Waiting for God Closing the Gap day 2





- Slides: 40
Waiting for God Closing the Gap day 2 A. 2017
Welcome to Day 2 Hello to anybody new today. Ice breaker Recap on last session Sick notes and benefits Calgary Cambridge framework Explanation – role play.
video Tom Hussey video Reflections of the past
Module 2 a – • • st 31 October Waiting for God – caring for the elderly Presentation Coffee Case discussion • Module 2 b • Case scenarios based on EOL care • Role play – active listening
Caring for older people: What are the issues? Group work Using your experience in general practice identify as many of the issues relating to this group of patients. What are the issues for: The patient The doctor Society Plenary
What are the issues? Change in demographics to a more elderly population More chronic disease management Greater complexity as more disease Polypharmacy Care of the elderly takes up a greater proportion of a GP’s workload Current drive to reduce hospital admissions Multi-disciplinary team working: community matrons, rapid response teams, care home staff.
Population growth UK population 1960 s - 52. 4 million 1980 s – 56. 3 million 2000 s – 58. 9 million 2020 - 67. 4 million (projected ) 5 th highest annual growth rate in the EU (after Luxembourg, Italy, Turkey and Norway) - UK make up 1/8 of EU population. This is due to increasing birth rates, net migration and also increased survival. 1974 - population over 65 = 13. 8% 2014 – population over 65 = 17. 7% 2034 – population over 65 = 23. 3% (projected)

Polypharmacy Homework Consider the challenges of polpyharmacy How many is too many drugs? What are the possible risks to patients? For further reading see BMJ feature article: “Polypharmacy: a necessary evil” Jacqui Wise (BMJ 2013: 347) System 1/ MM – STOPP policies.

What are the issues? Absent families caring from a distance Loss of role, dignity and respect Financial worries Bereavement Cognitive decline Physical decline Communication difficulties
What are the issues? Frailty End of life care Advance directives/ living wills DNAR orders Euthanasia? ?
Frailty ppt
video https: //www. youtube. com/watch? v=8 c. ACbzanitg
Consider these cases
Geoff . . . He always likes to make an appearance! Geoff is an 86 year old man. His daughter comes to see you for a chat. She is a nurse and lives down south but has popped up for a visit. You haven’t seen Geoff for the last 3 years but remember him as a large jovial man who was in relatively good health. She tells you that he has been getting a bit forgetful over the last year or so and is worried about him. She found some mouldy food in the fridge Geoff has been going to the toilet a lot recently When driving he has had a couple of small accidents in his car.
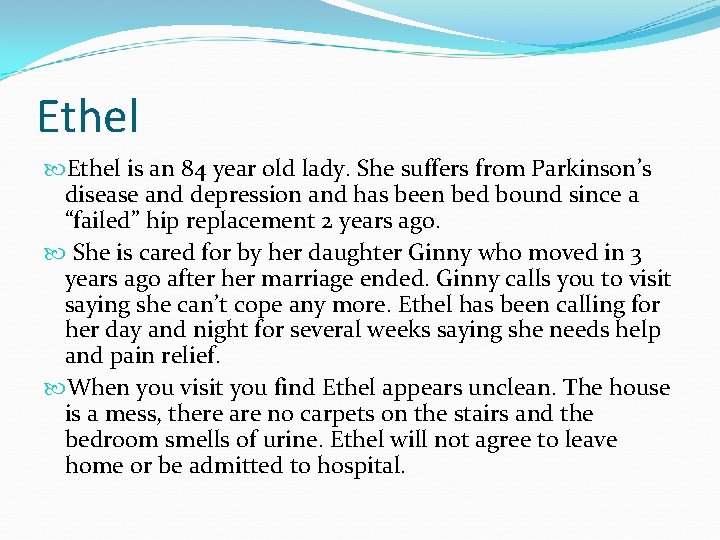
Ethel is an 84 year old lady. She suffers from Parkinson’s disease and depression and has been bed bound since a “failed” hip replacement 2 years ago. She is cared for by her daughter Ginny who moved in 3 years ago after her marriage ended. Ginny calls you to visit saying she can’t cope any more. Ethel has been calling for her day and night for several weeks saying she needs help and pain relief. When you visit you find Ethel appears unclean. The house is a mess, there are no carpets on the stairs and the bedroom smells of urine. Ethel will not agree to leave home or be admitted to hospital.
