Vulvar Conditions Shelley Miksis DNP ARNP 01 21

- Slides: 113
Vulvar Conditions Shelley Miksis, DNP, ARNP 01 -21 -10 University of Washington School of Nursing
Plan for today’s session • General considerations Basis for differential • Evaluation History, PE, Dx procedures • Management • Focus on specific conditions VIN, vulvar CA, LS, LP, & hyperplasia 2 University of Washington School of Nursing
General Considerations • Wide array of benign, premalignant & malignant lesions • Eyes alone insufficient to tell benign from malignant • Biopsy needed for diagnosis and to identify neoplasia 3 University of Washington School of Nursing
General Considerations • Symptoms related to vulvar disorders include: – Pruritus – Vulvodynia – Superficial dyspareunia – Lesions • White, red, pigmented, raised, or ulcerated • Patient may be asymptomatic 4 University of Washington School of Nursing
General Considerations • Vulvar symptoms may be caused by: – Infections – Dermatologic disorders – Neoplastic vulvar disorders – Non-neoplastic vulvar disorders 5 University of Washington School of Nursing
Definition of terms Neoplasia= Formation of new tissue, neoplasm Neoplasm = An abnormal new growth of tissue that grows by cellular proliferation more rapidly than normal, continues to grow after the stimuli that initiated the new growth cease, shows partial or complete lack of structural organization and functional coordination with the normal tissue, and usually forms a distinct mass of tissue which may be either benign or malignant. 6 University of Washington School of Nursing
Classification: Non-neoplastic epithelial disorders of skin and mucosa – Lichen sclerosus – Squamous hyperplasia – Other dermatoses [ psoriasis, lichen simplex, lichen planus, dermatits, etc. ] 7 University of Washington School of Nursing
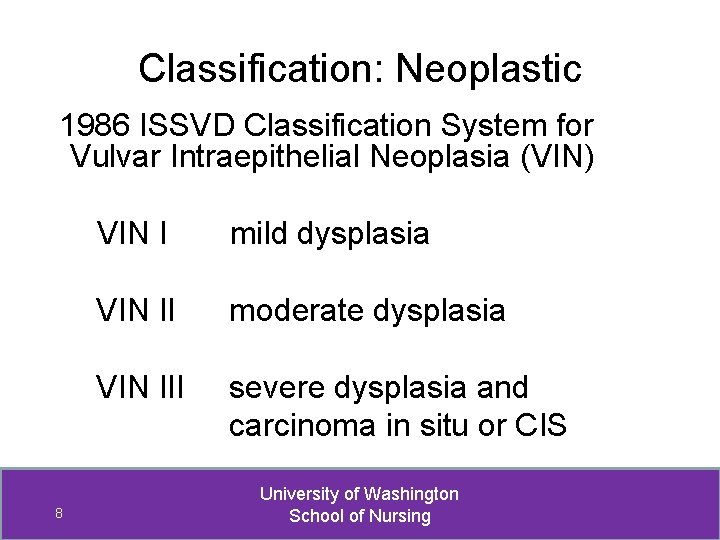
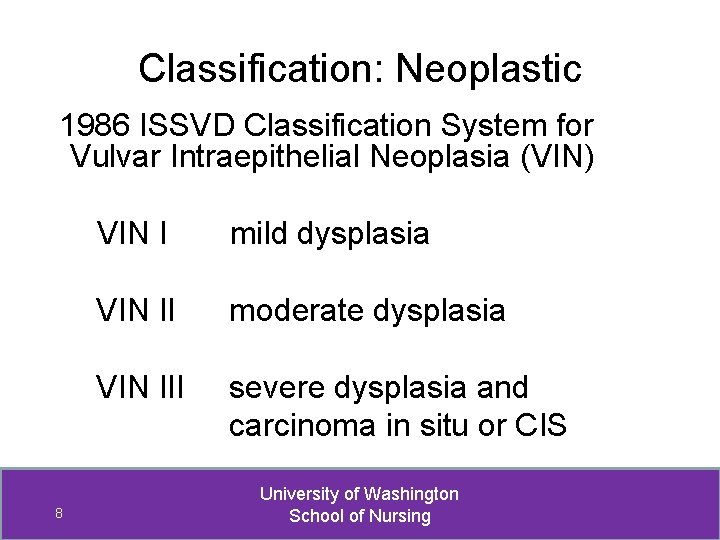
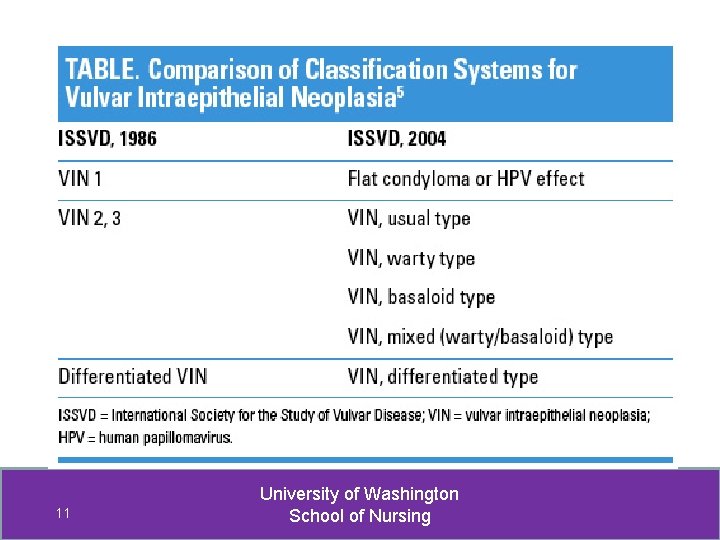
Classification: Neoplastic 1986 ISSVD Classification System for Vulvar Intraepithelial Neoplasia (VIN) 8 VIN I mild dysplasia VIN II moderate dysplasia VIN III severe dysplasia and carcinoma in situ or CIS University of Washington School of Nursing
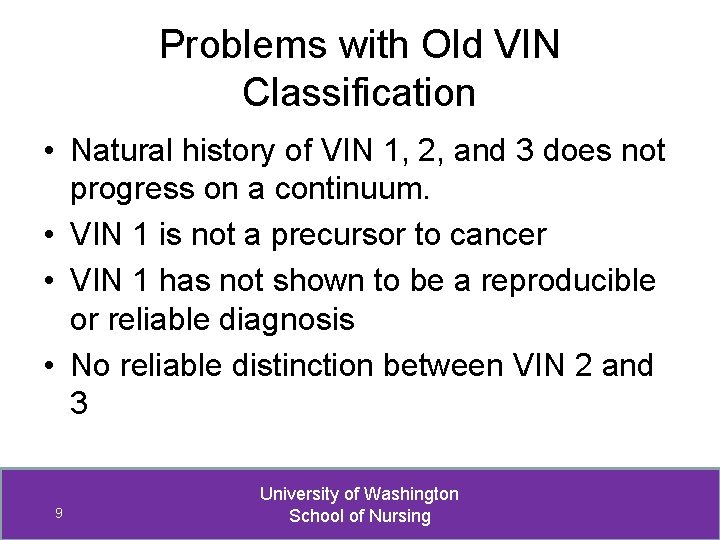
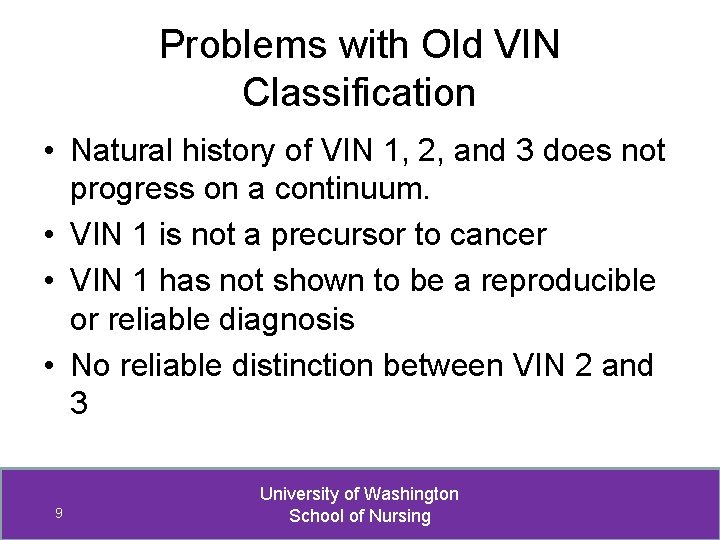
Problems with Old VIN Classification • Natural history of VIN 1, 2, and 3 does not progress on a continuum. • VIN 1 is not a precursor to cancer • VIN 1 has not shown to be a reproducible or reliable diagnosis • No reliable distinction between VIN 2 and 3 9 University of Washington School of Nursing
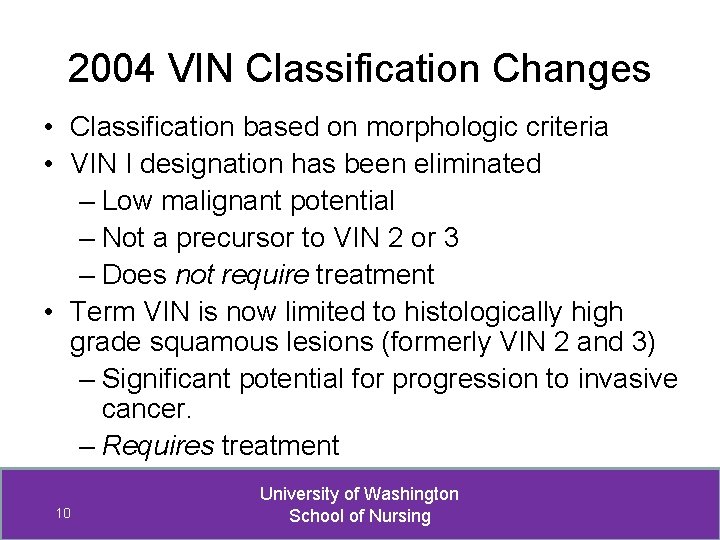
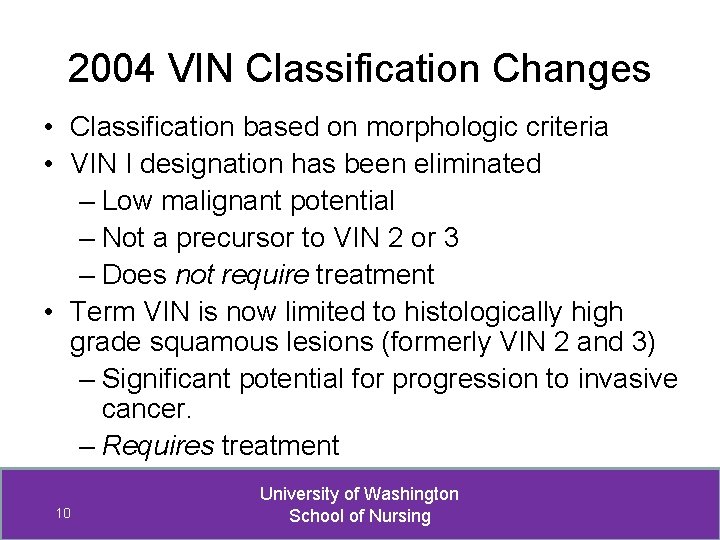
2004 VIN Classification Changes • Classification based on morphologic criteria • VIN I designation has been eliminated – Low malignant potential – Not a precursor to VIN 2 or 3 – Does not require treatment • Term VIN is now limited to histologically high grade squamous lesions (formerly VIN 2 and 3) – Significant potential for progression to invasive cancer. – Requires treatment 10 University of Washington School of Nursing
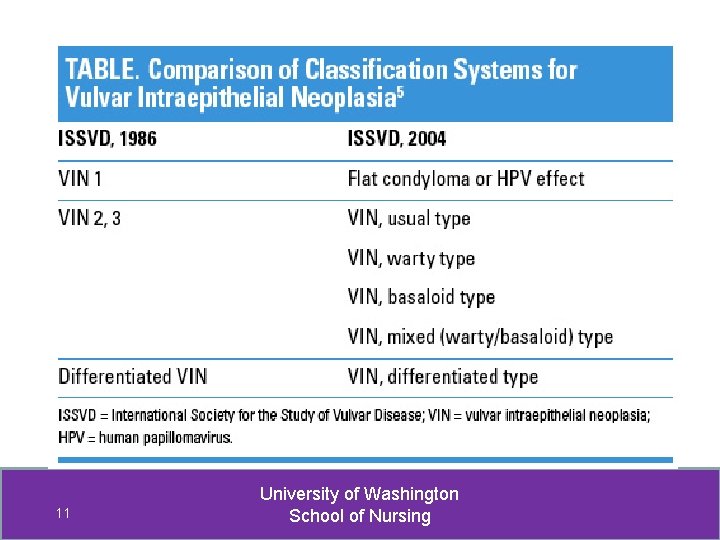
11 University of Washington School of Nursing
Classification: Neoplastic 2004 ISSVD Classification System for VIN a. VIN, usual type (r/t high risk HPV) – Warty type – Basaloid type – Mixed (warty, basaloid) type b. VIN, differentiated type (not r/t HPV) 12 University of Washington School of Nursing
Classification: Neoplastic • VIN, usual type – most common • Basaloid and warty subtypes based on morphologic and histologic features – Basaloid – thickened epithelium with relatively flat, smooth surface – Warty – undulating or spiking surface, giving condylomatous appearance 13 University of Washington School of Nursing
Approach to differential Based on morphology of lesion, not symptoms • • • White lesions Red lesions Dark or pigmented lesions Ulcerative or erosive lesions Solid and cystic tumors 14 University of Washington School of Nursing
