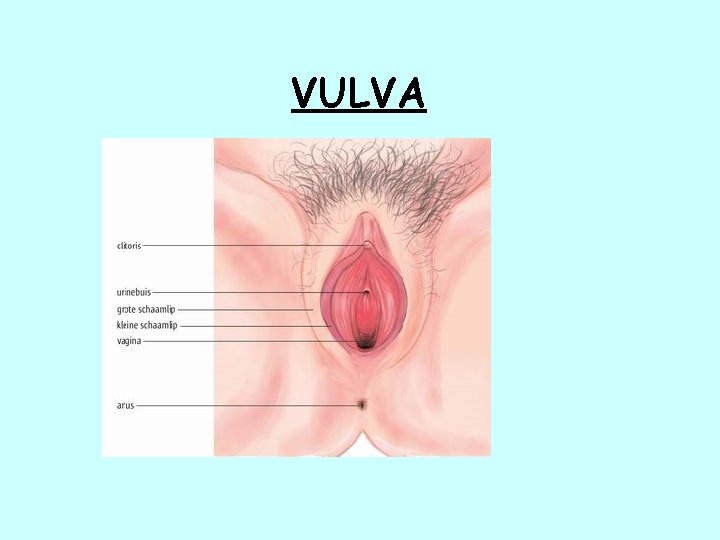
VULVA NORMAL HISTOLOGY Keratinizing stratified squamous epithelium epidermis



















- Slides: 48
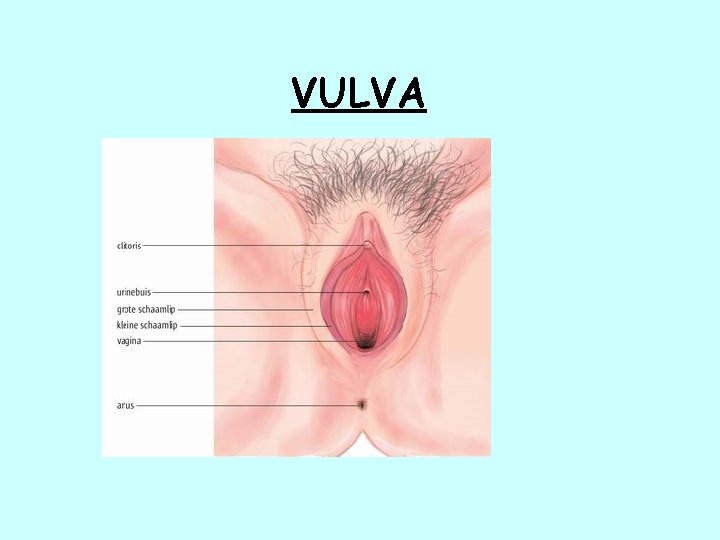
VULVA
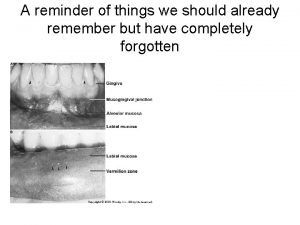
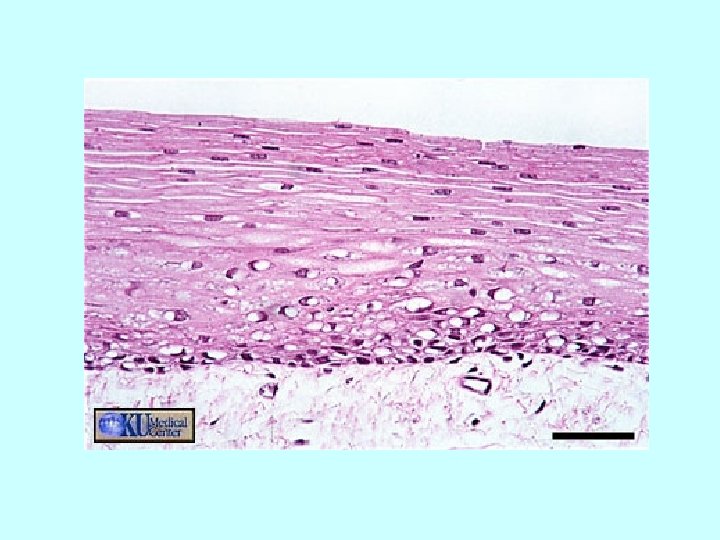
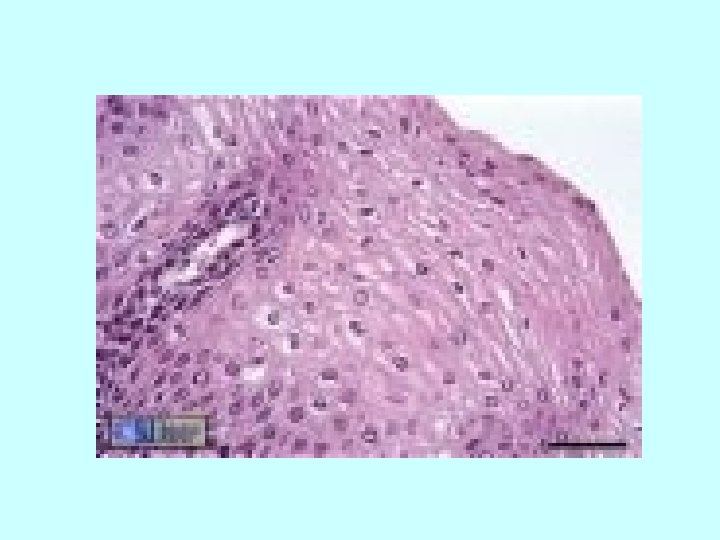
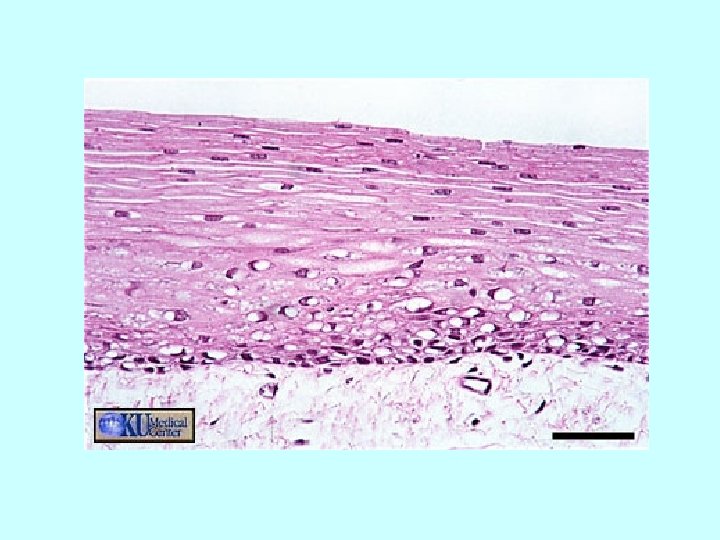
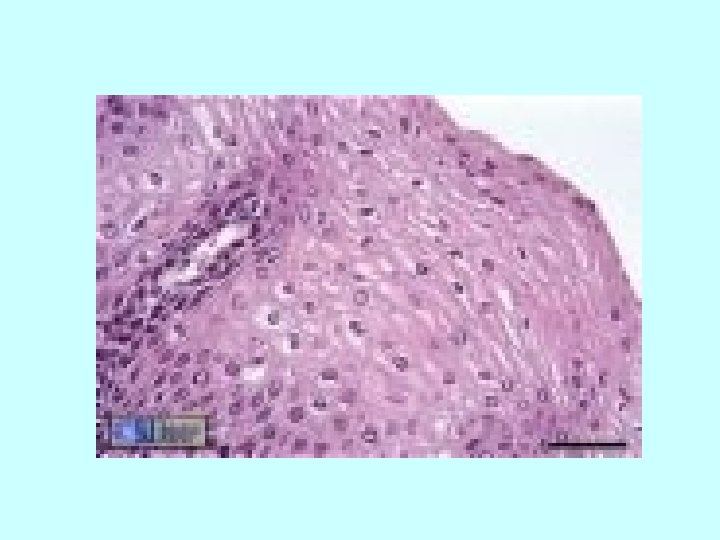
