Warm Greetings Andhra Pradesh Making a difference in


- Slides: 26
Warm Greetings !! Andhra Pradesh – Making a difference ! in ICDS and IYCF Department for Women, Children, Disabled & Senior Citizens Government of Andhra Pradesh
Importance of Infant and Young Child Feeding (IYCF) practices Interventions for improving IYCF practices in Andhra Pradesh
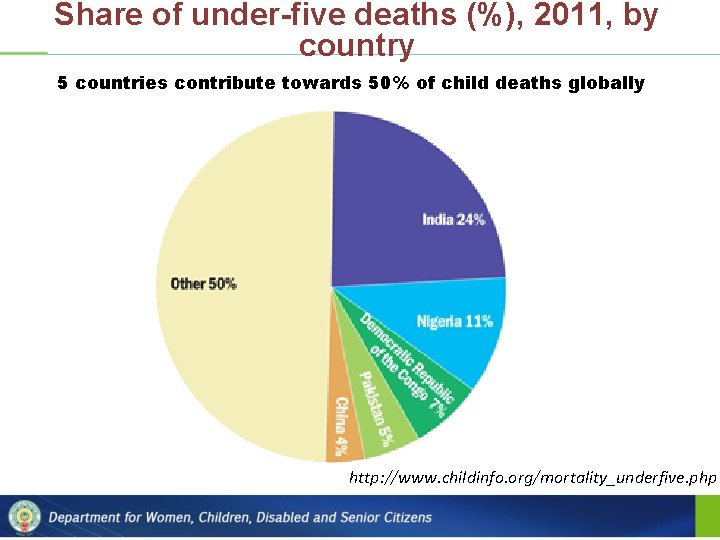
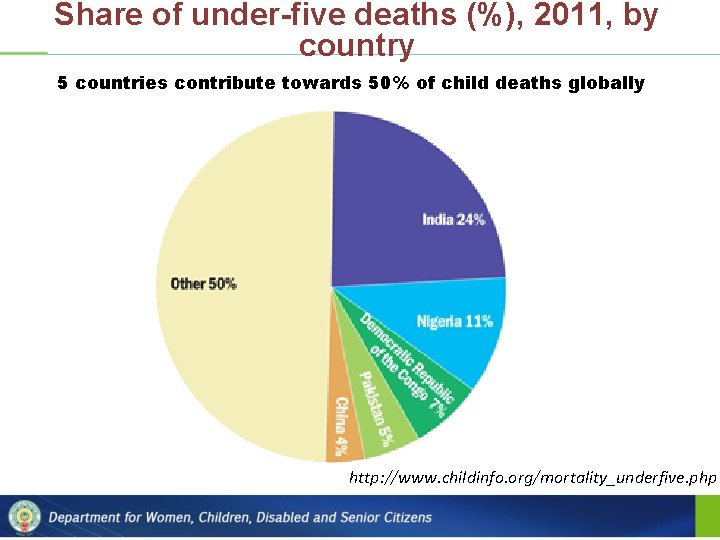
Share of under-five deaths (%), 2011, by country 5 countries contribute towards 50% of child deaths globally http: //www. childinfo. org/mortality_underfive. php
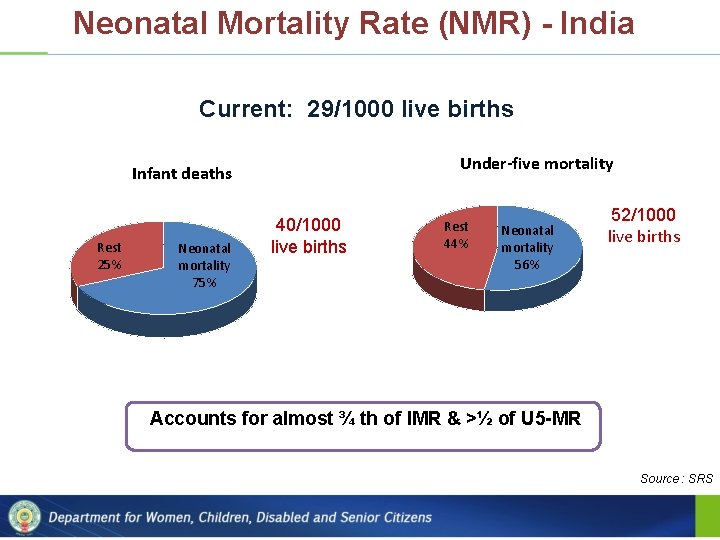
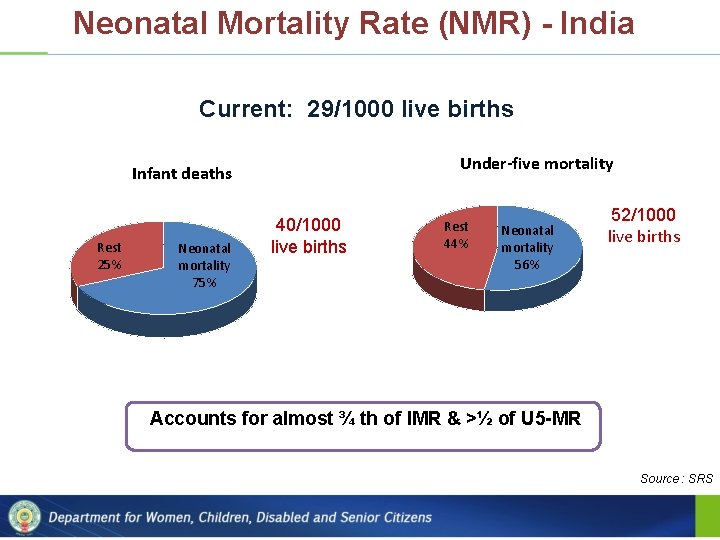
Neonatal Mortality Rate (NMR) - India Current: 29/1000 live births Under-five mortality Infant deaths Rest 25% Neonatal mortality 75% 40/1000 live births Rest 44% Neonatal mortality 56% 52/1000 live births Accounts for almost ¾ th of IMR & >½ of U 5 -MR Source : SRS
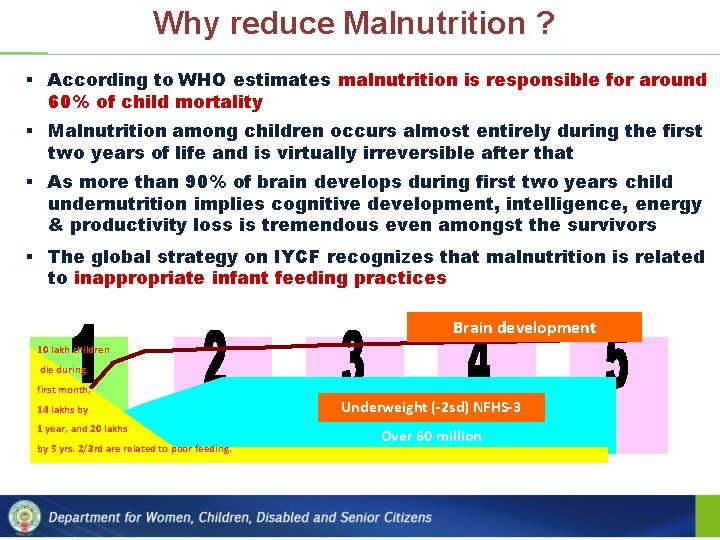
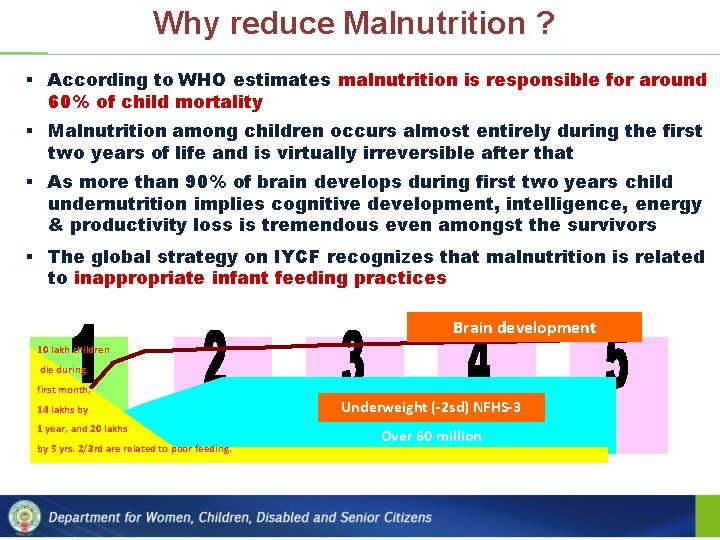
Why reduce Malnutrition ? § According to WHO estimates malnutrition is responsible for around 60% of child mortality § Malnutrition among children occurs almost entirely during the first two years of life and is virtually irreversible after that § As more than 90% of brain develops during first two years child undernutrition implies cognitive development, intelligence, energy & productivity loss is tremendous even amongst the survivors § The global strategy on IYCF recognizes that malnutrition is related to inappropriate infant feeding practices Brain development 10 lakh children die during first month, 14 lakhs by 1 year, and 20 lakhs by 5 yrs. 2/3 rd are related to poor feeding. Underweight (-2 sd) NFHS-3 Over 60 million
