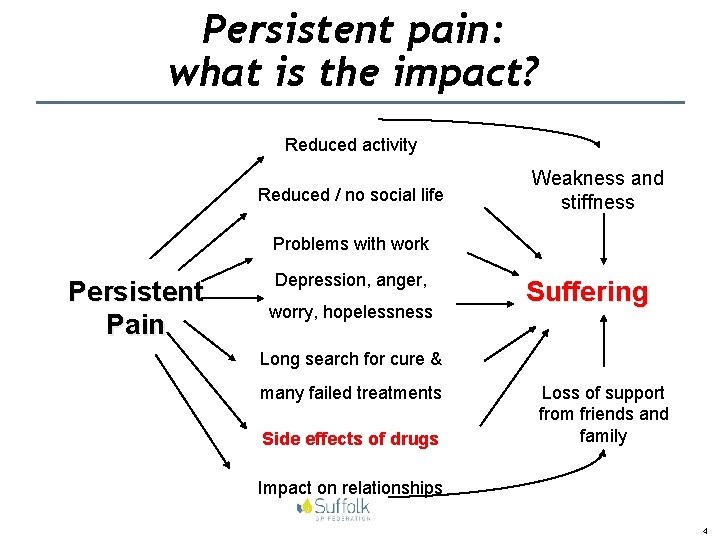
Persistent pain: what is the impact? Reduced activity Reduced / no social life Weakness and stiffness Problems with work Persistent Pain Depression, anger, worry, hopelessness Suffering Long search for cure & many failed treatments Side effects of drugs Loss of support from friends and family Impact on relationships 4
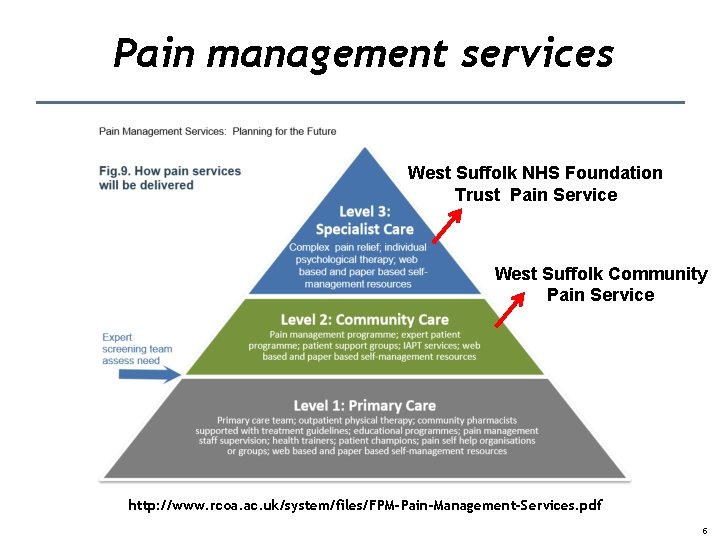
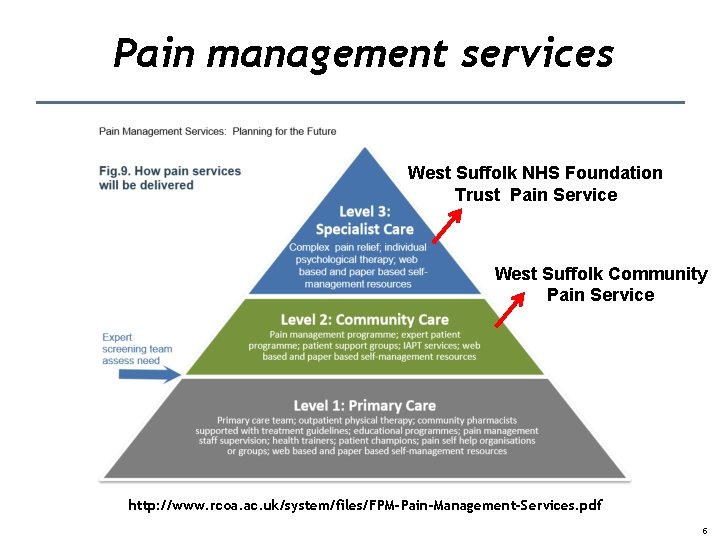
Pain management services West Suffolk NHS Foundation Trust Pain Service West Suffolk Community Pain Service http: //www. rcoa. ac. uk/system/files/FPM-Pain-Management-Services. pdf 5
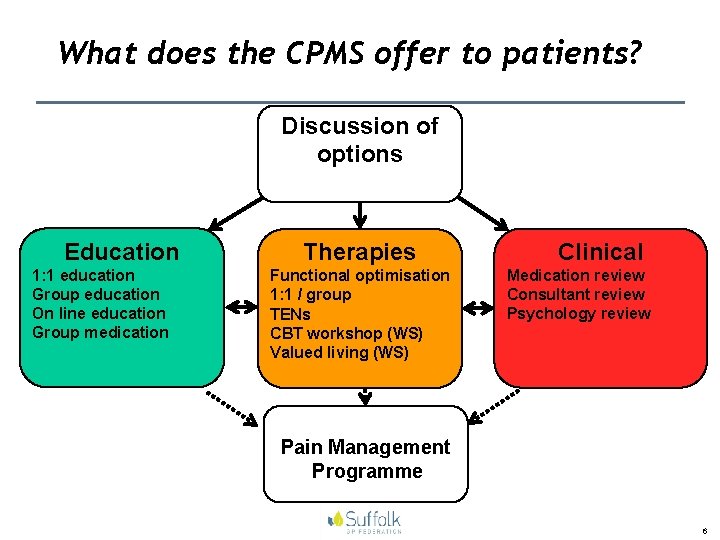
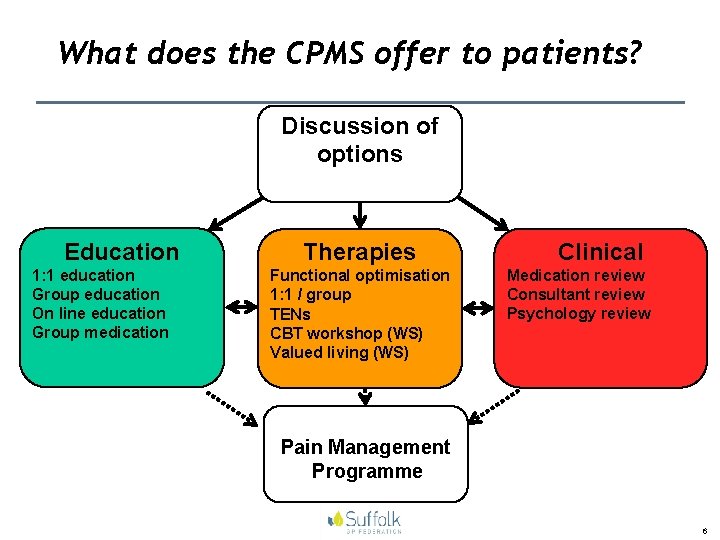
What does the CPMS offer to patients? Discussion of options Education Therapies 1: 1 education Group education On line education Group medication Functional optimisation 1: 1 / group TENs CBT workshop (WS) Valued living (WS) Clinical Medication review Consultant review Psychology review Pain Management Programme 6
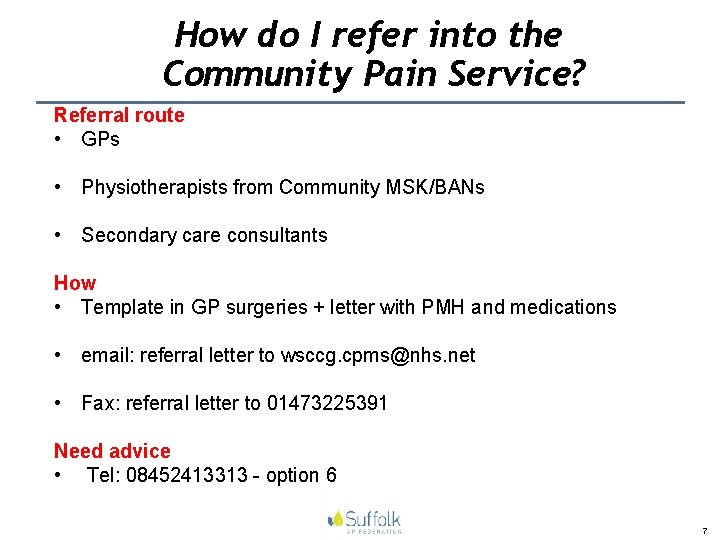
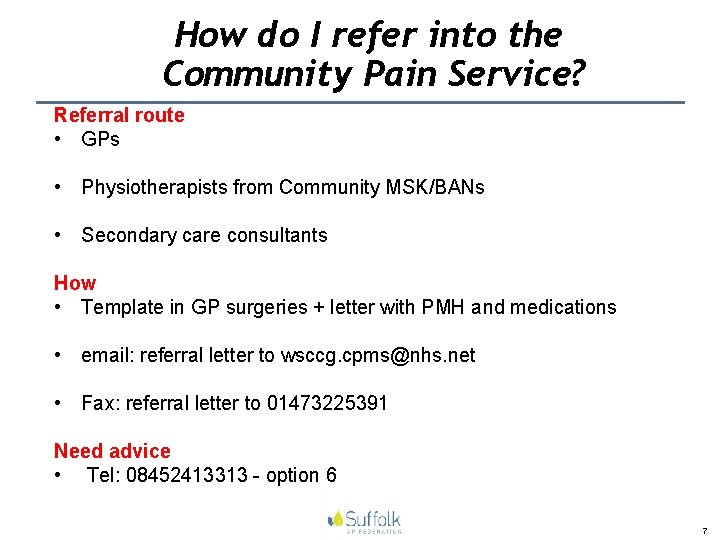
How do I refer into the Community Pain Service? Referral route • GPs • Physiotherapists from Community MSK/BANs • Secondary care consultants How • Template in GP surgeries + letter with PMH and medications • email: referral letter to wsccg. cpms@nhs. net • Fax: referral letter to 01473225391 Need advice • Tel: 08452413313 - option 6 7
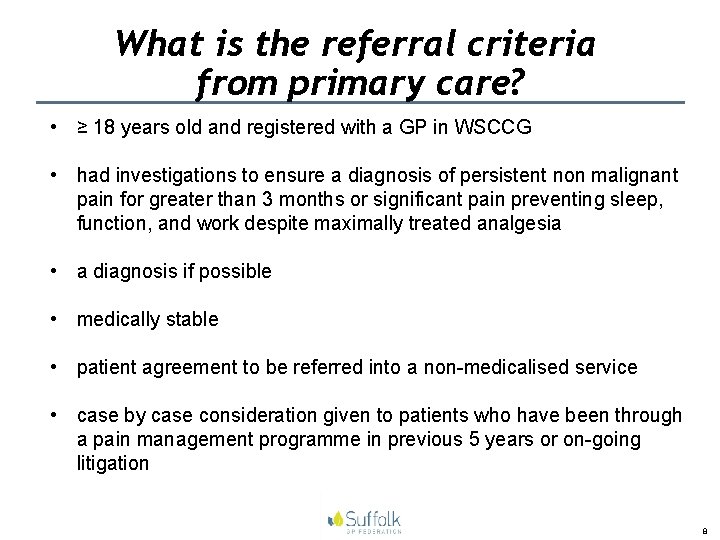
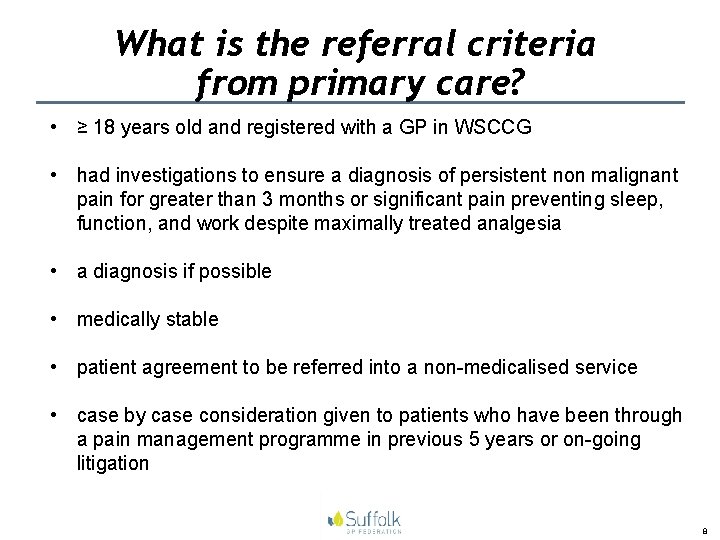
What is the referral criteria from primary care? • ≥ 18 years old and registered with a GP in WSCCG • had investigations to ensure a diagnosis of persistent non malignant pain for greater than 3 months or significant pain preventing sleep, function, and work despite maximally treated analgesia • a diagnosis if possible • medically stable • patient agreement to be referred into a non-medicalised service • case by case consideration given to patients who have been through a pain management programme in previous 5 years or on-going litigation 8
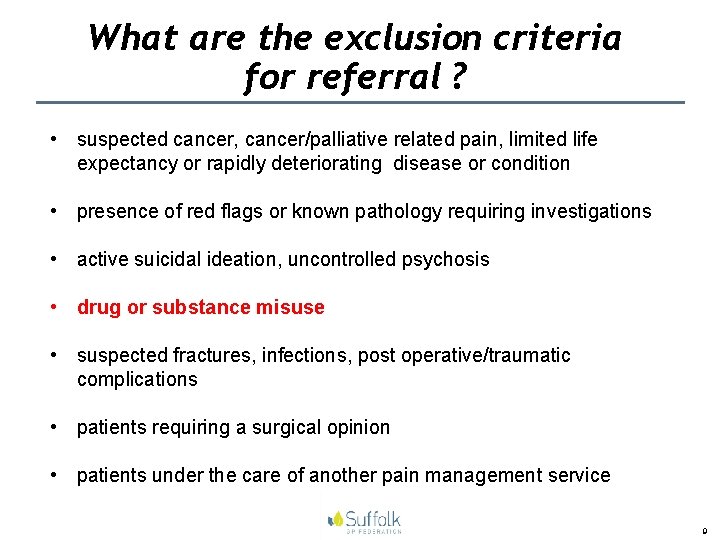
