WEEK 7 PSYCHOSOCIAL FACTORS THAT IMPACT AN INDIVIDUAL
- Slides: 94
WEEK 7: PSYCHOSOCIAL FACTORS THAT IMPACT AN INDIVIDUAL WITH A DISABILITY Special Topics in Rehabilitation: REH 6560
Assignment 7 has been posted to the Course Website Reading Assignment for Week 7 has been posted to the Course Website
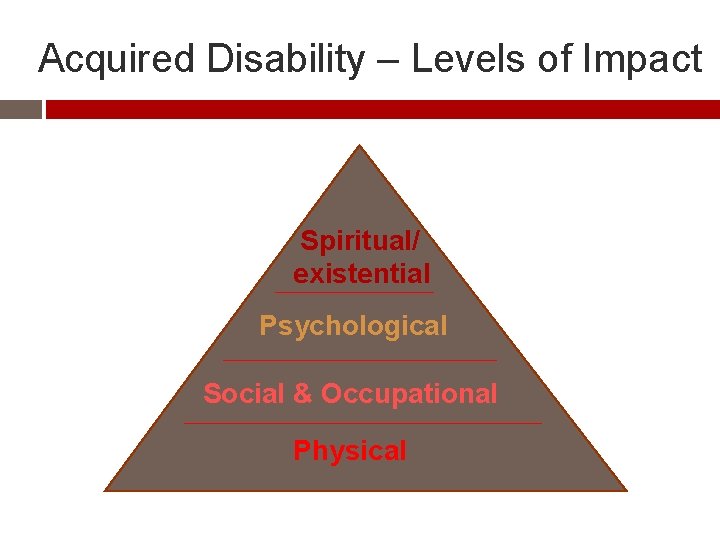
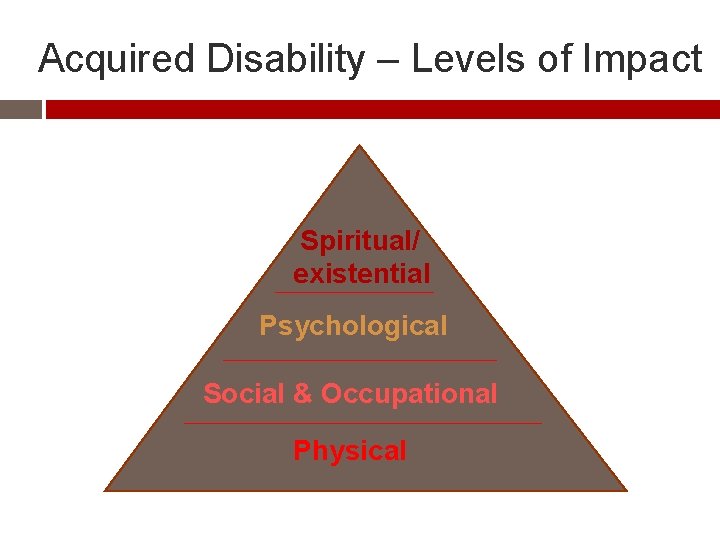
Acquired Disability – Levels of Impact Spiritual/ existential Psychological Social & Occupational Physical
Adjustment Issues with Acquired Disability (AD) Physical – being unable to cope with functional aspects of disability, loss of control of basic physical functions, pain, health changes
Adjustment Issues with Acquired Disability (AD) Social – difficulty with losing activities that give sense of pleasure & identity & achievement, finding new ones & coping with changed relationships with family, friends & sexual partners, loneliness & isolation
Adjustment Issues with Acquired Disability (AD) Occupational – difficulty revising educational & career plans or finding new job Emotional – high levels of denial, anxiety, grief, depression, aggression against staff
Adjustment Issues with Acquired Disability (AD) Motivational – failure to comply with therapist- & self-management, loss of initiative Self-conceptual – inability to accept changed body image, self-esteem, levels of competence
Adjustment Issues with Acquired Disability (AD) Existential/spiritual – Without sense of meaning & purpose AD can be an unbearable burden. When usual sources threatened or diminished “Why go on? ” questions arise
Psychosocial Impact is Critical 1. High prevalence of psychological distress in AD - wrought by often seemingly intolerable, devastating changes & adversities Most of those who treat, work & live with those with AD share humanitarian concern to prevent or reduce this distress & social impacts
Psychosocial Impact is Critical But veterans with psychosocial adjustment problems can distress health careers, often because veterans misunderstood – can be poorly serviced as result – in turn resulting in high dissatisfaction with rehab
Psychosocial Impact is Critical 2. Distress adds to existing impacts upon work, personal relations, leisure & social activities & so well-being & Quality of Life suffers - Sets up ‘vicious cycle’ effect
Psychosocial Impact is Critical 3. Unmanaged psychosocial adjustment problems interfere with self-care & physical rehab - One of most significant barriers to rehab outcomes!
