Warfarin Your Days are Numbered Linda R Kelly
Warfarin, Your Days are Numbered! Linda R. Kelly Pharm. D Ph. C CACP Pharmacy Anticoagulation Specialist Presbyterian Healthcare System
Objectives • Identify and classify the available oral anticoagulants • Evaluate patient characteristics that would suggest using one product over another • Design a plan for switching from one oral anticoagulant to another • Manage oral anticoagulants in the periprocedural period
Terminology • VKA-Vitamin K Antagonist (warfarin) • DOAC-Direct Oral Anticoagulant • TSOAC-Target Specific Oral Anticoagulant • NOAC-Novel (or New or Non-vitamin K) Oral Anticoagulant

Resources
Available Direct Acting Oral Anticoagulants (DOACs) • Dabigatran • Rivaroxaban • Apixaban • Edoxaban

DOAC Mechanism of Action Inhibits Factor Xa Direct Thrombin Inhibitor Rivaroxaban Dabigatran Apixaban Edoxaban
DOAC Indications and Dosing Focus on Venous Thromboembolism and Non-valvular Atrial Fibrillation
Meet Marge is a 72 year old female with non-valvular atrial fibrillation (NVAF). She has been taking warfarin for stroke prevention. Her history also includes hypertension. What is her CHA 2 DS 2 VASc score?
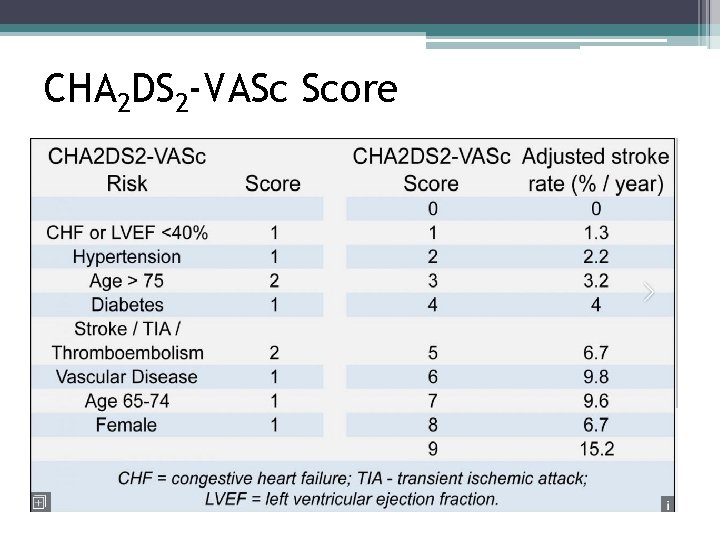
CHA 2 DS 2 -VASc Score
Marge comes to see you about starting a new product, bringing you a souvenir from her latest excursion. What factors should be considered when planning to start or switch a patient to a DOAC?
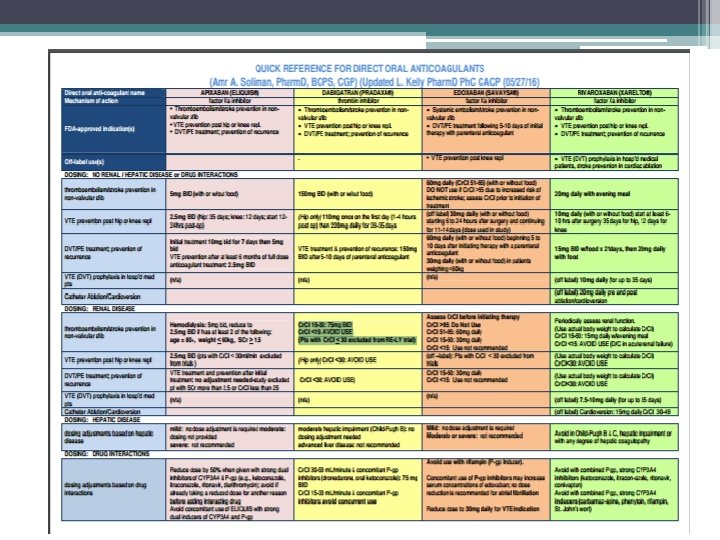
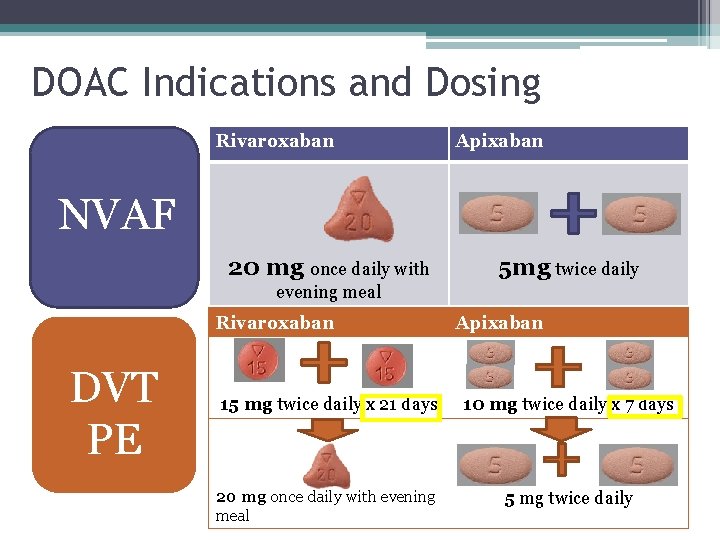
DOAC Indications and Dosing Rivaroxaban Apixaban NVAF 20 mg once daily with 5 mg twice daily evening meal Rivaroxaban DVT PE Apixaban 15 mg twice daily x 21 days 10 mg twice daily x 7 days 20 mg once daily with evening meal 5 mg twice daily
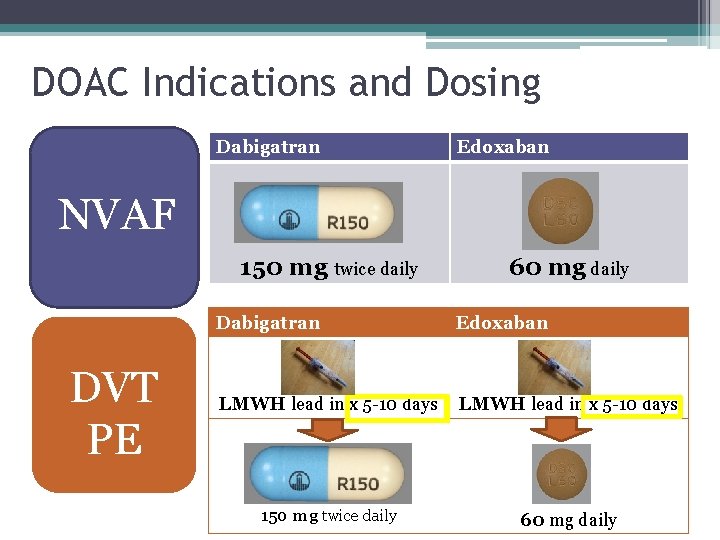
DOAC Indications and Dosing Dabigatran Edoxaban NVAF 150 mg twice daily DVT PE 60 mg daily Dabigatran Edoxaban LMWH lead in x 5 -10 days 150 mg twice daily 60 mg daily
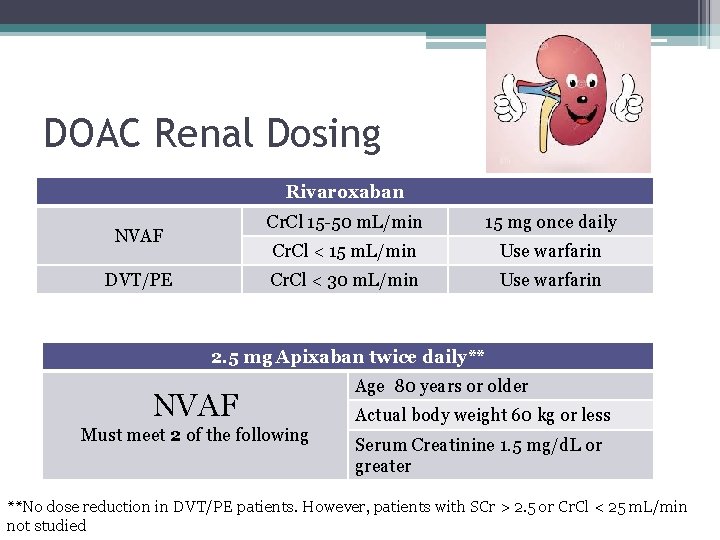
