VVOG PUS Gent 16 11 2006 Laparoscopic Surgery
- Slides: 32
VVOG – PUS Gent, 16 -11 -2006 Laparoscopic Surgery in Gynaecologic Oncology An Added Value? Philippe De Sutter Ph. De Sutter Laparoscopic Surgery in Gynaecologic Oncology
Laparoscopic surgery in gynaecologic oncology w ’Some disputable applications and one fruitful indication’ D. Dargent n n …LS has not become wide spread …Results confirm that LS reduces risks without jeopardizing chances for cure l n …First-level of evidence is still missing Because we can, we should consider LS l l …Radical operations are disputable indications …Laparoscopic staging is an authentic breaktrough D. Dargent, Editorial in Gynecol Oncol 2005 Ph. De Sutter Laparoscopic Surgery in Gynaecologic Oncology 2
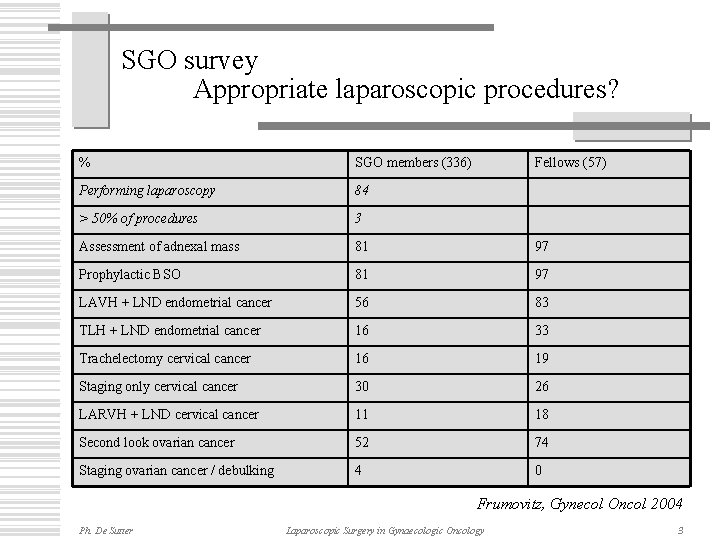
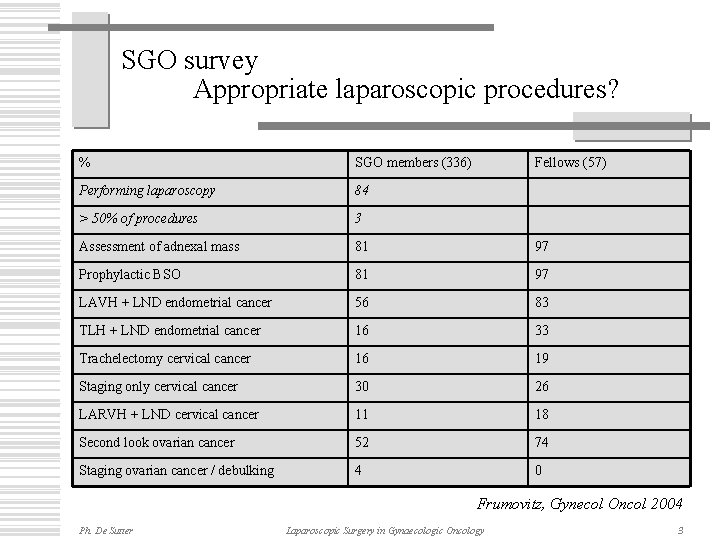
SGO survey Appropriate laparoscopic procedures? % SGO members (336) Fellows (57) Performing laparoscopy 84 > 50% of procedures 3 Assessment of adnexal mass 81 97 Prophylactic BSO 81 97 LAVH + LND endometrial cancer 56 83 TLH + LND endometrial cancer 16 33 Trachelectomy cervical cancer 16 19 Staging only cervical cancer 30 26 LARVH + LND cervical cancer 11 18 Second look ovarian cancer 52 74 Staging ovarian cancer / debulking 4 0 Frumovitz, Gynecol Oncol 2004 Ph. De Sutter Laparoscopic Surgery in Gynaecologic Oncology 3
Minimal Access Surgery Less invasive … more radical? w Laparoscopic / vaginal surgery w Advantages n n Less blood loss Lower overal morbidity and complications Shorter duration of hospital admission Faster recovery w Disadvantages n n n Ph. De Sutter Longer operative time Longer learning curve Laparoscopic specific complications BMI > 30 -35 Conversion to laparotomy Laparoscopic Surgery in Gynaecologic Oncology 4
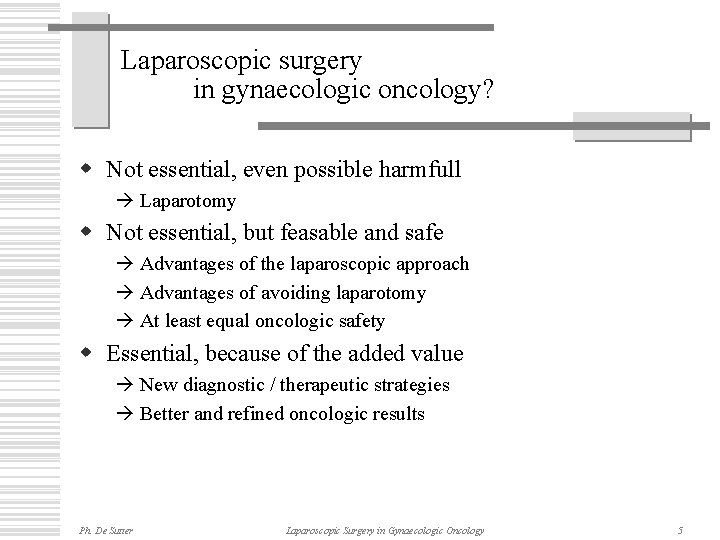
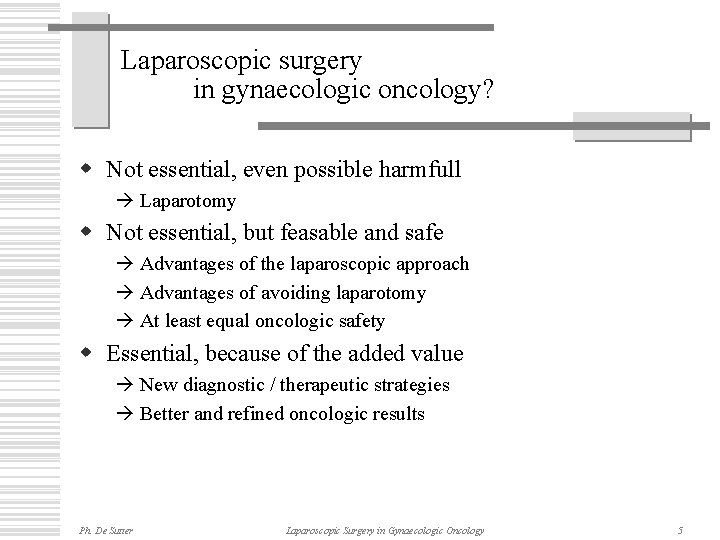