Psychosocial Impact is Critical 4. Left unattended, psychological & social effects usually worsen. Costs increase, both emotionally & financially e. g. repeated health service utilization
ADJUSTING Goal: Awareness of impact of AD on specific aspects of psychosocial functioning of individual & family & friends
Initial Reactions to AD Early responses to AD usually involve mixture of anxiety & depressed mood Worry & uncertainty about ability to cope with changes - usually high in early stages & short bursts Diagnoses can produce shock & denial
Initial Reactions to AD Denial & other avoidance strategies can be useful to help absorb the shock In excess, affects physical & psychological well-being e. g. - not absorbing or applying info that aids recovery or prevents health problems
Initial Reactions to AD Depressed mood: some say peaks shortly after diagnosis Others say when realize full extent of their disability & after many frustrating experiences Can take more than a year to fully emerge
Initial Reactions to AD Unlike anxiety which tends to appear in short-lived cycles, mood problems can be a long-term issue in AD lasting more than a year in many illnesses. Others though report cycles of despair & acceptance that can vary in length from less than 2 weeks to months
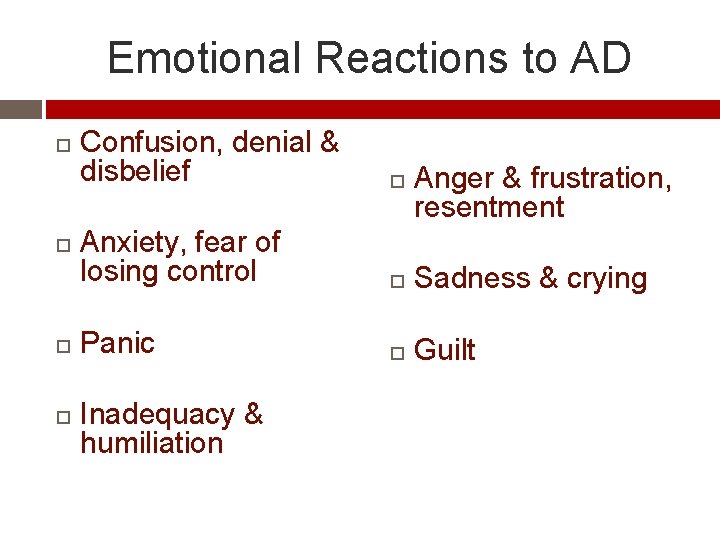
Emotional Reactions to AD Confusion, denial & disbelief Anxiety, fear of losing control Sadness & crying Panic Guilt Inadequacy & humiliation Anger & frustration, resentment
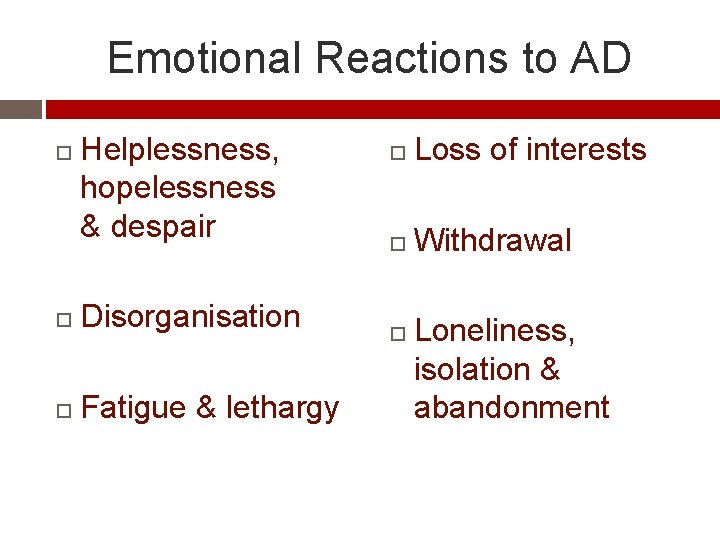
Emotional Reactions to AD Helplessness, hopelessness & despair Disorganisation Fatigue & lethargy Loss of interests Withdrawal Loneliness, isolation & abandonment
Adjusting: Family & Loved Ones Awareness of impact of acquired injury on specific aspects of psychosocial functioning of individual & family & friends