Optimal Infant and Young Child Feeding v Initiation of breastfeeding immediately after birth, preferably within one hour v Exclusive breastfeeding for 1 st six months i. e. , the infants receives only breast milk & nothing else, no other milk, food, drink or water v Appropriate and adequate complementary feeding after six months of age while continuing breastfeeding v Full Immunization for infants v Adequate nutrition for pregnant and lactating women
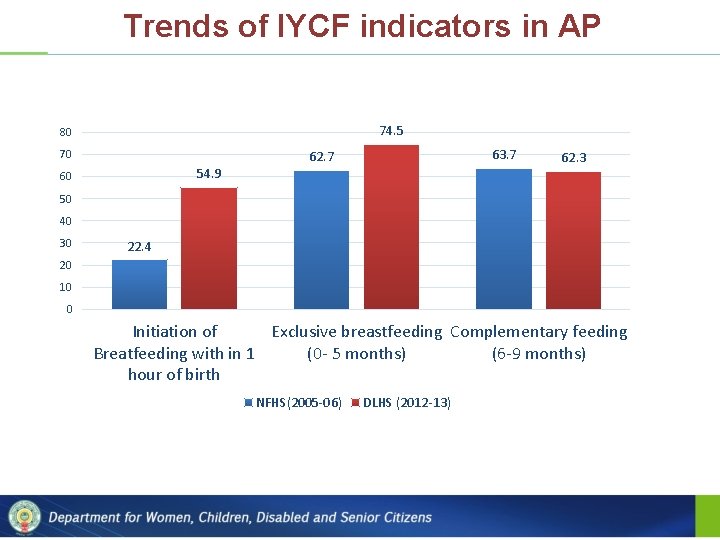
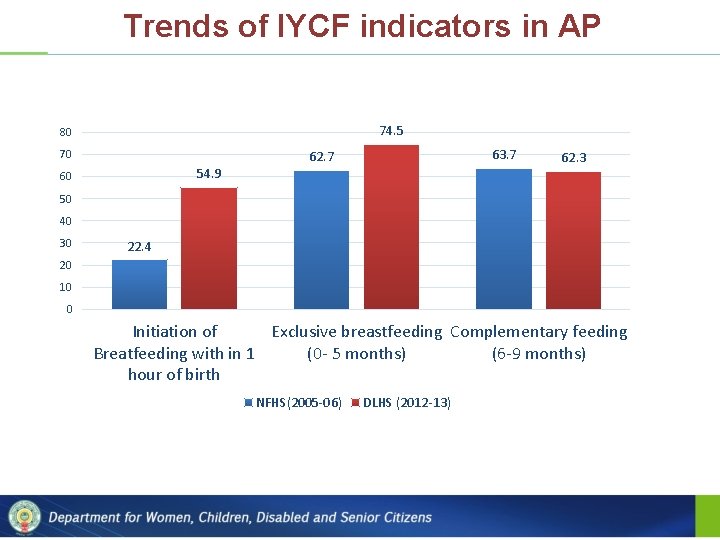
Trends of IYCF indicators in AP 74. 5 80 70 63. 7 62. 7 54. 9 60 62. 3 50 40 30 22. 4 20 10 0 Initiation of Exclusive breastfeeding Complementary feeding Breatfeeding with in 1 (0 - 5 months) (6 -9 months) hour of birth NFHS(2005 -06) DLHS (2012 -13)
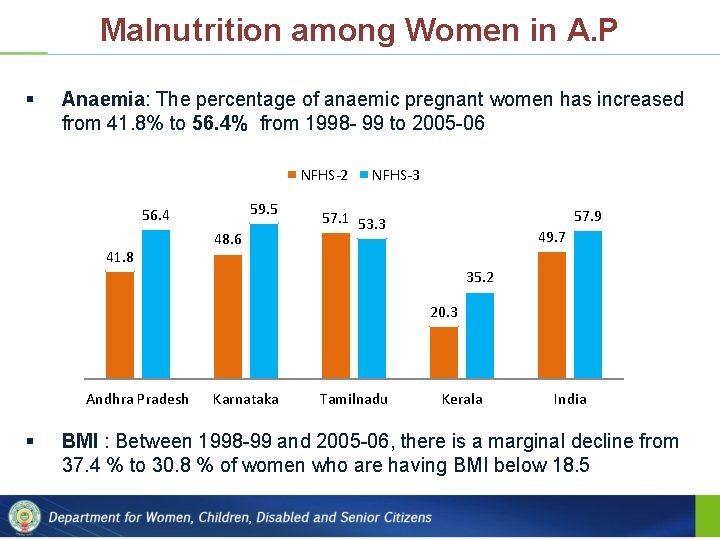
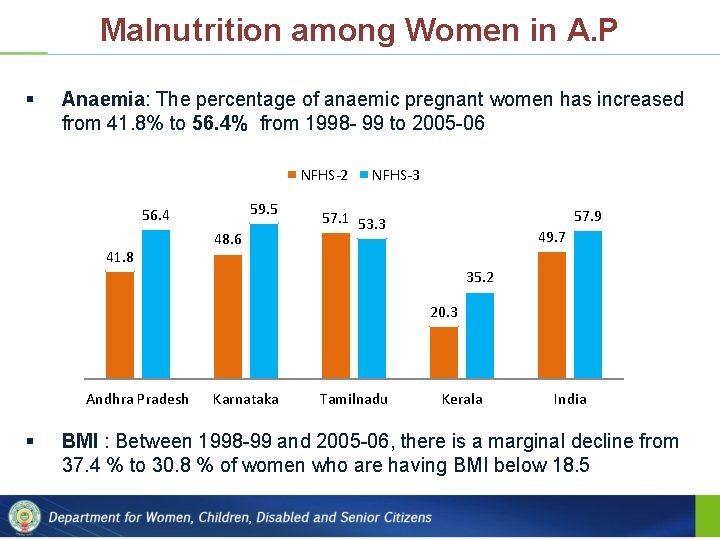
Malnutrition among Women in A. P § Anaemia: The percentage of anaemic pregnant women has increased from 41. 8% to 56. 4% from 1998 - 99 to 2005 -06 NFHS-2 59. 5 56. 4 41. 8 48. 6 NFHS-3 57. 9 57. 1 53. 3 49. 7 35. 2 20. 3 Andhra Pradesh § Karnataka Tamilnadu Kerala India BMI : Between 1998 -99 and 2005 -06, there is a marginal decline from 37. 4 % to 30. 8 % of women who are having BMI below 18. 5
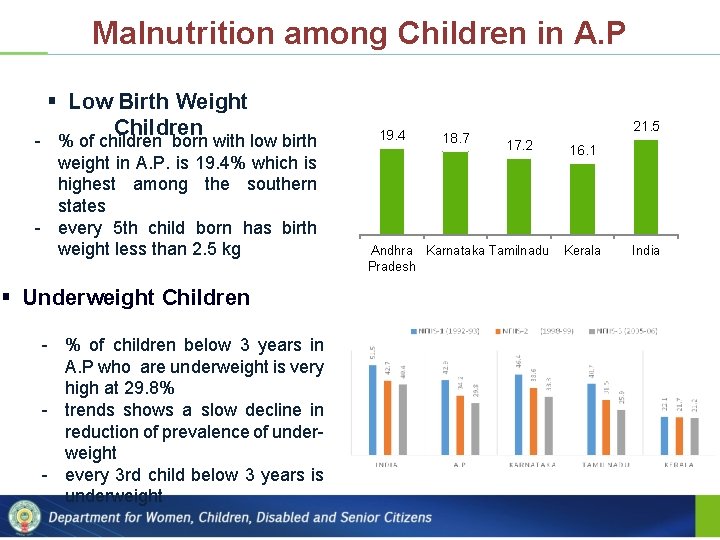
