Welcome To Third Party EMed NY Training Third

- Slides: 55

Welcome To: Third Party & EMed. NY Training
Third Party Liability & e. Med. NY
Third Party Liability Any individual, entity or program that is, or may be, liable to pay all or part of the expenditures for medical services furnished under the State plan
Various Types of TPL Medicare Coverage Employer Related Insurance Union Benefits Private Insurance Coverage Absent Parent
Various Types of TPL (cont’d) Tri. Care for Life Accident, including No-Fault Assignable Income Protection Policies Fraternal/Benefit Societies and Churches Student Health Insurance Workers’ Compensation
Purpose Maximizing the use of third party insurance saves money Insurance benefits that pay the cost of medical care and services reduces Medicaid expenditures
Payor of Last Resort Third party insurance must be applied first toward the cost of medical care/services Balance may then be billed to Medicaid
Exceptions to Payor of Last Resort Individuals covered by Children with Physical Disabilities Program Individuals covered by Crime Victims Compensation Program MA becomes payor of first resort after any other available TPHI have been applied
Condition of Eligibility Must pursue potential third party benefits Failure to comply could result in a denial or discontinue of MA coverage
MA Policy Treatment of TPLs depends on: Type of insurance If there is a premium cost to A/R If A/R is fully eligible for MA
Employer Provided Group Health Insurance NO cost to the A/R is allowed 30 days to enroll at first available open enrollment Once enrolled, must utilize available benefits
Employer Provided Group Health Insurance (cont’d) COST to the A/R supplies the LDSS with premium cost and coverage package LDSS makes a cost effectiveness determination If not cost effective, A/R is not required to enroll or maintain enrollment in health plan
Employer Provided Group Health Insurance (cont’d) COST to the A/R (cont’d) If policy is cost effective, A/R is required to enroll or maintain enrollment in the health plan LDSS will pay the cost of the premiums
Failure to Comply If A/R fails to comply with request to enroll w/in 30 days of the first available enrollment, they are denied or discontinued MA Only the employed individual is ineligible until compliance
Privately Purchased Health Insurance If privately purchased health insurance is in force at time of application, LDSS will do a cost effectiveness determination If not cost effective, applicant is not required to continue coverage If cost effective, LDSS offers to pay health insurance premiums
Medicare Individuals who are eligible for Medicaid must enroll in Part B Enrollment is a condition of eligibility Individuals who are enrolled in Part A and/or B should utilize benefits Individuals who are dual eligible must enroll in Medicare Part D
Medicare LDSS must make a determination for the Medicare Savings Program
General “Good Cause” Provision A/Rs are required to cooperate with IV-D in obtaining TPHI and medical payments for themselves and dependents LDSS is required to inform A/Rs of their right to claim “Good Cause”
“Good Cause” Physical and/or emotional harm to the child or parent/caretaker relative with whom the child is residing
What is Considered “Good Cause” Child conceived as a result of rape or incest, or; Legal proceeding is pending before court for adoption, or; Ongoing assistance by an authorized agency with decision to either parent the child or place for adoption Duration of discussion is less than 3 months
“Good Cause” FPBP Individuals Under Age 21 Worker needs an affirmative statement that third party insurance is available If no affirmative statement is provided, do not pursue third party insurance
“Good Cause” FPBP Individuals Age 21 and Over If the Individual has third party insurance they may request “good cause” not to bill the third party insurance Follow same guidelines for other good cause claims If accepted, do not pursue TPHI
Provider Requested “Good Cause” If patients want services kept confidential, providers may request good cause on their behalf if: Billing is for services related to reproductive health, family planning or pregnancy related Patient states billing for such services jeopardizes their safety or confidentiality
Provider Requested “Good Cause” If MEVS indicates TPHI, Provider must contact SDOH and ask for a determination of “good cause” If granted, provider zero fills claim form in order to bypass third party insurance and bill MA directly. Provider must also document in the patient’s billing record the date of the call and that “good cause” was granted by SDOH.
Good Cause Indicator A “good cause” indicator exists in e. Med. NY to allow Medicaid to be billed instead of third party. To enter Good Cause on e. Med. NY, enter the CIN and press ENTER. Select the TPL Good Cause tab Enter the Begin Date and the End Date (use an open end date, 12/31/99 for domestic violence situations) Hit ENTER.
