Week 5 Classroom focus Toddlers Lead Poisoning Pica


























- Slides: 108
Week 5 Classroom focus Toddlers & • • • Lead Poisoning, Pica Drowning Anaphylaxis Asthma Viral Respiratory Conditions • Bacterial respiratory Conditions • Poisonings- vapours, oil, petroleum, ASA & meds, etc. • Genetic Anomalies. CF
Resources used • • Sources from Hockenberry et al 2007 Wong Essentials of Pediatric Nursing, 2001 Mosby’s Electronic Image File Collection Ppte presentation by K. Fryer and P. Durocher 2007 & 2008, 63 -274 • Pptes from Partners in the Collaborative B. Sc. N. Programme, University of Windsor, 63 -277 • Notes of Dr. S. Mc. Mahon 63 -373 and 277 • Assorted websites as indicated on slides
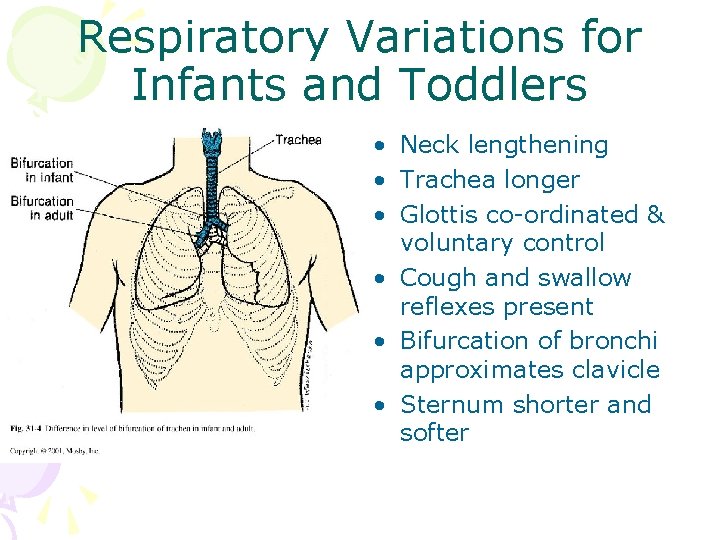
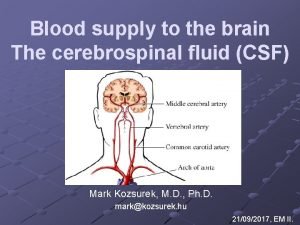
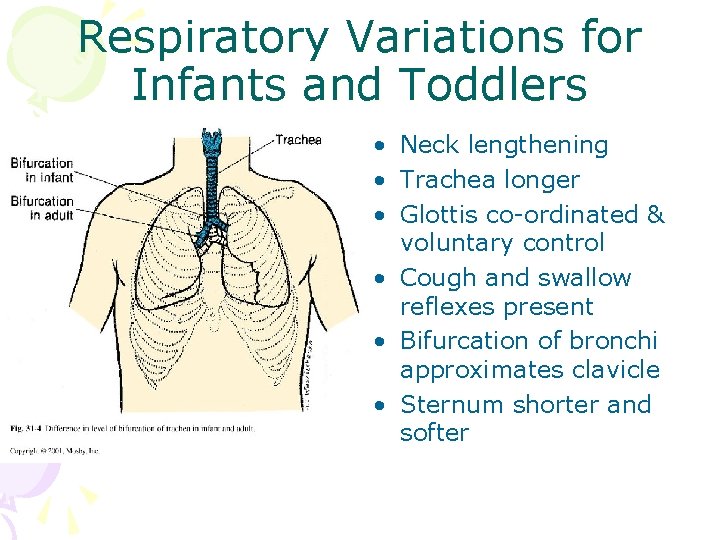
Respiratory Variations for Infants and Toddlers • Neck lengthening • Trachea longer • Glottis co-ordinated & voluntary control • Cough and swallow reflexes present • Bifurcation of bronchi approximates clavicle • Sternum shorter and softer
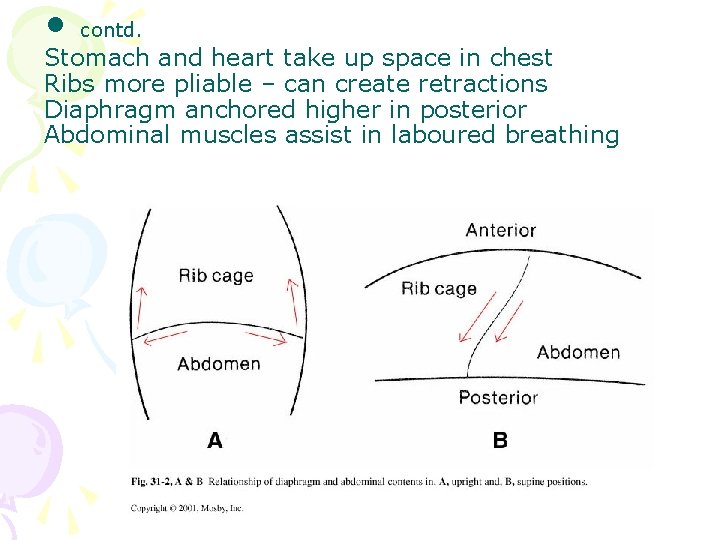
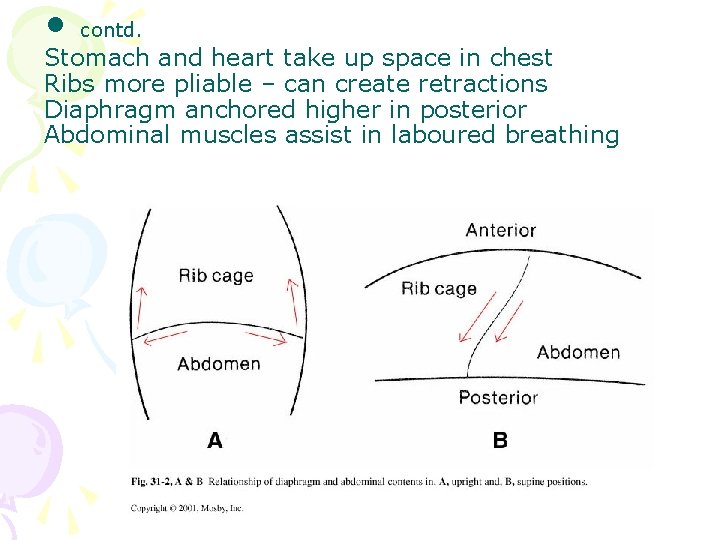
• contd. Stomach and heart take up space in chest Ribs more pliable – can create retractions Diaphragm anchored higher in posterior Abdominal muscles assist in laboured breathing
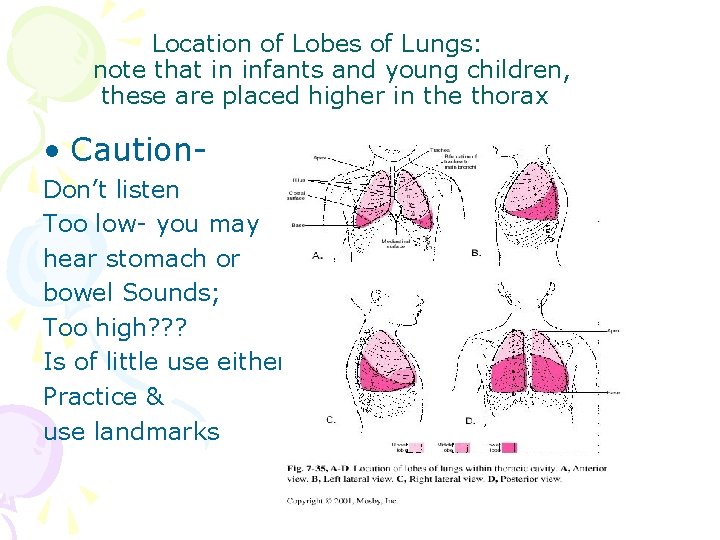
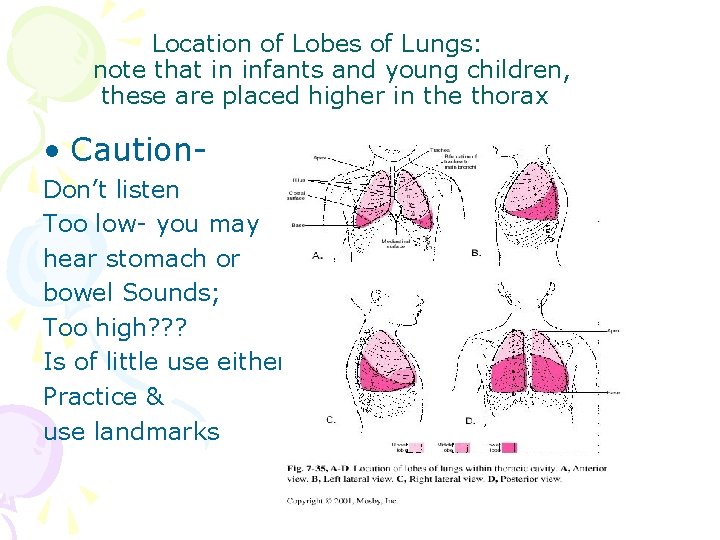
Location of Lobes of Lungs: note that in infants and young children, these are placed higher in the thorax • Caution. Don’t listen Too low- you may hear stomach or bowel Sounds; Too high? ? ? Is of little use either. Practice & use landmarks
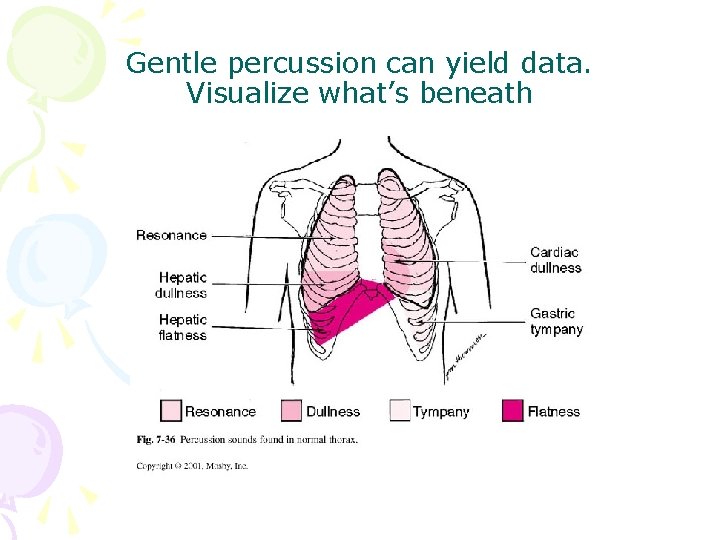
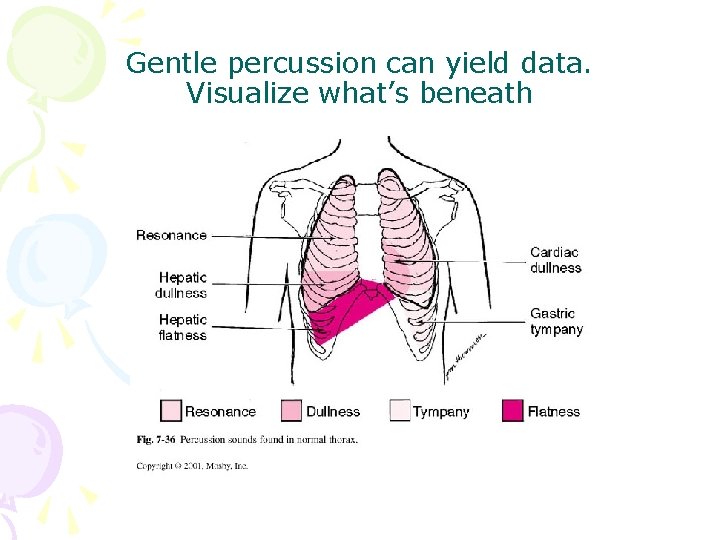
Gentle percussion can yield data. Visualize what’s beneath
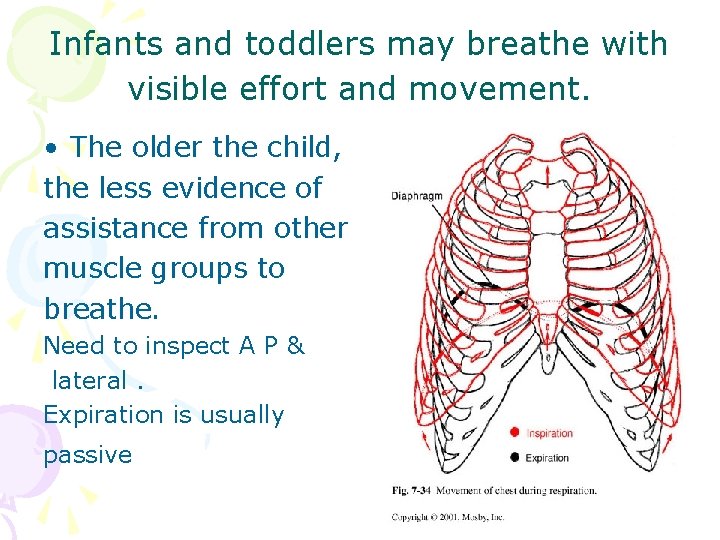
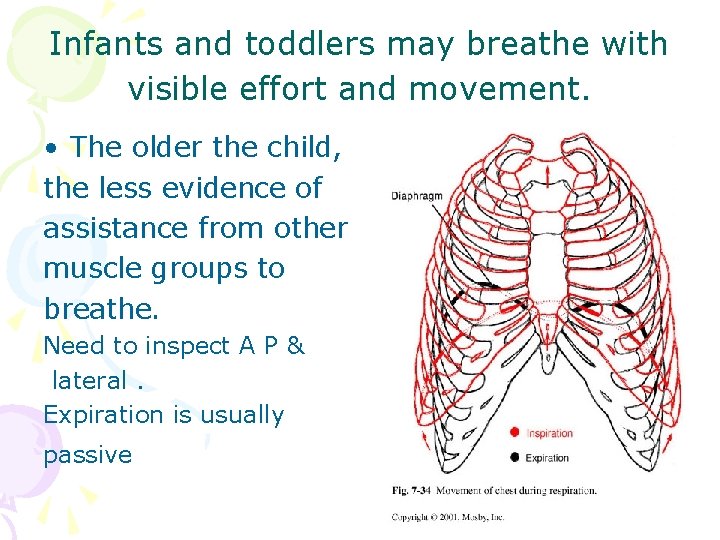
Infants and toddlers may breathe with visible effort and movement. • The older the child, the less evidence of assistance from other muscle groups to breathe. Need to inspect A P & lateral. Expiration is usually passive
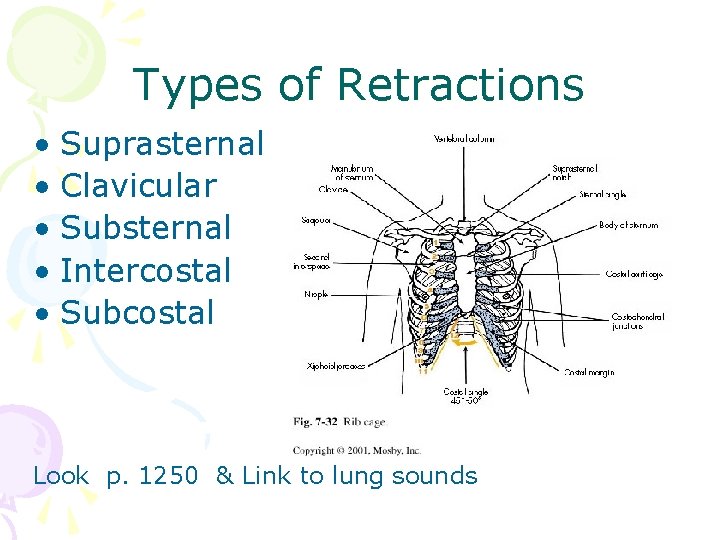
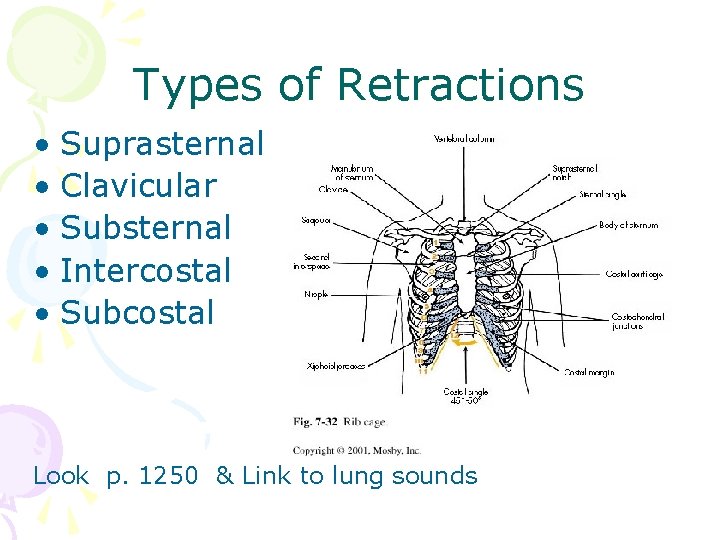
Types of Retractions • Suprasternal • Clavicular • Substernal • Intercostal • Subcostal Look p. 1250 & Link to lung sounds
Paediatric Respiratory chemistry influenced by • • • • Haemoglobin- mature or foetal types, anemia Body core temperature Hydration, dehydration, clotting Toxins Air Particulates, Pollutants and heavy metals Acid-base balance Medications Fear and stress O 2, Pco 2 ratio & tissue uptake( hypoxia) Carbonic acid, Na bicarb levels Calcium, magnesium, copper Lighting, radiant warmers Obstructive lung conditions, hypoventilation Diabetes. Insulin, glucose Altitude and atmospheric pressure
Some toddlers are considered medically fragile as they must rely on oxygenation via respirator, with humidification, and protection from infections. Nurses support families as they provide total care at home while creating a developmentally rich environment for their child.
The respiratory system must include: • Mouth, ears, nose, & throat & Developmental stage and Environment • Consider: Latex and other allergies- anaphylaxis • Variations in young children before and after 3 years of age- Dentition, eustachian tube angles, Swallowing, cough reflex, Sinuses, lymph glands / adenoids • Safety : mobility, curiosity, Use of soother, fingers, tooth brushing, hand washing • Normative hand to mouth & taste- smell-mouthtesting behaviours. Colour & Smell of things attract children • Learn YUCKY tastes and smells- link to symbols
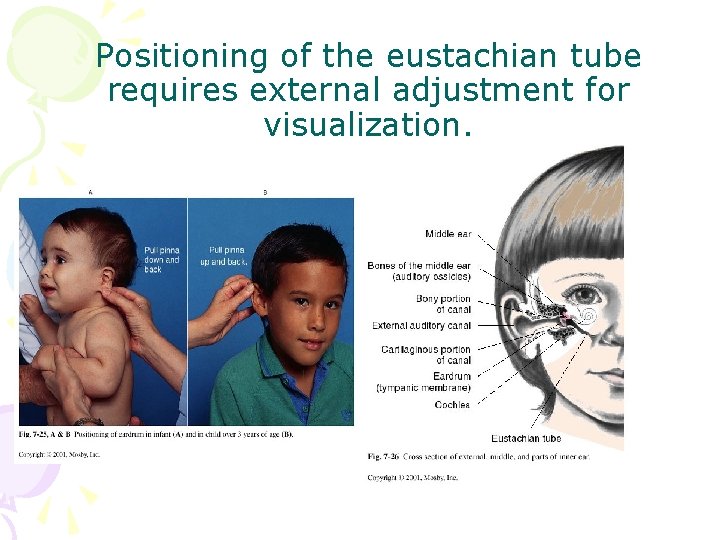
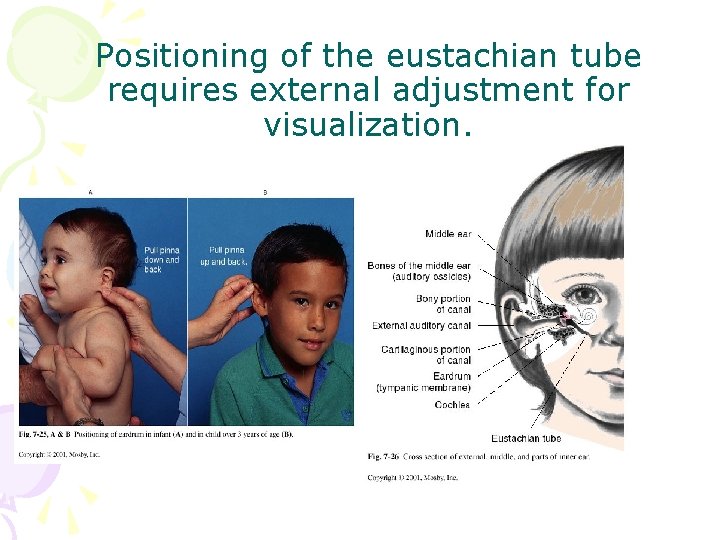
Positioning of the eustachian tube requires external adjustment for visualization.