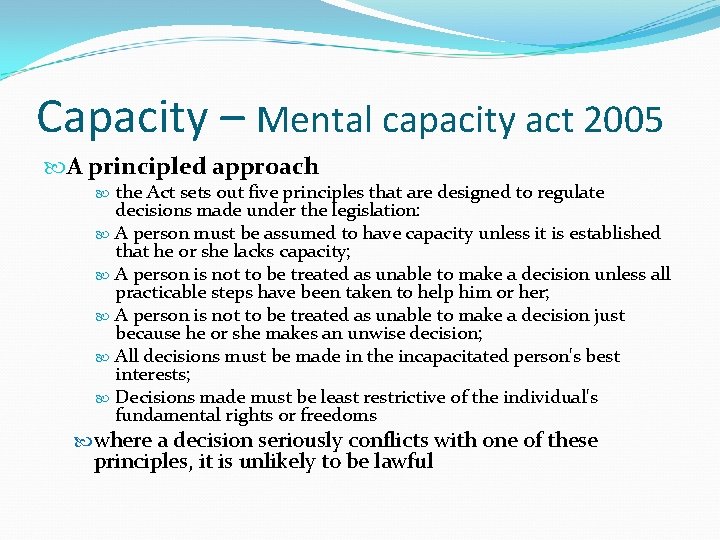
Capacity – Mental capacity act 2005 A principled approach the Act sets out five principles that are designed to regulate decisions made under the legislation: A person must be assumed to have capacity unless it is established that he or she lacks capacity; A person is not to be treated as unable to make a decision unless all practicable steps have been taken to help him or her; A person is not to be treated as unable to make a decision just because he or she makes an unwise decision; All decisions must be made in the incapacitated person's best interests; Decisions made must be least restrictive of the individual's fundamental rights or freedoms where a decision seriously conflicts with one of these principles, it is unlikely to be lawful
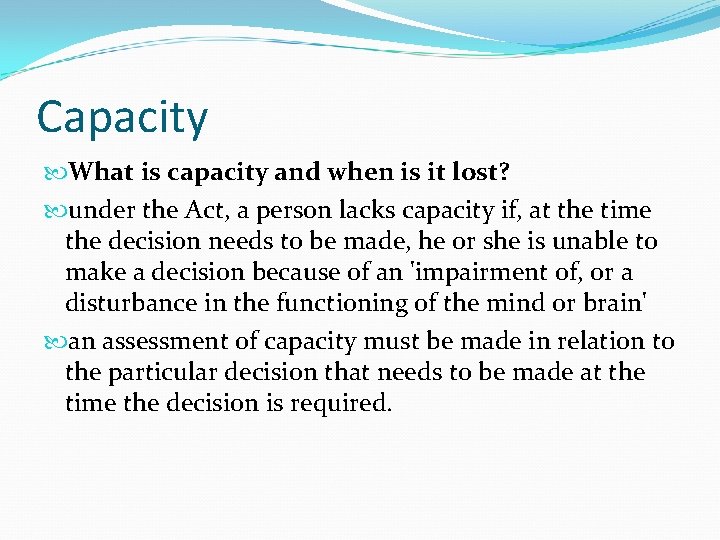
Capacity What is capacity and when is it lost? under the Act, a person lacks capacity if, at the time the decision needs to be made, he or she is unable to make a decision because of an 'impairment of, or a disturbance in the functioning of the mind or brain' an assessment of capacity must be made in relation to the particular decision that needs to be made at the time the decision is required.