NORMAL HISTOLOGY Keratinizing stratified squamous epithelium (epidermis) Adnexal structures may be presentpilosebaceous units, and sweat glands May be involved by dermatoses that involve skin elsewhere
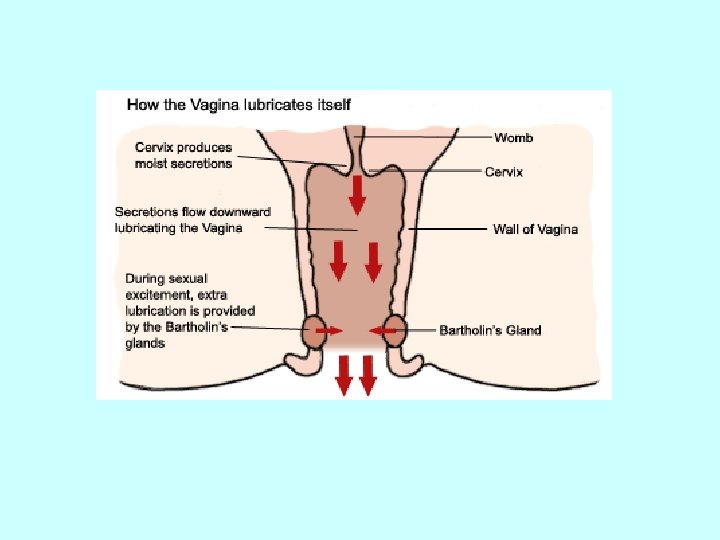
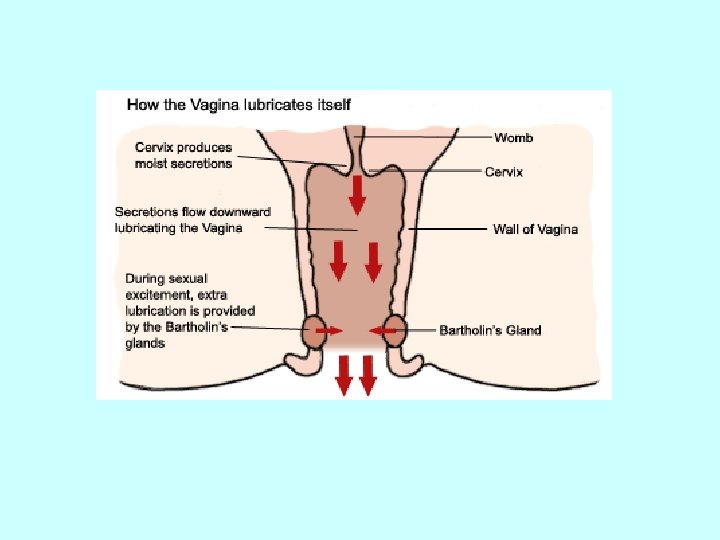
NON-NEOPLASTIC ENTITIES Bartholin's Cyst Common, all ages, secondary to obstruction, 3 -5 cm Lined by transitional or squamous metaplasia Excised or opened permanently(marsupialization)






Vestibular Adenitis Chronic, Recurrent, Painful Unknown Etiology Treatment is surgical removal of inflamed mucosa


LICHEN SCLEROSIS Slight increase in development of carcinoma(1 -4%) however not considered a premalignant lesion
Pale, gray parchment-like skin with atrophy of labia and narrowed introitus most commonly seen in post menopausal women
Histologic features are epidermal atrophy with loss of rete pegs, homogenized collagen of papillary dermis and underlying band of lymphocytes.