DOAC Renal Dosing Rivaroxaban NVAF DVT/PE Cr. Cl 15 -50 m. L/min 15 mg once daily Cr. Cl < 15 m. L/min Use warfarin Cr. Cl < 30 m. L/min Use warfarin 2. 5 mg Apixaban twice daily** NVAF Must meet 2 of the following Age 80 years or older Actual body weight 60 kg or less Serum Creatinine 1. 5 mg/d. L or greater **No dose reduction in DVT/PE patients. However, patients with SCr > 2. 5 or Cr. Cl < 25 m. L/min not studied
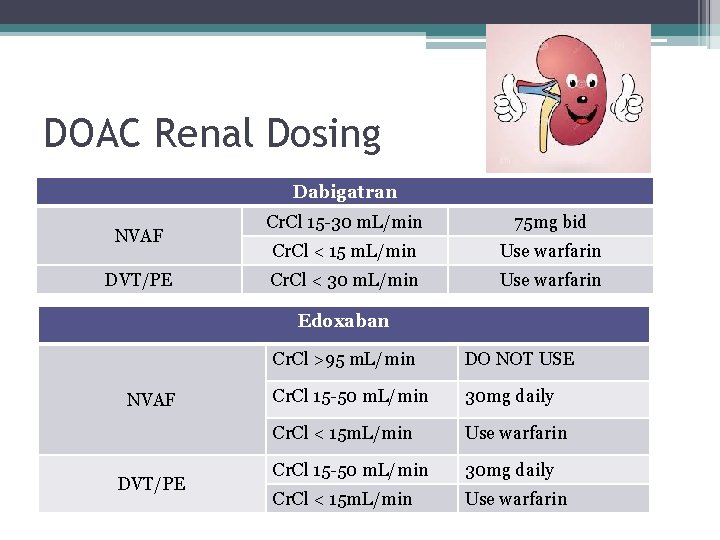
DOAC Renal Dosing Dabigatran NVAF DVT/PE Cr. Cl 15 -30 m. L/min 75 mg bid Cr. Cl < 15 m. L/min Use warfarin Cr. Cl < 30 m. L/min Use warfarin Edoxaban NVAF DVT/PE Cr. Cl >95 m. L/min DO NOT USE Cr. Cl 15 -50 m. L/min 30 mg daily Cr. Cl < 15 m. L/min Use warfarin
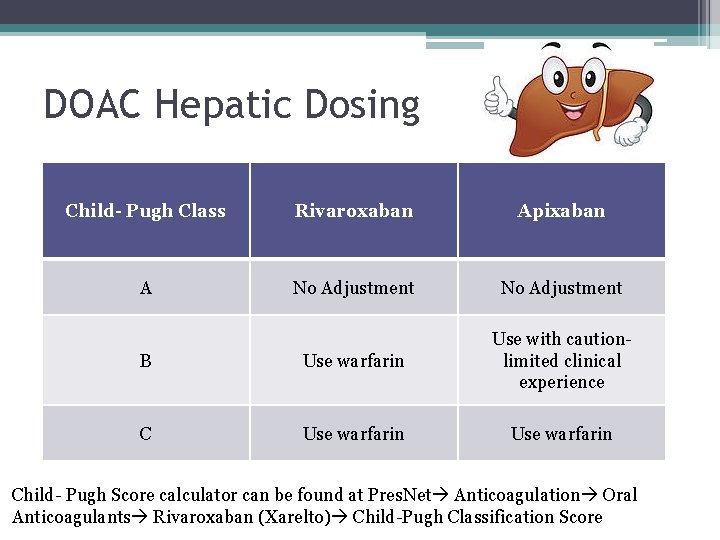
DOAC Hepatic Dosing Child- Pugh Class Rivaroxaban Apixaban A No Adjustment B Use warfarin Use with caution- limited clinical experience C Use warfarin Child- Pugh Score calculator can be found at Pres. Net Anticoagulation Oral Anticoagulants Rivaroxaban (Xarelto) Child-Pugh Classification Score
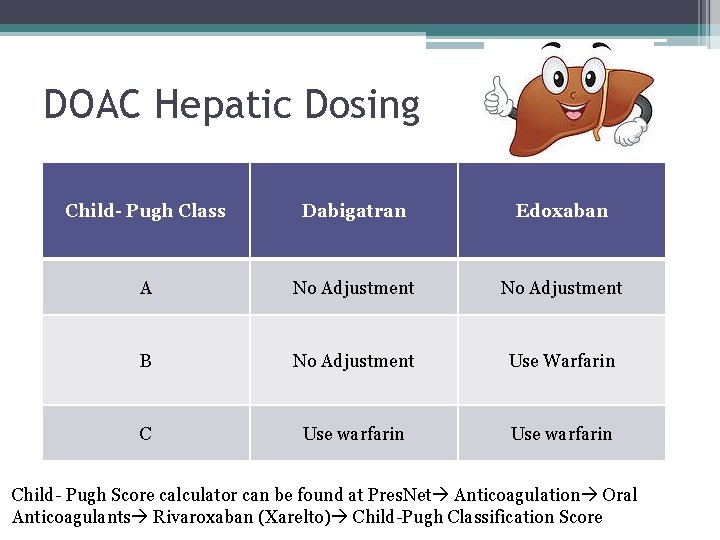
DOAC Hepatic Dosing Child- Pugh Class Dabigatran Edoxaban A No Adjustment B No Adjustment Use Warfarin C Use warfarin Child- Pugh Score calculator can be found at Pres. Net Anticoagulation Oral Anticoagulants Rivaroxaban (Xarelto) Child-Pugh Classification Score
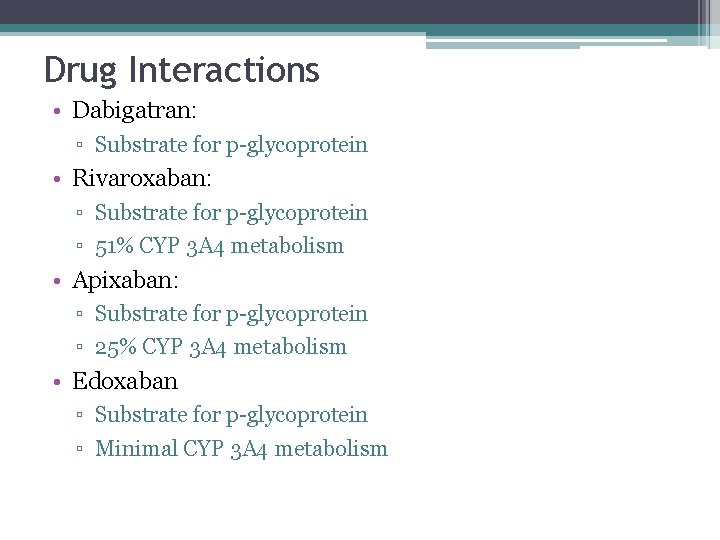
Drug Interactions • Dabigatran: ▫ Substrate for p-glycoprotein • Rivaroxaban: ▫ Substrate for p-glycoprotein ▫ 51% CYP 3 A 4 metabolism • Apixaban: ▫ Substrate for p-glycoprotein ▫ 25% CYP 3 A 4 metabolism • Edoxaban ▫ Substrate for p-glycoprotein ▫ Minimal CYP 3 A 4 metabolism

Drug Interactions Common Interacting Classes ▫ Anticonvulsants including barbiturates ▫ Antiretrovirals ▫ Antifungals ▫ Antiplatelet drugs and NSAIDS Your favorite drug interaction program is your best friend
Oral Anticoagulant Product Selection Focus on Venous Thromboembolism and Non-valvular Atrial Fibrillation