Adjusting: Family & Loved Ones Personal & environmental resources that determine reactions: Coping skills, Personalities, Beliefs & assumptions (‘schemas’), social supports – Comparisons of those who do & don’t cope
Adjusting: Family & Loved Ones Empirical & other predictors of coping Grief v. Depression
Strategies: How People Might Manage Distancing – try to detach from stress of situation (“I didn’t let it get to me. I refused to think about it too much”) Positive focus – try to see the positives in their situation/find meaning e. g. personal growth (“I came out of the experience better than when I went in”)
Strategies: How People Might Manage Seek out social support – have skills, access & receive encouragement to do so. (“The rehab people helped me find someone to talk to so I could find out more about my situation. ”)
Seek Out Social Support If done in ways that don’t drive people away, connecting with family, friends, organisations can result in people living longer, adjusting more positively, improving health habits (e. g. sticking to medical routines) & use health services appropriately
Strategies: How People Might Manage Denial is used sparingly e. g. in early stages Problem-solving focus (“I’ll figure out ways, or find out what others do, to deal with the specific effects of the condition”) on aspects of illness amenable to change but …
Strategies: How People Might Manage Use emotion-focused coping techniques (e. g. calming strategies) for aspects that can’t be controlled Flexible use of coping strategies – “try to change things I can & accept the things I can’t”
Strategies: How People Might Manage Open to ‘self-management’ view of illness that complements efforts of doctors, therapists, & carers Constructive schemas like “It’s not my fault that this happened to me. Factors outside my control lead to this illness but I do have a responsibility to help in my rehabilitation & care, as challenging as that will be. I can exert some control over the effects of this illness”
