Webinar 1 Introduction to virtual training Basics of
Webinar 1: Introduction to virtual training Basics of COVID-19 and why it matters to the workforce Increased protection risks during COVID-19 Webinar Training 17 th November, 2020
Opening remarks Overall aim of the training programme: To support the ongoing strengthening of Uganda’s social service workforce, with a particular emphasis on professional practitioners who work to protect and support children, women and families who are at risk of/have experienced protection concerns in the context of COVID-19.
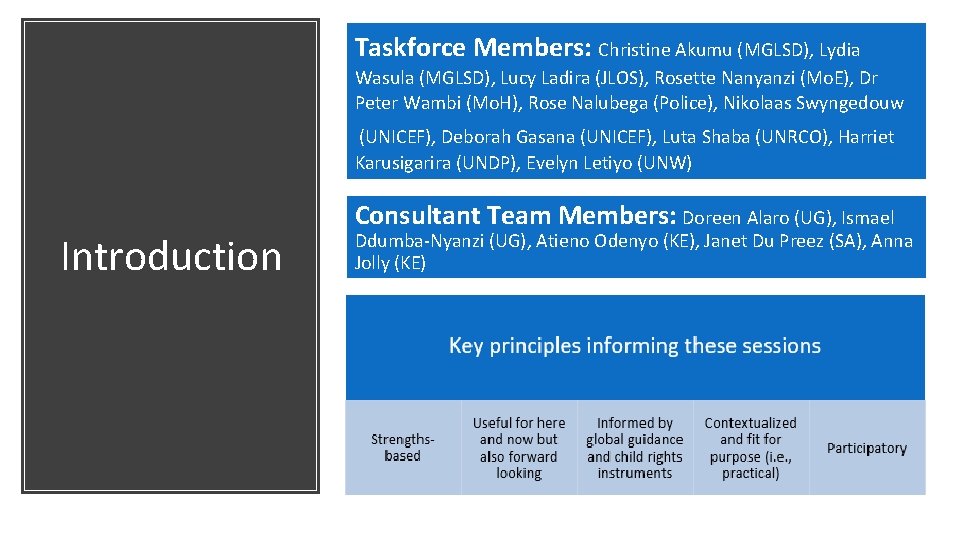
Taskforce Members: Christine Akumu (MGLSD), Lydia Wasula (MGLSD), Lucy Ladira (JLOS), Rosette Nanyanzi (Mo. E), Dr Peter Wambi (Mo. H), Rose Nalubega (Police), Nikolaas Swyngedouw (UNICEF), Deborah Gasana (UNICEF), Luta Shaba (UNRCO), Harriet Karusigarira (UNDP), Evelyn Letiyo (UNW) Introduction Consultant Team Members: Doreen Alaro (UG), Ismael Ddumba-Nyanzi (UG), Atieno Odenyo (KE), Janet Du Preez (SA), Anna Jolly (KE)
Chat box – asking and responding to questions Muting/unmuting your mic Getting to know Zoom Turning on/off your video Small group discussions (break out sessions) Post webinar survey