Is a DOAC a Good Choice For Marge? What should we consider before prescribing a DOAC?
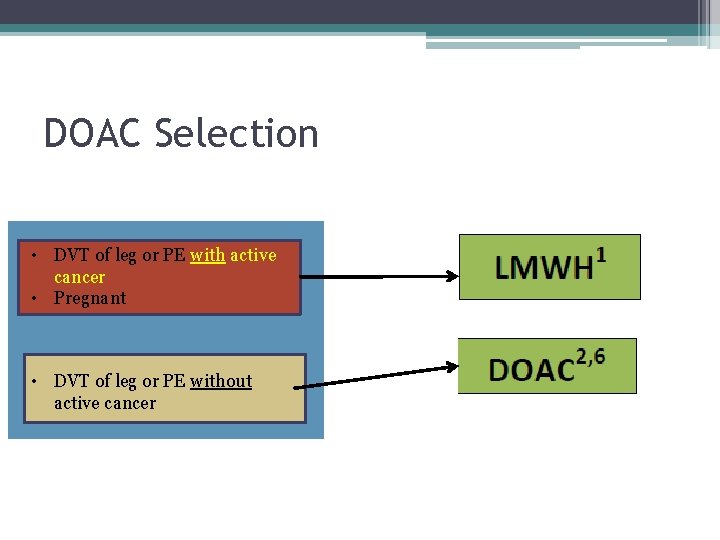
DOAC Selection • DVT of leg or PE with active cancer • Pregnant • DVT of leg or PE without active cancer

Anticoagulant Selection • Valvular atrial fibrillation • Valve replacement • Myocardial infarction requiring dual antiplatelet therapy • Breast feeding

Anticoagulant Selection • Valvular atrial fibrillation • Valve replacement • Myocardial infarction requiring dual antiplatelet therapy • Pregnant or breast feeding • Non-valvular atrial fibrillation • Secondary VTE prevention • VTE prophylaxis following knee/hip replacement surgery Will the patient have trouble paying for a DOAC? Yes No Does patient have Cr. Cl < 30, mechanical heart valve, moderate to severe hepatic impairment (Child. Pugh B or C), significant drug-drug interactions 6? No Yes
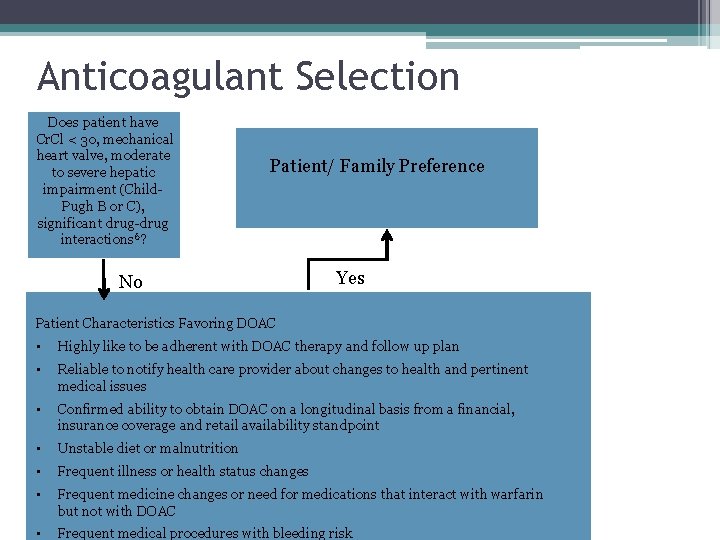
Anticoagulant Selection Does patient have Cr. Cl < 30, mechanical heart valve, moderate to severe hepatic impairment (Child. Pugh B or C), significant drug-drug interactions 6? Patient/ Family Preference No Yes Patient Characteristics Favoring DOAC • Highly like to be adherent with DOAC therapy and follow up plan • Reliable to notify health care provider about changes to health and pertinent medical issues • Confirmed ability to obtain DOAC on a longitudinal basis from a financial, insurance coverage and retail availability standpoint • Unstable diet or malnutrition • Frequent illness or health status changes • Frequent medicine changes or need for medications that interact with warfarin but not with DOAC • Frequent medical procedures with bleeding risk
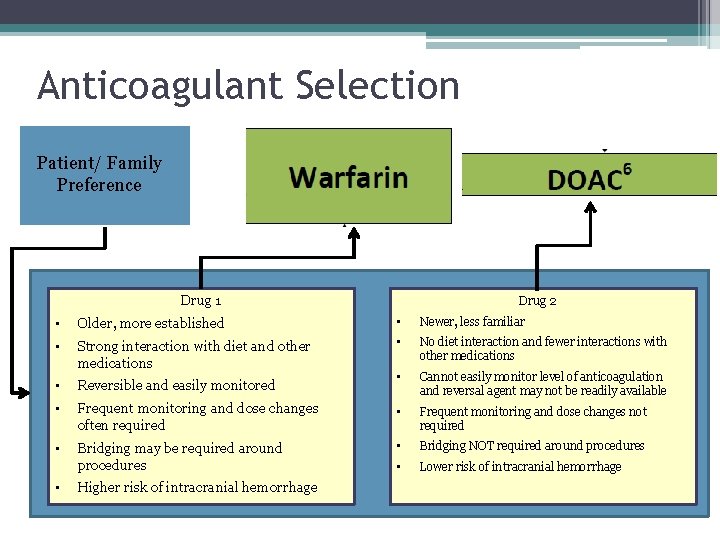
