Welcome to the Spirometry Course Developed by Felip
Welcome to the Spirometry Course Developed by: • Felip Burgos: Hospital Clínic of Barcelona • Jordi Giner: Hospital de la Santa Creu i Sant Pau of Barcelona • SIBELMED Barcelona 2015 1

Let's Begin 2
Spirometry History Let's Begin 3
History of Spirometry Let's Begin Etymologically, spirometry means the measurement of breath or breathing. The term is attributed to Lavoisier (1862), who discovered oxygen and gave it its name. 4
5
First Attempt to Measure Lung Capacity Galen (AD 129 -200) Doctor and Greek philosopher In his experiment, he asked a child to breath into a bladder, observing that the volume entering the bladder did not vary with each breath. (he did not record any measurements). 6
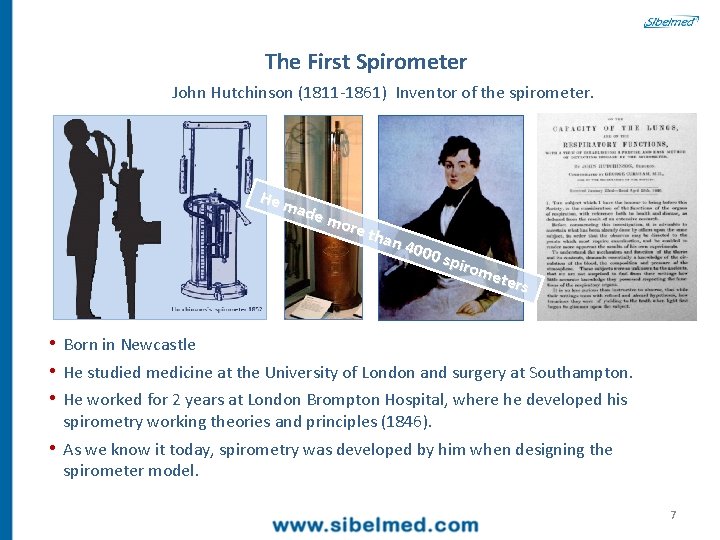
The First Spirometer John Hutchinson (1811 -1861) Inventor of the spirometer. He m ade mor e th an 4 000 spiro met ers • Born in Newcastle • He studied medicine at the University of London and surgery at Southampton. • He worked for 2 years at London Brompton Hospital, where he developed his spirometry working theories and principles (1846). • As we know it today, spirometry was developed by him when designing the spirometer model. 7
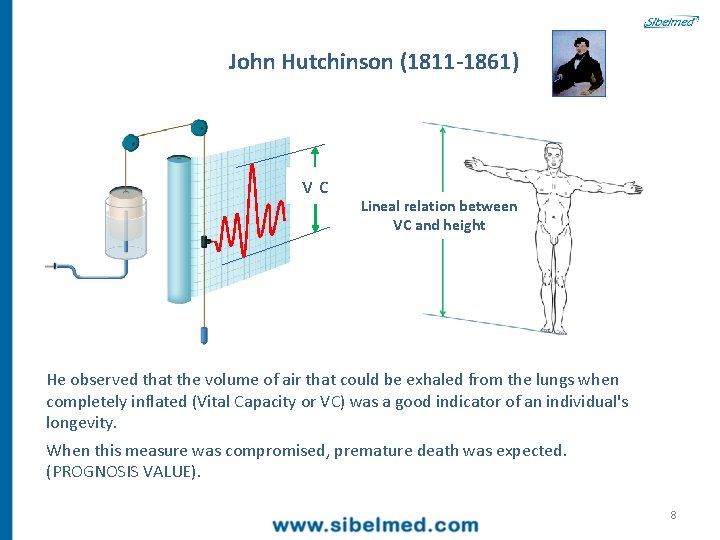
John Hutchinson (1811 -1861) vc Lineal relation between VC and height He observed that the volume of air that could be exhaled from the lungs when completely inflated (Vital Capacity or VC) was a good indicator of an individual's longevity. When this measure was compromised, premature death was expected. (PROGNOSIS VALUE). 8
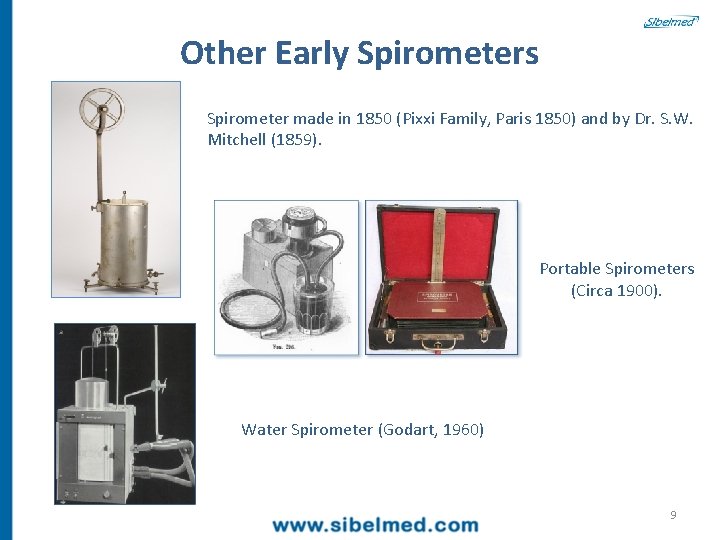
Other Early Spirometers Spirometer made in 1850 (Pixxi Family, Paris 1850) and by Dr. S. W. Mitchell (1859). Portable Spirometers (Circa 1900). Water Spirometer (Godart, 1960) 9
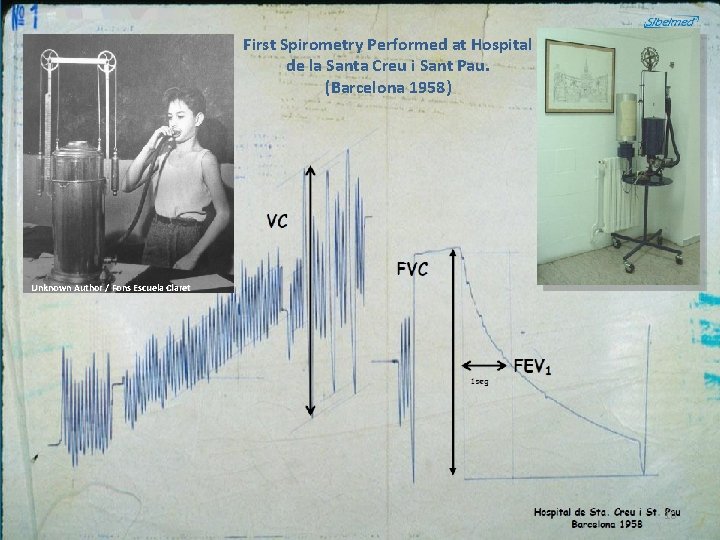
First Spirometry Performed at Hospital de la Santa Creu i Sant Pau. (Barcelona 1958) Unknown Author / Fons Escuela Claret 10
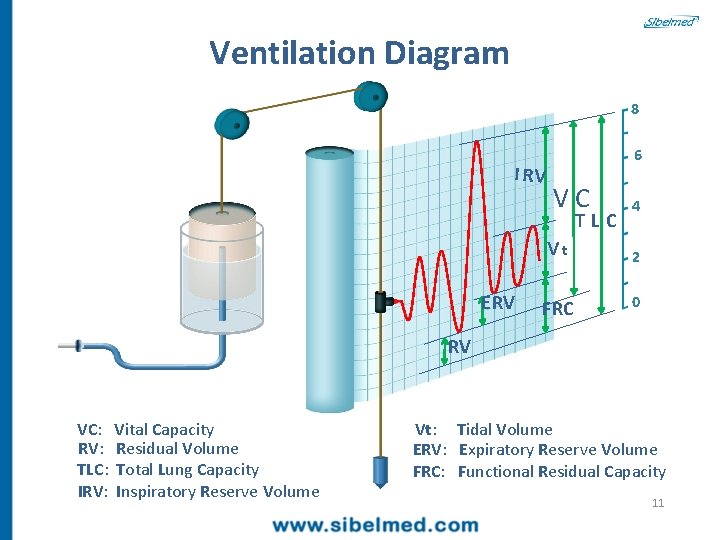
Ventilation Diagram 8 I RV 6 VC vt E RV FRC TLC 4 2 0 RV VC: Vital Capacity RV: Residual Volume TLC: Total Lung Capacity IRV: Inspiratory Reserve Volume Vt: Tidal Volume ERV: Expiratory Reserve Volume FRC: Functional Residual Capacity 11
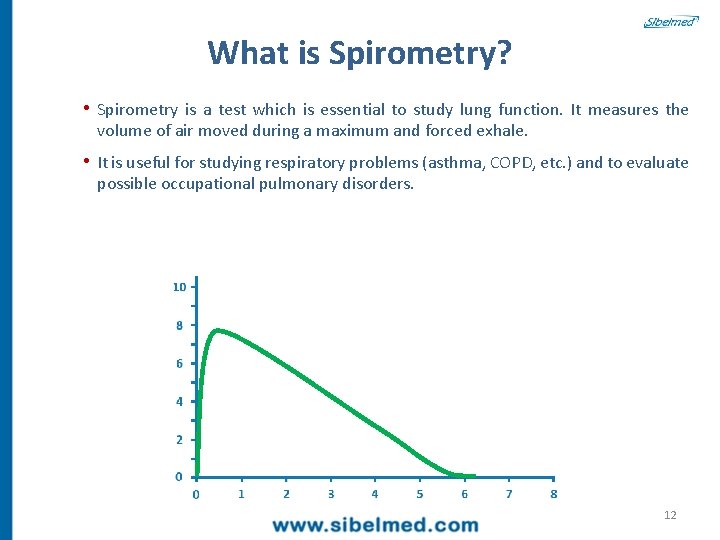
What is Spirometry? • Spirometry is a test which is essential to study lung function. It measures the volume of air moved during a maximum and forced exhale. • It is useful for studying respiratory problems (asthma, COPD, etc. ) and to evaluate possible occupational pulmonary disorders. 12

Spirometry 8 VEMS = FEV 1 6 FVC In the 1 st second 4 2 0 VEMS: Volume Expiratoire Maximum Seconde (Maximum Expiratory Volume in one Second) FEV 1: Forced Expiratory Volume in the first Second 13
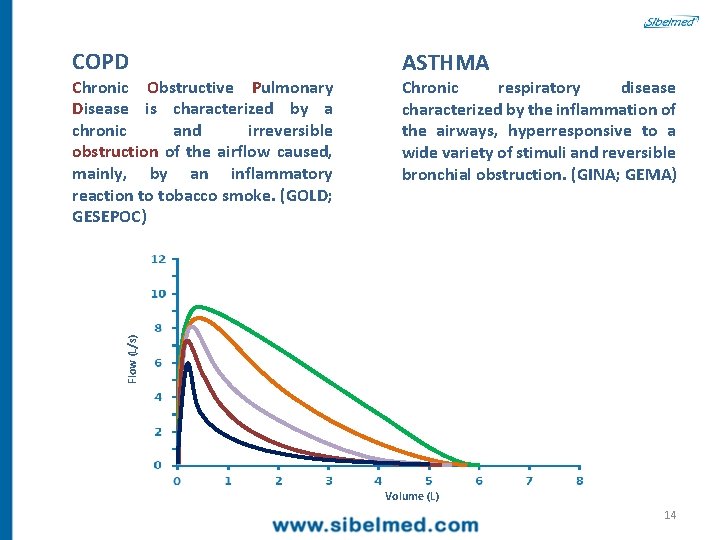