Laparoscopic surgery in gynaecologic oncology? w Not essential, even possible harmfull Laparotomy w Not essential, but feasable and safe Advantages of the laparoscopic approach Advantages of avoiding laparotomy At least equal oncologic safety w Essential, because of the added value New diagnostic / therapeutic strategies Better and refined oncologic results Ph. De Sutter Laparoscopic Surgery in Gynaecologic Oncology 5
Laparoscopic Surgery in Gynaecologic Oncology The suspect adnexal mass and ovarian cancer Ph. De Sutter Laparoscopic Surgery in Gynaecologic Oncology
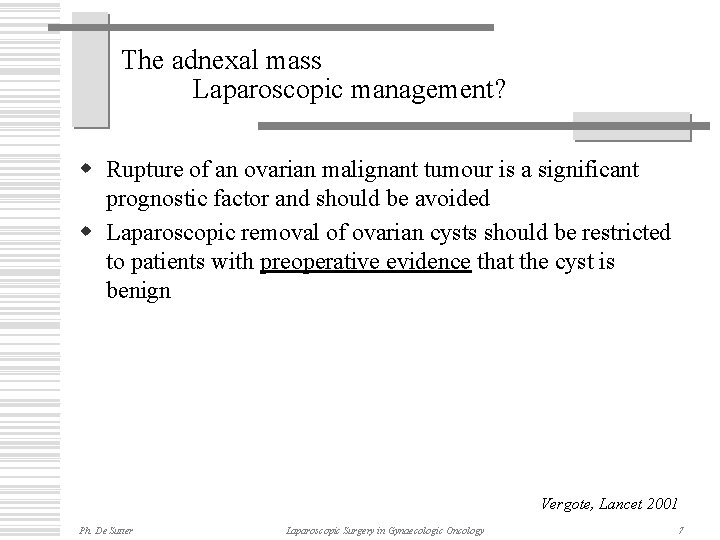
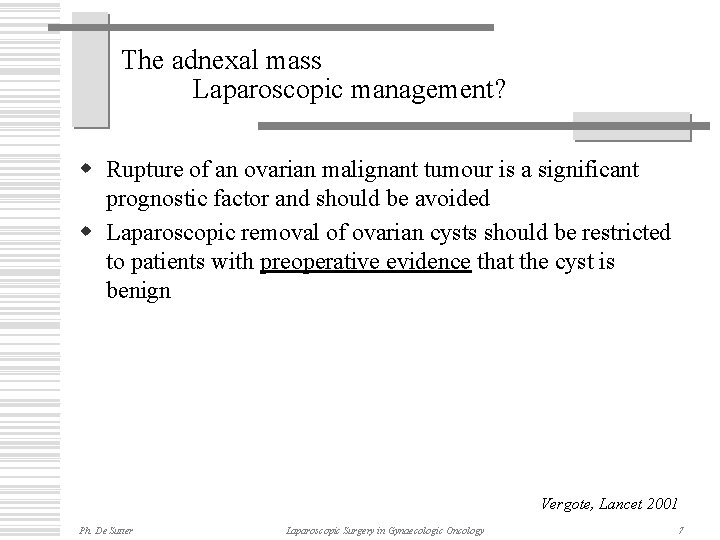
The adnexal mass Laparoscopic management? w Rupture of an ovarian malignant tumour is a significant prognostic factor and should be avoided w Laparoscopic removal of ovarian cysts should be restricted to patients with preoperative evidence that the cyst is benign Vergote, Lancet 2001 Ph. De Sutter Laparoscopic Surgery in Gynaecologic Oncology 7
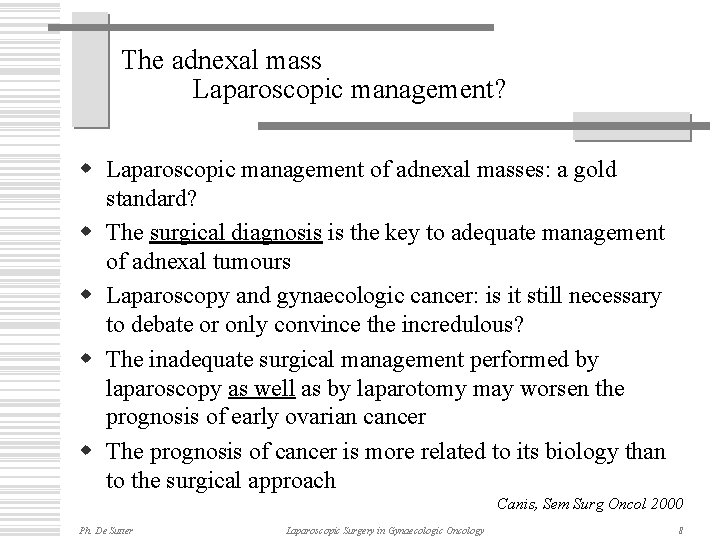
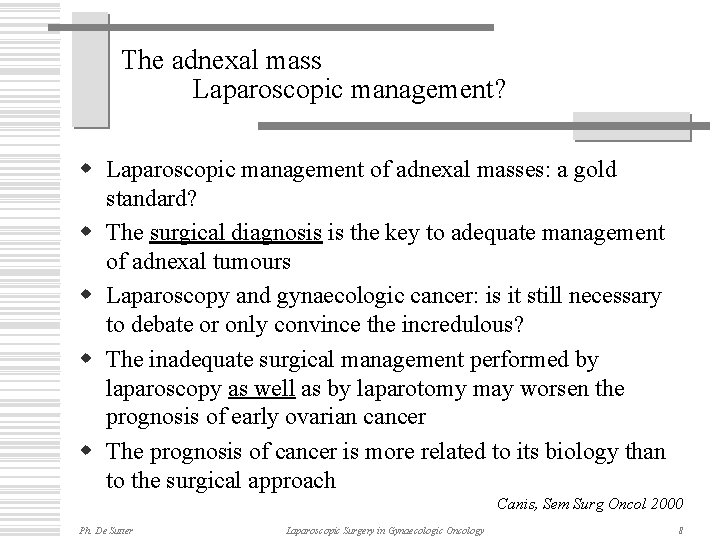
The adnexal mass Laparoscopic management? w Laparoscopic management of adnexal masses: a gold standard? w The surgical diagnosis is the key to adequate management of adnexal tumours w Laparoscopy and gynaecologic cancer: is it still necessary to debate or only convince the incredulous? w The inadequate surgical management performed by laparoscopy as well as by laparotomy may worsen the prognosis of early ovarian cancer w The prognosis of cancer is more related to its biology than to the surgical approach Canis, Sem Surg Oncol 2000 Ph. De Sutter Laparoscopic Surgery in Gynaecologic Oncology 8
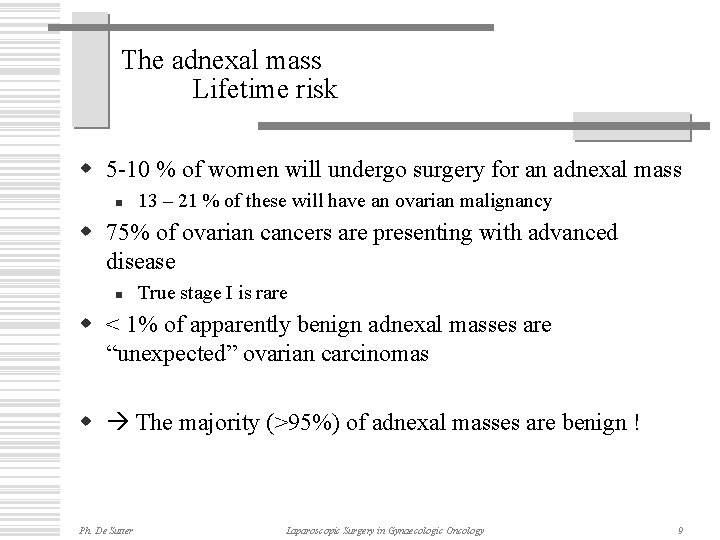
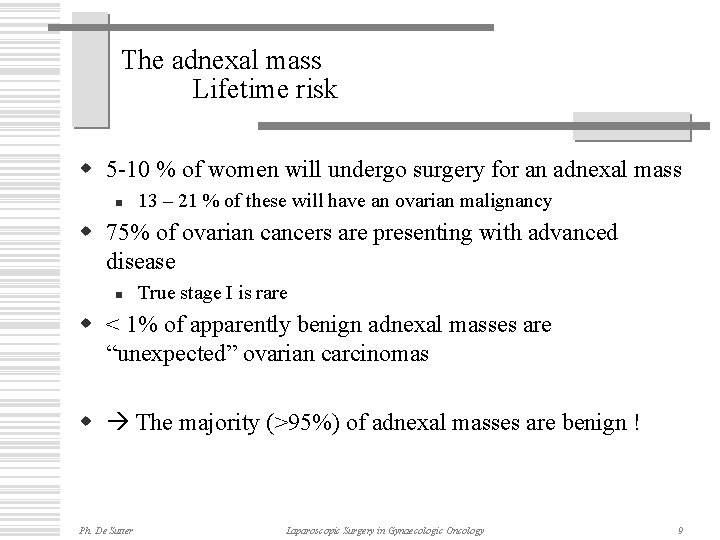
The adnexal mass Lifetime risk w 5 -10 % of women will undergo surgery for an adnexal mass n 13 – 21 % of these will have an ovarian malignancy w 75% of ovarian cancers are presenting with advanced disease n True stage I is rare w < 1% of apparently benign adnexal masses are “unexpected” ovarian carcinomas w The majority (>95%) of adnexal masses are benign ! Ph. De Sutter Laparoscopic Surgery in Gynaecologic Oncology 9