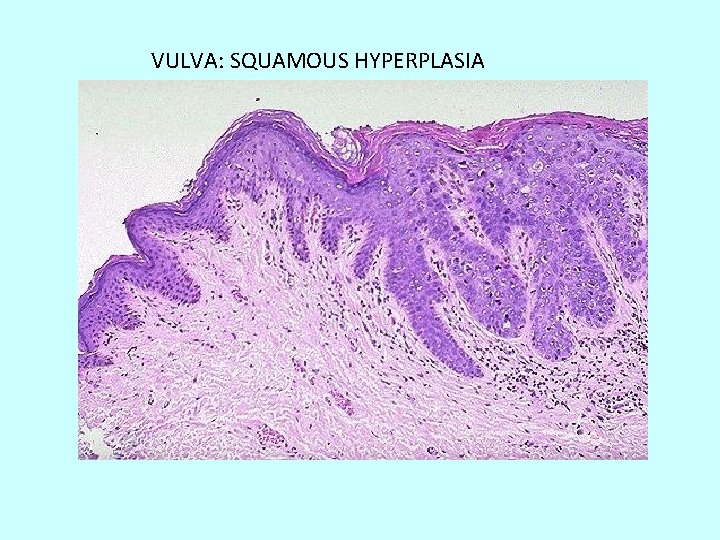
SQUAMOUS HYPERPLASIA Acanthosis usually with hyperkeratosis and variable dermal inflammation Sometimes associated with carcinoma however it is not considered a premalignant lesion unless there is atypia
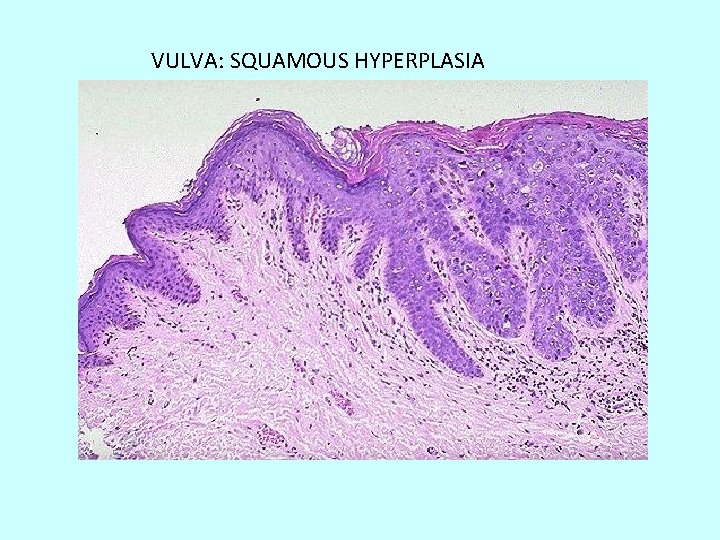
VULVA: SQUAMOUS HYPERPLASIA

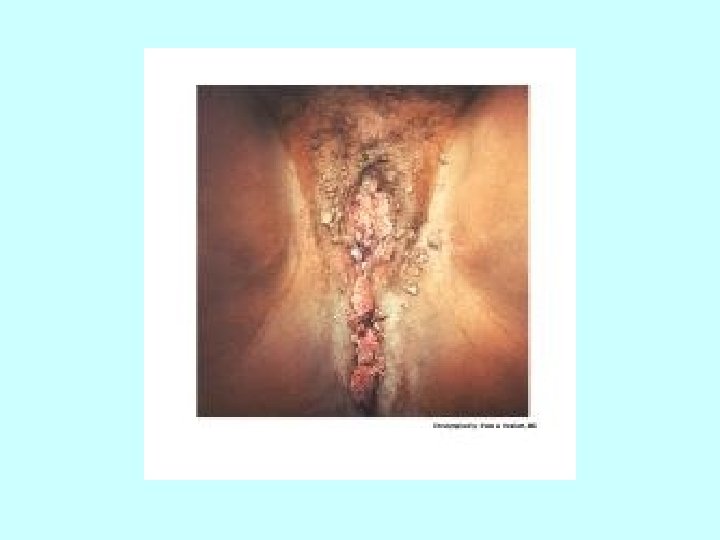
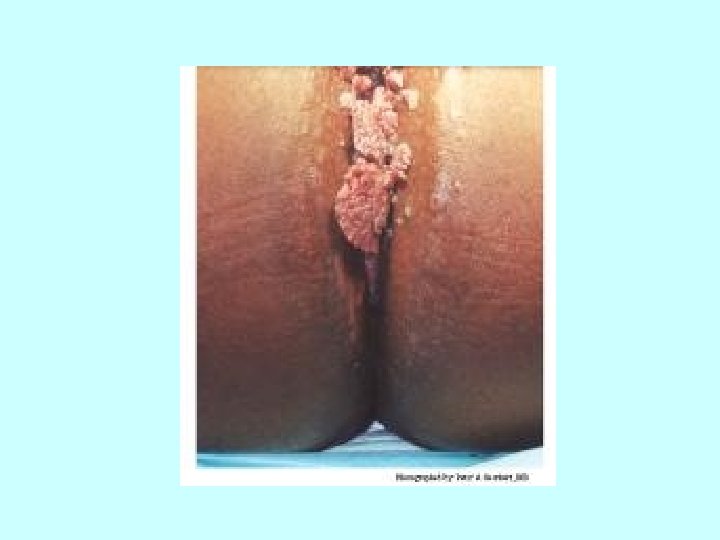
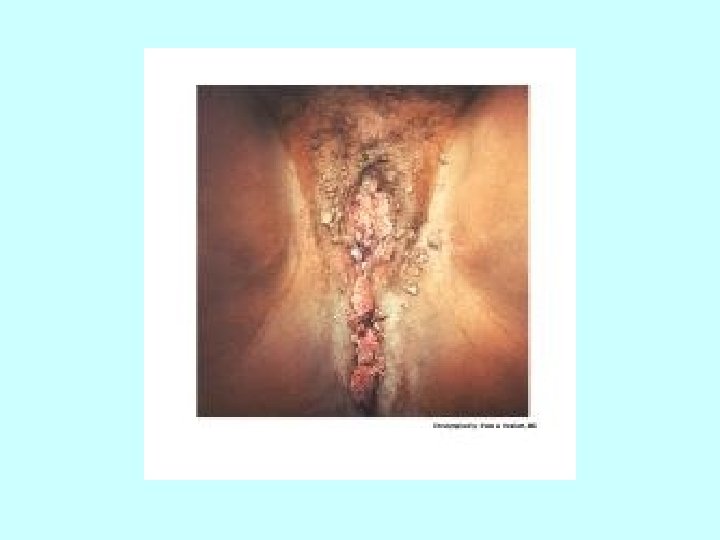
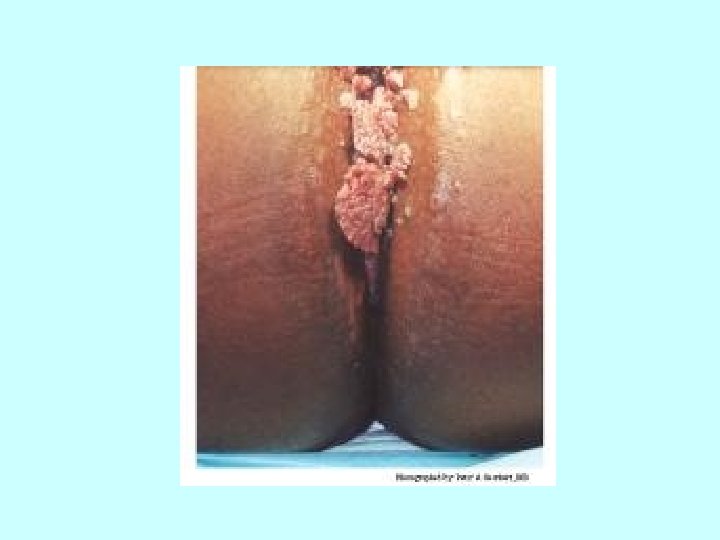
VULVA: BENIGH NEOPASMS Squamous Papilloma Condyloma Acuminatum- HPV(6 &11) induced squamous papilloma
