VSD post TAVR Mechanisms Presentation and Management Haim





- Slides: 17

VSD post TAVR: Mechanisms, Presentation and Management Haim Danenberg, MD Hadassah Hebrew University Medical Center Jerusalem, Israel
Haim Danenberg, MD Clinical proctor, Medtronic Consultant, 3 -D systems
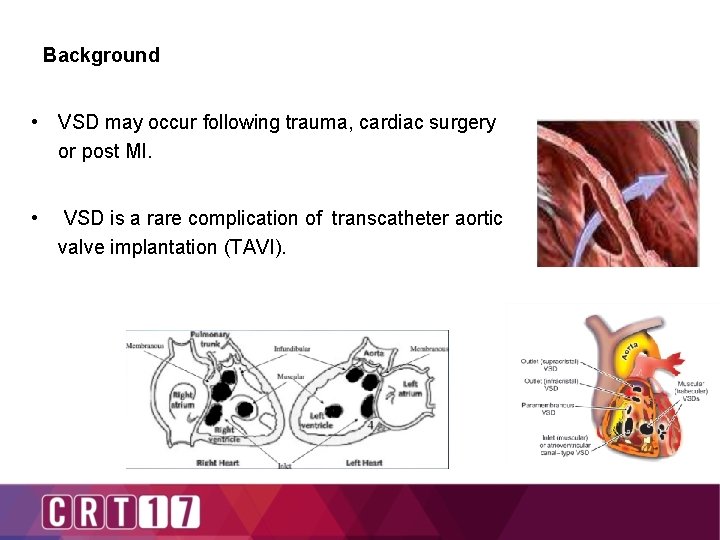
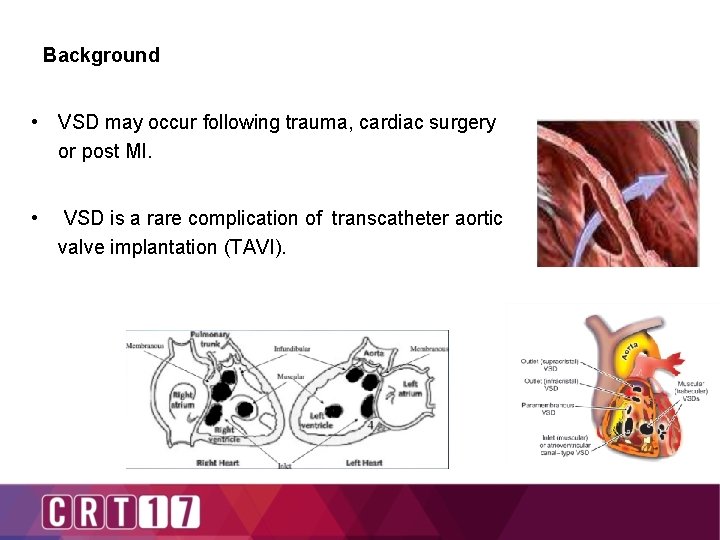
Background • VSD may occur following trauma, cardiac surgery or post MI. • VSD is a rare complication of transcatheter aortic valve implantation (TAVI).
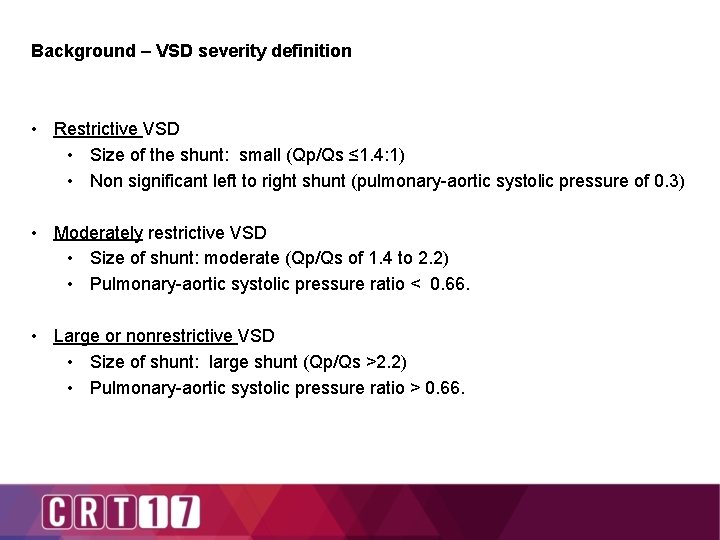
Background – VSD severity definition • Restrictive VSD • Size of the shunt: small (Qp/Qs ≤ 1. 4: 1) • Non significant left to right shunt (pulmonary-aortic systolic pressure of 0. 3) • Moderately restrictive VSD • Size of shunt: moderate (Qp/Qs of 1. 4 to 2. 2) • Pulmonary-aortic systolic pressure ratio < 0. 66. • Large or nonrestrictive VSD • Size of shunt: large shunt (Qp/Qs >2. 2) • Pulmonary-aortic systolic pressure ratio > 0. 66.