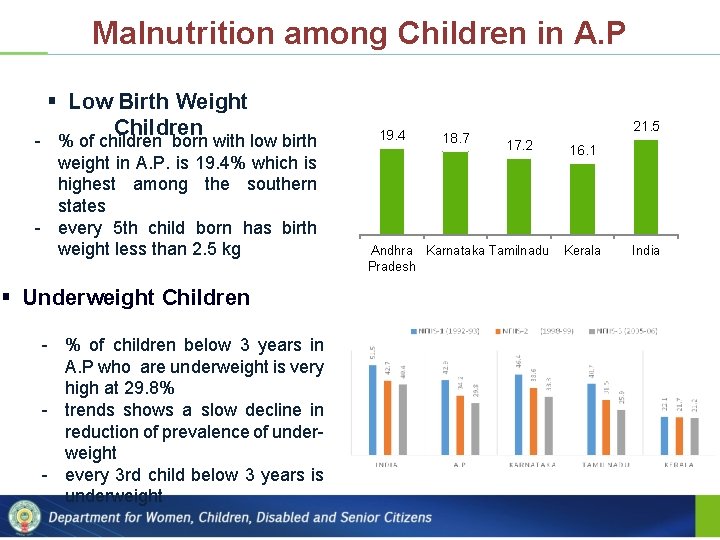
Malnutrition among Children in A. P § Low Birth Weight Children - % of children born with low birth weight in A. P. is 19. 4% which is highest among the southern states - every 5 th child born has birth weight less than 2. 5 kg § Underweight Children - % of children below 3 years in A. P who are underweight is very high at 29. 8% - trends shows a slow decline in reduction of prevalence of underweight - every 3 rd child below 3 years is underweight 19. 4 18. 7 21. 5 17. 2 Andhra Karnataka Tamilnadu Pradesh 16. 1 Kerala India
Interventions to improve IYCF Practices in AP – Special weaning food for children 7 months to 3 years and hot meal for children 3 to 6 years 1 Meaningful Food Models in ICDS – Supervised feeding for malnourished children – One full meal for pregnant and lactating women – Capacity building on skilled IYCF counselling through counselling courses 2 Intensified Health & Nutrition Education – Two Nutrition and Health Days (NHD), one for growth monitoring and other for health services – A convergence initiative of allied depts. with community
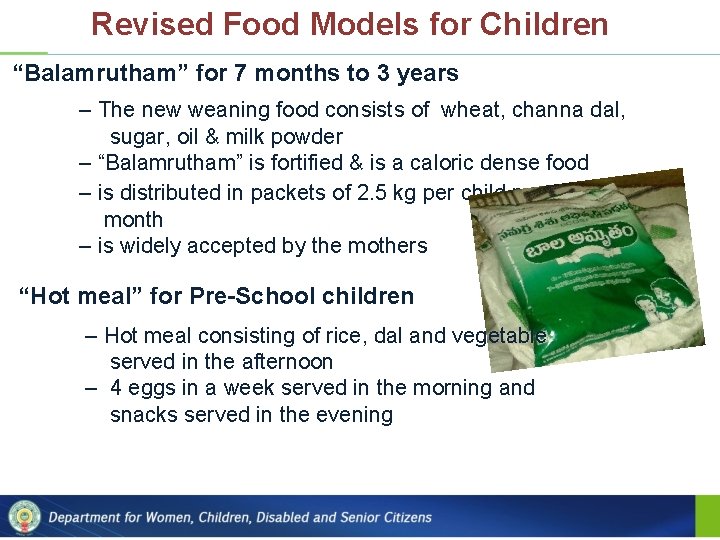
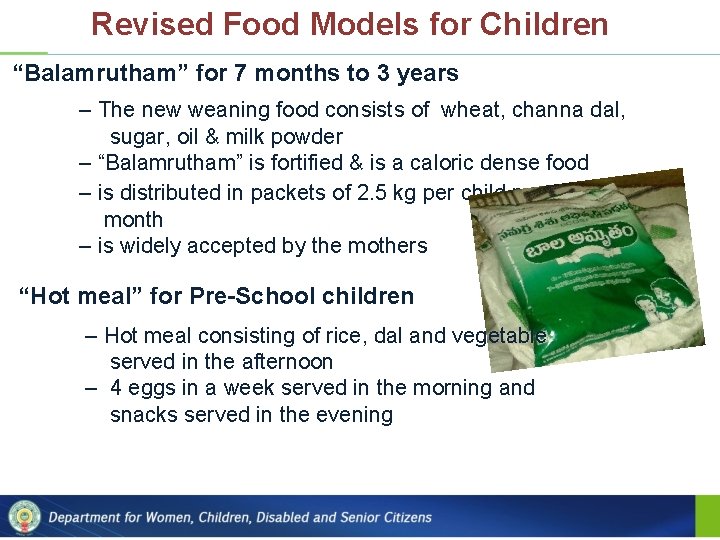
Revised Food Models for Children “Balamrutham” for 7 months to 3 years – The new weaning food consists of wheat, channa dal, sugar, oil & milk powder – “Balamrutham” is fortified & is a caloric dense food – is distributed in packets of 2. 5 kg per child per month – is widely accepted by the mothers “Hot meal” for Pre-School children – Hot meal consisting of rice, dal and vegetable served in the afternoon – 4 eggs in a week served in the morning and snacks served in the evening

