Welcome to the TIA Clinic Preventing stroke TPA
- Slides: 47
Welcome to the TIA Clinic
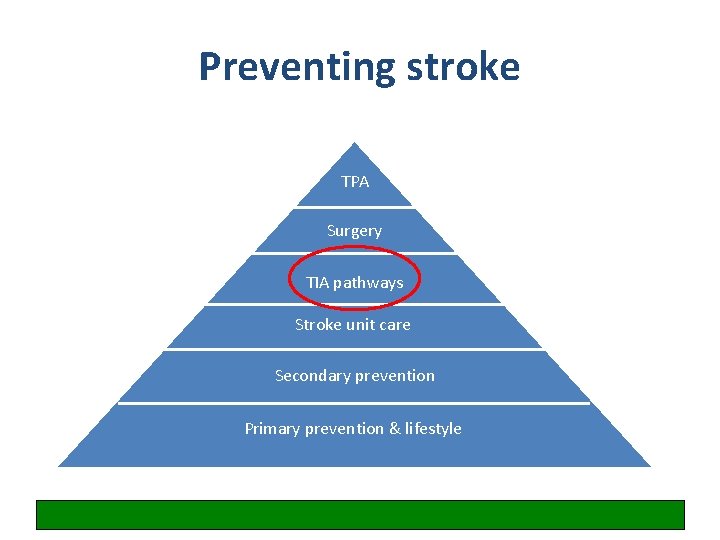
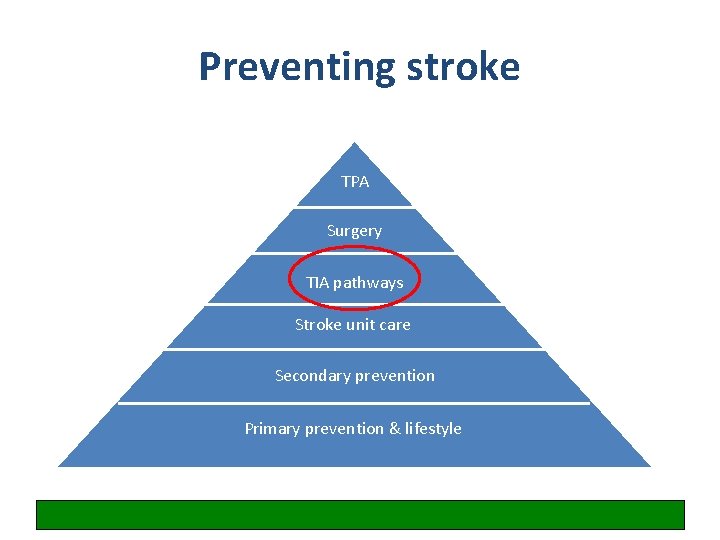
Preventing stroke TPA Surgery TIA pathways Stroke unit care Secondary prevention Primary prevention & lifestyle
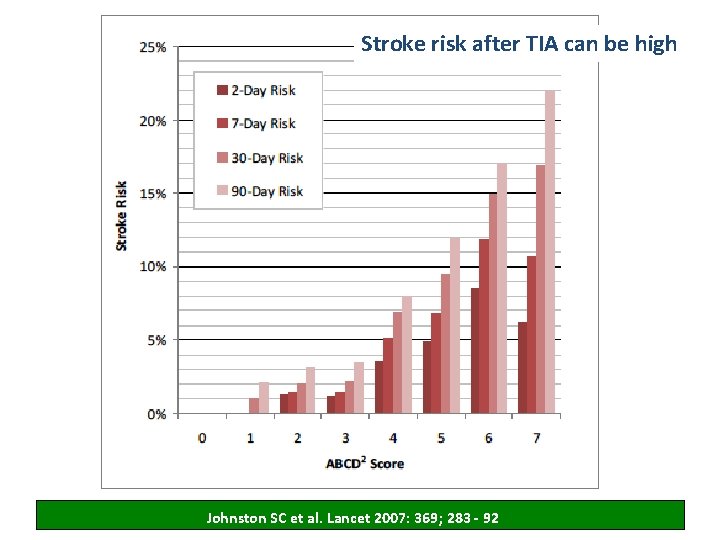
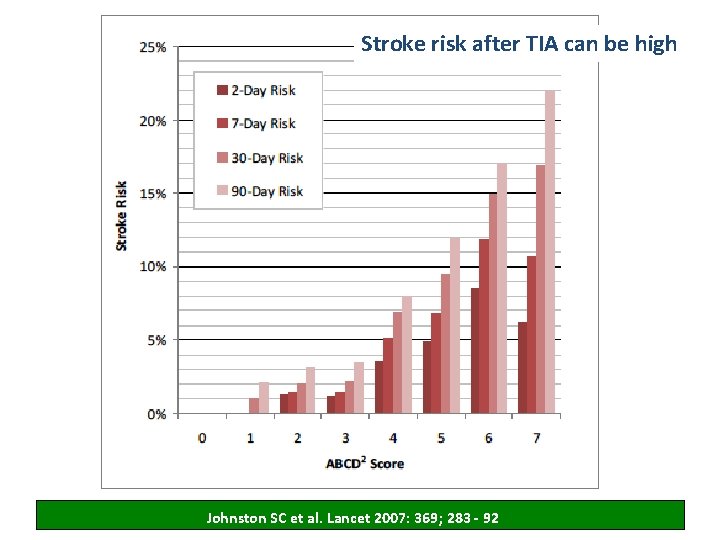
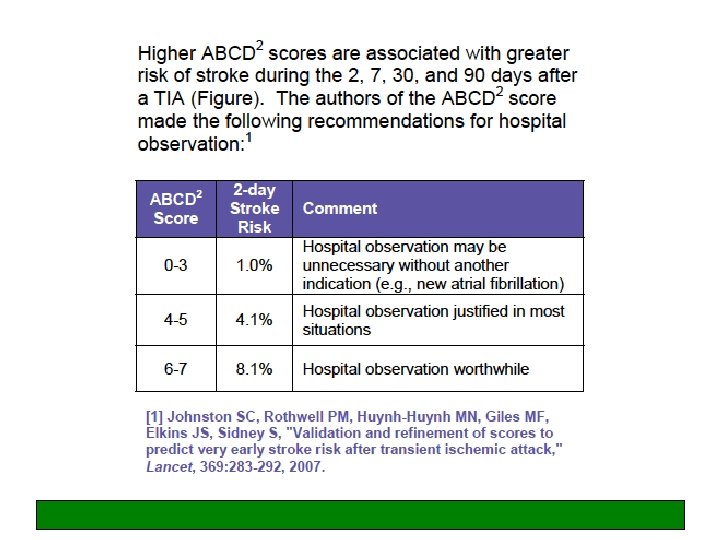
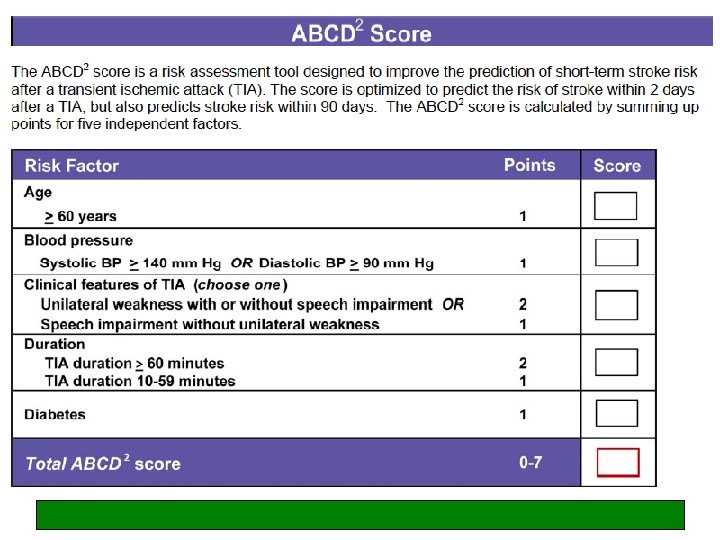
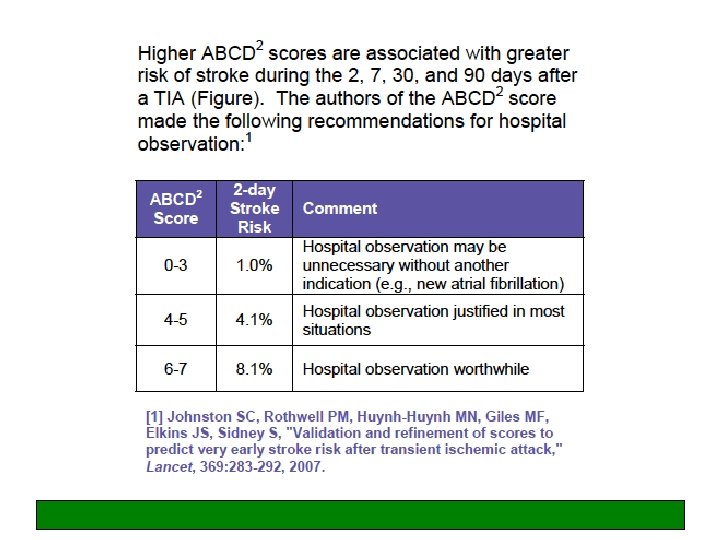
Stroke risk after TIA can be high Johnston SC et al. Lancet 2007: 369; 283 - 92
What is the definition of TIA?