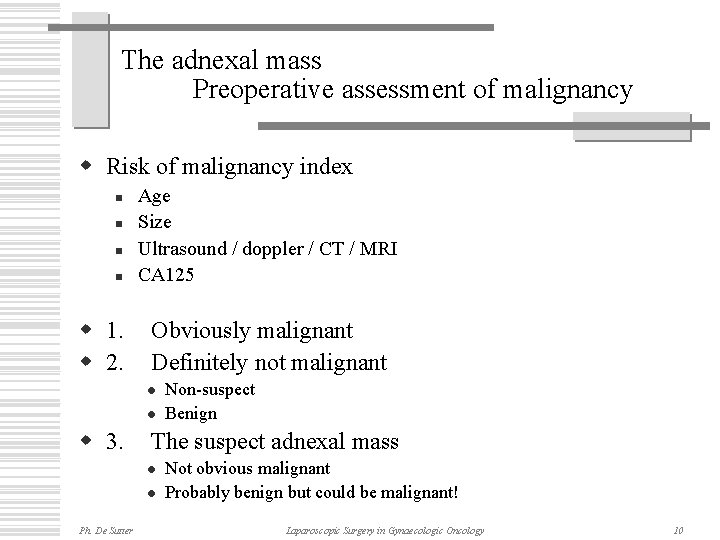
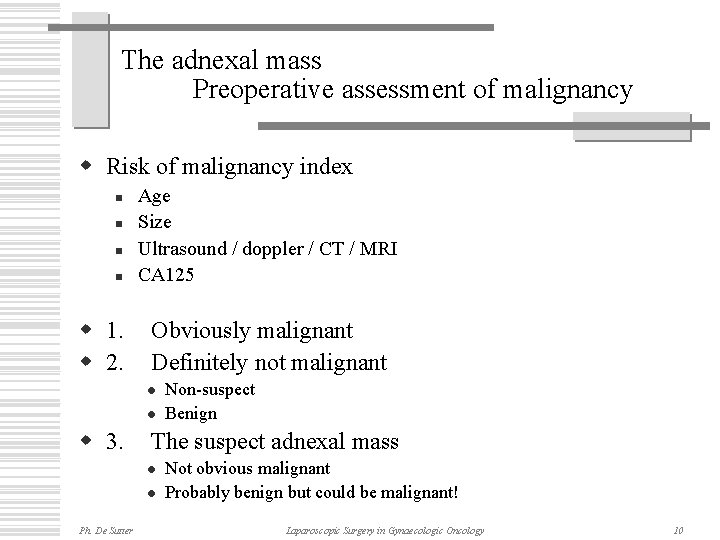
The adnexal mass Preoperative assessment of malignancy w Risk of malignancy index n n w 1. w 2. Age Size Ultrasound / doppler / CT / MRI CA 125 Obviously malignant Definitely not malignant l l w 3. The suspect adnexal mass l l Ph. De Sutter Non-suspect Benign Not obvious malignant Probably benign but could be malignant! Laparoscopic Surgery in Gynaecologic Oncology 10
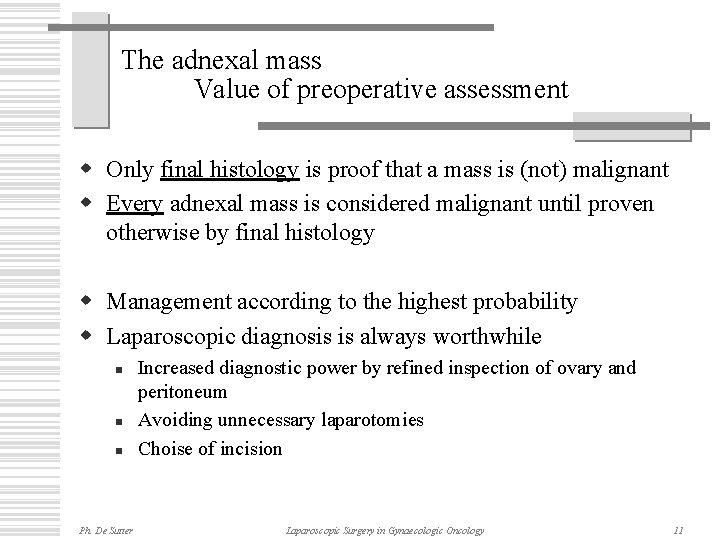
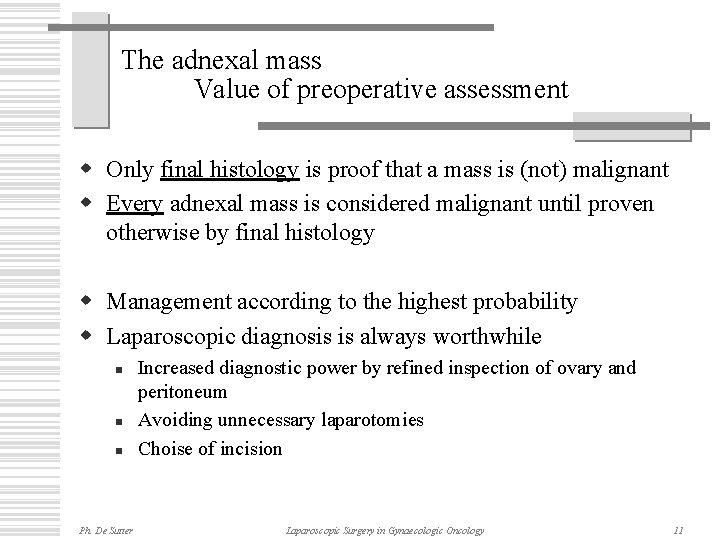
The adnexal mass Value of preoperative assessment w Only final histology is proof that a mass is (not) malignant w Every adnexal mass is considered malignant until proven otherwise by final histology w Management according to the highest probability w Laparoscopic diagnosis is always worthwhile n n n Ph. De Sutter Increased diagnostic power by refined inspection of ovary and peritoneum Avoiding unnecessary laparotomies Choise of incision Laparoscopic Surgery in Gynaecologic Oncology 11
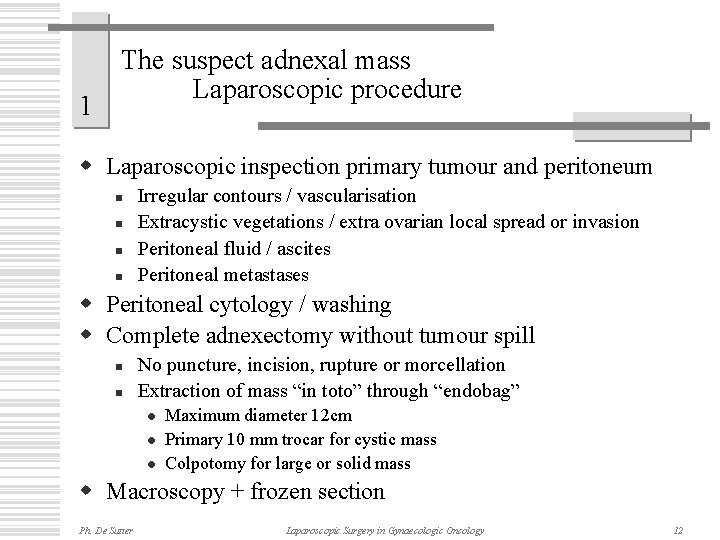
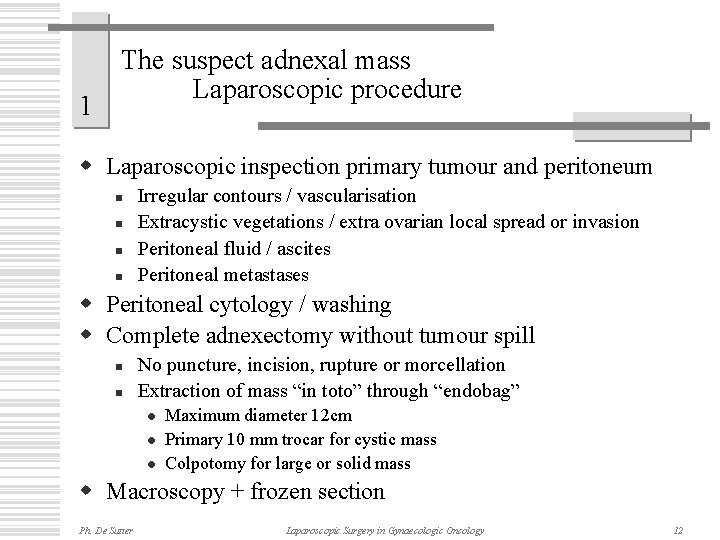
1 The suspect adnexal mass Laparoscopic procedure w Laparoscopic inspection primary tumour and peritoneum n n Irregular contours / vascularisation Extracystic vegetations / extra ovarian local spread or invasion Peritoneal fluid / ascites Peritoneal metastases w Peritoneal cytology / washing w Complete adnexectomy without tumour spill n n No puncture, incision, rupture or morcellation Extraction of mass “in toto” through “endobag” l l l Maximum diameter 12 cm Primary 10 mm trocar for cystic mass Colpotomy for large or solid mass w Macroscopy + frozen section Ph. De Sutter Laparoscopic Surgery in Gynaecologic Oncology 12
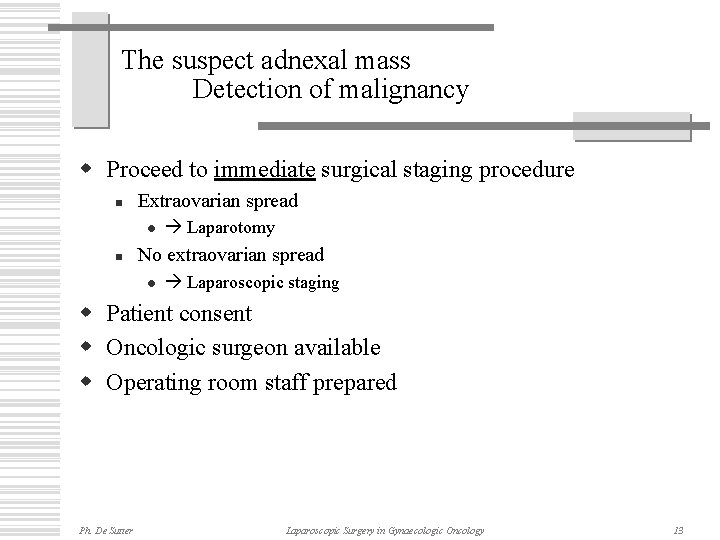
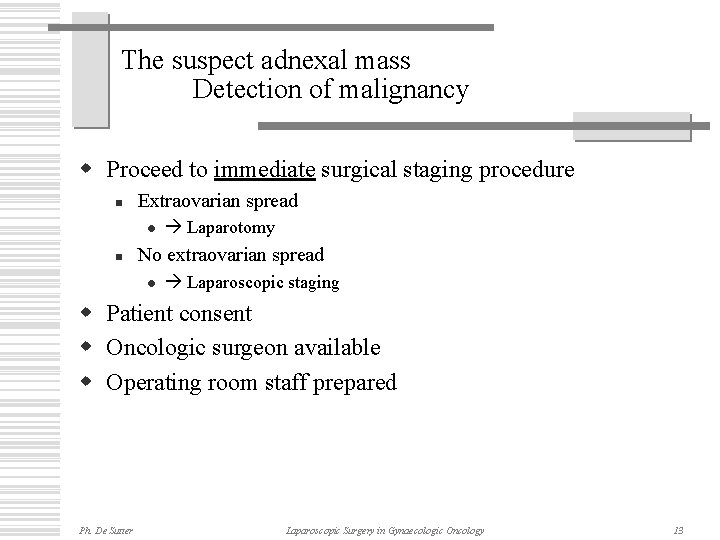