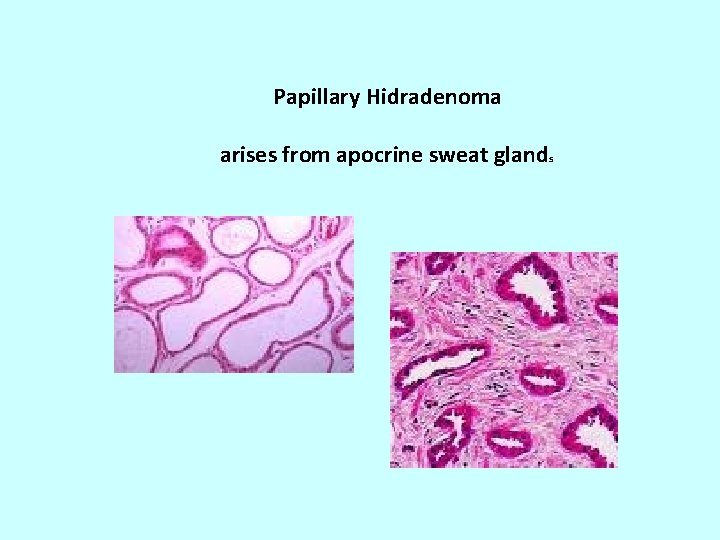
Except in immunosuppressed individuals this may regress and is not considered a premalignant lesion Marker for sexually transmitted disease Papillary Hidradenoma- arises from apocrine sweat glands


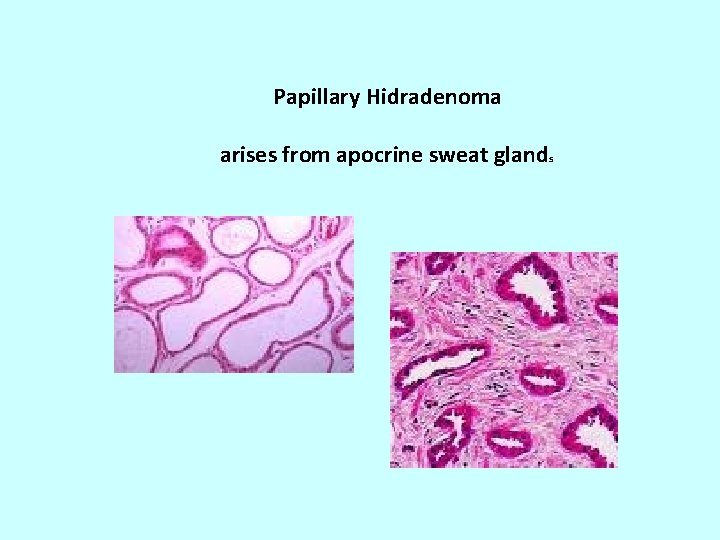
Papillary Hidradenoma arises from apocrine sweat glands

PREMALIGNANT INTRAEPITHELIAL NEOPLASIA Dysplasia (vulvar intraepithelial neoplasia) ( VIN I-III )
HPV related in 90% of cases May be multicentric 5% of VIN III(severe dysplasia) progress to carcinoma elderly and immunosuppressed 30% associated with vaginal or cervical carcinoma