The Nose knows! • • • Able to detect mother’s scent from birth. Can tell when feeding prepared. Have preferences. Alai Nasi flare when in distress Different EENT in genetic variations
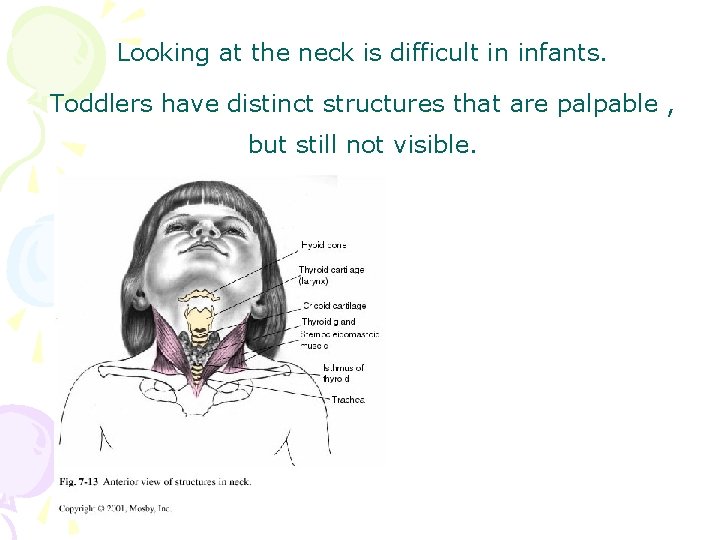
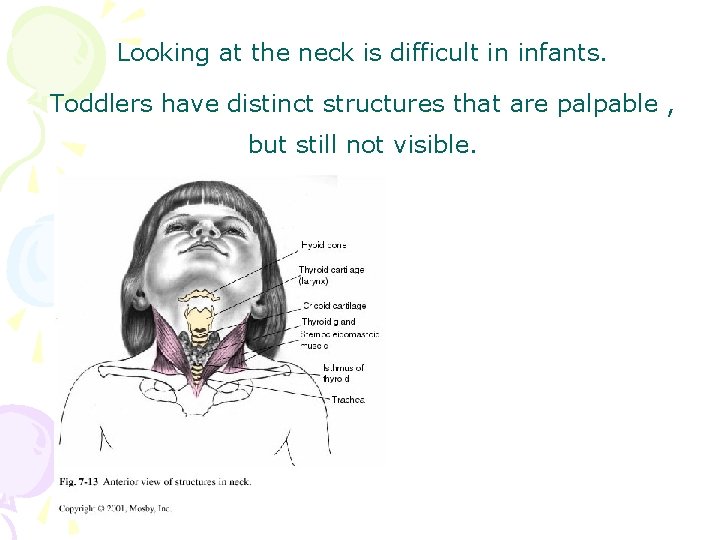
Looking at the neck is difficult in infants. Toddlers have distinct structures that are palpable , but still not visible.
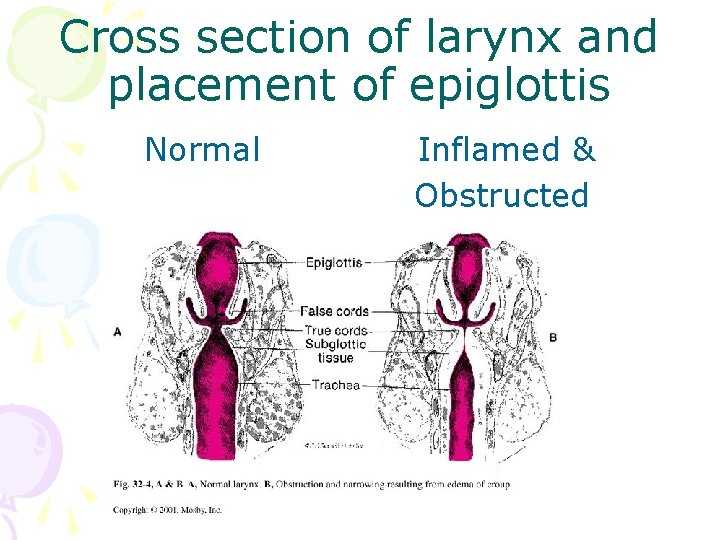
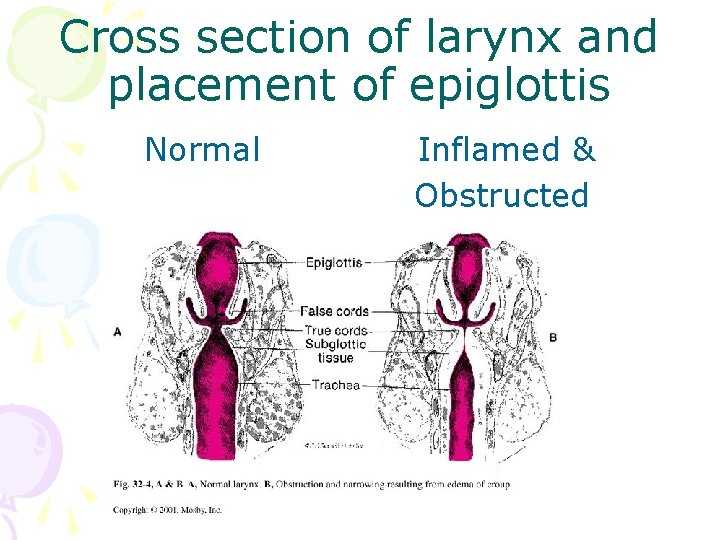
Cross section of larynx and placement of epiglottis Normal Inflamed & Obstructed
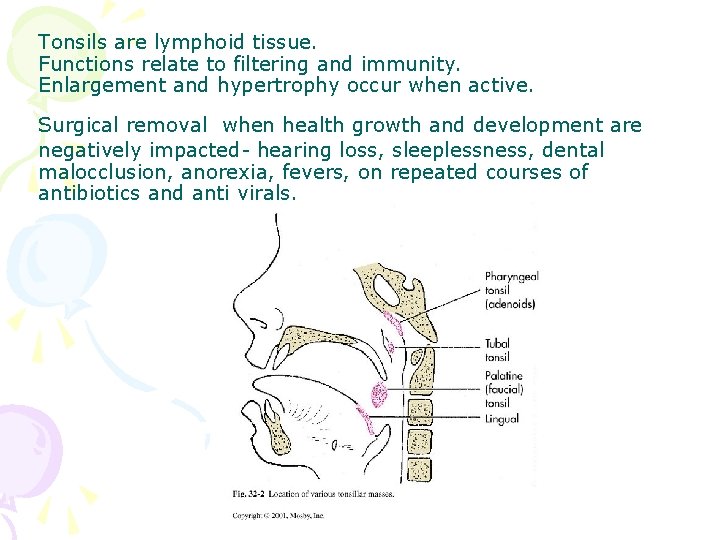
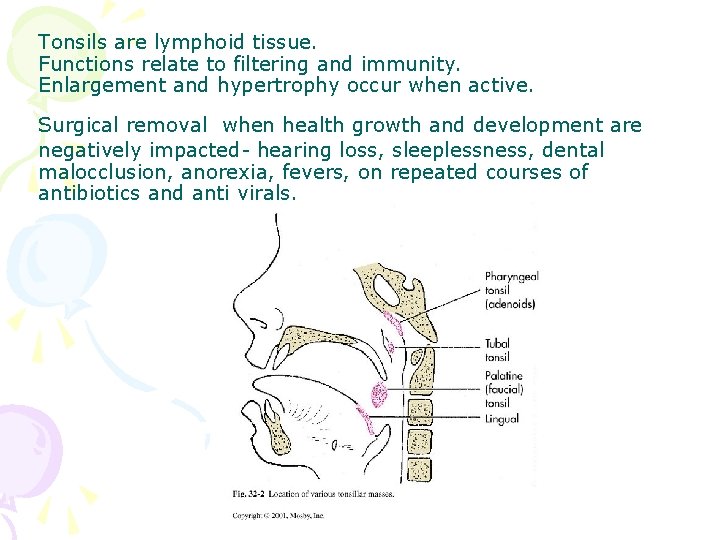
Tonsils are lymphoid tissue. Functions relate to filtering and immunity. Enlargement and hypertrophy occur when active. Surgical removal when health growth and development are negatively impacted- hearing loss, sleeplessness, dental malocclusion, anorexia, fevers, on repeated courses of antibiotics and anti virals.
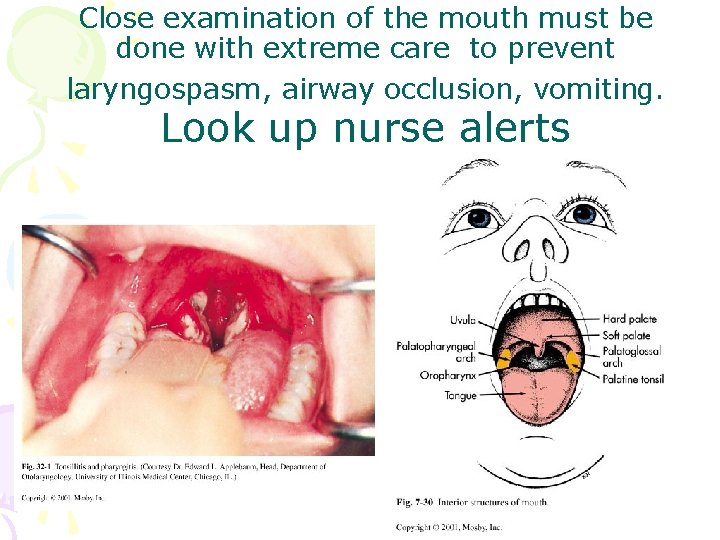
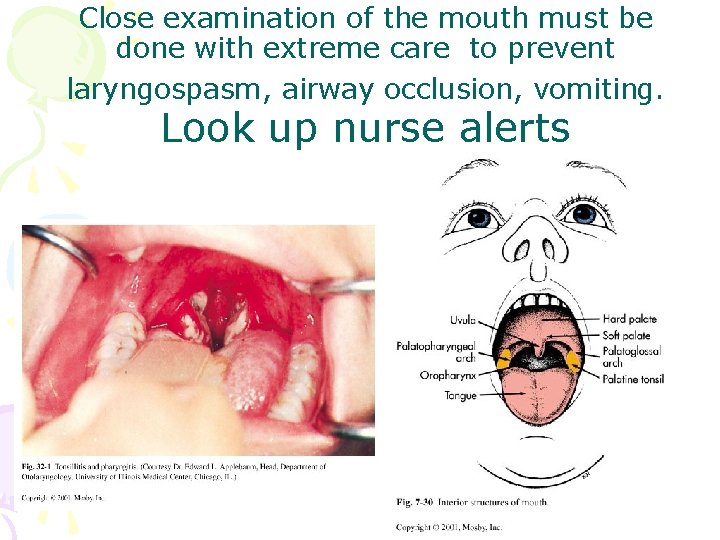
Close examination of the mouth must be done with extreme care to prevent laryngospasm, airway occlusion, vomiting. Look up nurse alerts
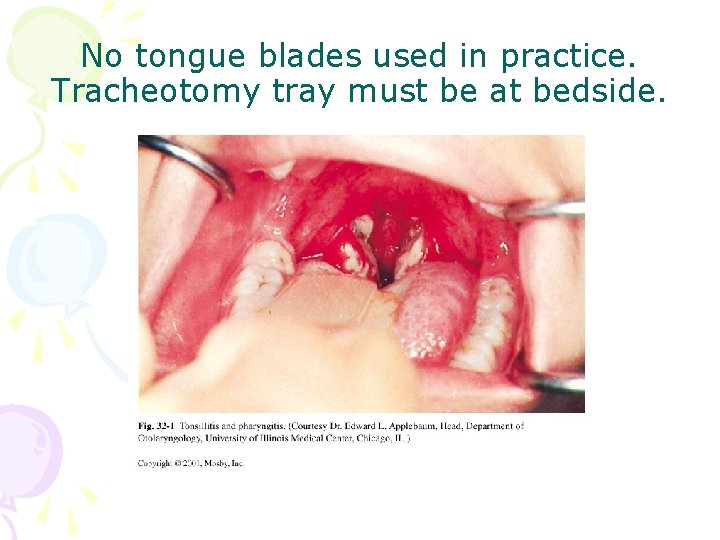
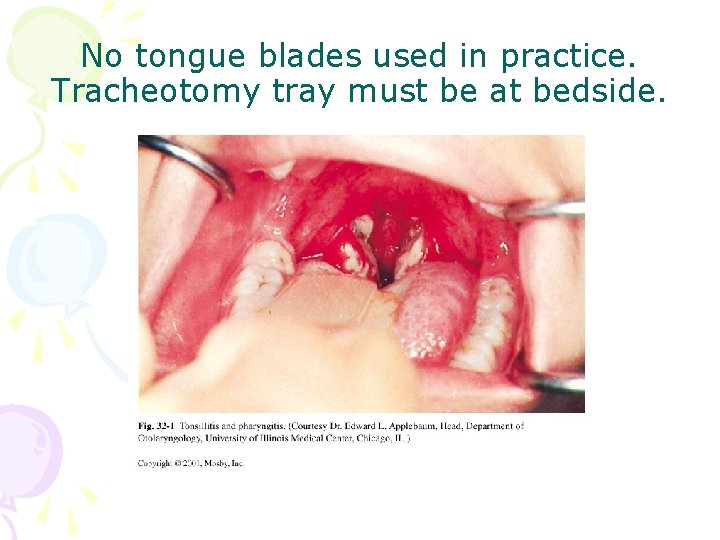
No tongue blades used in practice. Tracheotomy tray must be at bedside.
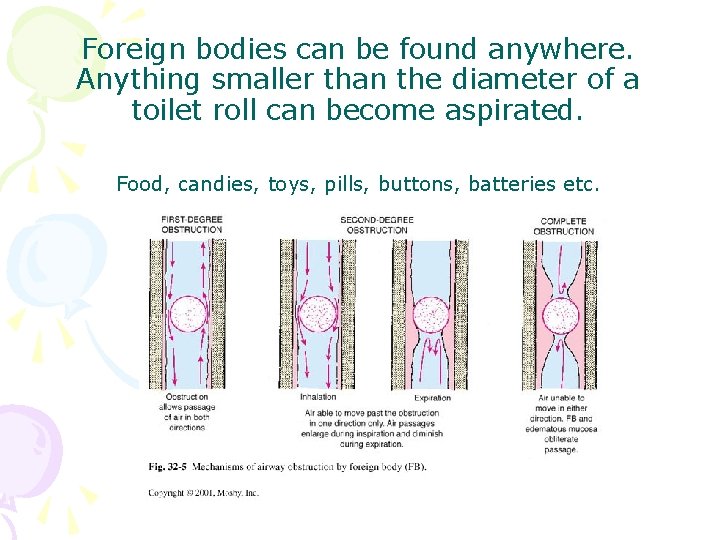
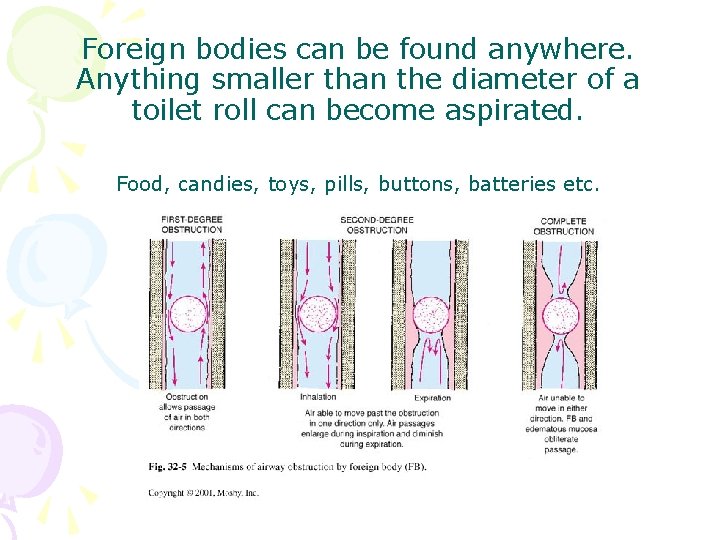
Foreign bodies can be found anywhere. Anything smaller than the diameter of a toilet roll can become aspirated. Food, candies, toys, pills, buttons, batteries etc.
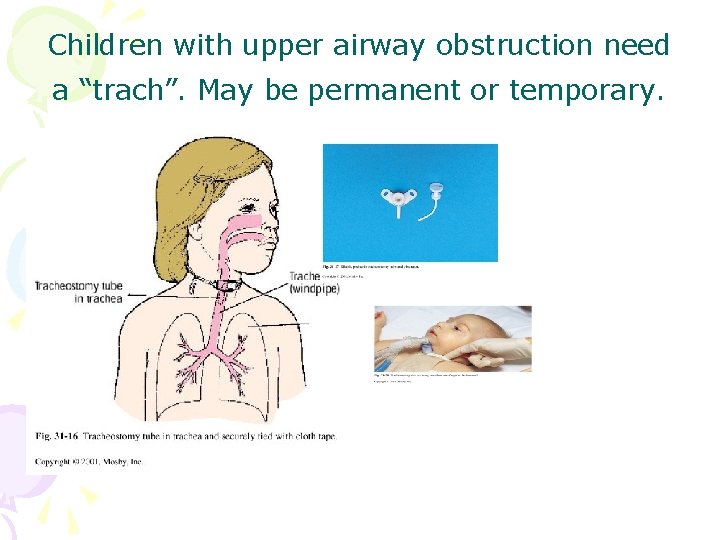
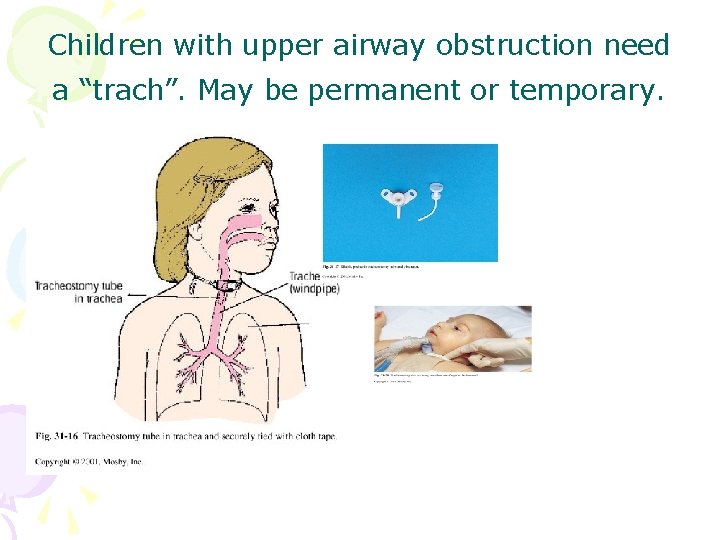
Children with upper airway obstruction need a “trach”. May be permanent or temporary.
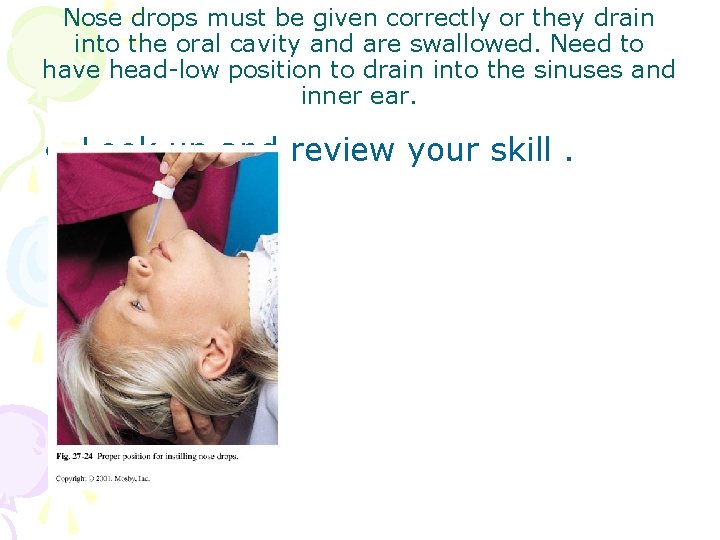
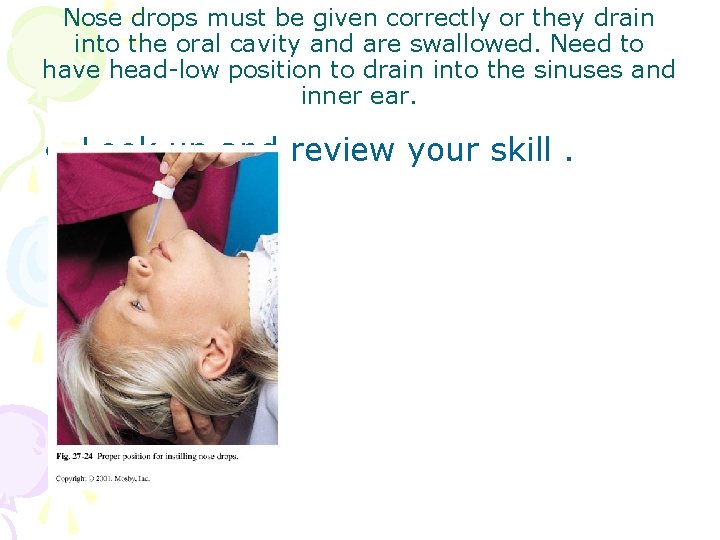
Nose drops must be given correctly or they drain into the oral cavity and are swallowed. Need to have head-low position to drain into the sinuses and inner ear. • Look up and review your skill.
DROWNING WATER SAFETY Drownproofing
Water Safety ? Drowning? • • Not in my backyard! We have gates. My child can bath himself. I’m right close by. My child knows how to swim. What good are those floaties? We don’t swim in our culture. There is only a MINUTE between a lifetime and a lifetime of regret !
Tubs, pools, ditches, boats, reservoirs, ponds, lakes, rivers