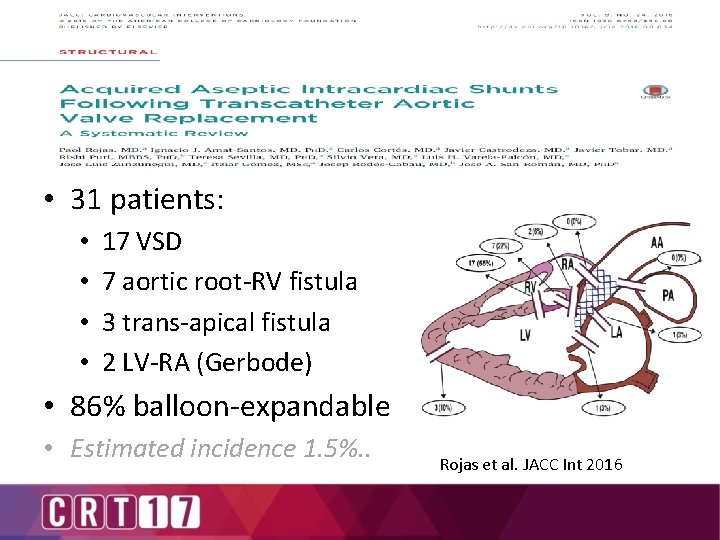
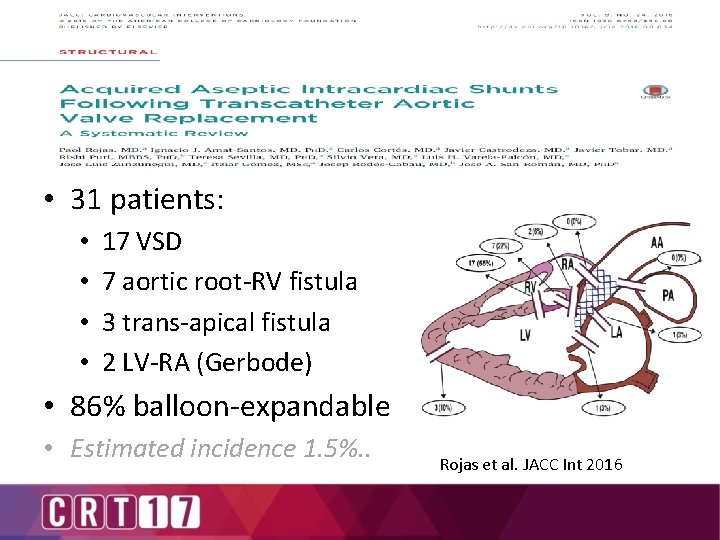
• 31 patients: • • 17 VSD 7 aortic root-RV fistula 3 trans-apical fistula 2 LV-RA (Gerbode) • 86% balloon-expandable • Estimated incidence 1. 5%. . Rojas et al. JACC Int 2016

• 18 VSD • 2 LV-RA (Gerbode) • Risk Factors: • • Severe annular calcification Oversizing Oval/assymetric annulus Ando et al. Heart, Lung and Circulation 2016 Post dilatation

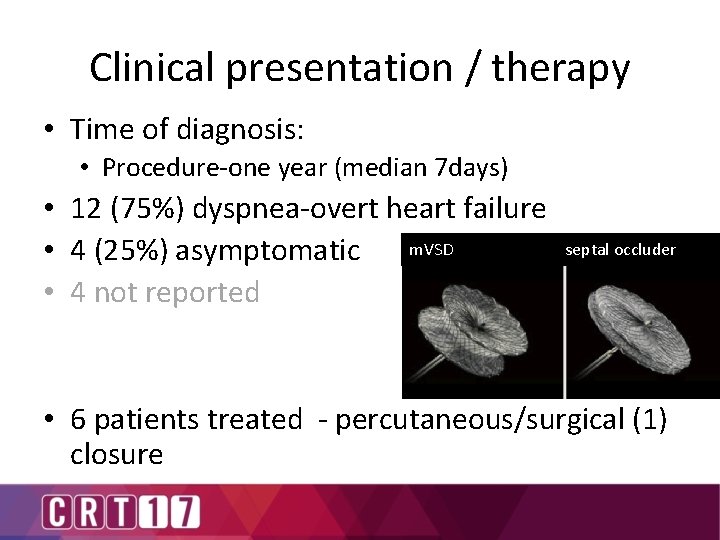
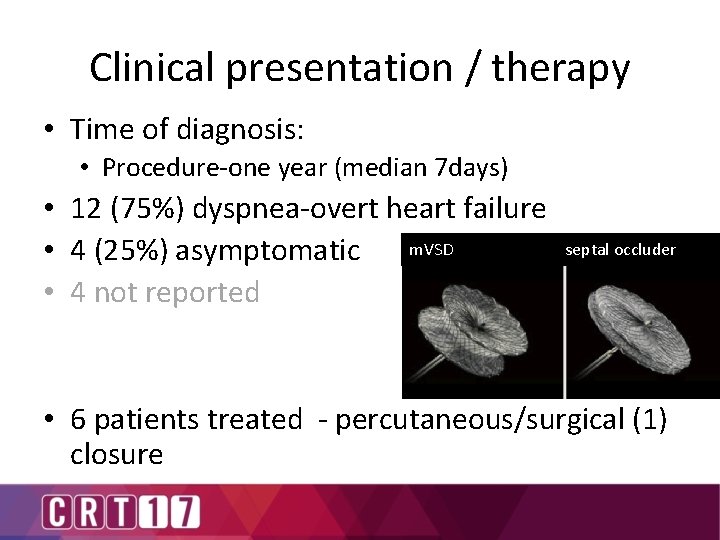
Clinical presentation / therapy • Time of diagnosis: • Procedure-one year (median 7 days) • 12 (75%) dyspnea-overt heart failure m. VSD septal occluder • 4 (25%) asymptomatic • 4 not reported • 6 patients treated - percutaneous/surgical (1) closure