Subrogation The right to substitute one creditor for another The LDSS “steps into the shoes” of the legally responsible relative
Subrogation (cont’d) Assignment is the means by which this is accomplished When an applicant signs the application, they are assigning their rights to third party insurance to the LDSS
Subrogation (cont’d) Direction of payments for services to the provider or LDSS Direction of payments to providers that do not participate in the insurance plan rather than to the recipient Requirement of Medicaid providers to seek reimbursement from liable third parties before submitting claims to the MA program
Subrogation (cont’d) • Allows LDSS to enroll dependents on the LRR’s insurance policy • When the LRR is court ordered to provide medical support
Eligibility Worker’s Role Question A/R about: Any current insurance Coverage through employer Coverage through an absent parent Other potential coverage including COBRA
Eligibility Worker’s Role (cont’d) Determine if any information is contained in the e. Med. NY file Review information for accuracy and make appropriate adjustments
Eligibility Worker’s Role (cont’d) Copy both sides of insurance card which usually includes: Name of carrier and effective dates Ask about persons and services covered by insurance
Eligibility Worker’s Role (cont’d) Document employer or Union name and address For accident victims, document date of accident, who is liable for claim, names of attorneys and status of any court action
Informing Third Party Worker completes the DSS 4198 and/or DSS 4384 Forward DSS 4198 and/or 4384 and all pertinent documentation to the Third Party Unit
TP Responsibilities (cont’d) TP worker investigates, verifies and documents the third party information Complete any missing information on DSS 4198 and/or 4384
TP Responsibilities (cont’d) Makes cost effective determination Ensures third party information is entered in e. Med. NY TP system TPL data will be maintained in a file at CSC
TP Responsibilities (cont’d) Sends copy of completed 4198 and/or 4384 back to eligibility worker for case record Generate a new DSS 4198 and/or 4384 anytime new info is received from the State, insurance company or employer
Cost Avoidance Process that ensures the cost to the MA program is avoided until all other available third parties are billed correctly
System Implications TPHI data entered into e. Med. NY Claims reviewed and matched with recipient’s third party record