Differential: Key to diagnoses listed • If a disease or condition regular font • If an infection Italics • If malignant or pre-malignant bold 15 University of Washington School of Nursing
White lesions • • • 16 Condyloma acuminate / genital warts Lichen sclerosus Post-inflammatory hypopigmentation Squamous cell hyperplasia VIN Vitiligo University of Washington School of Nursing
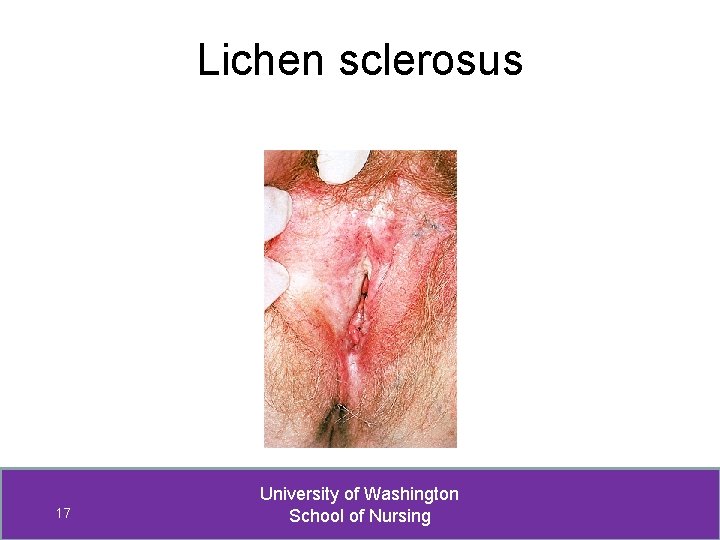
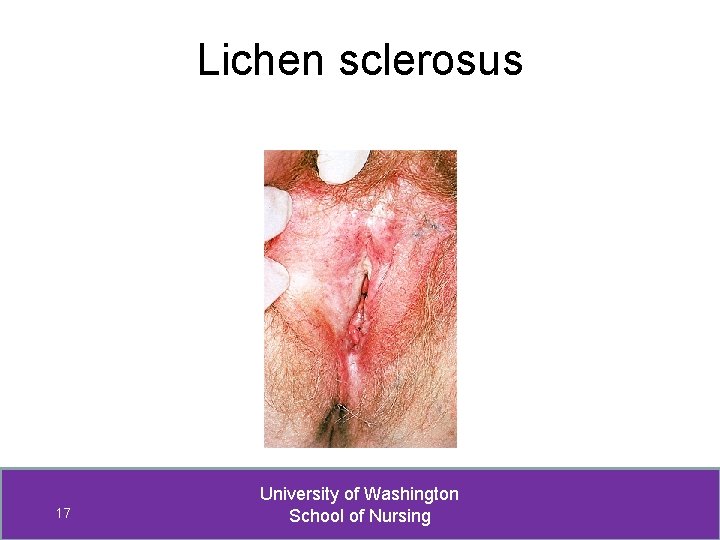
Lichen sclerosus 17 University of Washington School of Nursing
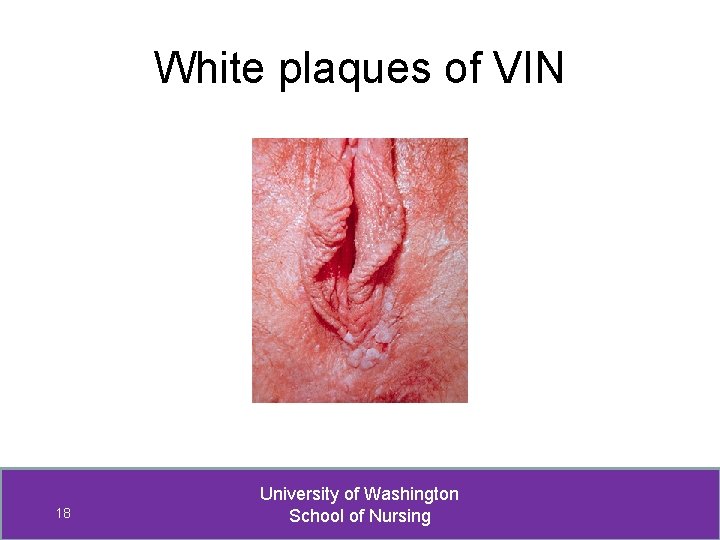
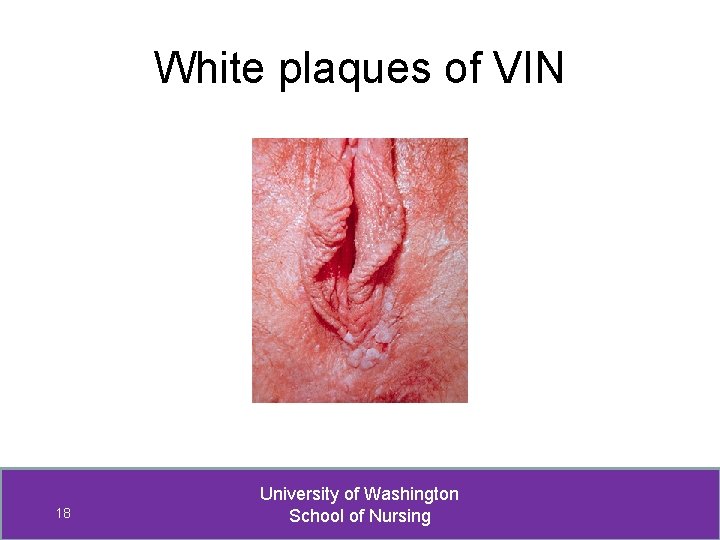
White plaques of VIN 18 University of Washington School of Nursing

Condyloma acuminata 19 University of Washington School of Nursing
Red Lesions • • • Allergic or contact/irritant dermatitis Cutaneous candidiasis Lichen planus Paget’s Disease Psoriasis VIN 20 University of Washington School of Nursing
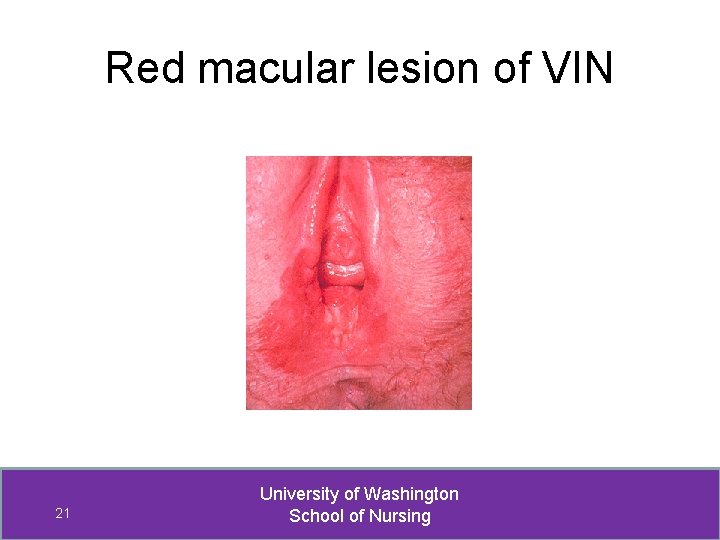
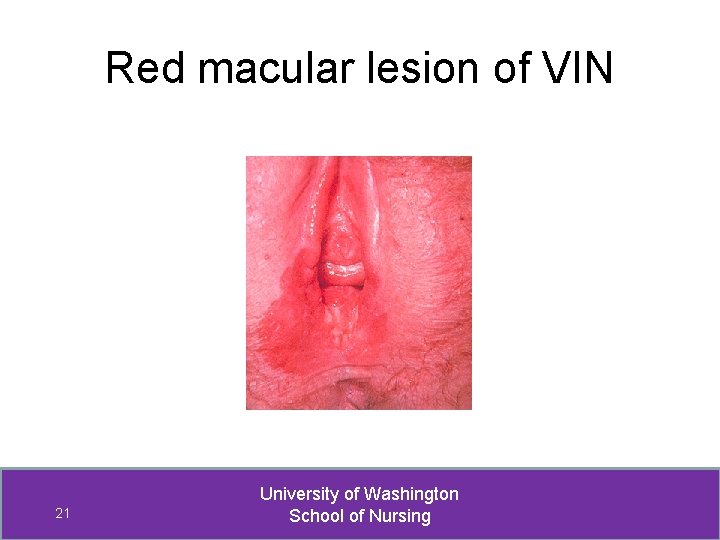
Red macular lesion of VIN 21 University of Washington School of Nursing
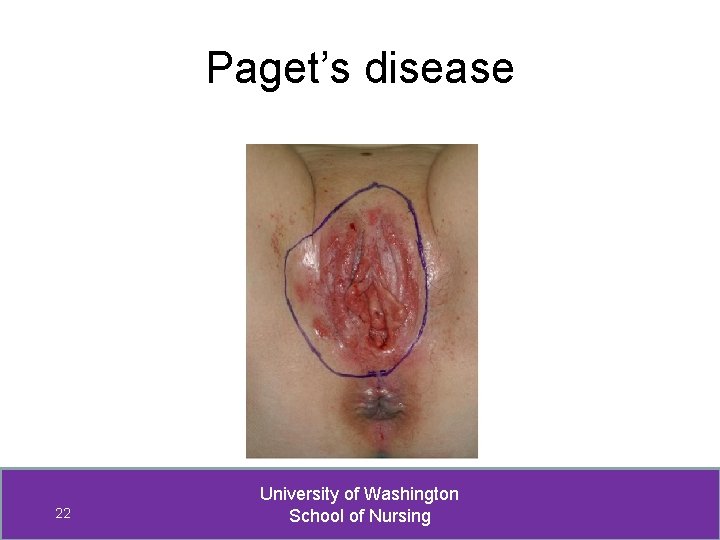
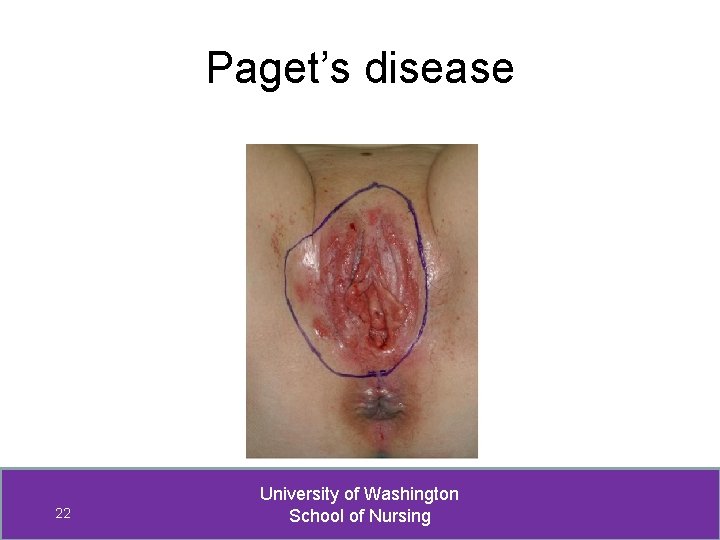
Paget’s disease 22 University of Washington School of Nursing
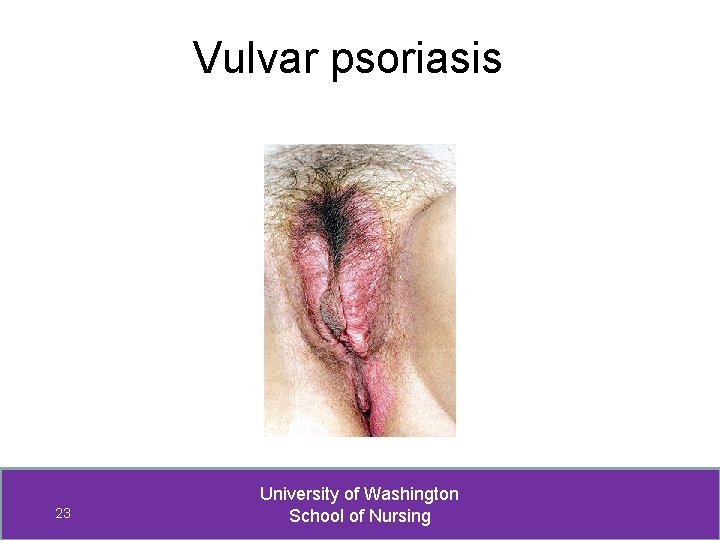
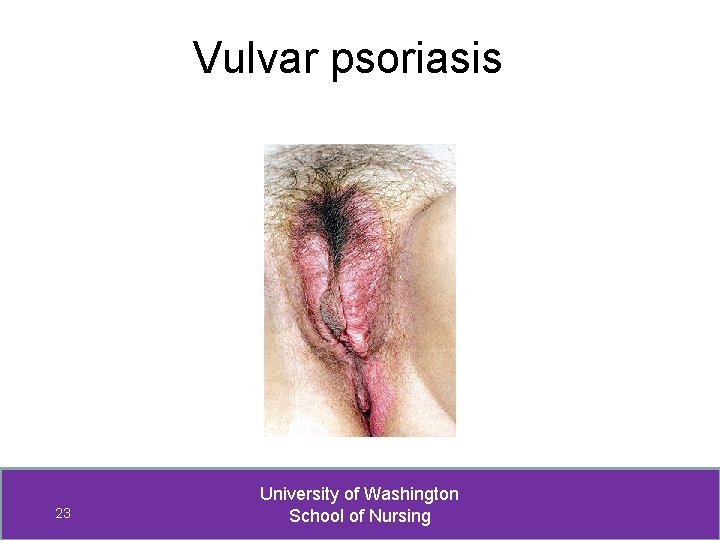
Vulvar psoriasis 23 University of Washington School of Nursing
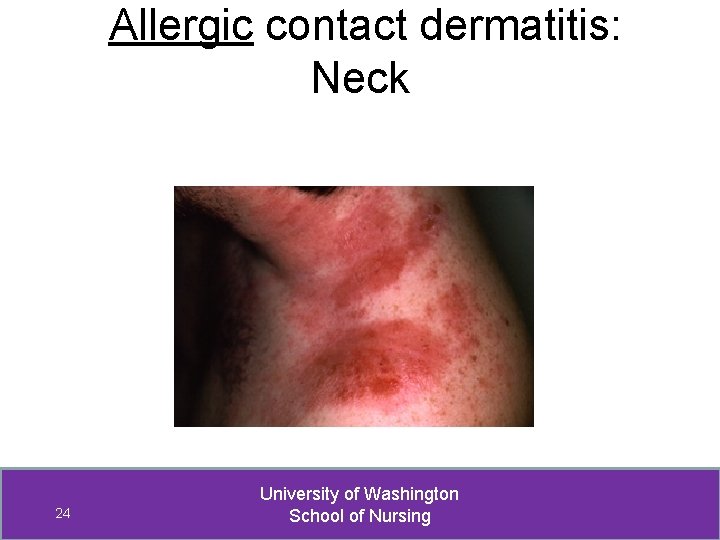
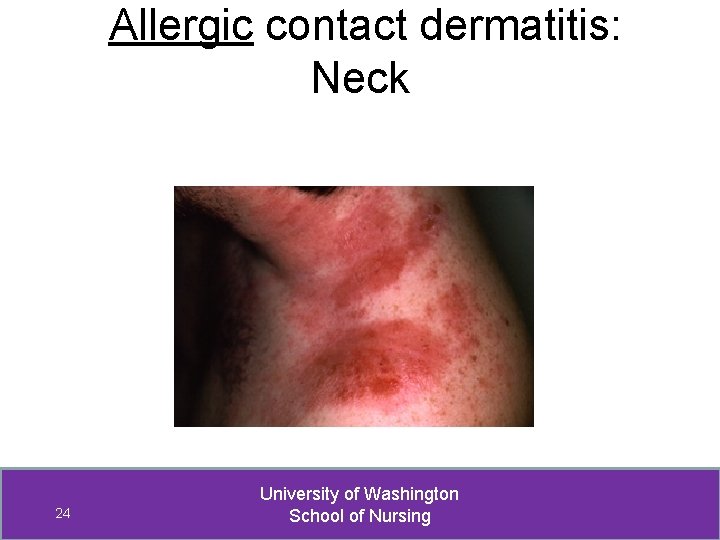
Allergic contact dermatitis: Neck 24 University of Washington School of Nursing
Dark lesions • • Acanthosis negricans Basal cell carcinoma Lentigo Melanoma Nevi Post-inflammatory hyperpigmentation Seborrheic keratosis VIN 25 University of Washington School of Nursing
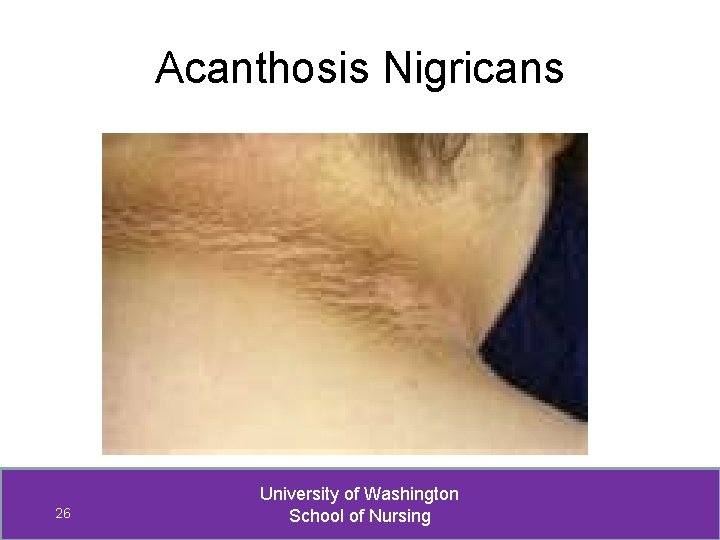
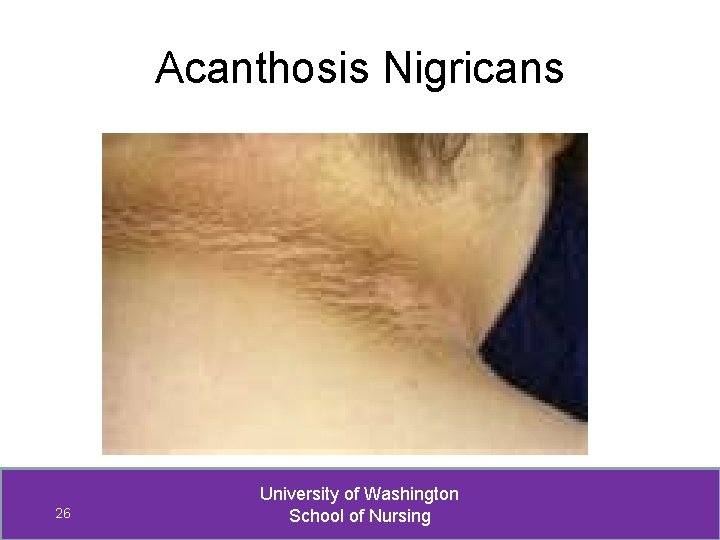
Acanthosis Nigricans 26 University of Washington School of Nursing
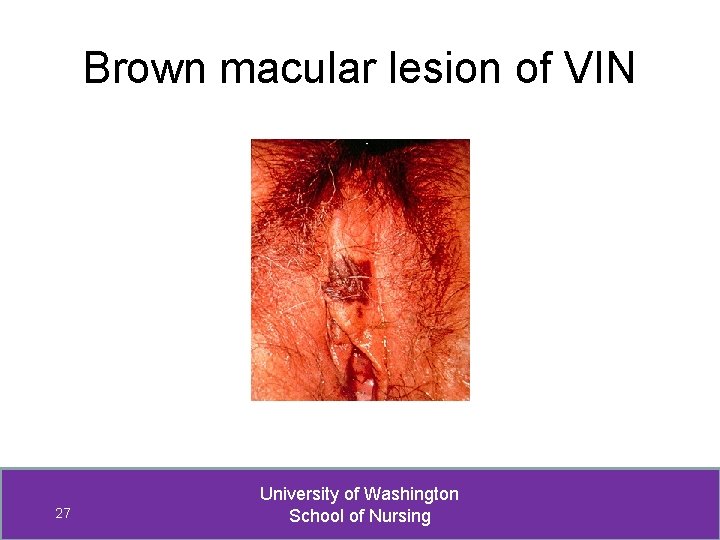
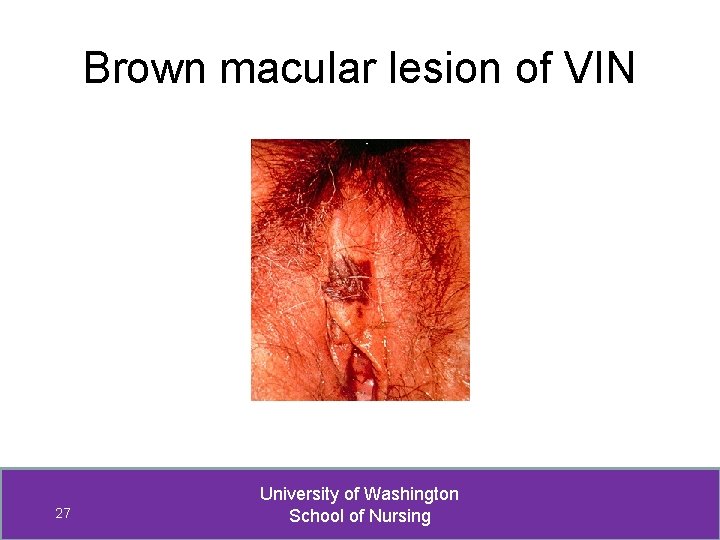
Brown macular lesion of VIN 27 University of Washington School of Nursing
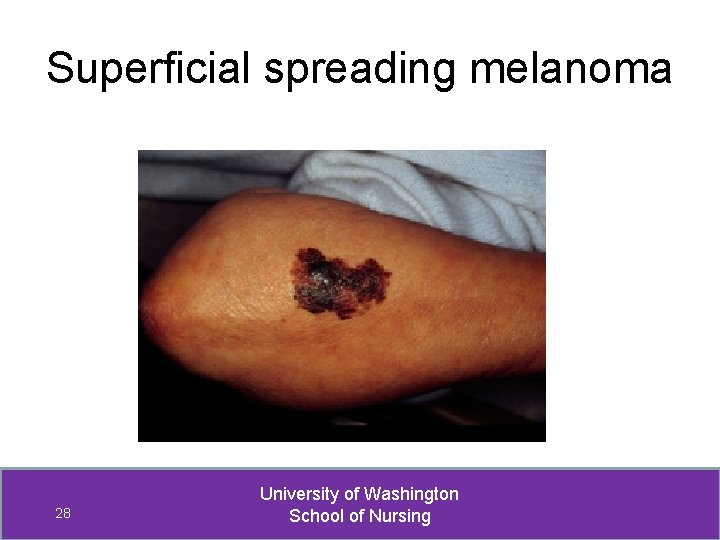
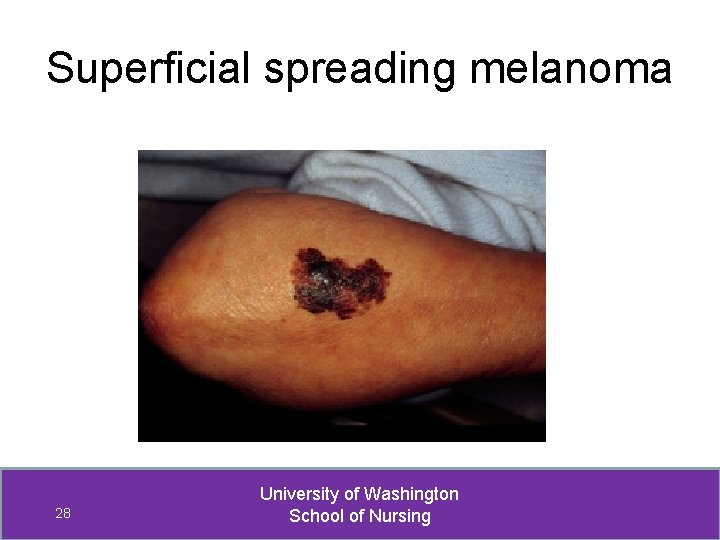
Superficial spreading melanoma 28 University of Washington School of Nursing
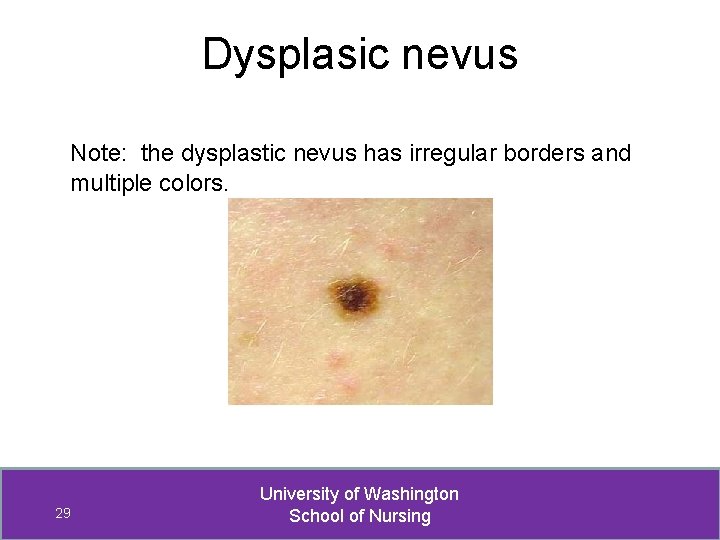
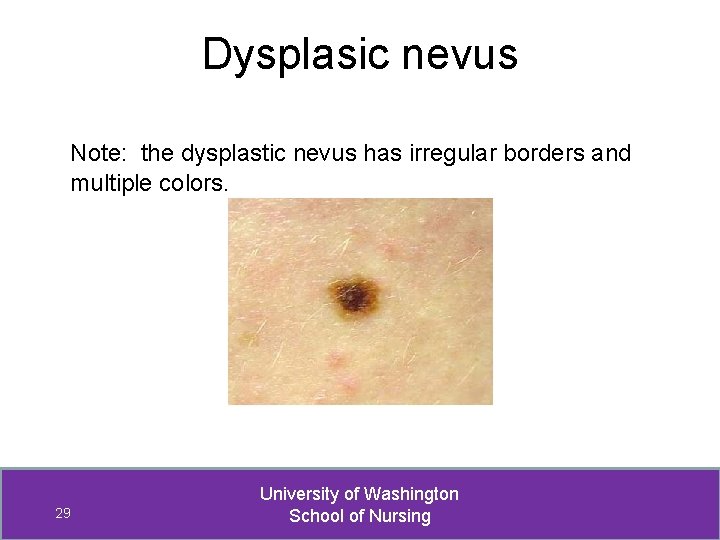
Dysplasic nevus Note: the dysplastic nevus has irregular borders and multiple colors. 29 University of Washington School of Nursing
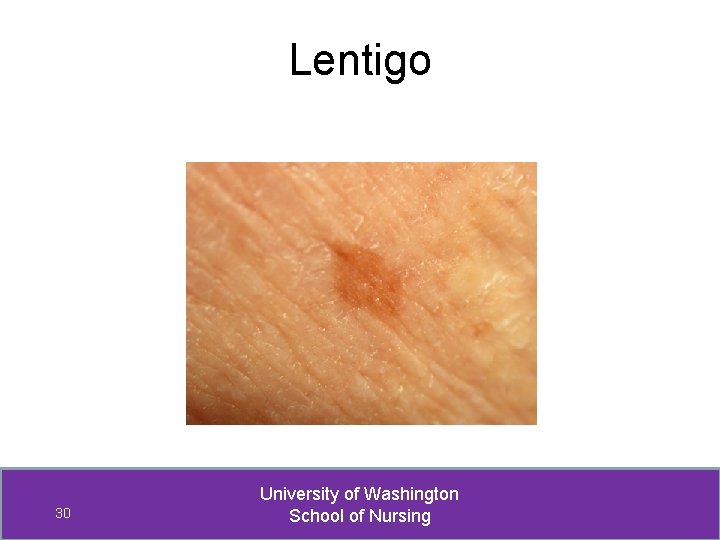
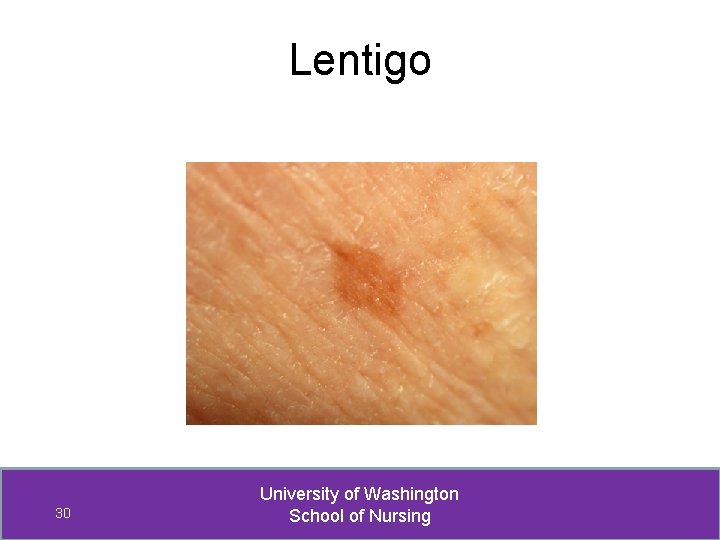
Lentigo 30 University of Washington School of Nursing
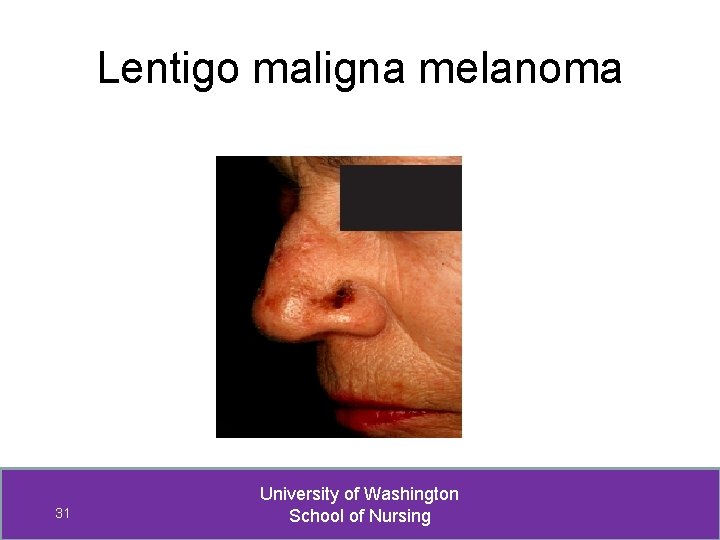
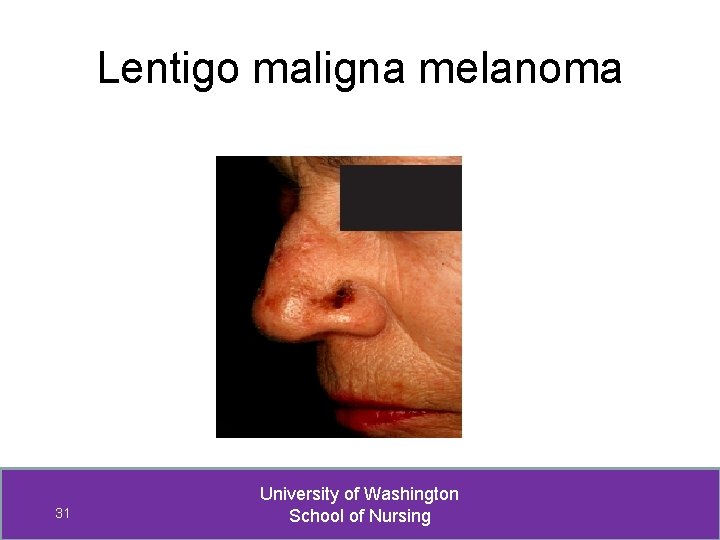
Lentigo maligna melanoma 31 University of Washington School of Nursing
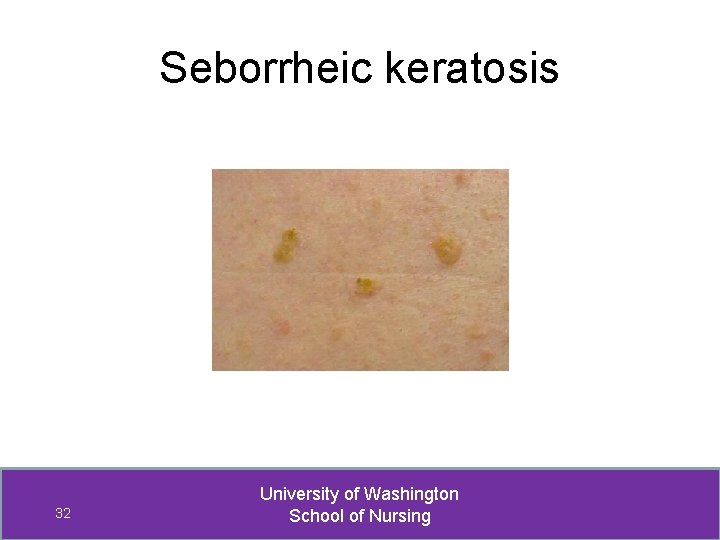
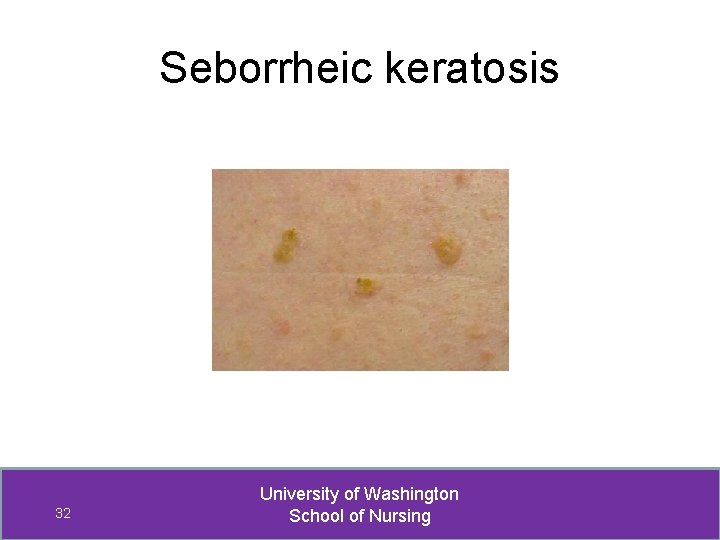
Seborrheic keratosis 32 University of Washington School of Nursing
Ulcerative lesions • • • Basal cell carcinoma Erosive lichen planus Genital herpes Primary syphilis Squamous cell carcinoma 33 University of Washington School of Nursing
Solid & Cystic Tumors Small lesions (usually < 1 cm in diameter) • Acrochordons (skin tags) • Epidermal cysts • Hidradenitis suppurativa 34 University of Washington School of Nursing
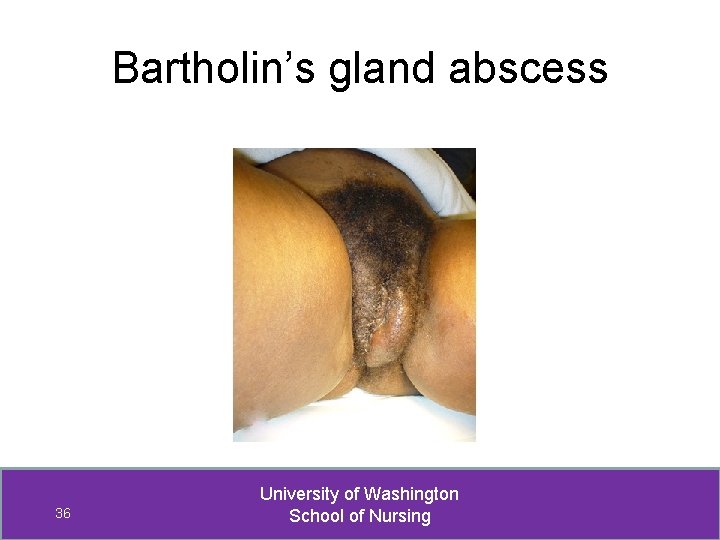
Solid & Cystic Tumors Large lesions • Bartholin’s Cyst • Bartholin’s Abscess • Verrucous carcinoma 35 University of Washington School of Nursing
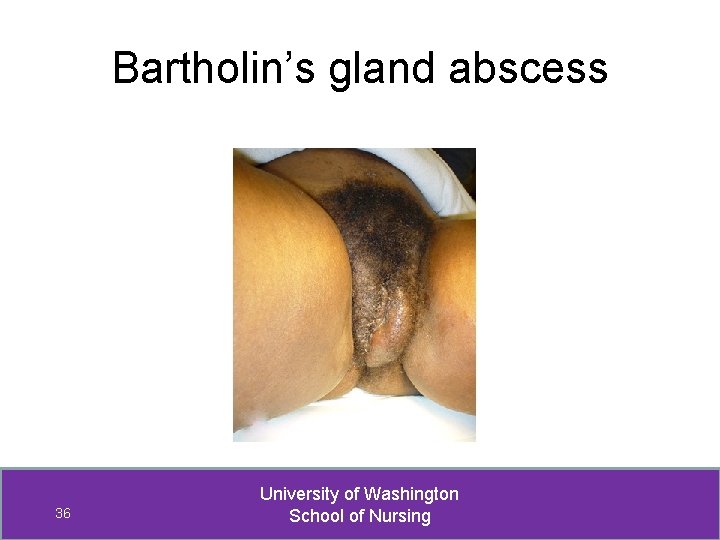
Bartholin’s gland abscess 36 University of Washington School of Nursing
Evaluation Consider both age and immune status Ø Higher risk of malignancy if postmenopause Ø Immune compromised - Increased risk of VIN & vulvar cancer - Exaggerated presentations of common infections 37 University of Washington School of Nursing