The suspect adnexal mass Detection of malignancy w Proceed to immediate surgical staging procedure n Extraovarian spread l n Laparotomy No extraovarian spread l Laparoscopic staging w Patient consent w Oncologic surgeon available w Operating room staff prepared Ph. De Sutter Laparoscopic Surgery in Gynaecologic Oncology 13
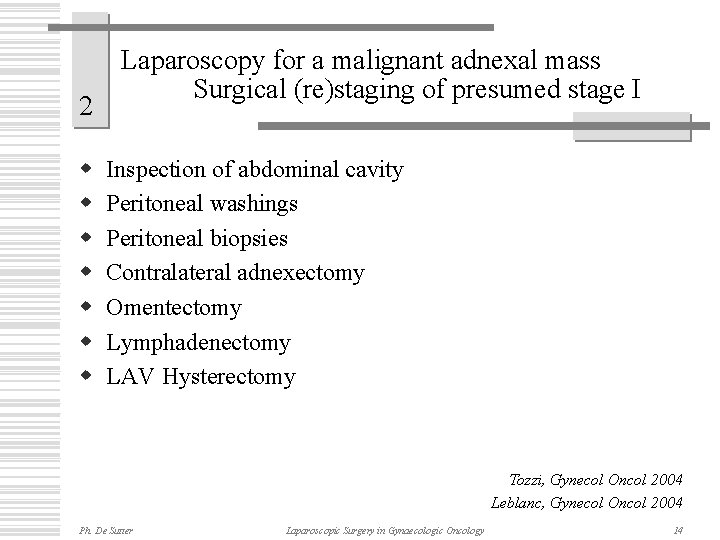
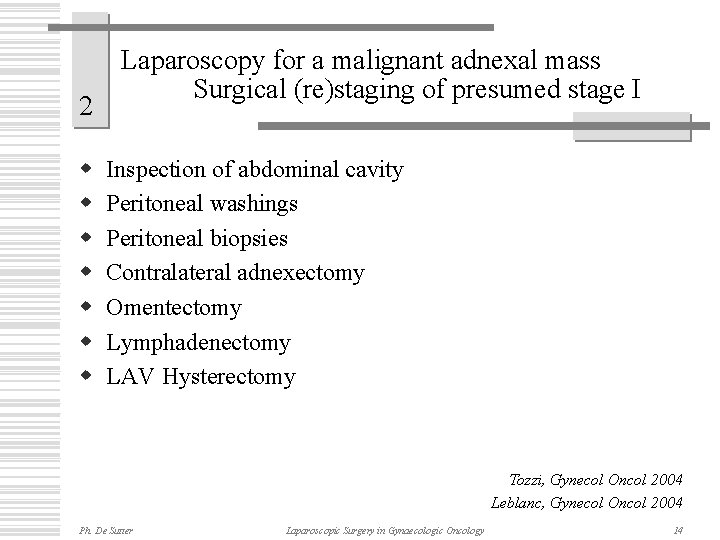
2 w w w w Laparoscopy for a malignant adnexal mass Surgical (re)staging of presumed stage I Inspection of abdominal cavity Peritoneal washings Peritoneal biopsies Contralateral adnexectomy Omentectomy Lymphadenectomy LAV Hysterectomy Tozzi, Gynecol Oncol 2004 Leblanc, Gynecol Oncol 2004 Ph. De Sutter Laparoscopic Surgery in Gynaecologic Oncology 14
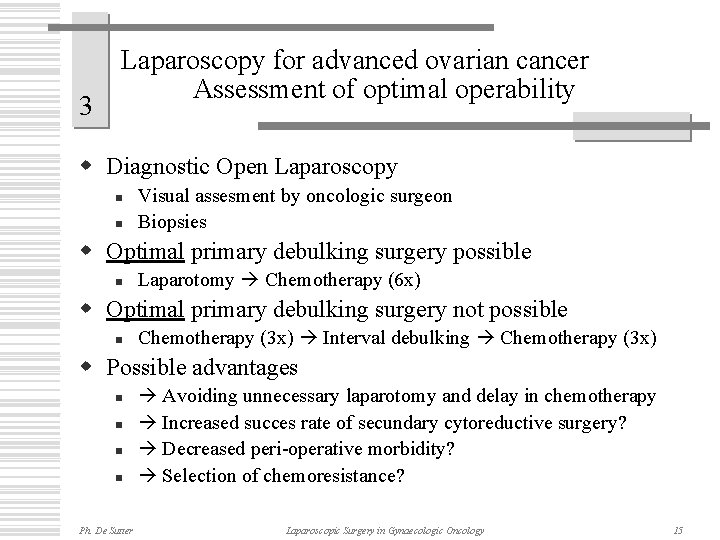
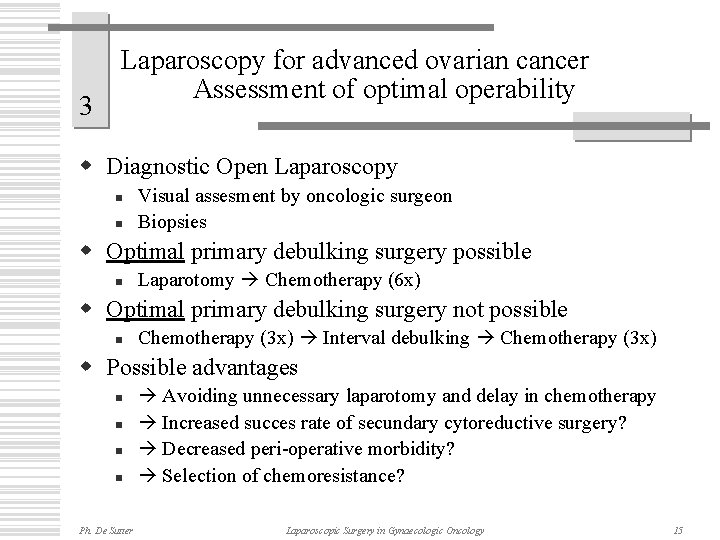
3 Laparoscopy for advanced ovarian cancer Assessment of optimal operability w Diagnostic Open Laparoscopy n n Visual assesment by oncologic surgeon Biopsies w Optimal primary debulking surgery possible n Laparotomy Chemotherapy (6 x) w Optimal primary debulking surgery not possible n Chemotherapy (3 x) Interval debulking Chemotherapy (3 x) w Possible advantages n n Ph. De Sutter Avoiding unnecessary laparotomy and delay in chemotherapy Increased succes rate of secundary cytoreductive surgery? Decreased peri-operative morbidity? Selection of chemoresistance? Laparoscopic Surgery in Gynaecologic Oncology 15
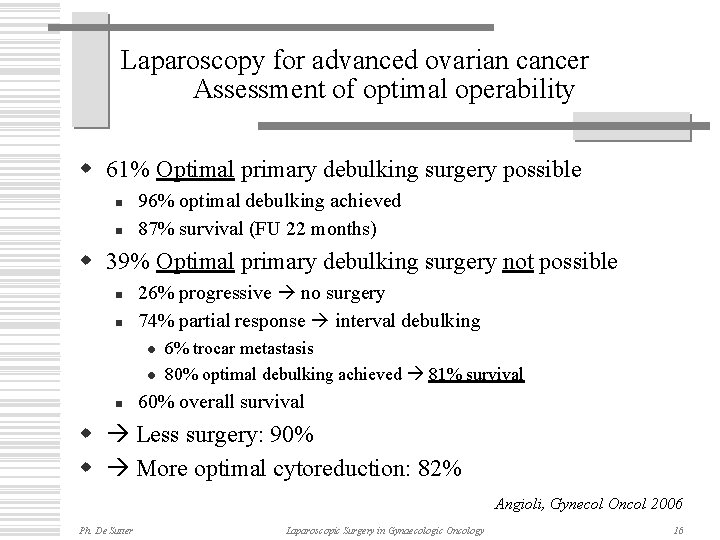
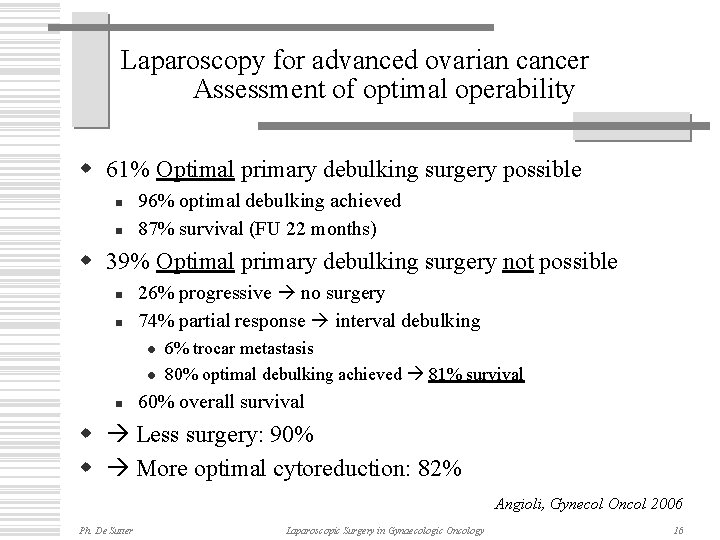
Laparoscopy for advanced ovarian cancer Assessment of optimal operability w 61% Optimal primary debulking surgery possible n n 96% optimal debulking achieved 87% survival (FU 22 months) w 39% Optimal primary debulking surgery not possible n n 26% progressive no surgery 74% partial response interval debulking l l n 6% trocar metastasis 80% optimal debulking achieved 81% survival 60% overall survival w Less surgery: 90% w More optimal cytoreduction: 82% Angioli, Gynecol Oncol 2006 Ph. De Sutter Laparoscopic Surgery in Gynaecologic Oncology 16
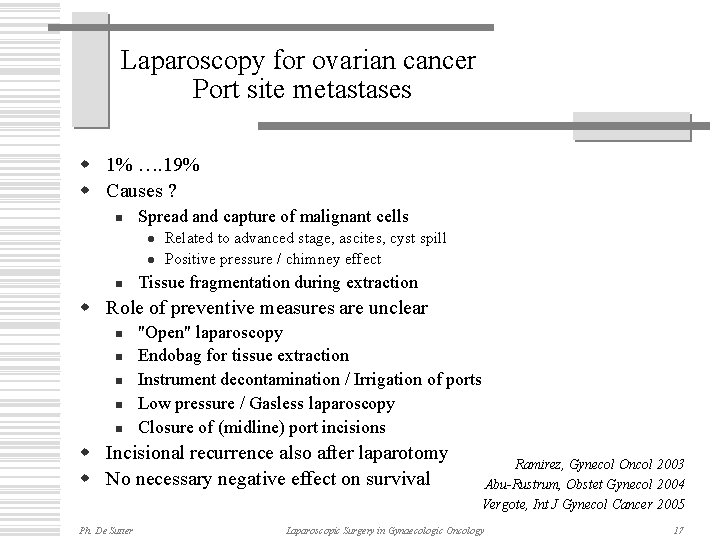
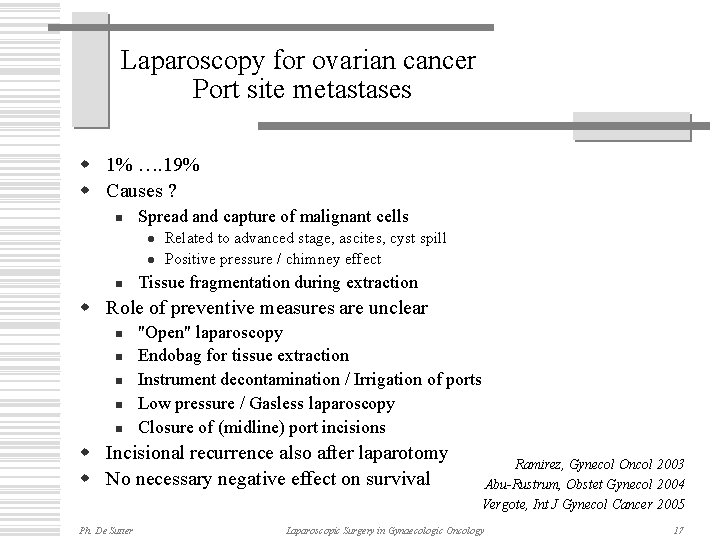