Problematic Strategies Lots of ‘escape fantasies’ or wishful/magical thinking e. g. “I wish that the situation would go away. ” Avoidance efforts – overeating, overdrinking, excessive smoking, overuse of medication Lots of self-blame, helplessness or anger/blaming others
Problematic Strategies Passive acceptance (vs. actively adjusting lifestyle to make best of situation), forgetting illness, fatalistic views of illness, withdrawal from others e. g. making doctors, pharmacy & therapists center of their world
Problematic Strategies Unable to access supportive networks in community as adjustment problems arise Unhelpful schemas e. g. about health “No pain means no problem. No need to get blood pressure checked. ”)
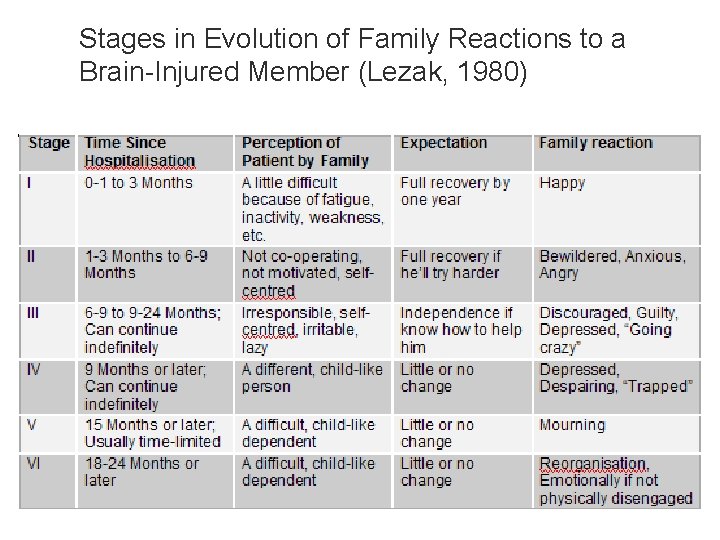
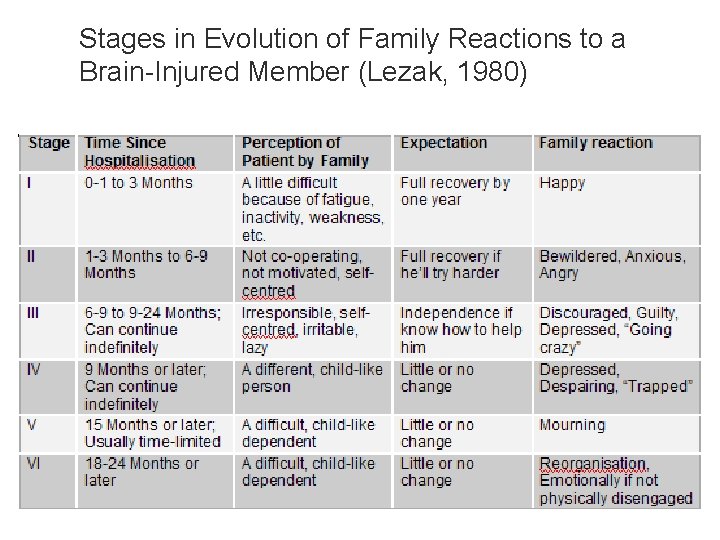
Stages in Evolution of Family Reactions to a Brain-Injured Member (Lezak, 1980)
EMPIRICAL PREDICTORS OF POOR ADJUSTMENT
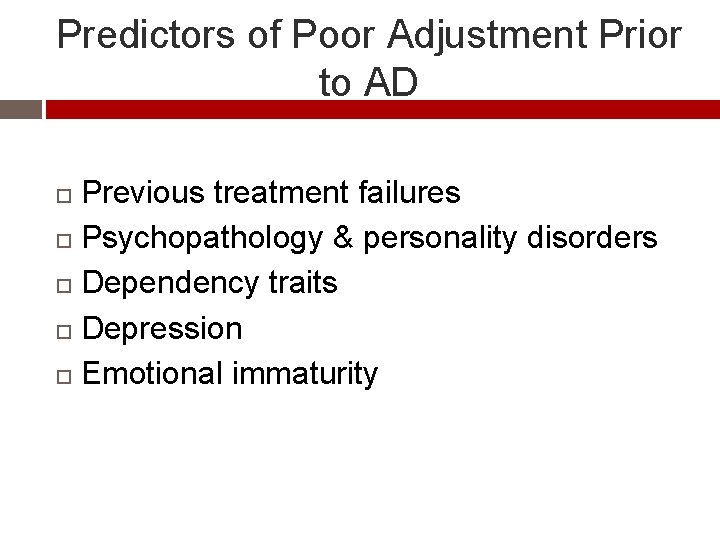
Predictors of Poor Adjustment Prior to AD Previous treatment failures Psychopathology & personality disorders Dependency traits Depression Emotional immaturity
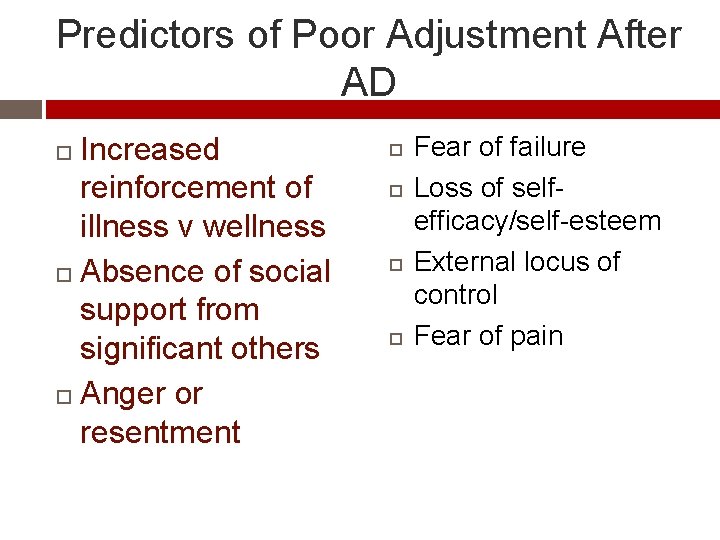
Predictors of Poor Adjustment After AD Increased reinforcement of illness v wellness Absence of social support from significant others Anger or resentment Fear of failure Loss of selfefficacy/self-esteem External locus of control Fear of pain
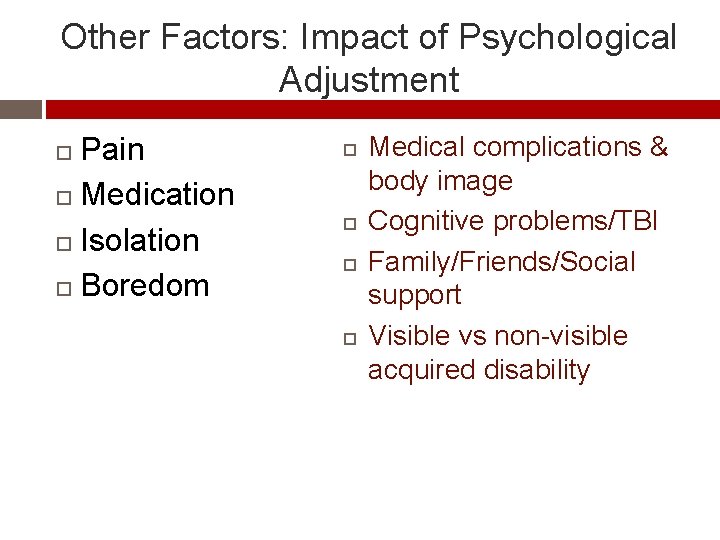
Other Factors: Impact of Psychological Adjustment Pain Medication Isolation Boredom Medical complications & body image Cognitive problems/TBI Family/Friends/Social support Visible vs non-visible acquired disability
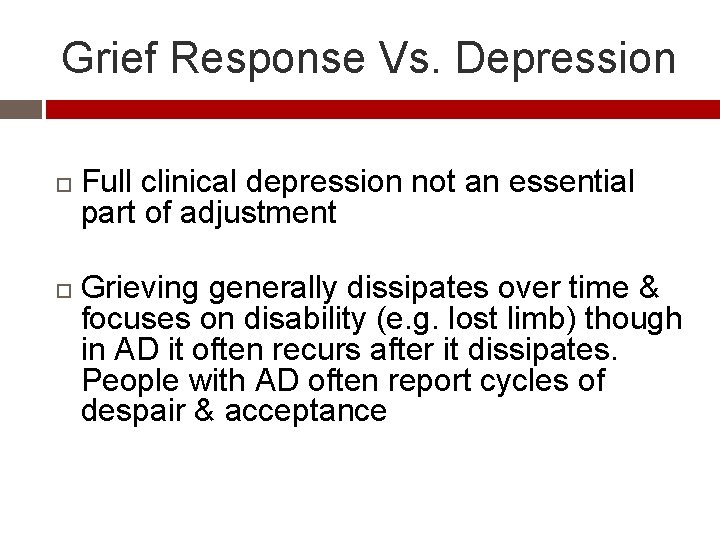
