VR Disorders Common Clinical Presentation Retinal Detachment RD








- Slides: 54

VR Disorders Common Clinical Presentation & Retinal Detachment (RD) Ayesha S Abdullah 31. 12. 2015
Learning outcomes By the end of this lecture the students would be able to; u Identify the common symptoms and signs of VR disorders (VRD) and correlate them with the underlying problem u Define retinal detachment, describe its epidemiology, identify symptoms and signs of retinal detachment and outline the principles of treatment
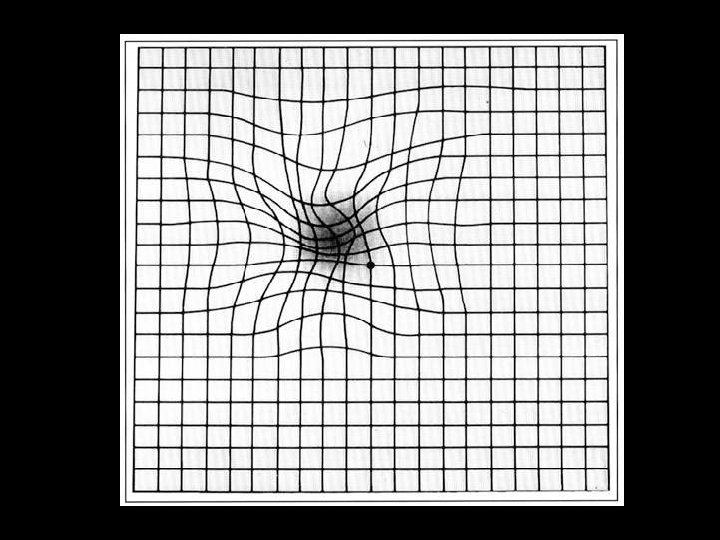
Common Presenting Symptoms in VRD u Visual loss, mostly painless, sudden/ gradual u Loss of central