COPD Chronic respiratory disease characterized by the inflammation of the airways, hyperresponsive to a wide variety of stimuli and reversible bronchial obstruction. (GINA; GEMA) Flow (L/s) Chronic Obstructive Pulmonary Disease is characterized by a chronic and irreversible obstruction of the airflow caused, mainly, by an inflammatory reaction to tobacco smoke. (GOLD; GESEPOC) ASTHMA Volume (L) 14
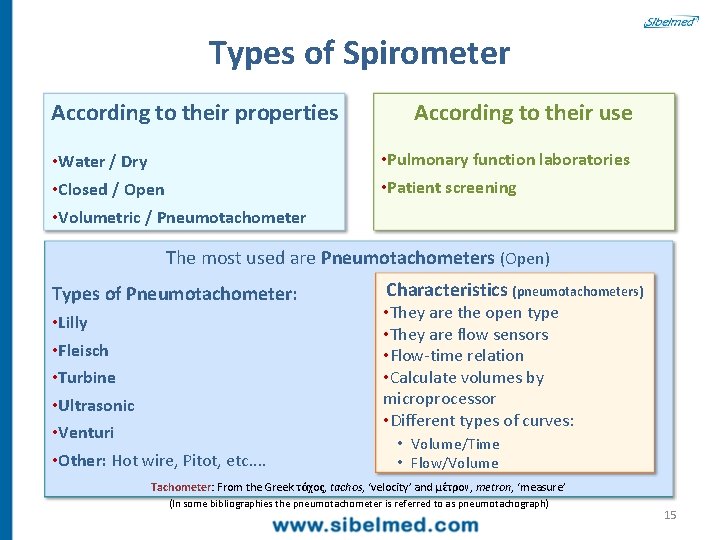
Types of Spirometer According to their properties • Water / Dry • Closed / Open • Volumetric / Pneumotachometer According to their use • Pulmonary function laboratories • Patient screening The most used are Pneumotachometers (Open) Types of Pneumotachometer: • Lilly • Fleisch • Turbine • Ultrasonic • Venturi • Other: Hot wire, Pitot, etc. . Characteristics (pneumotachometers) • They are the open type • They are flow sensors • Flow-time relation • Calculate volumes by microprocessor • Different types of curves: • Volume/Time • Flow/Volume Tachometer: From the Greek τάχος, tachos, ‘velocity’ and μέτρον, metron, ‘measure’ (In some bibliographies the pneumotachometer is referred to as pneumotachograph) 15
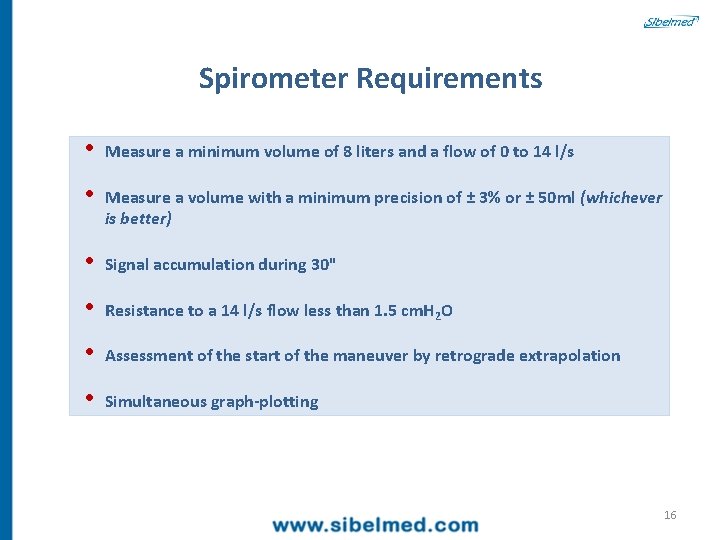
Spirometer Requirements • Measure a minimum volume of 8 liters and a flow of 0 to 14 l/s • Measure a volume with a minimum precision of ± 3% or ± 50 ml (whichever is better) • Signal accumulation during 30" • Resistance to a 14 l/s flow less than 1. 5 cm. H 2 O • Assessment of the start of the maneuver by retrograde extrapolation • Simultaneous graph-plotting 16

Water Bell Spirometer Water Spirometer The bell moves when exhaling Moves the paper and marker Results are plotted 17
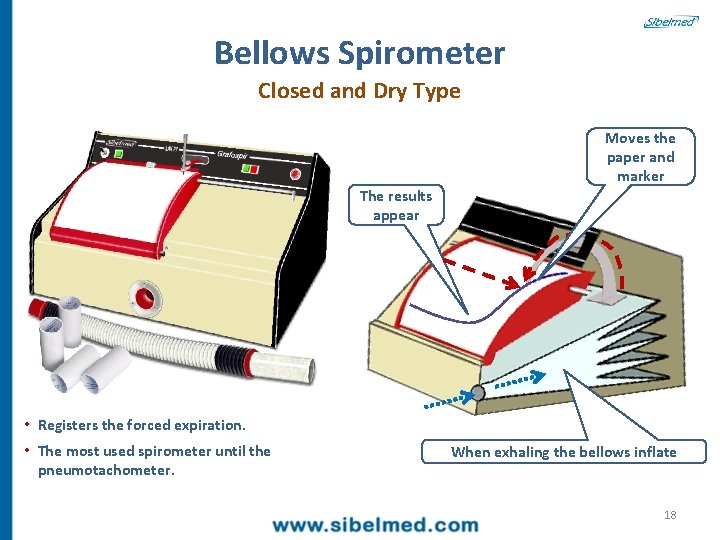
Bellows Spirometer Closed and Dry Type The results appear Moves the paper and marker • Registers the forced expiration. • The most used spirometer until the pneumotachometer. When exhaling the bellows inflate 18
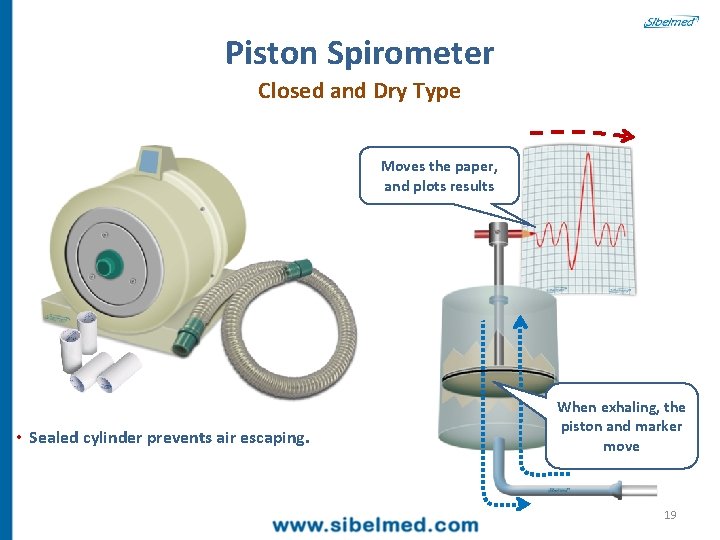
Piston Spirometer Closed and Dry Type Moves the paper, and plots results • Sealed cylinder prevents air escaping. When exhaling, the piston and marker move 19
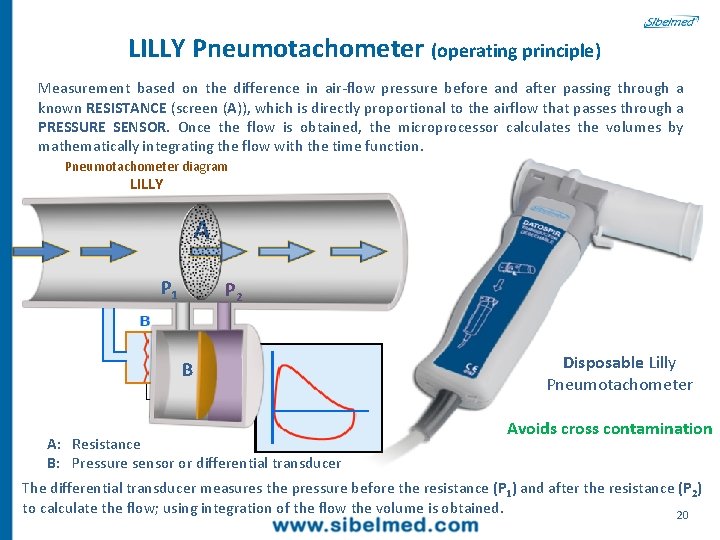
LILLY Pneumotachometer (operating principle) Measurement based on the difference in air-flow pressure before and after passing through a known RESISTANCE (screen (A)), which is directly proportional to the airflow that passes through a PRESSURE SENSOR. Once the flow is obtained, the microprocessor calculates the volumes by mathematically integrating the flow with the time function. Pneumotachometer diagram LILLY A P 1 P 2 B A: Resistance B: Pressure sensor or differential transducer Disposable Lilly Pneumotachometer Avoids cross contamination The differential transducer measures the pressure before the resistance (P 1) and after the resistance (P 2) to calculate the flow; using integration of the flow the volume is obtained. 20