Grief Response Vs. Depression Full clinical depression not an essential part of adjustment Grieving generally dissipates over time & focuses on disability (e. g. lost limb) though in AD it often recurs after it dissipates. People with AD often report cycles of despair & acceptance
Grief Response Vs. Depression has a self-critical focus with feelings of worthlessness, hopelessness & withdrawal from others Someone with depression is seriously distressed & not coping
Phases of Grief In many forms of AD characteristics of grief, its phases & elements, should be seen as chronic & recurring – not in a time-limited, lock-step linear fashion
Phases of Grief Can set up perilous expectations for all if grief seen too simply as stages that permanently end, sooner or later ‘Failure’ to do so can oppress people into ‘adjusting’ &‘accepting the unacceptable’
Phases of Grief: Rough Outline Avoidance Confrontation Re-establishment
When Coping Doesn’t Happen These are mental health issues to be on the alert for in working with Veterans
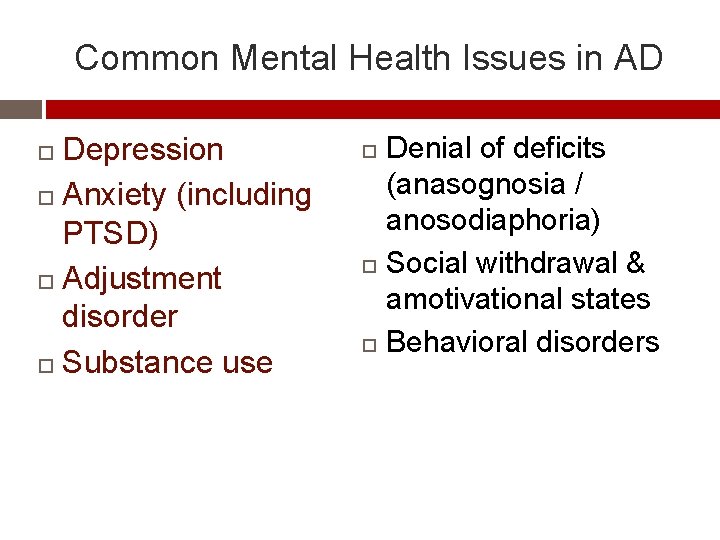
Common Mental Health Issues in AD Depression Anxiety (including PTSD) Adjustment disorder Substance use Denial of deficits (anasognosia / anosodiaphoria) Social withdrawal & amotivational states Behavioral disorders
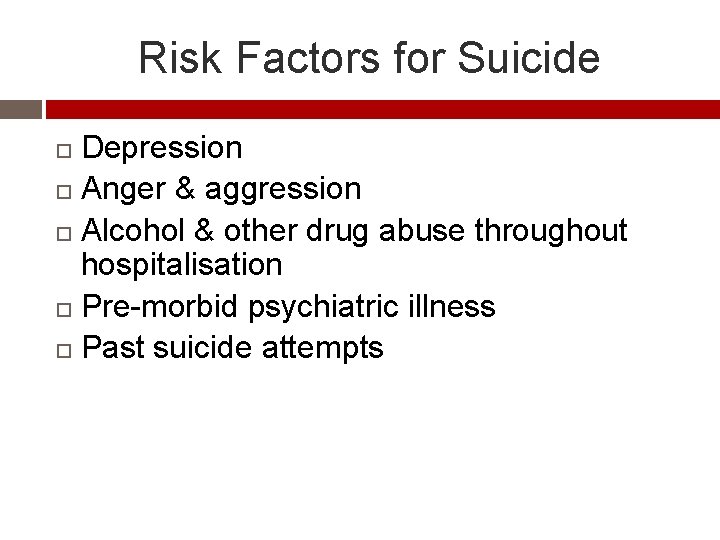
Risk Factors for Suicide Depression Anger & aggression Alcohol & other drug abuse throughout hospitalisation Pre-morbid psychiatric illness Past suicide attempts
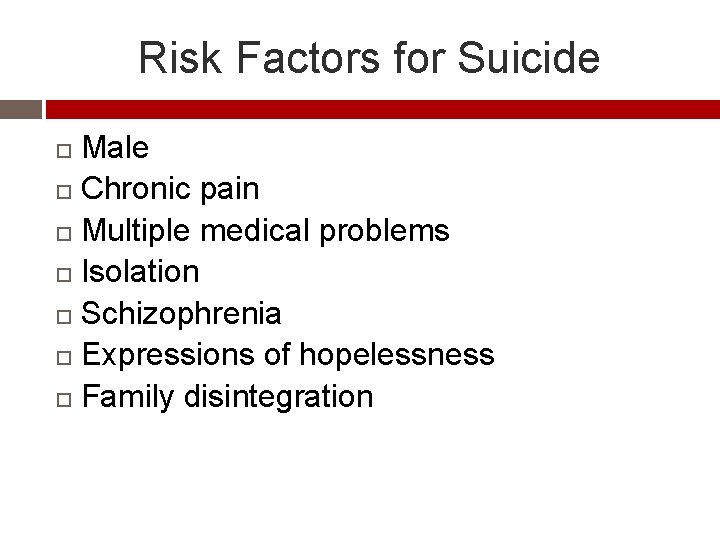
Risk Factors for Suicide Male Chronic pain Multiple medical problems Isolation Schizophrenia Expressions of hopelessness Family disintegration
Managing Potential Suicidal Behavior If an individual expresses suicidal ideation, ensure person’s immediate safety Obtain an urgent psychiatric consultation if person’s immediate safety at risk
Managing Potential Suicidal Behavior Determine appropriate setting of care Refer to treat underlying problems such as depression, substance abuse, pain, etc.