Balamrutham: Weaning Food for Children < 3 Years Composition per 100 g Ingredients Parts(g) Energy(kc al) Protein(g) Roasted Wheat Bengal Gram Skimmed Milk Powder Sugar Oil TOTAL 55 5 10 20 10 100 190. 3 18. 0 35. 7 80 90 414. 0 6. 4 1. 0 3. 6 0 0 11. 0 Nutritive value per 100 gm S. No. GOI Norms Available Nutrients Fortificatio n 1 2 3 4 5 6 7 8 9 10 Energy (kcal) Protein (g) Calcium (mg) Iron (mg) Vitamin A (µg) Vitamin B 1 (µg) Vitamin B 2 (mg) Vitamin C (mg) Folic Acid (µg) Niacin (mg) 414 11 167 3. 1 2. 5 0. 3 0. 2 0. 5 7. 1 2. 3 0 0 200 6 200 0. 35 15 15 4 Total 414 11 367 9. 1 202. 5 0. 6 0. 55 15. 5 22. 1 6. 3
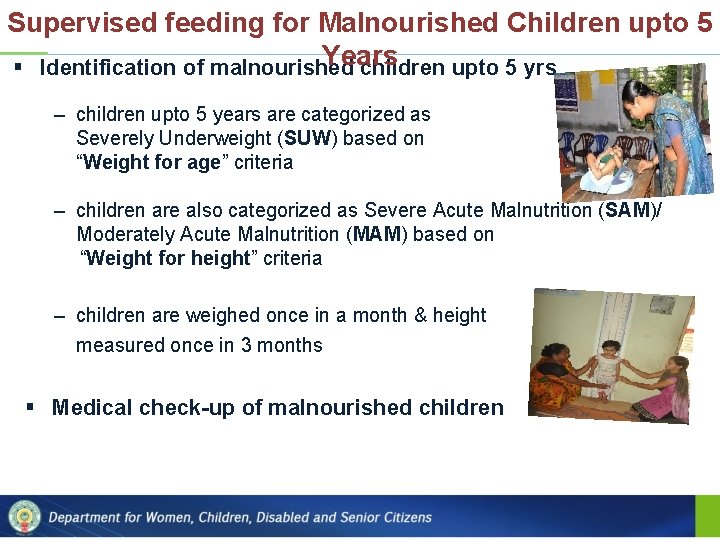
Supervised feeding for Malnourished Children upto 5 Years § Identification of malnourished children upto 5 yrs – children upto 5 years are categorized as Severely Underweight (SUW) based on “Weight for age” criteria – children are also categorized as Severe Acute Malnutrition (SAM)/ Moderately Acute Malnutrition (MAM) based on “Weight for height” criteria – children are weighed once in a month & height measured once in 3 months § Medical check-up of malnourished children
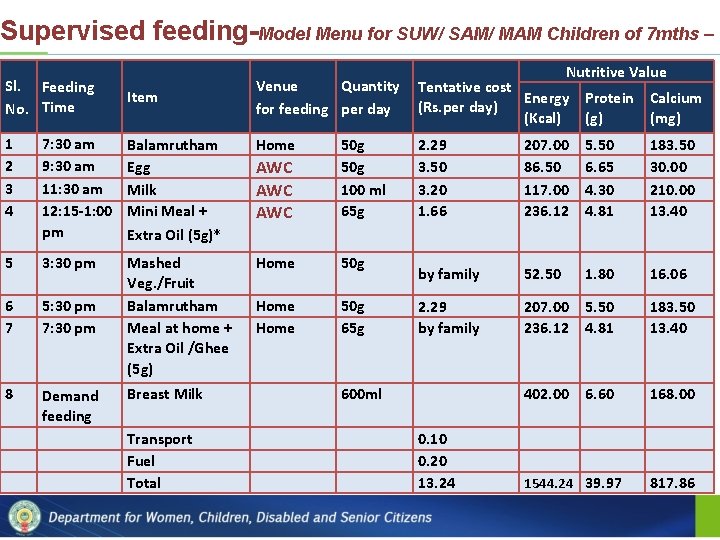
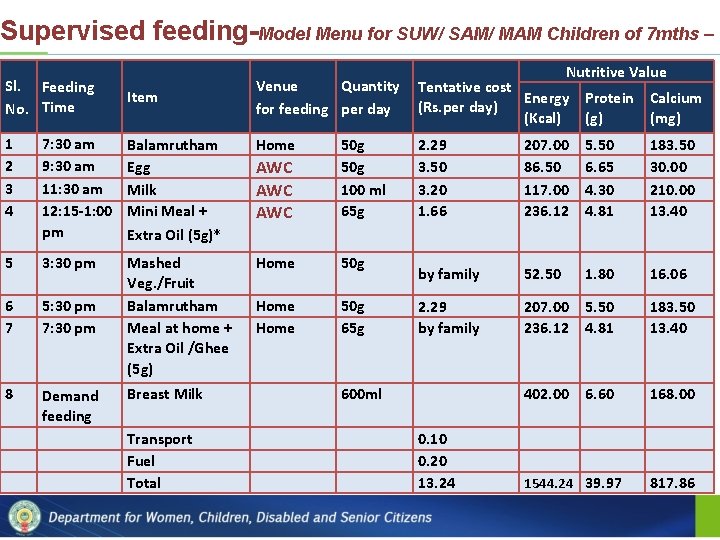