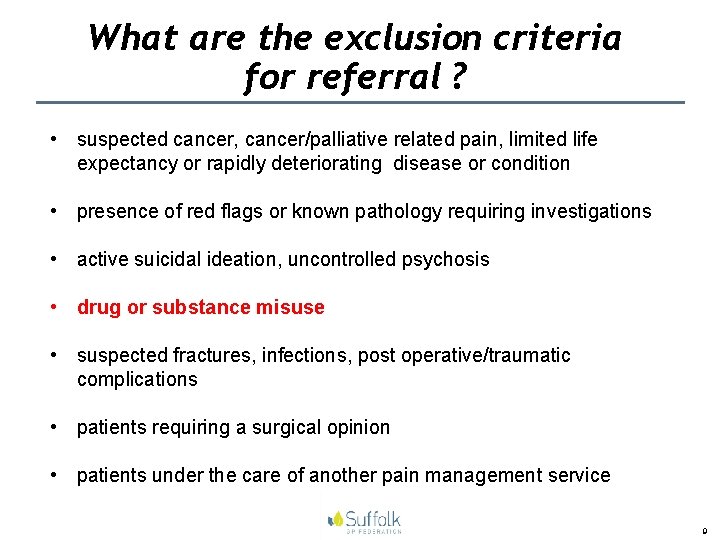
What are the exclusion criteria for referral ? • suspected cancer, cancer/palliative related pain, limited life expectancy or rapidly deteriorating disease or condition • presence of red flags or known pathology requiring investigations • active suicidal ideation, uncontrolled psychosis • drug or substance misuse • suspected fractures, infections, post operative/traumatic complications • patients requiring a surgical opinion • patients under the care of another pain management service 9

Who should I refer? Clinical - high service users - high pain intensity despite maximum analgesia - polypharmacy, opioid-polypharmacy - misuse of prescribed pain medication - abuse of prescribed pain medication Emotional - difficulties with: acceptance of diagnosis / lack of diagnosis or living with persistent pain - distress - depression - anxiety, catastrophisation Cognitive - unhelpful illness and treatment beliefs - lack of understanding of: why persistent pain does not go away treatment options self management strategies Physical and Social - difficulties with fear of movement undertaking normal activities - inability to work or fallen out of employment - difficulty with family relationships 10
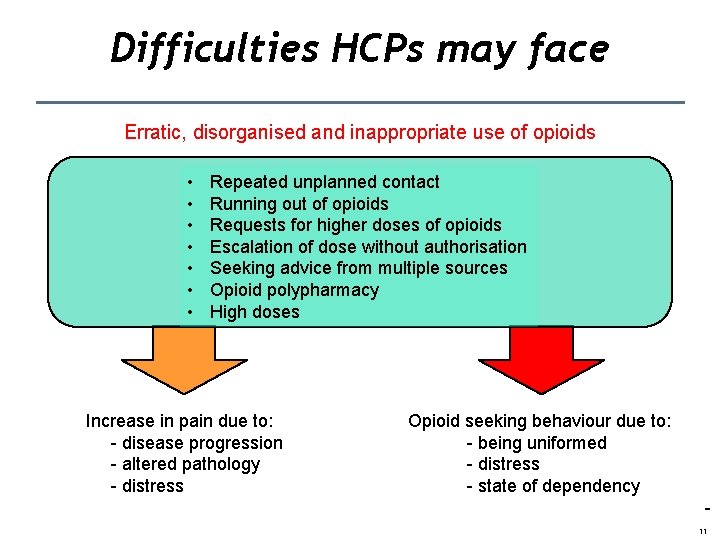
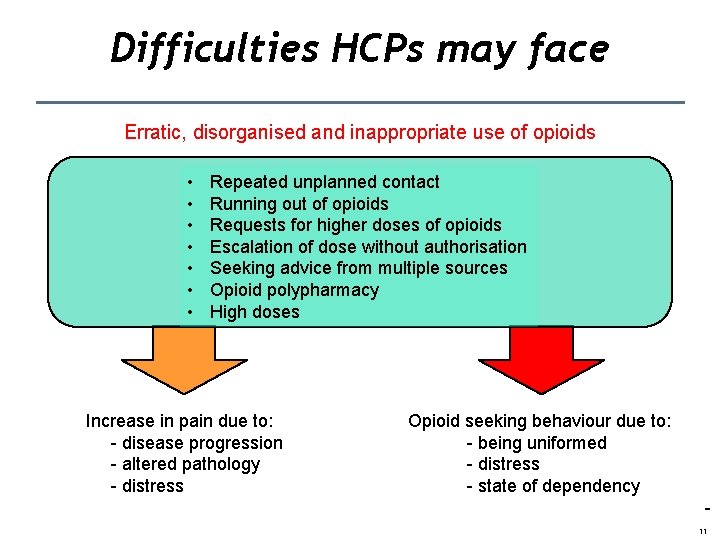
Difficulties HCPs may face Erratic, disorganised and inappropriate use of opioids • • Repeated unplanned contact Running out of opioids Requests for higher doses of opioids Escalation of dose without authorisation Seeking advice from multiple sources Opioid polypharmacy High doses Increase in pain due to: - disease progression - altered pathology - distress Opioid seeking behaviour due to: - being uniformed - distress - state of dependency 11
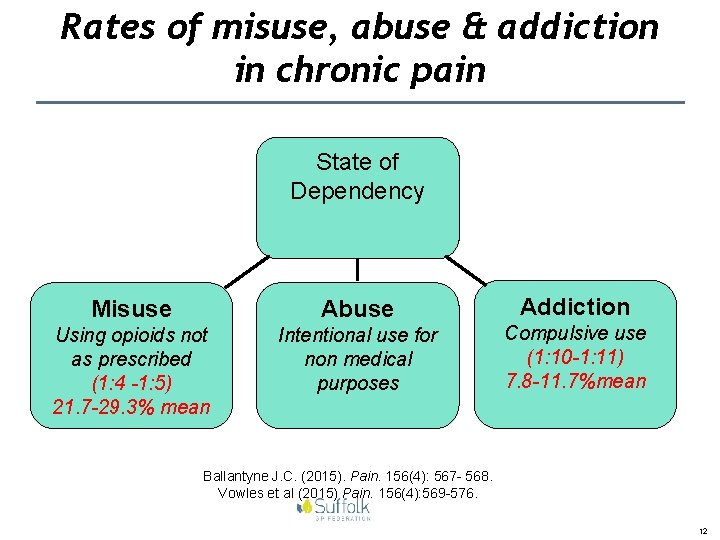
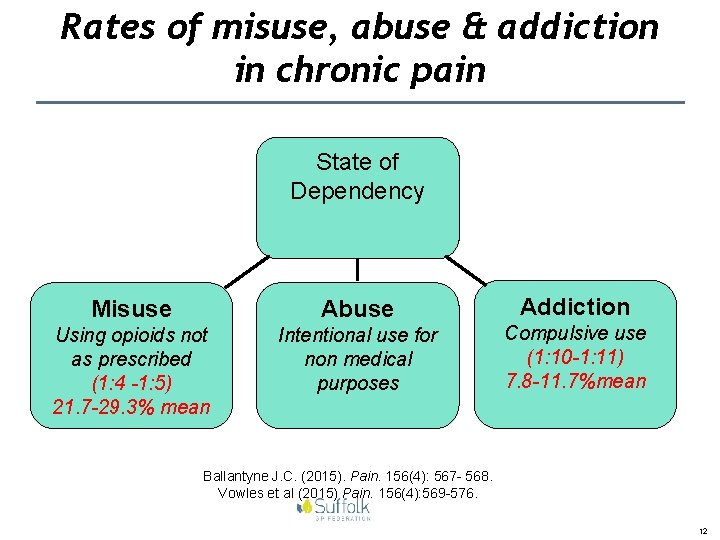
Rates of misuse, abuse & addiction in chronic pain State of Dependency Misuse Abuse Using opioids not as prescribed (1: 4 -1: 5) 21. 7 -29. 3% mean Intentional use for non medical purposes Addiction Compulsive use (1: 10 -1: 11) 7. 8 -11. 7%mean Ballantyne J. C. (2015). Pain. 156(4): 567 - 568. Vowles et al (2015) Pain. 156(4): 569 -576. 12