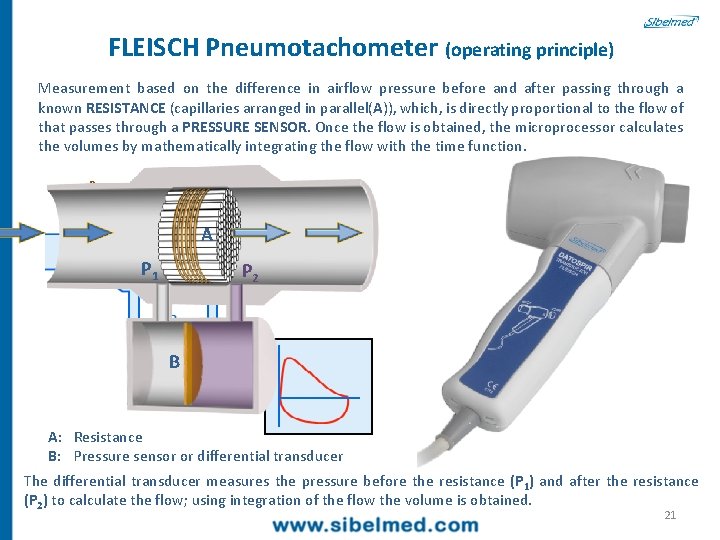
FLEISCH Pneumotachometer (operating principle) Measurement based on the difference in airflow pressure before and after passing through a known RESISTANCE (capillaries arranged in parallel(A)), which, is directly proportional to the flow of that passes through a PRESSURE SENSOR. Once the flow is obtained, the microprocessor calculates the volumes by mathematically integrating the flow with the time function. Pneumotachometer diagram FLEISCH A P 1 P 2 B A: Resistance B: Pressure sensor or differential transducer The differential transducer measures the pressure before the resistance (P 1) and after the resistance (P 2) to calculate the flow; using integration of the flow the volume is obtained. 21
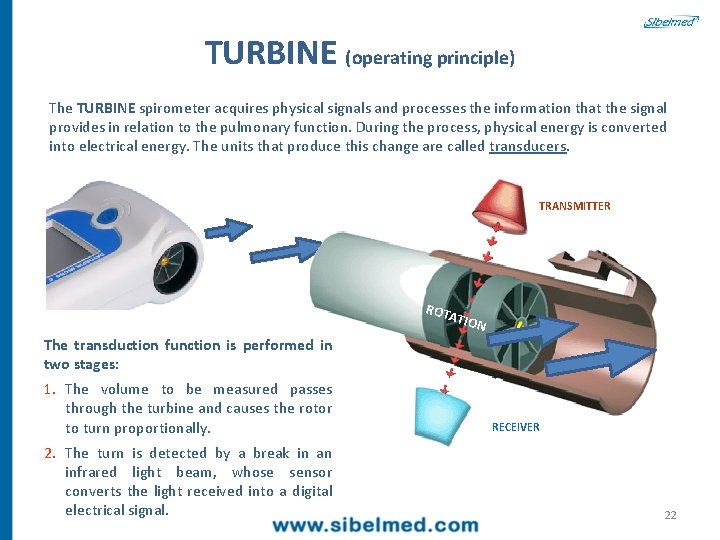
TURBINE (operating principle) The TURBINE spirometer acquires physical signals and processes the information that the signal provides in relation to the pulmonary function. During the process, physical energy is converted into electrical energy. The units that produce this change are called transducers. TRANSMITTER ROT ATIO N The transduction function is performed in two stages: 1. The volume to be measured passes through the turbine and causes the rotor to turn proportionally. 2. The turn is detected by a break in an infrared light beam, whose sensor converts the light received into a digital electrical signal. RECEIVER 22
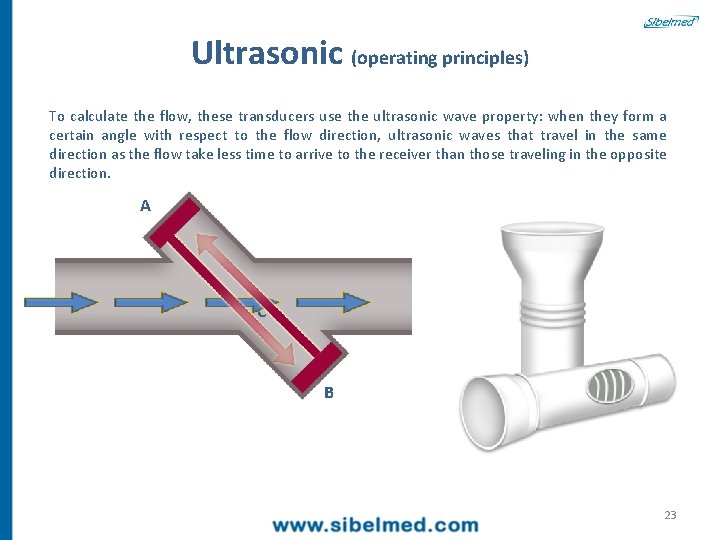
Ultrasonic (operating principles) To calculate the flow, these transducers use the ultrasonic wave property: when they form a certain angle with respect to the flow direction, ultrasonic waves that travel in the same direction as the flow take less time to arrive to the receiver than those traveling in the opposite direction. A C B 23
Spirometry Graphs 24
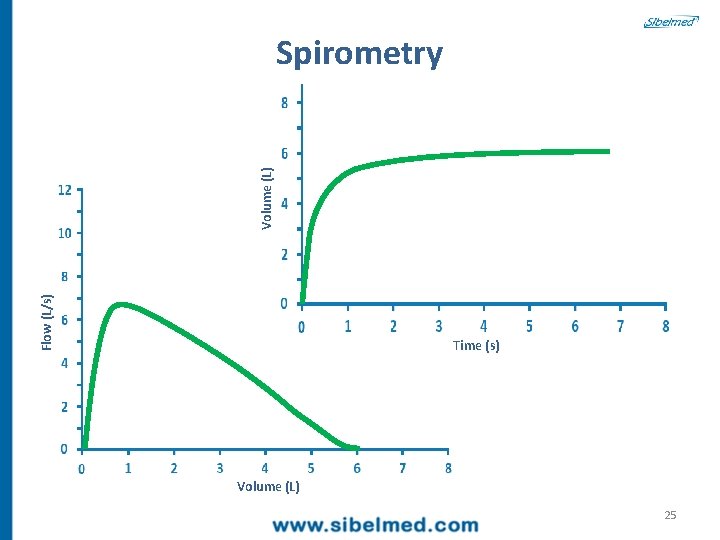
Flow (L/s) Volume (L) Spirometry Time (s) Volume (L) 25
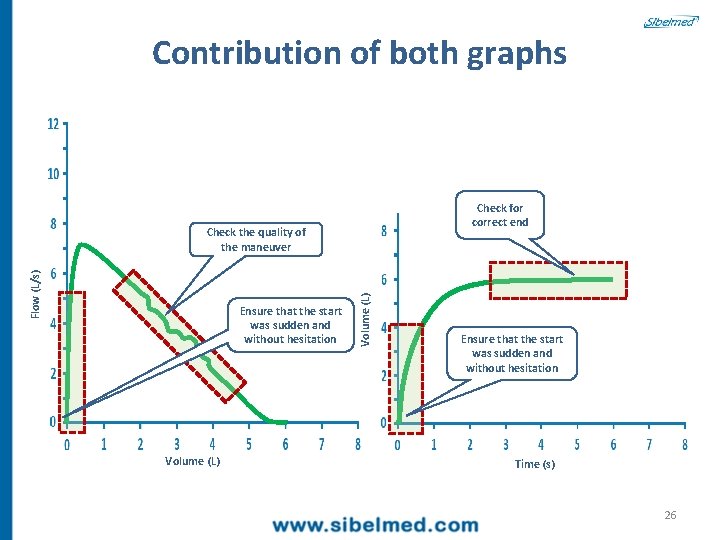
Contribution of both graphs Check for correct end Ensure that the start was sudden and without hesitation Volume (L) Flow (L/s) Check the quality of the maneuver Ensure that the start was sudden and without hesitation Time (s) 26
Functional Alterations: • Obstruction • No Obstruction 27
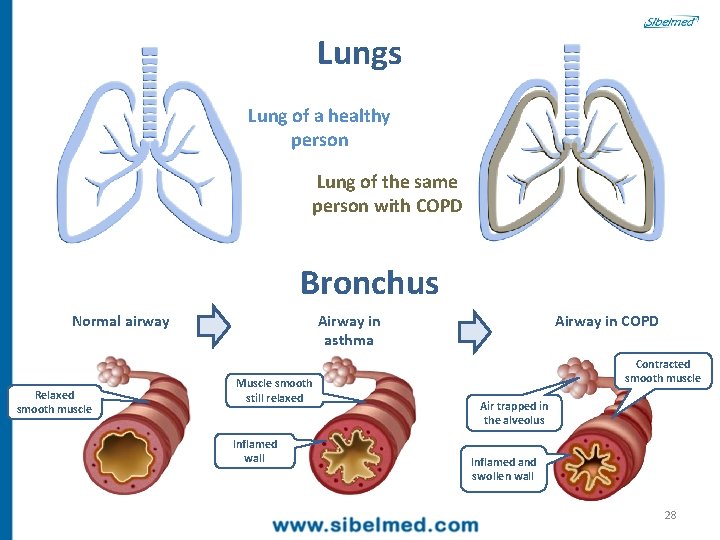
Lungs Lung of a healthy person Lung of the same person with COPD Bronchus Normal airway Relaxed smooth muscle Airway in asthma Muscle smooth still relaxed Inflamed wall Airway in COPD Contracted smooth muscle Air trapped in the alveolus Inflamed and swollen wall 28
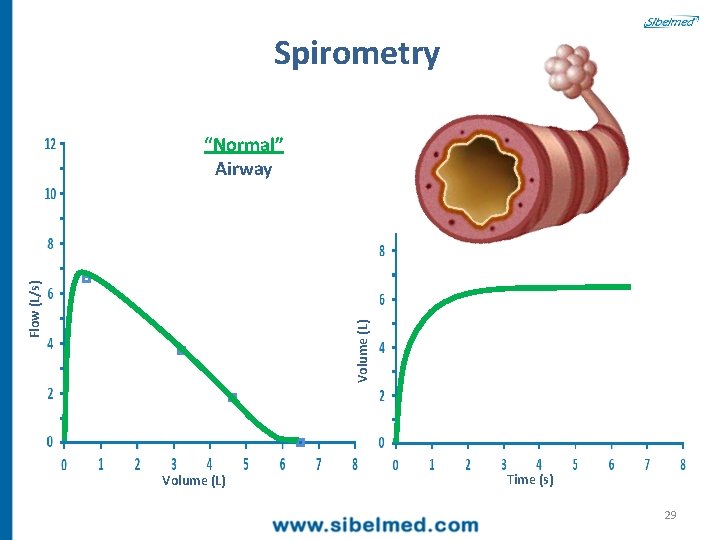
Spirometry Volume (L) Flow (L/s) “Normal” Airway Volume (L) Time (s) 29
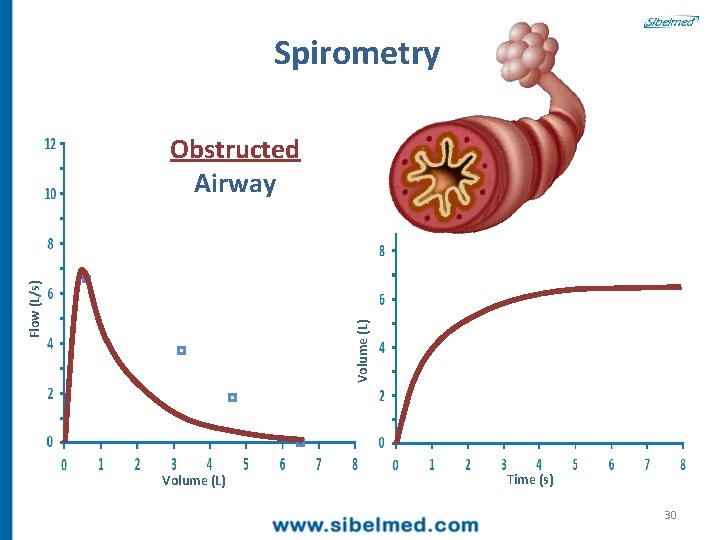
Spirometry Volume (L) Flow (L/s) Obstructed Airway Volume (L) Time (s) 30
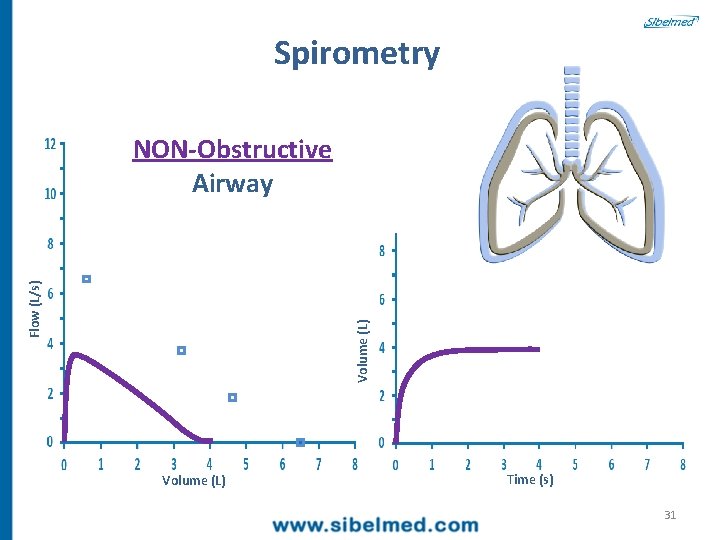
Spirometry Volume (L) Flow (L/s) NON-Obstructive Airway Volume (L) Time (s) 31