Laparoscopy for ovarian cancer Port site metastases w 1% …. 19% w Causes ? n Spread and capture of malignant cells l l n Related to advanced stage, ascites, cyst spill Positive pressure / chimney effect Tissue fragmentation during extraction w Role of preventive measures are unclear n n n "Open" laparoscopy Endobag for tissue extraction Instrument decontamination / Irrigation of ports Low pressure / Gasless laparoscopy Closure of (midline) port incisions w Incisional recurrence also after laparotomy w No necessary negative effect on survival Ph. De Sutter Ramirez, Gynecol Oncol 2003 Abu-Rustrum, Obstet Gynecol 2004 Vergote, Int J Gynecol Cancer 2005 Laparoscopic Surgery in Gynaecologic Oncology 17
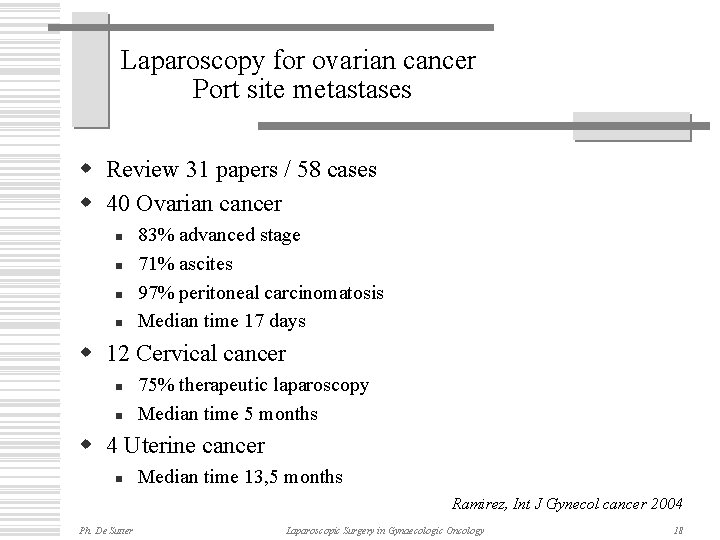
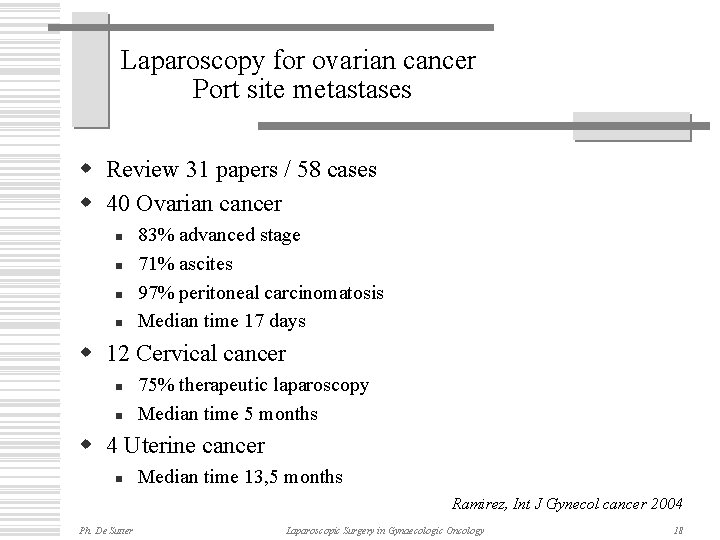
Laparoscopy for ovarian cancer Port site metastases w Review 31 papers / 58 cases w 40 Ovarian cancer n n 83% advanced stage 71% ascites 97% peritoneal carcinomatosis Median time 17 days w 12 Cervical cancer n n 75% therapeutic laparoscopy Median time 5 months w 4 Uterine cancer n Median time 13, 5 months Ramirez, Int J Gynecol cancer 2004 Ph. De Sutter Laparoscopic Surgery in Gynaecologic Oncology 18
Laparoscopic Surgery in Gynaecologic Oncology Cervical Cancer Ph. De Sutter Laparoscopic Surgery in Gynaecologic Oncology
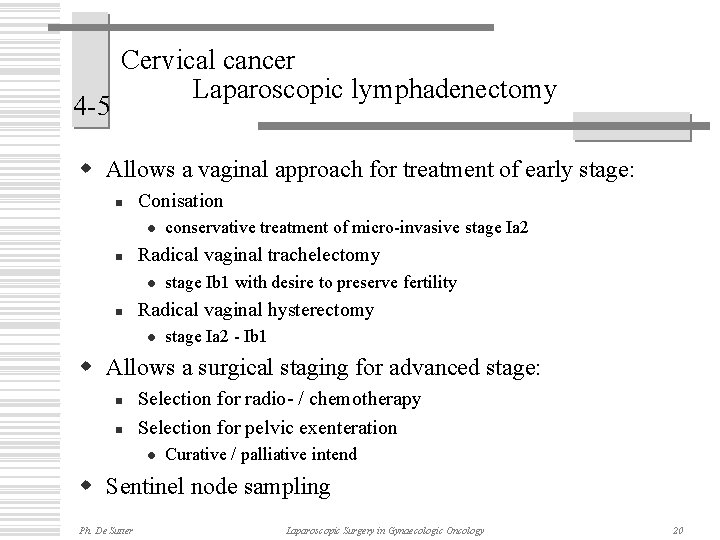
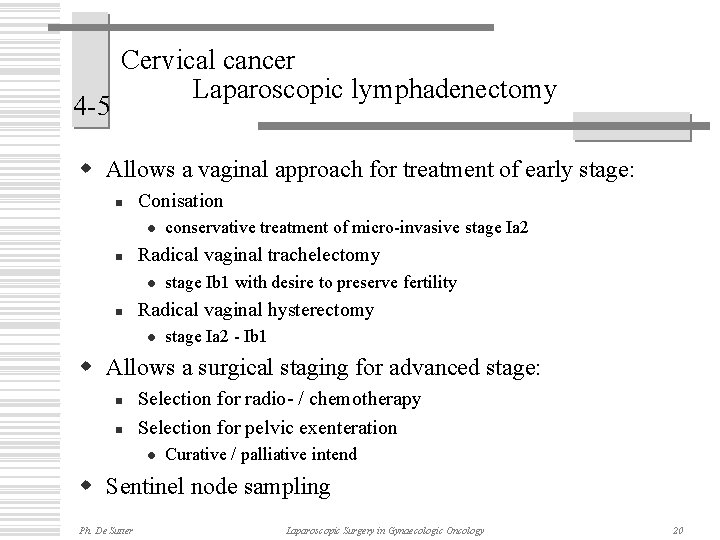
4 -5 Cervical cancer Laparoscopic lymphadenectomy w Allows a vaginal approach for treatment of early stage: n Conisation l n Radical vaginal trachelectomy l n conservative treatment of micro-invasive stage Ia 2 stage Ib 1 with desire to preserve fertility Radical vaginal hysterectomy l stage Ia 2 - Ib 1 w Allows a surgical staging for advanced stage: n n Selection for radio- / chemotherapy Selection for pelvic exenteration l Curative / palliative intend w Sentinel node sampling Ph. De Sutter Laparoscopic Surgery in Gynaecologic Oncology 20
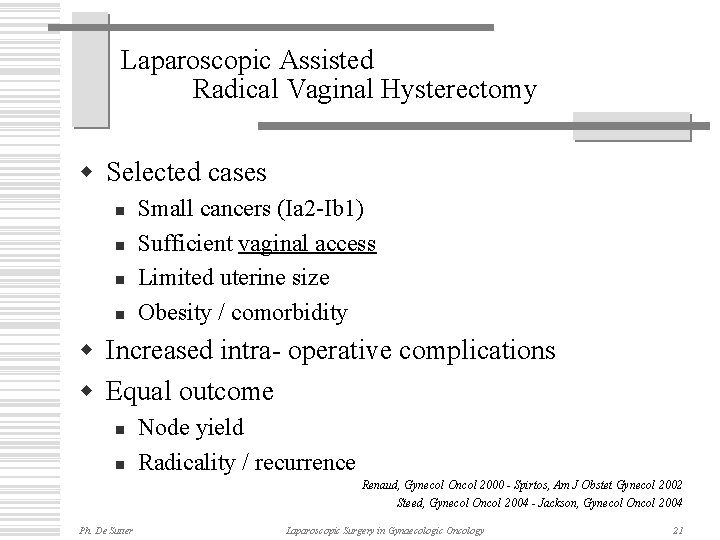