Managing Potential Suicidal Behavior Involve family & friends where possible Regular observation of the person is important Active listening by staff
Managing Potential Suicidal Behavior Encourage expression of feelings & encourage active coping In both out-patient & in-patient settings: Help with maintenance of health (e. g. hygiene, nutrition, bowel & bladder) programs while the person is in depressed state
Acute Stress Reactions in Vets Referral to General Practitioner/Psychologist/Psychiatrist for assessment Normalize reaction Encourage person to talk
Acute Stress Reactions in Vets Time Social support
Depression in Vets Referral to GP/Psychologist/Psychiatrist for assessment Individually managed treatment plan Be aware of stigma & bias against people with mental health issues
PTSD Referral to GP/Psychologist/Psychiatrist for assessment Treatment in this areas is specialized
Adjustment Disorder in Vets Offer a supportive relationship Encourage control of negative thoughts Assist & encourage problem solving Encourage involvement in positive activities Promote health maintenance
Psychosocial Intervention Strategies Veterans who adopt a self-management approach, to augment professional management, fare better with their condition Subjective experiences like degree of suffering/emotional components of pain diminish
Self-Management Skills q Self-education. q Learning as much as possible about condition. Becoming ‘expert’ at understanding & managing pain e. g. appropriate use of medication
Self-Management Skills q Adopting an internal locus of control attitude. q Open, experimental & “I control me” not “it (pain) or they (doctors) …” attitude
Self-Management Skills q Extending coping/self-care skills: q Balancing relaxation (mental, physical, behavioural skills) with activity (↑ pacing + ↑ movement + ↑ occupation)
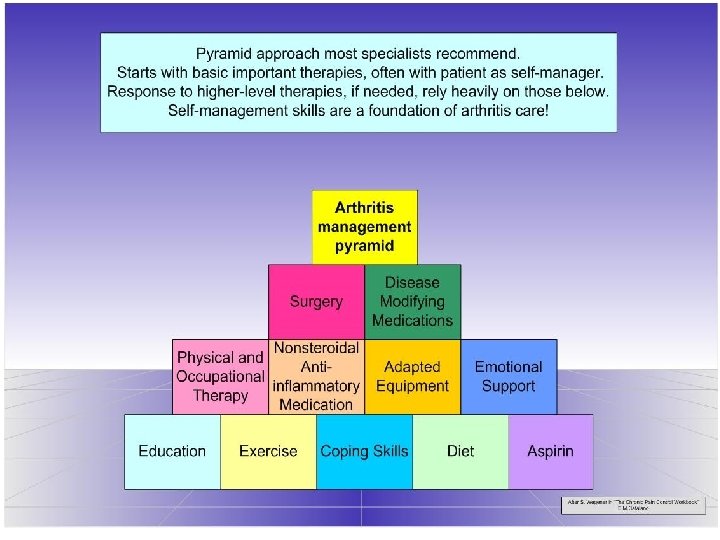
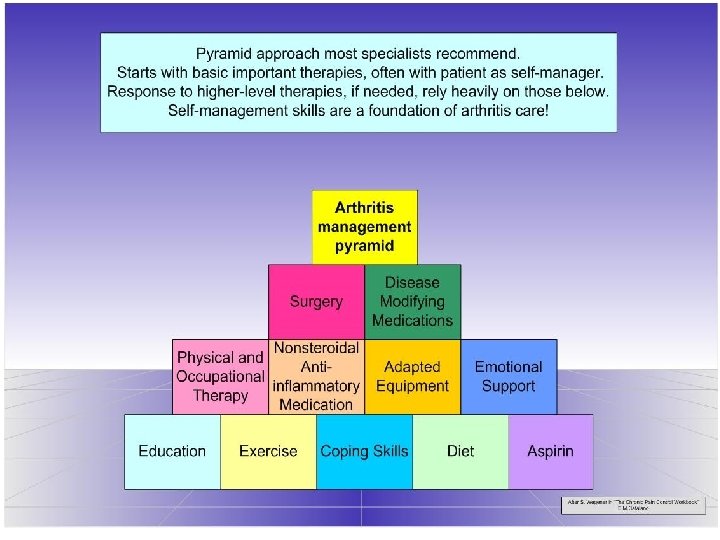
Self-Management Example This next slide uses a person with Rheumatoid Arthritis Keep in mind, higher-level treatments tend to be less effective if there are problems at lower levels
Psychological Interventions Multi-disciplinary Team Approach Psychological contributions largely focus on moderating psychosocial impacts (e. g. thru enhancing participation & adherence, emotion focused strategies) with counselling techniques, behavioural & cognitive principles that have produced many useful interventions
Specific Psychological Strategies Anxiety management Coping strategies for symptoms of disease e. g. via sleep-wake cycle therapy Increasing either mastery or pleasure activities to at least one per day to counter self-esteem & mood problems
Specific Psychological Strategies Cognitive therapy for distortions that can aggravate depression & other emotional responses to AD
Specific Psychological Strategies Stress Management (often within support group framework) especially for conditions more aggravated by stress e. g. epilepsy, pain, respiratory, gastro & musculoskeletal conditions, etc. Social Support sessions with family & friends + active listening by leaders
Specific Psychological Strategies Pain-coping skills Progressive Muscle Relaxation. Isometric Relaxation EMG & Thermal Biofeedback + Autogenic training Hypnosedation (e. g. in burns treatment)
Specific Psychological Strategies Guided imagery e. g. for symptom control Attention re-focussing (stimuli outside body, on to activity)
