Welcome to CUSP Communication Teamwork Tools Coaching Call



- Slides: 23
Welcome to CUSP Communication & Teamwork Tools Coaching Call 3 The session will begin shortly. To access the audio for the session, Dial: 800 -977 -8002, Participant code 083842#. The materials for this coaching call can be downloaded from the CUSP Communication & Teamwork Tools password-protected web page. Directions for how to access this web page can be found on each of the coaching call meeting notices (appointments) sent to you. The phone lines will be open during the presentation. Please keep your phone on mute unless you are asking a question. If you do not have a mute function on your phone, you can press *6 to mute your phone (and *6 again to unmute if you want to ask a question). PLEASE DO NOT PUT YOUR PHONE ON HOLD!!! If you experience any problems, please call Marilyn Nichols at the MOCPS office at 573 -636 -1014, ext 221 or mnichols@mocps. org.
Document 1 CUSP Communication & Teamwork Tools Coaching Call 3: Hardwiring Multidisciplinary Rounds with Daily Goals; Sample Huddles August 16, 2011 Pat Posa RN, BSN, MSA System Performance Improvement Leader St. Joseph Mercy Health System Ann Arbor, MI patposa@comcast. net Kimberly O’Brien, MHA Project Manager Missouri Center for Patient Safety Jefferson City, MO kobrien@mocps. org
Documents for this Session (All can downloaded from the CUSP Communication & Teamwork Tools password-protected web site. Detailed instructions are located on each of the coaching call meeting notices/appointments emailed to you by Kimberly O’Brien) 1. 2. 3. 4. 5. 3 This Power. Point presentation Monthly Team Leader Checklist Sample Agenda for August CUSP Team Meeting Sample MDR and huddle An audio file recording of this session will be emailed to you shortly after the call today
Agenda • Multidisciplinary Rounds with Daily Goals – – Review action plan status Creating rounding tool Questions –struggles—strategies Setting up a pilot/test of change • Structured Huddles – – 4 Review action plan status Questions--struggle—strategies Defining metrics Setting up pilot/test of change