Evaluation: History 1. Onset - how long lesion has been present? 2. Character - initial appearance? current appearance? 3. Location - where on genitals? similar lesions elsewhere? 4. Timing - come and go? always there? 5. Course - staying the same? getting worse? 38 University of Washington School of Nursing
Evaluation: History 6. Self treatment and outcome - What’s been tried? ( herbal, OTC, Rx meds ) - Response to each thing tried? ( better, worse, no change ) 7. Aggravating & alleviating factors - What makes it worse? - What makes it better? 39 University of Washington School of Nursing
Evaluation: History 8. Associated symptoms focused on lesion • Itching? • • • Pain? Burning or Stinging? Feeling of rawness? Dampness? Bleeding? 40 University of Washington School of Nursing
If itching, ask… • How intense is the itching? • Does itching awaken you from sleep? • Amount of scratching in response to itching? 41 University of Washington School of Nursing
Evaluation: History Additional associated symptoms re: • • Vaginal infections STIs Cervical cancer Derm conditions Low estrogren state Vulvar hygiene - See Outline, page 13 Dyspareunia 42 University of Washington School of Nursing
Evaluation: History Related PMH • • Vulvar conditions Cervical dysplasia HPV status Cervical, uterine, or ovarian cancer Allergies; asthma; skin problems Lowered immune status HIV status 43 University of Washington School of Nursing
Evaluation: History • Previous occurrences • Related FH: Diabetes, skin problems • Patient profile -- Stress -- Tobacco use • Impact on ADLs / quality of life 44 University of Washington School of Nursing
Evaluation: PE Not all vulvar conditions are symptomatic Careful inspection of external genitalia If find an asymptomatic lesion, then SA 45 University of Washington School of Nursing
Evaluation: PE • Inspect skin non-genital areas, esp skin folds Inspect mucous membranes Lymphadenopathy – inguinal External genitalia and vulva Speculum exam, if indicated • • 46 University of Washington School of Nursing
PE: more detail Inspection of external genitalia and vulva Good light essential Spread hair/labia/folds to inspect all aspects 47 University of Washington School of Nursing
PE: Lesion characteristics • Type of lesion • Size & shape of individual lesions • Solitary –or-- multiple & pattern • Color • Texture & if tender • Secondary changes– crusts, etc. 48 University of Washington School of Nursing
Diagnostic procedures 1. Macroscopic - Magnifying lens - Colposcopy 2. Microscopic - wet prep - vulvar cytology 3. Biopsy 49 University of Washington School of Nursing
Biopsy if suspicious for malignancy • • asymmetry irregular border variable color bleeds rapidly changing does not heal slight ulceration in raised lesion 50 University of Washington School of Nursing
Also biopsy if… • Diagnosis is not clear • Lesion does not resolve w/ therapy • Patient concerned & wants biopsy 51 University of Washington School of Nursing
Biopsies: Types • Shave • Punch • Excisional • Incisional 52 University of Washington School of Nursing
Management: General • • • Good vulvar hygiene Soaks Corticosteroids Estrogen (topical) Pt education Follow-up 53 University of Washington School of Nursing
Now for specific conditions… 54 University of Washington School of Nursing
VIN • Vulva, vagina, cervix, and anus share same embryonic origin • Oncogenic stimulus (e. g. HPV) neoplasia • Neoplasia influenced by host reaction • VIN, usual type and differentiated have malignant potential 55 University of Washington School of Nursing
VIN: Risk Factors • intraepithelial neoplasia in other lower genital tract sites HPV infection immunocompromised smoking chronic vulvar irritation lighter skin pigmentation • • • 56 University of Washington School of Nursing
Old VIN I – Now Condyloma/HPV Effect • • Well localized and delineated Flat or slightly elevated White and rough Less common red-brown 57 University of Washington School of Nursing