vision u Loss of peripheral vision u Loss of visual field u Loss of colour vision u Distorted vision; metamorphopsia, micropsia, macropsia
Common Presenting Symptoms in VRD u Loss of contrast sensitivity u Glare sensitivity u Night blindness u Photopsia/ flashes u Floaters ; 'specks', 'flies', 'spiders' and, ‘cobweb‘, ‘mosquitoes’.
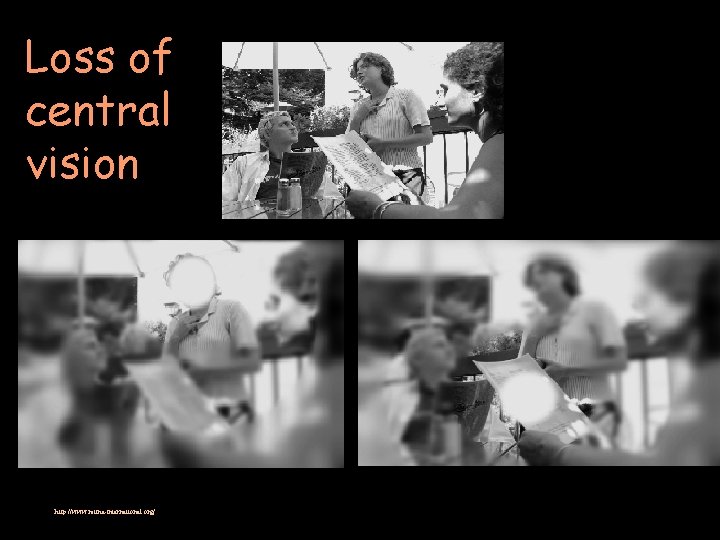
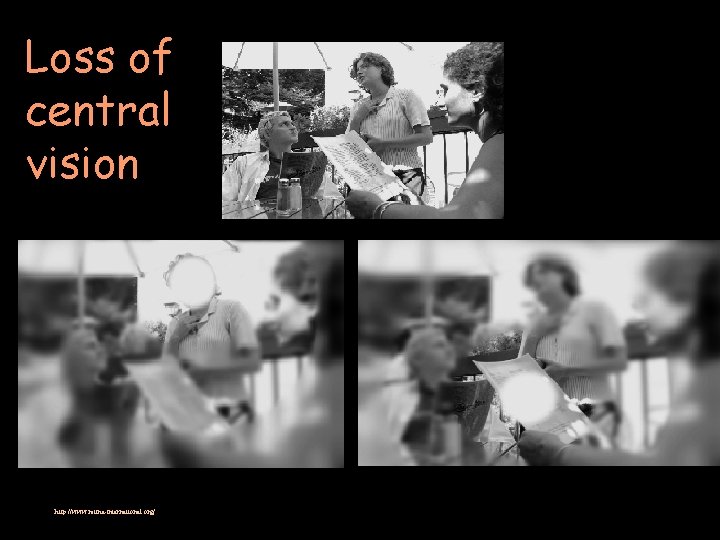
Loss of central vision http: //www. retina-international. org/
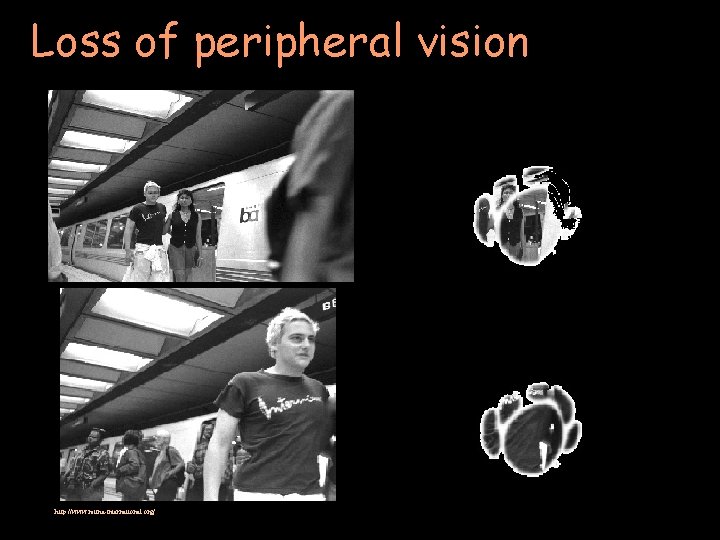
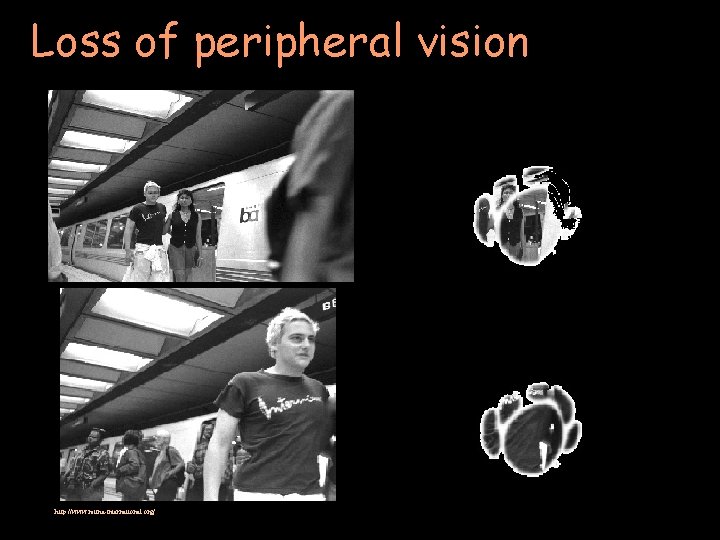
Loss of peripheral vision http: //www. retina-international. org/
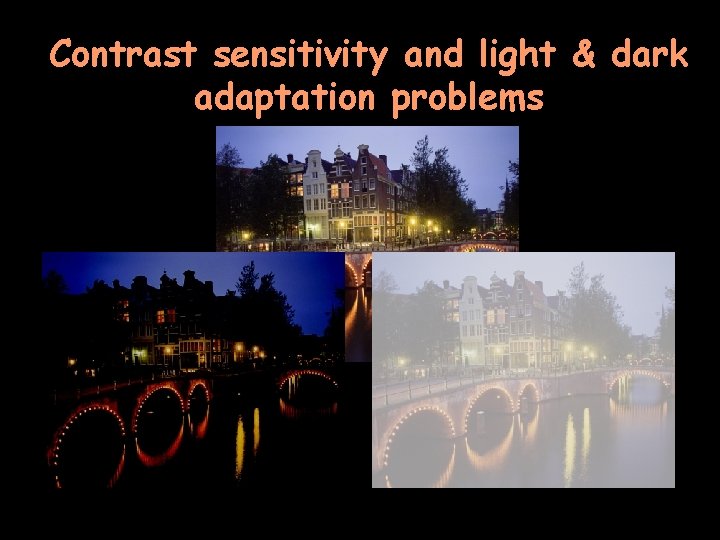