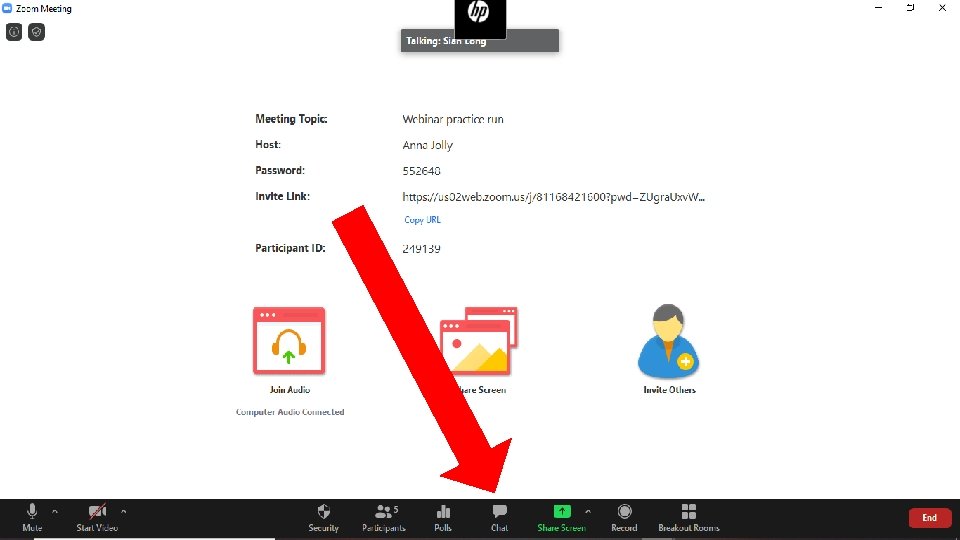
Chat box – asking and responding to questions Muting/unmuting your mic Getting to know Zoom Turning on/off your video Small group discussions (break out sessions) Post webinar survey
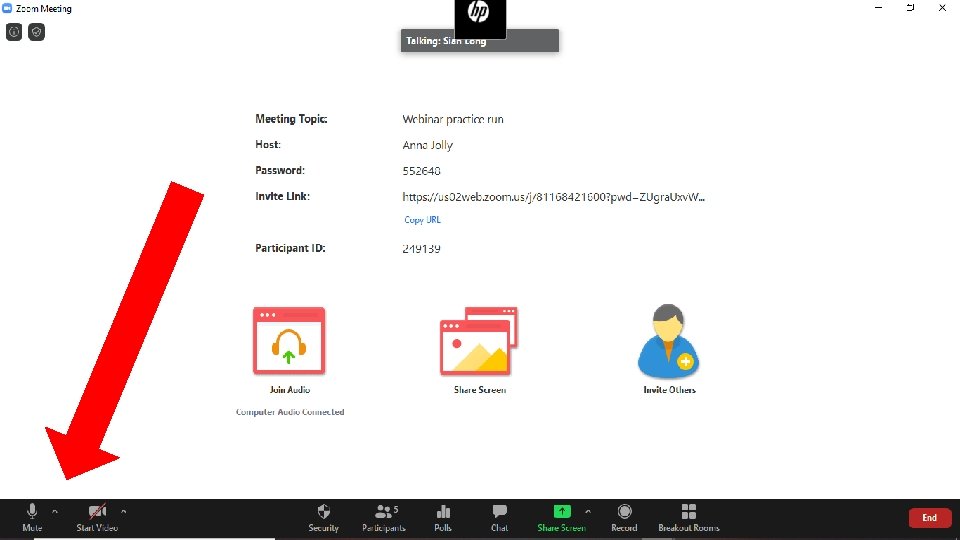
Chat box – asking and responding to questions Muting/unmuting your mic Getting to know Zoom Turning on/off your video Small group discussions (break out sessions) Post webinar survey

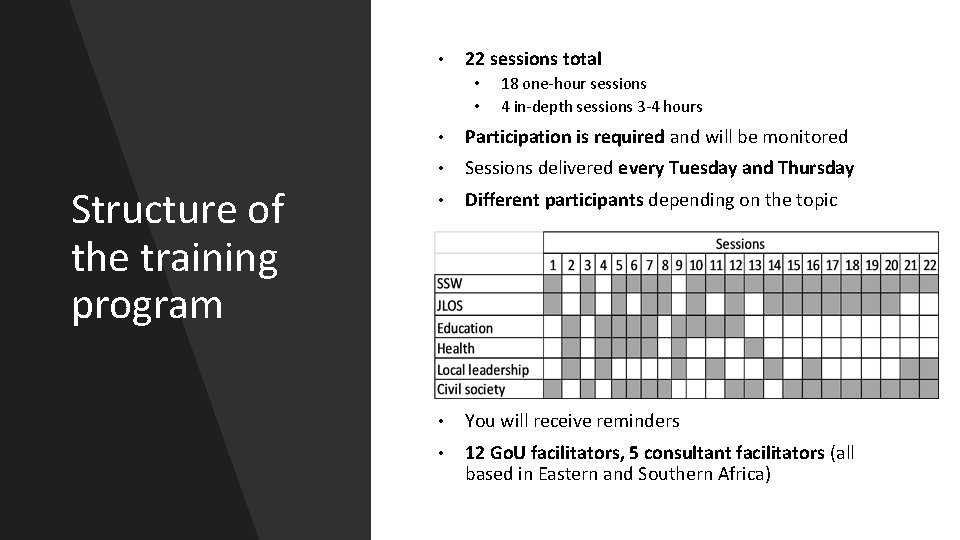
• 22 sessions total • • Structure of the training program 18 one-hour sessions 4 in-depth sessions 3 -4 hours • Participation is required and will be monitored • Sessions delivered every Tuesday and Thursday • Different participants depending on the topic • You will receive reminders • 12 Go. U facilitators, 5 consultant facilitators (all based in Eastern and Southern Africa)
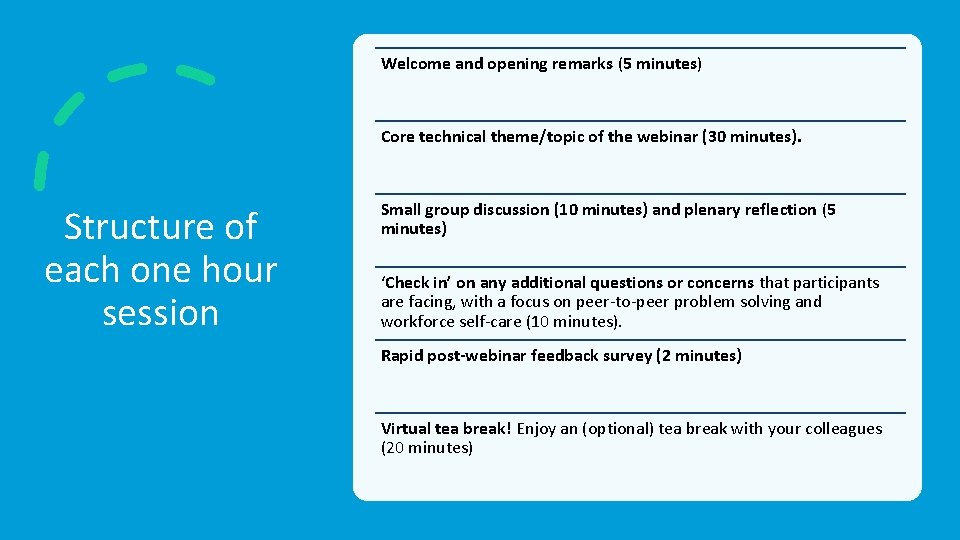
Welcome and opening remarks (5 minutes) Core technical theme/topic of the webinar (30 minutes). Structure of each one hour session Small group discussion (10 minutes) and plenary reflection (5 minutes) ‘Check in’ on any additional questions or