Spirometry Volume (L) Flow (L/s) Mixed Airway Volume (L) Time (s) 32
Spirometry parameters 33

Spirometric Parameters FVC : Forced Vital Capacity (FVC) Volume of air expelled during a forced expiration maneuver (L). Forced Spirometry FEV 1: Forced Expiratory Volume in the first second. Volume (L) FEV 1/FVC : FEV 6 FEV 1 FVC Expresses the volume of air expelled in the first second with respect to the maximum that can be expelled during the forced expiration maneuver. FEV 6: Time (s) Forced Expiratory Volume in the sixth second (L). 34

Spirometric Parameters Forced Spirometry PEF (Peak Flow) • Maximum expiratory flow or peak flow. • Maximum flow achieved during the forced expiration maneuver. PEF Flow (L/s) • It is generated before having expelled 15% of the FVC and must be maintained for a minimum of 10 ms (milliseconds) • Expressed in L/sec. • Effort-dependent parameter. Volume (L) 35

Spirometric Parameters Forced Spirometry FEF 50 % Flow (L/s) Maximum flow when the 50% of the FVC has been exhaled. FEF 25 -75 % FEF 25 Maximum flow between 25% and 75% of the FVC (mid-expiratory flows). FEF 50 FEF 75 Mid-expiratory flows may early detect obstruction (in the small tract), but they are highly variable. Volume (L) 36

Spirometry Obstructed Airway Volume (L) FVC ≈ FEV 6 Inflamed and swollen wall 1 sec 6 sec FEV 1 FVC Time (s) 37
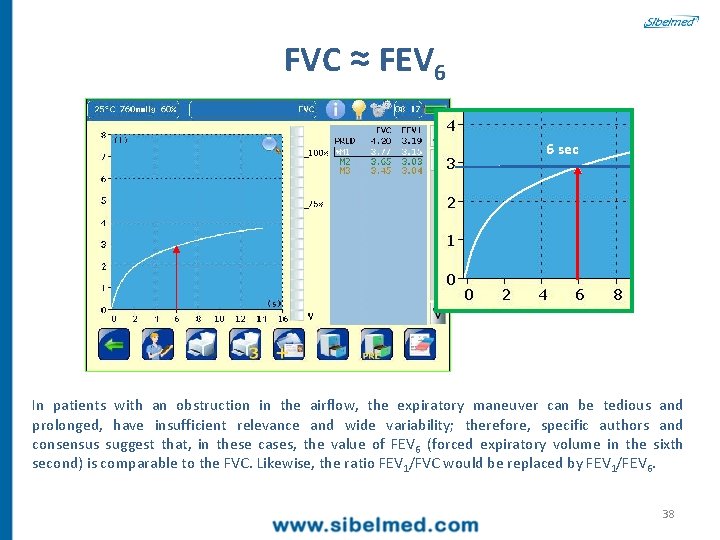
FVC ≈ FEV 6 6 sec In patients with an obstruction in the airflow, the expiratory maneuver can be tedious and prolonged, have insufficient relevance and wide variability; therefore, specific authors and consensus suggest that, in these cases, the value of FEV 6 (forced expiratory volume in the sixth second) is comparable to the FVC. Likewise, the ratio FEV 1/FVC would be replaced by FEV 1/FEV 6. 38
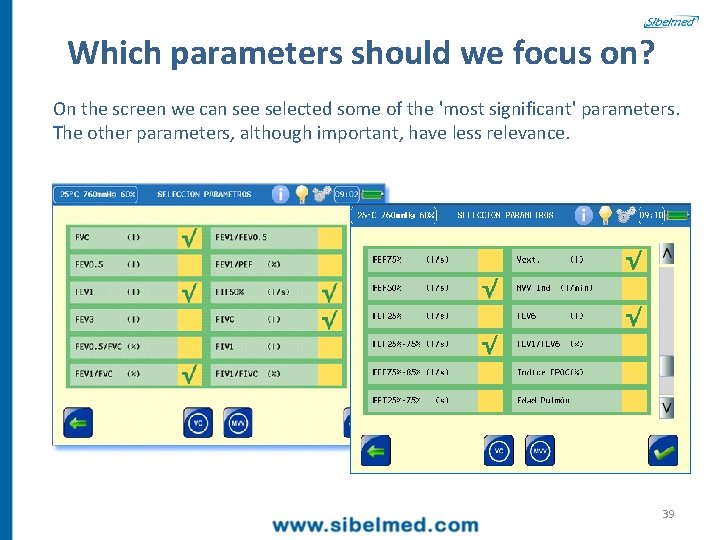
Which parameters should we focus on? On the screen we can see selected some of the 'most significant' parameters. The other parameters, although important, have less relevance. 39
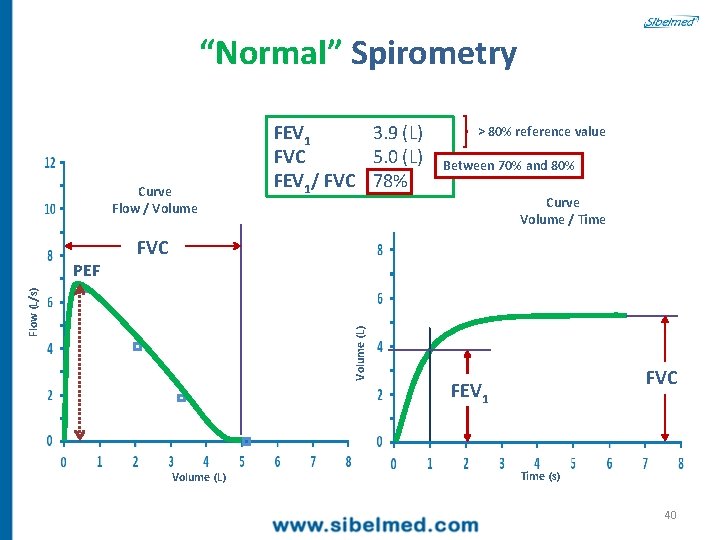
“Normal” Spirometry Curve Flow / Volume > 80% reference value Between 70% and 80% Curve Volume / Time FVC Volume (L) Flow (L/s) PEF FEV 1 3. 9 (L) FVC 5. 0 (L) FEV 1/ FVC 78% Volume (L) FVC FEV 1 Time (s) 40
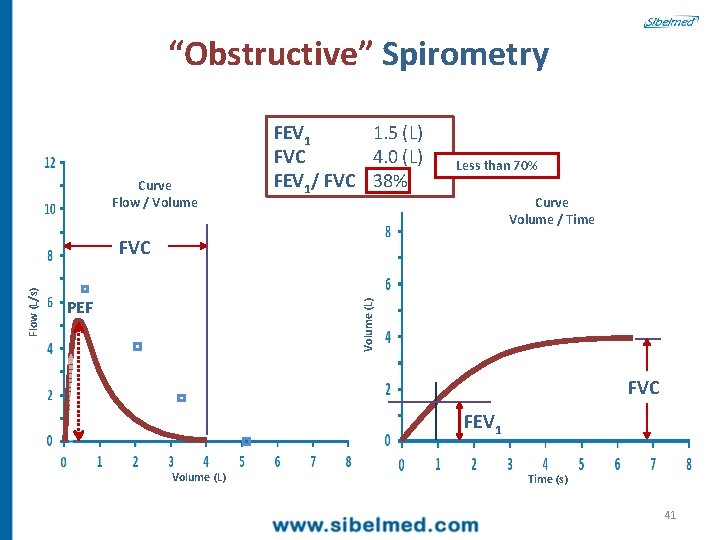
“Obstructive” Spirometry Curve Flow / Volume FEV 1 1. 5 (L) FVC 4. 0 (L) FEV 1/ FVC 38% Less than 70% Curve Volume / Time PEF Volume (L) Flow (L/s) FVC FEV 1 Volume (L) Time (s) 41
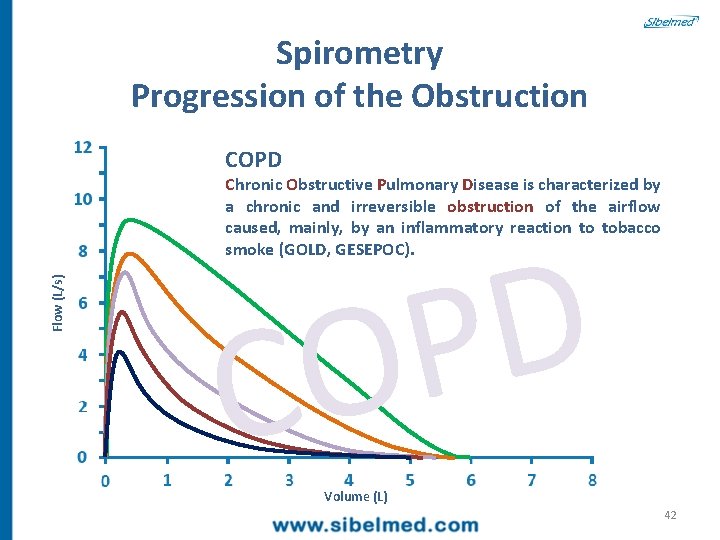
Spirometry Progression of the Obstruction COPD Flow (L/s) Chronic Obstructive Pulmonary Disease is characterized by a chronic and irreversible obstruction of the airflow caused, mainly, by an inflammatory reaction to tobacco smoke (GOLD, GESEPOC). D P O C Volume (L) 42
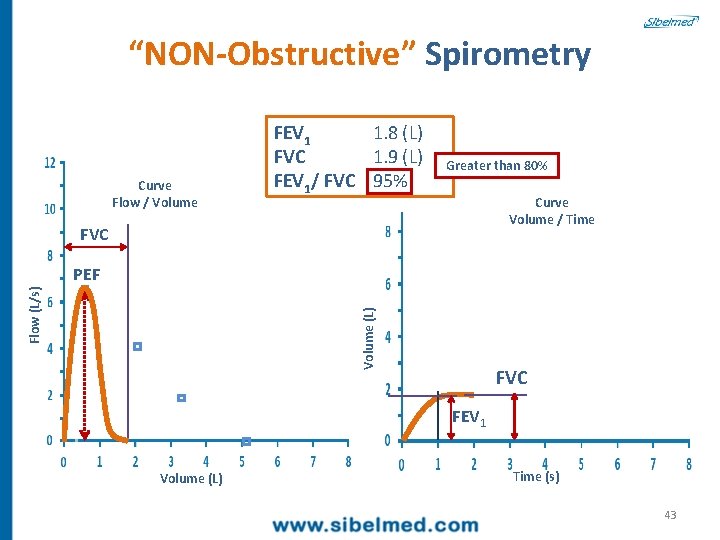
