Vulva Neoplasms and common benign lesions Maria Horvat
Vulva Neoplasms and common benign lesions Maria Horvat, MD, FACOG
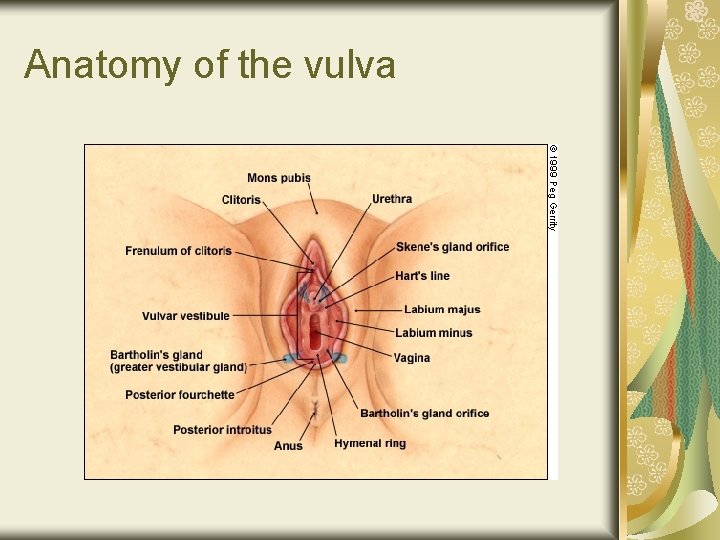
Anatomy of the vulva
Lymphatic drainage of the vulva
Vulvar Cancer 5% of female genital malignancies Usually occurs in the 70 -80 year old population Histology is necessary for diagnosis Occurs anywhere on vulva Surgically staged Most common type is squamous cell Melanoma is 2 nd most common – but still <5% Associated with HPV
Vulvar Cancer Spreads by direct extension Embolizes to lymphatics Hematogenous dissemination
Risks of vulvar cancer HPV Lichen sclerosis Long history of puritis Lymph nodes are single most important prognostic factor
Vulvar Intraepithelial Neoplasms VIN - preinvasive disease VIN 1 VIN 2 VIN 3
Vulvar Intraepithelial Neoplasms VIN 1 Abnormal cellular changes Confined to lower 1/3 Epithelium – no progressive vulvar cancer
Vulvar Intraepithelial Neoplasms VIN 2 “moderate” 1/3 -2/3 Epithelium involved
Vulvar Intraepithelial Neoplasms VIN 3 “severe” 2/3 – all If untreated most go on to cancer If treated 4% go on to cancer Treat with wide local excision
Cancer In-Situ All epithelium involved
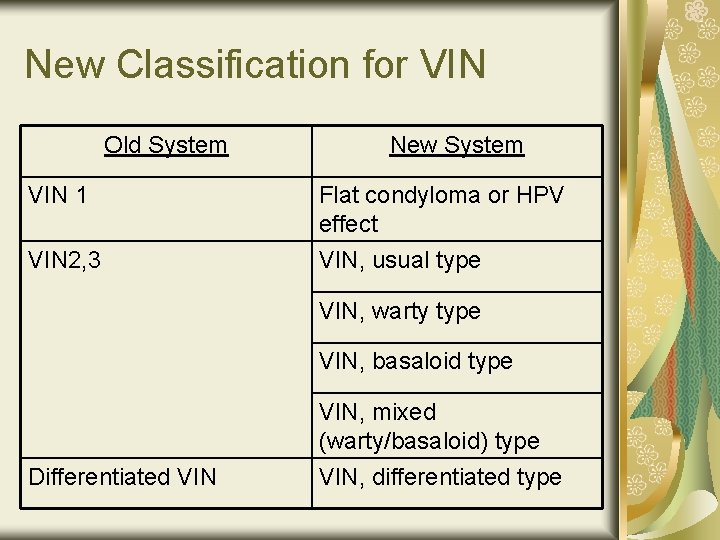