2015 Reports Conclusion • The use of prescription and OTC painkillers is on the increase. This is accompanied by rising mortality and inaugural data suggesting recreational use of these medicines. • With an ageing population, prescribing for pain is likely to increase further. • Evidence suggests that the cohort of those experiencing OPD is very different from the cohort traditionally using drug treatment services and new services need to be developed to cater for their needs. • Establishing services within GP surgeries would be a positive step forward. https: //painkilleraddictioninformationnetwork. files. wordpress. com/2015/09/opioid_painkiller_dependency_final_report_sept_201. pdf 13
Reports 2015 http: //idhdp. com/media/401215/bma. pdf 14 14

15
Opioid Prescribing Resource: OPIOIDS AWARE (Knaggs 2015) What is it? • On-line prescribing resource hosted by FPM • Evidence-based resource reviewing the harms and benefits of opioids What it is NOT? • Guidance • A manual about how to prescribe opioids safely • Prescribers can use to make an informed clinical decision for an individual patient, influenced by the individual's clinical • Re-statement of information from other sources presentation, comorbidities and circumstances • Extensive links to other sources 16
Who is OPIOIDS AWARE for? (Knaggs 2015) • Anyone involved in recommendation, prescribing, administration, dispensing of opioids • Different uses – Pain medicine specialist – GP – Community pharmacist – Nurses and other HCPs – Patients 17
Opioid prescribing resource: stakeholders (Knaggs 2015) • BNF • BPS • CQC • Department of Health • FPMRCo. A • MHRA • NICE • NHS England • Public Health England • RCGP • RCN • RCPsych • RPS • Service users 18

OPIOIDS AWARE: A resource for patients and prescribers (Knaggs 2015) Assess the patient condition and context Apply best professional practice Understanding the clinical use of the drug Information for patients 19
Main messages 20
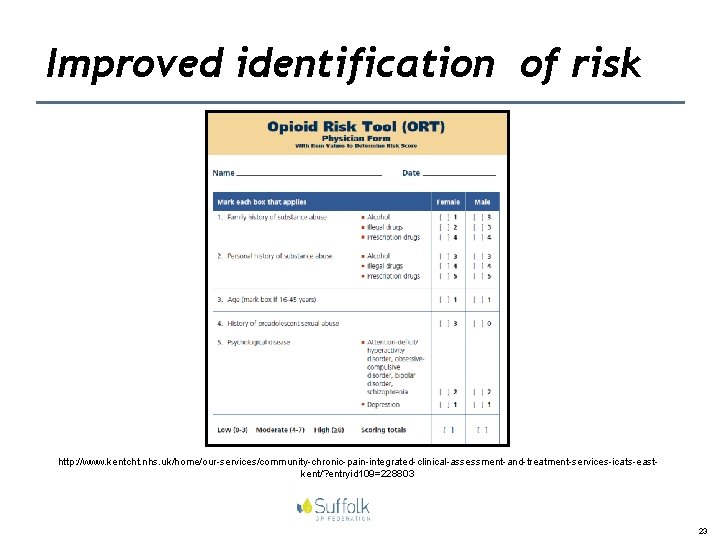