Anticoagulant Selection Patient/ Family Preference Drug 1 Drug 2 • Older, more established • Newer, less familiar • Strong interaction with diet and other medications • No diet interaction and fewer interactions with other medications • Reversible and easily monitored • Cannot easily monitor level of anticoagulation and reversal agent may not be readily available • Frequent monitoring and dose changes often required • Frequent monitoring and dose changes not required • Bridging may be required around procedures • Bridging NOT required around procedures • Lower risk of intracranial hemorrhage • Higher risk of intracranial hemorrhage
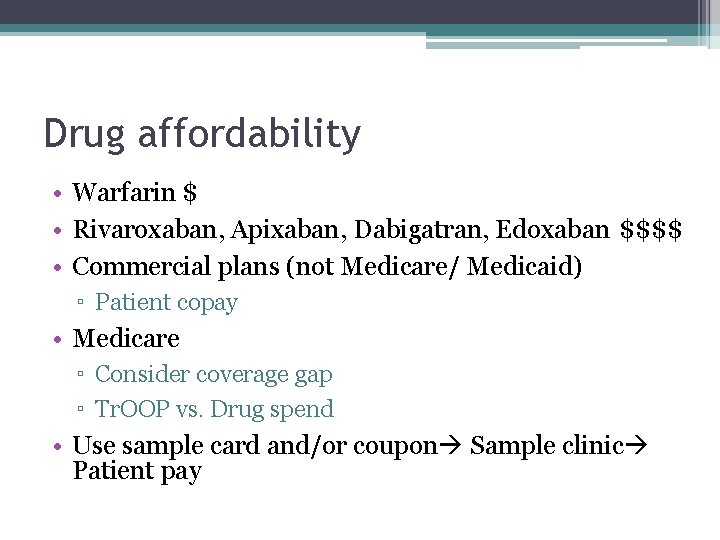
Drug affordability • Warfarin $ • Rivaroxaban, Apixaban, Dabigatran, Edoxaban $$$$ • Commercial plans (not Medicare/ Medicaid) ▫ Patient copay • Medicare ▫ Consider coverage gap ▫ Tr. OOP vs. Drug spend • Use sample card and/or coupon Sample clinic Patient pay
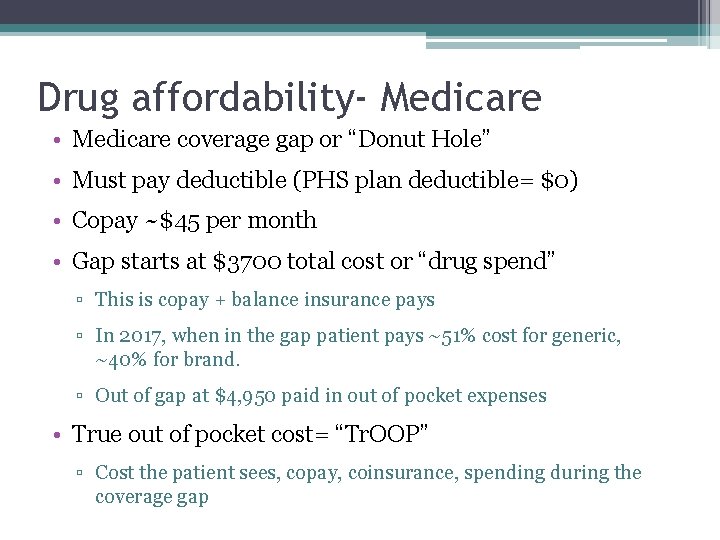
Drug affordability- Medicare • Medicare coverage gap or “Donut Hole” • Must pay deductible (PHS plan deductible= $0) • Copay ~$45 per month • Gap starts at $3700 total cost or “drug spend” ▫ This is copay + balance insurance pays ▫ In 2017, when in the gap patient pays ~51% cost for generic, ~40% for brand. ▫ Out of gap at $4, 950 paid in out of pocket expenses • True out of pocket cost= “Tr. OOP” ▫ Cost the patient sees, copay, coinsurance, spending during the coverage gap
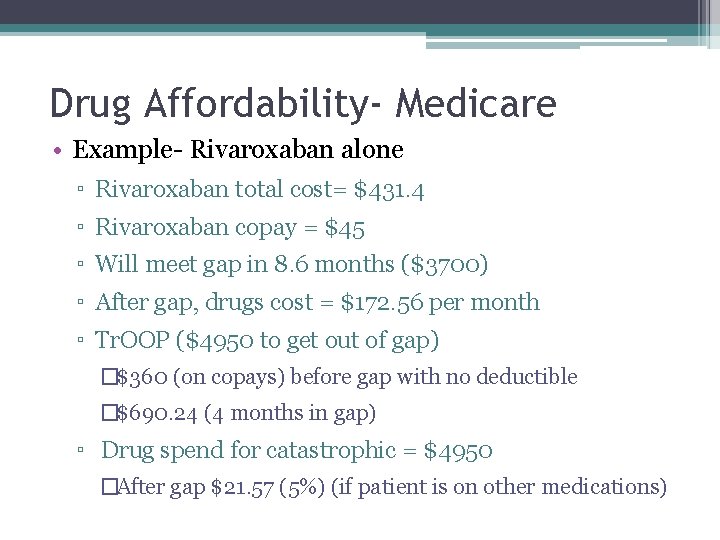
Drug Affordability- Medicare • Example- Rivaroxaban alone ▫ Rivaroxaban total cost= $431. 4 ▫ Rivaroxaban copay = $45 ▫ Will meet gap in 8. 6 months ($3700) ▫ After gap, drugs cost = $172. 56 per month ▫ Tr. OOP ($4950 to get out of gap) �$360 (on copays) before gap with no deductible �$690. 24 (4 months in gap) ▫ Drug spend for catastrophic = $4950 �After gap $21. 57 (5%) (if patient is on other medications)
Drug Affordability- Medicare • Example – Warfarin alone ▫ Warfarin total cost $6 (5 mg per day x 30 days. ) ▫ Warfarin copay= $4 ▫ Will not meet gap with warfarin ▫ In the gap, warfarin cost approx $3 ▫ After gap will pay $1. 60 per month