Capacity(2) Assessment of incapacity: a person lacks capacity if, at the time the decision needs to be made, he or she is unable to: Understand the information relevant to the decision; Retain the information; Use or weigh the information; Communicate the decision (by any means) where an individual fails one or more parts of this test, then they do not have the relevant capacity and the entire test is failed
Capacity (3) in assessing capacity, consideration should be given, where appropriate, to the views of those close to the individual. Family members and close friends may be able to provide valuable background information, although their views about what they might want for the individual must not be allowed to influence the assessment Is there any evidence of past wishes such as an advance care statement. A welfare attorney can be appointed to make decisions once capacity is lost – may require referral to court of protection. ‘next-of-kin’ has no legal definition/ status – this person, for example, cannot give or withhold consent to sharing of information.
Substitute decision making the Act allows people, while they retain capacity, to nominate an individual to take healthcare decisions on their behalf when they lose capacity the Act creates a new lasting power of attorney (LPA), which replaces and extends the enduring power of attorney, whose powers related only to management of property and affairs. Anyone creating an LPA can set conditions on the exercise of the powers, and it does not extend to decisions relating to life-sustaining treatment unless that is explicitly stated there are two types of LPA, the property and affairs LPA and the personal welfare LPA covers personal, welfare and health care decisions, including decisions relating to medical treatment. Although an LPA in relation to property and affairs can be used by the attorney even when the donor still has capacity, an LPA dealing with personal welfare can only operate if the individual lacks capacity in relation to the issue in question before an LPA can be used, it must be registered with the Office of the Public Guardian
Advance decisions refusing treatment the Act gives statutory force to advance decisions refusing treatment. Advance decisions will be binding on doctors if: The person making it was 18 or older and had the necessary capacity; It specifies the treatment to be refused and the circumstances in which the refusal is to apply; The person has not subsequently appointed an attorney to make the decision; The person has not done anything clearly inconsistent with the directive; The person does not have capacity at the time the decision has to be enforced The ADRT used to be called a ‘living will’ or an ‘advance directive’. A personal welfare LPA will supersede an ADRT if it is registered after the ADRT date. An ADRT requires capacity. An advance directive (prior to 2008) is not legally binding so should be replaced by an ADRT as a matter of urgency.
ADRT an advance refusal will apply only to life-sustaining treatment where it is in writing, signed and witnessed and contains a statement that it is to apply ‘even when life is at risk’ in an emergency or where there is doubt about the existence or validity of an advance decision, doctors can provide treatment that is immediately necessary to stabilize or to prevent a deterioration in the patient until the existence, and the validity and applicability, of the advance decision can be established
What is an advance care plan ? An ACP (ideally in writing) is a non-legal document stating your preferences and wishes, normally in response to a serious illness or death of a relative. It is designed to be helpful to those who care for you if you lose capacity or consciousness. An ACP can state a person to speak on your behalf who will often be your next of kin. But it does not replace a LPA and is not an ADRT It should be accompanied by a DNAR order if appropriate. Again this is advisory and not legally binding.
What is an emergency health care plan ? A EHCP is a document to record a plan of action in an anticipated emergency – usually applicable to individuals with complex health care needs where recovery is uncertain. Aim is to ensure appropriate care and unnecessary treatment – a DNACPR form must be filled in if CPR not appropriate. include a brief summary of the individual’s diagnosis and their understanding of it include a list of regular and prn medications, and indications for any rescue medications left in the patient’s home for emergency use indicate any ceilings of care that have been requested by the patient and any that have been recommended by healthcare professionals describe actions for emergencies arising at home If the individual lacks capacity for these decisions: any decisions must be made following the nine point checklist of the Mental Capacity Act.

Caring for the elderly.
Coffee
Palliative Care Case This scenario deals with different aspects of palliative care, from diagnosis to symptom management. We will use group discussion and role play to work through this case.