“NON-Obstructive” Spirometry Curve Flow / Volume FEV 1 1. 8 (L) FVC 1. 9 (L) FEV 1/ FVC 95% Greater than 80% Curve Volume / Time FVC Volume (L) Flow (L/s) PEF FVC FEV 1 Volume (L) Time (s) 43
Instructions and Limitations 44
Instructions • Evaluation of the respiratory capacity whenever there are respiratory symptoms. • Assessment of the respiratory impact of illnesses relating to other organs or systems (heart, kidney, liver or neuromuscular disease, etc. ). • Respiratory functional disorder screening in relation to possible health-risk diseases (tobacco, work related factors, allergic processes, etc. ). • Evaluation of the risks derived from surgical procedures. • Evaluation of the presence of respiratory disorders on request from professional incapacity or other types of legal evaluations. • Assessment of therapeutic response in view of different pharmaceuticals or clinical pharmacological trials • Epidemiological studies. 45
Limitations • Oral injuries. • Facial hemiparesis. • Nausea when introducing the mouthpiece or pneumotachometer. • In poorly-treated tracheotomies or with excessive secretions. Contraindications • Mentally or physically impossibility to correctly perform a forced maneuver. • Chest pain, pneumothorax, hemoptysis. • Unstable angor. • Retinal detachment. • Litigant patient behavior. 46
Reference Values (Also denoted THEORETICAL) 47
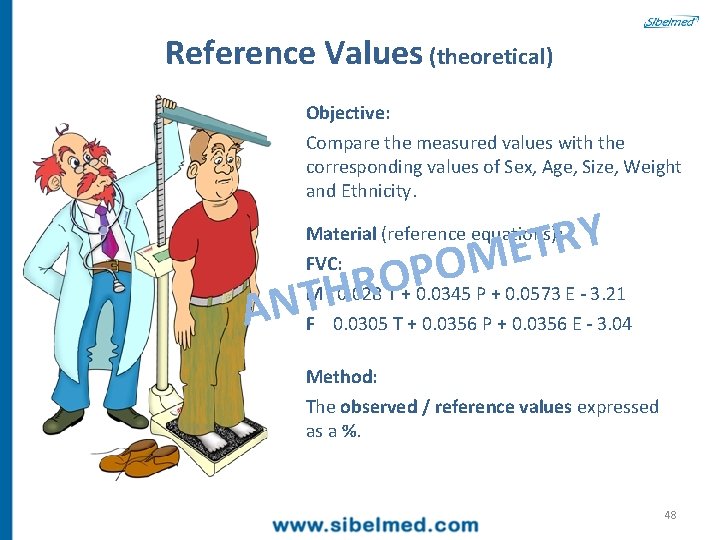
Reference Values (theoretical) Objective: Compare the measured values with the corresponding values of Sex, Age, Size, Weight and Ethnicity. Y R T E M O Material (reference equations): AN P O THR FVC: M 0. 028 T + 0. 0345 P + 0. 0573 E - 3. 21 F 0. 0305 T + 0. 0356 P + 0. 0356 E - 3. 04 Method: The observed / reference values expressed as a %. 48
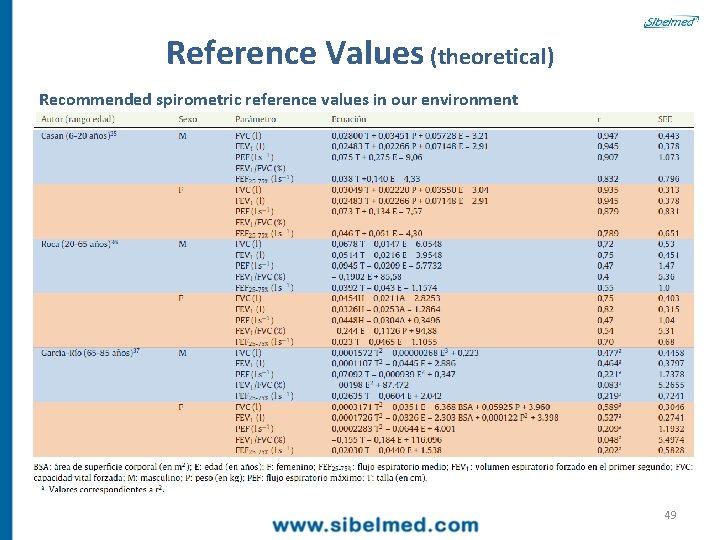
Reference Values (theoretical) Recommended spirometric reference values in our environment 49
Parameter Measuring Method 50
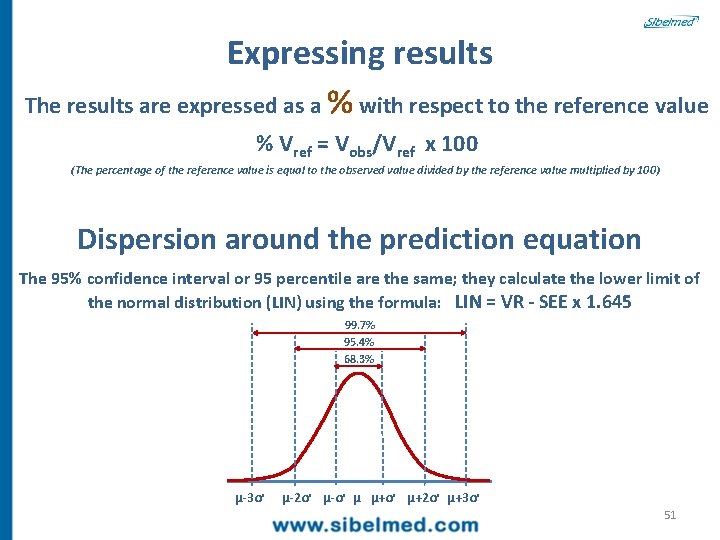
Expressing results The results are expressed as a % with respect to the reference value % Vref = Vobs/Vref x 100 (The percentage of the reference value is equal to the observed value divided by the reference value multiplied by 100) Dispersion around the prediction equation The 95% confidence interval or 95 percentile are the same; they calculate the lower limit of the normal distribution (LIN) using the formula: LIN = VR - SEE x 1. 645 99. 7% 95. 4% 68. 3% µ-3ơ µ-2ơ µ-ơ µ µ+ơ µ+2ơ µ+3ơ 51
Performing Spirometry 52
Decalogue for Performing Spirometry 1 TRAINING 2 QUALITY CONTROL the expert that will perform the spirometry and having notions of respiratory pathologies. Daily verification, with a known pattern, the correct operation of the spirometer, since this proves that it is functioning within the established limits. The daily verification and/or calibration (with a syringe of at least three liters) ensures verifiable quality control and confirms professional good practice. 53