CUSP Communication & Teamwork Tools Interventions ØMultidisciplinary Rounds with Daily Goals ØStructured Huddles 5
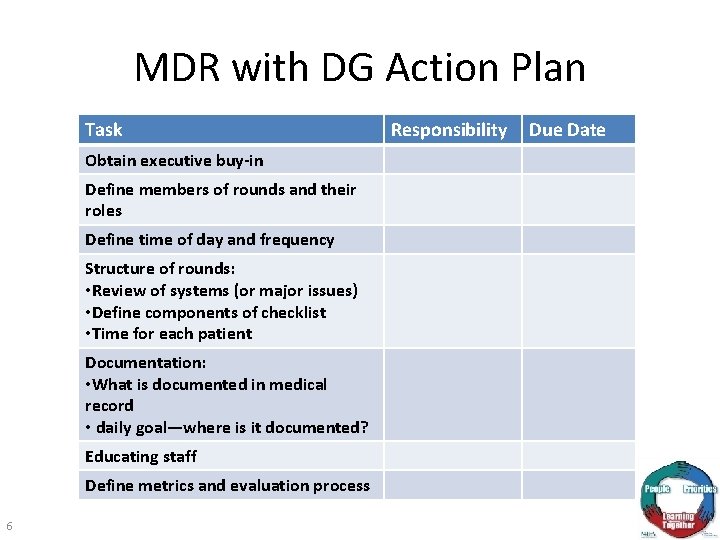
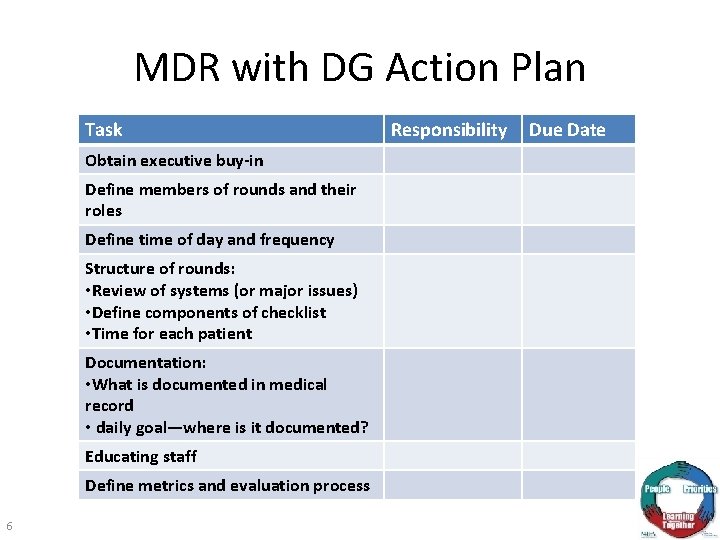
MDR with DG Action Plan Task Obtain executive buy-in Define members of rounds and their roles Define time of day and frequency Structure of rounds: • Review of systems (or major issues) • Define components of checklist • Time for each patient Documentation: • What is documented in medical record • daily goal—where is it documented? Educating staff Define metrics and evaluation process 6 Responsibility Due Date
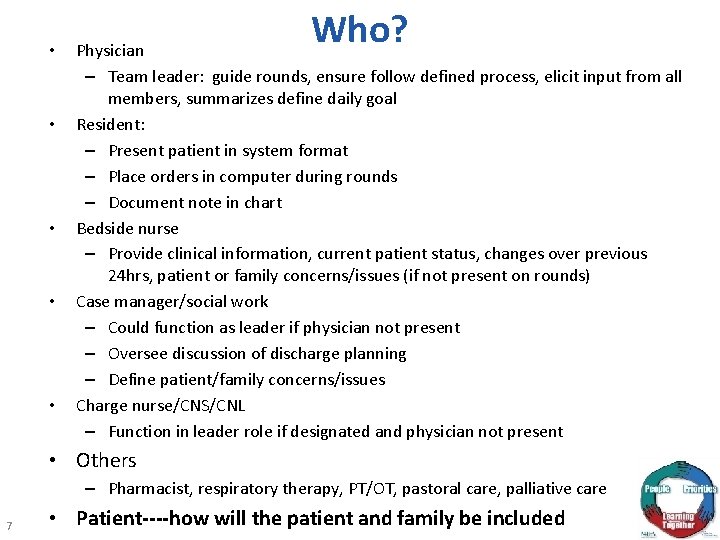
• • • Who? Physician – Team leader: guide rounds, ensure follow defined process, elicit input from all members, summarizes define daily goal Resident: – Present patient in system format – Place orders in computer during rounds – Document note in chart Bedside nurse – Provide clinical information, current patient status, changes over previous 24 hrs, patient or family concerns/issues (if not present on rounds) Case manager/social work – Could function as leader if physician not present – Oversee discussion of discharge planning – Define patient/family concerns/issues Charge nurse/CNS/CNL – Function in leader role if designated and physician not present • Others – Pharmacist, respiratory therapy, PT/OT, pastoral care, palliative care 7 • Patient----how will the patient and family be included
Structure of MDR • Time of day • Frequency • Process for each patient – Checklist • Documenting – Which pieces of rounds? – Daily goal • Define daily goal follow up process 8 8
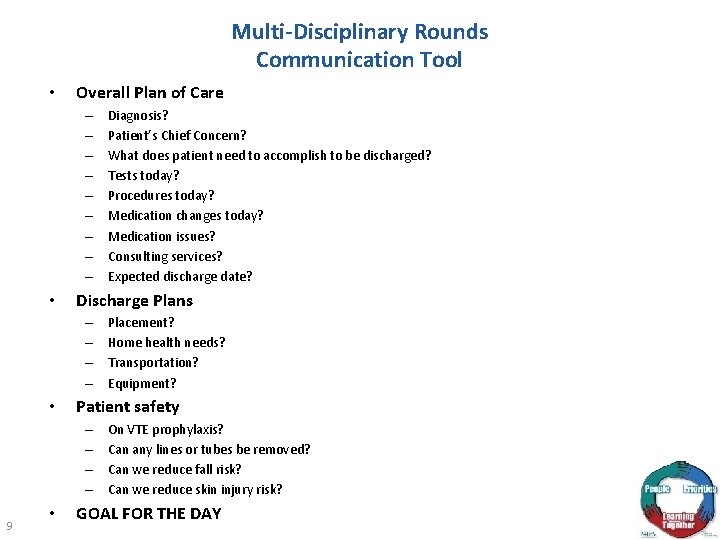
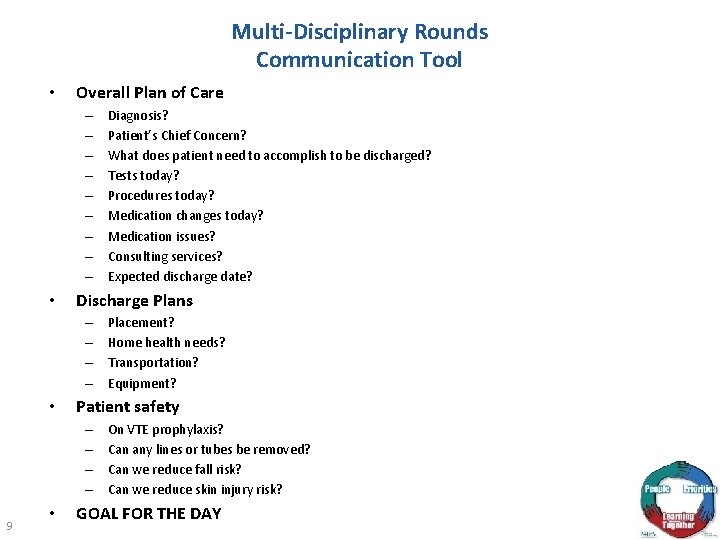
Multi-Disciplinary Rounds Communication Tool • Overall Plan of Care – – – – – • Discharge Plans – – • • Placement? Home health needs? Transportation? Equipment? Patient safety – – 9 Diagnosis? Patient’s Chief Concern? What does patient need to accomplish to be discharged? Tests today? Procedures today? Medication changes today? Medication issues? Consulting services? Expected discharge date? On VTE prophylaxis? Can any lines or tubes be removed? Can we reduce fall risk? Can we reduce skin injury risk? GOAL FOR THE DAY 9