Patient Assistance • Utilize patient savings cards ▫ Sample Cards � 1 st month free! Regardless of insurance plan. ▫ Copy Card �$0 copay for commercial insurance ▫ Samples may be available
Patient selections takeaway • LMWH preferred in patients with active cancer • DOAC preferred in patients with DVT/ PE • NVAF -2016 European and Canadian guidelines recommend DOAC over warfarin, 2014 AHA/ACC/HRS guidelines do not recommend one over the other • Must consider patient co-morbidities and ability to afford therapy
Is a DOAC a Good Choice For Marge?
Questions?
Oral Anticoagulant Switching
Enoxaparin TO/FROM DOAC Stop old medication and start new medication when the next dose is due Abo-Salem J Thrombolysis (2014)
DOAC TO DOAC Stop DOAC 1 and start DOAC 2 when the next dose is due Abo-Salem J Thrombolysis (2014)
DOAC to Warfarin/Warfarin to DOAC Abo-Salem J Thrombolysis (2014)
Warfarin to DOAC • Discontinue warfarin • Begin rivaroxaban when INR below 3. 0 • Begin dabigatran or apixaban when INR below 2. 0
DOAC to warfarin • Need overlap therapy until INR equal or above 2. 0 1. DOAC • May interfere with INR reading • Must use DOAC trough for INR draw • Make clear to the patient that they MUST go in for an INR draw right before next DOAC dose is due. OR 2. LMWH • Transition like normal LMWH bridge per PMG policy. • Start LMWH when next DOAC dose due.
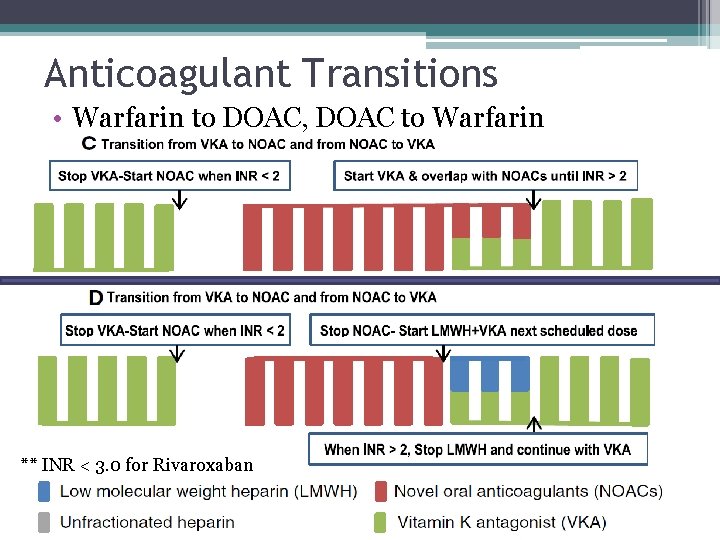
Anticoagulant Transitions • Warfarin to DOAC, DOAC to Warfarin ** INR < 3. 0 for Rivaroxaban
How Does Marge Switch from Warfarin to Rivaroxaban?
Peri-Procedural Anticoagulation
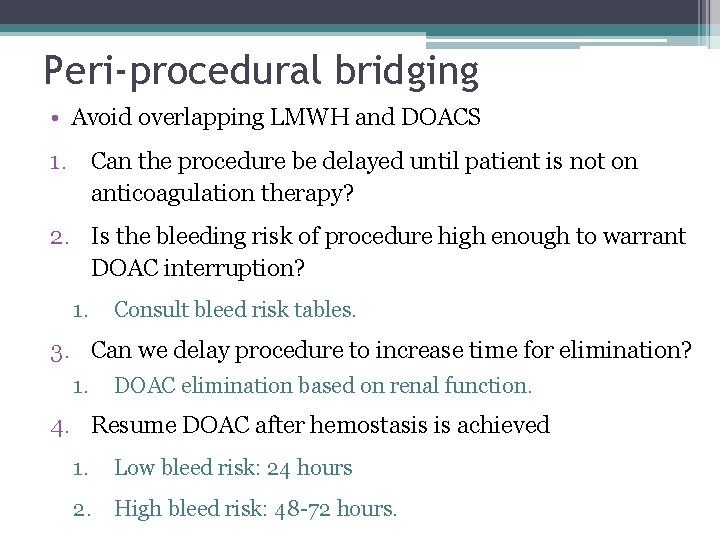
Peri-procedural bridging • Avoid overlapping LMWH and DOACS 1. Can the procedure be delayed until patient is not on anticoagulation therapy? 2. Is the bleeding risk of procedure high enough to warrant DOAC interruption? 1. Consult bleed risk tables. 3. Can we delay procedure to increase time for elimination? 1. DOAC elimination based on renal function. 4. Resume DOAC after hemostasis is achieved 1. Low bleed risk: 24 hours 2. High bleed risk: 48 -72 hours.