• • Drowning Age inquisitive, explore & unawareness of danger Accidental death ranks 2 nd for boys & 3 rd for girls ages 1 -4 years little ∆ despite prevention education bathtubs, pools, ditches, hot tubs, ponds, lakes etc Near-drowning one of leading causes of vegetative state in young children Can drown in as little as 6” of water http: //www. childrendrowningprev ention. com/index. html
Pathophysiology of drowning • Most organ systems affected • Extent of damage affected by factors such as anoxia and asphyxia • Cardiopulmonary arrest after 4 -6 min • Problems: hypoxia, aspiration, hypothermia , infection • All children should be hospitalized for 12 -48 hrs even in near-drowning
Path cont’d • Laryngospasm & aspiration • Hypoxia causes cellular damage— brain after 4 -6 minutes; heart and lungs after 30 minutes • Pulmonary edema, atelectasis, airway spasm, pneumonitis • Look at KLASSEN case : - Car plunging over bridge in Montreal ( the Windsor Star, 2/7/08, p. B 1)
Near Drowning • Prognosis is best if the water is cool and the victim is immersed for less than 5 minutes • 90% occur in swimming pools • Boys 5: 1 • 50% occur under age 4 years
Management • ICU-Respiratory assessments, V/S, mechanical ventilation and/or tracheostomy, blood gases, chest therapy, IV therapy • Emotional support for family • If no purposeful movement within 24 hours = severe neurological damage or death