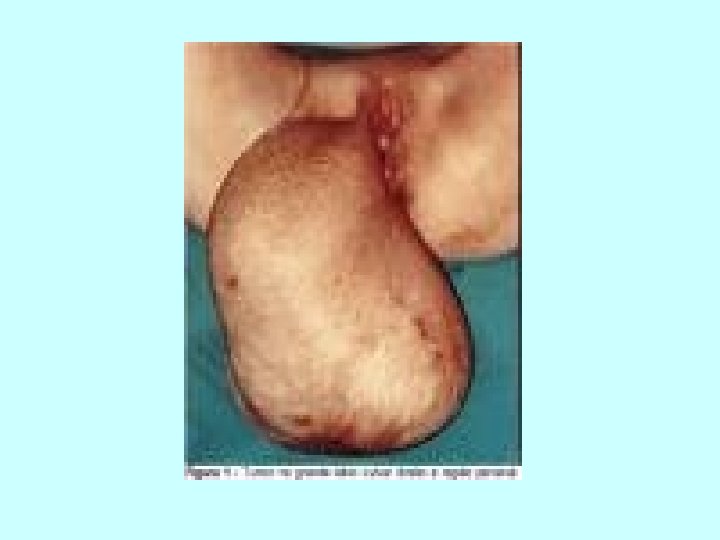
VULVAl CARCINOMA 3% of all genital cancers in the female. 85% are squamous cell carcinoma 15%-basal cell carcinoma, adenocarcinoma 65% have metastasized to regional nodes(inguinal, pelvic) at time of diagnosis



Lesions less than 2 cm - 80% five-year survival rate Larger lesions with positive nodes have less than 10% five year survival rate
Verrucous carcinomawell differentiated squamous cell carcinoma with features of condyloma. It has a good prognosis after wide local excision and is resistant to radiation.