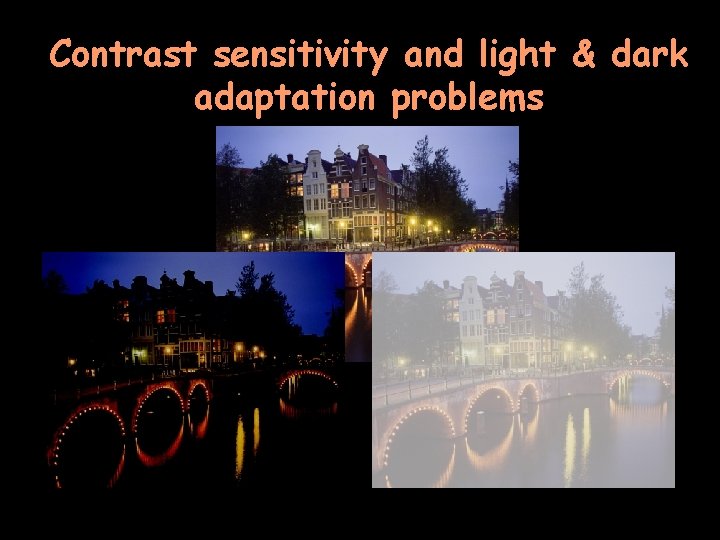
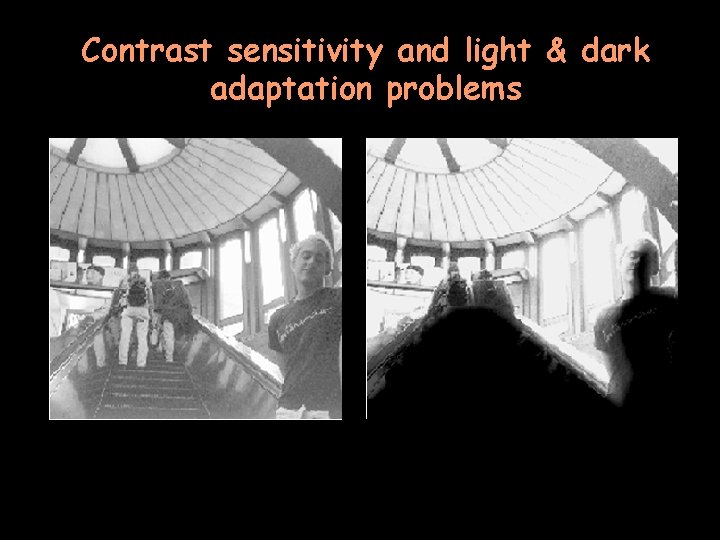
Contrast sensitivity and light & dark adaptation problems
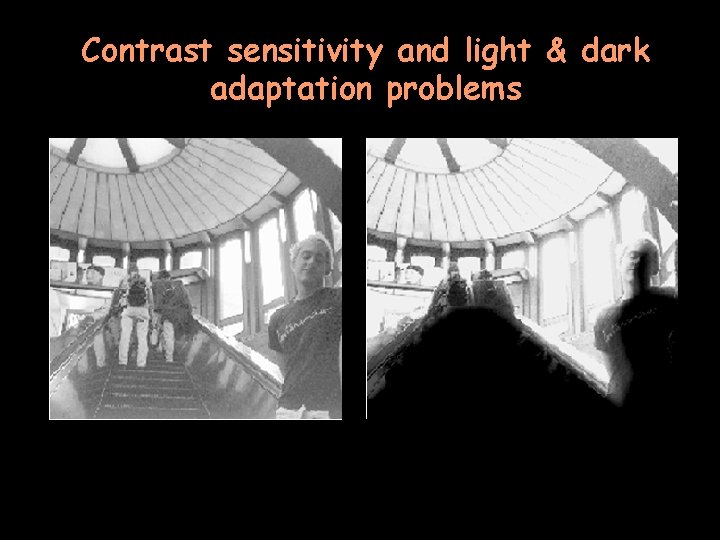
Contrast sensitivity and light & dark adaptation problems

Glare

Flashes of light/ photopsia
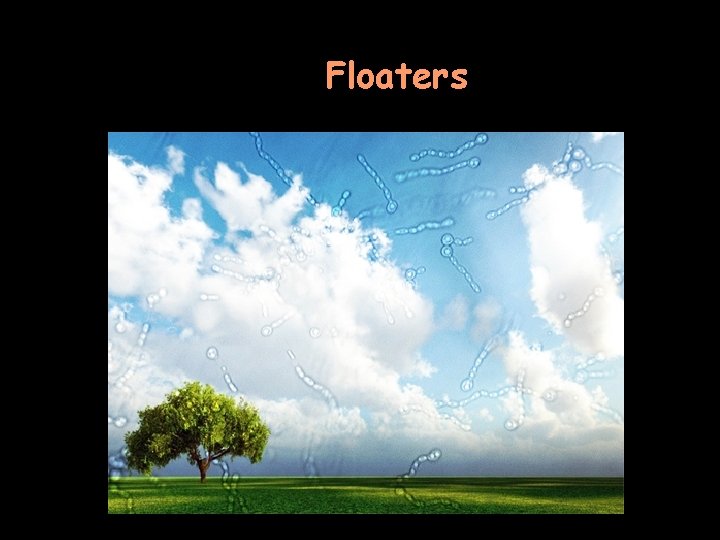
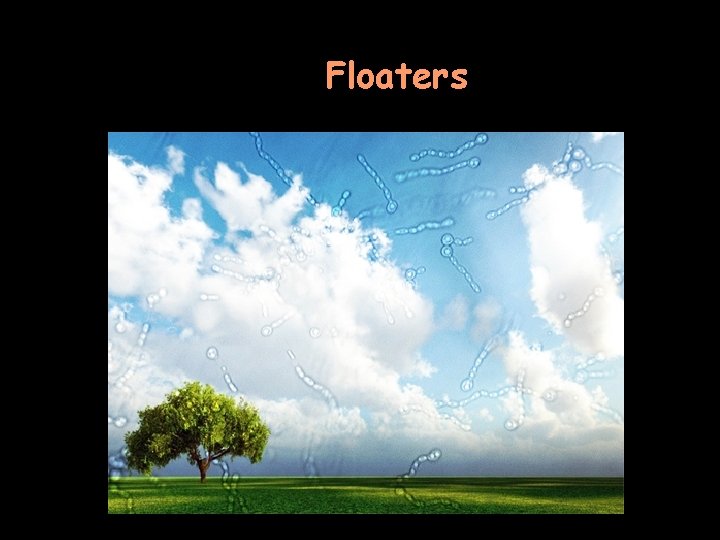
Floaters
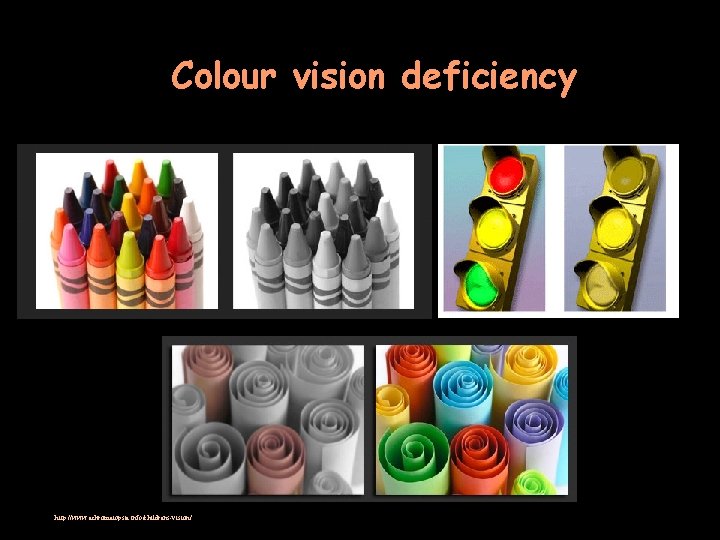
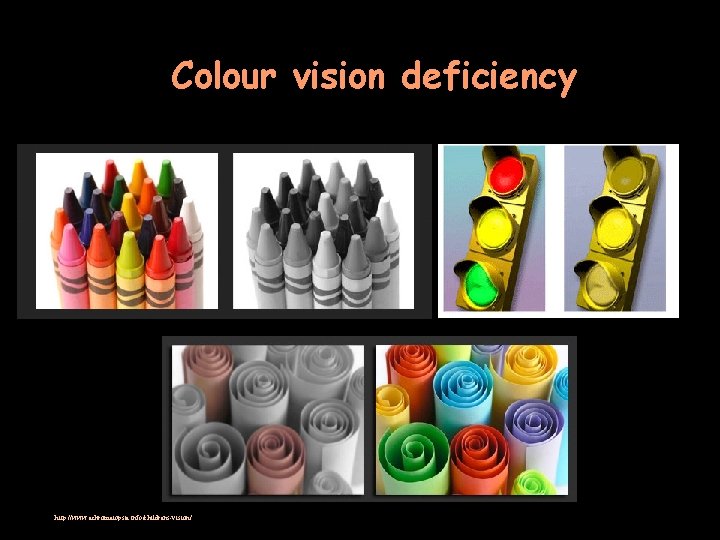
Colour vision deficiency http: //www. achromatopsia. info/childrens-vision/

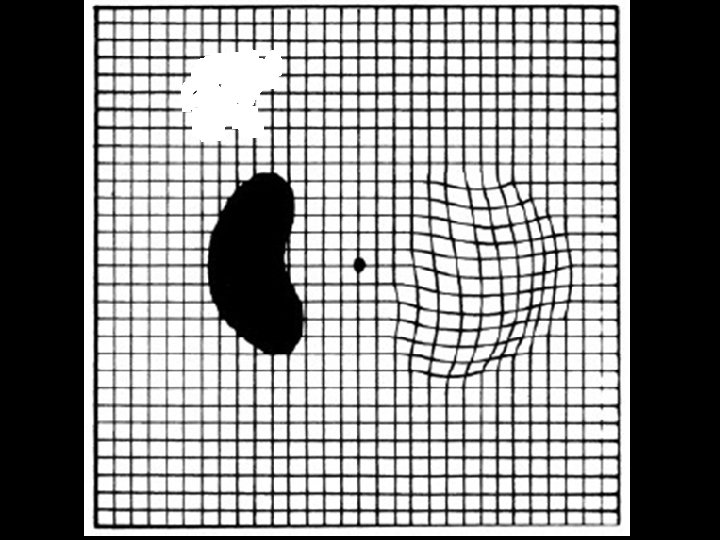
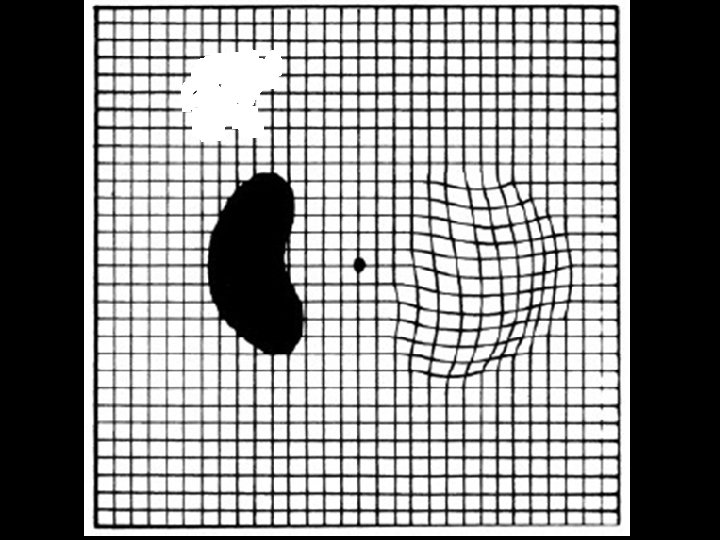
Field loss
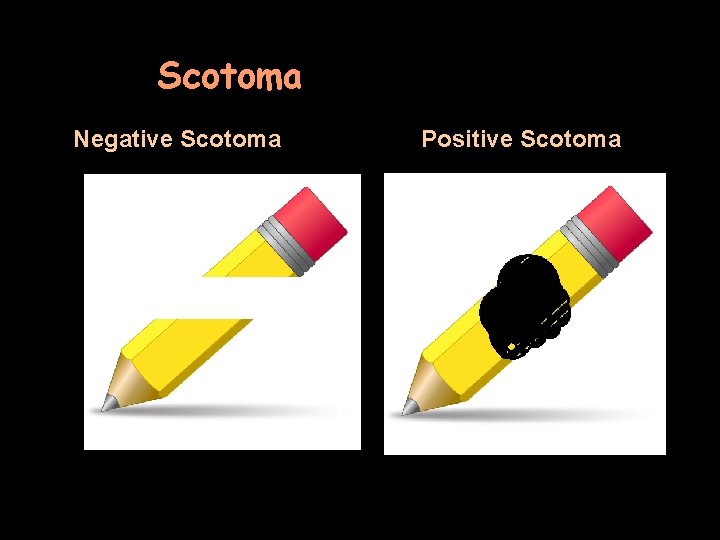