MAPPP Online and App www. mappp. ipro. org
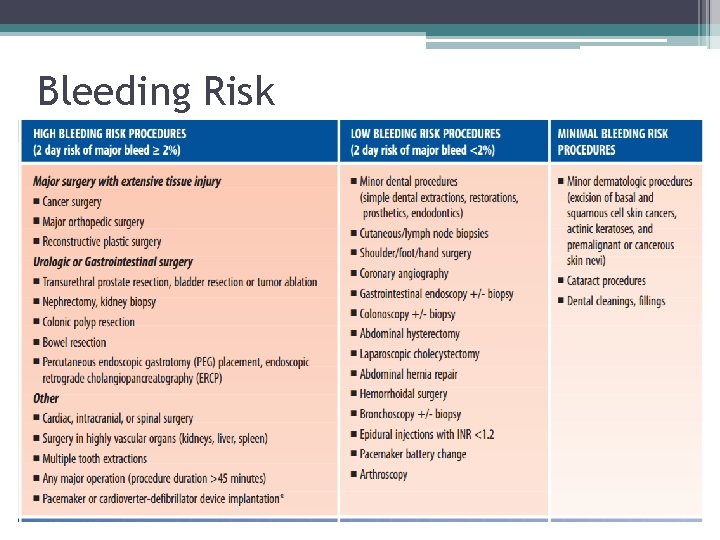
Bleeding Risk
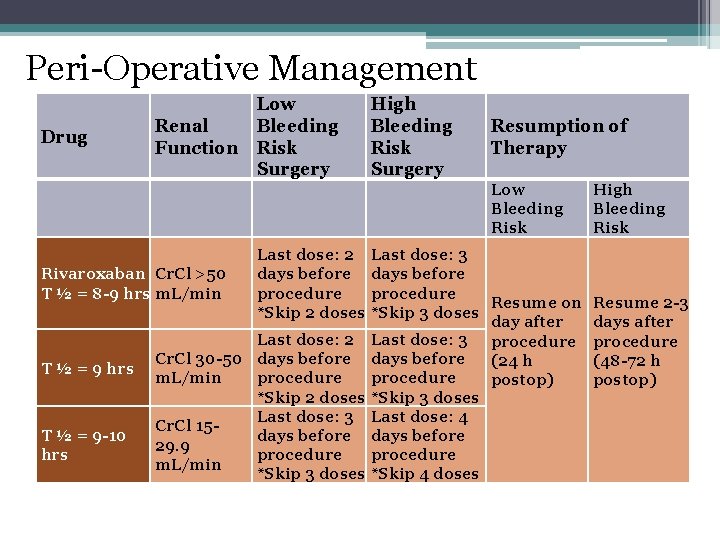
Peri-Operative Management Drug Renal Function Low Bleeding Risk Surgery High Bleeding Risk Surgery Rivaroxaban Cr. Cl >50 T ½ = 8 -9 hrs m. L/min T ½ = 9 hrs T ½ = 9 -10 hrs Last dose: 2 days before procedure *Skip 2 doses Last dose: 2 Cr. Cl 30 -50 days before m. L/min procedure *Skip 2 doses Last dose: 3 Cr. Cl 15 days before 29. 9 procedure m. L/min *Skip 3 doses Resumption of Therapy Low Bleeding Risk Last dose: 3 days before procedure Resume on *Skip 3 doses day after Last dose: 3 procedure days before (24 h procedure postop) *Skip 3 doses Last dose: 4 days before procedure *Skip 4 doses High Bleeding Risk Resume 2 -3 days after procedure (48 -72 h postop)
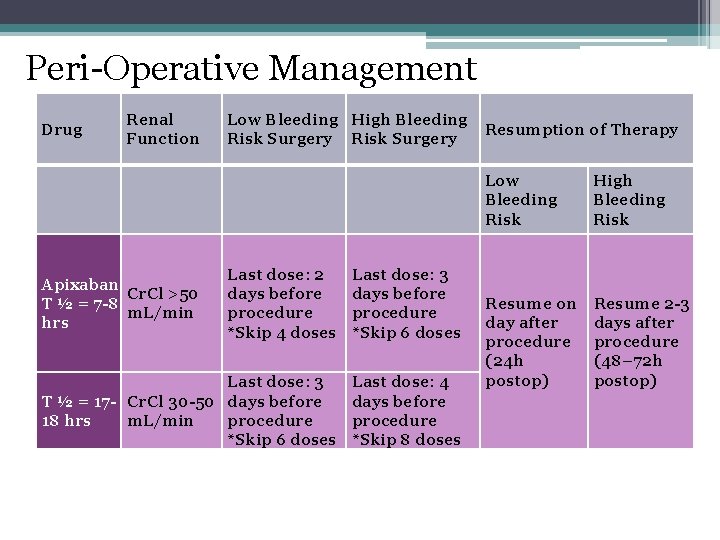
Peri-Operative Management Drug Renal Function Low Bleeding High Bleeding Resumption of Therapy Risk Surgery Last dose: 2 days before procedure *Skip 4 doses Last dose: 3 days before procedure *Skip 6 doses Last dose: 3 T ½ = 17 - Cr. Cl 30 -50 days before 18 hrs m. L/min procedure *Skip 6 doses Last dose: 4 days before procedure *Skip 8 doses Apixaban Cr. Cl >50 T ½ = 7 -8 m. L/min hrs Low Bleeding Risk High Bleeding Risk Resume on day after procedure (24 h postop) Resume 2 -3 days after procedure (48– 72 h postop)
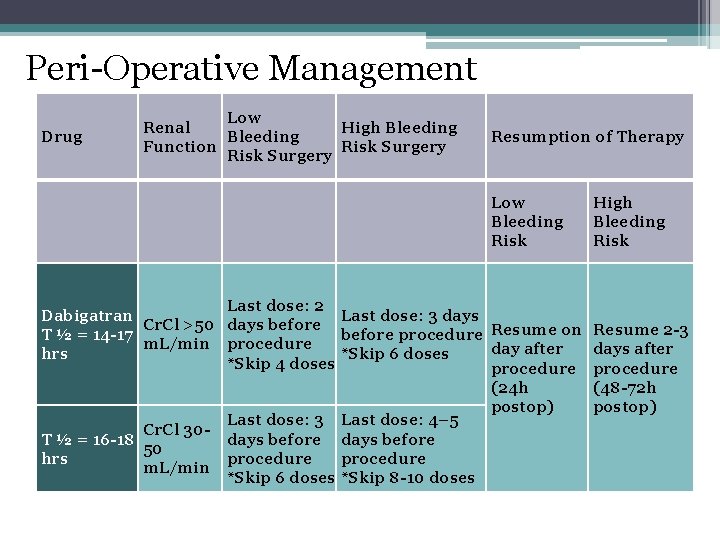