POISON CONTROL
Poison Prevention • Ingestion of toxic agent **can be usual household items • Curiosity as a toddler • Underdeveloped taste • Most common: • Over 90% occur at home • See case study p. 669
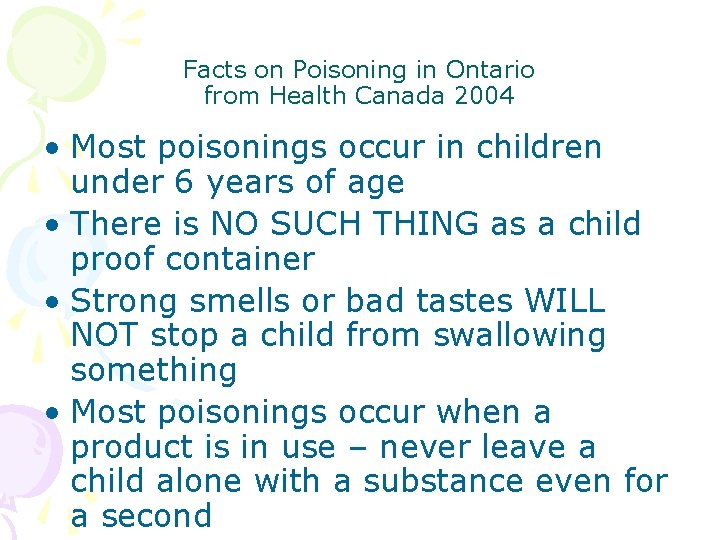
Facts on Poisoning in Ontario from Health Canada 2004 • Most poisonings occur in children under 6 years of age • There is NO SUCH THING as a child proof container • Strong smells or bad tastes WILL NOT stop a child from swallowing something • Most poisonings occur when a product is in use – never leave a child alone with a substance even for a second
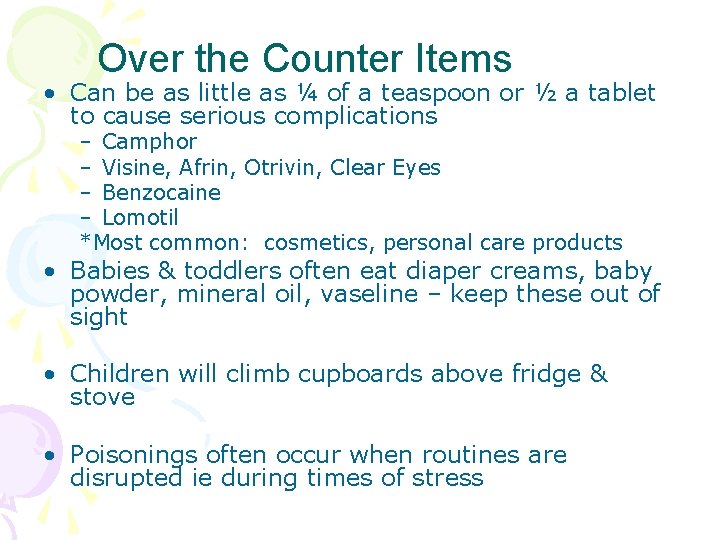
Over the Counter Items • Can be as little as ¼ of a teaspoon or ½ a tablet to cause serious complications – Camphor – Visine, Afrin, Otrivin, Clear Eyes – Benzocaine – Lomotil *Most common: cosmetics, personal care products • Babies & toddlers often eat diaper creams, baby powder, mineral oil, vaseline – keep these out of sight • Children will climb cupboards above fridge & stove • Poisonings often occur when routines are disrupted ie during times of stress
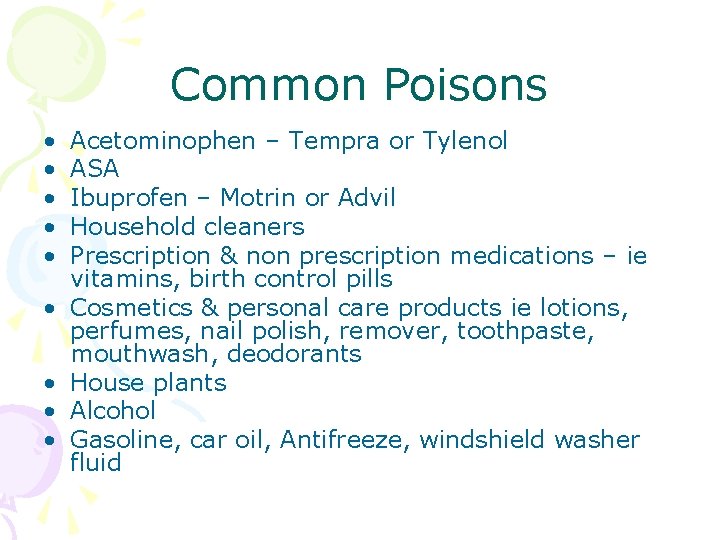
Common Poisons • • • Acetominophen – Tempra or Tylenol ASA Ibuprofen – Motrin or Advil Household cleaners Prescription & non prescription medications – ie vitamins, birth control pills Cosmetics & personal care products ie lotions, perfumes, nail polish, remover, toothpaste, mouthwash, deodorants House plants Alcohol Gasoline, car oil, Antifreeze, windshield washer fluid
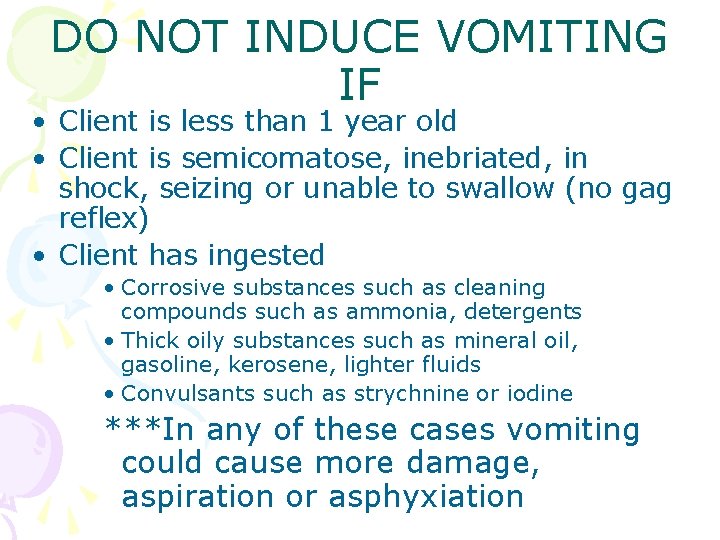
DO NOT INDUCE VOMITING IF • Client is less than 1 year old • Client is semicomatose, inebriated, in shock, seizing or unable to swallow (no gag reflex) • Client has ingested • Corrosive substances such as cleaning compounds such as ammonia, detergents • Thick oily substances such as mineral oil, gasoline, kerosene, lighter fluids • Convulsants such as strychnine or iodine ***In any of these cases vomiting could cause more damage, aspiration or asphyxiation
• Save all emesis – it may need to be sent to lab for contents analysis • May also order urine & blood tests • Closely monitor vital signs of client • Observe for any other symptoms such as confusion, tremors, convulsions, visual disturbances, loss of consciousness, respiratory distress or cardiac arrhythmias