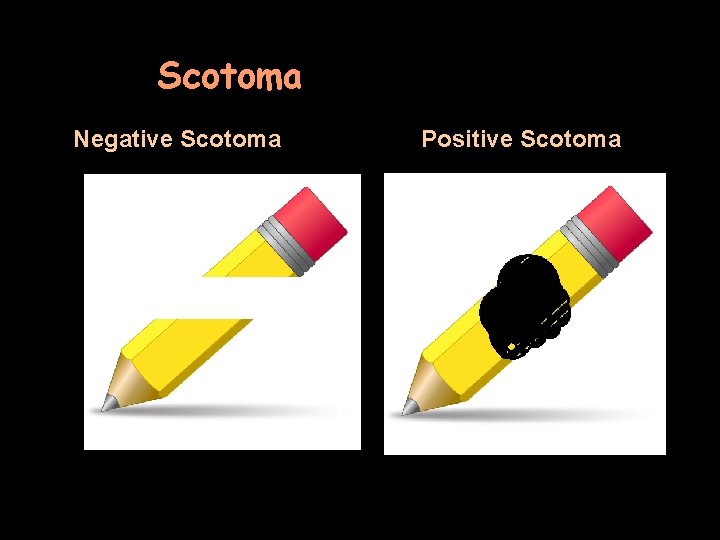
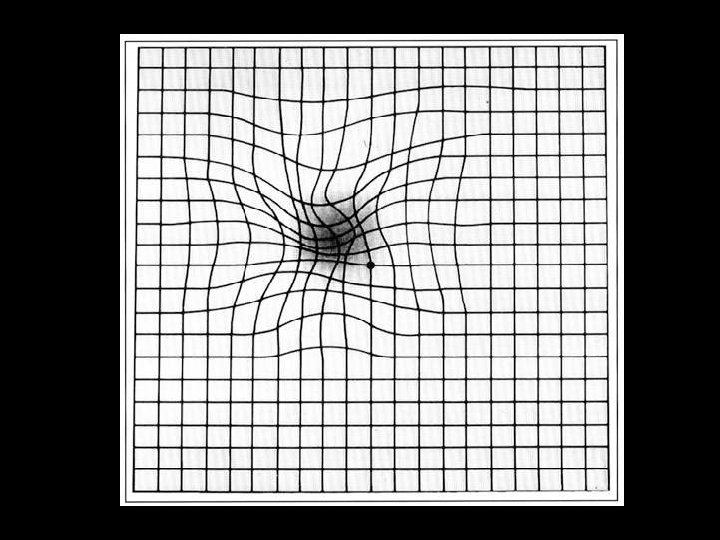
Scotoma Negative Scotoma Positive Scotoma
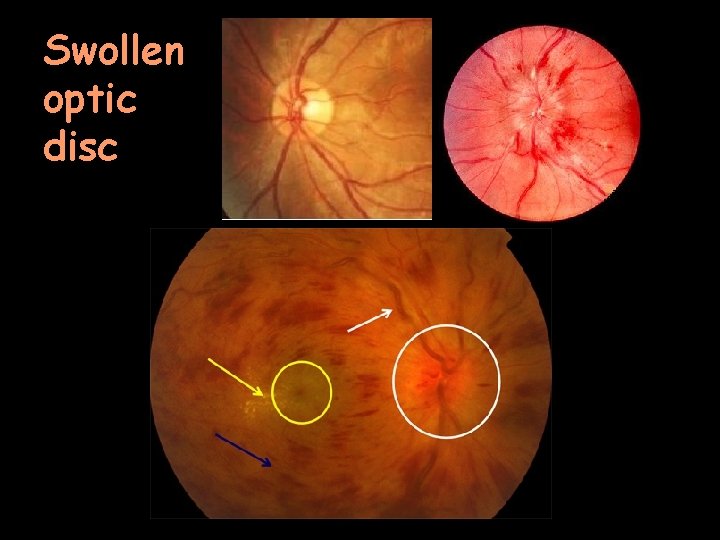
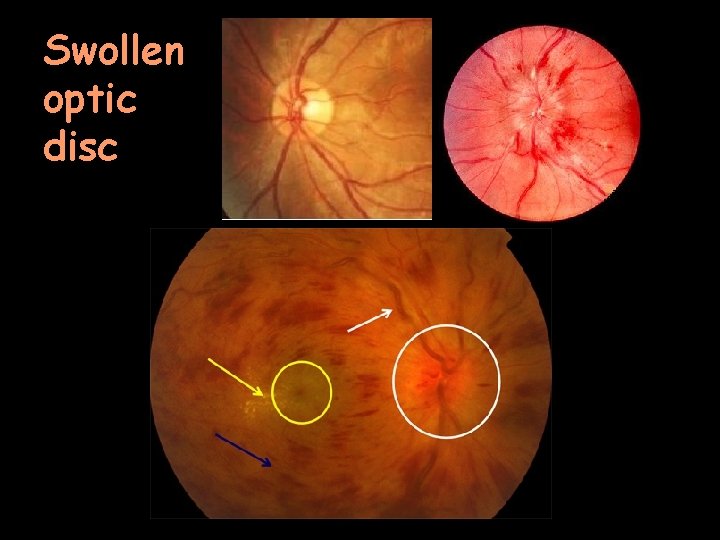
Swollen optic disc

Pale optic disc
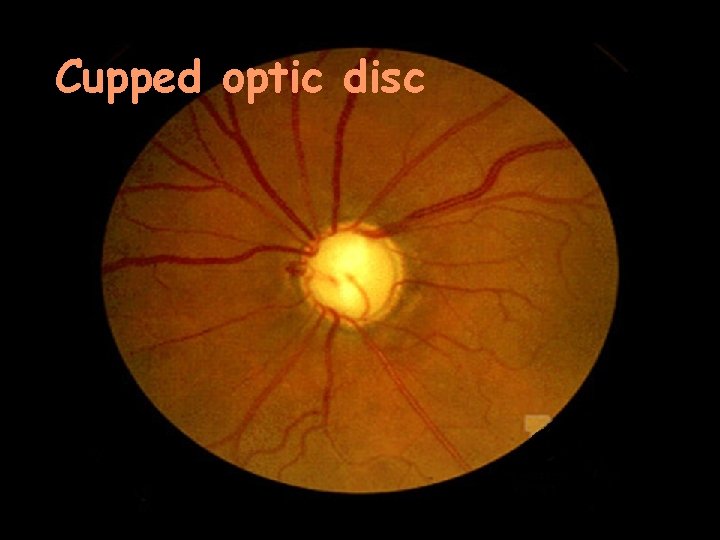
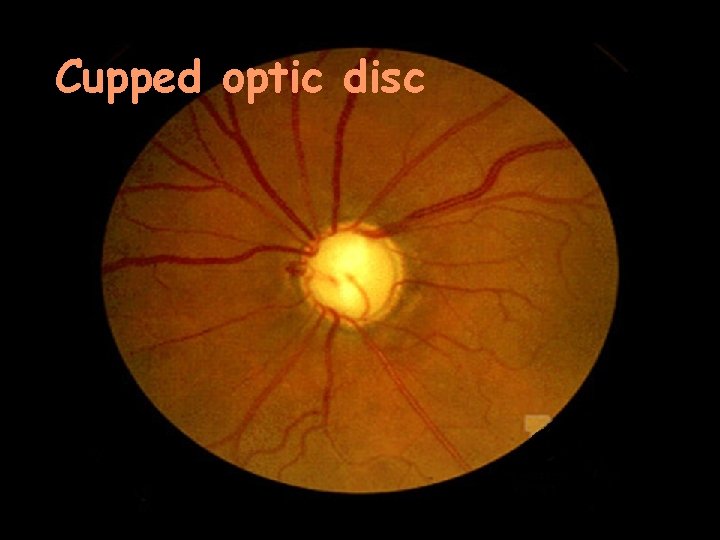
Cupped optic disc
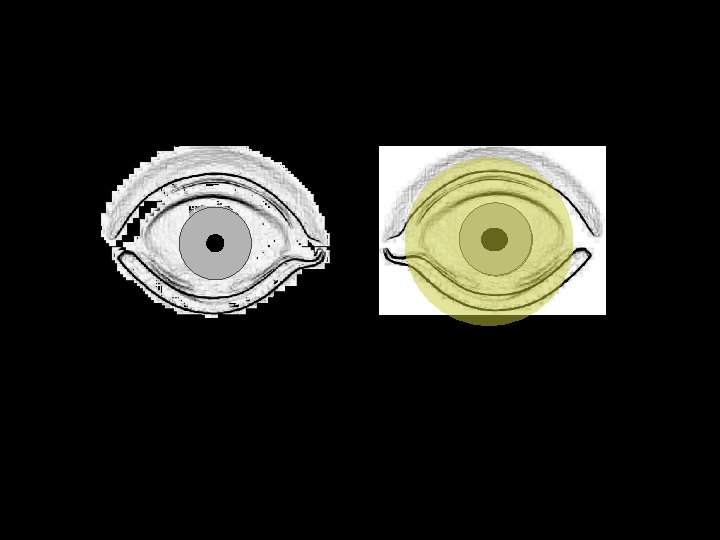
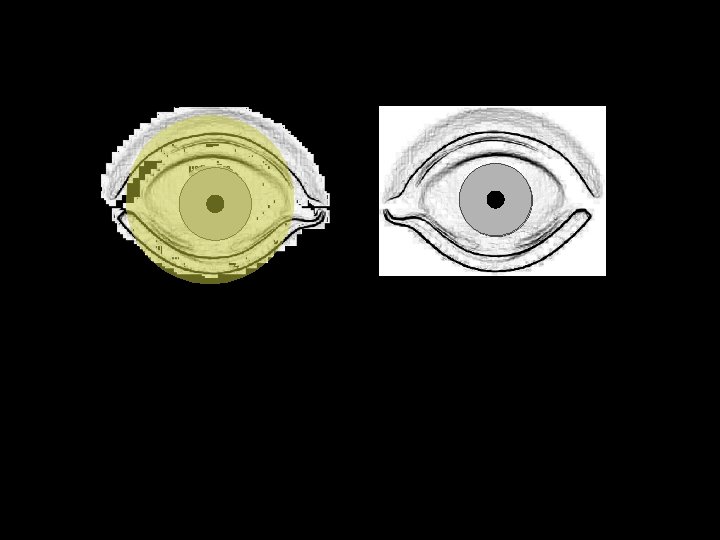
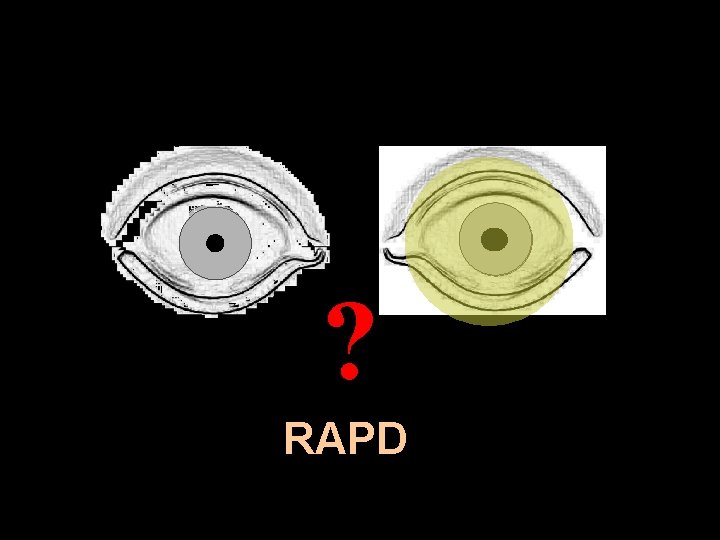
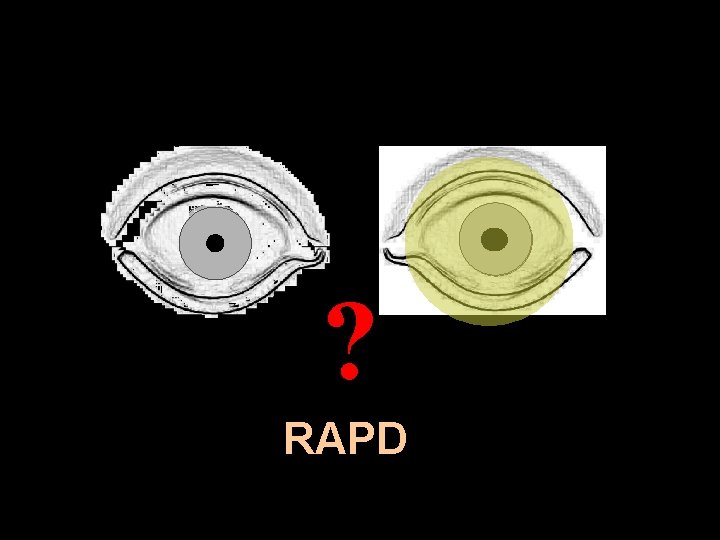
? RAPD


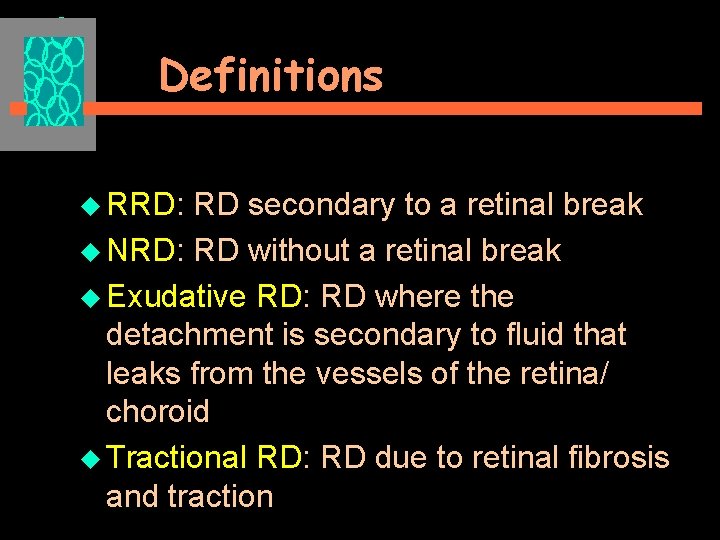
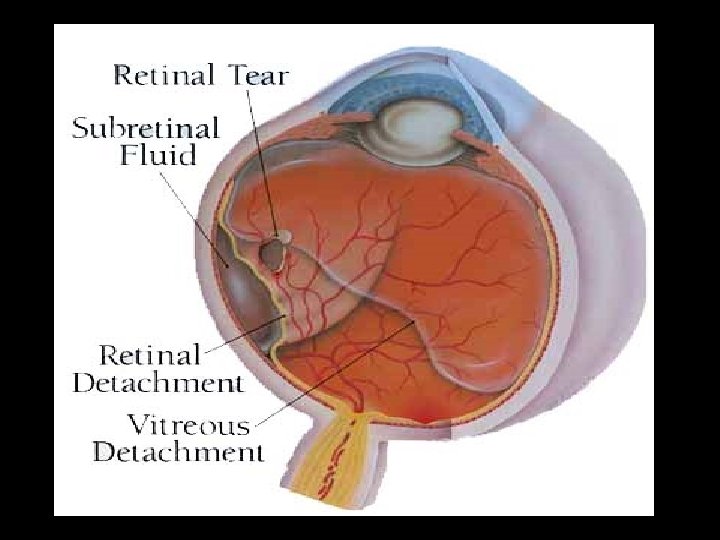
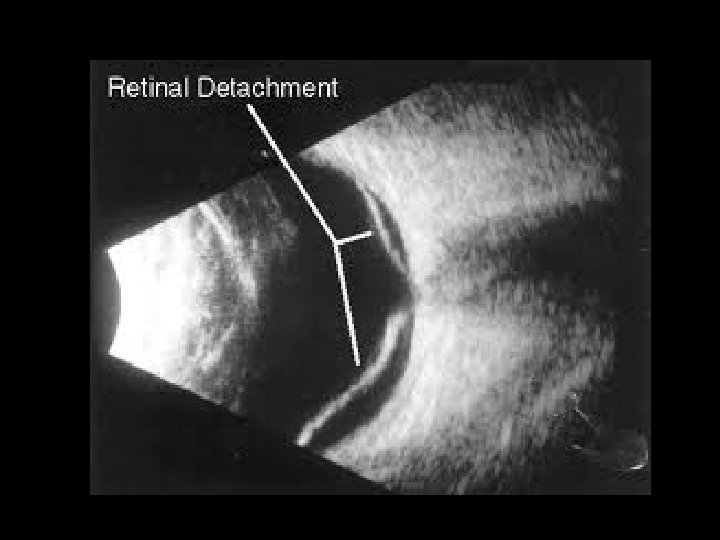