Objective: Quality control (calibration) • To establish a relationship between the pattern unit (syringe) and the degrees of measurement. Material: • Syringe (At least three liters). • Weather station (Quality spirometers already have one incorporated; otherwise, use conventional wall or desktop stations). 54
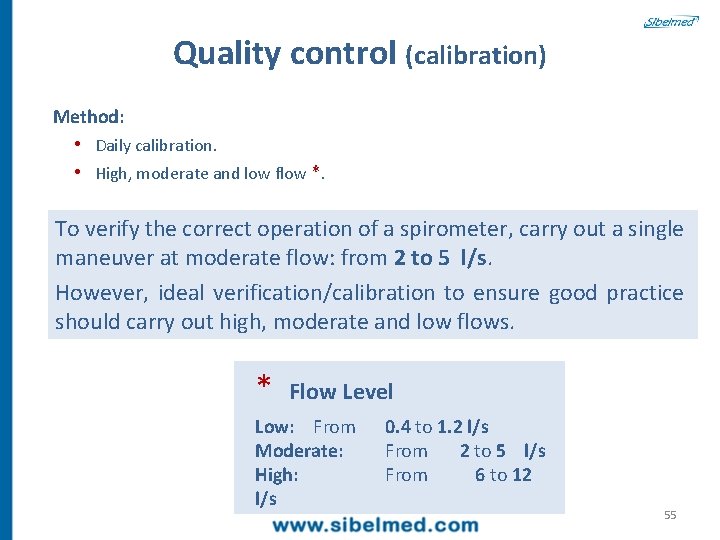
Quality control (calibration) Method: • Daily calibration. • High, moderate and low flow *. To verify the correct operation of a spirometer, carry out a single maneuver at moderate flow: from 2 to 5 l/s. However, ideal verification/calibration to ensure good practice should carry out high, moderate and low flows. * Flow Level Low: From Moderate: High: l/s 0. 4 to 1. 2 l/s From 2 to 5 l/s From 6 to 12 55
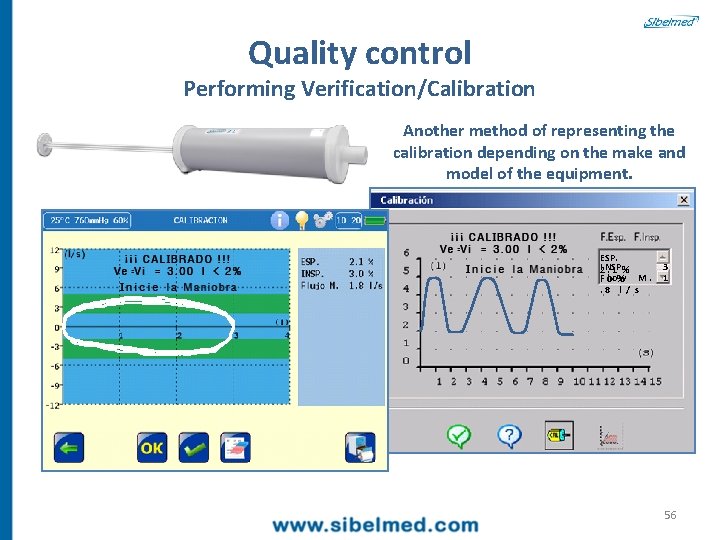
Quality control Performing Verification/Calibration Another method of representing the calibration depending on the make and model of the equipment. ESP. I NSP. 3 2. 1 % F l o w M. 1 . 0 %. 8 l / s 56
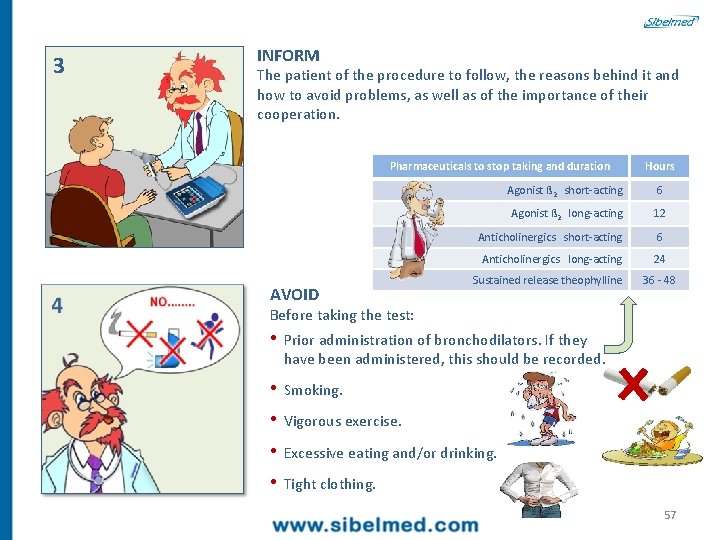
3 INFORM The patient of the procedure to follow, the reasons behind it and how to avoid problems, as well as of the importance of their cooperation. Pharmaceuticals to stop taking and duration AVOID Hours Agonist ß 2 short-acting 6 Agonist ß 2 long-acting 12 Anticholinergics short-acting 6 Anticholinergics long-acting 24 Sustained release theophylline 36 - 48 Before taking the test: • Prior administration of bronchodilators. If they have been administered, this should be recorded. • Smoking. • Vigorous exercise. • Excessive eating and/or drinking. • Tight clothing. 57
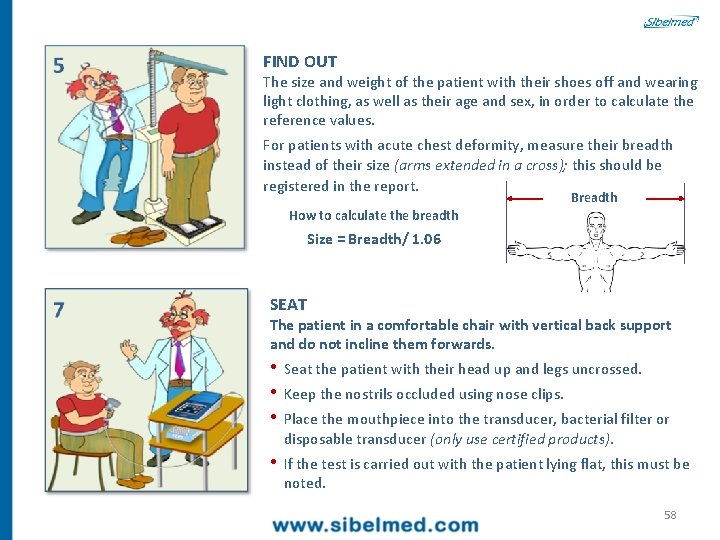
FIND OUT The size and weight of the patient with their shoes off and wearing light clothing, as well as their age and sex, in order to calculate the reference values. For patients with acute chest deformity, measure their breadth instead of their size (arms extended in a cross); this should be registered in the report. Breadth How to calculate the breadth Size = Breadth/ 1. 06 SEAT The patient in a comfortable chair with vertical back support and do not incline them forwards. • Seat the patient with their head up and legs uncrossed. • Keep the nostrils occluded using nose clips. • Place the mouthpiece into the transducer, bacterial filter or disposable transducer (only use certified products). • If the test is carried out with the patient lying flat, this must be noted. 58
EXPLAIN In a clear and simple way how to perform the spirometry maximum and forced maneuvers. 1. Inhale as much as possible 2. Place the mouthpiece into your mouth 3. Blow: 1. STRONGLY 2. CONTINUALLY 3. WITHOUT STOPPING UNTIL I SAY SO: it may seem that there is no more air to come out, but there is, I control it through the screen 59
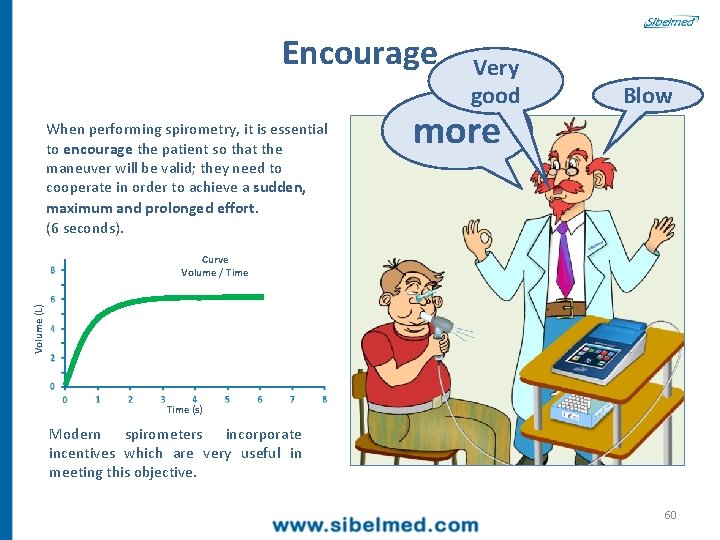