System Implications (cont’d) If claim does not show it was submitted to third party for payment it will be denied Once claim has been appropriately billed to the third party provider, the remainder of the claim is submitted to CSC for payment up to the MA rate
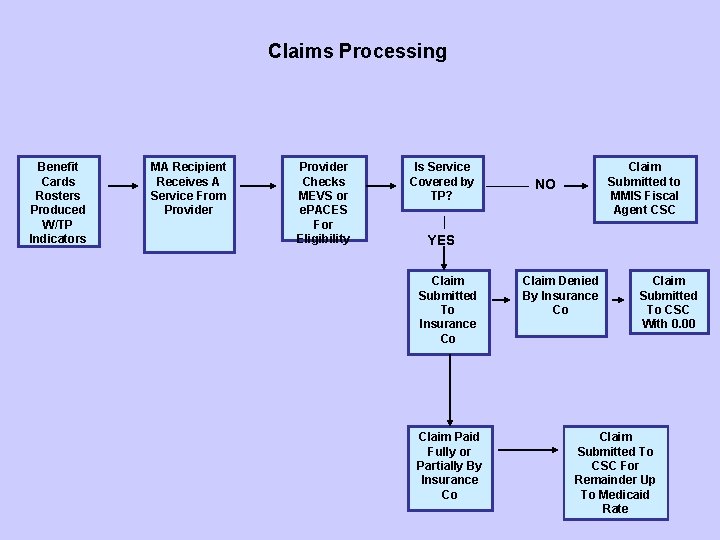
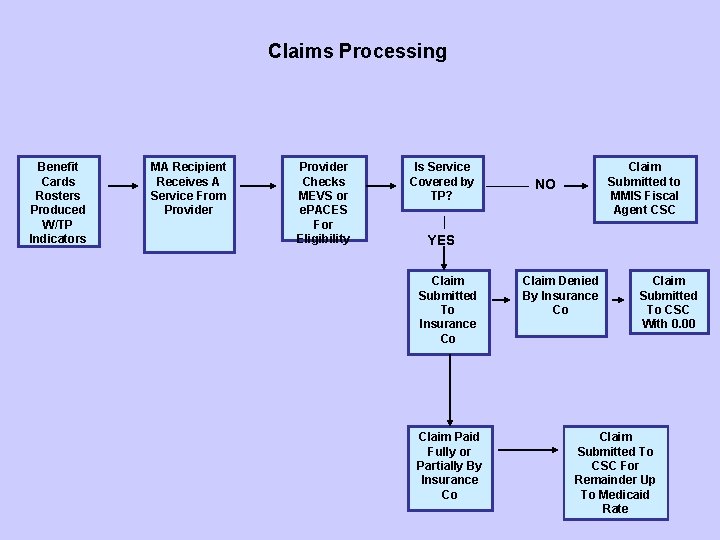
Claims Processing Benefit Cards Rosters Produced W/TP Indicators MA Recipient Receives A Service From Provider Checks MEVS or e. PACES For Eligibility Is Service Covered by TP? Claim Submitted to MMIS Fiscal Agent CSC NO YES Claim Submitted To Insurance Co Claim Paid Fully or Partially By Insurance Co Claim Denied By Insurance Co Claim Submitted To CSC With 0. 00 Claim Submitted To CSC For Remainder Up To Medicaid Rate
COBRA of 1985 Eligible individuals who have lost employer provided health insurance coverage, due to specific qualifying events, may elect to continue coverage for a period of time by paying the entire premium (group rate) Employers determine eligibility for COBRA and notify employee
OBRA of 1990 Allows states the option to pay the COBRA premium on behalf of the CCB This option was mandated by the State of New York NYS added additional requirements