• Poisoning by Inhalation • Requires fresh air, oxygen maybe CPR • If the person is not breathing begin CPR • Poisoning of Skin or Eyes • Requires removing any clothing touched by the poison • Flushing with continuous stream of water for 15 mins
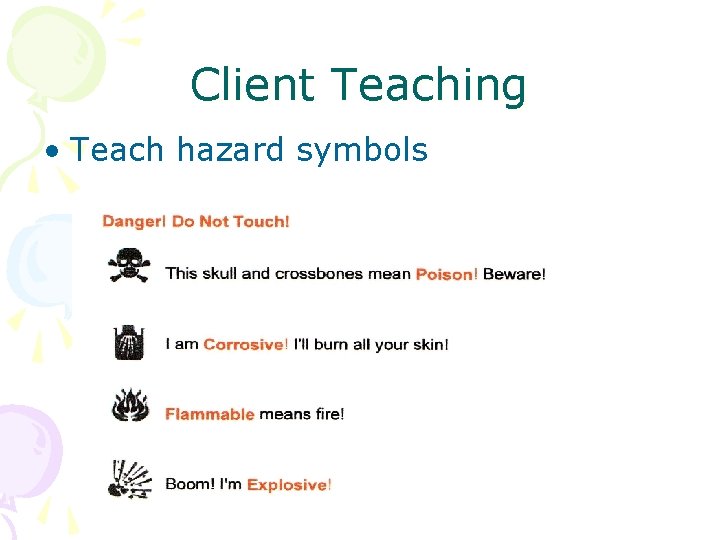
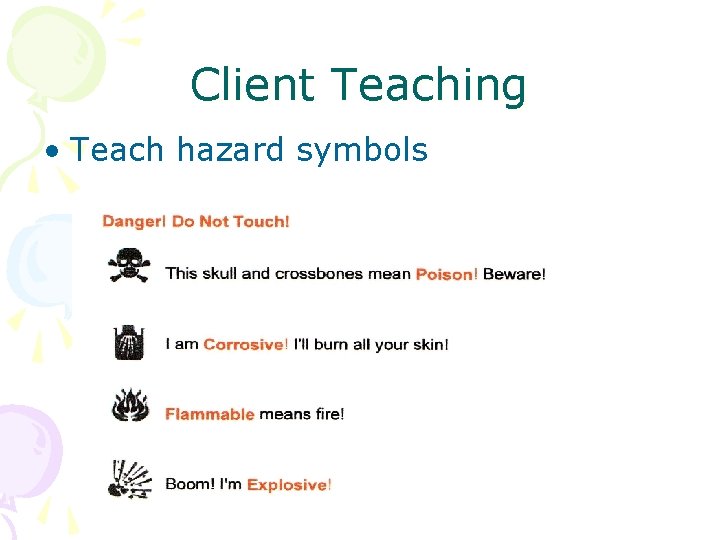
Client Teaching • Teach hazard symbols
Client Teaching
Heavy Metal Poisonings • Mercury • Sources: thermometers, food sources • Neuro, digestive, kidney damage • Chelation therapy • Lead • Learning disabilities, behavioral problems, seizures, neurological damage, anemia, coma • Chelation therapy
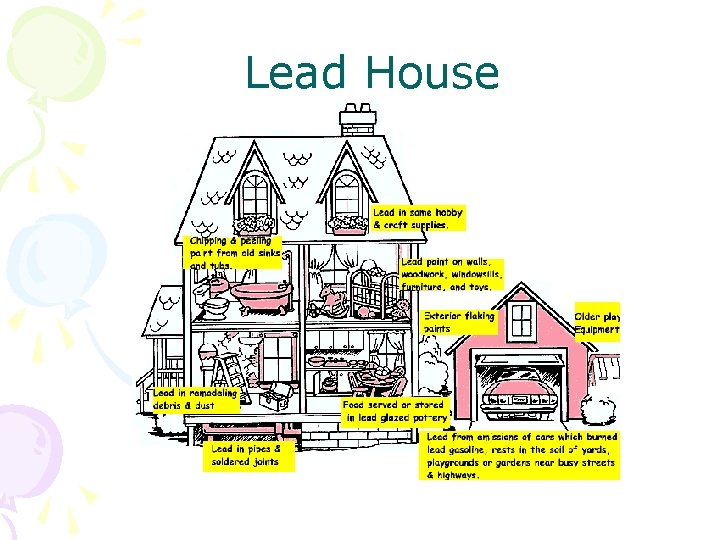
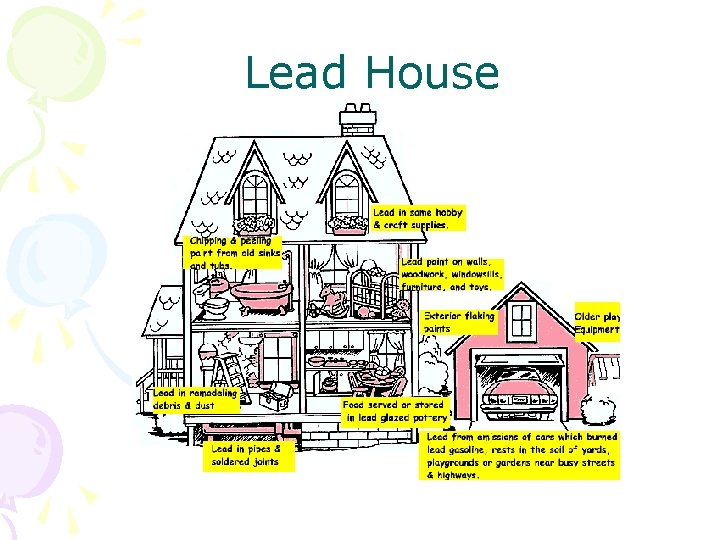
Lead House

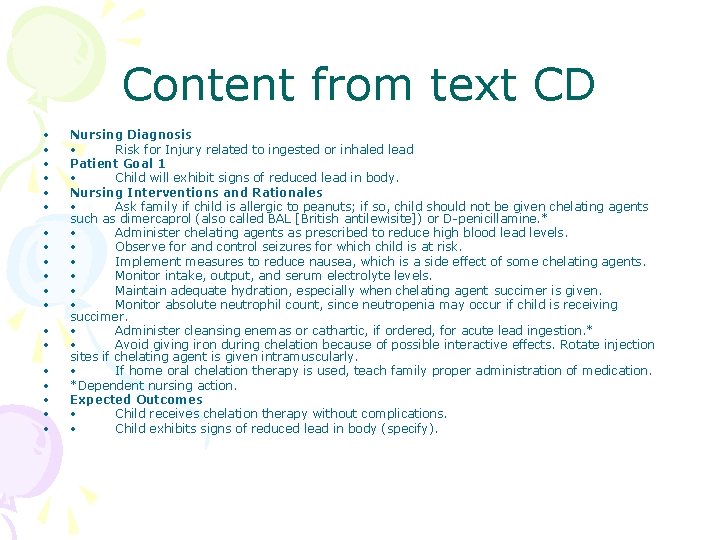
Look up Lead poisoning Guidelines and care plan on the CD that comes with the text Can print off or save to desktop.
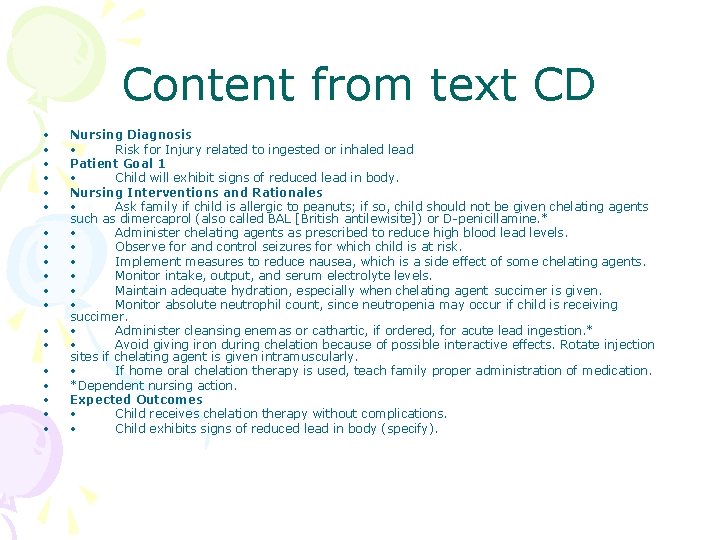
Content from text CD • • • • • Nursing Diagnosis • Risk for Injury related to ingested or inhaled lead Patient Goal 1 • Child will exhibit signs of reduced lead in body. Nursing Interventions and Rationales • Ask family if child is allergic to peanuts; if so, child should not be given chelating agents such as dimercaprol (also called BAL [British antilewisite]) or D-penicillamine. * • Administer chelating agents as prescribed to reduce high blood lead levels. • Observe for and control seizures for which child is at risk. • Implement measures to reduce nausea, which is a side effect of some chelating agents. • Monitor intake, output, and serum electrolyte levels. • Maintain adequate hydration, especially when chelating agent succimer is given. • Monitor absolute neutrophil count, since neutropenia may occur if child is receiving succimer. • Administer cleansing enemas or cathartic, if ordered, for acute lead ingestion. * • Avoid giving iron during chelation because of possible interactive effects. Rotate injection sites if chelating agent is given intramuscularly. • If home oral chelation therapy is used, teach family proper administration of medication. *Dependent nursing action. Expected Outcomes • Child receives chelation therapy without complications. • Child exhibits signs of reduced lead in body (specify).
Pica • Compulsive & excessive ingestion of food & non food substances • Common in children, pregnant women, autism, anemia, chronic renal failure, celiac disease • Often unrecognized • Consider with abdominal pain, GI symptoms or anemia