Peri-Operative Management Drug Low Renal High Bleeding Function Risk Surgery Resumption of Therapy Low Bleeding Risk High Bleeding Risk Last dose: 2 Dabigatran Last dose: 3 days Cr. Cl >50 days before T ½ = 14 -17 before procedure Resume on Resume 2 -3 m. L/min procedure day after days after hrs *Skip 6 doses *Skip 4 doses procedure (24 h (48 -72 h postop) Last dose: 3 Last dose: 4– 5 Cr. Cl 30 T ½ = 16 -18 days before 50 hrs procedure m. L/min *Skip 6 doses *Skip 8 -10 doses
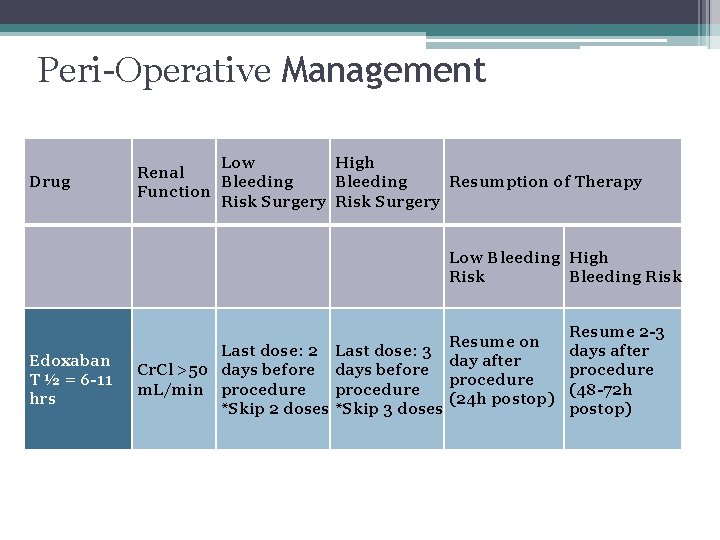
Peri-Operative Management Drug Low High Renal Bleeding Resumption of Therapy Function Risk Surgery Edoxaban T ½ = 6 -11 hrs Low Bleeding High Risk Bleeding Risk Resume on Last dose: 2 Last dose: 3 day after Cr. Cl >50 days before procedure m. L/min procedure (24 h postop) *Skip 2 doses *Skip 3 doses Resume 2 -3 days after procedure (48 -72 h postop)
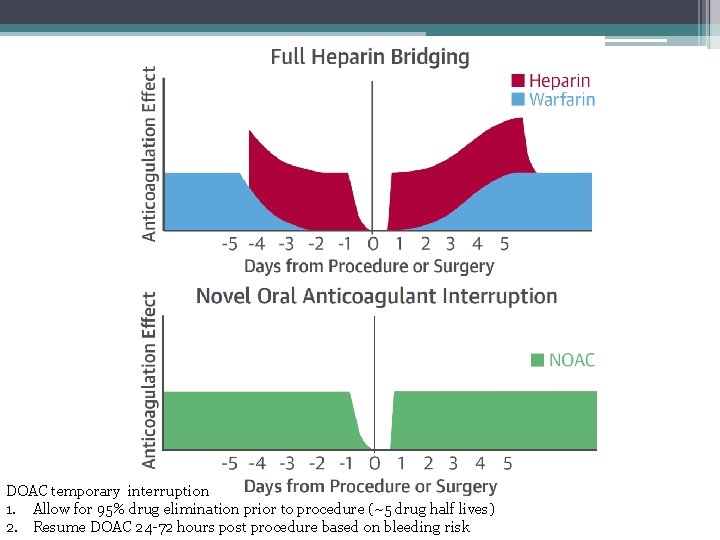
DOAC temporary interruption 1. Allow for 95% drug elimination prior to procedure (~5 drug half lives) 2. Resume DOAC 24 -72 hours post procedure based on bleeding risk
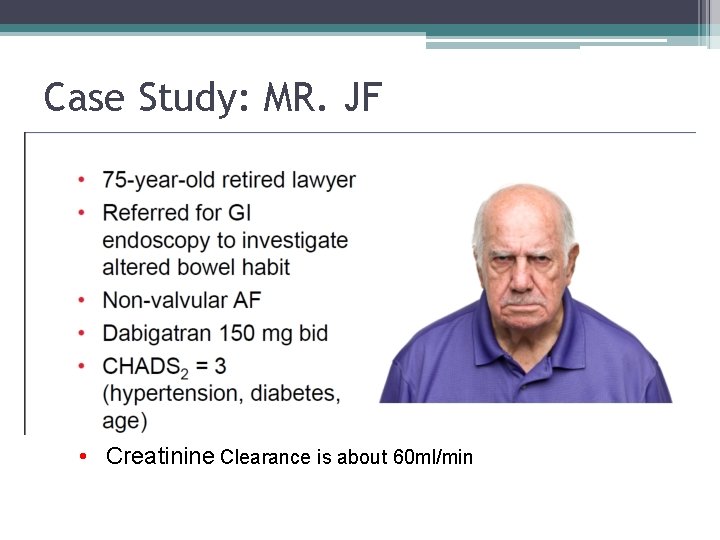
Case Study: MR. JF • Creatinine Clearance is about 60 ml/min
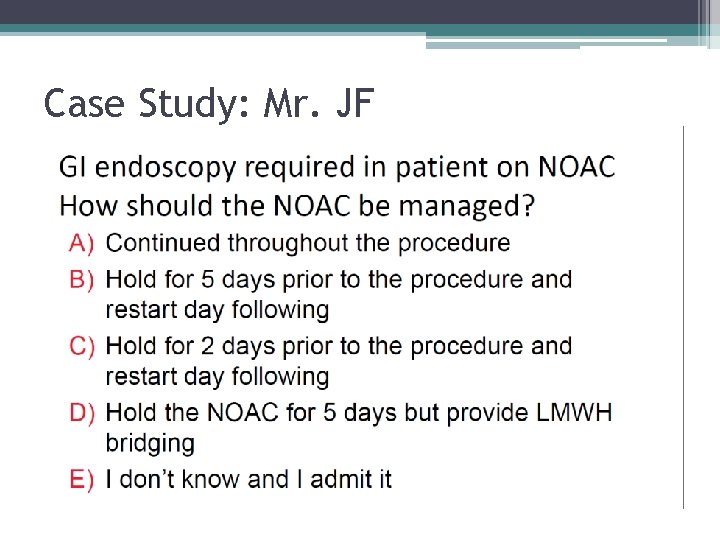
Case Study: Mr. JF
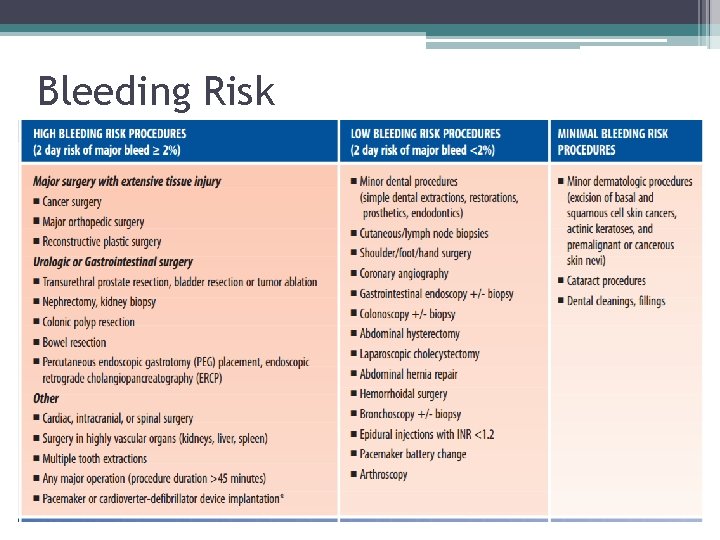
Bleeding Risk
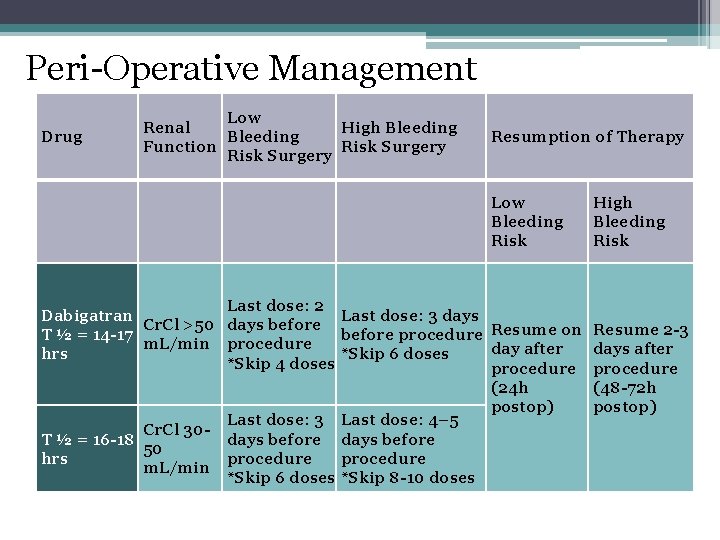
Peri-Operative Management Drug Low Renal High Bleeding Function Risk Surgery Resumption of Therapy Low Bleeding Risk High Bleeding Risk Last dose: 2 Dabigatran Last dose: 3 days Cr. Cl >50 days before T ½ = 14 -17 before procedure Resume on Resume 2 -3 m. L/min procedure day after days after hrs *Skip 6 doses *Skip 4 doses procedure (24 h (48 -72 h postop) Last dose: 3 Last dose: 4– 5 Cr. Cl 30 T ½ = 16 -18 days before 50 hrs procedure m. L/min *Skip 6 doses *Skip 8 -10 doses