MA COBRA Continuation Employer providing coverage has 75 or more employees Insurance is cost effective CCBs meet non-financial MA requirements Financial/Budgeting Implications
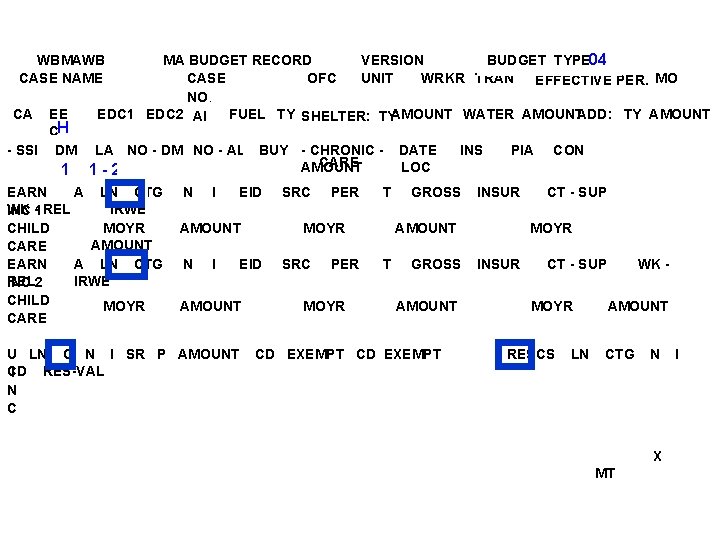
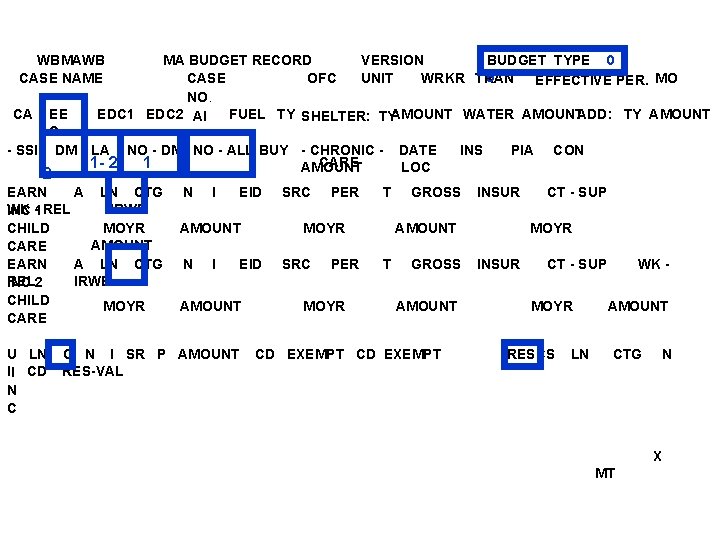
COBRA Budgeting for Adults and Children 18 -21 SSI-R budget type - 04 EEC code - H Deeming code -1 Buy-In Indicator must be Blank Living Arrangement - 1 or 2 No All – as appropriate for children under 18 in the HH Categorical Indicators as appropriate
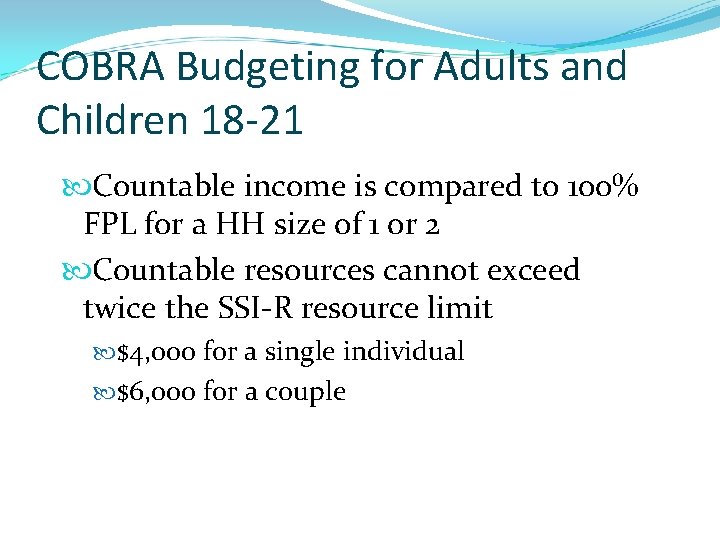
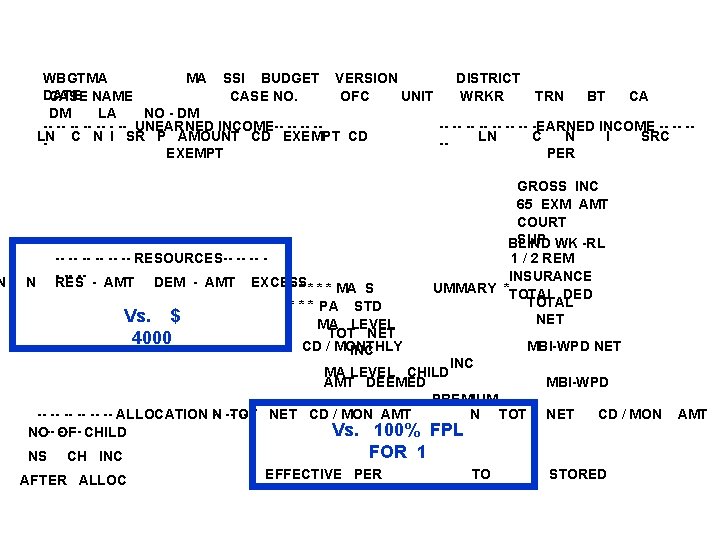
COBRA Budgeting for Adults and Children 18 -21 Countable income is compared to 100% FPL for a HH size of 1 or 2 Countable resources cannot exceed twice the SSI-R resource limit $4, 000 for a single individual $6, 000 for a couple
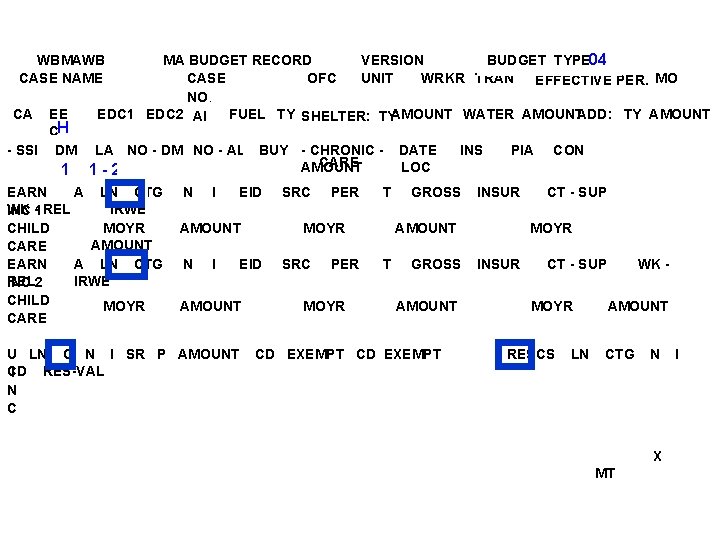
MA BUDGET RECORD VERSION BUDGET TYPE 04 CASE OFC UNIT WRKR TRAN EFFECTIVE PER. MO NO. EDC 1 EDC 2 AI FUEL TY SHELTER: TYAMOUNT WATER AMOUNTADD: TY AMOUNT WBMAWB CASE NAME CA EE CH - SSI - DM 1 LA NO - DM NO - ALL BUY - CHRONIC CARE AMOUNT 1 -2 EARN A LN CTG WK -1 REL IRWE INC CHILD MOYR AMOUNT CARE EARN A LN CTG REL 2 IRWE INC