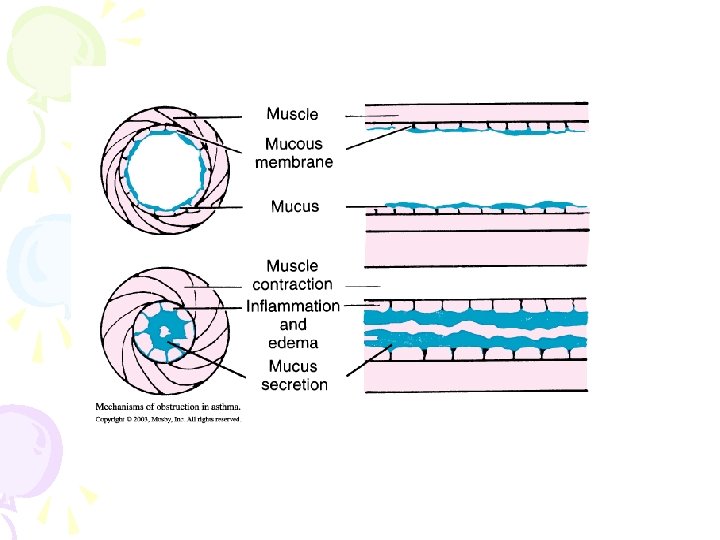
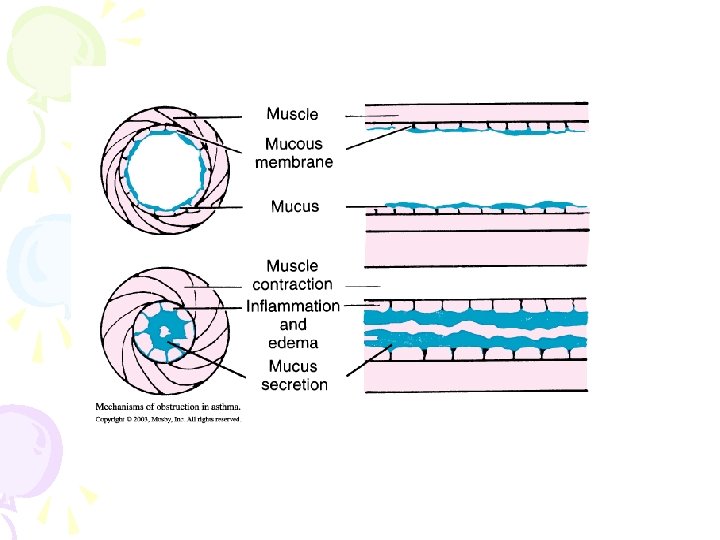
Asthma • Chronic, obstructive, often reversible • Hyper responsiveness of trachea & bronchi • Inflammation & edema; tenacious mucus • Trapped air • Severe respiratory acidosis & metabolic acidosis • Causes-genetics, triggers, allergies
Prevalence • 1997 - 12. 2% of children under age 20 years : Today 2007 - doubled + • 6. 7% of all hospitalizations for children • Males more frequently than females • Mortality rate is increasing yearly • Increasing along highways with heavy truck traffic and in drift areas due to micro particulates from coal powergeneration and pollution from industries.

• Watch the animation videos on the CD with the text. Asthma Care Plans • Also look up guidelines and Nclex questions • Text pp. 1355 -1373
Medications Treatment – Bronchodilators-by inhalers, compressors, aerochambers e. g. Ventolin – Leukotriene modifiers e. g. Singulair – Corticosteroids e. g. bechlomethasone inhalers Allergy-proof the home, avoid triggers Chest physio, education, “normalization” NSG Care pg. 1402 -1404
Refer to CD with text for • Guidelines, • Nursing care plans, • Animated videos • RNAO Best Practice Guidelines • Peak Flow Meter use and indications

Complications • Status Asthmaticus • Chronic bronchitis, bronchiolitis • Pneumonia, • Emphysema, • Cor Pulmonale, • atelectasis, pneumothorax, • Death

Allergic Rhinitis • Common to 20 -40% of pediatric population- aggravated by tobacco smoke , early intro of foods and milk • Cyclic, Perennial, or Seasonal: hayfever- trees, grasses, weeds, flowers, pollens, decay • Need familial predisposition and exposure to allergen for sensitization

WHAT HAPPENS? • Immune response to the allergenstimulates Ig. E production in B Lymphocytes. These sensitized cells patrol and trigger rapid release of histamine, prostaglandins and leukotrienes from the mast cells when allergen is recognized. Rapid onset is followed by slower acting cytokines. • Histamines cause vasodilation, swelling, mucosal edema, mucus. • Cytokines produce inflammation, and cell destruction- exudate, redness

Common Allergens: Pet dander, feathers, cockroach dung, dust mites, pollens, mold, grass, dust, micro particles, wool, foods, medications, chemicals, insect stings/bites


Treatment of allergies is vital: but first step is recognition • Assessment : Allergic shiners, nasal obstruction, snoring, mouth breathing, hearing deficit and ear infections, allergic salute, horizontal nasal crease , pale and swollen nasal turbinates, red swollen eyes, red-rimmed, pale colour generally, nasal drip , tickle in throat, headache, wheezing, eczema(atopic dermatitis), pruritis, urticaria, exercise intolerance, delayed speech, abdominal pain, cramps, digestive upsets, swollen lips and tongue, burning skin, clear nasal discharge, sneezing
ANAPHYLAXIS • Sudden and severe systemic response to allergens- foreign proteins. Body reacts in dual mode, instantly and chronically. • Life threatening- odours, oils, particles, proteins- miniscule amounts create dramatic response, can occlude airways, cyanosis, mucosal membranes swell up, cause spasms, create kidney shutdown, cerebral edema, cell rupture, death. • EMERGENCY – NO TIME AT ALL ! STAT
Management • Avoid contact • Eliminate allergens- triggers • Create a zone of protection right on the person- carry an Epipen and know how to use it. Everyone needs to know and practice • Medic Alert Bracelet; tell everyone • Read labels, eliminate offending things • Fragrance –free zones, peanut-free zones. • No eating out • Private Member’s Bill passed into Law- anaphylaxis plan in place- on buses, in public places, Epipen training • food labels, consumer products( cosmetics) • nut free products
Allergy Testing should take place but no sooner than 2 years • Other diagnostics are: • Observations associated with first immunizations- beyond normal reactions • Nasal Swab for eosinophils, Blood work for immunogobulin assay( all Immunoglobulins ) particularly Ig. E, • Skin scratch tests for specific reagentsallergens [done in an allergists office or hospital setting in case of anaphylaxis & need for Epinephrine] • Food challenge
Food allergies Foreign Protein response • Commonly to eggs, citrus fruits, strawberries, tomatoes, grains, cow’s milk, peanut butter, nuts, sesame seeds & oil, chocolate, seafood • Red dyes, food additives, preservatives, artificial flavourings • After periods of avoidance and perhaps desensitization treatments, some children will want to be “medically challenged” [at about 7 years]- admitted to hospital[HSC] to test their responses to “deadly” allergens. May not be overly sensitized with maturity of physiologyoutgrown it
Allergy management • Clean house and environment. Vacuum, remove black mould, pets • Immunotherapy- desensitization “hayfever shots” start 2 -6 weeks before season. • Antihistamines- nasal spray, pill, liquid, injection, ( 1 st generation. Benadryl: 2 nd Generation- Claritin, Zyrtec) Ok for kids 6 months and older. Allegra for >6 years. Watch for sedation effects. School performance, driving, riding bikes, sports co-ordination • Leukotriene modifiers – montelukast approved for >2 yrs. • Nasal decongestants and anti inflammatory sprays – cortocosteroids • care taken with ephedrines and pseudoephedrines- now off the shelves, • Prevent Drug misuse, rebound, habituation • Cromolyn Sodium prevents histamine response • Caution re decreased linear growth with ongoing use of corticosteroids
Respiratory Infections • Upper Respiratory tract • Lower Respiratory tract • Viral • Bacterial • Primary • Secondary • Episodic acute • Chronic acute
Croup Syndromes • • General term: croup Boys>girls Children between 2 -6 years of age Pathophysiology – obstruction of airway (larynx) – usually viral cause • S/S: hoarseness, resonant cough “barking”, “seal”, inspiratory stridor, respiratory distress

– Spasmodic or laryngotracheobronchitis (LTB) – Differentiate between croup and potential life-threatening epiglottitis – Treatment: cool mist – take child outside if cool enough, keep child calm, oral steroids • Racemic Epinephrine given via nebulizer Why?
Epiglottitis • Key differences from croup: 1. Absence of cough 2. Presence of dysphagia 3. High degree of toxicity “Children with epiglottitis usually look worse than they sound, in contrast to children with croup who sound worse than they look. ”
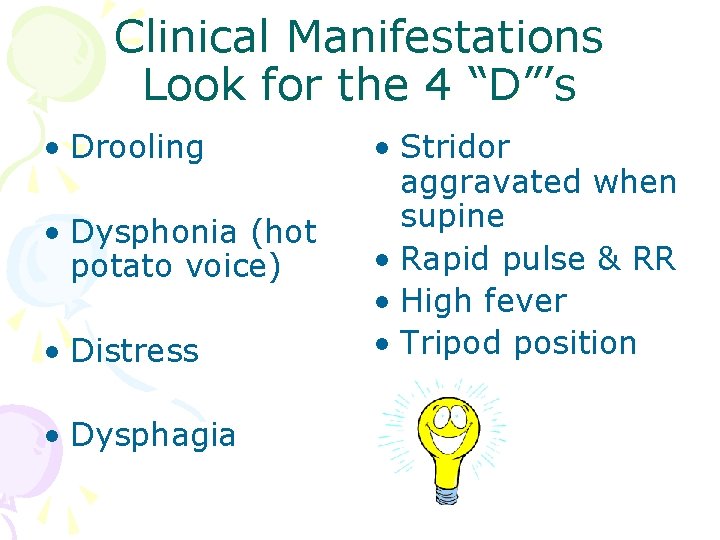
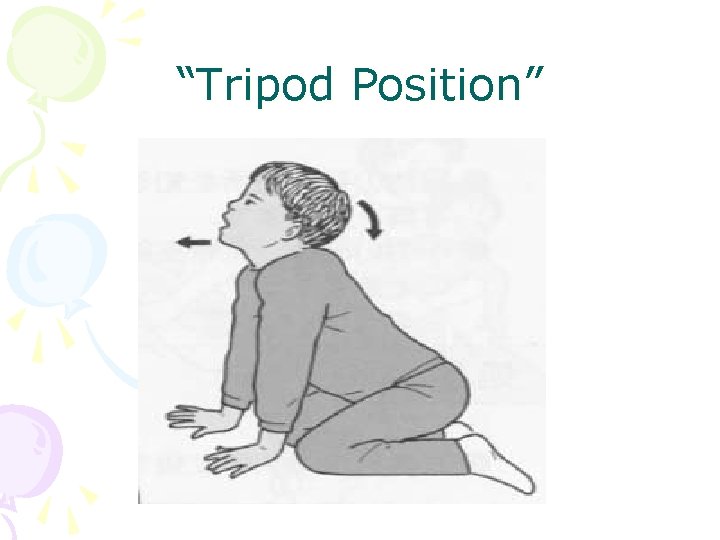
Clinical Manifestations Look for the 4 “D”’s • Drooling • Dysphonia (hot potato voice) • Distress • Dysphagia • Stridor aggravated when supine • Rapid pulse & RR • High fever • Tripod position
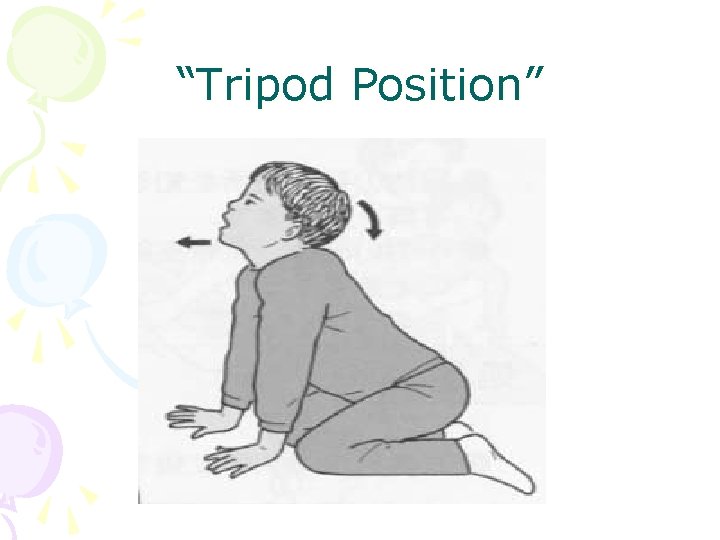
“Tripod Position”
• Abrupt onset of symptoms • Obstruction of airway IS A MEDICAL EMERGENCY • Constant monitoring is necessary • Reduce stress – keep child calm • NEVER examine throat of a child suspected of epiglottitis
Management • PROTECT AIRWAY!!!!! • IV antibiotics • Steroids • Allow child to remain in position that is most comfortable • Intubation may be necessary • In severe cases: tracheostomy