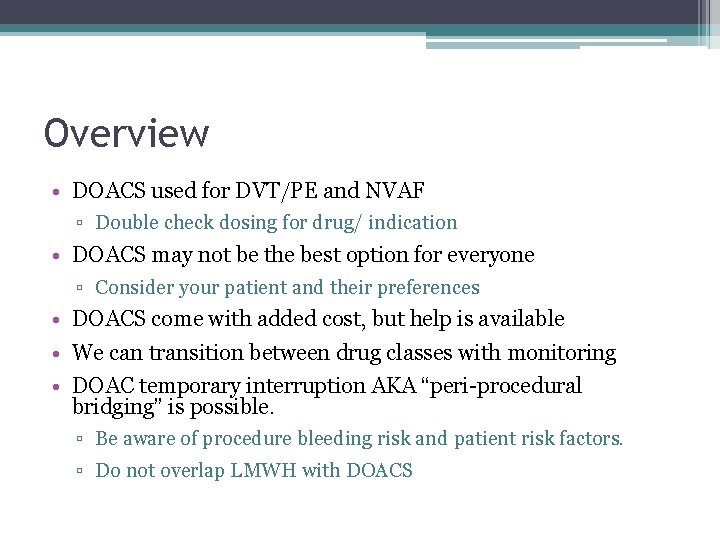
Overview • DOACS used for DVT/PE and NVAF ▫ Double check dosing for drug/ indication • DOACS may not be the best option for everyone ▫ Consider your patient and their preferences • DOACS come with added cost, but help is available • We can transition between drug classes with monitoring • DOAC temporary interruption AKA “peri-procedural bridging” is possible. ▫ Be aware of procedure bleeding risk and patient risk factors. ▫ Do not overlap LMWH with DOACS
Questions?
References • www. xarelto. com • Antithrombotic Therapy For Vte Disease: Chest Guideline And Expert Panel Report. Kearon C, Akl EA, Ornelas J, et al. Chest. 2016; 149(2): 315 -352. doi: 10. 1016/j. chest. 2015. 11. 026 • Abo-salem E, Becker R. Transitioning to and from the novel oral anticoagulants: a management strategy for clinicians. J Thrombolysis. 2014; 37(3): 3729. • Connolly SJ, Milling TJ, Eikelboom JW, et al. Andexanet Alfa for Acute Major Bleeding Associated with Factor Xa Inhibitors. N Engl J Med. 2016; 375(12): 113141. • Burnett AE, Mahan CE, Vazquez SR, Oertel LB, Garcia DA, Ansell J. Guidance for the practical management of the direct oral anticoagulants (DOACs) in VTE treatment. J Thrombolysis. 2016; 41(1): 206 -32. • Rechenmacher SJ, Fang JC. Bridging Anticoagulation: Primum Non Nocere. J Am Coll Cardiol. 2015; 66(12): 1392 -403. • www. drugsafety. ipro. org Management of Anticoagulation in the Peri-Procedural Period • Thrombosis Canada. New/ Novel oral anticoagulants (NOACS): Peri-Operative Management
- Slides: 58