Encourage When performing spirometry, it is essential to encourage the patient so that the maneuver will be valid; they need to cooperate in order to achieve a sudden, maximum and prolonged effort. (6 seconds). Very good more Blow Volume (L) Curve Volume / Time (s) Modern spirometers incorporate incentives which are very useful in meeting this objective. 60
PERFORM 1. A slow, maximum inhalation, pause < 1 sec. 2. Maximum expiration, quick and forced with a sudden start. • Perform a minimum of 3 and a maximum of 8 maneuvers, ensuring that 2 of them are error-free and that the FVC and the FEV 1 differences are less than 5% or 150 ml (100 if the FVC is less than 1 liter). • The duration time for each maneuver should not be less than 6 seconds (3 seconds for children). 3. Check the lines. 61
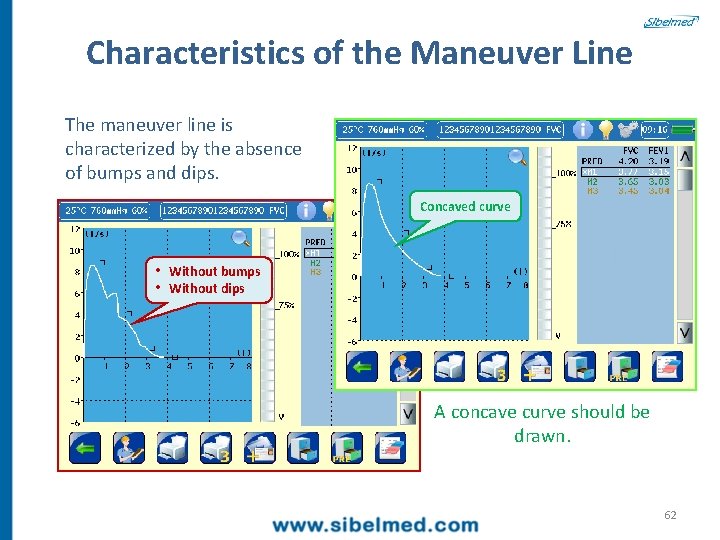
Characteristics of the Maneuver Line The maneuver line is characterized by the absence of bumps and dips. Concaved curve • Without bumps • Without dips A concave curve should be drawn. 62
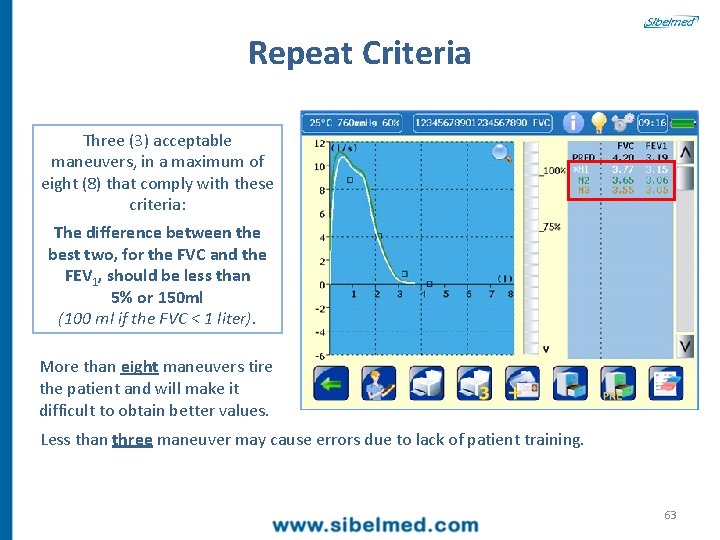
Repeat Criteria Three (3) acceptable maneuvers, in a maximum of eight (8) that comply with these criteria: The difference between the best two, for the FVC and the FEV 1, should be less than 5% or 150 ml (100 ml if the FVC < 1 liter). More than eight maneuvers tire the patient and will make it difficult to obtain better values. Less than three maneuver may cause errors due to lack of patient training. 63
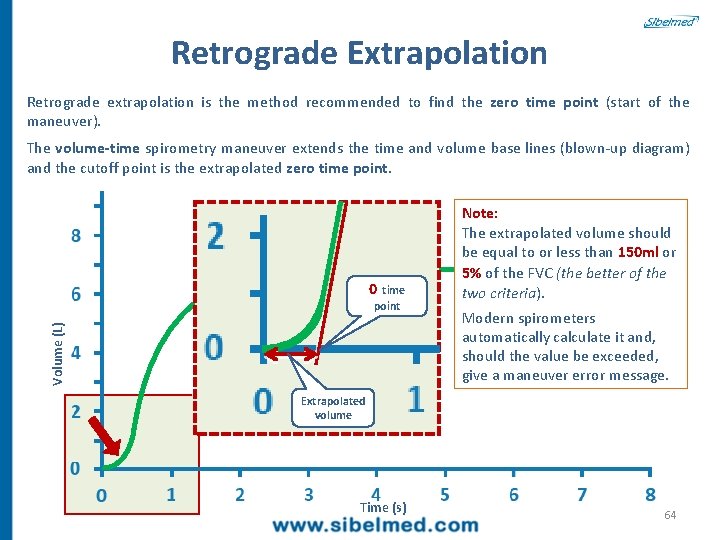
Retrograde Extrapolation Retrograde extrapolation is the method recommended to find the zero time point (start of the maneuver). The volume-time spirometry maneuver extends the time and volume base lines (blown-up diagram) and the cutoff point is the extrapolated zero time point. 0 time Volume (L) point Note: The extrapolated volume should be equal to or less than 150 ml or 5% of the FVC (the better of the two criteria). Modern spirometers automatically calculate it and, should the value be exceeded, give a maneuver error message. Extrapolated volume Time (s) 64
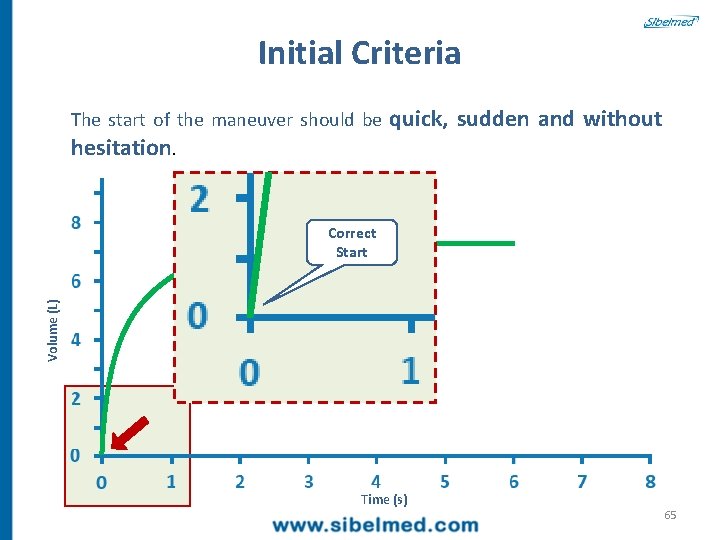
Initial Criteria The start of the maneuver should be quick, sudden and without hesitation. Volume (L) Correct Start Time (s) 65
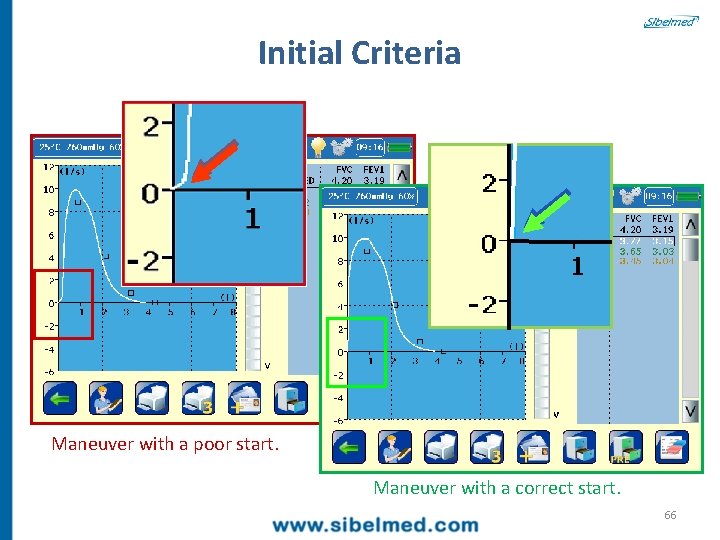
Initial Criteria Maneuver with a poor start. Maneuver with a correct start. 66
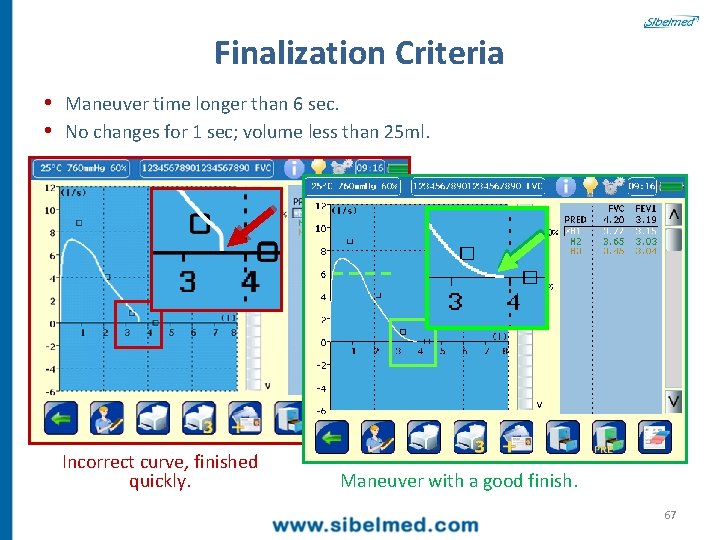
Finalization Criteria • Maneuver time longer than 6 sec. • No changes for 1 sec; volume less than 25 ml. Incorrect curve, finished quickly. Maneuver with a good finish. 67
9 SELECT The best FVC and FEV 1 values even if they come from different maneuvers; but they meet the previous criteria. The rest of the parameters are taken from the maneuver with the greater sum of FVC and FEV 1. 68
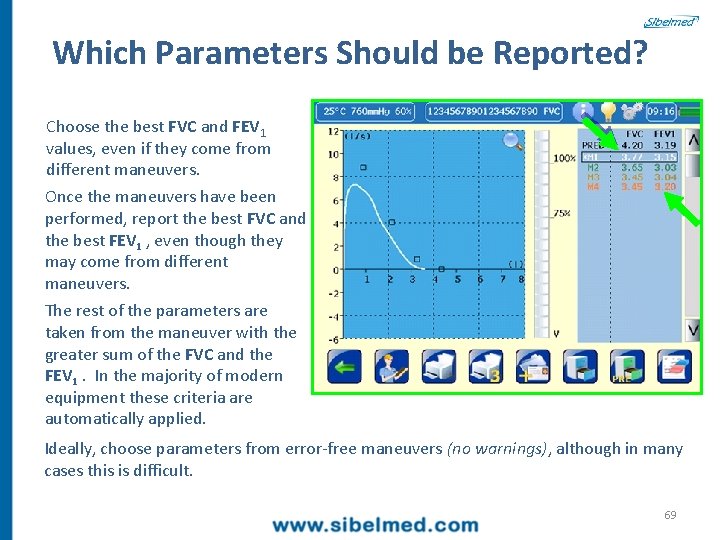