Specific Psychological Strategies Teaching significant others to reinforce positive pain behaviour (e. g. selfmassage) & ignore negative (e. g. groaning++) Relapse prevention to preserve behavioural & attitudinal gains e. g. groups for maintenance of treatment gains
PSYCHOSOCIAL REHABILITATION OVERVIEW: VA PROGRAM
VA Program Psychosocial Rehabilitation Services (PSR) is a component of the Mental Health Strategic Health Group within the Department of Veterans Affairs.
Psychosocial Rehabilitation Services (PSR) The mission of Psychosocial Rehabilitation Services (PSR) is to provide a supportive, stable & structured program utilizing a community approach to work & residential rehabilitation. Treatment that allows veterans an opportunity to strengthen, identify & maximize their potential based on skills, abilities & rehabilitation needs.
PSR PSR looks at their needs in relationship to their functioning level. The goal of returning this individual to community working & living as independently as possible. PSR employs client centered approach to rehabilitation, putting the veterans desires & need first.
PSR Individualized, originates from anticipated outcomes & considers the total spectrum of needs & obstacles. PSR strives to reintegrate the “whole person” back into their respective community utilizing VA services.
PSR The process is accomplished by providing a collaborative, multi-disciplinary team approach to the reintegration process that is individualized to each veteran. The veteran is a proactive member in this process & is a fully functioning participant from the time of submission to discharge
PSR Programs under Psychosocial Rehabilitation Include Incentive Therapy (IT) Transitional Work Experience (TWE) Compensated Work Therapy (CWT) Supported Education Supported Volunteering Supported Employment
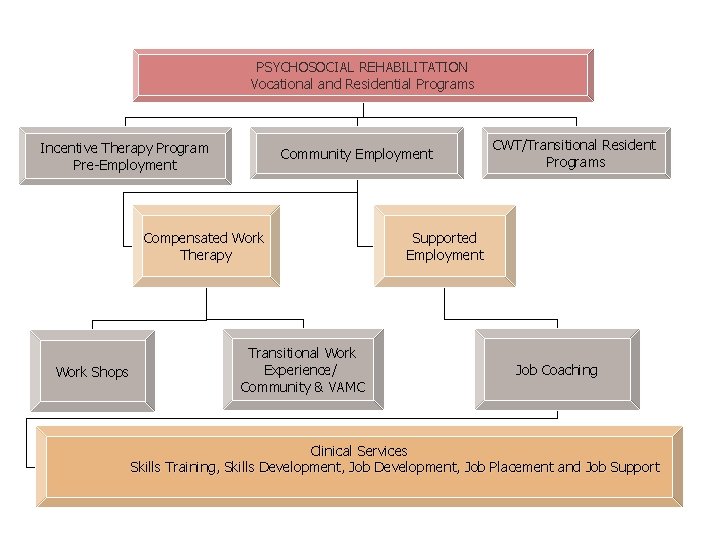
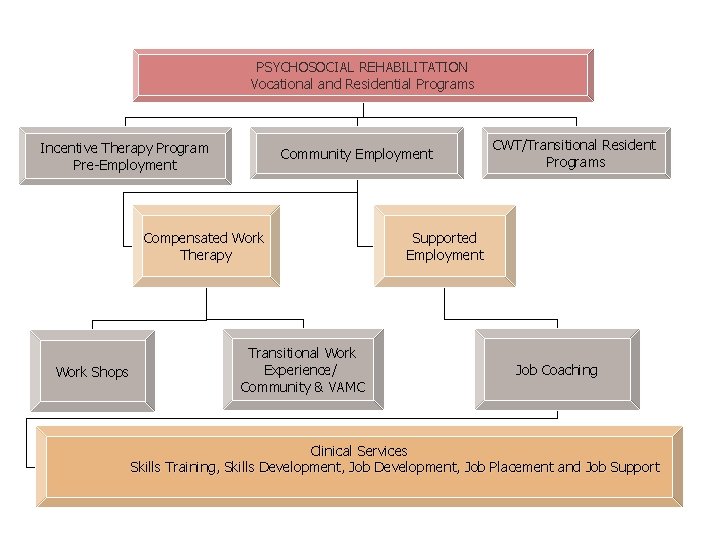
PSYCHOSOCIAL REHABILITATION Vocational and Residential Programs Incentive Therapy Program Pre-Employment Community Employment Compensated Work Therapy Work Shops Transitional Work Experience/ Community & VAMC CWT/Transitional Resident Programs Supported Employment Job Coaching Clinical Services Skills Training, Skills Development, Job Placement and Job Support
Compensated Work Therapy (CWT) CWT is a Department of Veterans Affairs (VA) vocational rehabilitation program that endeavors to match & support work ready veterans in competitive jobs Also consults with business & industry regarding their specific employment needs
Compensated Work Therapy (CWT) In some locations CWT is also known as Veterans Industries; these designations are synonymous.
Supported Employment (SE) SE is an evidence-based clinical model that helps individuals with serious mental illness or physical impairments cooccurring with mental illnesses engage in competitive employment in the community
Transitional Work Experience (TWE) TWE is a transitional work program in VAMCs or in the community to enable participants to gain work experience & work hardening while in CWT therapeutic rehabilitation treatment that prepares Veteran participants for community employment.
Goal of CWT/TWE/SE : To provide work skills development through “work therapy” and also community placement assistance for veterans who have, as one of their vocational goals, returning to community work “when ready” and “as soon as possible. ”