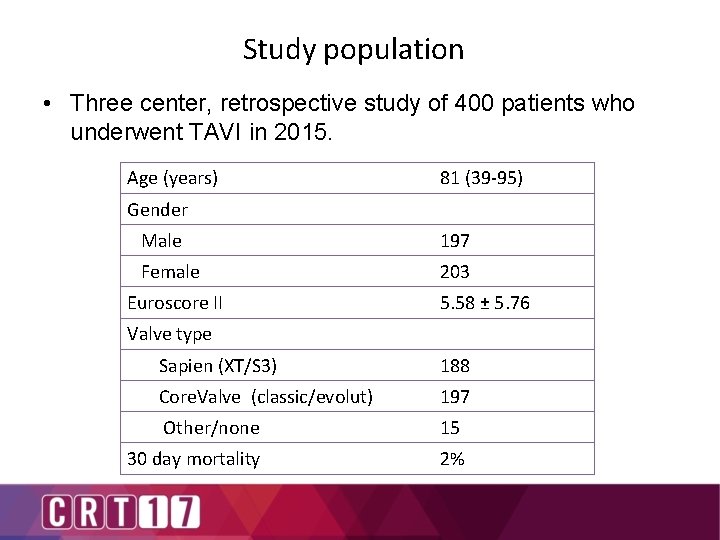
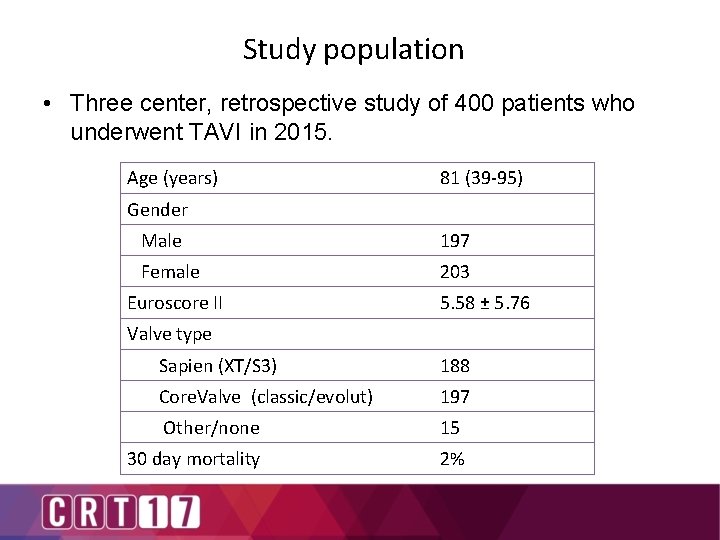
Study population • Three center, retrospective study of 400 patients who underwent TAVI in 2015. Age (years) 81 (39 -95) Gender Male 197 Female 203 Euroscore II 5. 58 ± 5. 76 Valve type Sapien (XT/S 3) 188 Core. Valve (classic/evolut) 197 Other/none 15 30 day mortality 2%
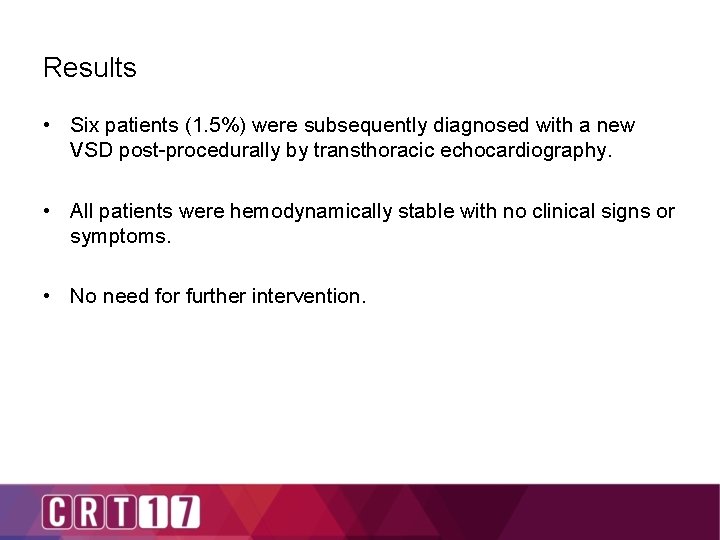
Results • Six patients (1. 5%) were subsequently diagnosed with a new VSD post-procedurally by transthoracic echocardiography. • All patients were hemodynamically stable with no clinical signs or symptoms. • No need for further intervention.
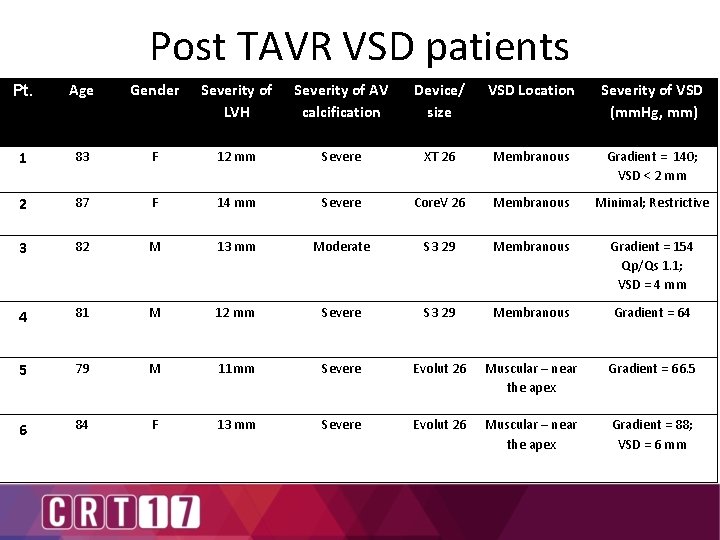
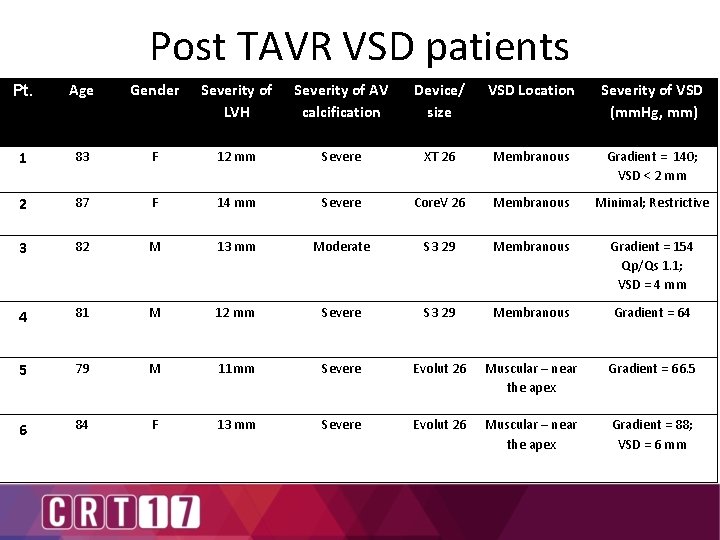