Pneumonias • Acute inflammation of lung parenchyma • Bacterial pneumonia – High fever, nasal flaring, retractions – Rx-antibiotics – Consolidation, air entry, rales & rhonchi, dullness on percussion
• Viral Pneumonia – Most common ; patchy or diffuse infiltration – Mild fever, malaise – Rales & rhonchi – Rx-no antibiotics Chlamydial Pneumonia § ages 1 -3 months severe, diffuse § Persistent cough & dyspnea § Rx - Erythromycin for 14 -21 days

Viral – most common type of pneumonia -RSV, parainfluenza, adenovirus -Onset acute or insidious Rx – promote oxygenation & comfort Primary Atypical -mycoplasma most common age 5 -12 Onset –fever, chills, myalgia, cough, crackles Rx –symptomatic –recovery 7 -10 days
Respiratory Therapy • Oxygen–cannula, masks, tent 30 -50% – Oxygen toxicity, CO 2 narcosis • Aerosols • Bronchodilators, steroids, antibiotics • Nebulizers, metered dose inhaler, aerochamber • Ventilators, Resuscibags, CPAP, IPPB, Bi. Pap( watch CD for text, Animation) • Endotracheal airways, tacheostomy • Suctioning
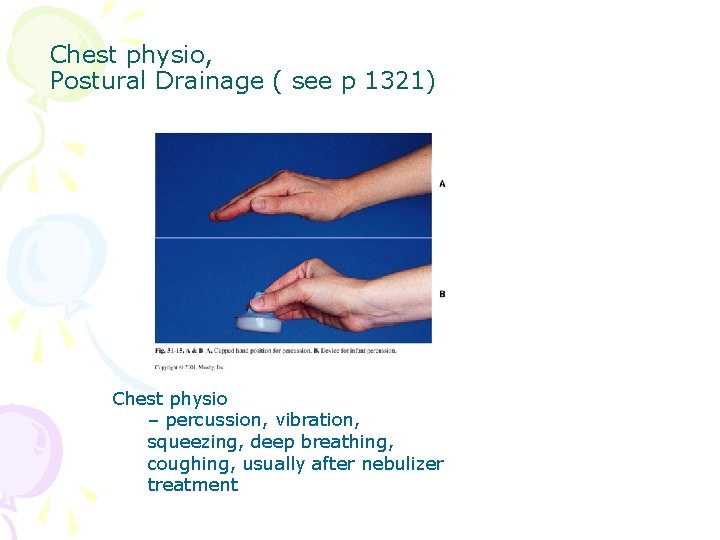
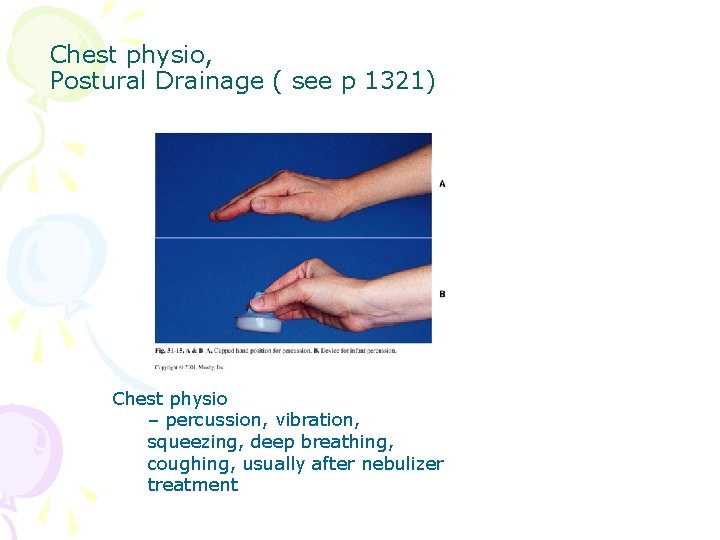
Chest physio, Postural Drainage ( see p 1321) Chest physio – percussion, vibration, squeezing, deep breathing, coughing, usually after nebulizer treatment

CYSTIC FIBROSIS

CYSTIC FIBROSIS • Genetic anomaly defect on Chromosome 7 • Discovered in Canada- HSC, Windsor Family( Nadan) helped as 4 generations available for gene testing • Mostly a Caucasian defect • Systemic effect defect in chloride transport and use on cell membrane
Cystic Fibrosis (CF) • Exocrine gland dysfunction that produces multisystem involvement • Most common lethal genetic illness among white children • Approximately 3% of U. S. white population are symptom-free carriers
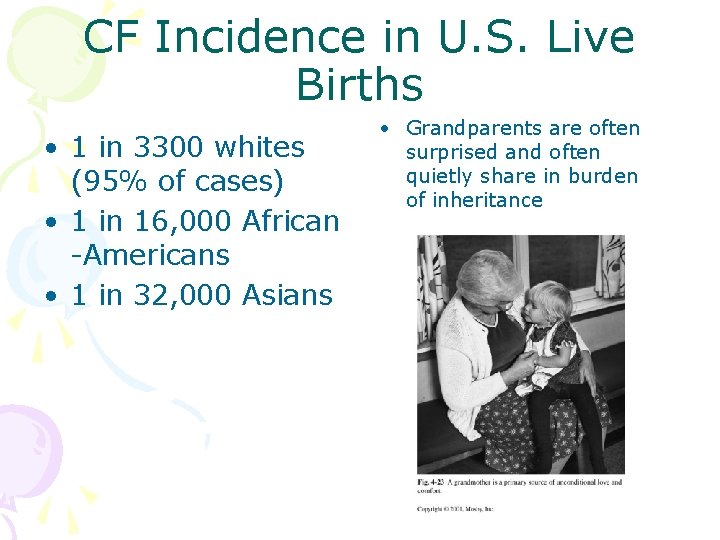
CF Incidence in U. S. Live Births • 1 in 3300 whites (95% of cases) • 1 in 16, 000 African -Americans • 1 in 32, 000 Asians • Grandparents are often surprised and often quietly share in burden of inheritance

Etiology • Autosomal recessive trait • Inherits defective gene from both parents with an overall incidence of 1: 4
Pathophysiology • Characterized by several unrelated clinical features
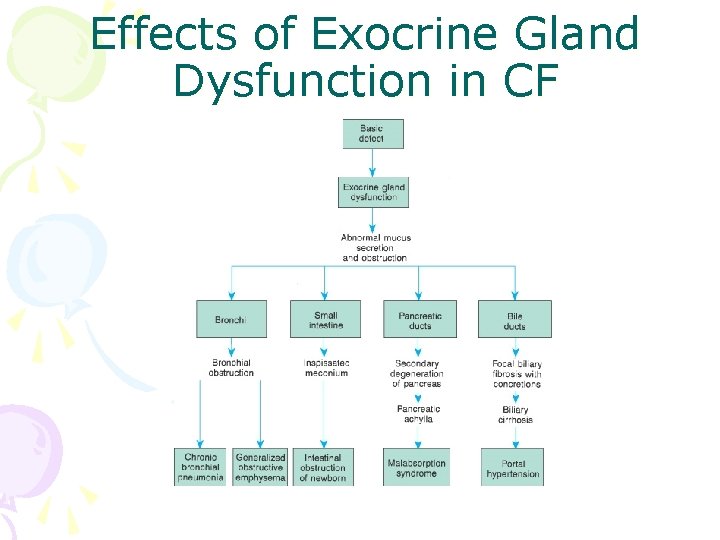
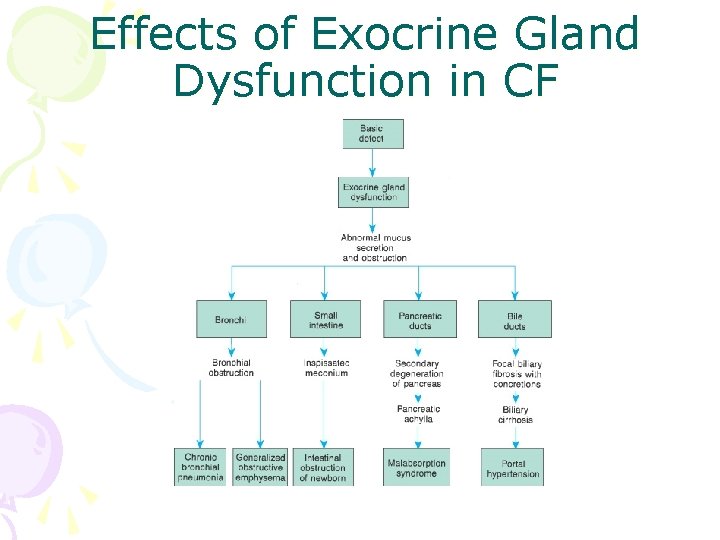
Effects of Exocrine Gland Dysfunction in CF
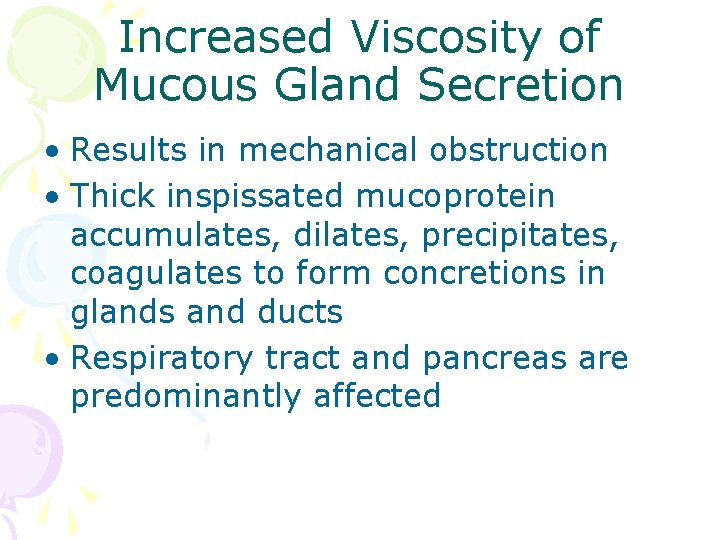
Increased Viscosity of Mucous Gland Secretion • Results in mechanical obstruction • Thick inspissated mucoprotein accumulates, dilates, precipitates, coagulates to form concretions in glands and ducts • Respiratory tract and pancreas are predominantly affected
Increased Sweat Electrolytes • Basis of the most reliable diagnostic procedure—sweat chloride test • Sodium and chloride will be two to five times greater than the controls
Other Factors • Increased organic/enzymatic constituents of saliva • Abnormalities of the autonomic nervous system
Respiratory Manifestations • Present in almost all CF patients, but onset/extent is variable • Stagnation of mucus and bacterial colonization result in destruction of lung tissue • Tenacious secretions are difficult to expectorate—obstruct bronchi/bronchioles
Respiratory Manifestations (cont. ) • Decreased O 2/CO 2 exchange • Results in hypoxia, hypercapnea, acidosis • Compression of the pulmonary blood vessels and progressive lung dysfunction lead to pulmonary hypertension, cor pulmonale, respiratory failure, and death