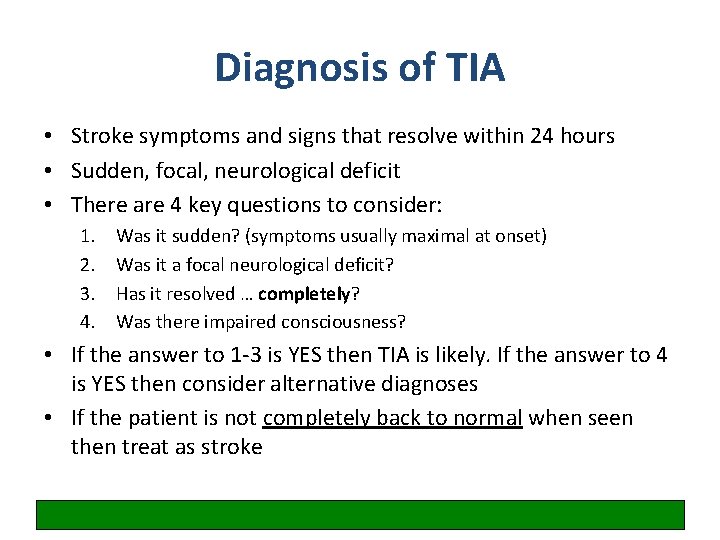
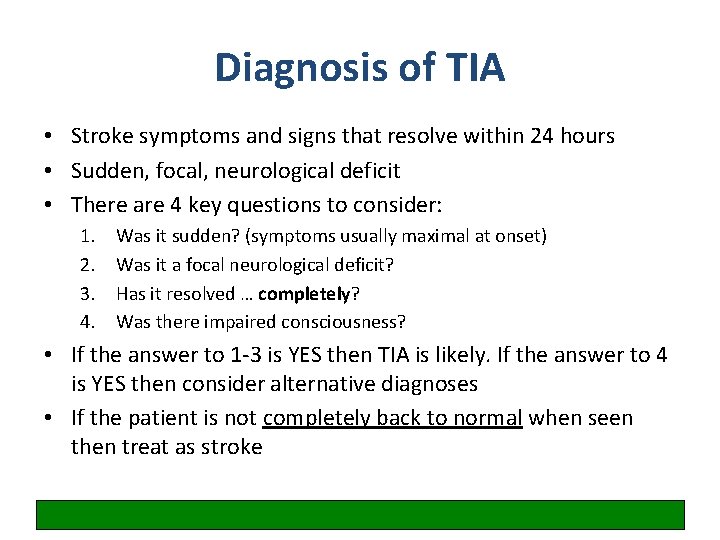
Diagnosis of TIA • Stroke symptoms and signs that resolve within 24 hours • Sudden, focal, neurological deficit • There are 4 key questions to consider: 1. 2. 3. 4. Was it sudden? (symptoms usually maximal at onset) Was it a focal neurological deficit? Has it resolved … completely? Was there impaired consciousness? • If the answer to 1 -3 is YES then TIA is likely. If the answer to 4 is YES then consider alternative diagnoses • If the patient is not completely back to normal when seen then treat as stroke
Write down the neurological symptoms people get during a TIA (most common first) and then tell me whether it is an anterior or posterior circulation symptom
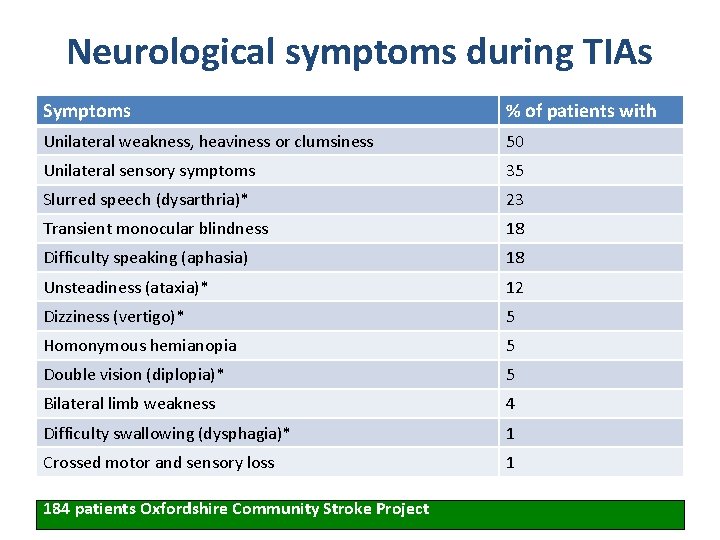
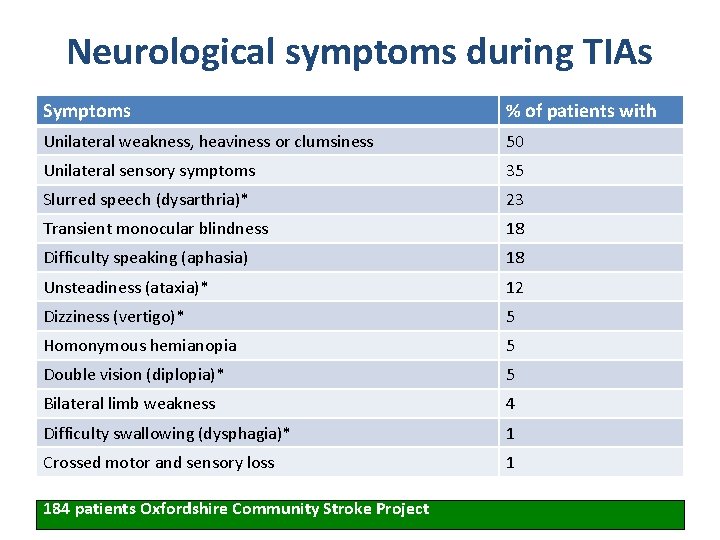
Neurological symptoms during TIAs Symptoms % of patients with Unilateral weakness, heaviness or clumsiness 50 Unilateral sensory symptoms 35 Slurred speech (dysarthria)* 23 Transient monocular blindness 18 Difficulty speaking (aphasia) 18 Unsteadiness (ataxia)* 12 Dizziness (vertigo)* 5 Homonymous hemianopia 5 Double vision (diplopia)* 5 Bilateral limb weakness 4 Difficulty swallowing (dysphagia)* 1 Crossed motor and sensory loss 1 184 patients Oxfordshire Community Stroke Project
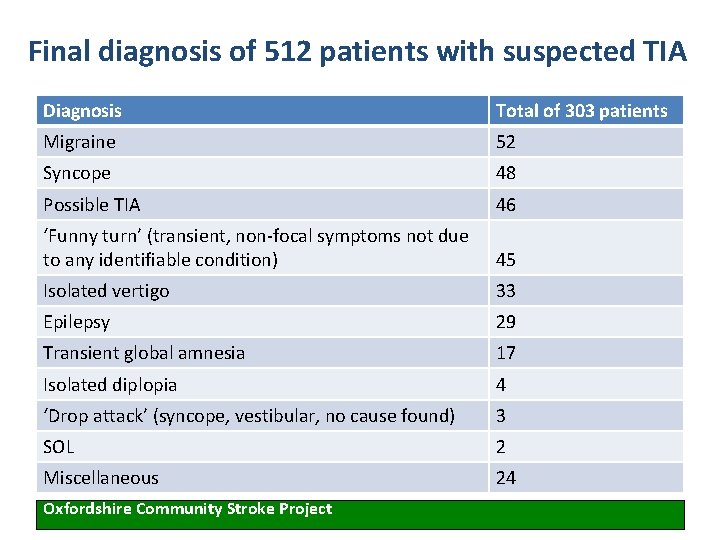