Stage 0. During this stage, the cancer is a preinvasive disease called severe dysplasia, vulvar intraepithelial neoplasia (VIN), or carcinoma in situ (CIS).
This means that the lesion is still on the surface of the vulva and has not invaded more deeply. If detected early and treated, this stage cancer should be curable.
stages of invasive vulvar cancer. Stage. I. Cancer is only in the vulva or the space between the opening of the rectum and the vagina, (perineum), or both. The tumor is 2 cm or less in size. The lymph glands and other sites do not contain cancer.

Stage II. Cancer is in the vulva or the perineum, or both. The tumor is greater than 2 cm. The lymph nodes and other sites do not contain cancer.
Stage III. Cancer is found in the vulva or the perineum, or both. It has spread to nearby tissues such as the lower part of the urethra, the vagina, and the anus. It also may have spread to nearby groin lymph nodes. It has not spread to distant parts of the body.
Stage IV. Cancer has spread beyond the urethra, vagina, and anus into the lining of the bladder and the intestine. It may have also spread to lymph nodes on both sides of the pelvis, the groin, or to other parts of the body.
Recurrent. The cancer has come back after it has been treated. It may come back in the vulva or another place in the body.
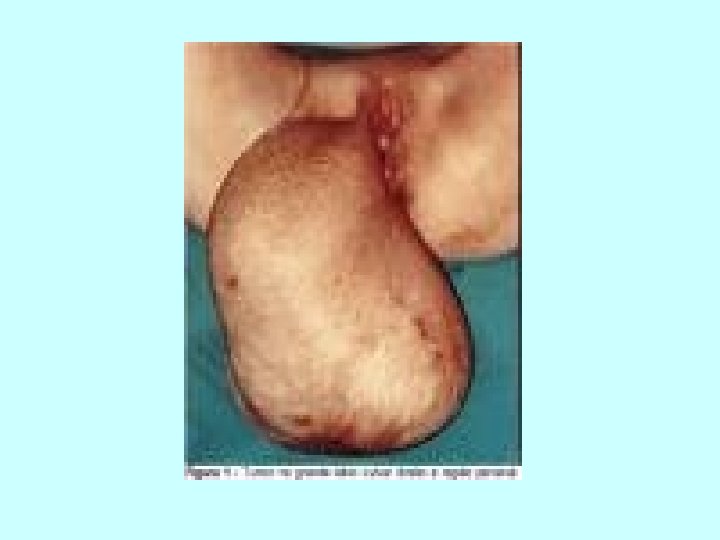
VULVA: EXTRAMAMMARY PAGET'S DISEASE Large tumor cells lying singly or in small clusters within the epidermis and its appendages
EXTRAMAMMARY PAGET'S DISEASE
The tumor cells contain mucopolysaccharides which stain positively with PAS, alcian blue and mucicarmine Underlying adenocarcinoma is uncommon
May be associated with carcinoma of breast, vulva or bladder-poor prognosis Otherwise it may persist for years without evidence of invasion The tumor can be present beyond the grossly apparent lesion resulting in recurrences

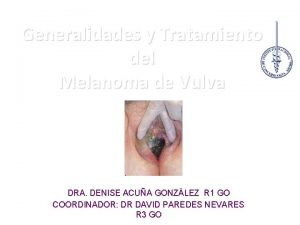
MALIGNANT MELANOMA 5 -10% of vulvar malignancies and 2% of all melanomas in women Peak incidence 6 th to 7 th decade Overall survival rate is 32% Histologically it may mimic paget's disease
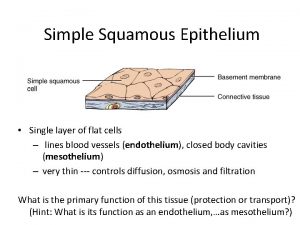
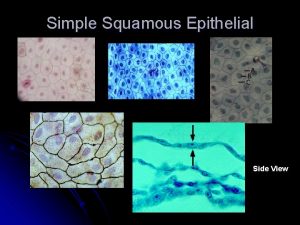
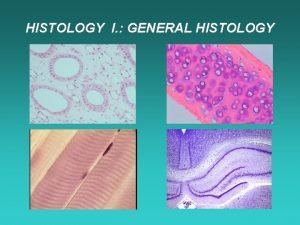