Joan 72 year old lady admitted to hospital by your GP colleague three weeks ago, when she presented with acute shortness of breath. The GP notes from the time suggest a diagnosis of either pneumonia/pleural effusion. Today she requests a home visit, having been discharged from hospital 2 days before. The visit request says: “left leg pain. ” The discharge letter from the hospital states: “Malignant pleural effusion: treated with chest drain. CT abdo and pelvis; suspicious ovarian mass, likely malignant. No obvious mets in abdomen or pelvis. Referred to gynae oncology as “OP. ”
Joan: Part one It is not clear from the discharge letter, how much the patient was told, if anything, about the diagnosis/scan findings. After discussion, Joan knows that she has fluid on her lung and possible ovarian cancer. She is fairly pragmatic about the news and hopeful that the gynaecologist can offer treatment, as the cancer hasn’t spread outside of the ovary. How would you respond to this?
Joan: Part two Some weeks later, Joan’s husband requests a home visit. Since you last saw her she has required drainage of abdominal ascites. She has been told that she cannot have any curative treatment for her condition. Joan’s main symptoms are nausea. She is eating very little. Her husband wants to know what can be done to improve her appetite and help with weight gain. How would you proceed?
Joan: Part three You see Joan again, a month later, on a follow-up visit. As you’re about to leave for the visit, the district nurse stops you with the new multi-agency DNAR form, created by the local palliative care team. She asks if you can discuss this with Joan and complete the form during your visit. Joan is spending most of her time in bed and now eating very little. She is quite comfortable, taking oral MST 30 mg bd for pain and cyclizine 50 mg tds for nausea.
Deciding Right Initiative North of England Cancer Network See: www. theclinicalnetwork. org Guidance on: Shared decision making Emergency care planning Recognise the individual with capacity as key to making decisions in advance Create regional documentation, for use in any setting, recognised by all health care professionals: single DNAR form
Deciding right.

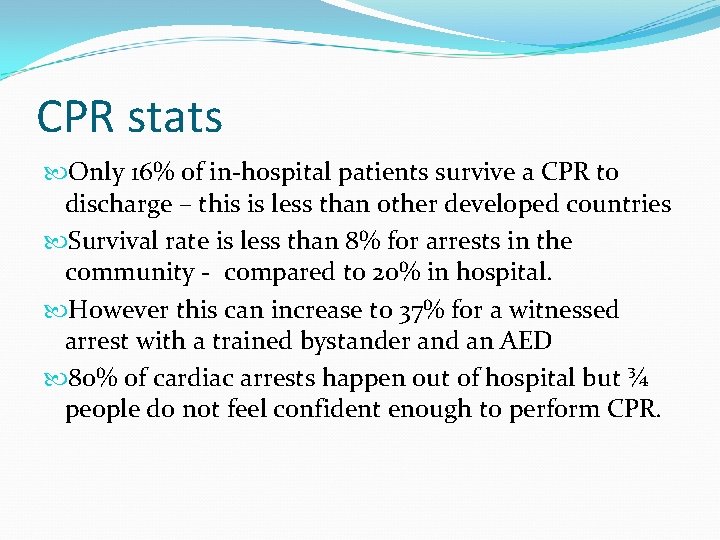
End of life care: Cardiopulmonary resuscitation (CPR) When someone suffers sudden cardiac or respiratory arrest, CPR attempts to restart their heart or breathing and restore their circulation. CPR interventions are invasive and include chest compressions, electric shock by an external or implanted defibrillator, injection of drugs and ventilation. If attempted promptly, CPR has a reasonable success rate in some circumstances. Generally, however, CPR has a very low success rate and the burdens and risks of CPR include harmful side effects such as rib fracture and damage to internal organs; adverse clinical outcomes such as hypoxic brain damage; and other consequences for the patient such as increased physical disability. If the use of CPR is not successful in restarting the heart or breathing, and in restoring circulation, it may mean that the patient dies in an undignified and traumatic manner.
CPR stats Only 16% of in-hospital patients survive a CPR to discharge – this is less than other developed countries Survival rate is less than 8% for arrests in the community - compared to 20% in hospital. However this can increase to 37% for a witnessed arrest with a trained bystander and an AED 80% of cardiac arrests happen out of hospital but ¾ people do not feel confident enough to perform CPR.