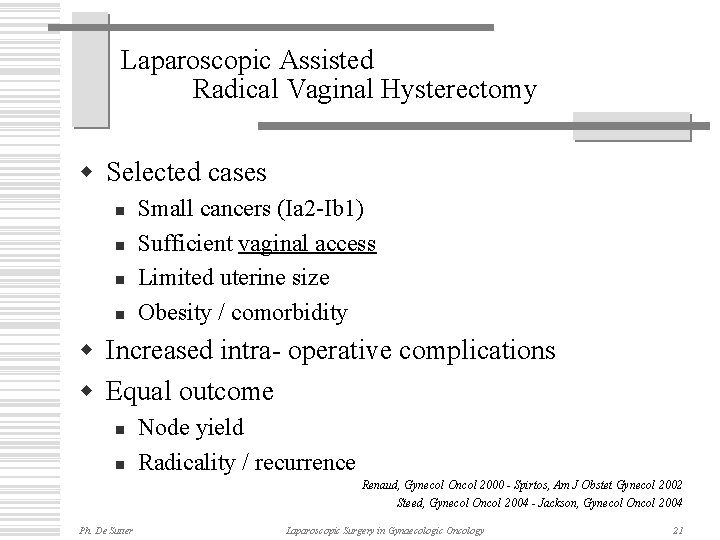
Laparoscopic Assisted Radical Vaginal Hysterectomy w Selected cases n n Small cancers (Ia 2 -Ib 1) Sufficient vaginal access Limited uterine size Obesity / comorbidity w Increased intra- operative complications w Equal outcome n n Node yield Radicality / recurrence Renaud, Gynecol Oncol 2000 - Spirtos, Am J Obstet Gynecol 2002 Steed, Gynecol Oncol 2004 - Jackson, Gynecol Oncol 2004 Ph. De Sutter Laparoscopic Surgery in Gynaecologic Oncology 21
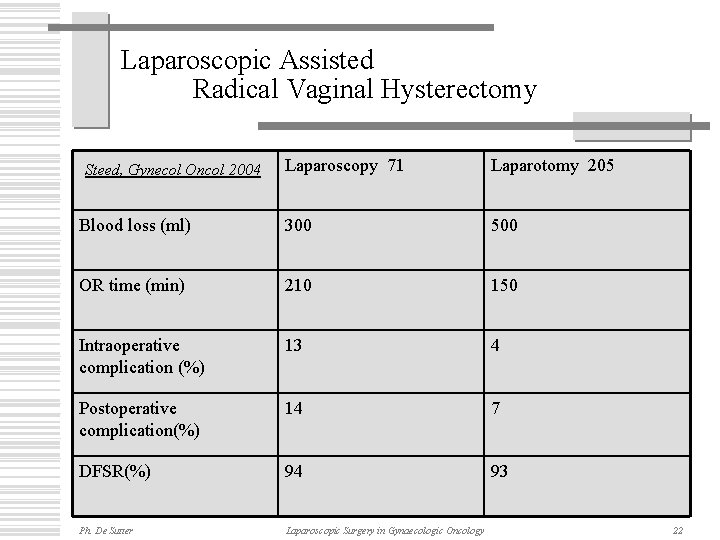
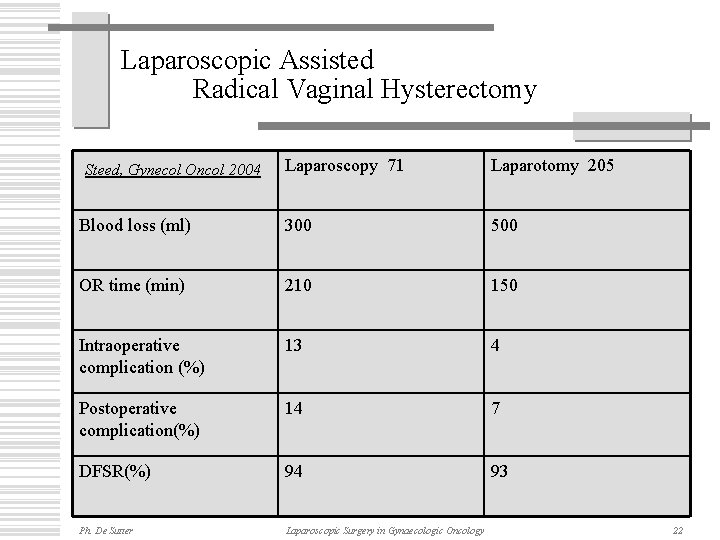
Laparoscopic Assisted Radical Vaginal Hysterectomy Laparoscopy 71 Laparotomy 205 Blood loss (ml) 300 500 OR time (min) 210 150 Intraoperative complication (%) 13 4 Postoperative complication(%) 14 7 DFSR(%) 94 93 Ph. De Sutter Laparoscopic Surgery in Gynaecologic Oncology Steed, Gynecol Oncol 2004 22
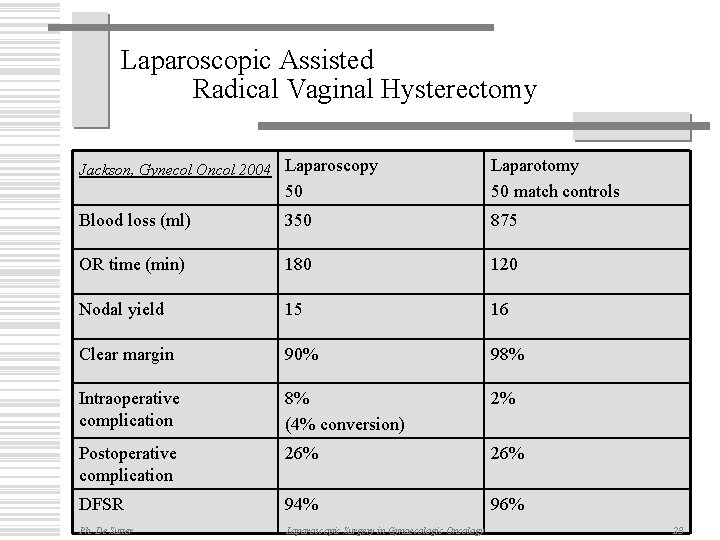
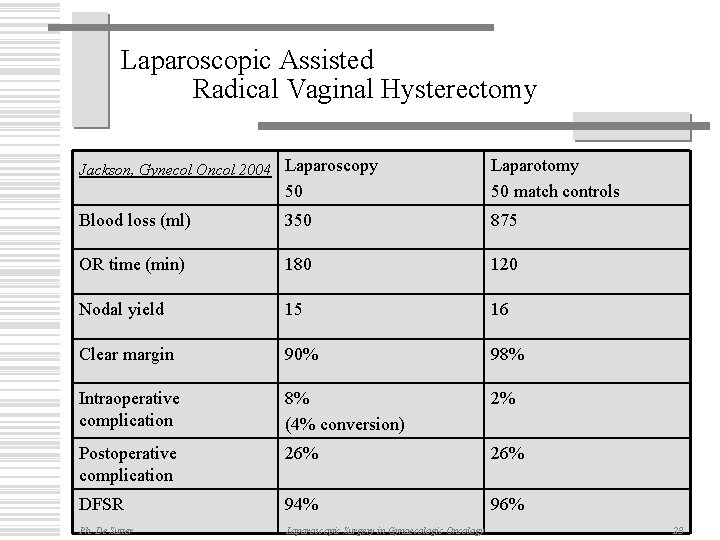
Laparoscopic Assisted Radical Vaginal Hysterectomy Jackson, Gynecol Oncol 2004 Laparoscopy 50 Laparotomy 50 match controls Blood loss (ml) 350 875 OR time (min) 180 120 Nodal yield 15 16 Clear margin 90% 98% Intraoperative complication 8% (4% conversion) 2% Postoperative complication 26% DFSR 94% 96% Ph. De Sutter Laparoscopic Surgery in Gynaecologic Oncology 23
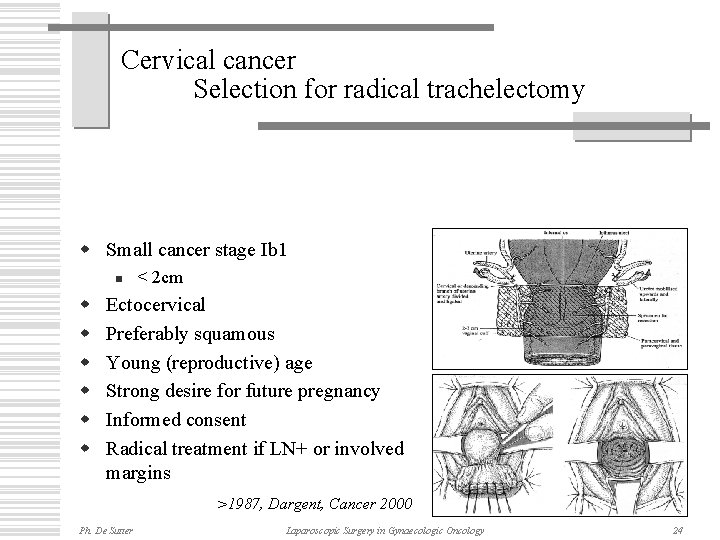
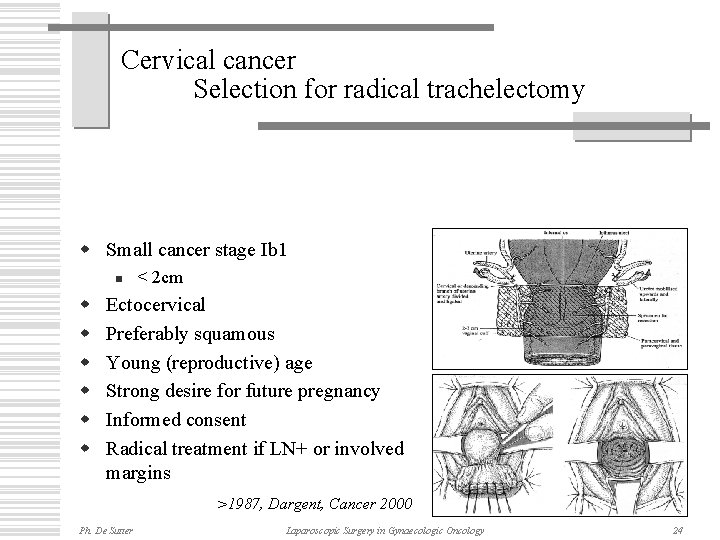
Cervical cancer Selection for radical trachelectomy w Small cancer stage Ib 1 n w w w < 2 cm Ectocervical Preferably squamous Young (reproductive) age Strong desire for future pregnancy Informed consent Radical treatment if LN+ or involved margins >1987, Dargent, Cancer 2000 Ph. De Sutter Laparoscopic Surgery in Gynaecologic Oncology 24
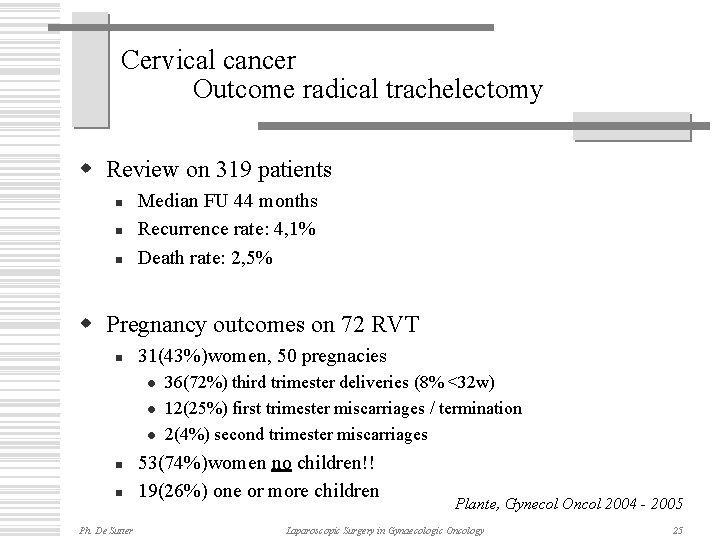
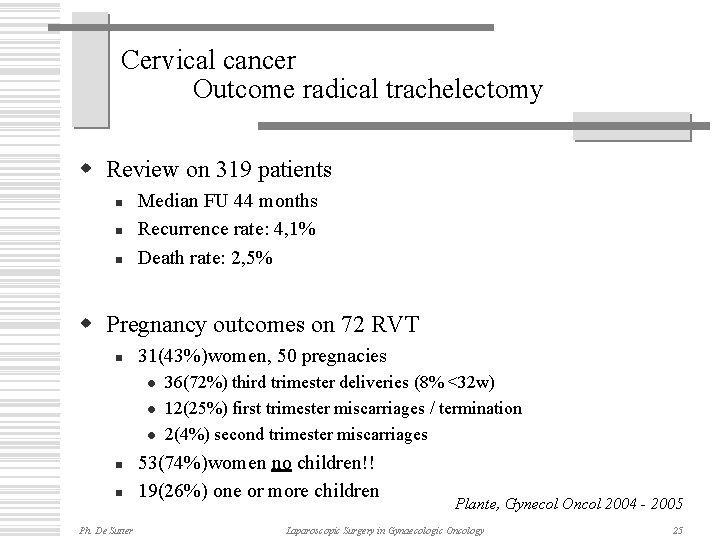