Supervised feeding-Model Menu for SUW/ SAM/ MAM Children of 7 mths – Sl. Feeding No. Time 3 yrs Item Tentative cost Energy Protein Calcium (Rs. per day) (Kcal) (g) (mg) 2. 29 3. 50 3. 20 1. 66 207. 00 86. 50 117. 00 236. 12 5. 50 6. 65 4. 30 4. 81 183. 50 30. 00 210. 00 13. 40 by family 52. 50 1. 80 16. 06 2. 29 by family 207. 00 236. 12 5. 50 4. 81 183. 50 13. 40 402. 00 6. 60 168. 00 1 2 3 4 7: 30 am 9: 30 am 11: 30 am 12: 15 -1: 00 pm Balamrutham Egg Milk Mini Meal + Extra Oil (5 g)* Home AWC AWC 50 g 100 ml 65 g 5 3: 30 pm Home 50 g 6 7 5: 30 pm 7: 30 pm Mashed Veg. /Fruit Balamrutham Meal at home + Extra Oil /Ghee (5 g) Home 50 g 65 g 8 Demand feeding Breast Milk 600 ml Transport Fuel Total Nutritive Value Venue Quantity for feeding per day 0. 10 0. 20 13. 24 1544. 24 39. 97 817. 86
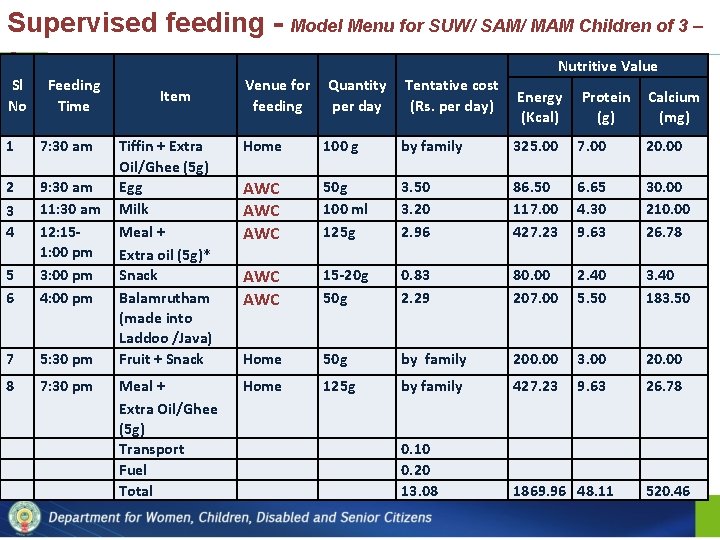
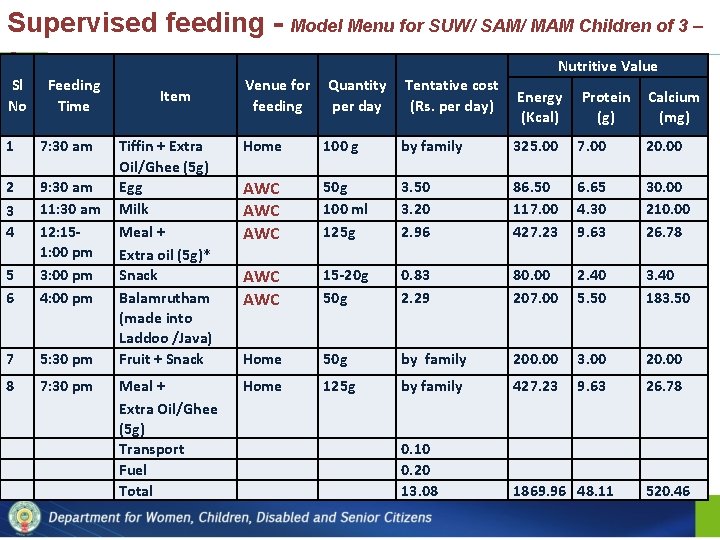
Supervised feeding - Model Menu for SUW/ SAM/ MAM Children of 3 – 6 yrs Sl No Feeding Time 1 7: 30 am 2 3 4 5 6 9: 30 am 11: 30 am 12: 151: 00 pm 3: 00 pm 4: 00 pm 7 5: 30 pm 8 7: 30 pm Nutritive Value Item Venue for Quantity Tentative cost Energy Protein Calcium feeding per day (Rs. per day) (Kcal) (g) (mg) Tiffin + Extra Oil/Ghee (5 g) Egg Milk Meal + Extra oil (5 g)* Snack Balamrutham (made into Laddoo /Java) Fruit + Snack Home 100 g by family 325. 00 7. 00 20. 00 AWC AWC 50 g 100 ml 125 g 3. 50 3. 20 2. 96 86. 50 117. 00 427. 23 6. 65 4. 30 9. 63 30. 00 210. 00 26. 78 AWC 15 -20 g 50 g 0. 83 2. 29 80. 00 207. 00 2. 40 5. 50 3. 40 183. 50 Home 50 g by family 200. 00 3. 00 20. 00 Meal + Extra Oil/Ghee (5 g) Transport Fuel Total Home 125 g by family 427. 23 9. 63 26. 78 0. 10 0. 20 13. 08 1869. 96 48. 11 520. 46