CHILD MOYR CARE N I EID AMOUNT N I U LN C N I SR P AMOUNT CD RES-VAL I N C PER T MOYR EID AMOUNT SRC PER MOYR DATE LOC INS GROSS PIA INSUR AMOUNT T GROSS AMOUNT CD EXEMPT CON CT - SUP MOYR INSUR CT - SUP MOYR RESCS LN WK AMOUNT CTG N X MT I
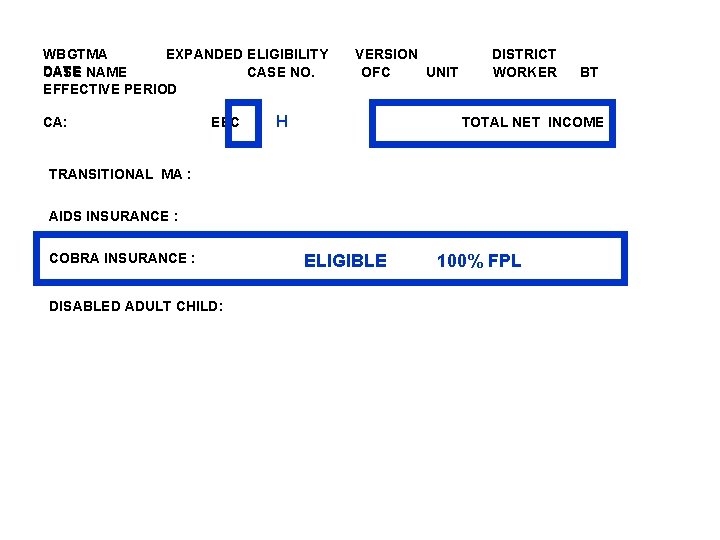
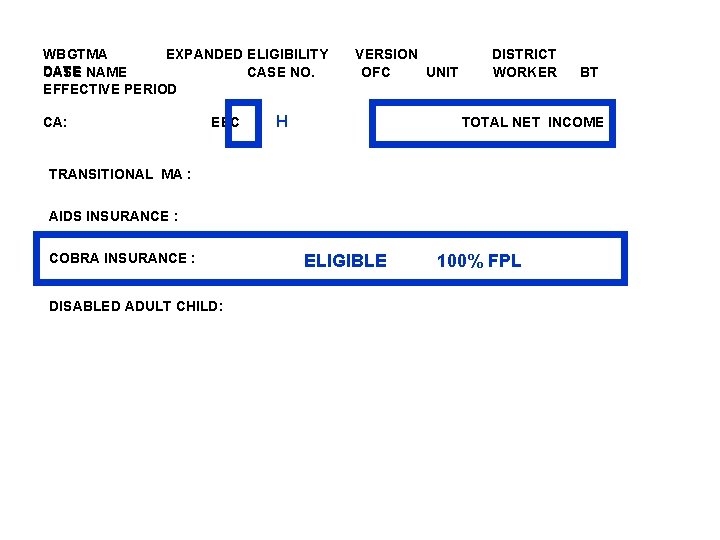
WBGTMA EXPANDED ELIGIBILITY DATE CASE NAME CASE NO. EFFECTIVE PERIOD CA: EEC VERSION OFC UNIT H DISTRICT WORKER TOTAL NET INCOME : TRANSITIONAL MA : AIDS INSURANCE : COBRA INSURANCE : DISABLED ADULT CHILD: BT ELIGIBLE 100% FPL
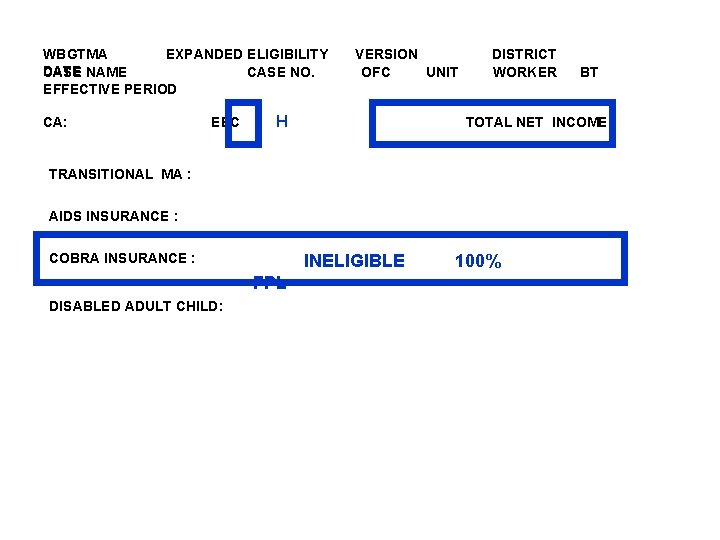
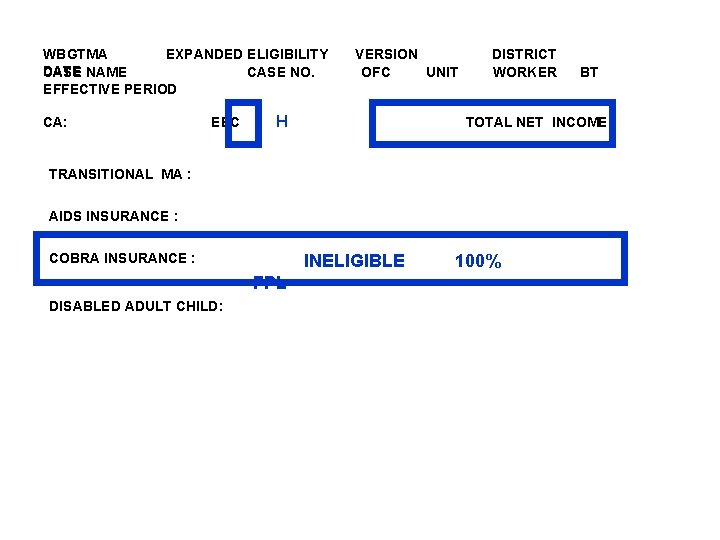
WBGTMA EXPANDED ELIGIBILITY DATE CASE NAME CASE NO. EFFECTIVE PERIOD CA: EEC VERSION OFC UNIT H DISTRICT WORKER TOTAL NET INCOME : TRANSITIONAL MA : AIDS INSURANCE : COBRA INSURANCE : INELIGIBLE FPL DISABLED ADULT CHILD: BT 100%
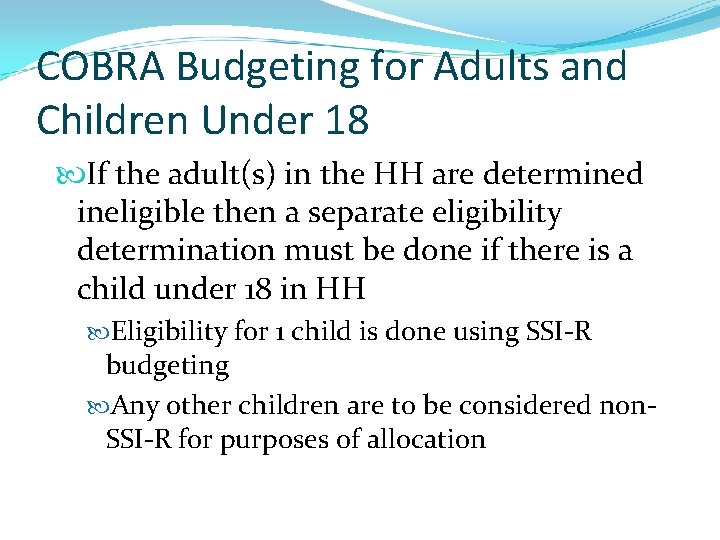
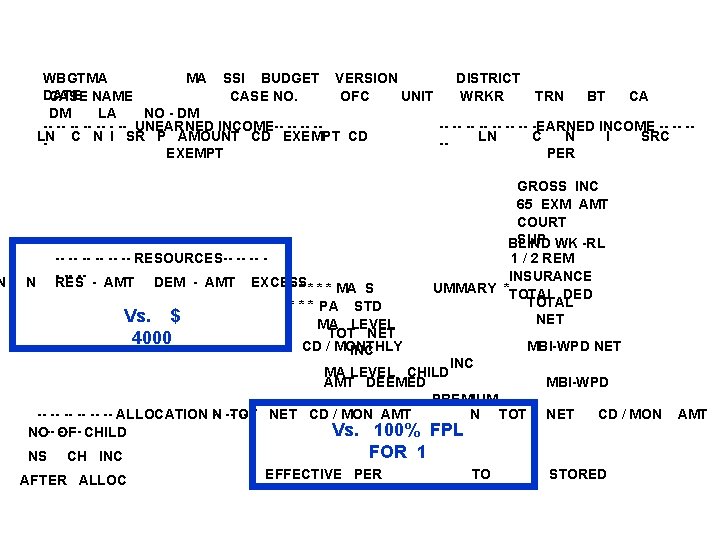
COBRA Budgeting for Adults and Children Under 18 If the adult(s) in the HH are determined ineligible then a separate eligibility determination must be done if there is a child under 18 in HH Eligibility for 1 child is done using SSI-R budgeting Any other children are to be considered non. SSI-R for purposes of allocation