concerns that participants are facing, with a focus on peer-to-peer problem solving and workforce self-care (10 minutes). Rapid post-webinar feedback survey (2 minutes) Virtual tea break! Enjoy an (optional) tea break with your colleagues (20 minutes)
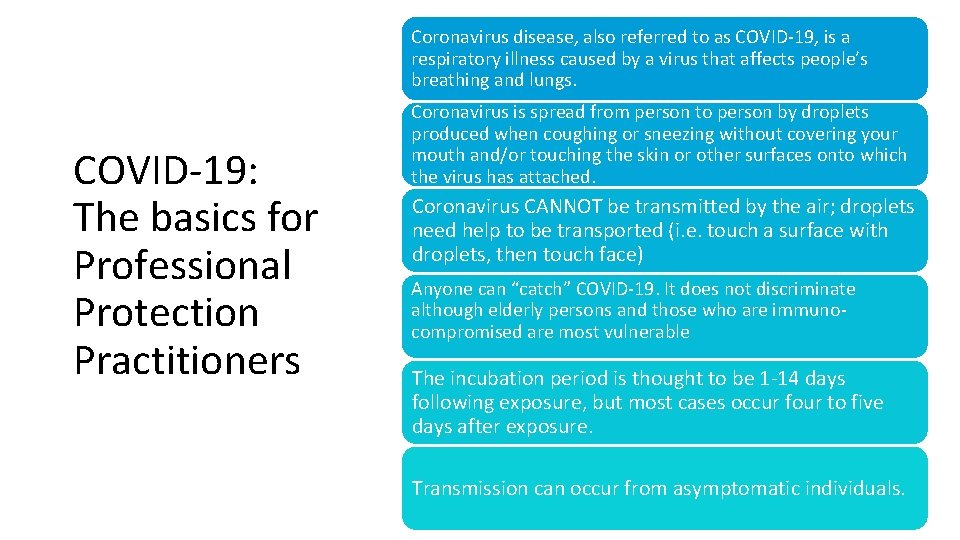
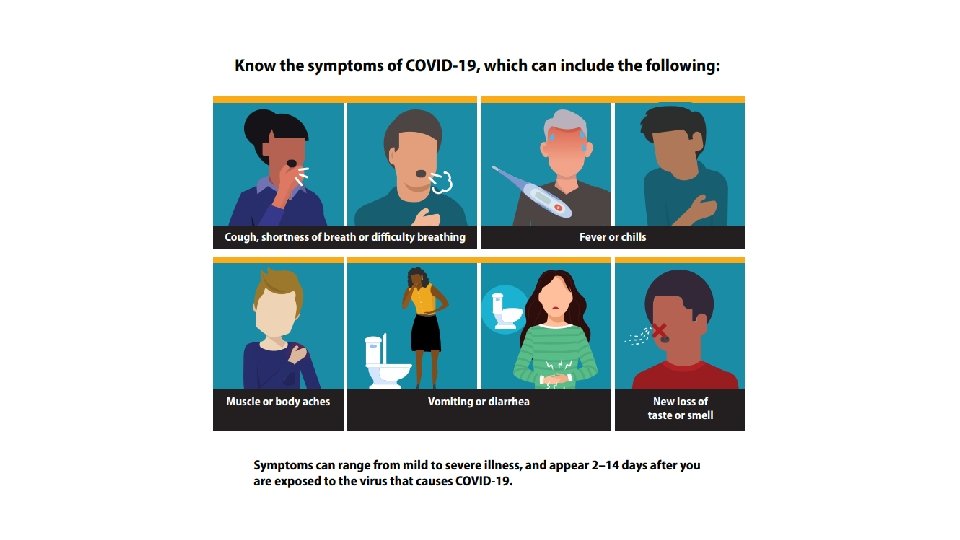
Coronavirus disease, also referred to as COVID-19, is a respiratory illness caused by a virus that affects people’s breathing and lungs. COVID-19: The basics for Professional Protection Practitioners Coronavirus is spread from person to person by droplets produced when coughing or sneezing without covering your mouth and/or touching the skin or other surfaces onto which the virus has attached. Coronavirus CANNOT be transmitted by the air; droplets need help to be transported (i. e. touch a surface with droplets, then touch face) Anyone can “catch” COVID-19. It does not discriminate although elderly persons and those who are immunocompromised are most vulnerable The incubation period is thought to be 1 -14 days following exposure, but most cases occur four to five days after exposure. Transmission can occur from asymptomatic individuals.