Where are you struggling? • Buy-in? Physician? Nurses? • Defining roles? • Creating structure/checklist? 10 10
Test of Change • One nurse, one physician, one day, one patient • Test the roles and process(checklist) • Get feedback – Observe rounds – Survey participants • Make revisions 11 11

Evaluate Attending: Resident: RN: Intern: Circle others in attendance: Pharmacy Nutrition Respiratory Therapy CNL Room #: _________ Rounding outside patient room: yes no Nursing notified: yes no n/a Nursing present during rounds: yes no RT present during rounds: yes no Checklist followed as outlined: yes no (If no, what objectives were omitted) _____________________ Sepsis screen, sepsis bundles reviewed/signed by team: yes no Daily goals in room board updated by intern: yes no Plan of care/daily goals clarified with team: yes no Nursing questions/concerns addressed: yes no n/a Physician questions/concerns addressed: yes no n/a Patient/family questions/concerns addressed: yes no n/a Were team members listening to each other: yes no Did leaders ask others for input: yes no Feedback to team members (professionalism, team interaction, timeliness, efficiency, thoroughness, organization and clarity): _____________________________________________________ Was criticism positively presented: yes no 12 12

Evaluate • Survey participants: (5 point scale) – Was your voice/opinions heard and valued? – Did you have a understanding of what the goals and plan for the patient was for the day? – Did the leader facilitate the rounds to ensure efficiency and open communication? – Did MDR with DG improve how you cared for your patient? – What worked? – What could be improved? 13 13
Structured Huddles • Enable teams to have frequent but short briefings so that they can stay informed, review work, make plans, and move ahead rapidly. • Allow fuller participation of front-line staff and bedside caregivers, who often find it impossible to get away for the conventional hour-long improvement team meetings. • They keep momentum going, as teams are able to meet more frequently. Use this strategy to begin to recovery immediately from defects---IE: falls, sepsis and daily to focus on unit outcomes 14