Other safety initiatives Educational • Principles of safe opioid prescribing Clinical • Prescribing audits to identify patients with elevated risk status • Use of risk assessment tools for risk stratification • Prescribing review appointments • Standardised patient information, consent & agreement • Local treatment pathways including specialised clinics 21
Opioid safety workshops 22
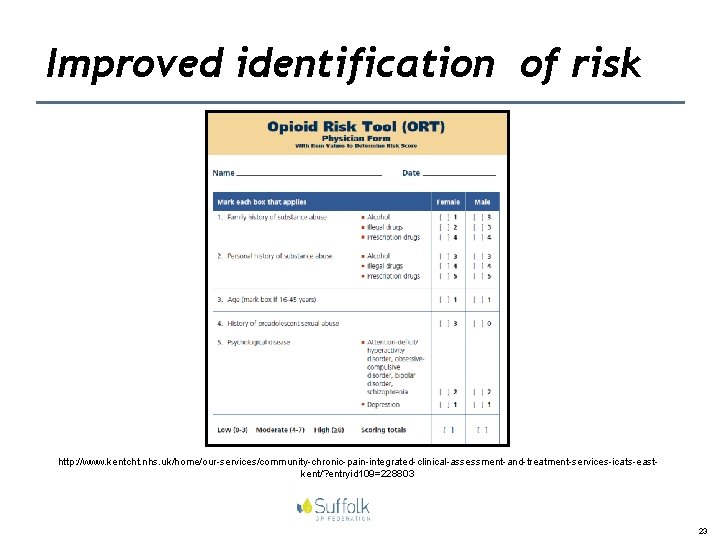
Improved identification of risk http: //www. kentcht. nhs. uk/home/our-services/community-chronic-pain-integrated-clinical-assessment-and-treatment-services-icats-eastkent/? entryid 109=228803 23
Consent and Agreement 24
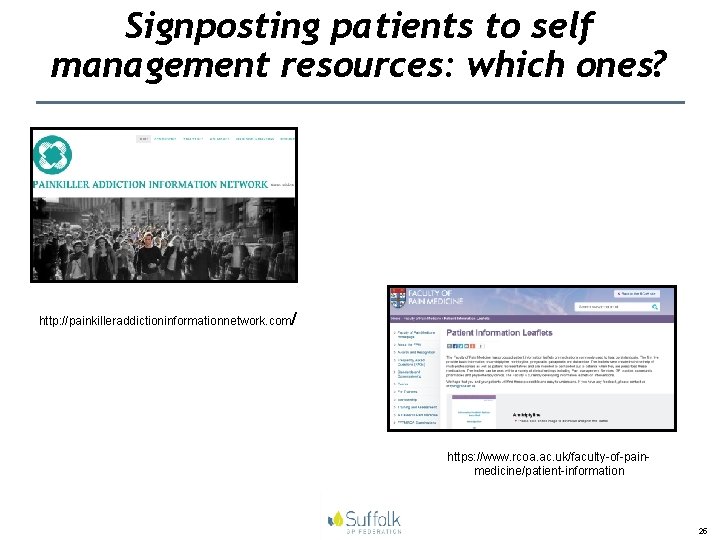
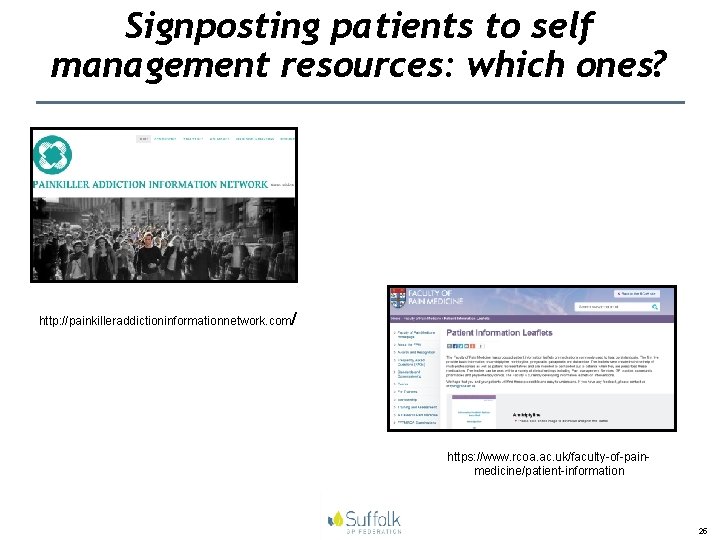
Signposting patients to self management resources: which ones? http: //painkilleraddictioninformationnetwork. com/ https: //www. rcoa. ac. uk/faculty-of-painmedicine/patient-information 25
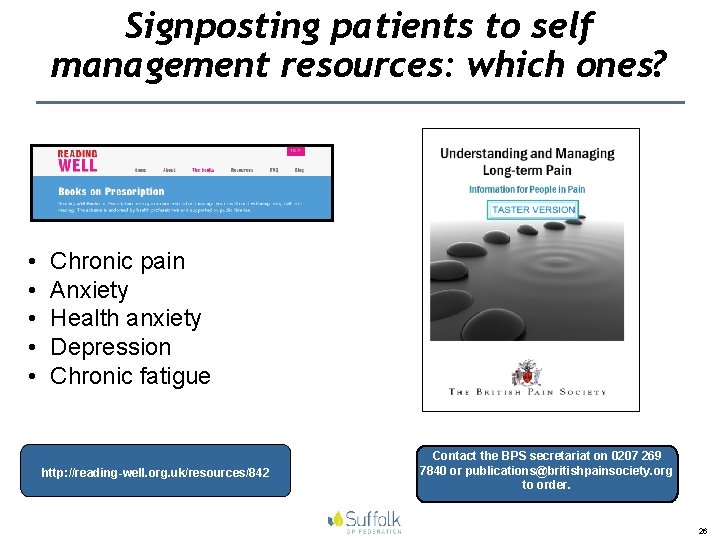
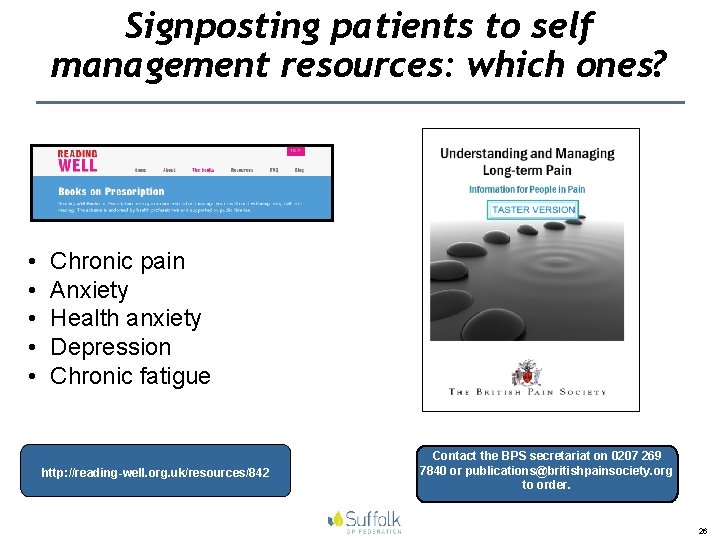
Signposting patients to self management resources: which ones? • • • Chronic pain Anxiety Health anxiety Depression Chronic fatigue http: //reading-well. org. uk/resources/842 Contact the BPS secretariat on 0207 269 7840 or publications@britishpainsociety. org to order. 26
Signposting patients to self management resources: which ones? ü Tool 1 - Accept that you have persistent pain…. and then begin to move on ü Tool 2 - Get involved -building a support team ü Tool 3 - Pacing ü Tool 4 - Learn to prioritise and plan out your days ü Tool 5 - Setting Goals/Action Plans ü Tool 6 - Being patient with yourself ü Tool 7 - Learn relaxation skills ü Tool 8 - Stretching & Exercise ü Tool 9 - Keep a diary and track your progress ü Tool 10 - Have a set-back plan ü Tool 11 - Team Work ü Tool 12 - is keeping it up…putting into daily practice the tools from 1 -11. www. paintoolkit. org 27

CPD resources in opioid management for HCPs • WSCPMS group medication clinic • WSH opioid clinic • N and N opioid clinic • Pharmacists with a special interest in improving safety in opioid management in chronic pain • British Pain Society study days • RCGP fact sheets and e-learning joint project 28