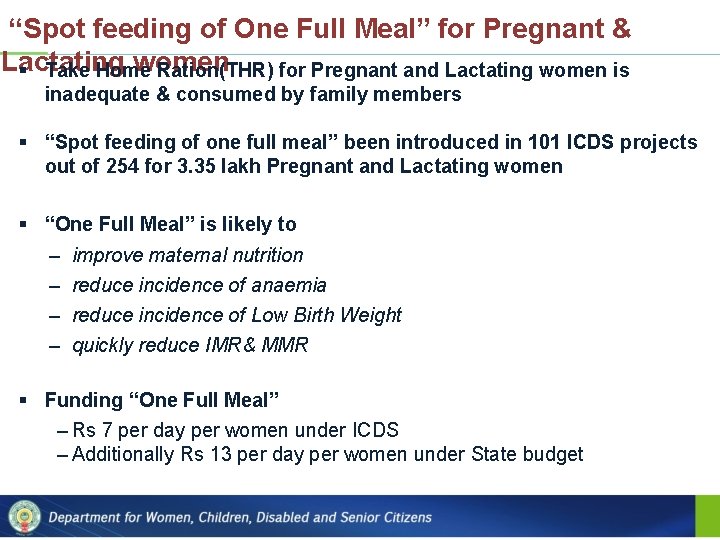
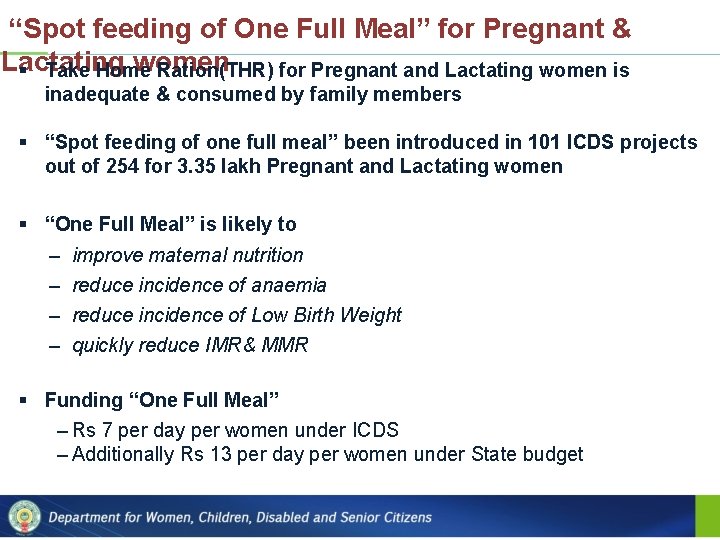
“Spot feeding of One Full Meal” for Pregnant & Lactating women § Take Home Ration(THR) for Pregnant and Lactating women is inadequate & consumed by family members § “Spot feeding of one full meal” been introduced in 101 ICDS projects out of 254 for 3. 35 lakh Pregnant and Lactating women § “One Full Meal” is likely to – – improve maternal nutrition reduce incidence of anaemia reduce incidence of Low Birth Weight quickly reduce IMR& MMR § Funding “One Full Meal” – Rs 7 per day per women under ICDS – Additionally Rs 13 per day per women under State budget
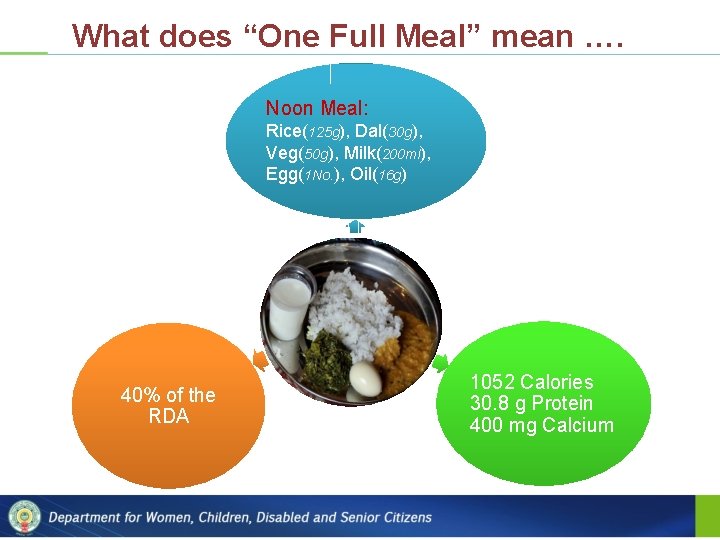
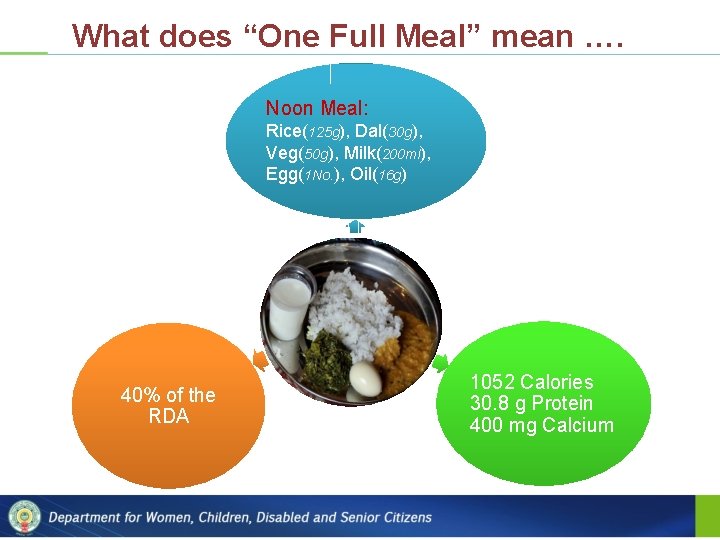
What does “One Full Meal” mean …. Noon Meal: Rice(125 g), Dal(30 g), Veg(50 g), Milk(200 ml), Egg(1 No. ), Oil(16 g) 40% of the RDA 1052 Calories 30. 8 g Protein 400 mg Calcium
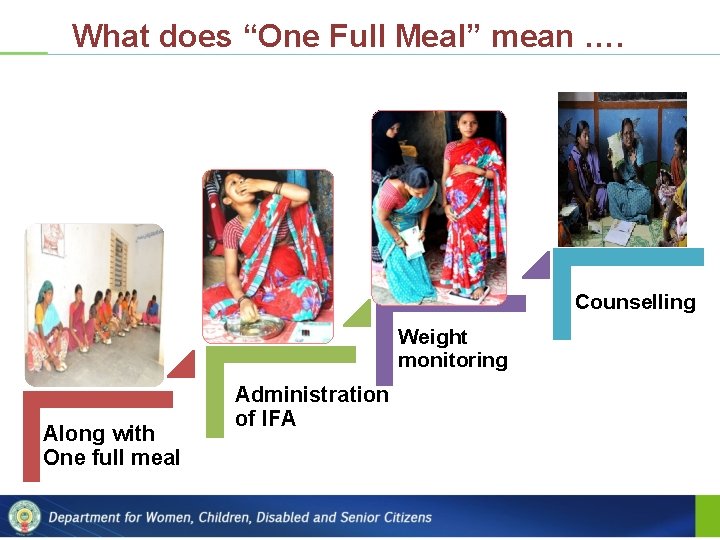
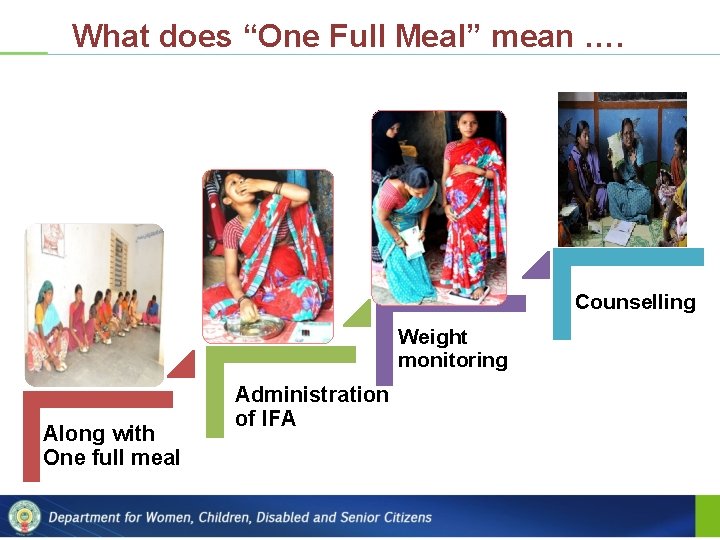
What does “One Full Meal” mean …. Counselling Weight monitoring Along with One full meal Administration of IFA
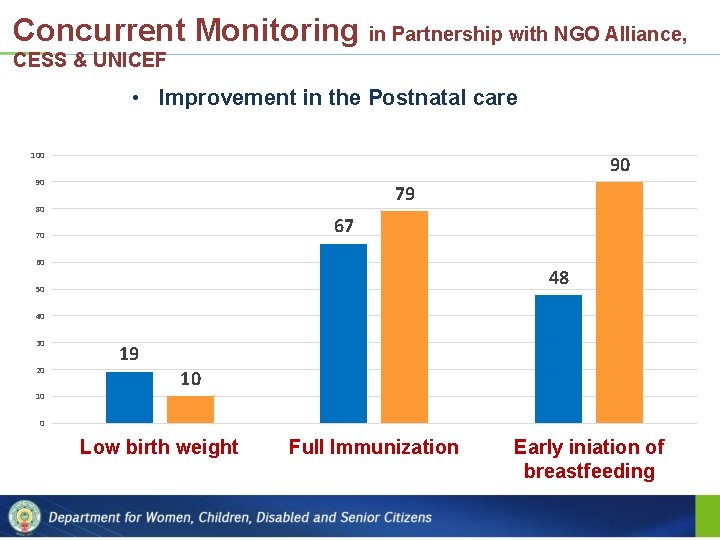
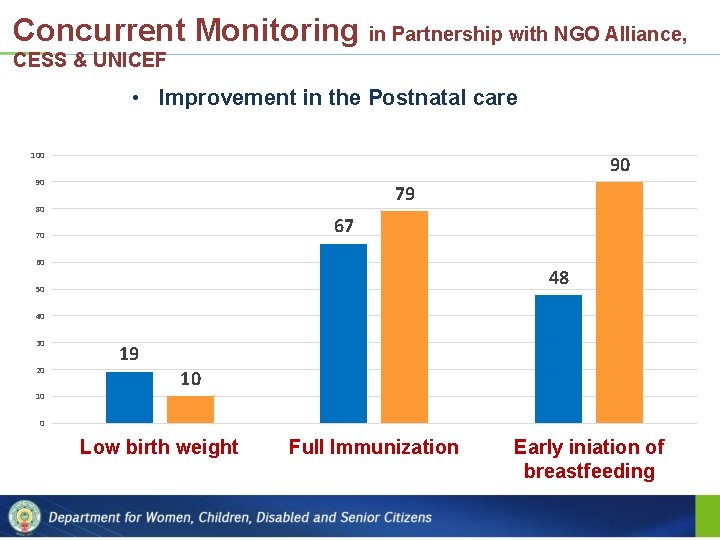
Concurrent Monitoring in Partnership with NGO Alliance, CESS & UNICEF • Improvement in the Postnatal care 100 90 90 79 80 67 70 60 48 50 40 30 20 19 10 10 0 Low birth weight Full Immunization Early iniation of breastfeeding