Definitions u What is Retinal Detachment? Separation of the neurosensory retina from the retinal pigment epithelium u Types u u Rhegmatogenous RD (RRD) u Non- rhegmatogenous RD (NRD) § Exudative RD § Tractional RD u Combined Tractional RNC
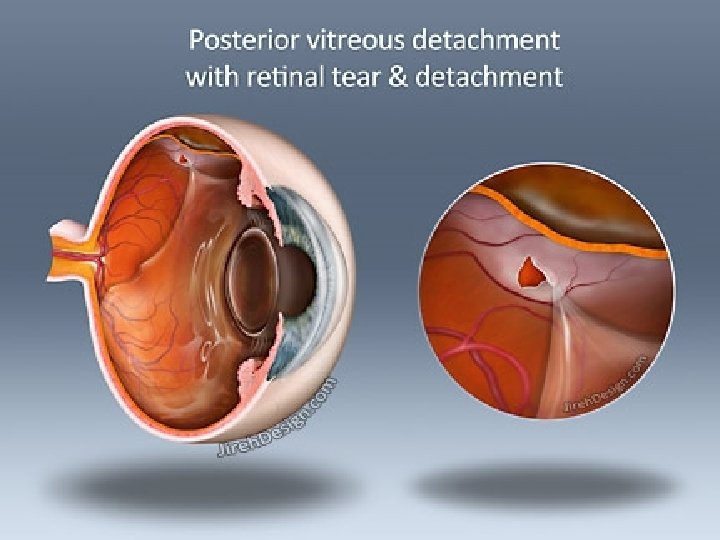
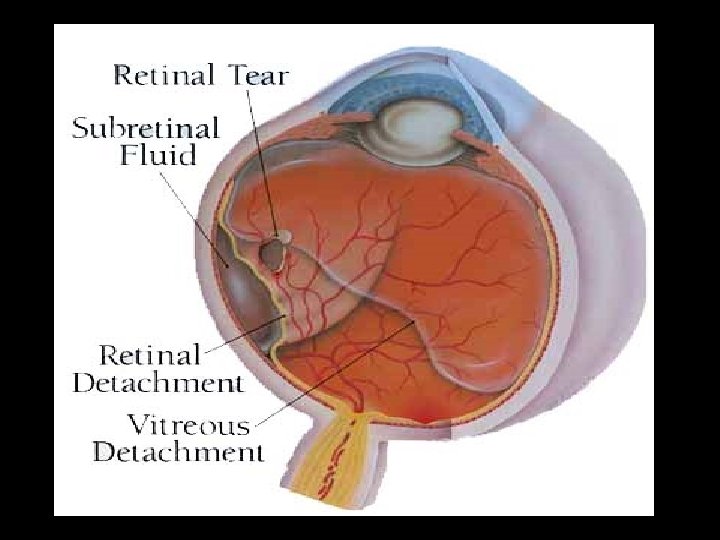
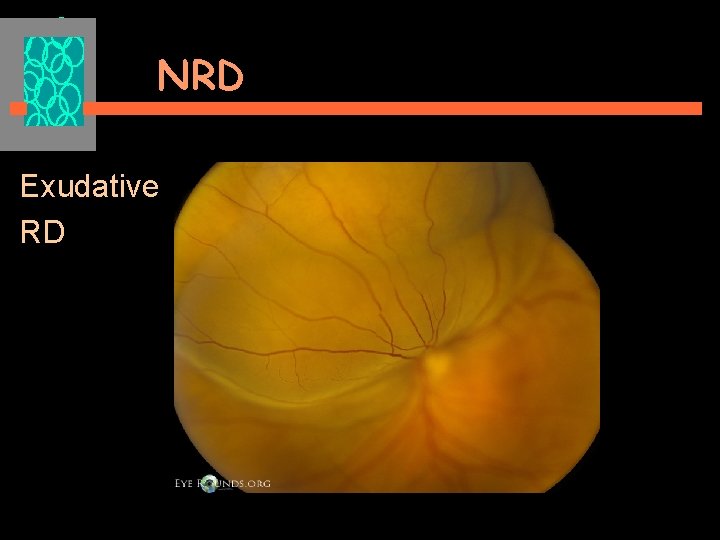
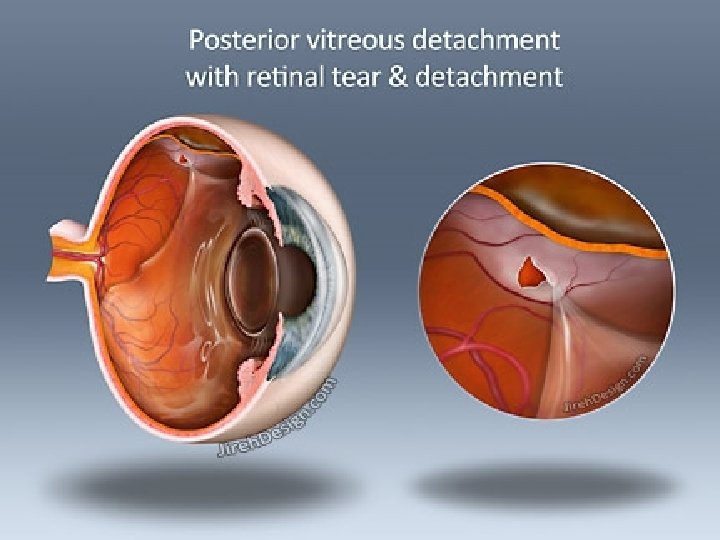
Definitions u RRD: RD secondary to a retinal break u NRD: RD without a retinal break u Exudative RD: RD where the detachment is secondary to fluid that leaks from the vessels of the retina/ choroid u Tractional RD: RD due to retinal fibrosis and traction
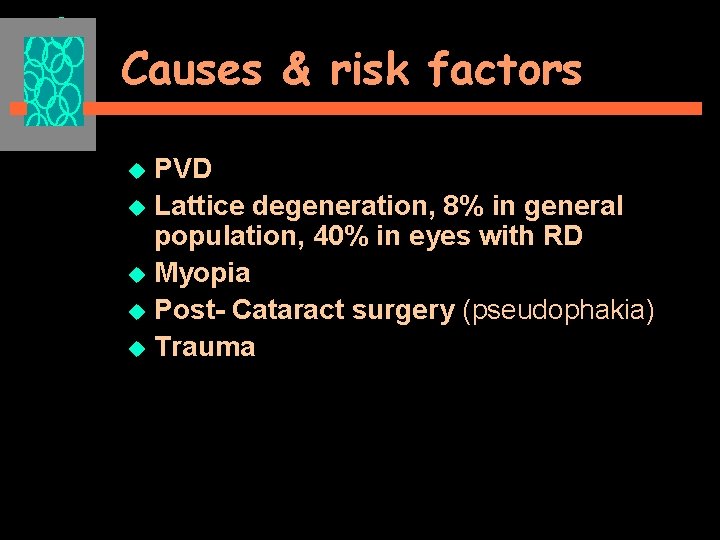