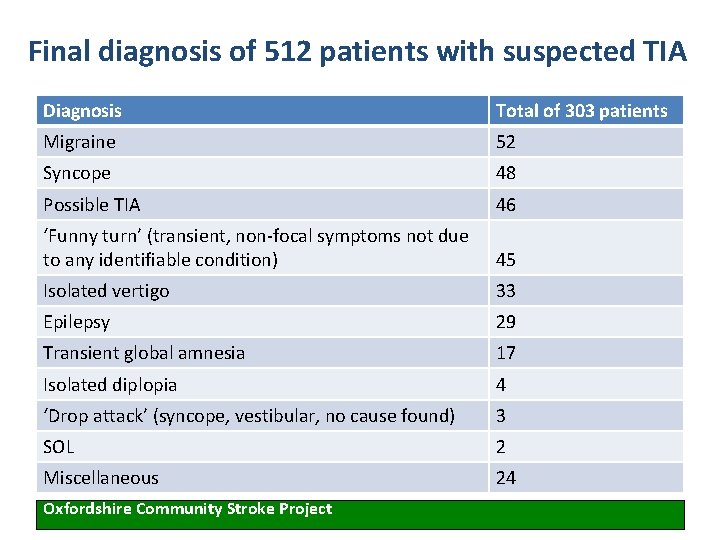
Final diagnosis of 512 patients with suspected TIA Diagnosis Total of 303 patients Migraine 52 Syncope 48 Possible TIA 46 ‘Funny turn’ (transient, non-focal symptoms not due to any identifiable condition) 45 Isolated vertigo 33 Epilepsy 29 Transient global amnesia 17 Isolated diplopia 4 ‘Drop attack’ (syncope, vestibular, no cause found) 3 SOL 2 Miscellaneous 24 Oxfordshire Community Stroke Project
Case 1 A 65 -year-old woman described being unable to speak properly for 10 minutes while she was talking to her neighbour. She said she could not find the right words and wrong words kept coming out – “like double Dutch”. PMH: hypertension, OA. Meds: bendroflumethiazide 2. 5 mg od, prn codeine. What other questions do you need to ask?
Born right handed Driver (Group 1 licence) Never smoked Not known to have diabetes or high cholesterol • Never experienced palpitations • This was a single episode • •
What are the key parts of the physical examination, and what tests should be performed?
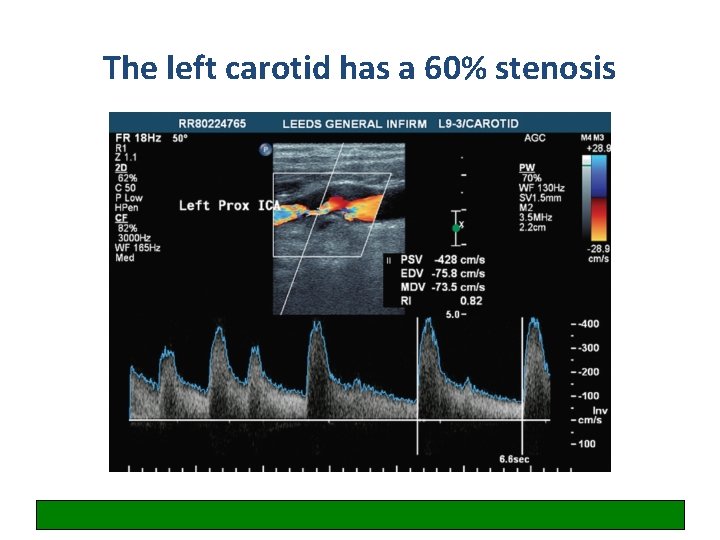
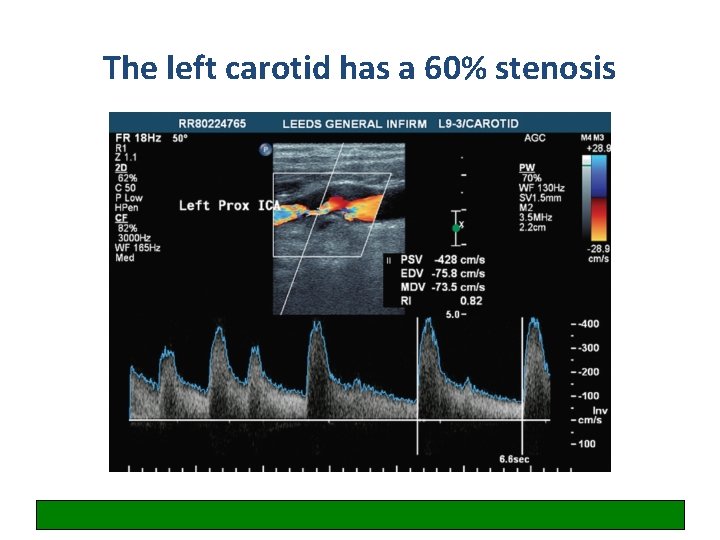
The left carotid has a 60% stenosis
Write down your overall management plan for this patient
Specialist assessment 1. Was this a TIA? 2. If yes, what arterial territory was it in? 3. What was the cause/underlying risk factors? (Remember: TIA/stroke is multifactorial)