Capacity Building on IYCF practices • Capacity building on skilled IYCF counselling through counselling courses been taken up by WCD • Nearly 400 plus people (AWTC Instructors, CDPOs, Supervisors) have been trained as middle level trainers in IYCF using BPNI material at Hindupur • Using these Middle Level Trainers the frontline workers have been trained
Nutrition and Health Days (NHDs) – Growth Monitoring & Counselling § Instead of one NHD in a month, two NHDs are being conducted § The focus of NHD-1 is on Growth Monitoring & THR ‒ NHD-1 is conducted on 1 st of every month ‒ It allows focus on growth monitoring and categorization of children as SUW/SAM/MAM ‒ It ensures availability of food stock before 1 st of every month § The focus of NHD-2 is on providing immunization and ANC services by ANM § Counselling of mothers is conducted on both NHDs
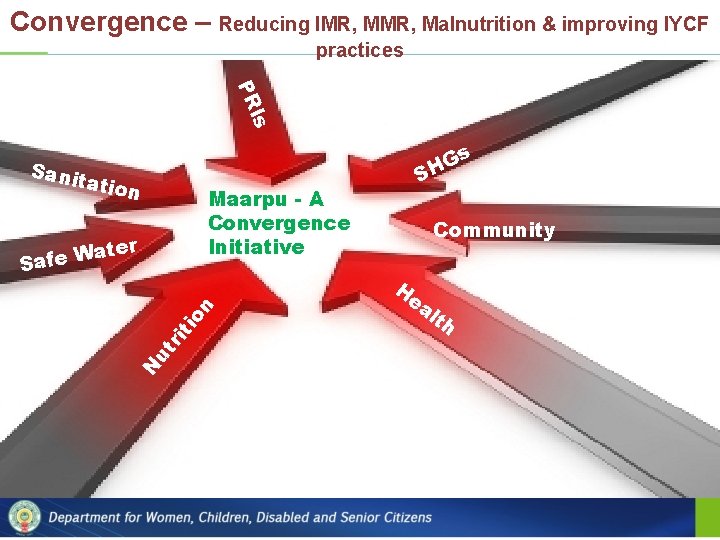
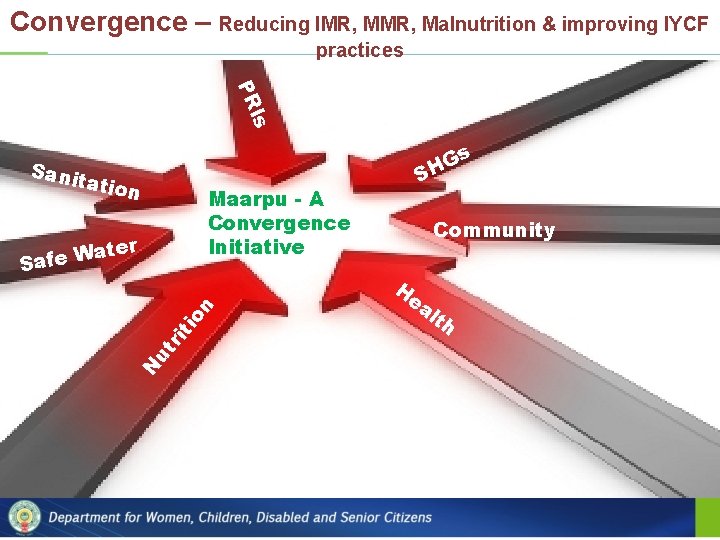
Convergence – Reducing IMR, Malnutrition & improving IYCF practices Is PR s G H Sani tatio n Maarpu - A Convergence Initiative A Key ater W e f Sa N ut ri ti on H S Community ea lth
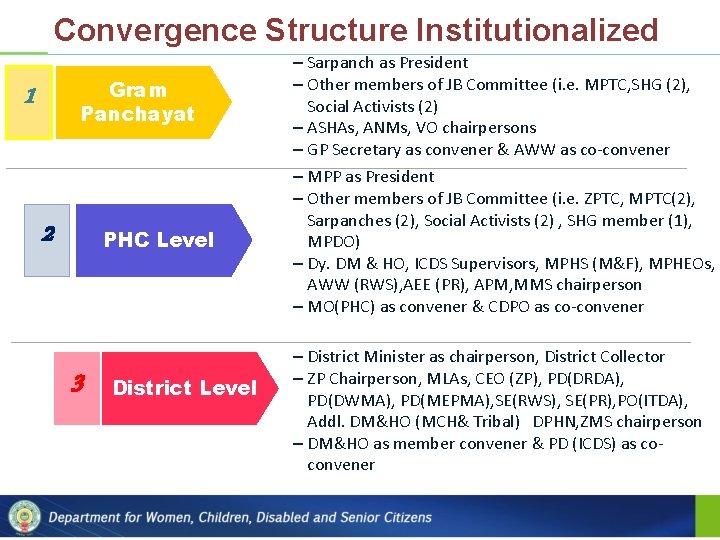
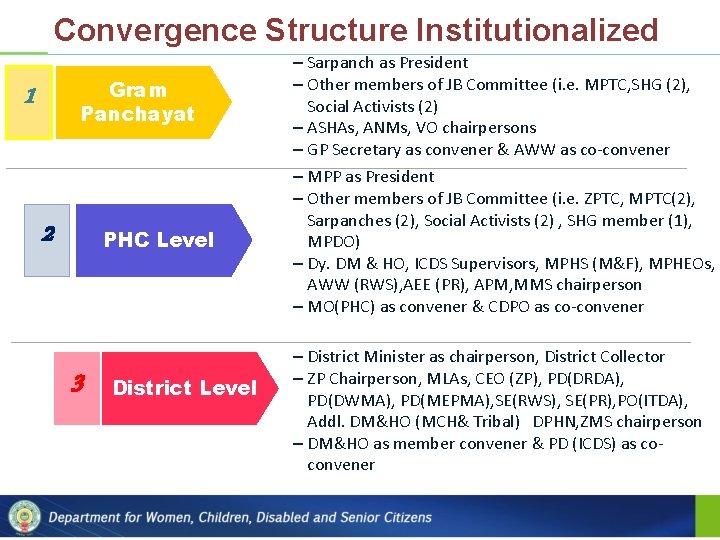
Convergence Structure Institutionalized Gram Panchayat 1 2 PHC Level 3 District Level – Sarpanch as President – Other members of JB Committee (i. e. MPTC, SHG (2), Social Activists (2) – ASHAs, ANMs, VO chairpersons – GP Secretary as convener & AWW as co-convener – MPP as President – Other members of JB Committee (i. e. ZPTC, MPTC(2), Sarpanches (2), Social Activists (2) , SHG member (1), MPDO) – Dy. DM & HO, ICDS Supervisors, MPHS (M&F), MPHEOs, AWW (RWS), AEE (PR), APM, MMS