Are there any on line CPD resources in pain management for HCPs? • e-learning for pain management http: //portal. e-lfh. org. uk • Cardiff Pain Community Centre http: //www. paincommunitycentre. org/ • University of Edinburgh: CPD courses in pain management http: //www. ed. ac. uk/schools-departments/clinical-sciences/pain- management/opportunities/cpd 29
Are there local CPD resources? West Suffolk NHS Foundation Trust Library: • library@wsufftrust. org. uk • 01284 713112 or 01284 713113 Study days • pain and the older person Workshops • pain assessment and the older person • understanding pharmacological options for acute and chronic pain (to include neuropathic pain) • non pharmacological strategies in pain management • Safe opioid prescribing 30
Summary Do you have a better awareness of : üWest Suffolk Community Pain Service üOpioids Aware – the new on line resource üInitiatives to improve benefits and reduce risk of chronic opioid therapy üPatient resources for signposting üCPD resources relating to pain management 31
Questions…. discussion • What challenges do you see in clinical practice? • What changes are needed (educational, training, organisational/structural and policy) to improve the identification and management of patients affected by involuntary dependence to prescribed opioids? • What changes are needed (educational, training, organisational/ structural and policy to promote best prescribing practice including nonpharmacological strategies? • Any interest in a representative to sit on West Suffolk Educational Pain Network? (if this group becomes established) 32
Recommended reading (1) Akbik H. et al. (2006). Validation and clinical application of the Screener and Opioid Assessment for Patients with Pain (SOAPP). J Pain Symptom Manage. 32 (3): 287 -293. Anderson E. and Burris S. (2010). Opioid treatment agreements are the answer. What is the question? The American Journal of Bioethics. 