New Classification for VIN Old System New System VIN 1 Flat condyloma or HPV effect VIN 2, 3 VIN, usual type VIN, warty type VIN, basaloid type Differentiated VIN, mixed (warty/basaloid) type VIN, differentiated type
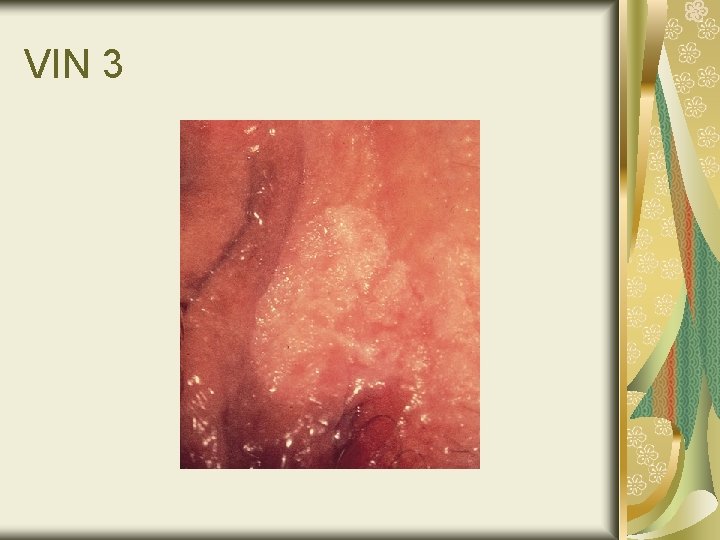
VIN 3
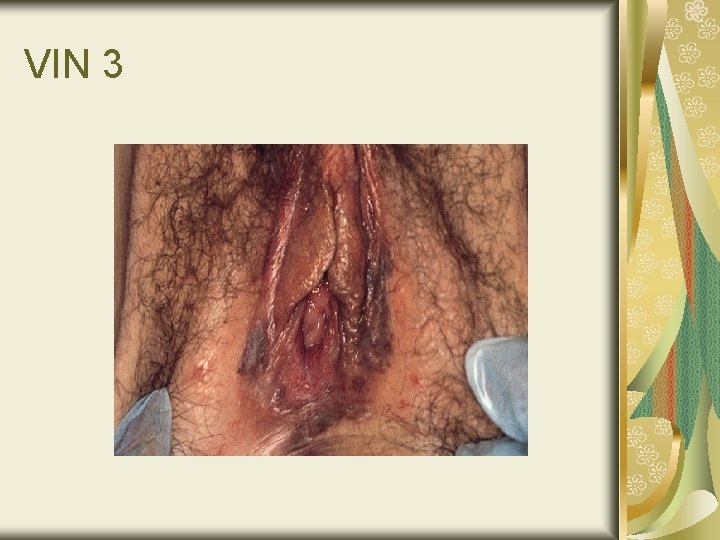
VIN 3
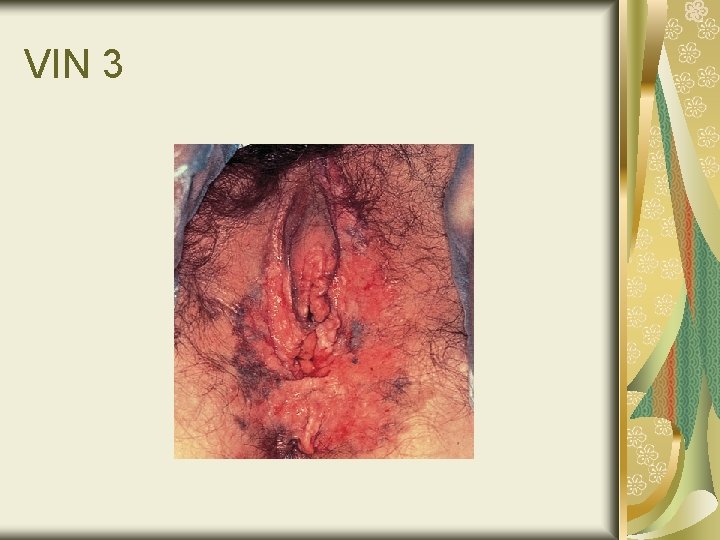
VIN 3
VIN - Treatment Local excision Local destruction
VIN 50% asymptomatic 25% hyperpigmented Typically: raised surface
VIN – Diagnosis 3% acetic acid Punch biopsy

Staging of Vulvar Carcinoma Stage Characteristics Stage 0 Carcinoma in situ; intraepithelial neoplasia grade III Stage I Lesion <2 cm; confined to the vulva or perineum; no nodal metastasis Stage Ia Lesion <2 cm; confined to the vulva or perineum and with stromal invasion <1 mm; no nodal metastasis Stage Ib Lesion <2 cm; confined to the vulva or perineum and with stromal invasion >1 mm; no nodal metastasis Stage II Tumor >2 cm in greatest dimension; confined to the vulva and/or perineum; no nodal metastasis Stage III Tumor of any size with adjacent spread to the lower urethra and/or vagina or anus and/or unilateral regional lymph node metastasis Stage Iva Tumor invasion of any of the