VIN, usual type (warty, basaloid, and mixed) • Most common type of VIN (90 -95%) • Precursor lesion to HPV-associated invasive squamous cell carcinoma (SCC) • HPV associated (HPV types 16, 18, 31) • Presents in younger, premenopausal women 58 University of Washington School of Nursing
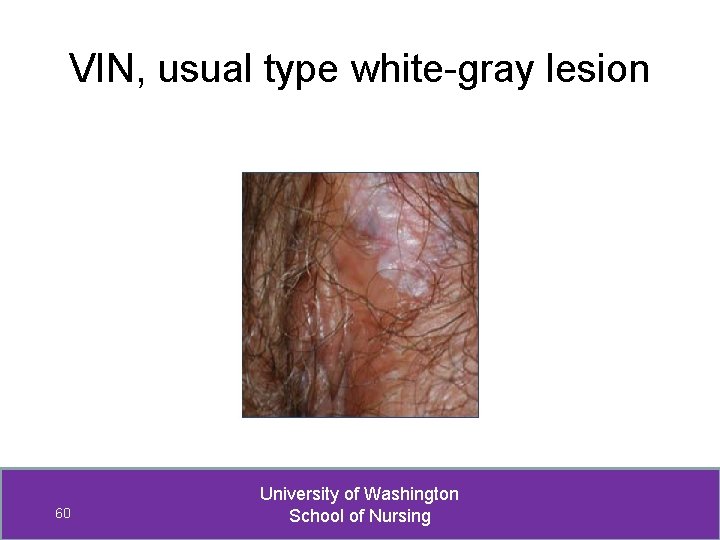
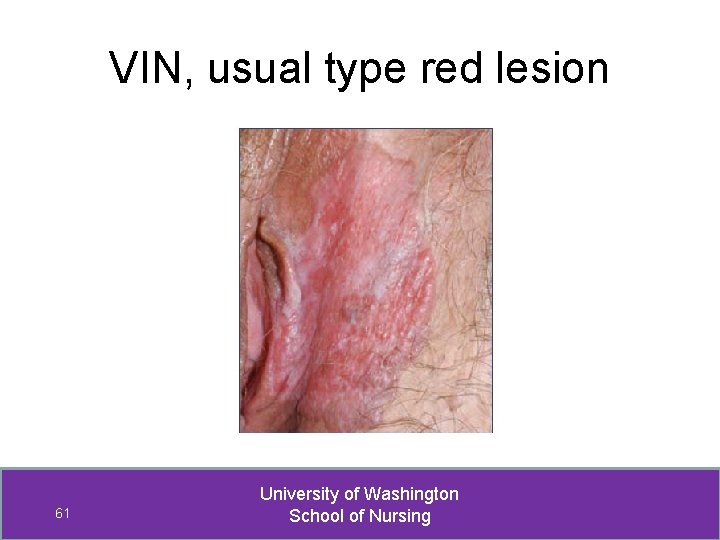
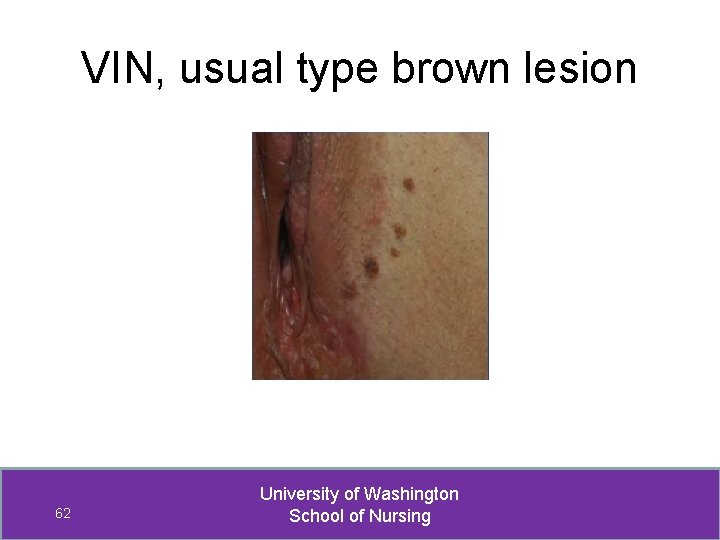
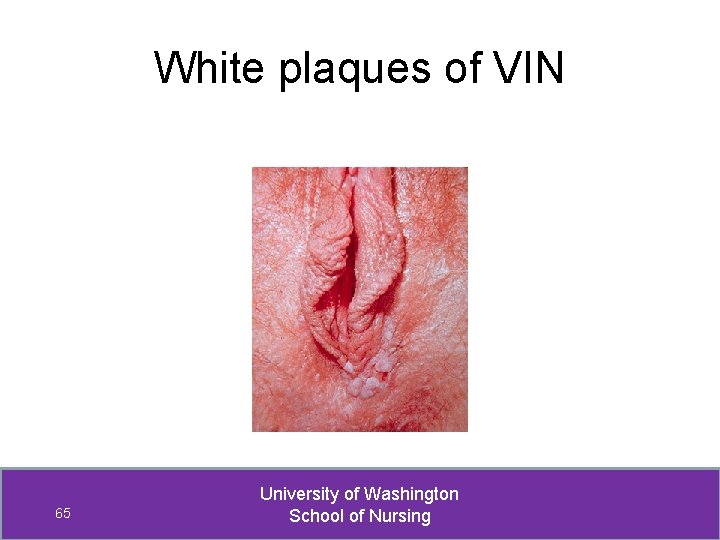
PE findings: VIN, usual type • Multifocal lesions • Well localized and delineated • Lesions most often in interlabial grooves, posterior fourchette, & perineum • Slightly elevated, white-gray, rough • Less common – red-brown color or redwhite patches 59 University of Washington School of Nursing
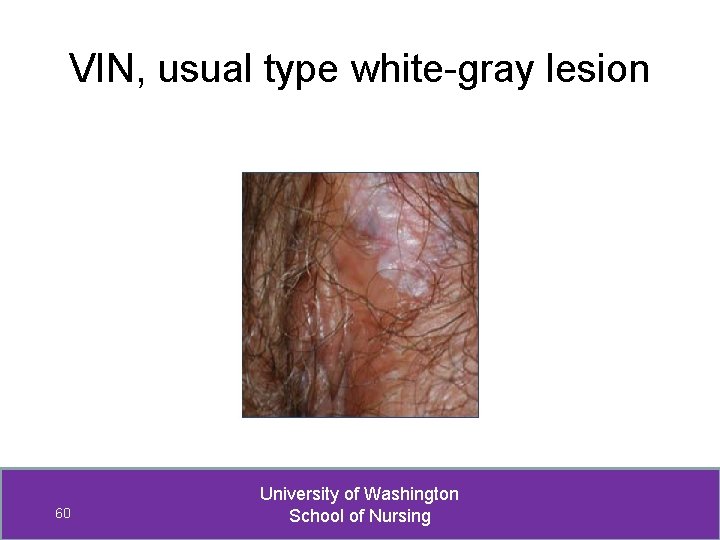
VIN, usual type white-gray lesion 60 University of Washington School of Nursing
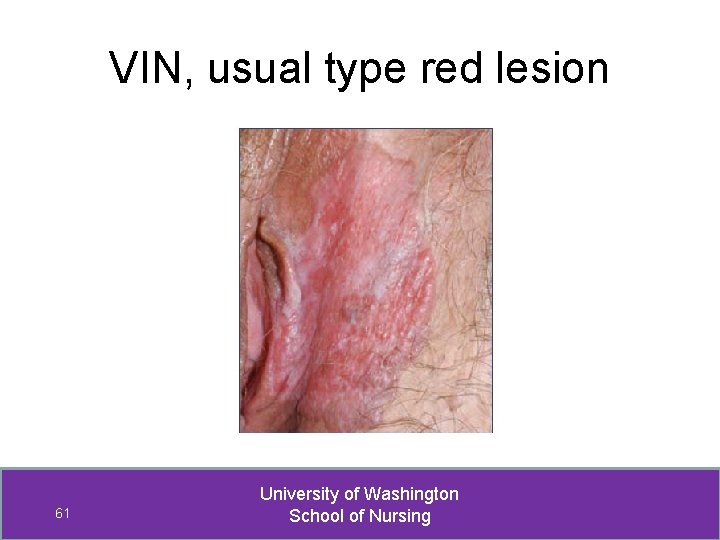
VIN, usual type red lesion 61 University of Washington School of Nursing
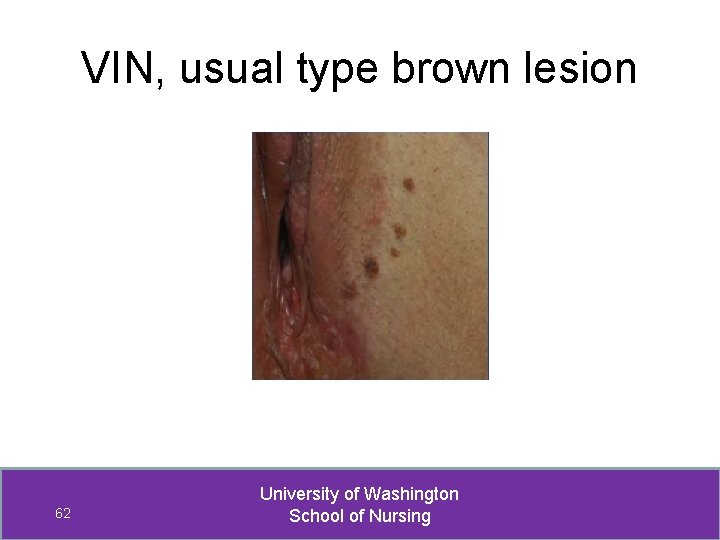
VIN, usual type brown lesion 62 University of Washington School of Nursing
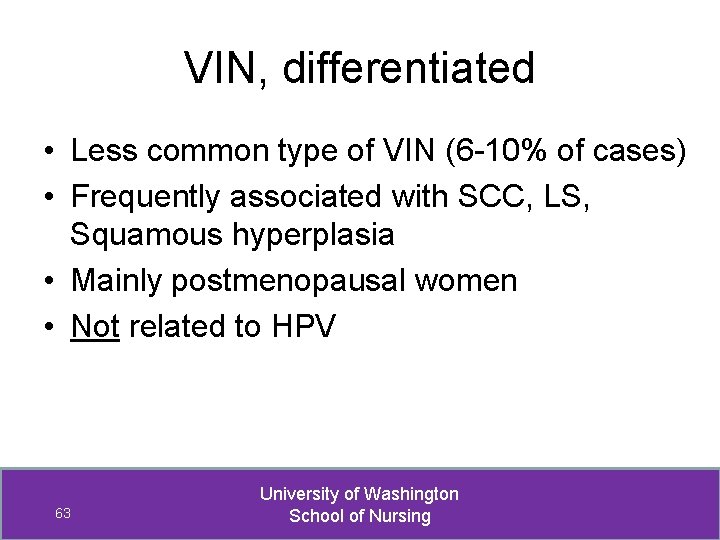
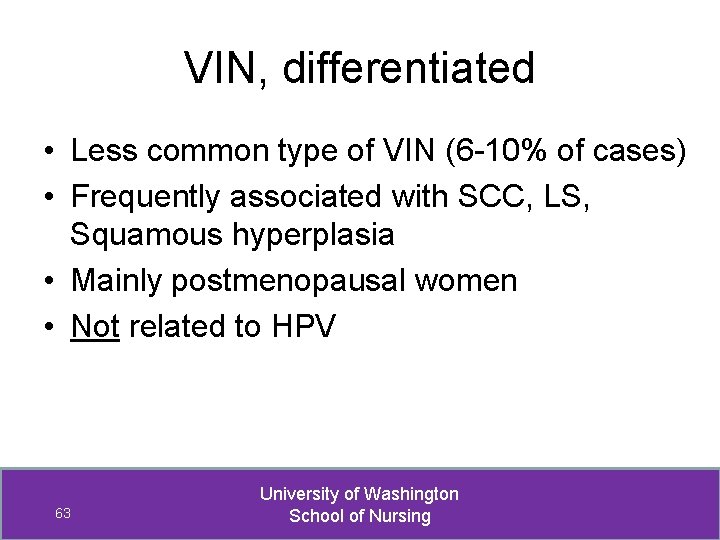
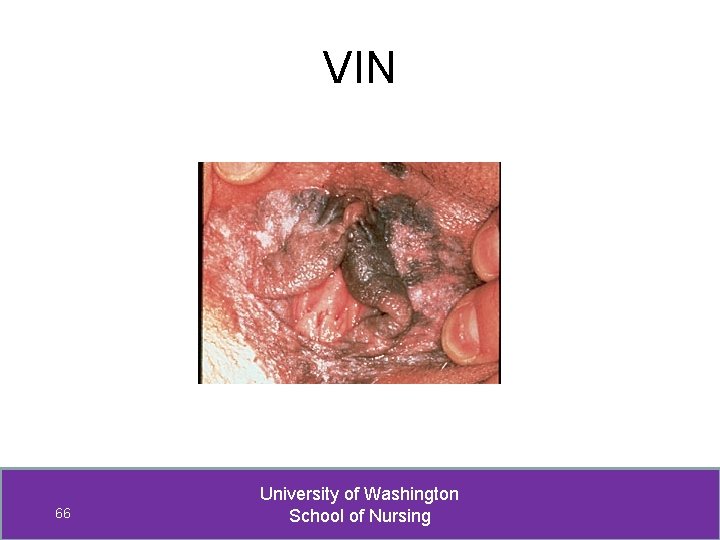
VIN, differentiated • Less common type of VIN (6 -10% of cases) • Frequently associated with SCC, LS, Squamous hyperplasia • Mainly postmenopausal women • Not related to HPV 63 University of Washington School of Nursing
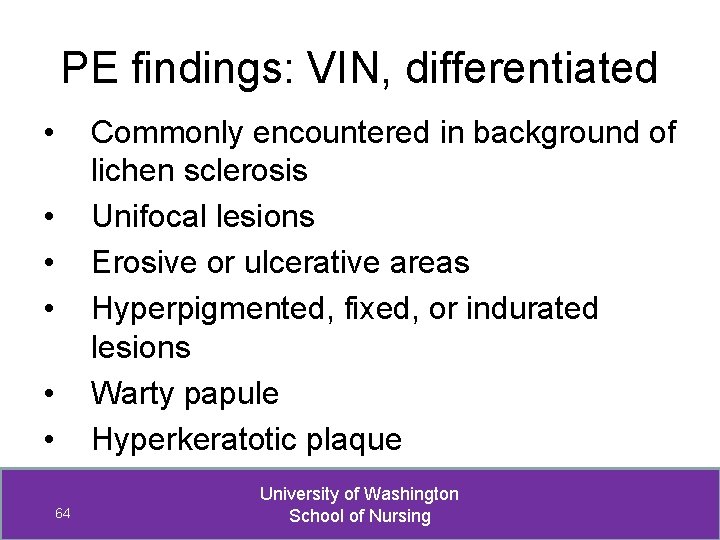
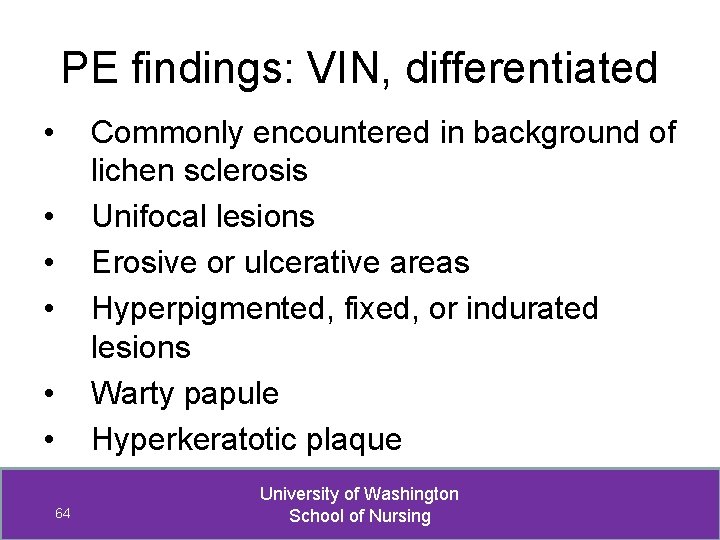
PE findings: VIN, differentiated • Commonly encountered in background of lichen sclerosis Unifocal lesions Erosive or ulcerative areas Hyperpigmented, fixed, or indurated lesions Warty papule Hyperkeratotic plaque • • • 64 University of Washington School of Nursing
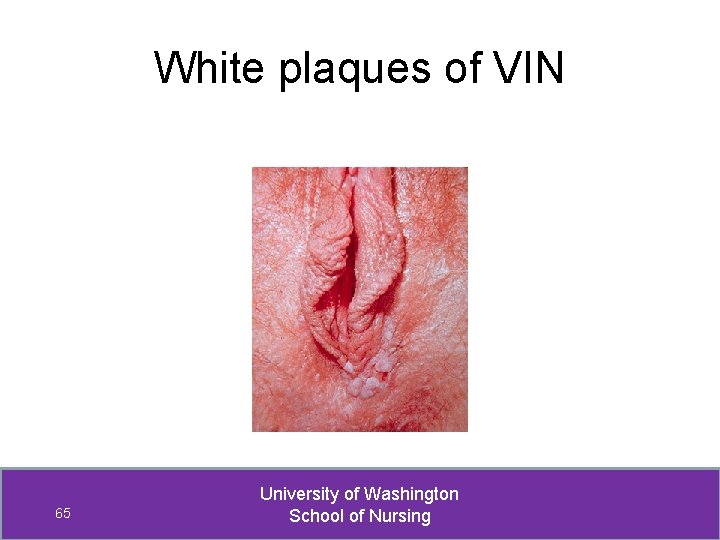
White plaques of VIN 65 University of Washington School of Nursing
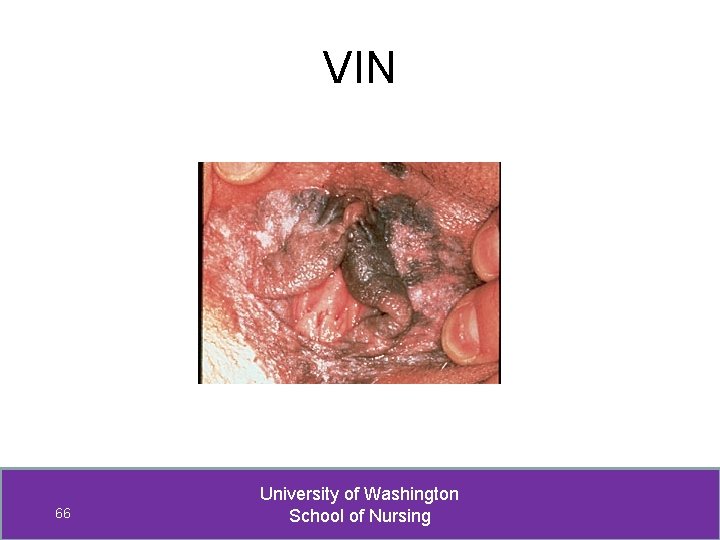
VIN 66 University of Washington School of Nursing
VIN: Diagnosis • Early dx depends on regular vulvar exams • High index of suspicion • If suspect, biopsy (via colposcopy best) • Refer confirmed VIN to MD 67 University of Washington School of Nursing
VIN: Treatment • Wide local excision • Laser vaporization • Skinning vulvectomy (w/ or w/out graft) • Immunomodulators *Agents that enhance or induce a strong cell -mediated immune response likely hold the greatest promise not only for control of HPV-related disease, but also for reduction of future recurrences 68 University of Washington School of Nursing
Vulvar Cancer • 4 th most common gyn cancer • Bimodal age distribution – represents two distinct etiologies – Young women – related to HPV (60% of vulvar CAs) – Older women – not related to HPV (chronic inflammatory or auto-immune process) • Most ( > 90%) are squamous cell CAs • Risk factors same as VIN risk factors, plus if PMH of VIN • Many women are asymptomatic 69 University of Washington School of Nursing
Vulvar Cancer: Symptoms • Most common Pruritus • Less common, when more advanced -- vulvar bleeding or discharge -- dysuria -- enlarged lymph node in groin 70 University of Washington School of Nursing
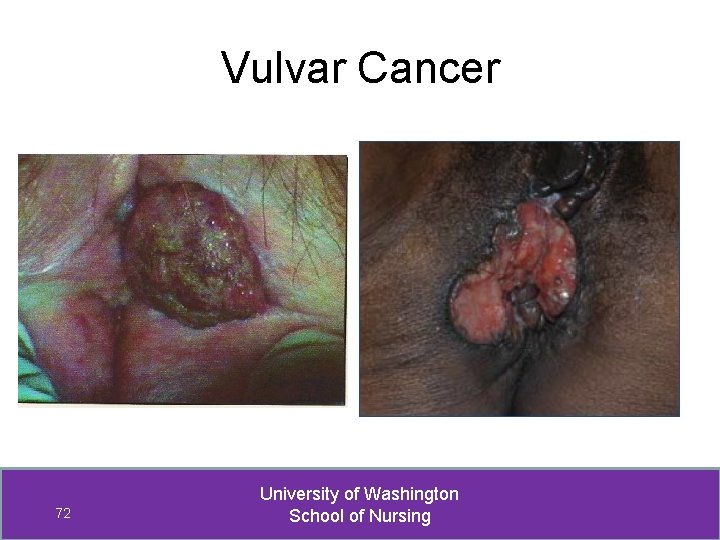
Vulvar Cancer: PE Findings Most often unifocal vulvar plaque, ulcer, or mass (fleshy, nodule, or warty) on labia majora 71 University of Washington School of Nursing
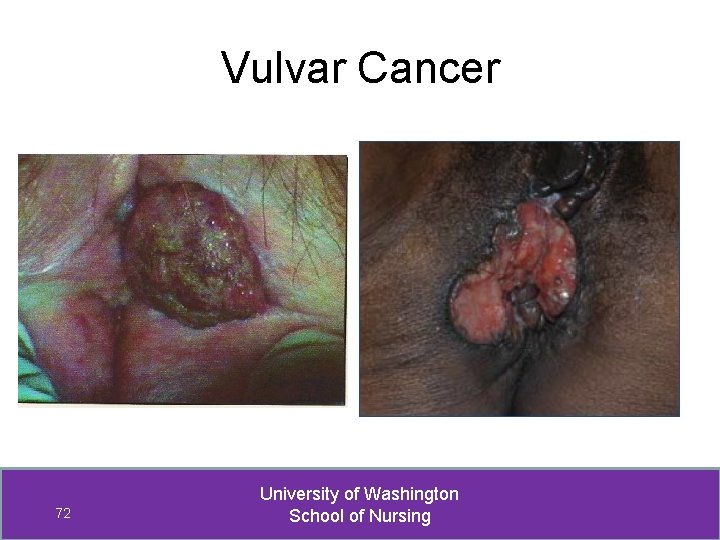
Vulvar Cancer 72 University of Washington School of Nursing
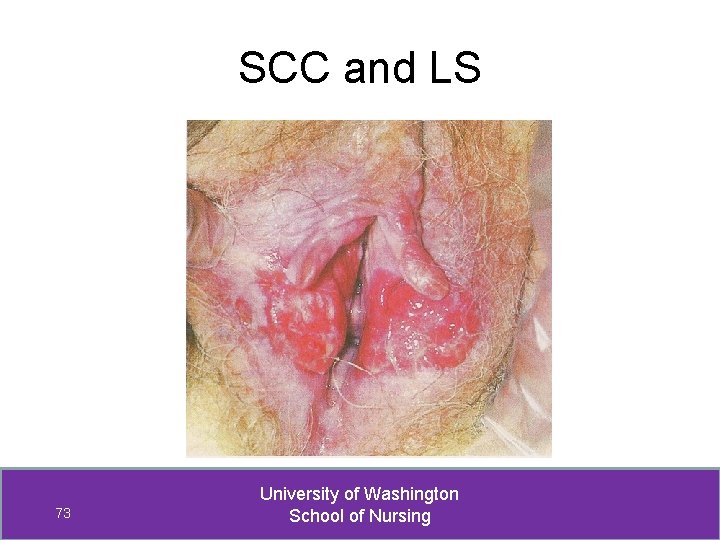
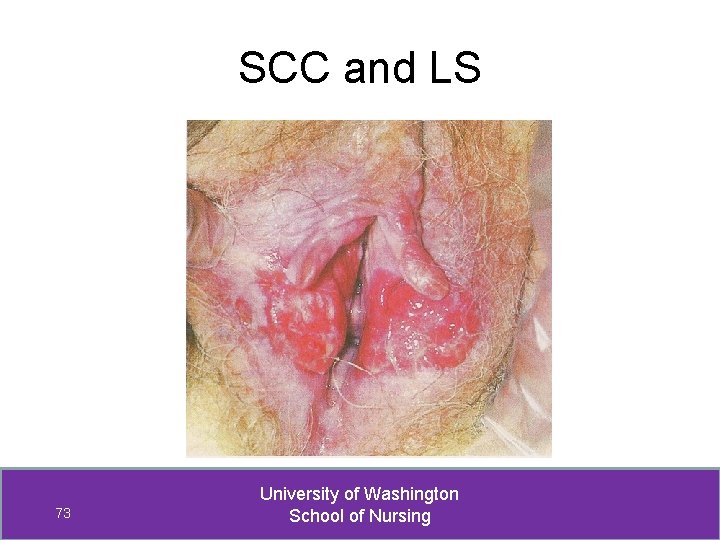
SCC and LS 73 University of Washington School of Nursing
Vulvar Cancer: Diagnosis • Histological evaluation essential - diagnosis - depth of involvement biopsy center of lesion • If suspect or diagnose vulvar cancer, must refer to an MD 74 University of Washington School of Nursing