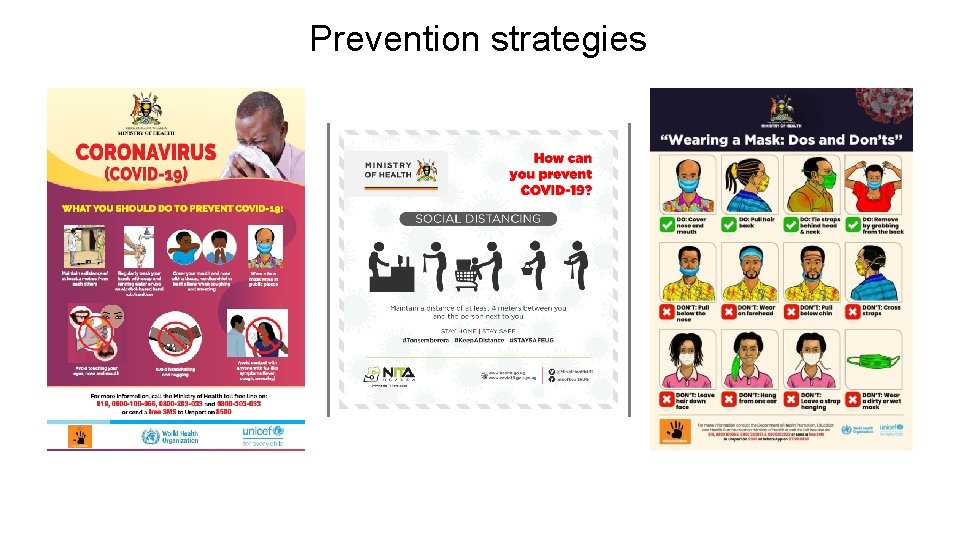
Prevention strategies
Chat box Where do you access reliable information?
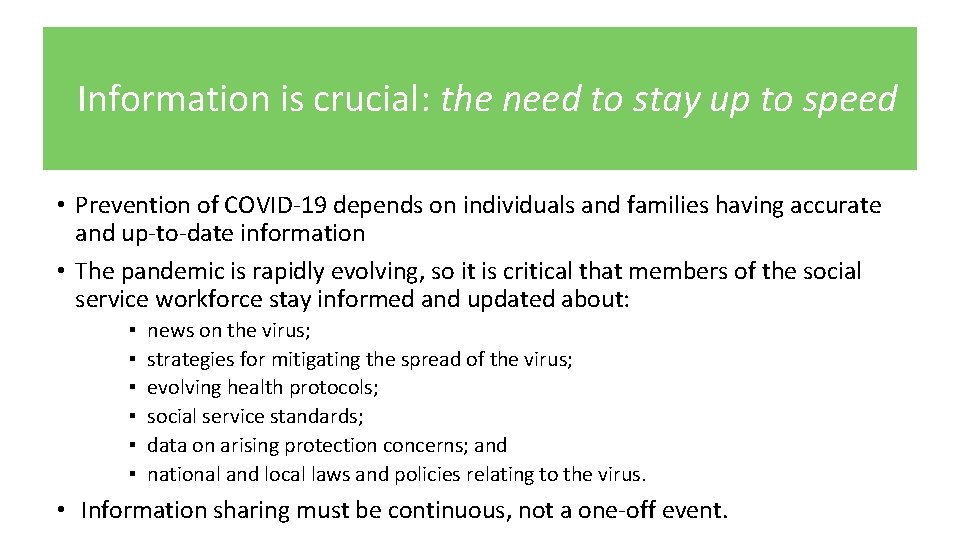
Information is crucial: the need to stay up to speed • Prevention of COVID-19 depends on individuals and families having accurate and up-to-date information • The pandemic is rapidly evolving, so it is critical that members of the social service workforce stay informed and updated about: ▪ ▪ ▪ news on the virus; strategies for mitigating the spread of the virus; evolving health protocols; social service standards; data on arising protection concerns; and national and local laws and policies relating to the virus. • Information sharing must be continuous, not a one-off event.
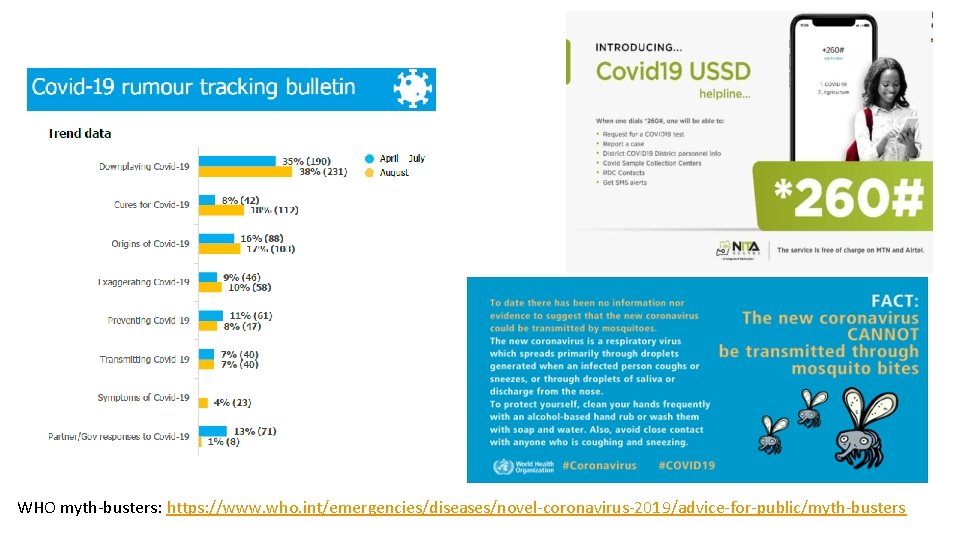
WHO myth-busters: https: //www. who. int/emergencies/diseases/novel-coronavirus-2019/advice-for-public/myth-busters
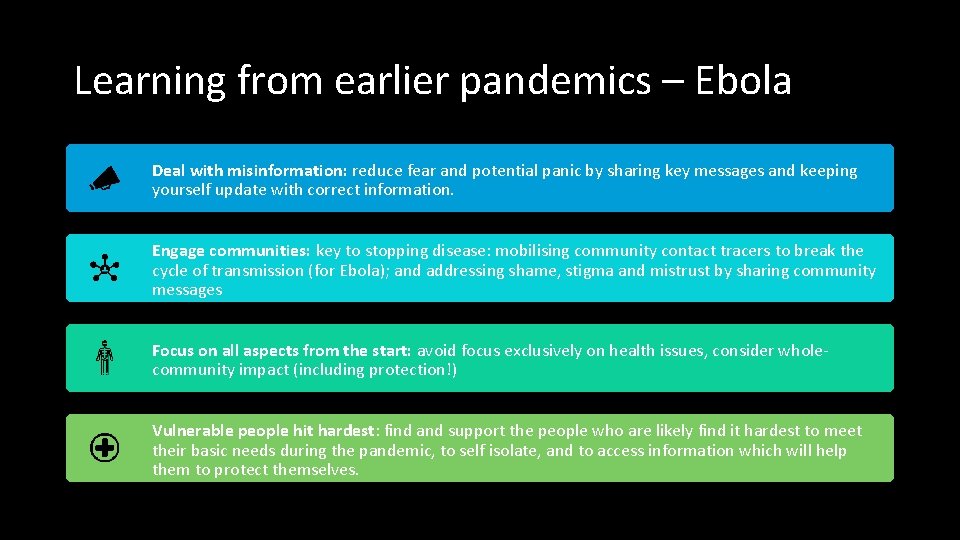
Learning from earlier pandemics – Ebola Deal with misinformation: reduce fear and potential panic by sharing key messages and keeping yourself update with correct information. Engage communities: key to stopping disease: mobilising community contact tracers to break the cycle of transmission (for Ebola); and addressing shame, stigma and mistrust by sharing community messages Focus on all aspects from the start: avoid focus exclusively on health issues, consider wholecommunity impact (including protection!) Vulnerable people hit hardest: find and support the people who are likely find it hardest to meet their basic needs during the pandemic, to self isolate, and to access information which will help them to protect themselves.