following: upper urethra, bladder mucosa, rectal mucosa, and/or pelvic bone and/or bilateral regional node metastases Stage Ivb Any distant metastasis, including pelvic lymph nodes

Vulvar Cancer – prognostic factors For nodal involvement Size Depth of invasion Lesion thickness Grade Vascular space involvement For survival Positive inguinal nodes Positive pelvic nodes
VIN - Treatment Cancer-in-situ Excision with at least 1 cm margins topical Invasive Cancer Inguinal-femoral lymph nodes Radical excision Radiation Pelvic exenteration
Melanoma Usually arises from nevi Blue/black Ulcerated RX: wide excision with 2 cm free border If depth of invasion <1. 5 mm, 100%survival

Vulvar Melanoma
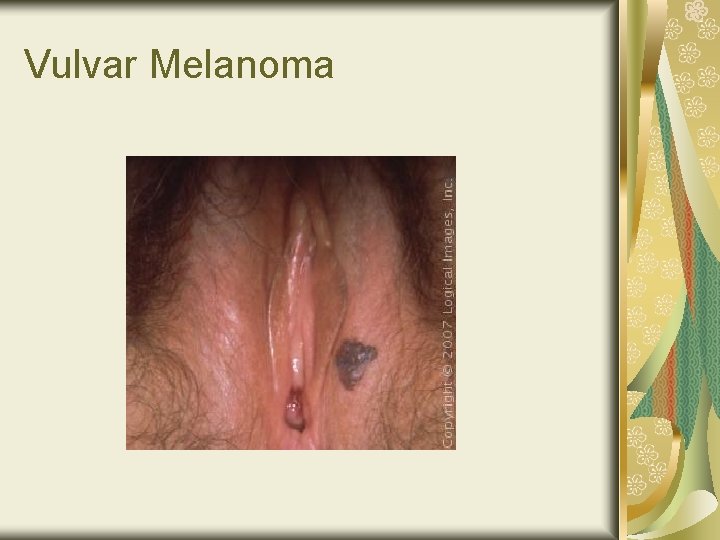
Vulvar Melanoma
Pagets Disease of the Vulva Hyperemic tissue Cake icing effect Rx: wide local excision 30% will develop adenocarcinoma of the breast, colon, and rectum

Pagets Disease
Lichen Sclerosis Itching Diagnosed by biopsy Can eventually become VIN or vulvar cancer 20% hypothyroid
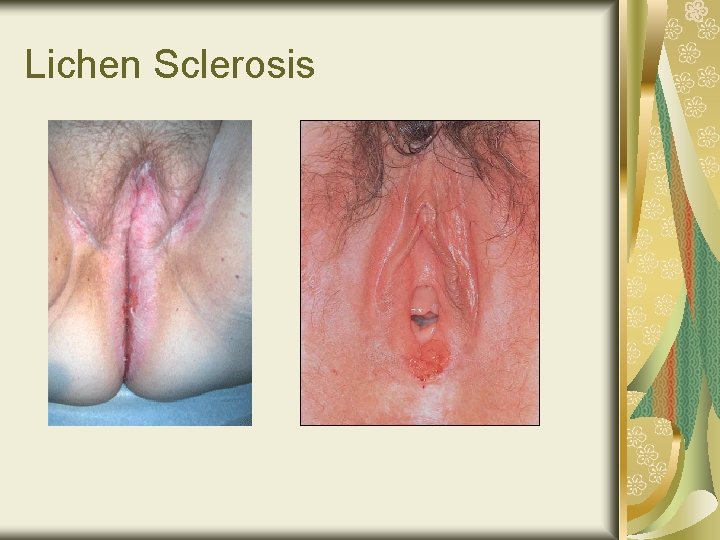
Lichen Sclerosis
Remember! BIOPSY anything suspicious!
References The Female Patient; April 2008 Clinical Gynecology; Bieber www. Images. MD
- Slides: 31