10(11): 15 -17. Argoff C. E. et al. (2014). Preventing and managing aberrant drug related behaviour in primary care: Systematic review of outcomes evidence. Journal of Opioid Management. 2 (10): 119 -134. Belgrade M. J. et al. (2006). The DIRE Score: Predicting outcomes of opioid prescribing for chronic pain. Journal of Pain. 7(9): 671 -681. Butler S. F. et al. (2007). Development and validation of the Current Opioid Misuse Measure. Pain. 130 (1 -2): 144 -156. Cheatle M. D. and Savage S. R. (2012). Informed consent in opioid therapy: a potential obligation and opportunity. Journal of Pain and Symptom Control. 44(1): 105 -116. Fishman S. M et al. (2010). The opioid treatment agreement: a real world perspective. The American Journal of Bioethics. 10(11): 14 -15. Franklin G. M. (2014). Opioids for chronic non cancer pain. A position paper of the American Academy of Neurology. 83: 1277 -1284. . 33
Recommended reading (1) Godlee F. (2015). New rules of consent: the patient decides. British Medical Journal. 350: h 1534. Hegmann K. T. et al. (2014). ACOEM Practice Guidelines: Opioids for treatment of acute, subacute, chronic and postoperative pain. Journal of Occupational and Environmental Medicine. 56(12) e 143 -e 159. Jamison R. N. (2010). Substance misuse treatment for high – risk chronic pain patients on opioid therapy: a randomised trial. Pain. 150, : 390 -400. Passik S. D. et al. (2004). A new tool to assess and document pain outcomes in chronic pain patients receiving opioid therapy. Clin Ther. 26 (4): 552 -561. Payne R. et al. (2010). A rose by any other name: pain contracts/ agreements. The American Journal of Bioethics. 10(11): 5 -12. Penko J. et al. (2012). Do patients know they are on pain medication agreements? Results from a sample of high risk patients on chronic opioid therapy. Pain Medicine. 13: 1174 -1180. Rowe W. (2010). Pain treatment agreements. The American Journal of Bioethics. 10(11): 3 -4. Savage S. (2010). The patient-centred opioid treatment agreement. The American Journal of Bioethics. 10(11): 18 -19. Starrels J. et al. (2014). It made my life a little easier: primary care providers’ beliefs and attitudes about opioid treatment agreements. Journal of Opioid Management. 10(2): 95 -102 34