Evidence Based Practices The mandate for requiring community work “as soon as possible” is born out of research & experience indicating that community reintegration with treatment support in real-life roles is the most beneficial vocational rehabilitation modality for those seeking these kind of services.
Purpose of Work Therapy in TWE Develop “prevocational skills in order to prepare the veteran for community employment or some other community work opportunity. These “prevocational skills” include:
Purpose of Work Therapy in TWE 1. 2. 3. 4. 5. 6. 7. These “prevocational skills” include: Personal appearance and hygiene Attendance and punctuality Acceptance of Supervision Ability to get along with co-workers Quality of production Work attitude Ability to learn
Additional Purposes of Work Therapy in TWE In addition to the primary purpose of developing pre-vocational skills, TWE can also be utilized to address other psychosocial needs of veterans in order to facilitate the goal of community reintegration. This includes, but is not limited to, the following:
Additional Purposes of Work Therapy in TWE This includes, but is not limited to, the following: 1. To restore and/or develop the ability and motivation for community work;
Additional Purposes of Work Therapy in TWE 2. To allow the time needed for the establishment of a stronger recovery program (for Mental Health, Alcohol/Substance Abuse, and/or Physical Rehabilitation); and/or 3. Provide funds in order to overcome the transportation barrier for obtaining community work.
Customized/Supported Employment? May include employment developed through job carving, self-employment entrepreneurial initiatives, or other job development. Restructuring strategies that result in job responsibilities being customized and individually negotiated to fit the specific needs of each individual with a disability.
Key Features of Customized/Supported Employment Partner ships between employment resources and supports in the form of integrated treatment team. Veterans Vocational Specialist Employer Medial Staff
Key Features of Customized/Supported Employment (Con’t) Dollars that follow the individual providing for creativity & flexibility in the negotiations with employers Training moneys available from the Federal and State Government agencies The Federal and State Governments tax credits for employers
Customized Employment Individualizing the employment relationship between employees and employers in ways that meet the needs of both. It is based on an individual determination of the strengths, needs and interests of the person with a disability. It is also designed to meet the specific needs of each employer.
Supported Employment Setting wherein the veteran is an actual employee of the sponsoring company & receives follow up support services from a job coach/ employment specialist.
Key Process Components of Supported Employment Rehabilitation is considered an integral component of treatment The goal of Individual Placement & Support (IPS) is competitive employment in integrated work settings Vocational assistance is continuous & based in competitive work experience
Key Process Components of Supported Employment Follow-along support continues based on individual needs after start of employment Job finding, disclosure, & job supports are based on clients’ preferences choices. A multi-disciplinary team approach is used for support