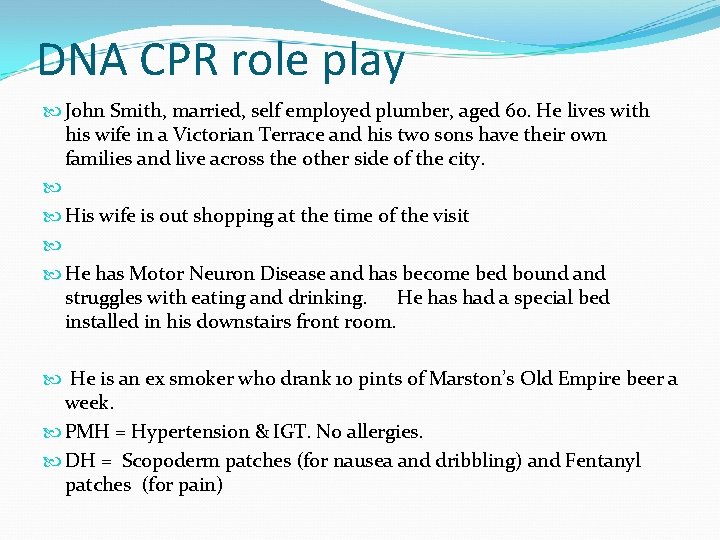
DNA CPR role play John Smith, married, self employed plumber, aged 60. He lives with his wife in a Victorian Terrace and his two sons have their own families and live across the other side of the city. His wife is out shopping at the time of the visit He has Motor Neuron Disease and has become bed bound and struggles with eating and drinking. He has had a special bed installed in his downstairs front room. He is an ex smoker who drank 10 pints of Marston’s Old Empire beer a week. PMH = Hypertension & IGT. No allergies. DH = Scopoderm patches (for nausea and dribbling) and Fentanyl patches (for pain)

The patient. Ideas - You will not be expecting the DNR form discussion but it is something you have been thinking about yourself. You realise that you are dying and that you don’t want the paramedics trying to restart your heart you when you die BUT you do want good ongoing medical care. Concerns – DNR form indicates that the GPs will no longer treat any intercurrent illness and may just give up on him. Also worried about what will happen in the days leading up to death. Expectations – To be kept comfortable and for the GPs not to give up on him. You would be happy to agree to the DNR form and OOH handover if you felt appropriately reassured regards continued ongoing care
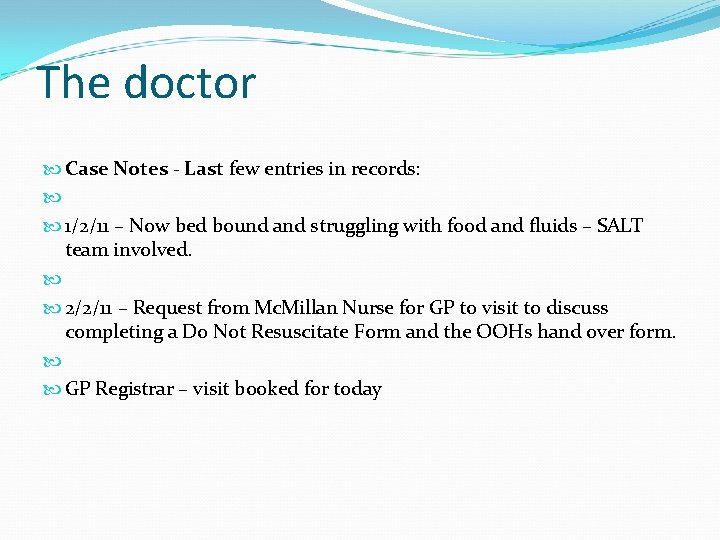
The doctor Case Notes - Last few entries in records: 1/2/11 – Now bed bound and struggling with food and fluids – SALT team involved. 2/2/11 – Request from Mc. Millan Nurse for GP to visit to discuss completing a Do Not Resuscitate Form and the OOHs hand over form. GP Registrar – visit booked for today