We must: Considerations for the workforce ▪ Understand what COVID-19 is, the risks that our target populations face, how to prevent infection and what to do if someone has symptoms. ▪ Be a leader in your community and model good behaviour, including addressing stigma or myths. ▪ Work to keep clients healthy and safe when you have to work virtually. ▪ Keep yourself and your own family safe and healthy.
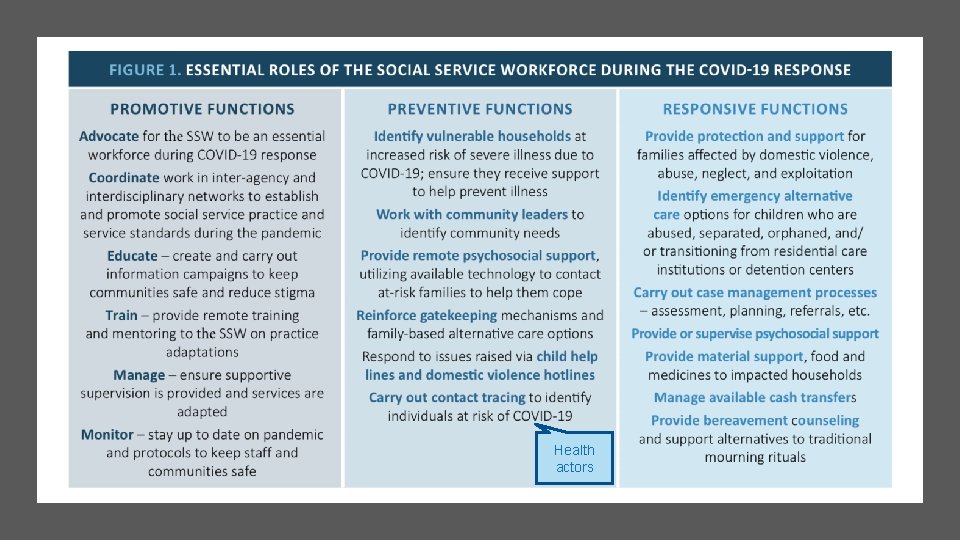
Health actors
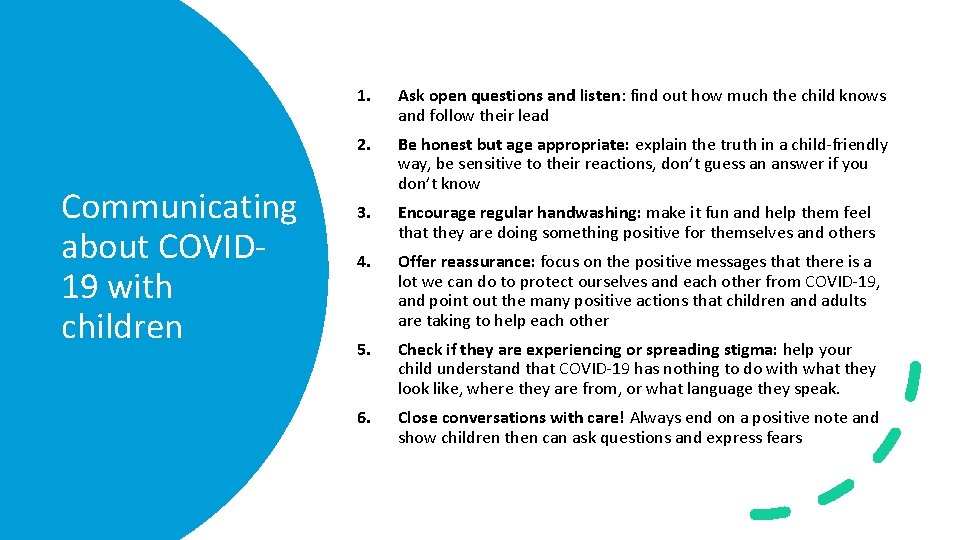
Communicating about COVID 19 with children 1. Ask open questions and listen: find out how much the child knows and follow their lead 2. Be honest but age appropriate: explain the truth in a child-friendly way, be sensitive to their reactions, don’t guess an answer if you don’t know 3. Encourage regular handwashing: make it fun and help them feel that they are doing something positive for themselves and others 4. Offer reassurance: focus on the positive messages that there is a lot we can do to protect ourselves and each other from COVID-19, and point out the many positive actions that children and adults are taking to help each other 5. Check if they are experiencing or spreading stigma: help your child understand that COVID-19 has nothing to do with what they look like, where they are from, or what language they speak. 6. Close conversations with care! Always end on a positive note and show children then can ask questions and express fears
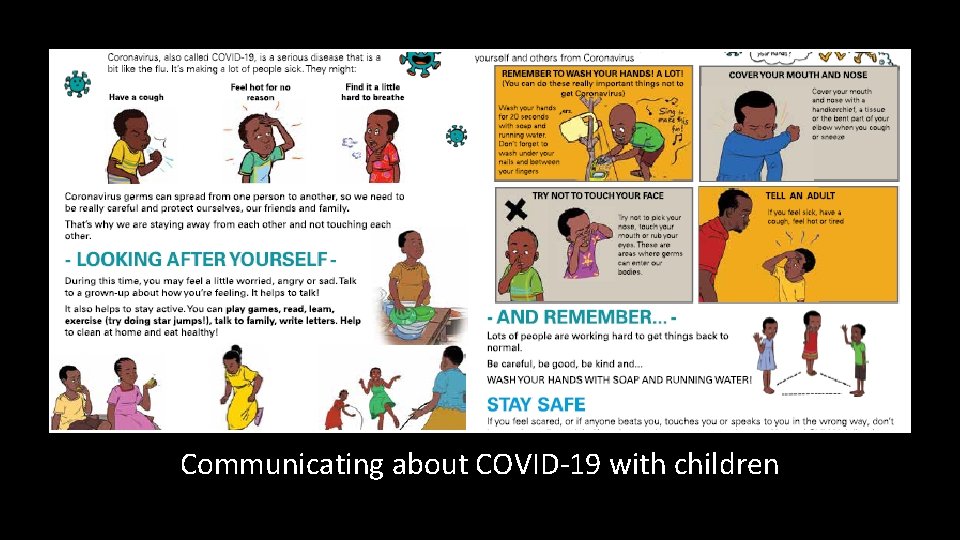
Communicating about COVID-19 with children
Chat box What advice would you offer your colleagues about how to discuss the pandemic with children?

BREAK TIME