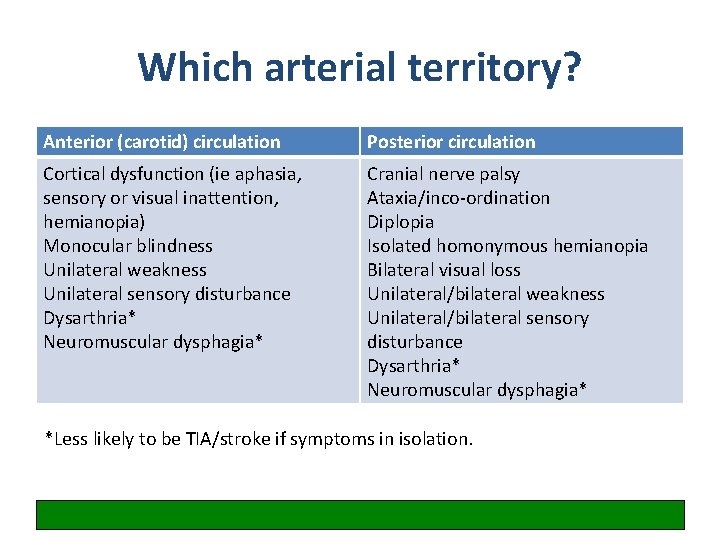
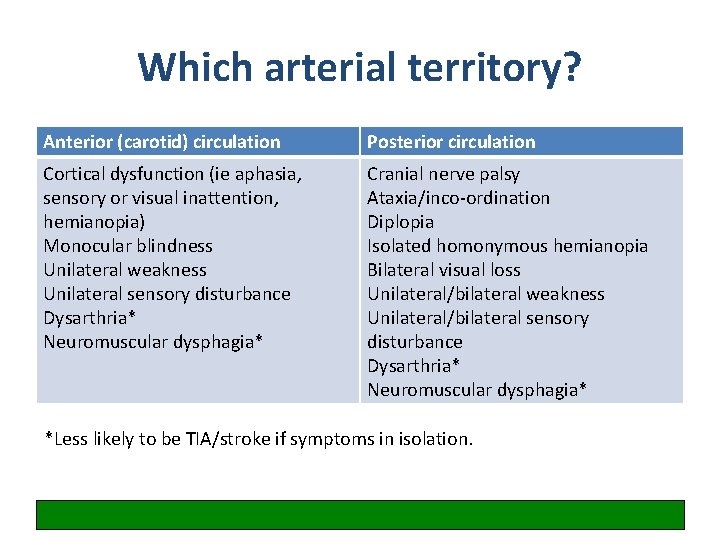
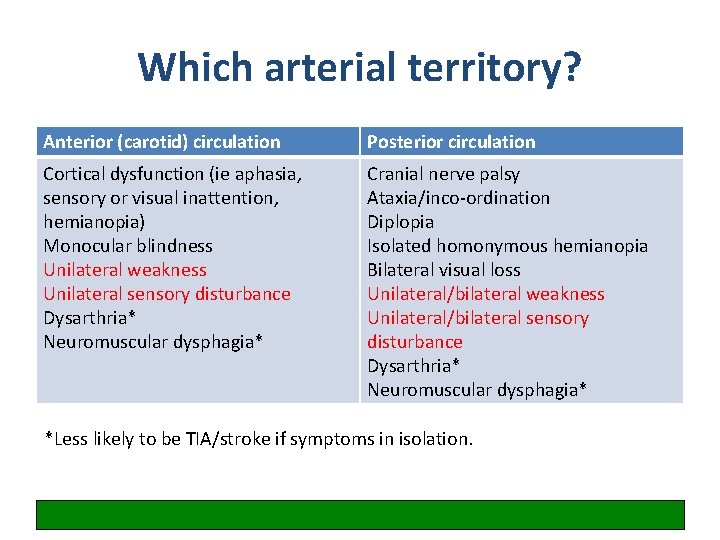
Which arterial territory? Anterior (carotid) circulation Posterior circulation Cortical dysfunction (ie aphasia, sensory or visual inattention, hemianopia) Monocular blindness Unilateral weakness Unilateral sensory disturbance Dysarthria* Neuromuscular dysphagia* Cranial nerve palsy Ataxia/inco-ordination Diplopia Isolated homonymous hemianopia Bilateral visual loss Unilateral/bilateral weakness Unilateral/bilateral sensory disturbance Dysarthria* Neuromuscular dysphagia* *Less likely to be TIA/stroke if symptoms in isolation.
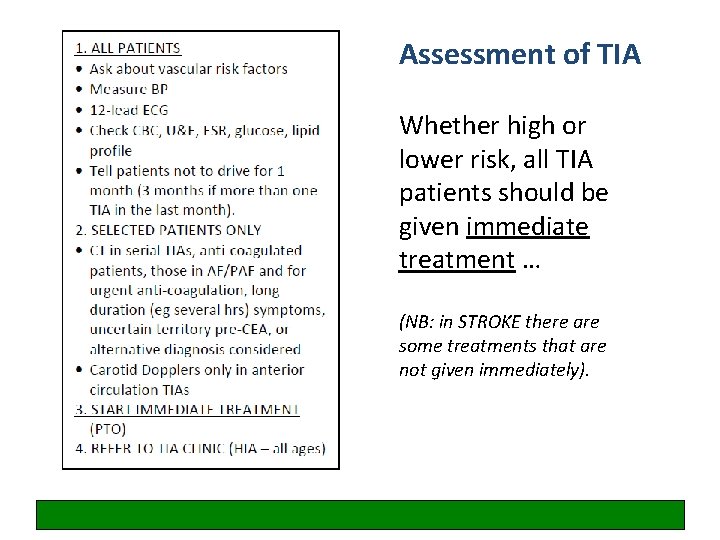
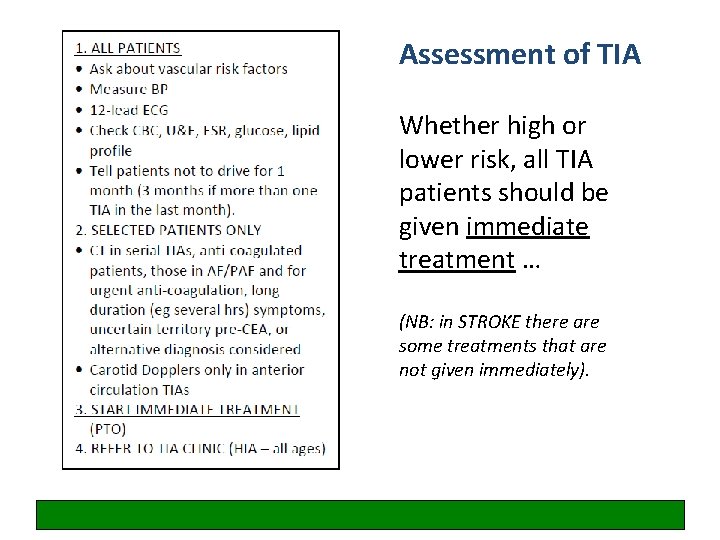
Assessment of TIA Whether high or lower risk, all TIA patients should be given immediate treatment … (NB: in STROKE there are some treatments that are not given immediately).
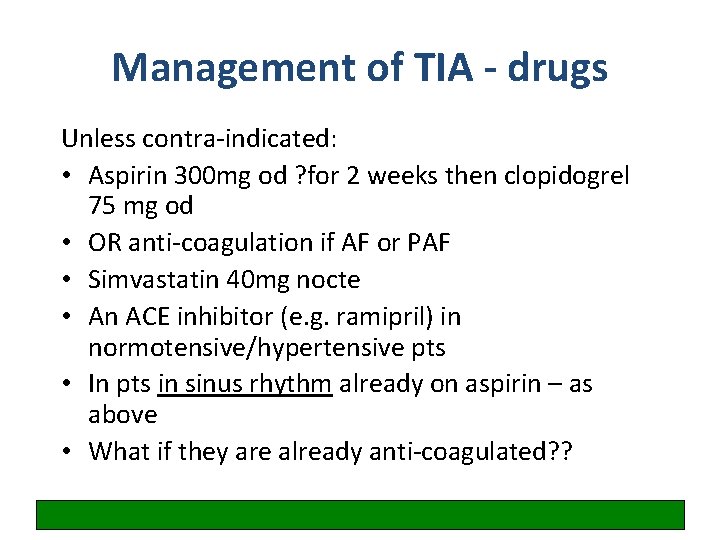
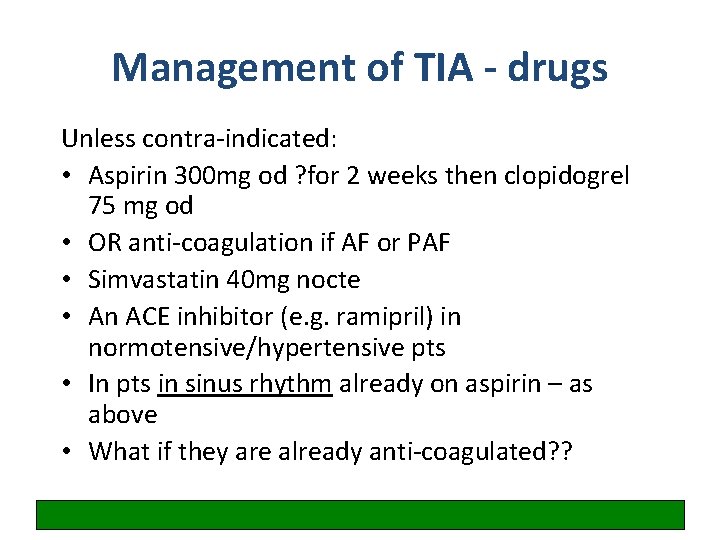
Management of TIA - drugs Unless contra-indicated: • Aspirin 300 mg od ? for 2 weeks then clopidogrel 75 mg od • OR anti-coagulation if AF or PAF • Simvastatin 40 mg nocte • An ACE inhibitor (e. g. ramipril) in normotensive/hypertensive pts • In pts in sinus rhythm already on aspirin – as above • What if they are already anti-coagulated? ?