Post TAVR VSD patients Pt. Age Gender Severity of LVH Severity of AV calcification Device/ size VSD Location Severity of VSD (mm. Hg, mm) 1 83 F 12 mm Severe XT 26 Membranous Gradient = 140; VSD < 2 mm 2 87 F 14 mm Severe Core. V 26 Membranous Minimal; Restrictive 3 82 M 13 mm Moderate S 3 29 Membranous Gradient = 154 Qp/Qs 1. 1; VSD = 4 mm 4 81 M 12 mm Severe S 3 29 Membranous Gradient = 64 5 79 M 11 mm Severe Evolut 26 Muscular – near the apex Gradient = 66. 5 6 84 F 13 mm Severe Evolut 26 Muscular – near the apex Gradient = 88; VSD = 6 mm
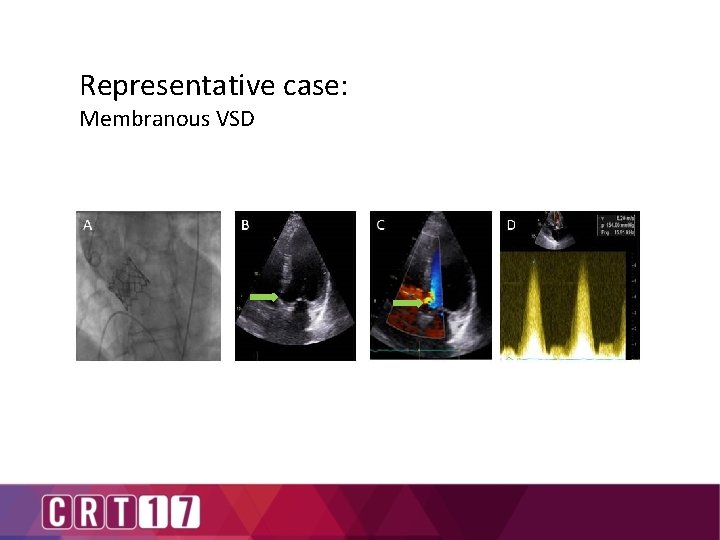
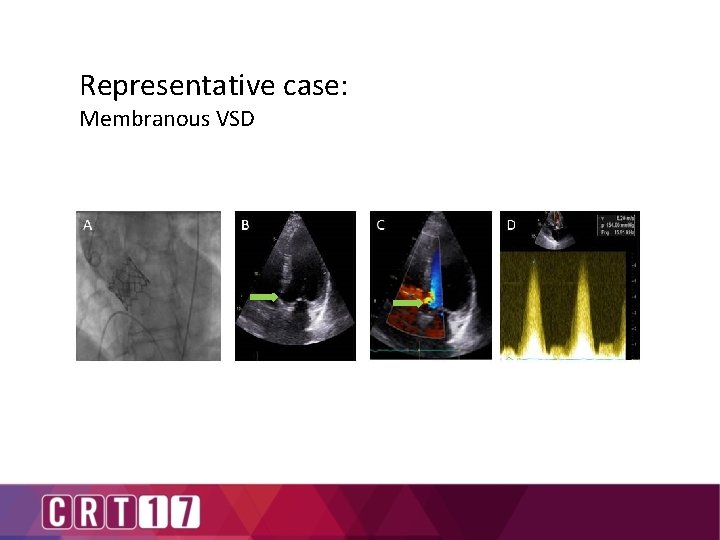
Representative case: Membranous VSD
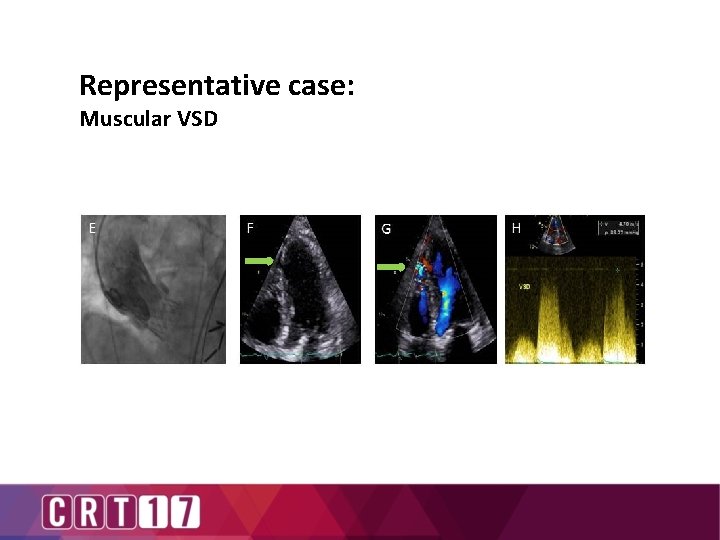
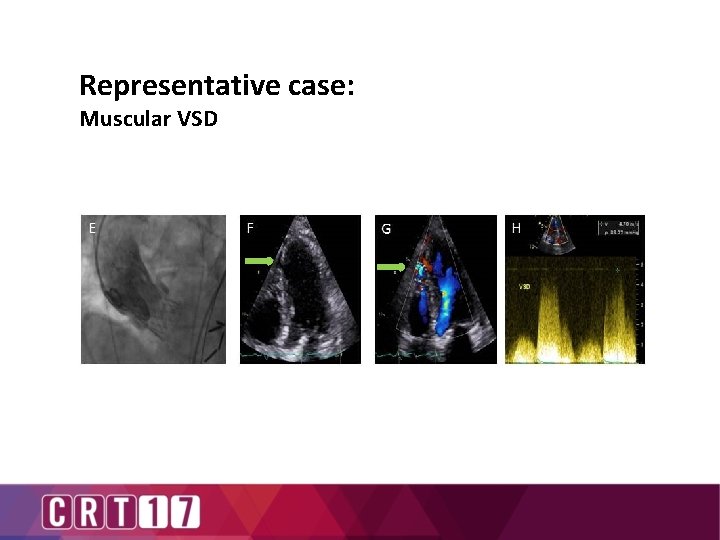
Representative case: Muscular VSD