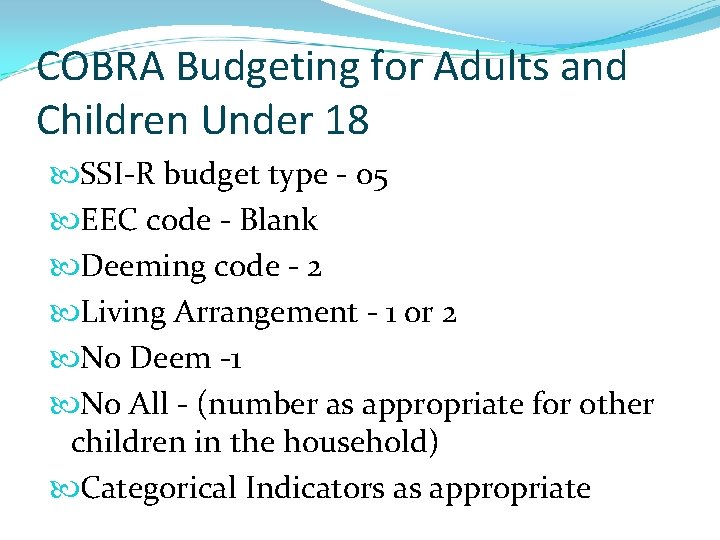
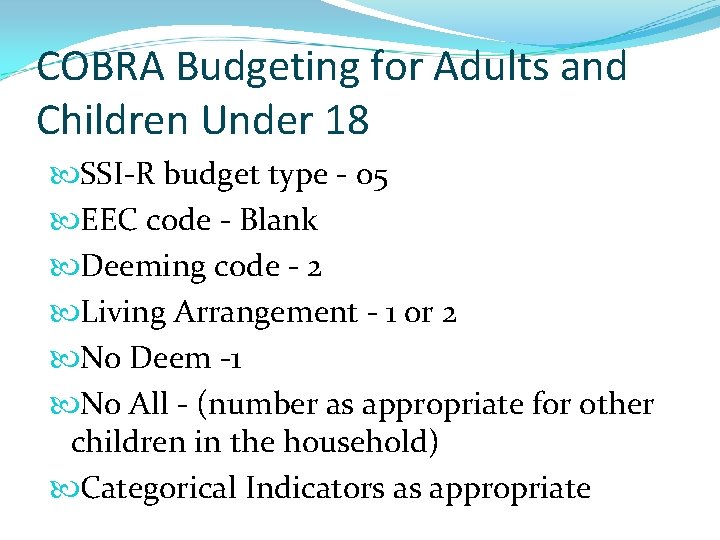
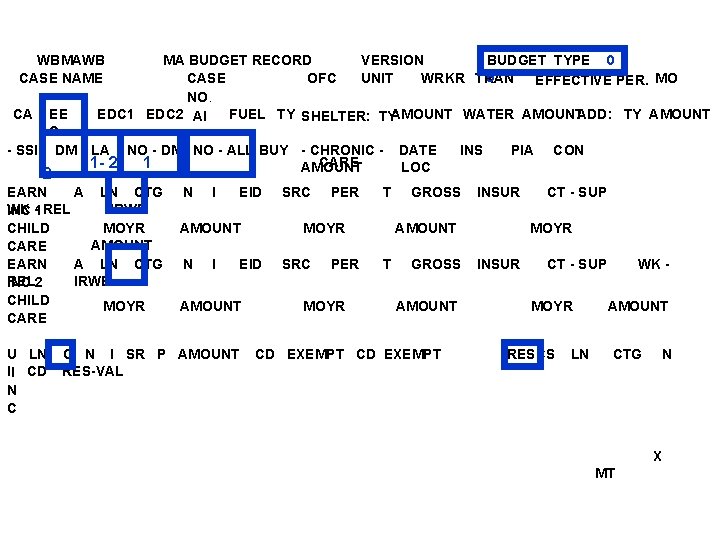
COBRA Budgeting for Adults and Children Under 18 SSI-R budget type - 05 EEC code - Blank Deeming code - 2 Living Arrangement - 1 or 2 No Deem -1 No All - (number as appropriate for other children in the household) Categorical Indicators as appropriate
WBMAWB CASE NAME CA EE C - SSI - DM 2 MA BUDGET RECORD VERSION BUDGET TYPE 0 5 CASE OFC UNIT WRKR TRAN EFFECTIVE PER. MO NO. EDC 1 EDC 2 AI FUEL TY SHELTER: TYAMOUNT WATER AMOUNTADD: TY AMOUNT LA 1 - 2 NO - DM NO - ALL BUY - CHRONIC CARE 1 AMOUNT EARN A LN CTG WK -1 REL IRWE INC CHILD MOYR AMOUNT CARE EARN A LN CTG REL 2 IRWE INC CHILD MOYR CARE U LN II CD N C N I EID AMOUNT N I C N I SR P AMOUNT RES-VAL PER T MOYR EID AMOUNT SRC PER MOYR DATE LOC INS GROSS PIA INSUR AMOUNT T GROSS AMOUNT CD EXEMPT CON CT - SUP MOYR INSUR CT - SUP MOYR RESCS LN WK AMOUNT CTG N X MT
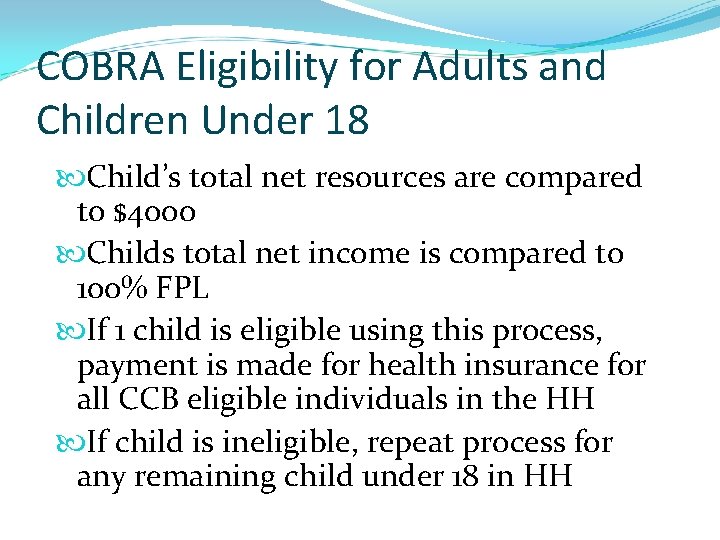
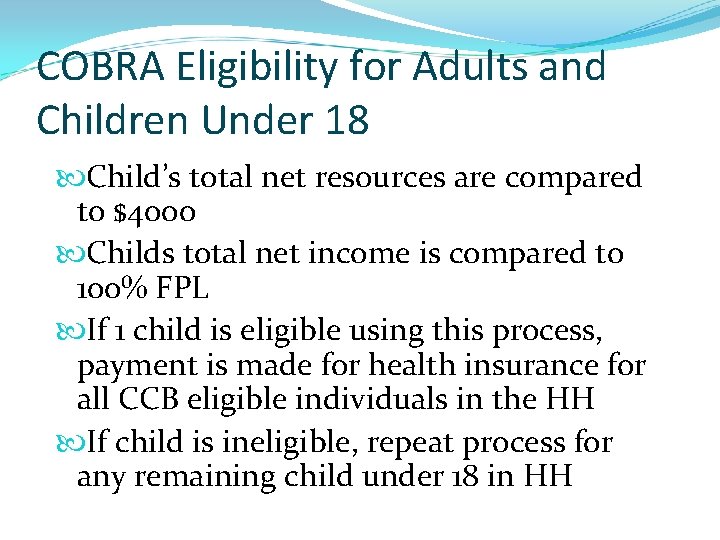