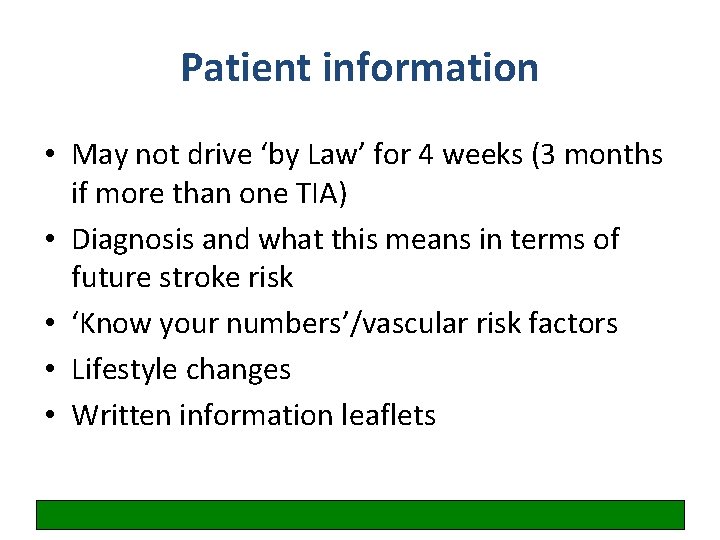
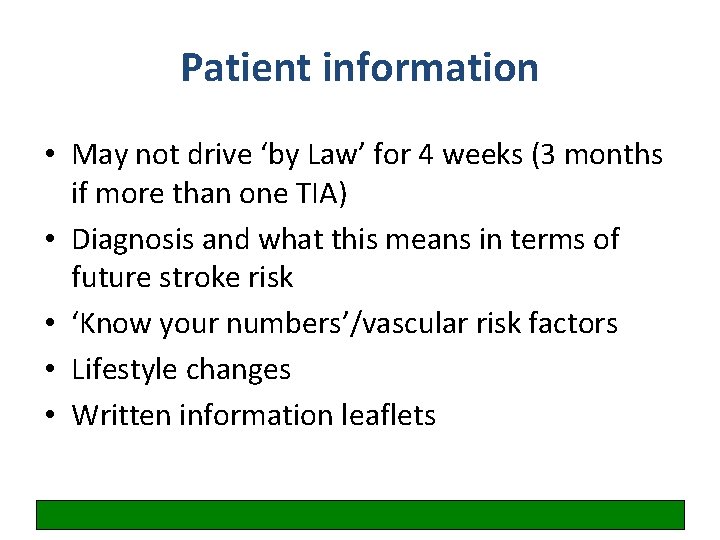
Patient information • May not drive ‘by Law’ for 4 weeks (3 months if more than one TIA) • Diagnosis and what this means in terms of future stroke risk • ‘Know your numbers’/vascular risk factors • Lifestyle changes • Written information leaflets
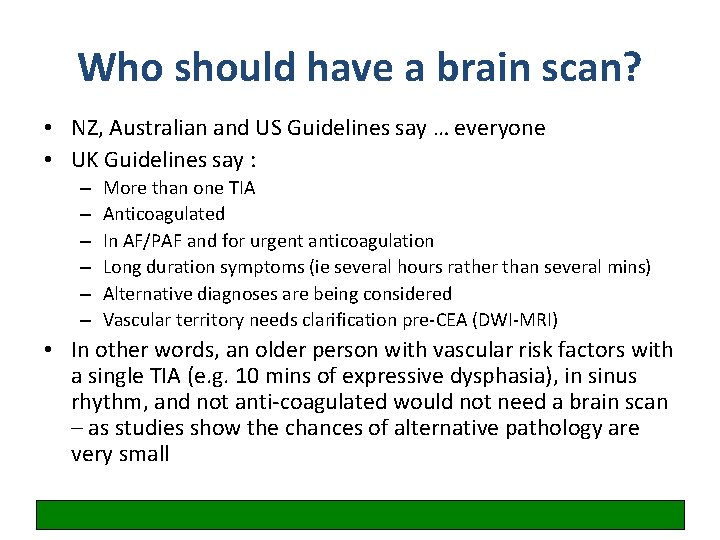
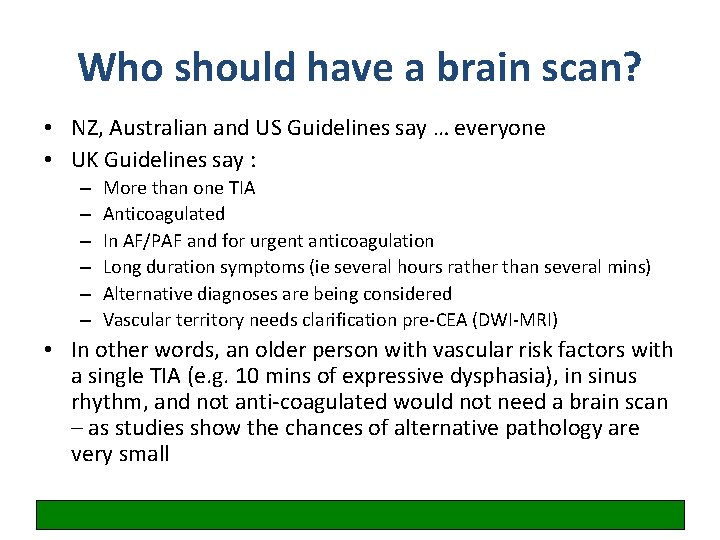
Who should have a brain scan? • NZ, Australian and US Guidelines say … everyone • UK Guidelines say : – – – More than one TIA Anticoagulated In AF/PAF and for urgent anticoagulation Long duration symptoms (ie several hours rather than several mins) Alternative diagnoses are being considered Vascular territory needs clarification pre-CEA (DWI-MRI) • In other words, an older person with vascular risk factors with a single TIA (e. g. 10 mins of expressive dysphasia), in sinus rhythm, and not anti-coagulated would not need a brain scan – as studies show the chances of alternative pathology are very small
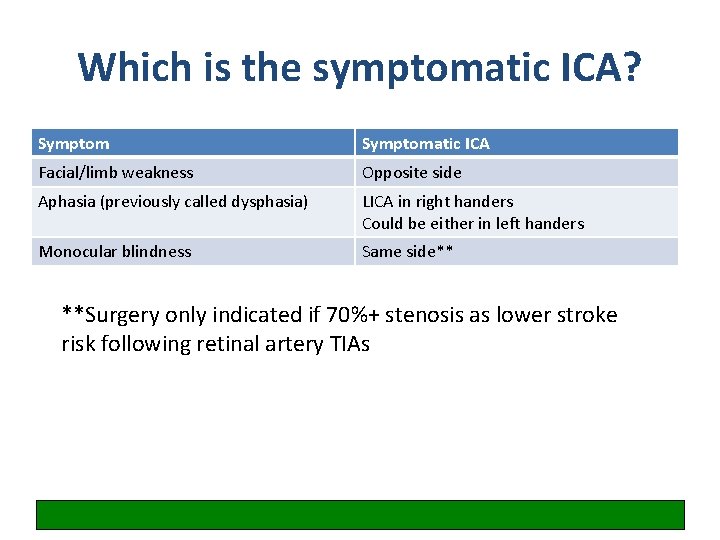
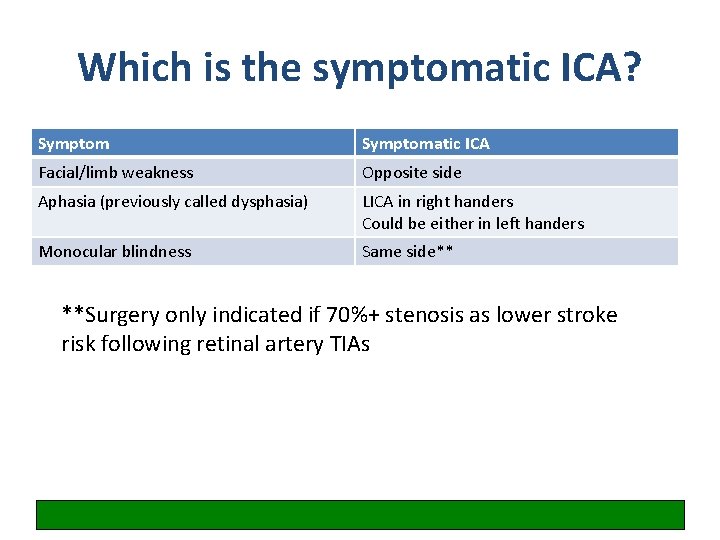
Which is the symptomatic ICA? Symptomatic ICA Facial/limb weakness Opposite side Aphasia (previously called dysphasia) LICA in right handers Could be either in left handers Monocular blindness Same side** **Surgery only indicated if 70%+ stenosis as lower stroke risk following retinal artery TIAs
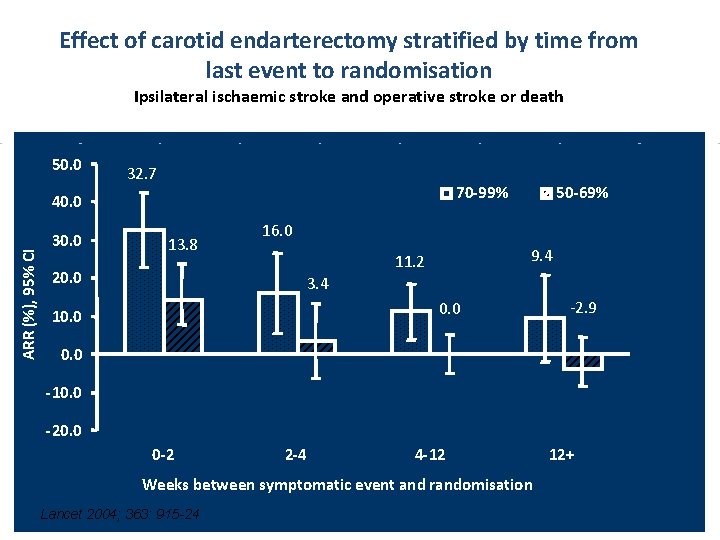
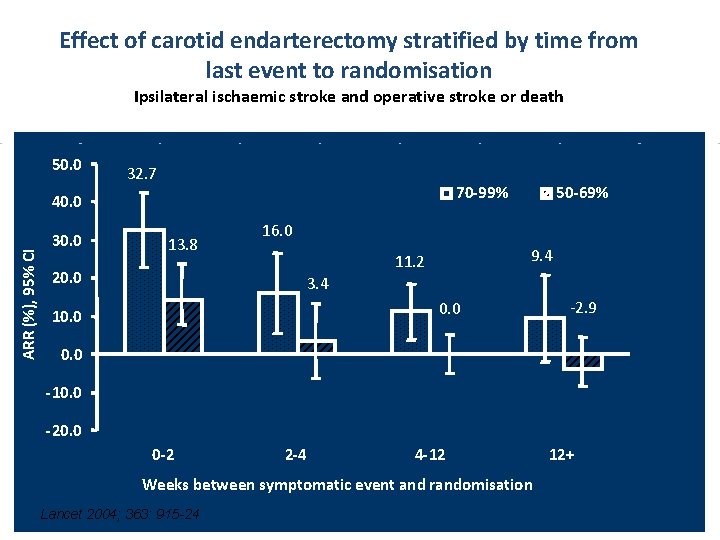
Effect of carotid endarterectomy stratified by time from last event to randomisation Ipsilateral ischaemic stroke and operative stroke or death 50. 0 32. 7 70 -99% ARR (%), 95% CI 40. 0 30. 0 13. 8 20. 0 50 -69% 16. 0 9. 4 11. 2 3. 4 0. 0 10. 0 -2. 9 0. 0 -10. 0 -20. 0 0 -2 2 -4 4 -12 Weeks between symptomatic event and randomisation Lancet 2004; 363: 915 -24 12+