Mechanism of Membranous VSD – Hypothesis • Overestimation of bioprosthetic valve size or highly calcific / narrow LVOT leading to high pressure exerted on the membranous part of the septum, potentially leading to its tearing and VSD formation. • Prevention: – Meticulous analysis of all imaging modalities enabling optimal choice of the most suitable valve and size. – Modeling / 3 -D printing of valve apparatus?
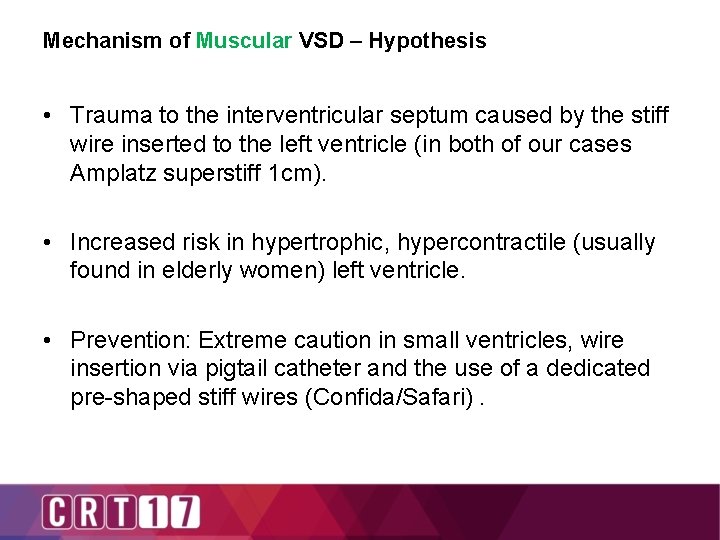
Mechanism of Muscular VSD – Hypothesis • Trauma to the interventricular septum caused by the stiff wire inserted to the left ventricle (in both of our cases Amplatz superstiff 1 cm). • Increased risk in hypertrophic, hypercontractile (usually found in elderly women) left ventricle. • Prevention: Extreme caution in small ventricles, wire insertion via pigtail catheter and the use of a dedicated pre-shaped stiff wires (Confida/Safari).
Post TAVR VSD: conclusions • VSD is a rare complication of TAVR with an incidence ranging 0. 5 -1. 5% • Most VSDs are of no hemodynamic significance, probably underdiagnosed and call for no special therapy. Large, hemodynamic significant VSDs may warrant defect closure • To minimize the risk of VSD formation it is recommended to: - Perform meticulous evaluation of the aortic valve annulus and LVOT with special focus on calcium dispersion - Accurate positioning of the bioprosthetic valve - Proper pre-shaping of the stiff wire or use of a dedicated stiff wire & deployment of wire via pigtail catheter