How COVID-19 has quickly changed children, women’s and families’ lives Containment and social distancing measures have resulted in: ▪ Loss of income or reduced employment ▪ Increased pressure and stress at home ▪ Changes to income or employment (working from home) ▪ Increased caregiving duties ▪ More time spent at home generally ▪ Less physical connection to extended networks, and higher risk of social isolation ▪ Closures of school, community and religious functions and venues �� less access to safe spaces ▪ Reduced avenues for reporting of GBV and VAC cases (informal and formal) ▪ Some reduction in support services or diversion toward health services ▪ Prohibitions of families visiting children in alternative care and women in shelters ▪ Rapid reunification of children from institutions to families with little preparation or support
Chat box What has been the impact of these changes on the protection of children and women? https: //www. menti. com/n 3 s 21 p 9531
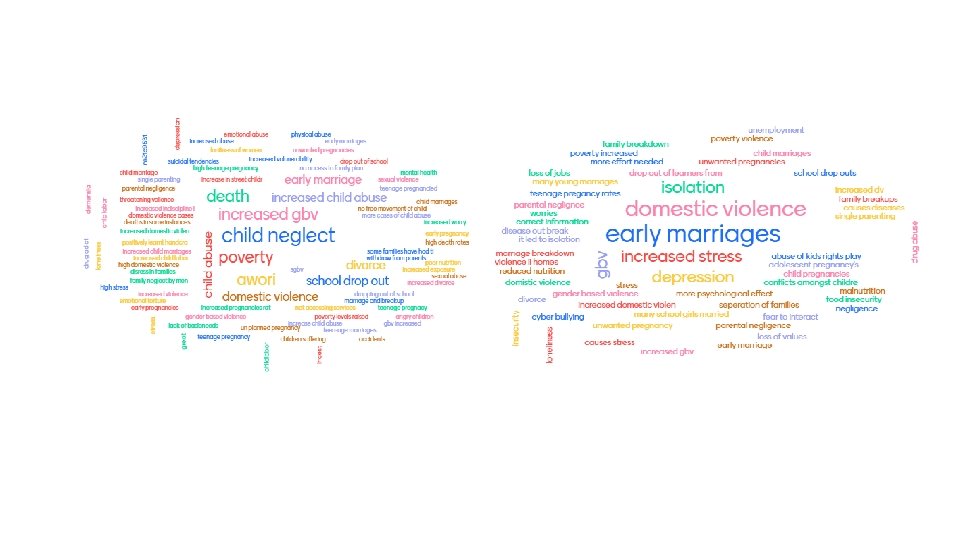
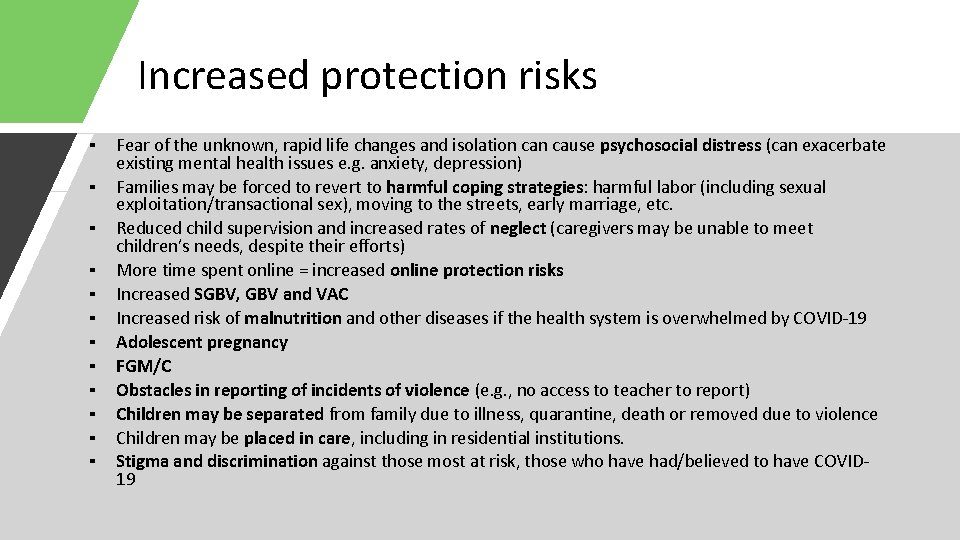
Increased protection risks ▪ ▪ ▪ Fear of the unknown, rapid life changes and isolation cause psychosocial distress (can exacerbate existing mental health issues e. g. anxiety, depression) Families may be forced to revert to harmful coping strategies: harmful labor (including sexual exploitation/transactional sex), moving to the streets, early marriage, etc. Reduced child supervision and increased rates of neglect (caregivers may be unable to meet children’s needs, despite their efforts) More time spent online = increased online protection risks Increased SGBV, GBV and VAC Increased risk of malnutrition and other diseases if the health system is overwhelmed by COVID-19 Adolescent pregnancy FGM/C Obstacles in reporting of incidents of violence (e. g. , no access to teacher to report) Children may be separated from family due to illness, quarantine, death or removed due to violence Children may be placed in care, including in residential institutions. Stigma and discrimination against those most at risk, those who have had/believed to have COVID 19