Look at your management plan again – does it need to change?
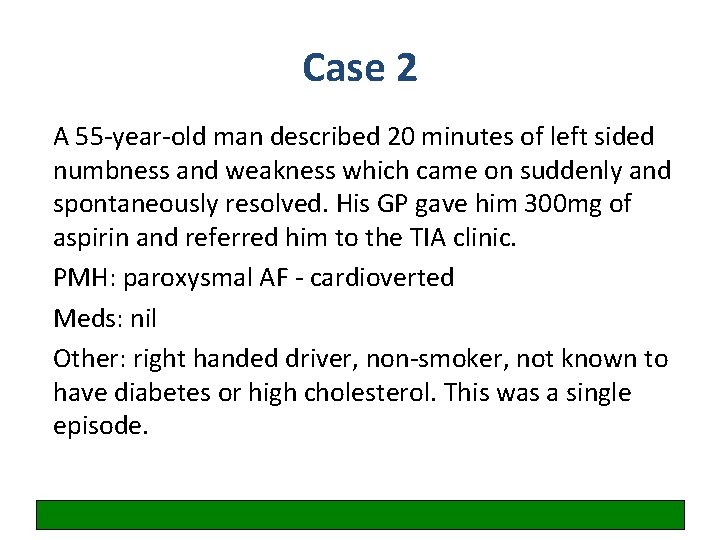
Case 2 A 55 -year-old man described 20 minutes of left sided numbness and weakness which came on suddenly and spontaneously resolved. His GP gave him 300 mg of aspirin and referred him to the TIA clinic. PMH: paroxysmal AF - cardioverted Meds: nil Other: right handed driver, non-smoker, not known to have diabetes or high cholesterol. This was a single episode.
Examination: Normal BP = 140/80 mm. Hg Test results: 12 -lead ECG shows atrial fibrillation Blood results normal
Write down your overall management plan for this patient
Case 2: management Same day investigations and treatment: • CT of the head to exclude bleed before starting urgent anticoagulation with clexane • On the other hand – would we want to do a DWI-MRI to decide whether this was a posterior or anterior circulation event? • Carotid Doppler USS • Ramipril, simvastatin, driving and lifestyle advice
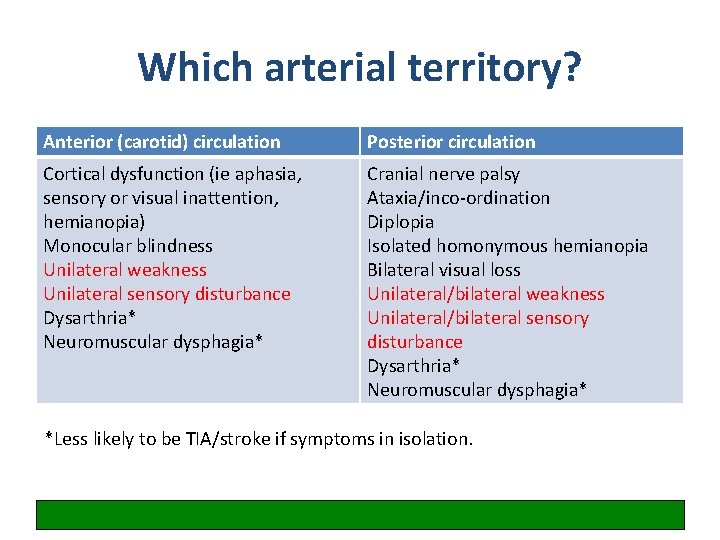
Which arterial territory? Anterior (carotid) circulation Posterior circulation Cortical dysfunction (ie aphasia, sensory or visual inattention, hemianopia) Monocular blindness Unilateral weakness Unilateral sensory disturbance Dysarthria* Neuromuscular dysphagia* Cranial nerve palsy Ataxia/inco-ordination Diplopia Isolated homonymous hemianopia Bilateral visual loss Unilateral/bilateral weakness Unilateral/bilateral sensory disturbance Dysarthria* Neuromuscular dysphagia* *Less likely to be TIA/stroke if symptoms in isolation.