Infectious Pathogens • Pseudomonas aeruginosa • Burkholderia cepacia • Staphylococcus aureus • Haemophilus influenzae • Escherichia coli • Klebsiella pneumoniae
Respiratory Progression • Gradual progression follows chronic infection • Bronchial epithelium is destroyed • Infection spreads to peribronchial tissues, weakening bronchial walls • Peribronchial fibrosis • Decreased O 2/CO 2 exchange
Further Respiratory Progression • Chronic hypoxemia causes contraction/hypertrophy of muscle fibers in pulmonary arteries/arterioles • Pulmonary hypertension • Cor pulmonale • Pneumothorax • Hemoptysis
GI Tract • Thick secretions block ducts → cystic dilation → degeneration → diffuse fibrosis • Prevents pancreatic enzymes from reaching duodenum • Impaired digestion/absorption of fat → steatorrhea • Impaired digestion/absorption of protein → azotorrhea
GI Tract (cont. ) • Endocrine function of pancreas initially stays unchanged • Eventually pancreatic fibrosis occurs; may result in diabetes mellitus • Focal biliary obstruction results in multilobular biliary cirrhosis • Impaired salivation


Clinical Manifestations • Pancreatic enzyme deficiency • Progressive COPD associated with infection • Sweat gland dysfunction • Failure to thrive • Increased weight loss despite increased appetite • Gradual respiratory deterioration

Presentation • Wheezing respiration, dry nonproductive cough • Generalized obstructive emphysema • Patchy atelectasis • Cyanosis • Clubbing of fingers and toes • Repeated bronchitis and pneumonia
Presentation (cont. ) • Meconium ileus • Distal intestinal obstruction syndrome • Excretion of undigested food in stool —increased bulk, frothy, and foul • Tissue wasting • Prolapse of the rectum
Diagnostic Evaluation • Quantitative sweat chloride test • Chest x-ray • PFT • Stool fat and/or enzyme analysis • Barium enema
Presentation (cont. ) • Delayed puberty in females • Sterility in males • Parents report children taste “salty” • Dehydration • Hyponatremic/hypochloremic alkalosis • Hypoalbuminemia

Goals • Prevent/minimize pulmonary complications • Adequate nutrition for growth • Assist in adapting to chronic illness
Respiratory Management • CPT • Bronchodilator medication • Forced expiration • Aggressive treatment of pulmonary infections • Home IV antibiotic therapy • Aerosolized antibiotics
Respiratory Management (cont. ) • Pneumothorax • Hemoptysis • Nasal polyps • Steroid use/non-steroidal antiinflammatory • Transplantation
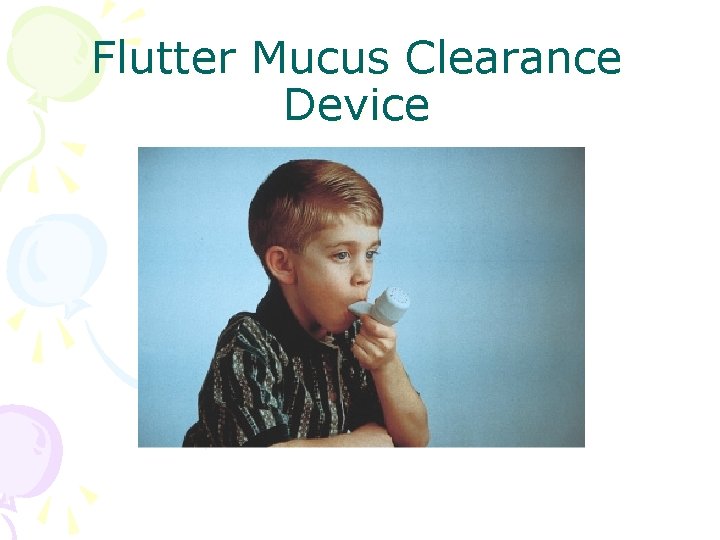
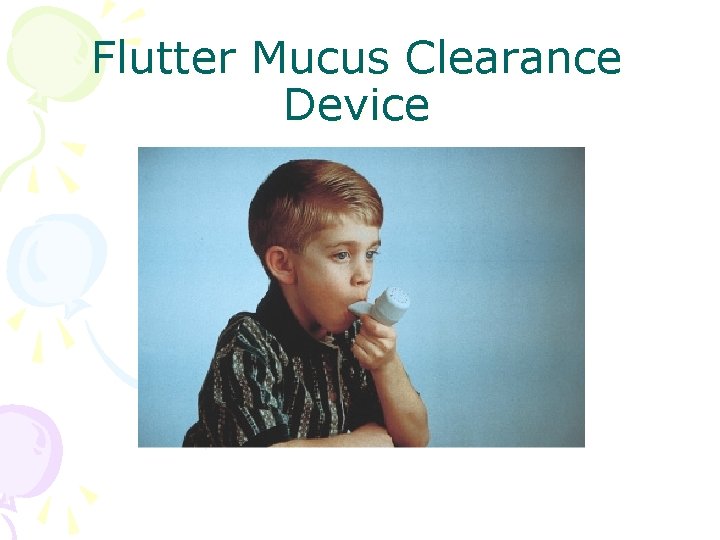
Flutter Mucus Clearance Device

GI Management • Replacement of pancreatic enzymes • High-protein, high-calorie diet as much as 150% RDA • Intestinal obstruction • Reduction of rectal prolapse • Salt supplementation
Family Support • Coping with emotional needs of child and family • Child requires treatments multiple times per day • Frequent hospitalization • Implications of genetic transmission of disease
Prognosis of CF • Estimated life expectancy for child born with CF in 2003 is 40 to 50 years • Maximize health potential – Nutrition – Prevention/early aggressive treatment of infection – Pulmonary hygiene
Prognosis of CF (cont. ) • New research—hope for the future – Gene therapy – Bilateral lung transplants – Improved pharmacologic agents
 Tripod position
Tripod position Cucaracha cucharita trabalenguas
Cucaracha cucharita trabalenguas Nero lead poisoning
Nero lead poisoning Lead poisoning children
Lead poisoning children Common factors that can lead to food poisoning
Common factors that can lead to food poisoning Blood smear
Blood smear Actor focus vs object focus
Actor focus vs object focus Focus on form vs focus on forms
Focus on form vs focus on forms Porters generic strategy
Porters generic strategy Differentiation cost leadership
Differentiation cost leadership Creative curriculum intentional teaching cards
Creative curriculum intentional teaching cards Toddler fever 102
Toddler fever 102 Amebiasis
Amebiasis Negativism in toddlers
Negativism in toddlers Socialization of toddlers worksheet answers
Socialization of toddlers worksheet answers Best travel toys for toddlers
Best travel toys for toddlers Milk for toddlers with milk allergynon dairy
Milk for toddlers with milk allergynon dairy Play definition
Play definition Night terror
Night terror Week by week plans for documenting children's development
Week by week plans for documenting children's development Cse smart class
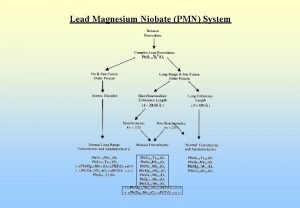
Cse smart class Lead magnesium niobate/lead titanate
Lead magnesium niobate/lead titanate Pica politeísta
Pica politeísta Dr teresa pica
Dr teresa pica Vue pica
Vue pica Gregorio de matos pica flor
Gregorio de matos pica flor Contemporary perspectives
Contemporary perspectives Ni la víbora me pica ni quema mi frente el sol
Ni la víbora me pica ni quema mi frente el sol Dr teresa pica
Dr teresa pica Pica griega
Pica griega La piedra feliz leyenda
La piedra feliz leyenda De pica
De pica Pica bibliothekssoftware
Pica bibliothekssoftware Virelangue portugais
Virelangue portugais Division en cantos de la epopeya
Division en cantos de la epopeya Epiteto epico
Epiteto epico Pica tamu
Pica tamu Pica griega
Pica griega Kalkulacija cijena primjer
Kalkulacija cijena primjer Sarah pica
Sarah pica Maladie du pica
Maladie du pica Pata peta pita pota trabalenguas
Pata peta pita pota trabalenguas Picerija mahir
Picerija mahir Sso
Sso Aica pica sca
Aica pica sca Symptoms of pica
Symptoms of pica Wobbler syndroom paard
Wobbler syndroom paard Foodafactoflife
Foodafactoflife Certified defenses for data poisoning attacks
Certified defenses for data poisoning attacks Temazolam
Temazolam Hygronium drug
Hygronium drug Methanol poisoning
Methanol poisoning Dioxin poisoning
Dioxin poisoning Pyrethroid poisoning
Pyrethroid poisoning Chapter 16:5 providing first aid for poisoning
Chapter 16:5 providing first aid for poisoning Cyanide poisoning
Cyanide poisoning Gastroenterritis
Gastroenterritis Chapter 17.11 providing first aid for sudden illness
Chapter 17.11 providing first aid for sudden illness Seo poisoning wikipedia
Seo poisoning wikipedia Poisoning that disables the na+/k+ pump would
Poisoning that disables the na+/k+ pump would Food poisoning
Food poisoning Was edgar allan poe an alcoholic
Was edgar allan poe an alcoholic Barbiturates classification
Barbiturates classification Diya kaduru
Diya kaduru What does carbonara smell like
What does carbonara smell like Mercury poisoning symptoms
Mercury poisoning symptoms Dh-mo-1
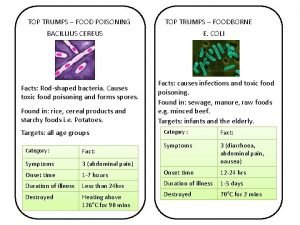
Dh-mo-1 Top trumps food
Top trumps food Food poisoning or hangover
Food poisoning or hangover Food poisoning cause
Food poisoning cause Dose of atropine in op poisoning
Dose of atropine in op poisoning Rip, ospf, bgp
Rip, ospf, bgp Satirical argument
Satirical argument Dimethoate poisoning
Dimethoate poisoning Recursive name server
Recursive name server Alcohol poisoning
Alcohol poisoning Food poisoning cause
Food poisoning cause Dose of atropine in op poisoning
Dose of atropine in op poisoning Diya kaduru tree
Diya kaduru tree Icd 10 intoksikasi makanan
Icd 10 intoksikasi makanan Atropine action
Atropine action Lesson plan on food poisoning
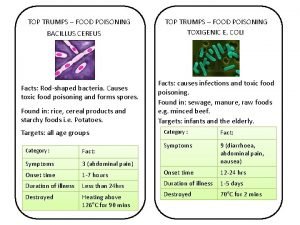
Lesson plan on food poisoning B. cereus food poisoning
B. cereus food poisoning Jim holliman
Jim holliman Dns cache poisoning attack tutorial
Dns cache poisoning attack tutorial Arp cache poisoning attack fix
Arp cache poisoning attack fix General principle of treatment of poisoning
General principle of treatment of poisoning Organophosphate poisoning
Organophosphate poisoning Dioxin poisoning
Dioxin poisoning Oxygen poisoning
Oxygen poisoning Chapter 17:7 providing first aid for heat exposure
Chapter 17:7 providing first aid for heat exposure Poisoning the well
Poisoning the well Prinso poisoning
Prinso poisoning Oxygen therapy
Oxygen therapy Curare poisoning
Curare poisoning Gamaxin powder poisoning
Gamaxin powder poisoning Dioxin poisoning
Dioxin poisoning Carbon monoxide poisoning
Carbon monoxide poisoning Whats a focus group
Whats a focus group Focus or ongoing assessment
Focus or ongoing assessment Did you see the letter it came yesterday morning
Did you see the letter it came yesterday morning Focus on the family malaysia
Focus on the family malaysia Radiographic grid
Radiographic grid Stop tb
Stop tb Language focus
Language focus Focus module
Focus module Focus flare design thinking
Focus flare design thinking Language focus
Language focus Camtasia smart focus
Camtasia smart focus