How to prevent protection risks and violations ▪ Disseminate information about increased protection risks via local radio; equip communities to know what to look/listen for ▪ Collaborate with community-level actors to support identification of vulnerable children, women, families (e. g. , CPVs, CHVs, chiefs, women’s groups leaders, religious or cultural leaders, etc. ) ▪ Coordinate with others and make referrals to help meet client’s urgent basic needs e. g. , emergency food provision ▪ Provide guidance e. g. , share WHO positive parenting materials aimed at preventing VAC, guidance on positive communication in intimate relationships, etc. ▪ Reinforce gatekeeping—encourage at-risk families TO NOT separate from their children. ▪ Mobilise community-level actors to support monitoring and call you if additional concerns
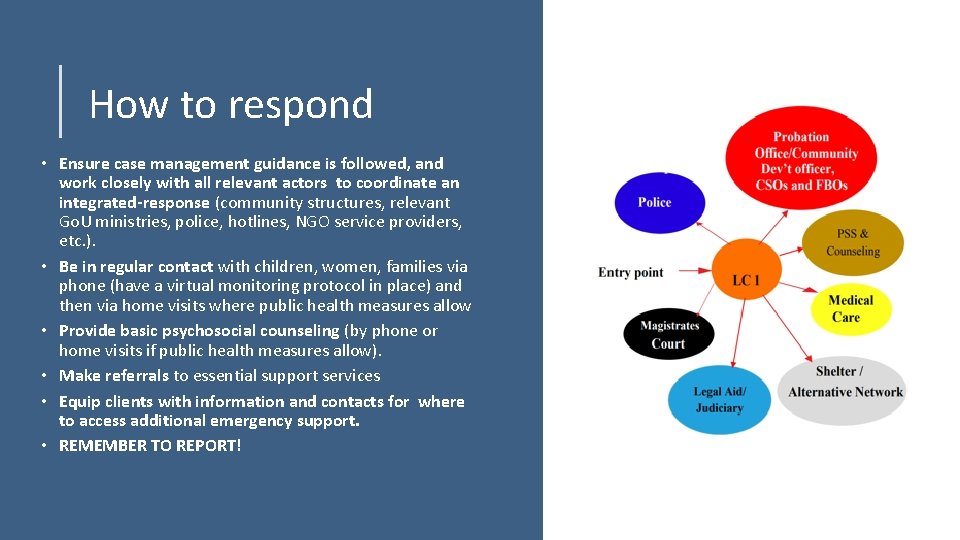
How to respond • Ensure case management guidance is followed, and work closely with all relevant actors to coordinate an integrated-response (community structures, relevant Go. U ministries, police, hotlines, NGO service providers, etc. ). • Be in regular contact with children, women, families via phone (have a virtual monitoring protocol in place) and then via home visits where public health measures allow • Provide basic psychosocial counseling (by phone or home visits if public health measures allow). • Make referrals to essential support services • Equip clients with information and contacts for where to access additional emergency support. • REMEMBER TO REPORT!