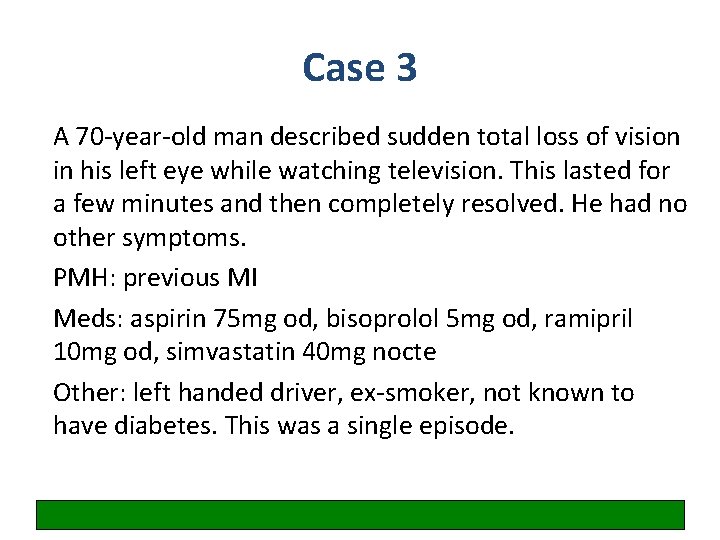
Case 3 A 70 -year-old man described sudden total loss of vision in his left eye while watching television. This lasted for a few minutes and then completely resolved. He had no other symptoms. PMH: previous MI Meds: aspirin 75 mg od, bisoprolol 5 mg od, ramipril 10 mg od, simvastatin 40 mg nocte Other: left handed driver, ex-smoker, not known to have diabetes. This was a single episode.
Examination: Normal BP = 130/75 mm. Hg Test results: 12 -lead ECG – old inferior MI Blood results normal
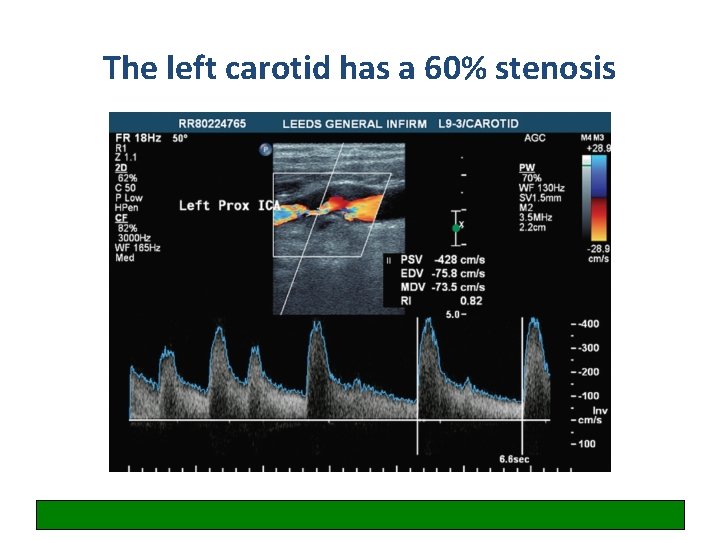
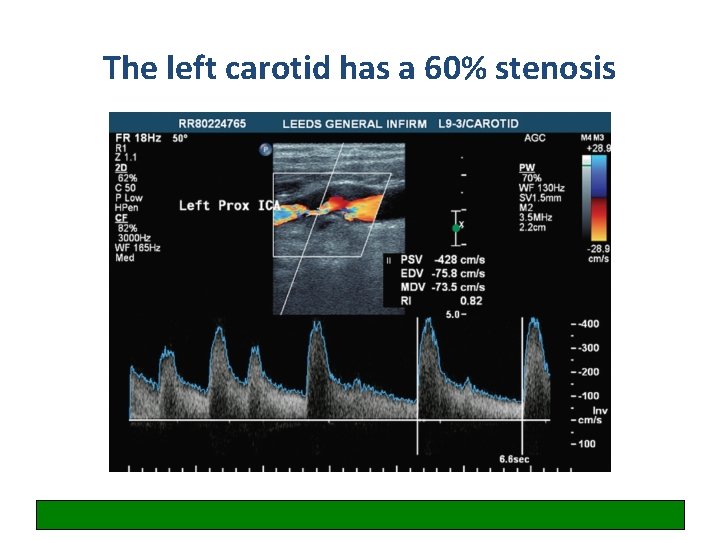
The left carotid has a 60% stenosis
Write down your overall management plan for this patient
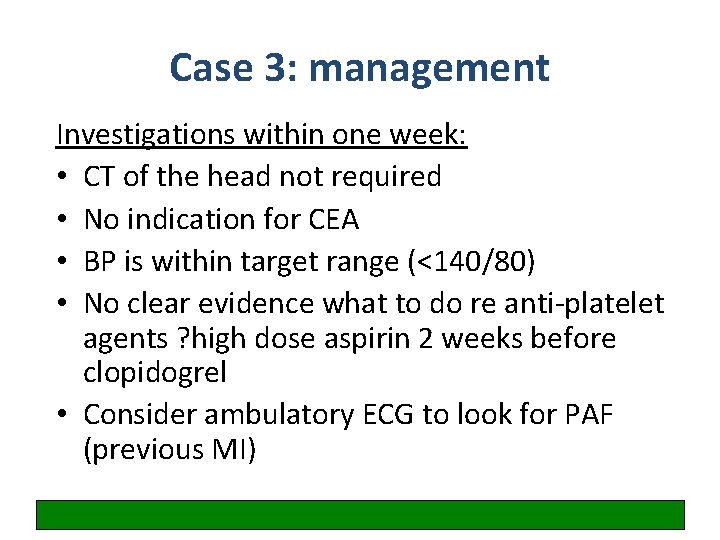
Case 3: management Investigations within one week: • CT of the head not required • No indication for CEA • BP is within target range (<140/80) • No clear evidence what to do re anti-platelet agents ? high dose aspirin 2 weeks before clopidogrel • Consider ambulatory ECG to look for PAF (previous MI)
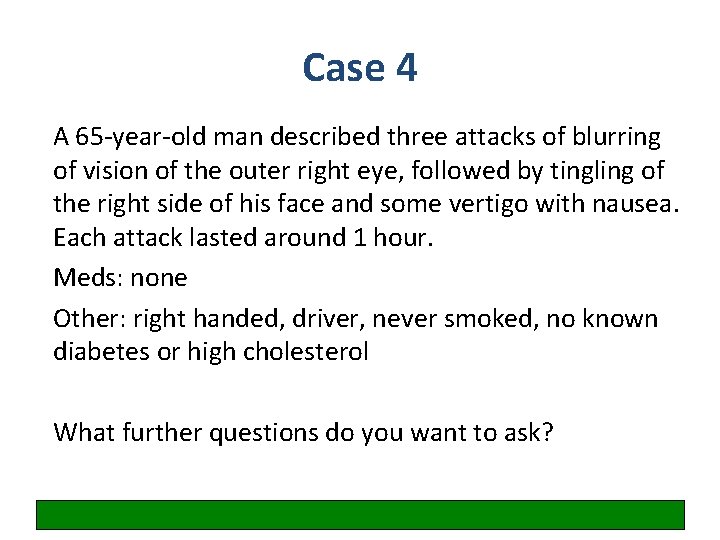
Case 4 A 65 -year-old man described three attacks of blurring of vision of the outer right eye, followed by tingling of the right side of his face and some vertigo with nausea. Each attack lasted around 1 hour. Meds: none Other: right handed, driver, never smoked, no known diabetes or high cholesterol What further questions do you want to ask?