Lichen Sclerosus • Chronic, progressive, inflammatory skin condition found most often in the anogenital region. • Does not occur in the vagina • Accounts for ~70% of non-neoplastic vulvar lesions • Occurs most in post-menopausal women, although not exclusively 75 University of Washington School of Nursing
Lichen Sclerosus: Symptoms PRURITIS is HALLMARK of LS Intensity may awaken Other symptoms: • Rectal itching, fissures, bleeding, painful defecation • Dyspareunia • Decreased sexual sensation, anorgasmia • Dysuria, difficulty voiding *May be asymptomatic – 1/3 of patients 76 University of Washington School of Nursing
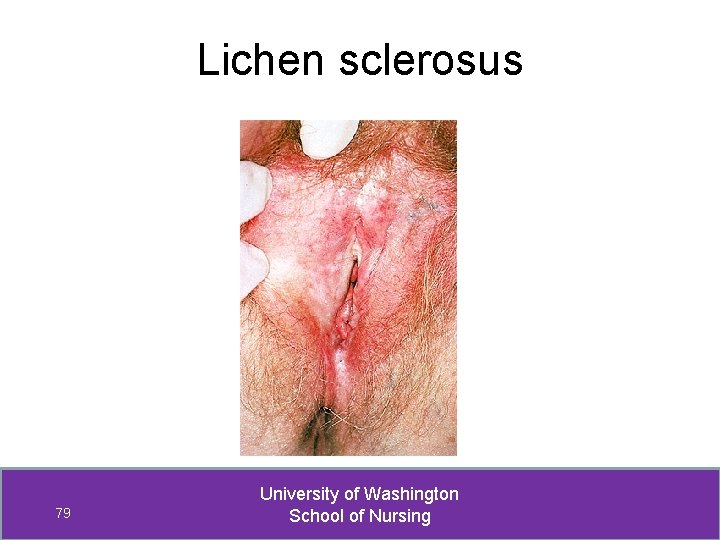
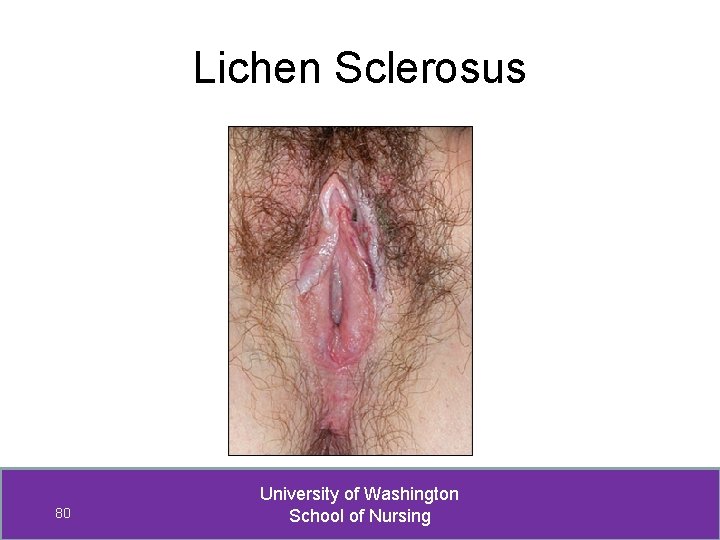
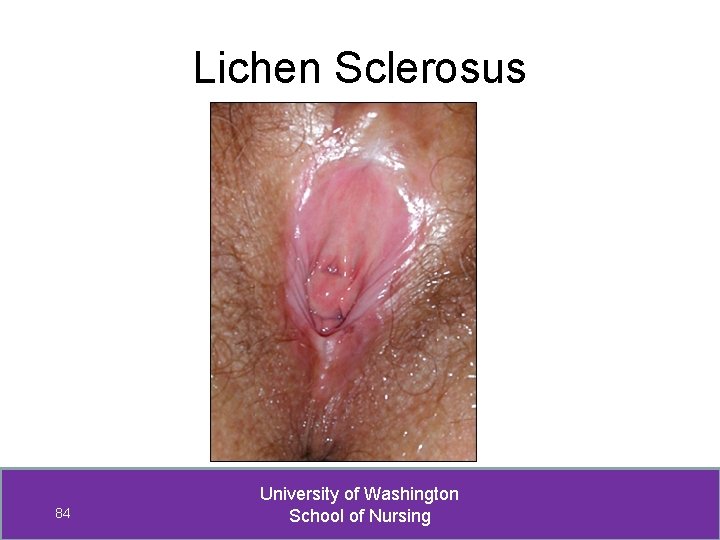
LS: PE findings • Classic LS = thin, white, wrinkled skin on labia minora and/or labia majora. “Parchment-like” • “Keyhole” pattern • Fissures in labial folds, around clitoris or anus • Excoriations and lichenification r/t scratching • Telangiectasia / hematoma / ecchymoses • Changes in vulvar architecture 77 University of Washington School of Nursing
LS: Changes in vulvar architecture • None early in course of LS • Labia majora/minora become less distinct. - Adhesion of labia minora to majora • Clitoris covered under fused prepuce. - Edema or agglutination of prepuce and frenulum “bury clitoris” • Stenosis or constriction of introitus 78 University of Washington School of Nursing
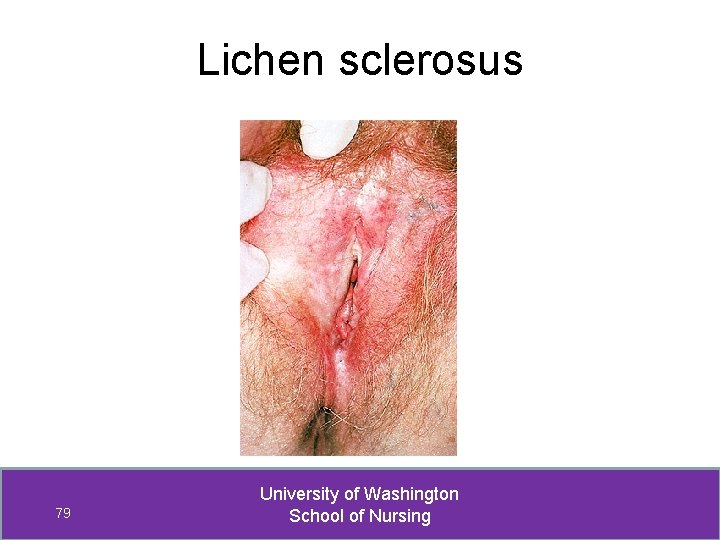
Lichen sclerosus 79 University of Washington School of Nursing
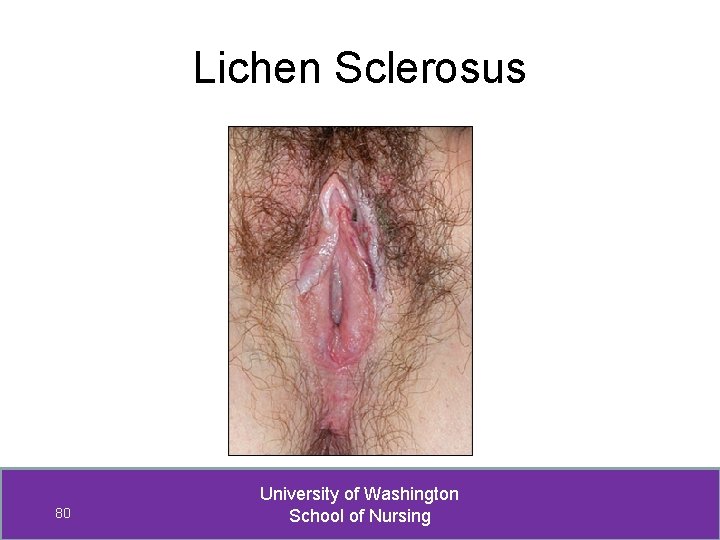
Lichen Sclerosus 80 University of Washington School of Nursing
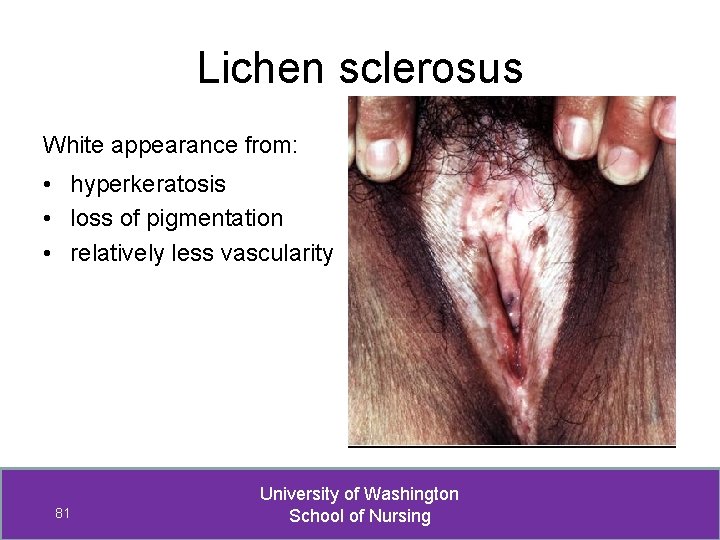
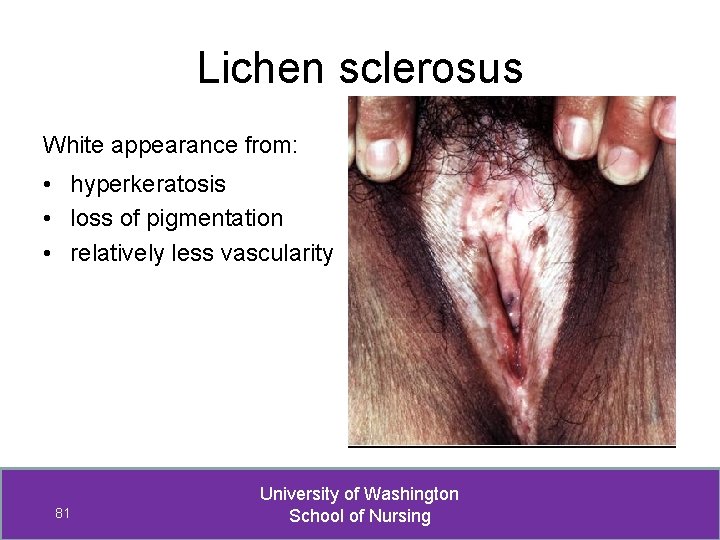
Lichen sclerosus White appearance from: • hyperkeratosis • loss of pigmentation • relatively less vascularity 81 University of Washington School of Nursing
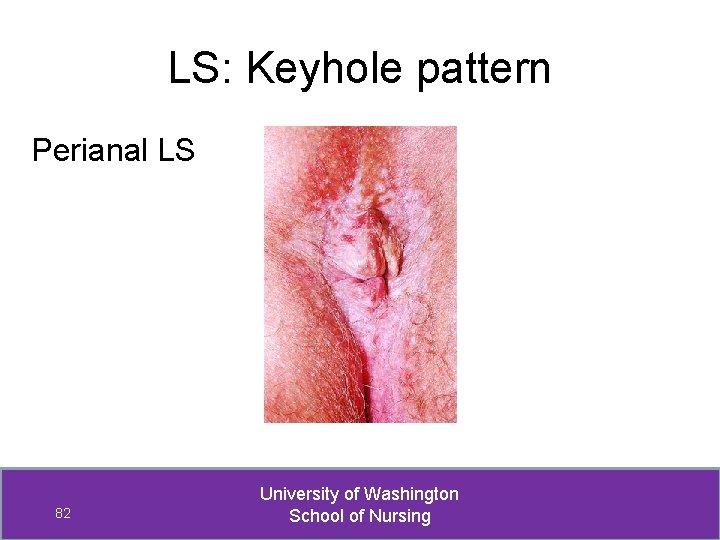
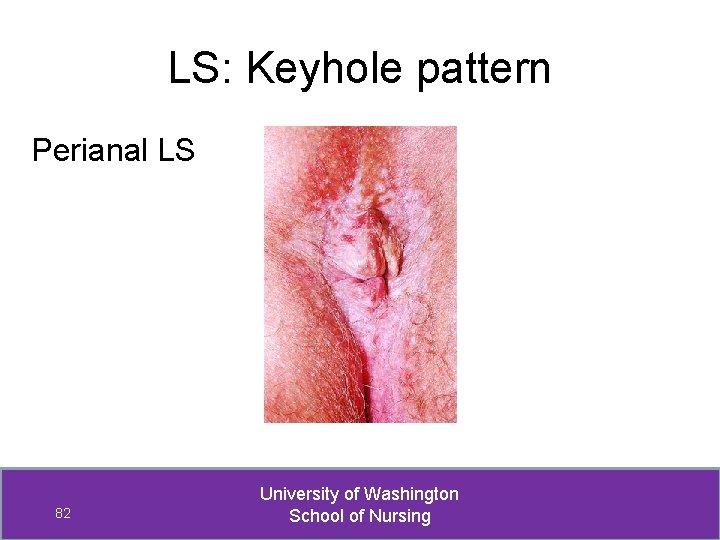
LS: Keyhole pattern Perianal LS 82 University of Washington School of Nursing
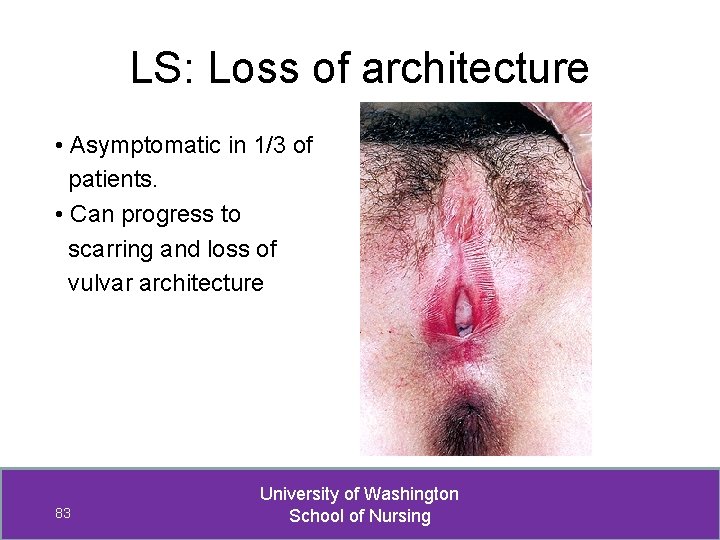
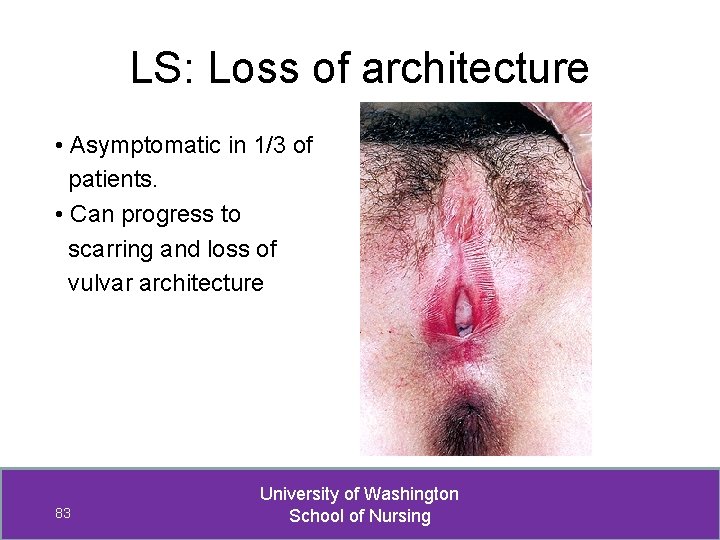
LS: Loss of architecture • Asymptomatic in 1/3 of patients. • Can progress to scarring and loss of vulvar architecture 83 University of Washington School of Nursing
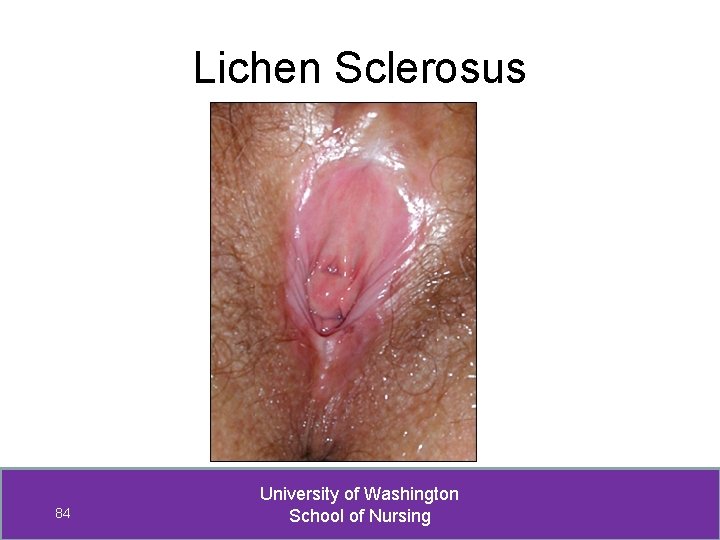
Lichen Sclerosus 84 University of Washington School of Nursing
When suspect LS, differential includes: • Lichen planus • Squamous cell hyperplasia (usually lichen simplex chronicus) • Vitiligo • Psoriasis • Candidiasis 85 University of Washington School of Nursing
When suspect LS… MUST rule out VIN and vulvar cancer before initiating treatment. Women w/ vulvar LS have increased risk for invasive squamous cell cancer. 86 University of Washington School of Nursing
LS: Biopsy • Biopsy to confirm diagnosis 3 -4 mm punch Specimen from advancing margin • Biopsy to identify VIN or vulvar CA Biopsy center to ensure sample most severe pathology 87 University of Washington School of Nursing
LS: Management • Initiate treatment asap, even if asymptomatic • Wet dressings or soaks x 20 -30 min w/ Burrow’s sln • Corticosteroids relief of pruritus and resolution of hyperkeratosis, fissures, and ecchymoses. -- Will not reverse atrophy, whiteness or scarring. Rx: Clobetasol or halobetasol propionate 0. 05% ointment BID x 4 weeks, then qhs x 4 weeks, then 1 -3 x per week for maintenance. Directions: Spread sparingly to cover affected area with thin film 88 University of Washington School of Nursing
LS: Management Evaluate for possible associated problems • Autoimmune disorders, e. g. , alopecia areata, vitiligo, thyroid disease, and pernicious anemia (21% - most commonly thyroid disorder) • Premature menopause • Infection 89 University of Washington School of Nursing