Epidemiology u 1 in 10, 000/ year u Bilateral in about 10% u Risk factors? u An ophthalmic emergency
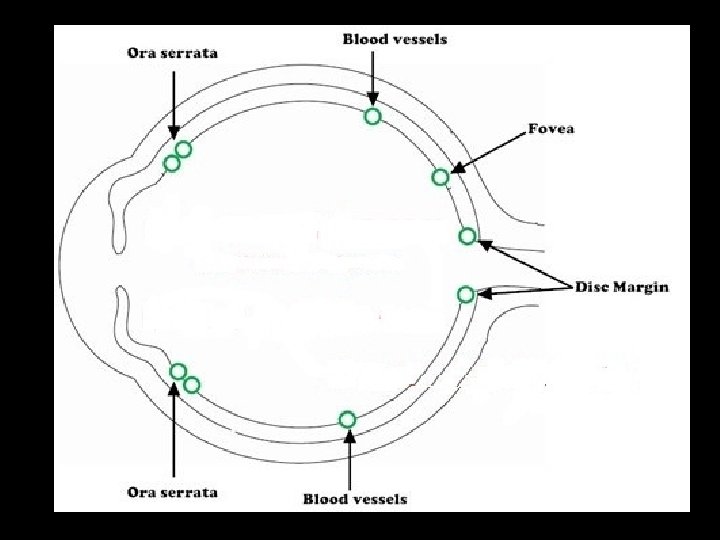
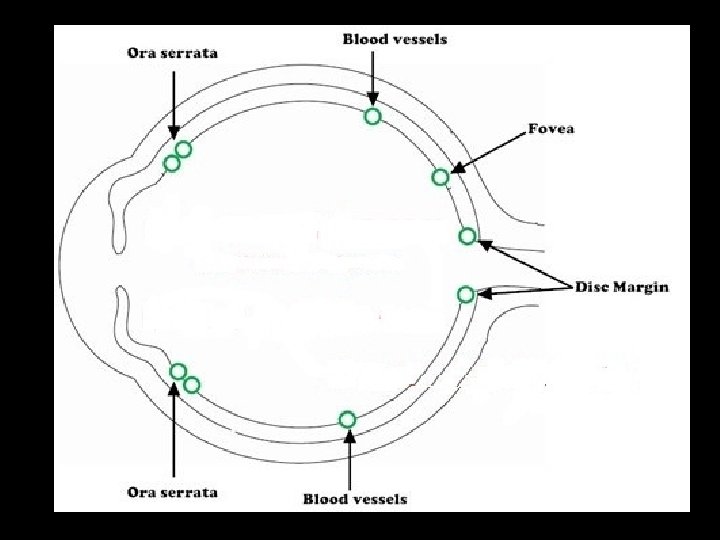
RRD Some Anatomical Considerations u Vitreo-retinal adhesions disc, ora, blood vessels & at fovea u Potential subretinal space
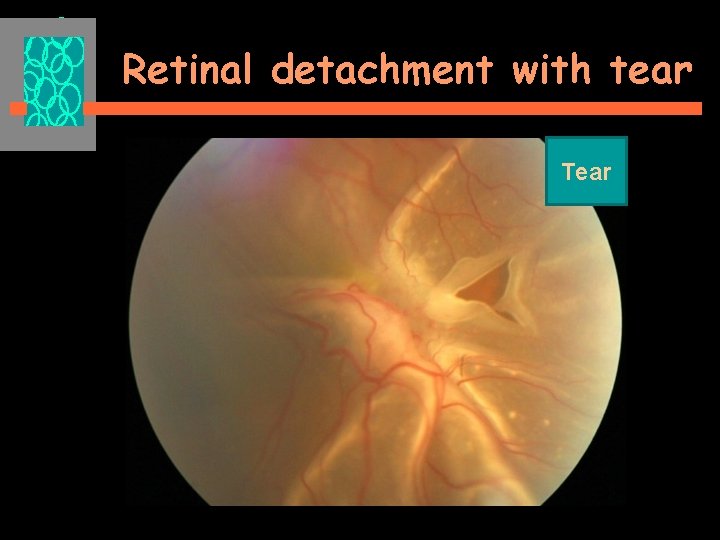
RRD RD secondary to a break in the retina
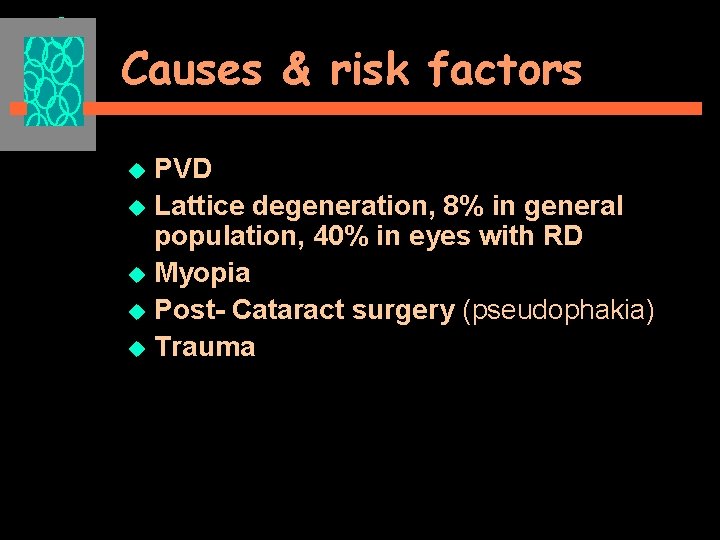
Causes & risk factors PVD u Lattice degeneration, 8% in general population, 40% in eyes with RD u Myopia u Post- Cataract surgery (pseudophakia) u Trauma u