Examination: Normal BP = 160/90 mm. Hg Test results: 12 -lead ECG – normal Blood results normal
Write down your overall management plan for this patient
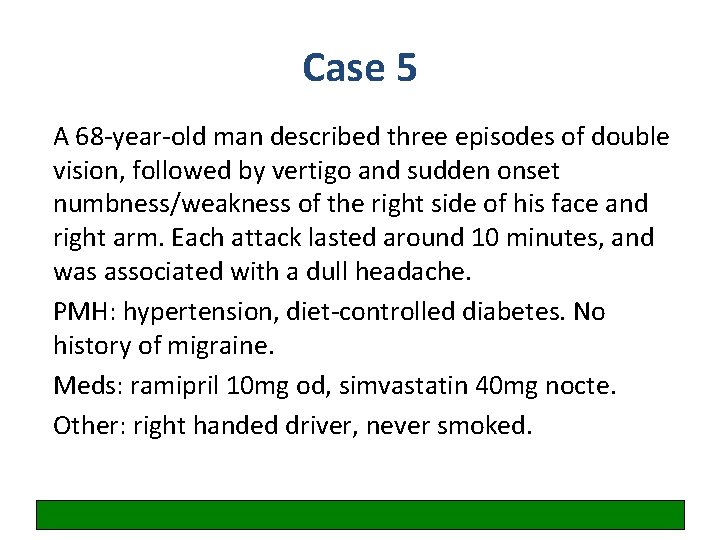
Case 5 A 68 -year-old man described three episodes of double vision, followed by vertigo and sudden onset numbness/weakness of the right side of his face and right arm. Each attack lasted around 10 minutes, and was associated with a dull headache. PMH: hypertension, diet-controlled diabetes. No history of migraine. Meds: ramipril 10 mg od, simvastatin 40 mg nocte. Other: right handed driver, never smoked.
Examination: Normal BP = 130/75 mm. Hg Test results: 12 -lead ECG – normal Blood results normal
Write down your overall management plan for this patient
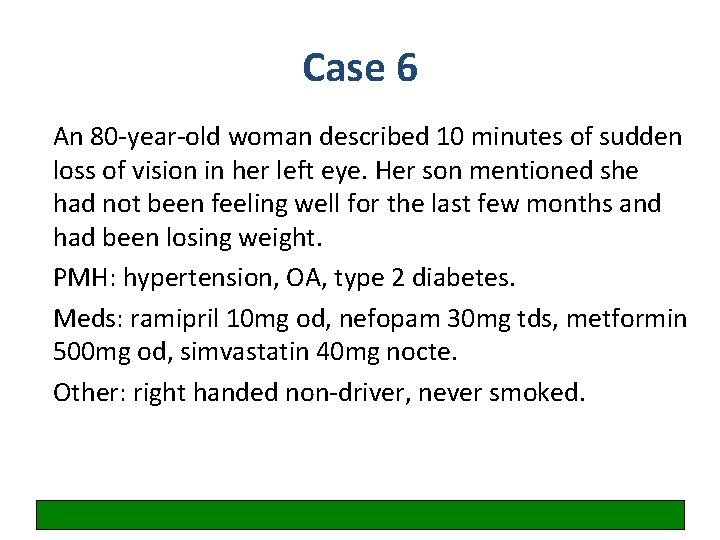
Case 6 An 80 -year-old woman described 10 minutes of sudden loss of vision in her left eye. Her son mentioned she had not been feeling well for the last few months and had been losing weight. PMH: hypertension, OA, type 2 diabetes. Meds: ramipril 10 mg od, nefopam 30 mg tds, metformin 500 mg od, simvastatin 40 mg nocte. Other: right handed non-driver, never smoked.
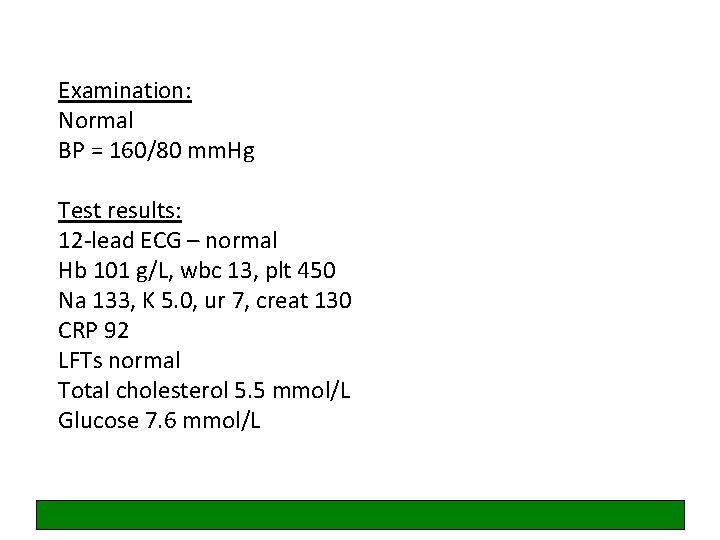
Examination: Normal BP = 160/80 mm. Hg Test results: 12 -lead ECG – normal Hb 101 g/L, wbc 13, plt 450 Na 133, K 5. 0, ur 7, creat 130 CRP 92 LFTs normal Total cholesterol 5. 5 mmol/L Glucose 7. 6 mmol/L
What further Qs / examination of this patient is required? Write down your overall management plan for this patient
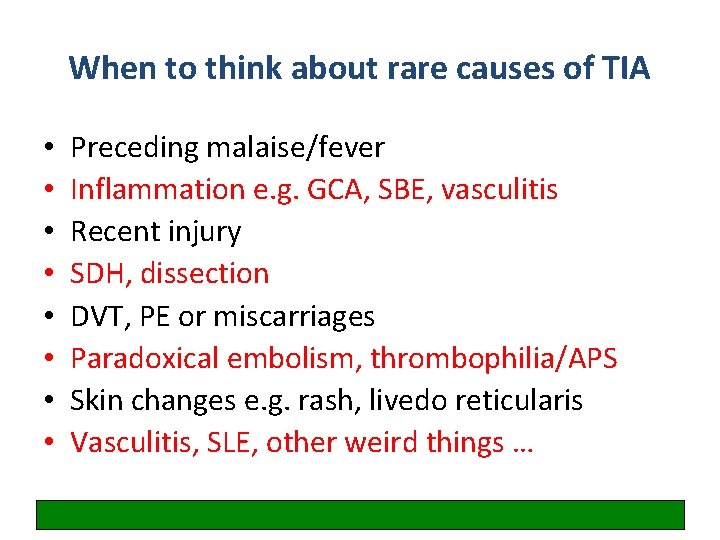
When to think about rare causes of TIA • • Preceding malaise/fever Inflammation e. g. GCA, SBE, vasculitis Recent injury SDH, dissection DVT, PE or miscarriages Paradoxical embolism, thrombophilia/APS Skin changes e. g. rash, livedo reticularis Vasculitis, SLE, other weird things …
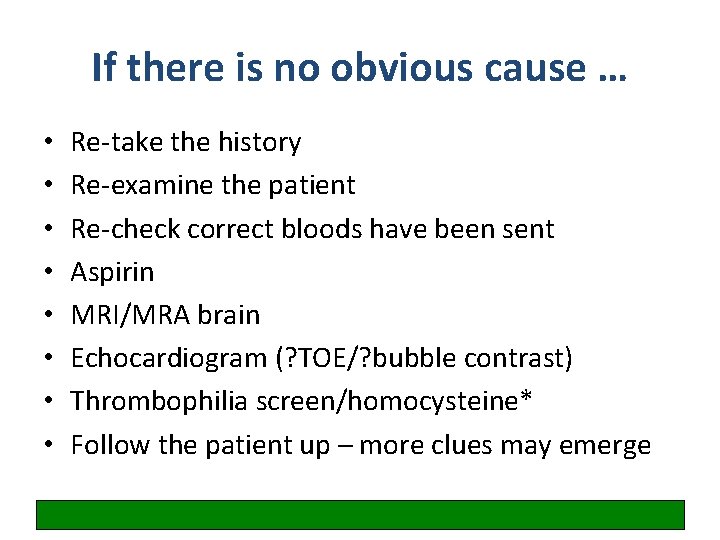
If there is no obvious cause … • • Re-take the history Re-examine the patient Re-check correct bloods have been sent Aspirin MRI/MRA brain Echocardiogram (? TOE/? bubble contrast) Thrombophilia screen/homocysteine* Follow the patient up – more clues may emerge
Weird things • • • Limb shaking syndrome Low flow TIAs Capsular warning syndrome Basilar artery thrombosis Cerebral amyloid angiopathy (‘amyloid spells’) – thought to be due to focal seizures
Discussion