LS Management: Patient Education • • • Chronic, progressive condition; ? cause Symptom relief and treatment options Lesions do not always disappear w/ tx Do NOT stop treatment when itching stops! Continued topical therapy can slow progression Encourage sufficient sleep, diet, and exercise Encourage stress reduction techniques Support group available, if interested Regular self and clinician evaluation essential 90 University of Washington School of Nursing
LS Management: Follow-up • On-going evaluation is essential -- Visits every 1 -3 months until stable -- Every 6 months while stable • Biopsy progressive, recurrent, persistent, or suspicious lesions – risk of SCC. • Refer to MD, if not responsive to therapy 91 University of Washington School of Nursing
Lichen Planus • An inflammatory autoimmune skin disorder which may affect only the vagina, vulva or may occur elsewhere on skin; also nails and mucous membranes • Vulvar LP is uncommon • Peak incidence, women 30 -60 yrs old 92 University of Washington School of Nursing
Lichen Planus: Symptoms • Irritating vaginal discharge and/or vulvar soreness, thought to be yeast infection • Intense pruritus • Burning • Dyspareunia • Post-coital bleeding 93 University of Washington School of Nursing
Lichen Planus: 3 types 1. Papulosquamous LP: • small, violaceous, intensely pruritic papules on keratinzed skin. • Papules are poorly demarcated, pink, and opaque. • Associated w/ “milky striae” on inner aspects of the labia. 94 University of Washington School of Nursing
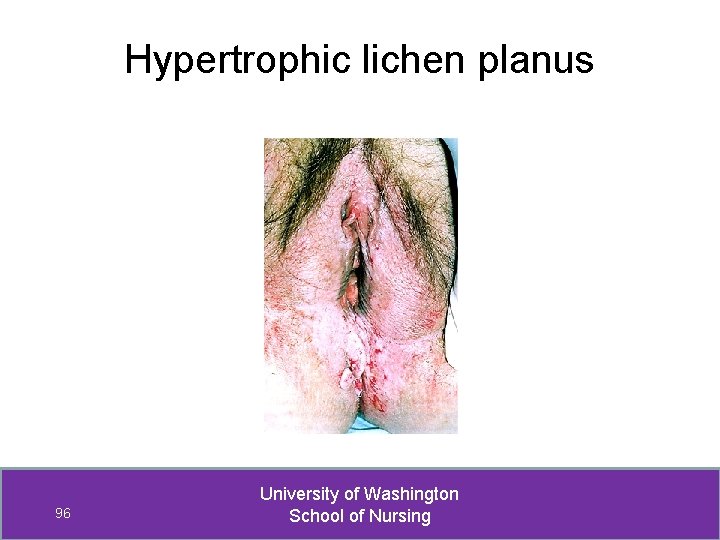
Lichen Planus: 3 types 2. Hypertrophic LP: • hyperkeratotic, rough lesions on perineum and perianal area. • May appear similar to squamous cell CA. 95 University of Washington School of Nursing
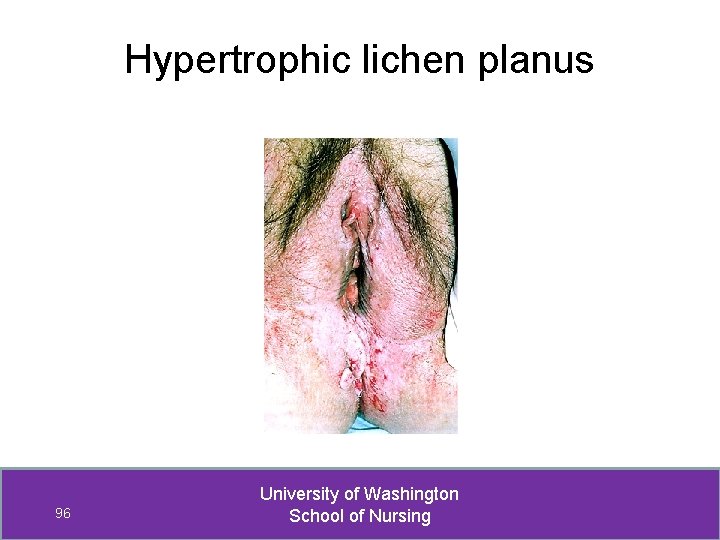
Hypertrophic lichen planus 96 University of Washington School of Nursing
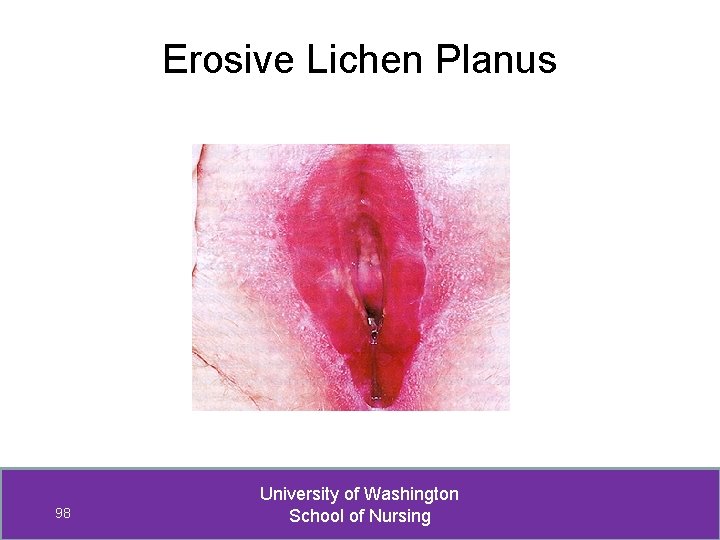
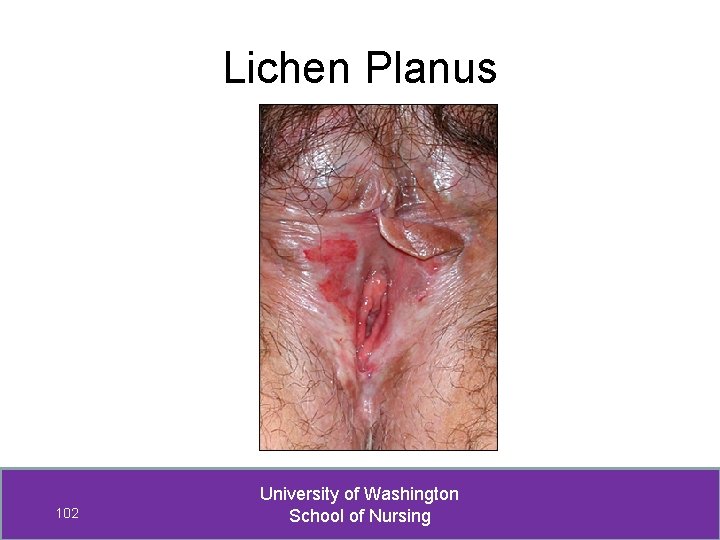
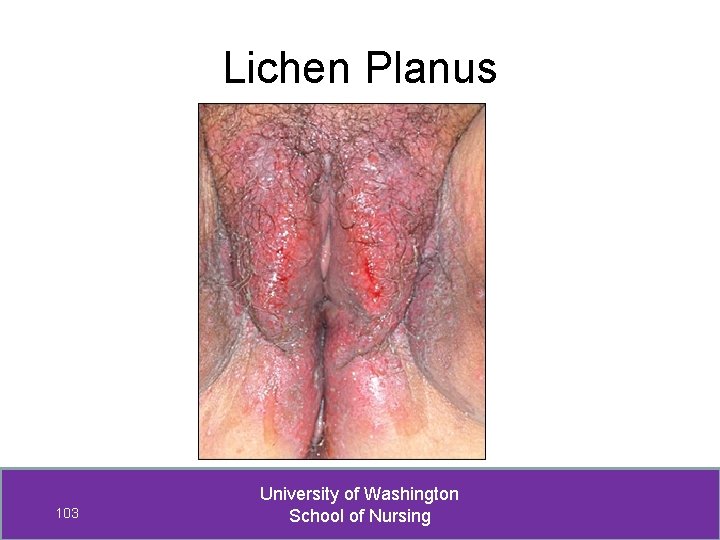
Lichen Planus: 3 types 3. Erosive LP: • Most common variant of LP • Involves vagina 70% of the time • Violaceous erosions that look like glassy, reticulated, white papules and plaques. • White striae along lesion margins. • Progression leads to extensive erosion and ulceration and destruction of vulvar architecture. 97 University of Washington School of Nursing
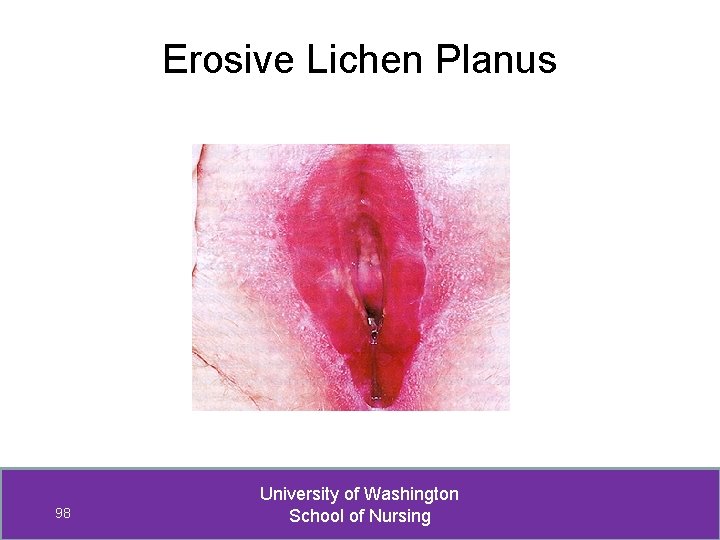
Erosive Lichen Planus 98 University of Washington School of Nursing
Erosive Lichen Planus 99 University of Washington School of Nursing
Lichen Planus 100 University of Washington School of Nursing
Lichen Planus 101 University of Washington School of Nursing
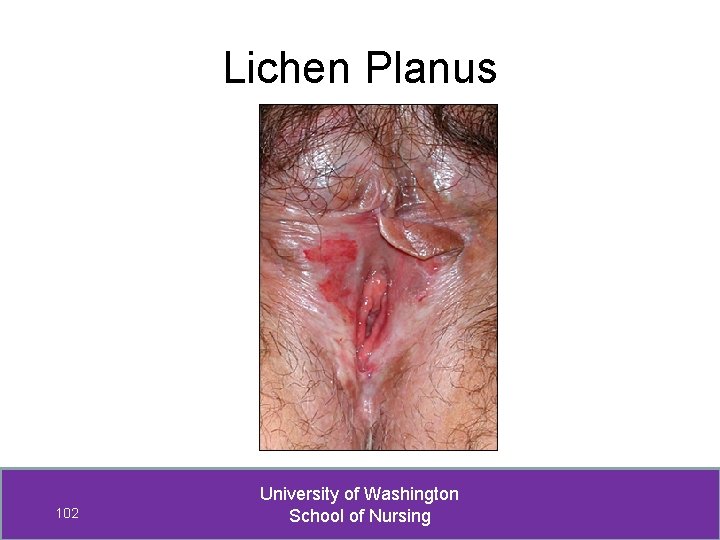
Lichen Planus 102 University of Washington School of Nursing
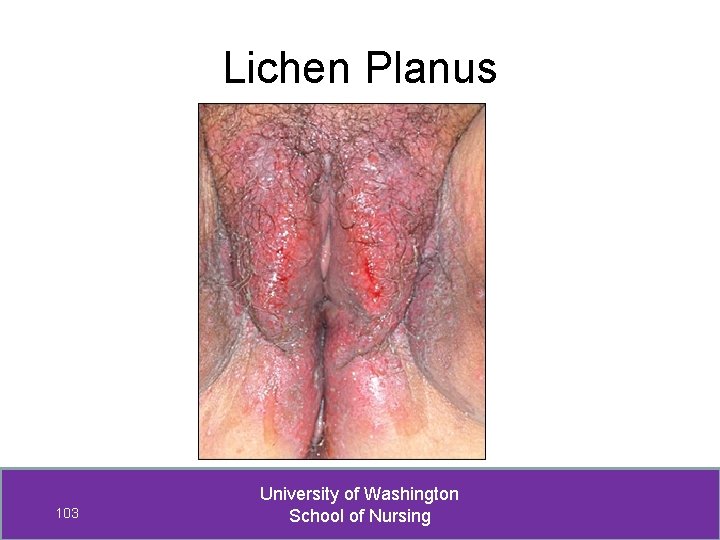
Lichen Planus 103 University of Washington School of Nursing
Lichen Planus Hard to diagnosis! Difficult to treat! If suspect lichen planus refer to MD 104 University of Washington School of Nursing
Squamous cell hyperplasia • Most squamous cell hyperplasia is lichen simplex chronicus • Occurs in all ages • Thickened skin (lichenification) is result of scratching or rubbing Squamous cell hyperplasia may coexist with LS 105 University of Washington School of Nursing
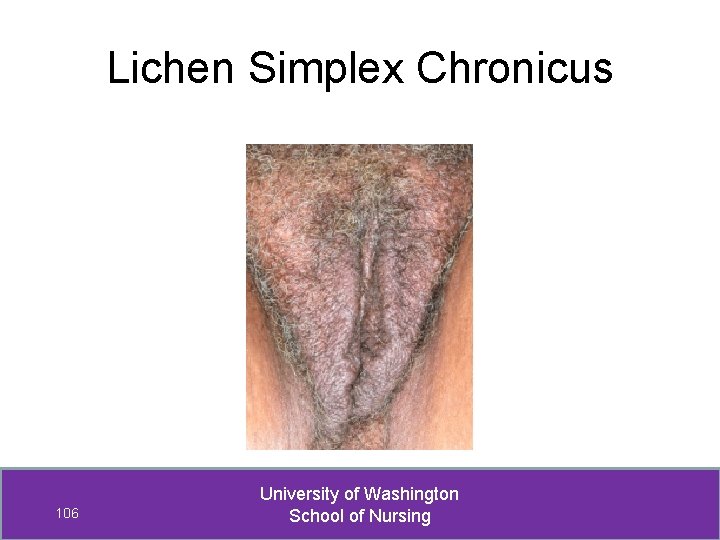
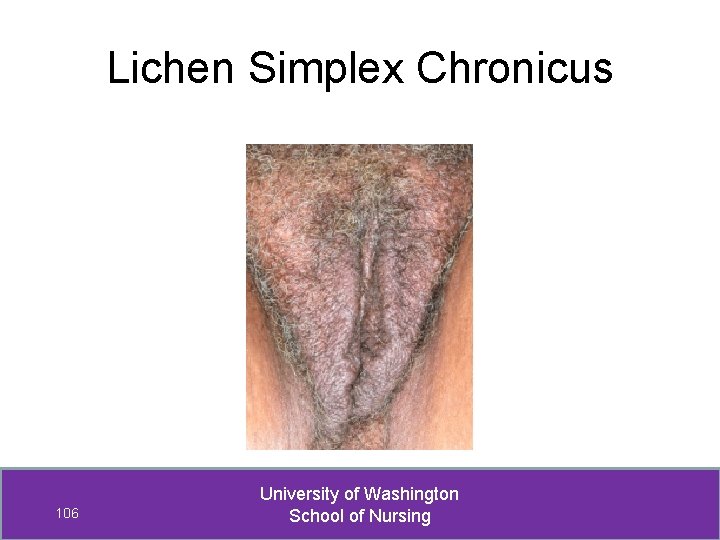
Lichen Simplex Chronicus 106 University of Washington School of Nursing
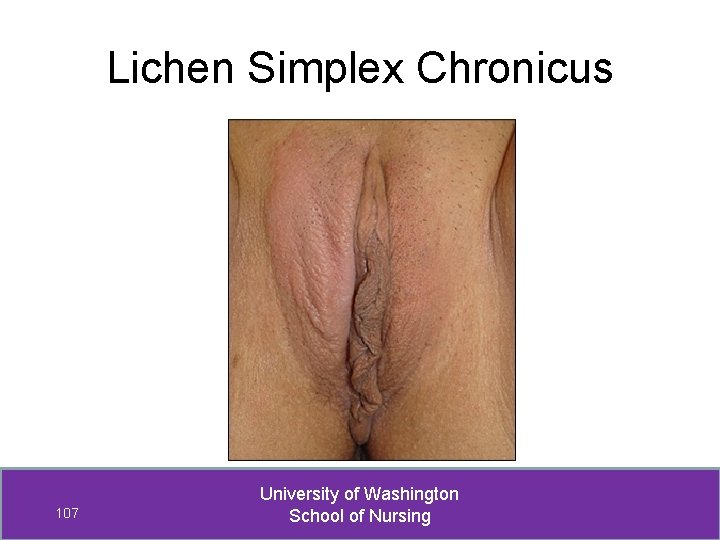
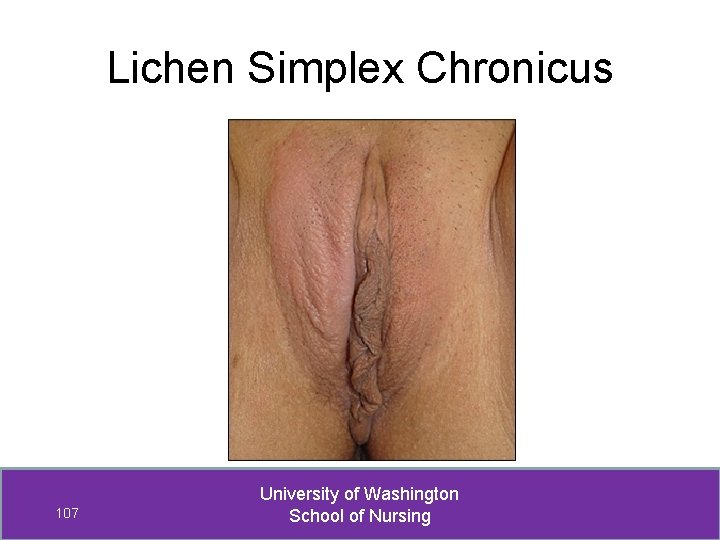
Lichen Simplex Chronicus 107 University of Washington School of Nursing
Squamous cell hyperplasia Diagnosis of exclusion. Need to rule out— • Lichen sclerosis • Psoriasis • Lichen planus • Eczema • HPV • Candidiasis 108 University of Washington School of Nursing
Squamous cell hyperplasia Consider possibility of malignancy (VIN, vulvar CA) before starting treatment. • Goal of treatment is to— break “itch-scratch” cycle 109 University of Washington School of Nursing