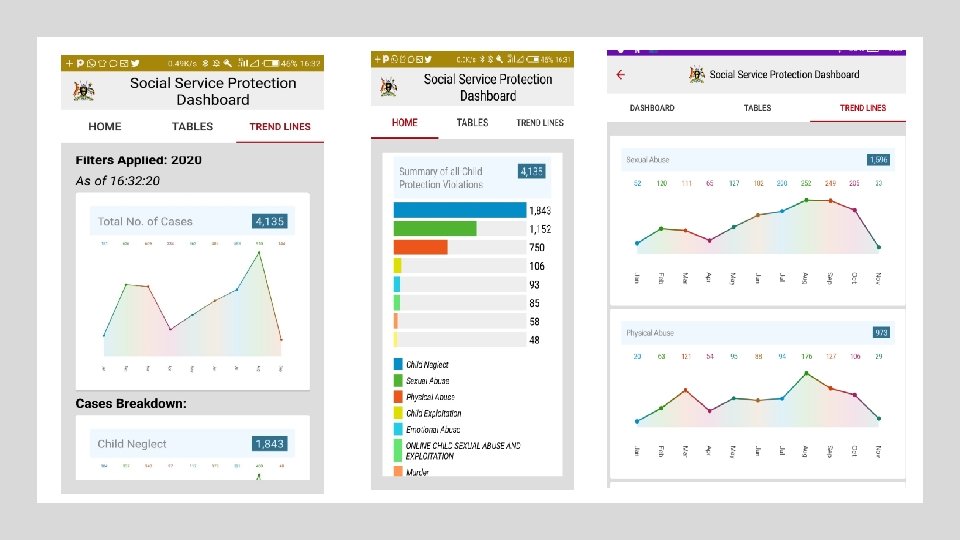
How to report ▪ ALL violence cases should be reported ▪ Child cases must be routinely entered into the OVCIMS ▪ This applies even when a report or a contact with child or family is virtual
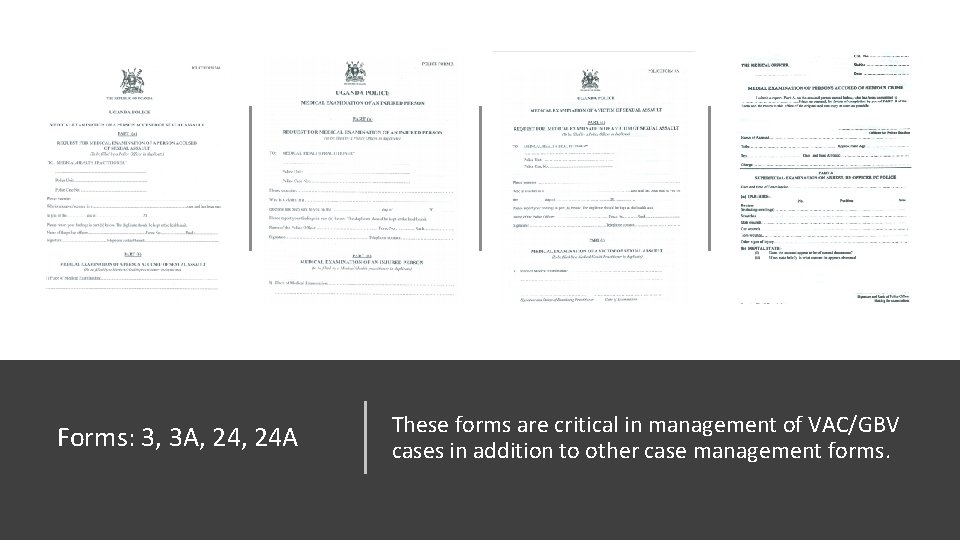
Forms: 3, 3 A, 24 A These forms are critical in management of VAC/GBV cases in addition to other case management forms.

Adapting to the pandemic through different stages As Uganda moves into transition and recovery, the following will occur: school reopening, transport increase, more economic activity. Consider the following: Addressing any fears as children, women and families re-engage with group activities Reassessing child, women and family risk and vulnerability to reflect any economic or social changes during the containment phase Assessing if and when community support services reopen, to support prevention and early interventions Planning case load and capacity to follow children, women and families if Uganda moves in and out of COVID-19 stages

Breakout time! Based on what you’ve learned in this webinar, how can you recognize increased protection risks or violations in your community and what action will you take? • Nominate one facilitator • Nominate one rapporteur • You have 10 minutes in your breakout room • Provide feedback on the three main points
Thank you!
Tea break! The zoom meeting will remain open for 10 minutes for anyone who wants an optional social catch up or to practice using zoom!
- Slides: 37