Recommended reading(2) Ballantyne, J. C. (2015). Opioid therapy in chronic pain. Physical Medicine and Rehabilitation Clinics. 26(1). Article in Press. Published online: http: //dx. doi. org/10. 1016/j. pmr. 2014. 12. 001 Ballantyne J. C. (2015). Assessing the prevalence of opioid misuse, abuse, and addiction in chronic pain. Pain. 156(4): 567 - 568. Chou R. et al. (2014). The Effectiveness and Risks of Long-Term Opioid Treatment of Chronic Pain. Evidence report/technology assessment no. 218. (Prepared by the Pacific Northwest Evidence-based Practice Centre under contract no. 290 -2012 -00014 -I). AHRQ publication no. 14 -E 005 -EF. Rockville, MD: Agency for Healthcare Research and Quality; 2014. Accessed at: www. effectivehealthcare. ahrq. gov/ehc/products/557/1971/chronic-pain-opioid-treatment-report 141007. pdf on 3 rd March 2015. Chou R. et al. (2015). The Effectiveness and Risks of Long-Term Opioid Therapy for Chronic Pain: A Systematic Review for a National Institutes of Health Pathways to Prevention Workshop. Annals of Internal Medicine. 162(4): 276 -286. Gourlay D. L. et al. (2005). Universal precautions in pain medicine: A rational approach to the treatment of chronic pain. Pain Medicine. 6(2): 107 -112. IASP. (2008). Screening for opioid abuse potential. Pain Clinical Updates. XVI: 7. Accessed at: http: //iasp. files. cmsplus. com/Content. Folders/Publications 2/Pain. Clinical. Updates/Archives/December 2008_XVI 7_1390262104180_1. pdf. on 3 rd March 2015. . 35
Recommended reading (2) Jeynes L. C. et al. (2012). Reducing the risk, improving the benefit: an opioid pathway for patients on long term opioids for chronic non-malignant pain. Pain News. 10(4): 225 -228. Nuckols T. K. et al. (2014). Opioid prescribing: a systematic review and critical appraisal of guidelines for chronic pain. Annals of Internal Medicine. 160(1): 38 -47. Smith H. S. and Fine P. G. (2014). Oxford American Pocket Notes: Opioid Risk Management–Tools and Tips. (2 nd ed) Oxford: University Press. Starrels J. et al. (2010). Systematic review: treatment agreements and urine drug testing to reduce opioid misuse in patients with chronic pain. Annals of Internal Medicine. 152(11): 712 -720. Waters C. and Riggs H. (2012). A pathway for chronic opioid therapy-users’ experiences. Pain News. 10(4): 229 -231 36