Clinical presentation –symptoms u Flashes of light u Floaters u Visual loss u Visual field loss u Usually an acute event u History of predisposing factors, myopia, cataract surgery, trauma etc
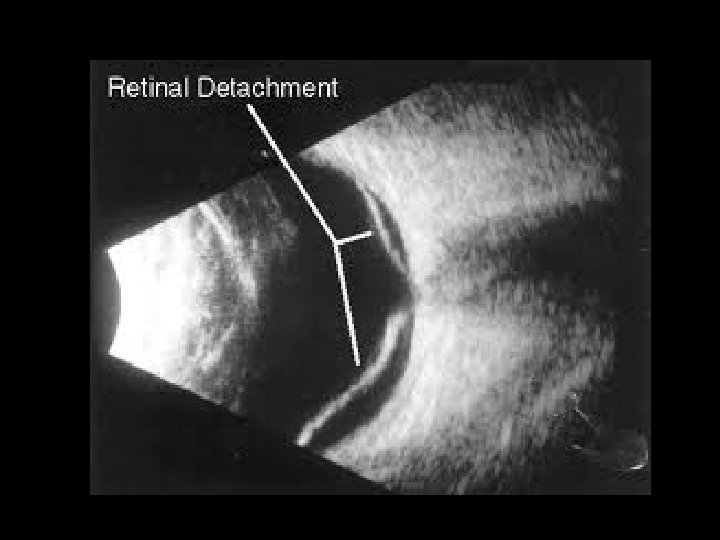
Clinical examination –signs Reduced Visual acuity Anterior segment examination Pupils, (RAPD) Posterior segment examination Vitreous- tobacco dust Retinal signs IOP ( may be low)
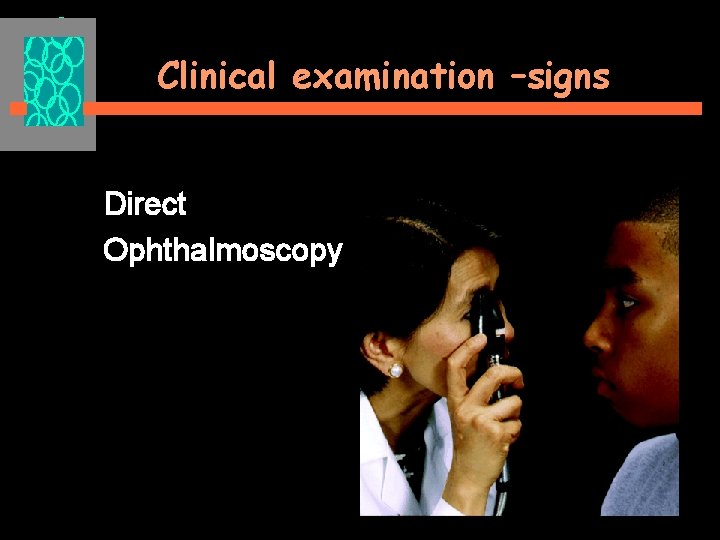
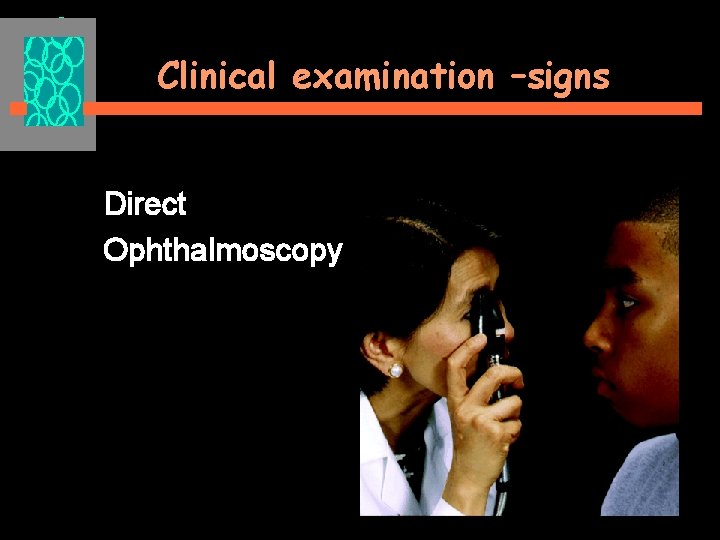
Clinical examination –signs Direct Ophthalmoscopy
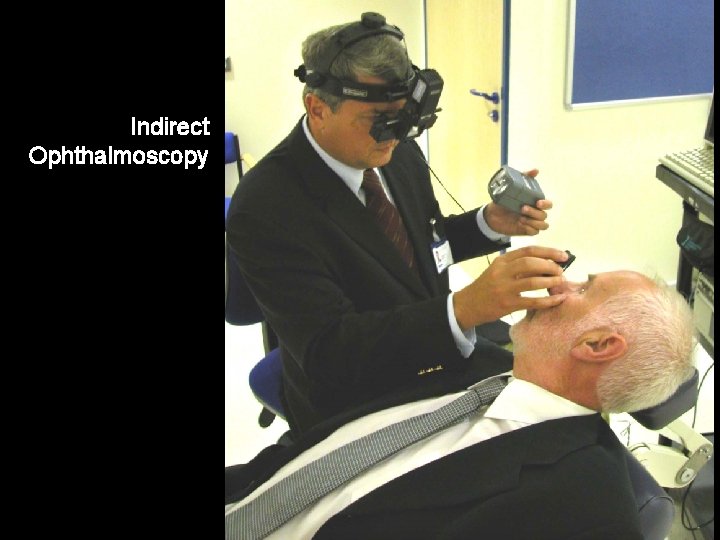
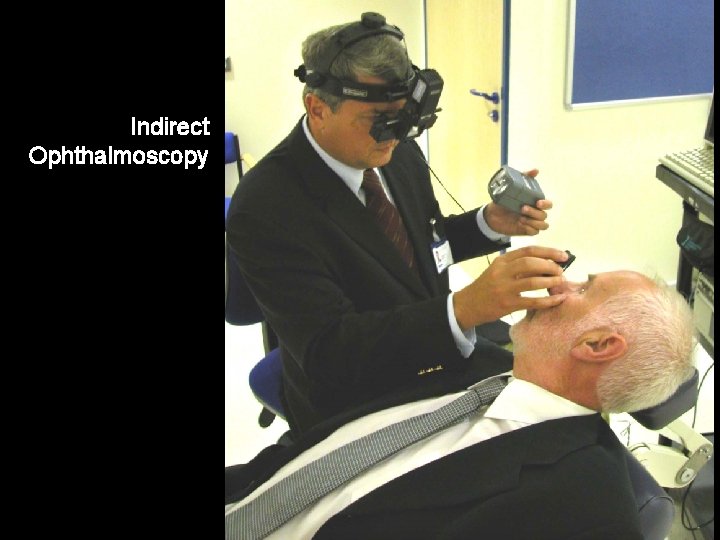
Indirect Ophthalmoscopy
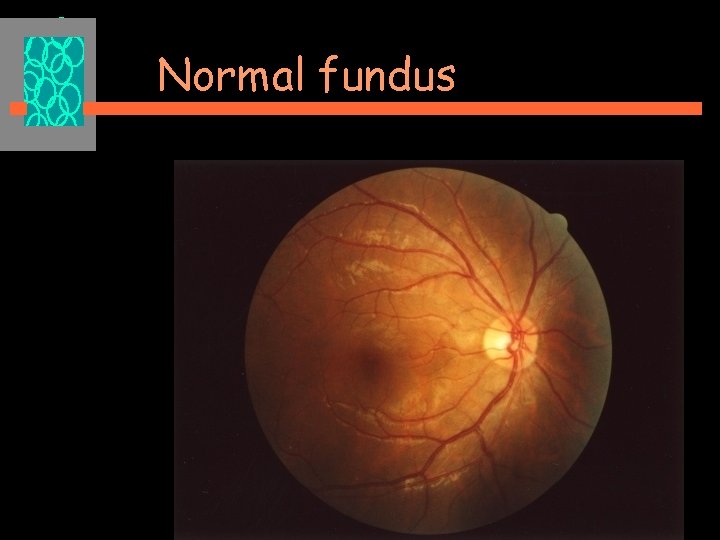
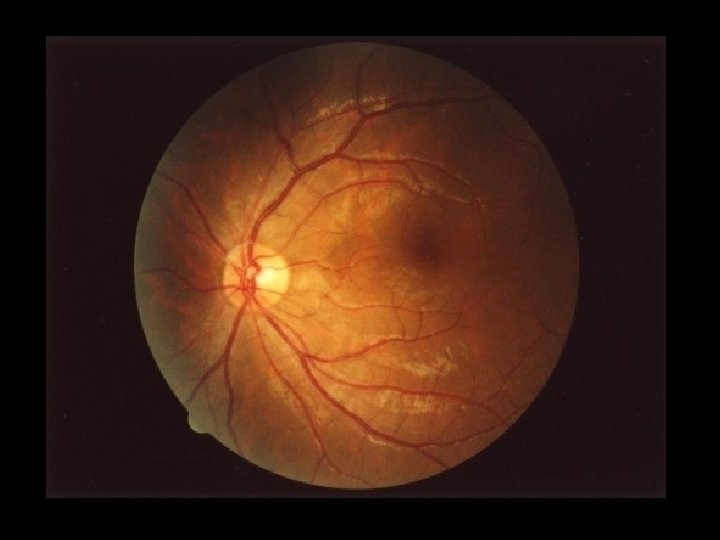