Which Parameters Should be Reported? Choose the best FVC and FEV 1 values, even if they come from different maneuvers. Once the maneuvers have been performed, report the best FVC and the best FEV 1 , even though they may come from different maneuvers. The rest of the parameters are taken from the maneuver with the greater sum of the FVC and the FEV 1. In the majority of modern equipment these criteria are automatically applied. Ideally, choose parameters from error-free maneuvers (no warnings), although in many cases this is difficult. 69
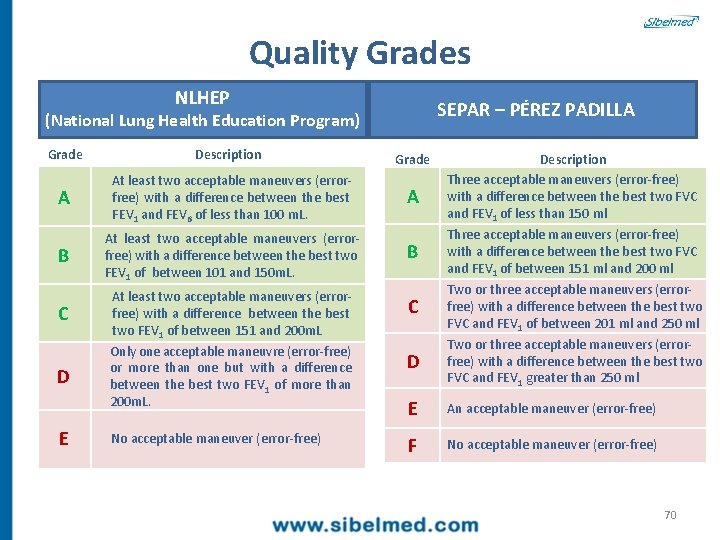
Quality Grades NLHEP SEPAR – PÉREZ PADILLA (National Lung Health Education Program) Grade Description A At least two acceptable maneuvers (errorfree) with a difference between the best FEV 1 and FEV 6 of less than 100 m. L. B At least two acceptable maneuvers (errorfree) with a difference between the best two FEV 1 of between 101 and 150 m. L. C D E At least two acceptable maneuvers (errorfree) with a difference between the best two FEV 1 of between 151 and 200 m. L Only one acceptable maneuvre (error-free) or more than one but with a difference between the best two FEV 1 of more than 200 m. L. No acceptable maneuver (error-free) Grade A Description Three acceptable maneuvers (error-free) with a difference between the best two FVC and FEV 1 of less than 150 ml B Three acceptable maneuvers (error-free) with a difference between the best two FVC and FEV 1 of between 151 ml and 200 ml C Two or three acceptable maneuvers (errorfree) with a difference between the best two FVC and FEV 1 of between 201 ml and 250 ml D Two or three acceptable maneuvers (errorfree) with a difference between the best two FVC and FEV 1 greater than 250 ml E An acceptable maneuver (error-free) F No acceptable maneuver (error-free) 70

Bronchodilation test Contracted smooth muscle Inhale bronchodilator Air trapped in the alveolus Relaxed smooth muscle Inflamed and swollen wall Airway in asthma Bronchodilated airway 4 inhalations (with camera) PRE POST PARAMETER PRE REF (%) POST (%) FVC 3. 21 3. 89 85 3. 56 7 FEV 1 2. 32 3. 14 74 2. 65 13 FEV 1/FVC 69. 91 79. 38 88 74. 37 6 The test is considered positive if it produces an increase equal to or greater than: • FVC: 12% or FEV 1: 12% • and additionally, a minimum of 200 ml 71
10 CLEANING Given that the transducer is directly exposed to the patient, it must be kept in perfect physical and hygienic conditions. Clean and disinfect it as per the manufacturer's instructions. If this is not possible use soap and water and, wherever possible, sterilize periodically the pieces exposed to the patient. For potentially contagious patients (HIV+, hepatitis C, pulmonary tuberculosis, etc. ), use single-use pneumotachometers or carry out the test at the end of the day using antibacterial filters. Then, proceed to clean it thoroughly. 72

Thank You Let's Begin 73
- Slides: 73