Cervical cancer Outcome radical trachelectomy w Review on 319 patients n n n Median FU 44 months Recurrence rate: 4, 1% Death rate: 2, 5% w Pregnancy outcomes on 72 RVT n 31(43%)women, 50 pregnacies l l l n n Ph. De Sutter 36(72%) third trimester deliveries (8% <32 w) 12(25%) first trimester miscarriages / termination 2(4%) second trimester miscarriages 53(74%)women no children!! 19(26%) one or more children Plante, Gynecol Oncol 2004 - 2005 Laparoscopic Surgery in Gynaecologic Oncology 25
Laparoscopic Surgery in Gynaecologic Oncology Endometrial Cancer Ph. De Sutter Laparoscopic Surgery in Gynaecologic Oncology
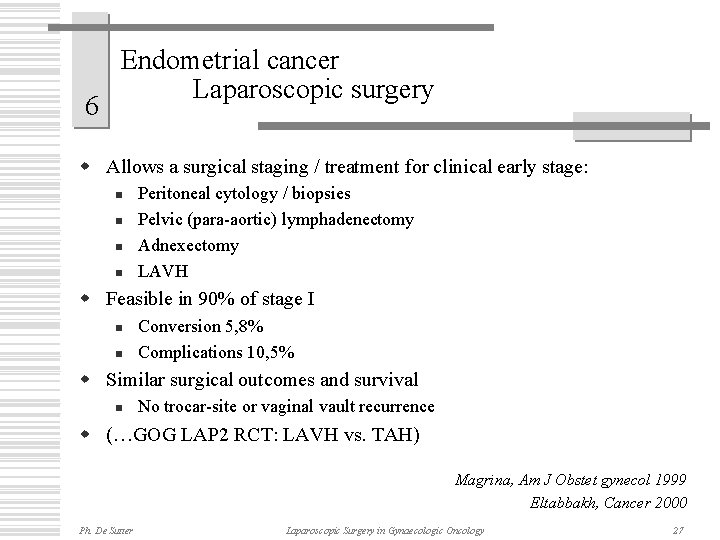
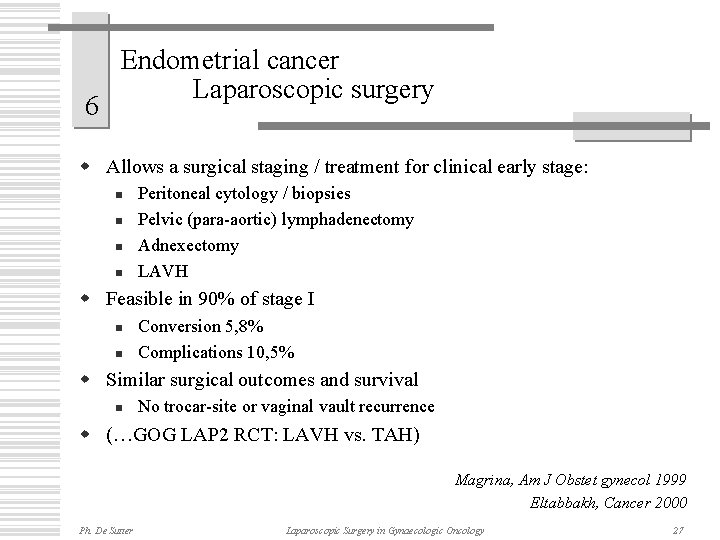
6 Endometrial cancer Laparoscopic surgery w Allows a surgical staging / treatment for clinical early stage: n n Peritoneal cytology / biopsies Pelvic (para-aortic) lymphadenectomy Adnexectomy LAVH w Feasible in 90% of stage I n n Conversion 5, 8% Complications 10, 5% w Similar surgical outcomes and survival n No trocar-site or vaginal vault recurrence w (…GOG LAP 2 RCT: LAVH vs. TAH) Magrina, Am J Obstet gynecol 1999 Eltabbakh, Cancer 2000 Ph. De Sutter Laparoscopic Surgery in Gynaecologic Oncology 27
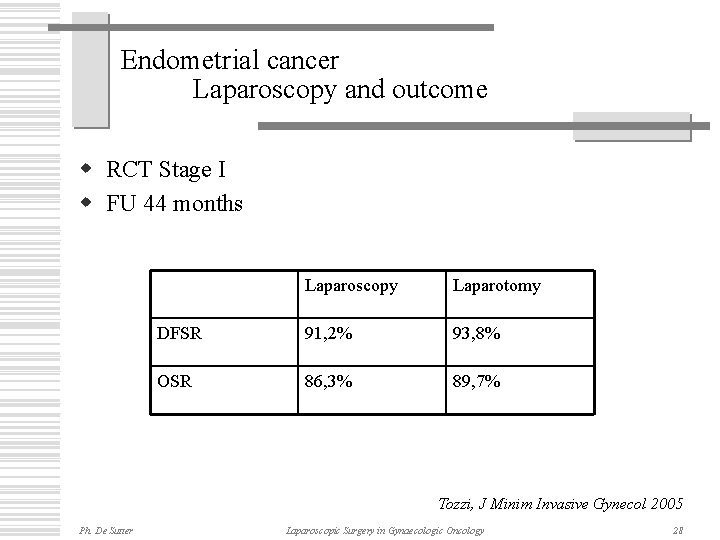
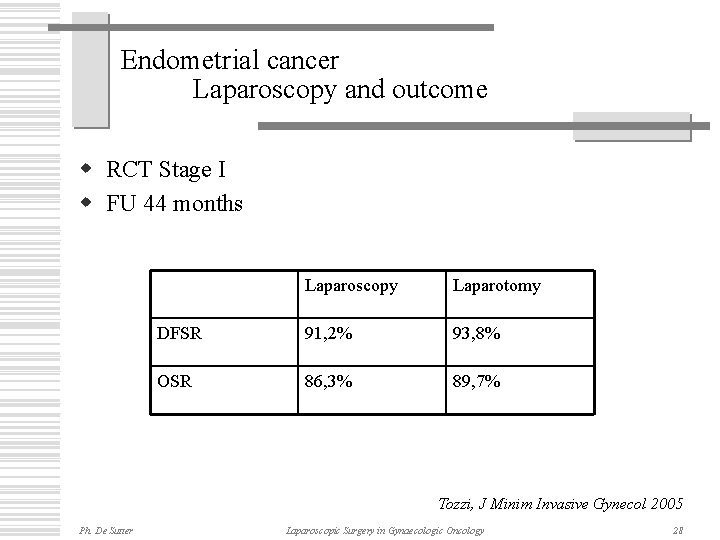
Endometrial cancer Laparoscopy and outcome w RCT Stage I w FU 44 months Laparoscopy Laparotomy DFSR 91, 2% 93, 8% OSR 86, 3% 89, 7% Tozzi, J Minim Invasive Gynecol 2005 Ph. De Sutter Laparoscopic Surgery in Gynaecologic Oncology 28
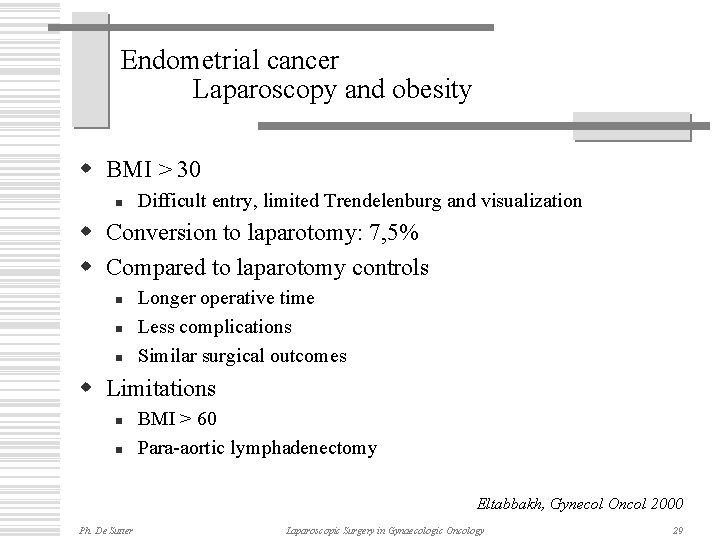
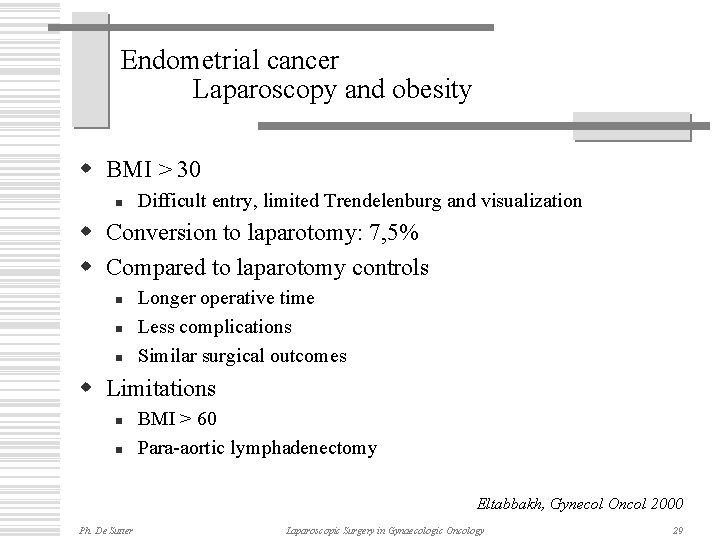
Endometrial cancer Laparoscopy and obesity w BMI > 30 n Difficult entry, limited Trendelenburg and visualization w Conversion to laparotomy: 7, 5% w Compared to laparotomy controls n n n Longer operative time Less complications Similar surgical outcomes w Limitations n n BMI > 60 Para-aortic lymphadenectomy Eltabbakh, Gynecol Oncol 2000 Ph. De Sutter Laparoscopic Surgery in Gynaecologic Oncology 29