chairperson – MO(PHC) as convener & CDPO as co-convener – District Minister as chairperson, District Collector – ZP Chairperson, MLAs, CEO (ZP), PD(DRDA), PD(DWMA), PD(MEPMA), SE(RWS), SE(PR), PO(ITDA), Addl. DM&HO (MCH& Tribal) DPHN, ZMS chairperson – DM&HO as member convener & PD (ICDS) as coconvener
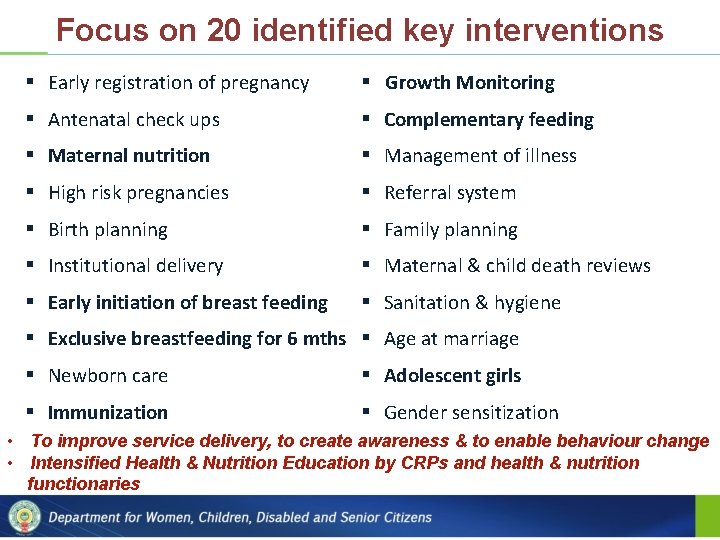
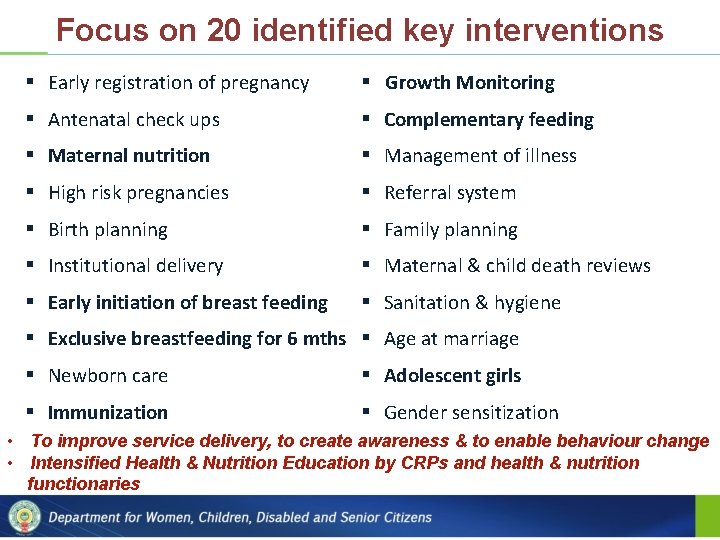
Focus on 20 identified key interventions § Early registration of pregnancy § Growth Monitoring § Antenatal check ups § Complementary feeding § Maternal nutrition § Management of illness § High risk pregnancies § Referral system § Birth planning § Family planning § Institutional delivery § Maternal & child death reviews § Early initiation of breast feeding § Sanitation & hygiene § Exclusive breastfeeding for 6 mths § Age at marriage § Newborn care § Adolescent girls § Immunization § Gender sensitization • To improve service delivery, to create awareness & to enable behaviour change • Intensified Health & Nutrition Education by CRPs and health & nutrition functionaries

Way forward…. . § To prepare annual plans for imparting Nutrition and Health Education § Need to position additional staff of ICDS mission to strengthen counselling § To actively involve community, SHGs and PRIs as partners in these efforts § To have close coordination with Health Department for effective convergence § To re-design food models in particular for malnourished children & pregnant women § To continue the skilled IYCF Counselling training courses
Thank You