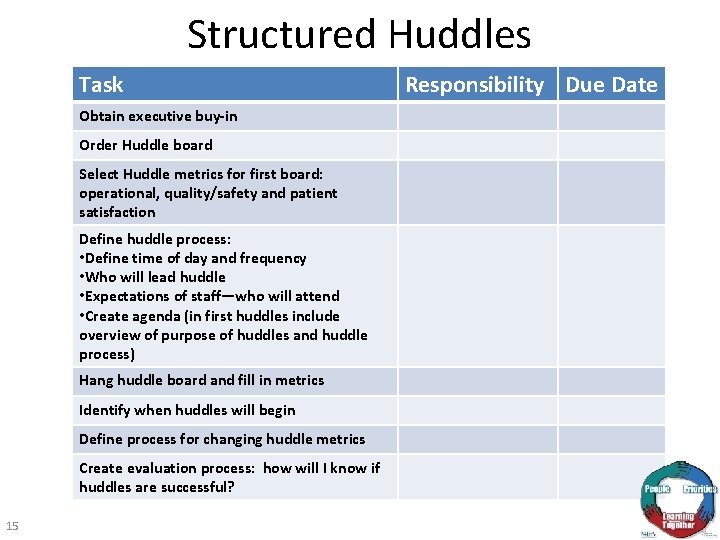
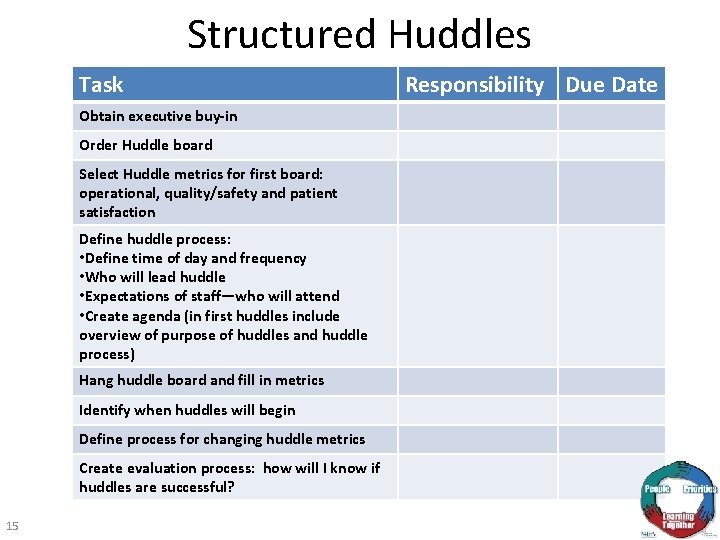
Structured Huddles Task Obtain executive buy-in Order Huddle board Select Huddle metrics for first board: operational, quality/safety and patient satisfaction Define huddle process: • Define time of day and frequency • Who will lead huddle • Expectations of staff—who will attend • Create agenda (in first huddles include overview of purpose of huddles and huddle process) Hang huddle board and fill in metrics Identify when huddles will begin Define process for changing huddle metrics Create evaluation process: how will I know if huddles are successful? 15 Responsibility Due Date
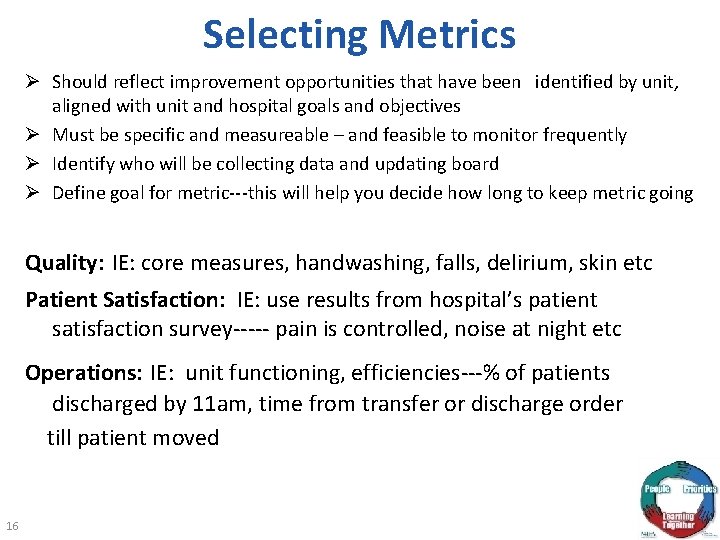
Selecting Metrics Ø Should reflect improvement opportunities that have been identified by unit, aligned with unit and hospital goals and objectives Ø Must be specific and measureable – and feasible to monitor frequently Ø Identify who will be collecting data and updating board Ø Define goal for metric---this will help you decide how long to keep metric going Quality: IE: core measures, handwashing, falls, delirium, skin etc Patient Satisfaction: IE: use results from hospital’s patient satisfaction survey----- pain is controlled, noise at night etc Operations: IE: unit functioning, efficiencies---% of patients discharged by 11 am, time from transfer or discharge order till patient moved 16 16
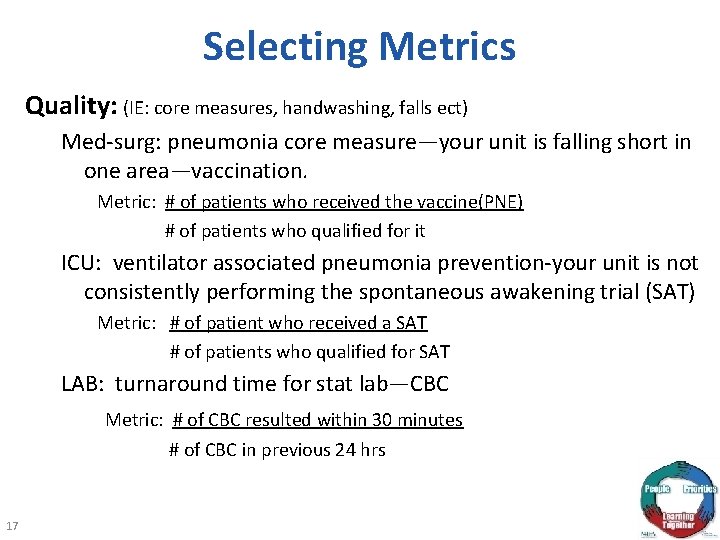
Selecting Metrics Quality: (IE: core measures, handwashing, falls ect) Med-surg: pneumonia core measure—your unit is falling short in one area—vaccination. Metric: # of patients who received the vaccine(PNE) # of patients who qualified for it ICU: ventilator associated pneumonia prevention-your unit is not consistently performing the spontaneous awakening trial (SAT) Metric: # of patient who received a SAT # of patients who qualified for SAT LAB: turnaround time for stat lab—CBC Metric: # of CBC resulted within 30 minutes # of CBC in previous 24 hrs 17 17