 Suffolk eu alliance
Suffolk eu alliance Logisticare suffolk county
Logisticare suffolk county Mad pain
Mad pain Period or pregnant
Period or pregnant Early pregnancy symptoms cramps
Early pregnancy symptoms cramps Ann coyne suffolk university
Ann coyne suffolk university Ovelhas suffolk espanha
Ovelhas suffolk espanha Lisa chandler east suffolk
Lisa chandler east suffolk Suffolk county council hr
Suffolk county council hr Substance
Substance Strategic planning process suffolk
Strategic planning process suffolk Domba suffolk indonesia
Domba suffolk indonesia Bawdsey manor pgl
Bawdsey manor pgl Suffolk eu alliance
Suffolk eu alliance Interactive touch screen presentation software
Interactive touch screen presentation software Suffolk coastal local plan
Suffolk coastal local plan Ctse suffolk
Ctse suffolk Suffolk region pta
Suffolk region pta Horizontal movement of air
Horizontal movement of air What creates wind
What creates wind Kaart met noord oost zuid west
Kaart met noord oost zuid west East is east and west is west
East is east and west is west Old west vs new west
Old west vs new west Bury integrated pain service
Bury integrated pain service Bury integrated pain service
Bury integrated pain service West african community council kent
West african community council kent What are headwaters
What are headwaters Waters of millan
Waters of millan Olfactory groove keros classification
Olfactory groove keros classification Waters of gold
Waters of gold Esther earl
Esther earl Sphenoid strut
Sphenoid strut Saber preterite vs imperfect meaning
Saber preterite vs imperfect meaning The calm waters metaphor
The calm waters metaphor William wordsworth london
William wordsworth london Devilfish in egyptian waters
Devilfish in egyptian waters Waters en pasado participio
Waters en pasado participio