COBRA Eligibility for Adults and Children Under 18 Child’s total net resources are compared to $4000 Childs total net income is compared to 100% FPL If 1 child is eligible using this process, payment is made for health insurance for all CCB eligible individuals in the HH If child is ineligible, repeat process for any remaining child under 18 in HH
N WBGTMA MA SSI BUDGET VERSION DISTRICT DATE CASE NAME CASE NO. OFC UNIT WRKR TRN BT CA DM LA NO - DM -- -- -- UNEARNED INCOME-- -- -- -EARNED INCOME -- -- -LN C N I SR P AMOUNT CD EXEMPT CD LN C N I SRC -EXEMPT PER N -- -- -- RESOURCES-- -- -- -RES - AMT DEM - AMT EXCESS * * * MA S * * * PA STD Vs. $ MA LEVEL TOT NET 4000 CD / MONTHLY INC GROSS INC 65 EXM AMT COURT SUP WK -RL BLIND 1 / 2 REM INSURANCE UMMARY *TOTAL DED TOTAL NET MBI-WPD NET INC MA LEVEL CHILD AMT DEEMED PREMIUM N TOT -- -- -- ALLOCATION N -- --TOT -- - NET CD / MON AMT - -- OF -- -- CHILD Vs. 100% FPL NO NS CH INC AFTER ALLOC MBI-WPD NET CD / MON FOR 1 EFFECTIVE PER TO STORED AMT
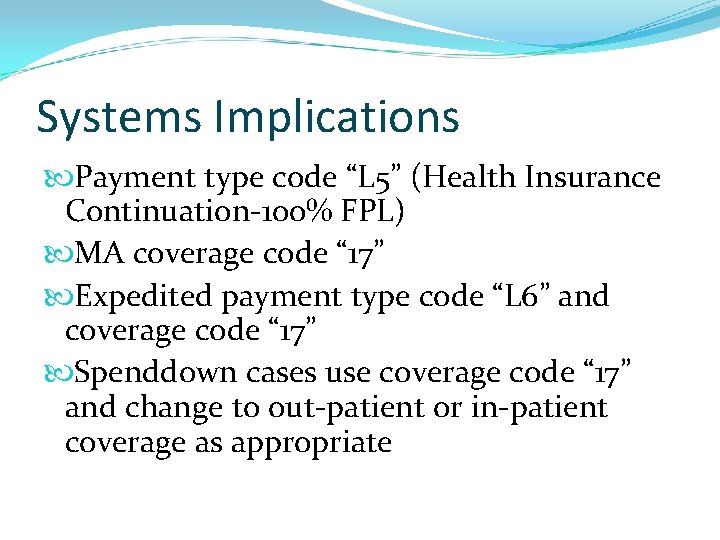
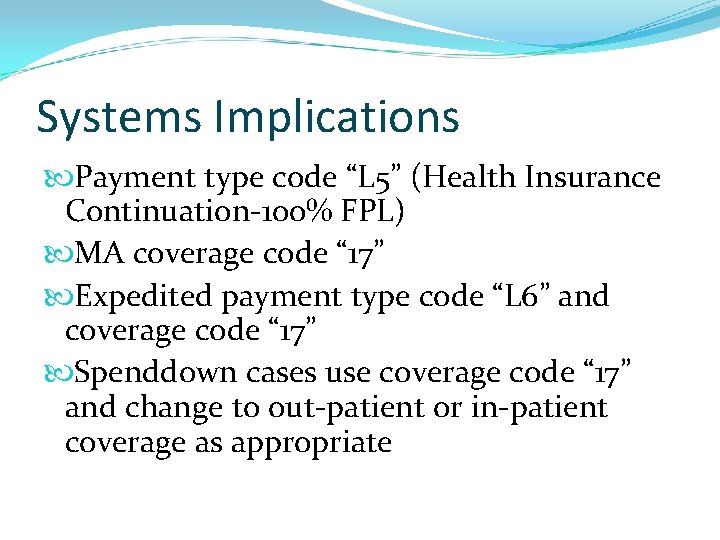
Systems Implications Payment type code “L 5” (Health Insurance Continuation-100% FPL) MA coverage code “ 17” Expedited payment type code “L 6” and coverage code “ 17” Spenddown cases use coverage code “ 17” and change to out-patient or in-patient coverage as appropriate