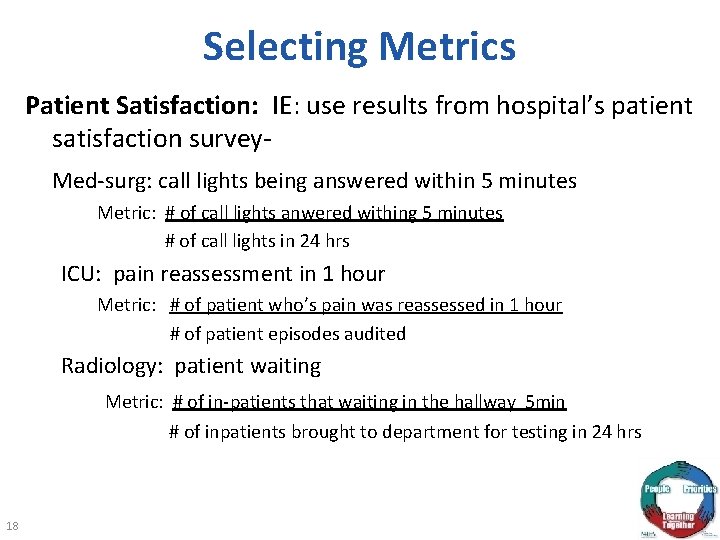
Selecting Metrics Patient Satisfaction: IE: use results from hospital’s patient satisfaction survey- Med-surg: call lights being answered within 5 minutes Metric: # of call lights anwered withing 5 minutes # of call lights in 24 hrs ICU: pain reassessment in 1 hour Metric: # of patient who’s pain was reassessed in 1 hour # of patient episodes audited Radiology: patient waiting Metric: # of in-patients that waiting in the hallway 5 min # of inpatients brought to department for testing in 24 hrs 18 18

Selecting Metrics Operations: IE: unit functioning, efficiencies- Med-surg: percent of patients discharged by 11 am Metric: # patients discharged by 11 am # of patients with discharge orders in place before 11 am ICU: delirium assessment Metric: # of patient with 2 documented CAM-ICU in last 24 hours # of patient in ICU Radiology: no show rate Metric: # of out patients that miss schedule appointment # of outpatients scheduled for testing in 24 hrs 19 19
Where are you struggling? • Buy-in? Physician? Nurses? • Picking best time of day? • Creating metrics? 20 20
CUSP Communication & Teamwork Tools Next Steps • Multidisciplinary Rounds – Complete action plan and a test of change • Structured Huddles – Complete action plan – Define first metric and do a practice huddle on one shift, one day • Learning from a Defect – Identify next defect to solve (if haven’t done it yet) – Begin/complete through LFD steps • CUSP Team Agenda – Choose next defect to take through the Learning from a Defect Tool or begin LFD process – Complete MDR with DG action plan – Show video’s of structured huddle; get feedback/questions from CUSP team and unit leadership for next Coaching Call – Ensure that concepts of Multidisciplinary Rounds and Structured Huddles are vetted by executive sponsor for unit and VPMA/CMO 21
We Are On a Continuous Journey • We have toolkits, manuals, websites, and monthly calls to learn from and with each other. • Your job is to join the calls, share with us your successes and more importantly the barriers you face. • Commit to the premise that harm is untenable. 22
Questions? 23