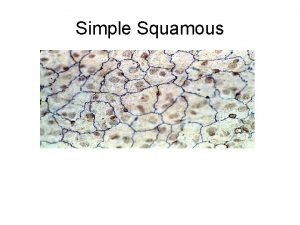
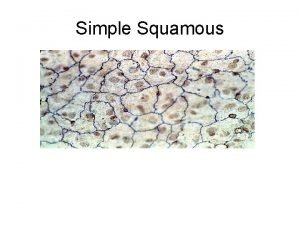
 Simple squamos
Simple squamos Zonula adherens
Zonula adherens Epithelial tissue
Epithelial tissue Epitel
Epitel Stratified squamous non-keratinized epithelium
Stratified squamous non-keratinized epithelium Basal lamina
Basal lamina Zonula occludens
Zonula occludens Orthokeratinized stratified squamous epithelium
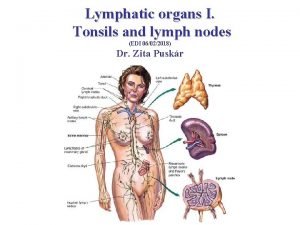
Orthokeratinized stratified squamous epithelium Lymphatic system organs
Lymphatic system organs Simple squamos
Simple squamos Stratified squamous epithelium
Stratified squamous epithelium Characteristics of stratified columnar epithelium
Characteristics of stratified columnar epithelium Keratinized stratified squamous epithelium
Keratinized stratified squamous epithelium Simple columnar epithelium
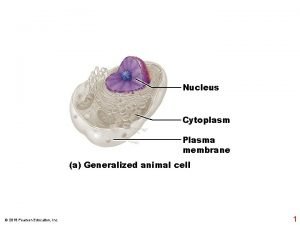
Simple columnar epithelium Cytoplasm
Cytoplasm Epitelio glandular holocrino
Epitelio glandular holocrino Simple squamous epithelium is found lining the
Simple squamous epithelium is found lining the What kind of tissue
What kind of tissue Characteristics of simple squamous epithelium?
Characteristics of simple squamous epithelium? Cuboidal epithelial tissue function
Cuboidal epithelial tissue function Imple squamous epithelium
Imple squamous epithelium Fibroblast plasma
Fibroblast plasma Stratified cuboidal epithelium
Stratified cuboidal epithelium Stratified columnar epithelium
Stratified columnar epithelium Fibroepithelial polyp vulva
Fibroepithelial polyp vulva Vulva real
Vulva real Innervation of ovary
Innervation of ovary Vulva
Vulva Vulva rings
Vulva rings Altura uterina gravidez
Altura uterina gravidez Kerozis
Kerozis Dr kenneth loaiciga
Dr kenneth loaiciga Vulva caracteristicas
Vulva caracteristicas Vulva
Vulva Vulvitis herpetica
Vulvitis herpetica Ashley fuller swedish
Ashley fuller swedish Vulva
Vulva Woman body parts name
Woman body parts name Vulva
Vulva Lymphatic drainage of vulva
Lymphatic drainage of vulva Vulva blood supply
Vulva blood supply Cortonen adalah
Cortonen adalah útero em anteversão
útero em anteversão Curunculus
Curunculus Vulva
Vulva Vin 1 photos
Vin 1 photos Wikipedia
Wikipedia Keratitis eyes
Keratitis eyes Lateral white column
Lateral white column