Squamous cell hyperplasia: Treatment Mild symptoms – use low to medium potency corticosteroid ointments Hydrocortisone 1 –or- 2. 5 % Triamcinolone 0. 1 % Rx: Apply twice daily for 2 -4 weeks, then x 2 /week. Continue therapy at min frequency to control pruritus. More than mild symptoms – use high potency corticosteroid ointment -- Clobetasol propionate 0. 05% ointmt each night x 30 days, then re-evaluate [usually 2 -3 months, then taper] 110 University of Washington School of Nursing
Squamous cell hyperplasia: Treatment If night time itching scratching, Rx sedating antihistamine (e. g. , hydroxizine) in pediatric dosage ( 10 mg at hs) 111 University of Washington School of Nursing
Consulting & Referring Vulvar biopsy • Consult if uncertain if vulvar biopsy indicated • Refer if not skilled in vulvar biopsy techniques VIN • Consult if suspect VIN • Refer if VIN diagnosed 112 University of Washington School of Nursing
Consulting & Referring Management • Whenever unfamiliar with indicated meds Consult with NP/PA specialists in derm, pharmacist, or MD to ensure appropriate med, dose, route, and timing. • Refer if lesion persists despite treatment • Refer whenever surgery or laser treatment is indicated (e. g. , for VIN) 113 University of Washington School of Nursing
 Shelley miksis
Shelley miksis Papilosis vulvar
Papilosis vulvar Leucorrea profusa
Leucorrea profusa Vulvar dermatozlar
Vulvar dermatozlar Vulvar intraepitelyal neoplazi
Vulvar intraepitelyal neoplazi Vulvar dystrophy thyroid
Vulvar dystrophy thyroid Cin
Cin Que es el sicodis
Que es el sicodis Chamberlain fnp reviews
Chamberlain fnp reviews Uca dnp program
Uca dnp program Ciclo de vida de un proyecto de inversión
Ciclo de vida de un proyecto de inversión Shelley knuth
Shelley knuth Summary of the poem ozymandias
Summary of the poem ozymandias Riassunto frankenstein mary shelley
Riassunto frankenstein mary shelley Ozymandias lesson plan
Ozymandias lesson plan Laura shelley
Laura shelley Frankenstein chapter 3
Frankenstein chapter 3 Biography of percy bysshe shelley
Biography of percy bysshe shelley Mary shelley born
Mary shelley born Shelley duffy
Shelley duffy Frankenstein letters summary
Frankenstein letters summary Shelley curran
Shelley curran Frankenstein plot
Frankenstein plot Shelley heaton
Shelley heaton Shelley stangler
Shelley stangler Byron shelley and keats mastery test
Byron shelley and keats mastery test Mary shelley frankenstein biography
Mary shelley frankenstein biography Shelley chesney
Shelley chesney Shelley monk
Shelley monk Ode to skylark
Ode to skylark Robert walton frankenstein
Robert walton frankenstein Harriet westbrook
Harriet westbrook William blake
William blake John n evenson
John n evenson Shelley bs
Shelley bs Shelley moore strength based student profile
Shelley moore strength based student profile Ten soldiers poem
Ten soldiers poem In mary ainsworth's strange situation experiment
In mary ainsworth's strange situation experiment Mary shelley marido
Mary shelley marido Frankenstein literary elements
Frankenstein literary elements Irony in frankenstein
Irony in frankenstein Percy bysshe shelley childhood
Percy bysshe shelley childhood Shelley aggarwal
Shelley aggarwal Mary shelley
Mary shelley Frankenstein chapter 3 and 4
Frankenstein chapter 3 and 4 Keats byron shelley
Keats byron shelley Shelley jaye
Shelley jaye What does victor say about his childhood in chapter xix?
What does victor say about his childhood in chapter xix? Job description computer programmer
Job description computer programmer Describe the conditions necessary for sublimation to occur.
Describe the conditions necessary for sublimation to occur. Name weather conditions
Name weather conditions Tasks conditions and standards