Laparoscopic surgery in gynaecologic oncology Added value 1. Management of adnexal masses 2. Surgical (re)staging of stage I ovarian cancer 3. Assessment of optimal operability for advanced ovarian cancer 4. Allows a vaginal approach for treatment of early stage cervical cancer 5. Allows a surgical staging for advanced stage cervical cancer 6. Allows a surgical / pathological staging for treatment of clinical early stage endometrial cancer Ph. De Sutter Laparoscopic Surgery in Gynaecologic Oncology 30
Laparoscopic surgery in gynaecologic oncology Conclusion w Oncologic safety n n Initial treatment final outcome Exception is not the rule w Appropriate selection of cases!! n n n Clinical stage Vaginal access! Meaningful indication w Anticipation of unsuspected findings n Ph. De Sutter …. . Conversion to laparotomy Laparoscopic Surgery in Gynaecologic Oncology 31
Ph. De Sutter Laparoscopic Surgery in Gynaecologic Oncology
 Vvog gynaecologie
Vvog gynaecologie Disadvantages of laparoscopic hysterectomy
Disadvantages of laparoscopic hysterectomy Pyloroplasty cpt code
Pyloroplasty cpt code Ompetency
Ompetency Corso mongo db
Corso mongo db Packet utilization standard
Packet utilization standard Al khader proteins
Al khader proteins What does coughing up pus look like
What does coughing up pus look like Pus formation
Pus formation Splinter with pus
Splinter with pus In mormant viata
In mormant viata Gemeentehuis gent zuid
Gemeentehuis gent zuid Krc gent atletiek
Krc gent atletiek Housing first gent
Housing first gent Https://gentcode.co.uk/
Https://gentcode.co.uk/ Anne gent
Anne gent Zalenzoeker gent
Zalenzoeker gent Studente ontvangt gent
Studente ontvangt gent Portugese wijn gent
Portugese wijn gent Blaisantvest
Blaisantvest Simon says gent
Simon says gent Site:slidetodoc.com
Site:slidetodoc.com Ian gent
Ian gent Kongostraat 42 9000 gent
Kongostraat 42 9000 gent Buurtstewards gent
Buurtstewards gent Ugent taalcursus
Ugent taalcursus Samen een plan
Samen een plan Esb therapie gent
Esb therapie gent Lop
Lop Wespenbestrijding brugge
Wespenbestrijding brugge Verhuizers gent
Verhuizers gent Https://gentcode.co.uk/
Https://gentcode.co.uk/ Hostel de draecke
Hostel de draecke