Tasks conditions and standards Advantages of changing criterion design
Advantages of changing criterion design Economic conditions
Economic conditions Gao rexford conditions
Gao rexford conditions What is standard pressure
What is standard pressure Diaphanous test
Diaphanous test Civil service modernised terms and conditions
Civil service modernised terms and conditions Boundary conditions for perfect dielectric materials
Boundary conditions for perfect dielectric materials Post mortem changes
Post mortem changes Robert gagne theory
Robert gagne theory What is the dependent variable
What is the dependent variable Necessary and sufficient conditions examples
Necessary and sufficient conditions examples Integral test conditions
Integral test conditions Mendel equilibrium
Mendel equilibrium Excelsior scholarship eligibility
Excelsior scholarship eligibility Jump instruction in 8086 example
Jump instruction in 8086 example Series de fourier
Series de fourier Knowledge and demand conditions
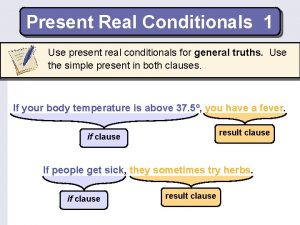
Knowledge and demand conditions Real present conditional
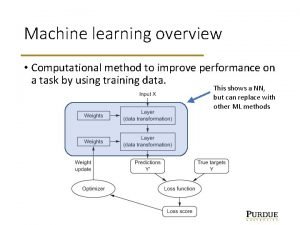
Real present conditional Taxonomic group
Taxonomic group Natural selection conditions
Natural selection conditions Vmware ela terms and conditions
Vmware ela terms and conditions Kkt conditions
Kkt conditions Conditions for parallelograms
Conditions for parallelograms Location conditions
Location conditions Describe the conditions under which new species may arise.
Describe the conditions under which new species may arise. Treaty of versailles terms
Treaty of versailles terms Chapter 12 driving in adverse conditions
Chapter 12 driving in adverse conditions 15.7 conditions for rectangles rhombuses and squares
15.7 conditions for rectangles rhombuses and squares Title 22 restricted health conditions
Title 22 restricted health conditions P/q
P/q Task condition standards
Task condition standards The average weather conditions of a place
The average weather conditions of a place Plicatured nail
Plicatured nail Stp conditions
Stp conditions Elimination reaction conditions
Elimination reaction conditions European working conditions survey 2020
European working conditions survey 2020 Conditional 1,2,3
Conditional 1,2,3 Gibbs free energy equation
Gibbs free energy equation Contact process conditions
Contact process conditions The weather conditions of a particular place
The weather conditions of a particular place Standard conditions vs stp
Standard conditions vs stp Overdriving headlights definition
Overdriving headlights definition Gauss law
Gauss law Conditions of decision making
Conditions of decision making Particle on a ring boundary conditions
Particle on a ring boundary conditions Input controls in webi
Input controls in webi Contoh terms and conditions
Contoh terms and conditions Conditions of decision making
Conditions of decision making Brave new world questions
Brave new world questions Conditions of precipitation in gravimetric analysis
Conditions of precipitation in gravimetric analysis Standard conditions vs stp
Standard conditions vs stp Is milk a perfectly competitive market
Is milk a perfectly competitive market What condition do fungal organisms favor for growth
What condition do fungal organisms favor for growth Average weather conditions over time
Average weather conditions over time Brainpop humidity
Brainpop humidity Monopoly conditions
Monopoly conditions What is delta g
What is delta g 6-5 conditions for special parallelograms answer key
6-5 conditions for special parallelograms answer key Poisson distribution conditions
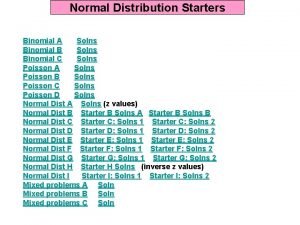
Poisson distribution conditions Groupthink occurs when
Groupthink occurs when Controlling extraneous variables
Controlling extraneous variables Civil service modernised terms and conditions
Civil service modernised terms and conditions