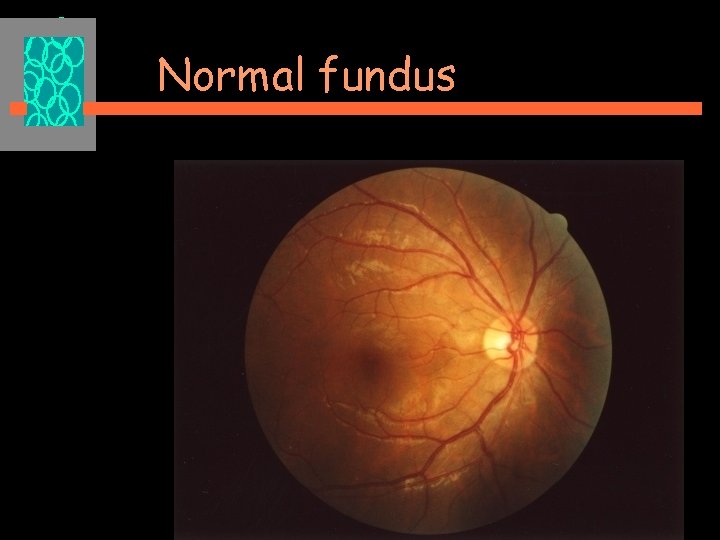
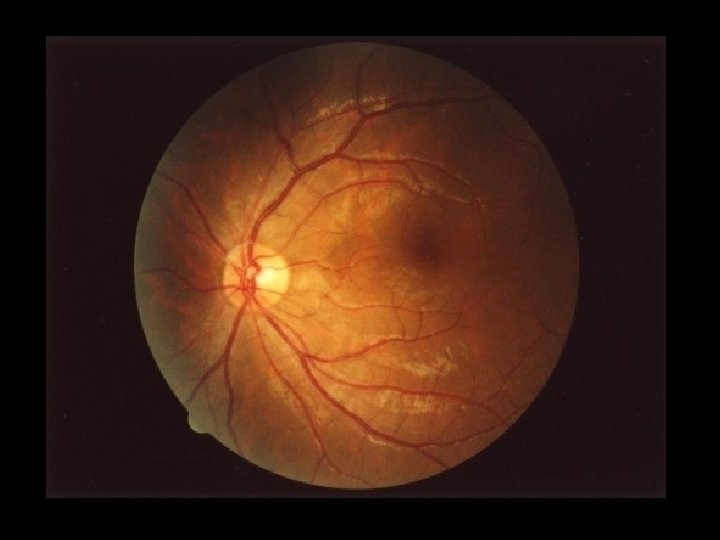
Normal fundus
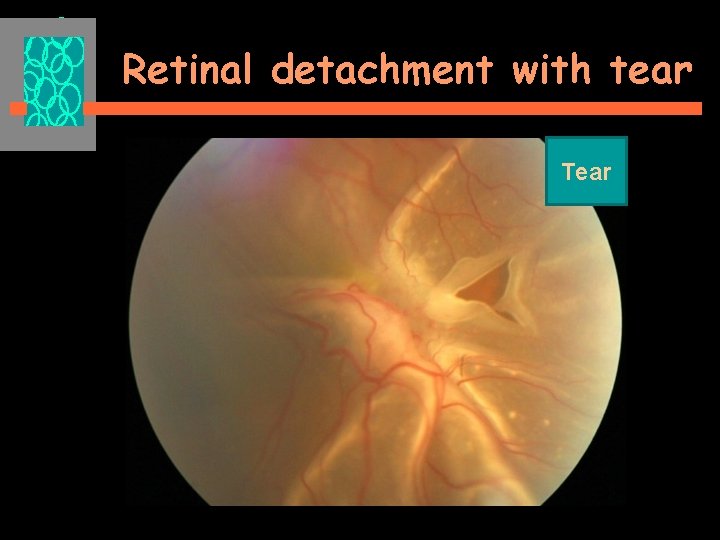
Retinal detachment with tear Tear
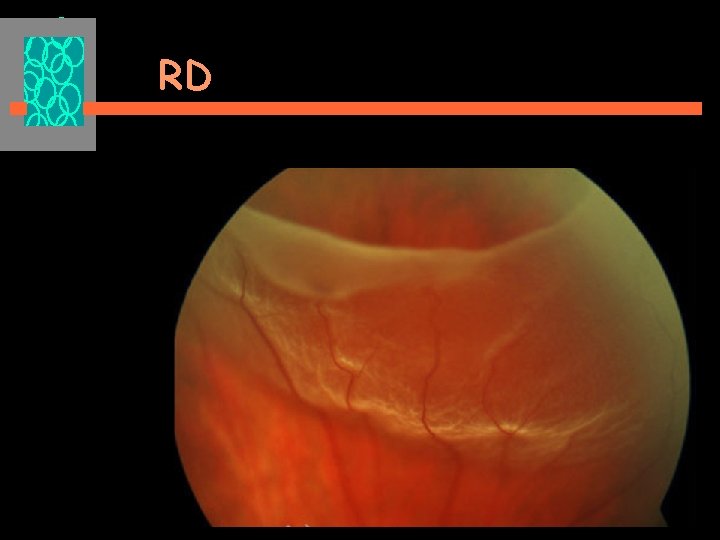
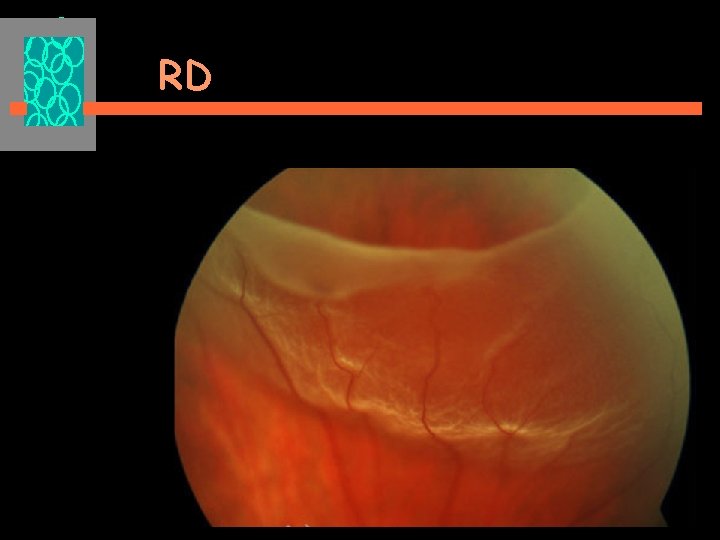
RD
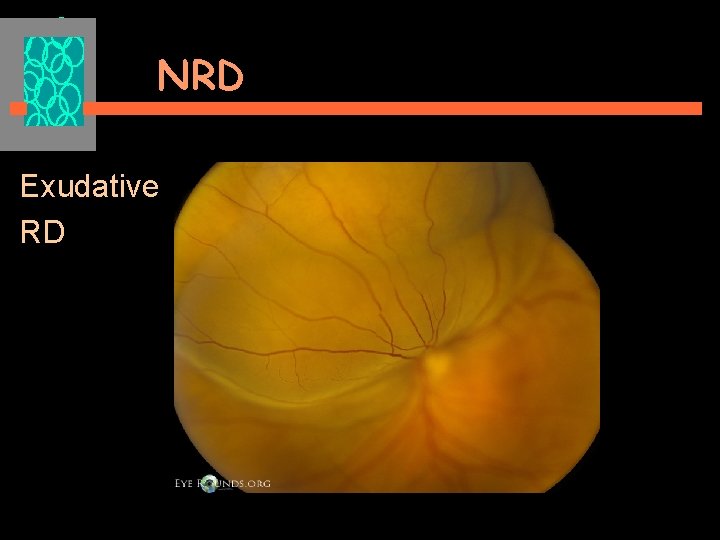
NRD Exudative RD

Exudative RD
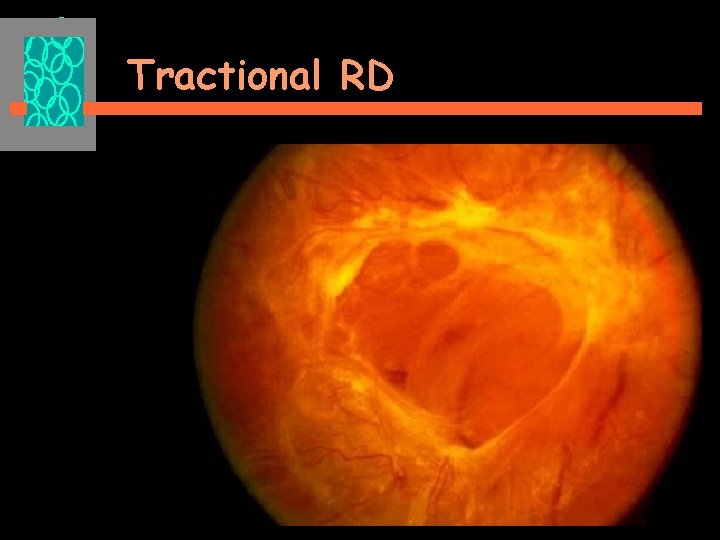
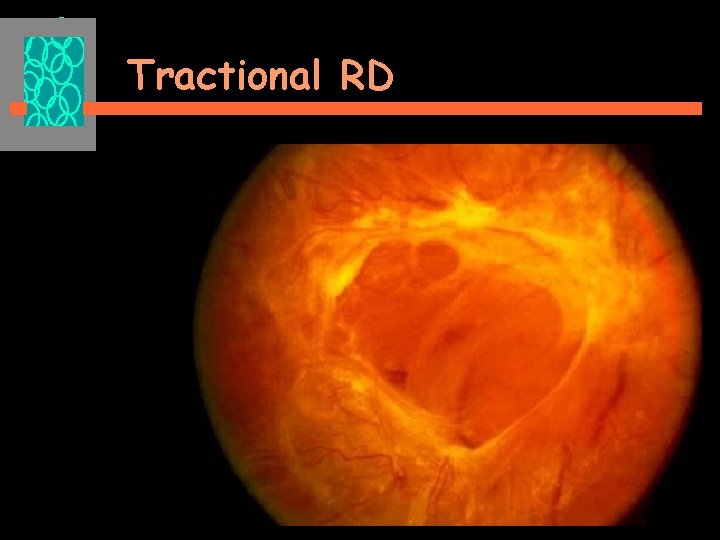
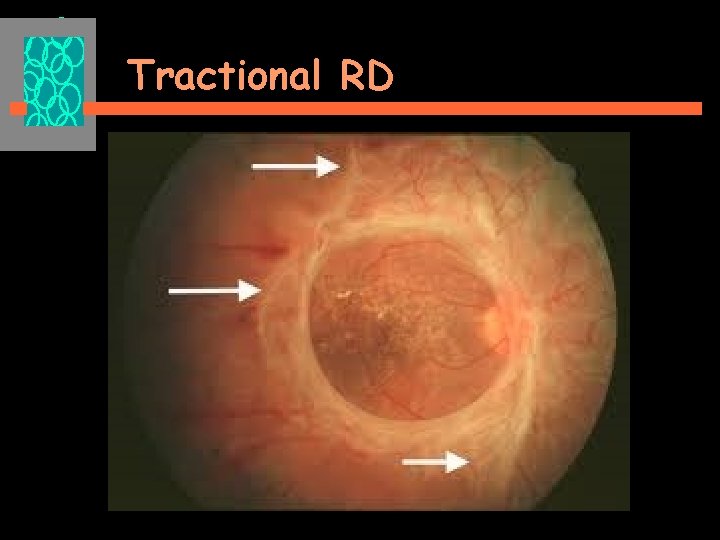
Tractional RD
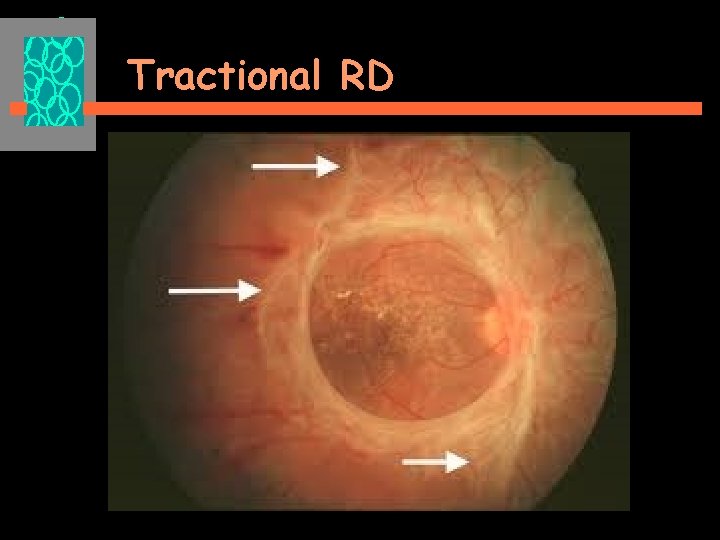
Tractional RD
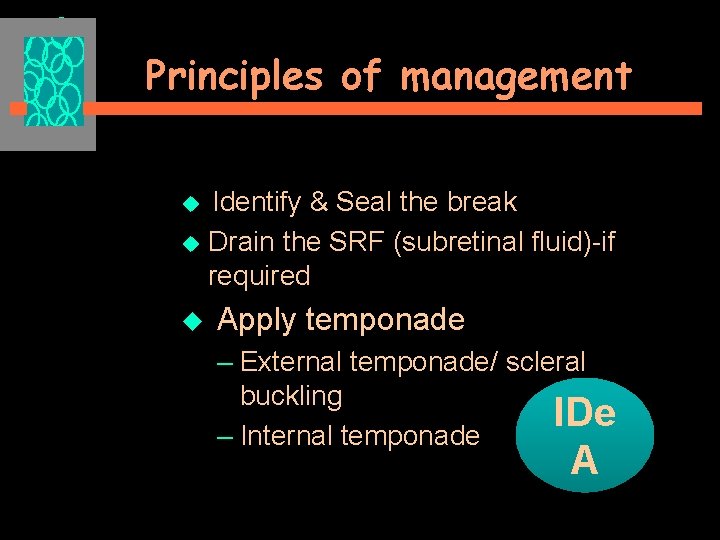
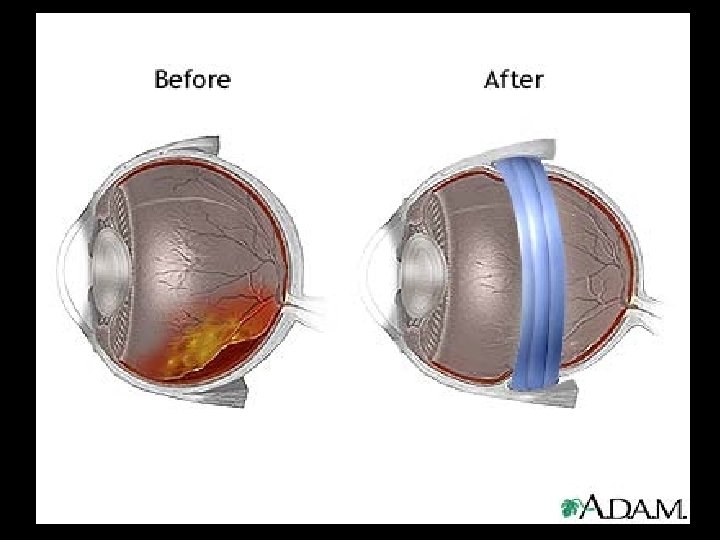
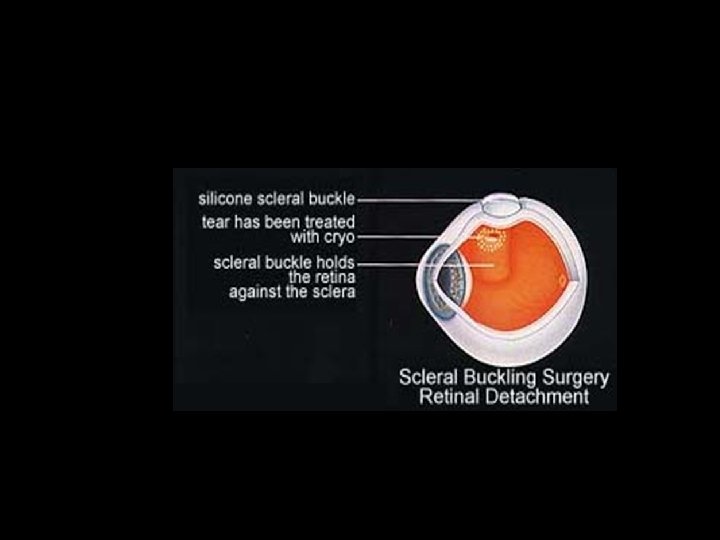
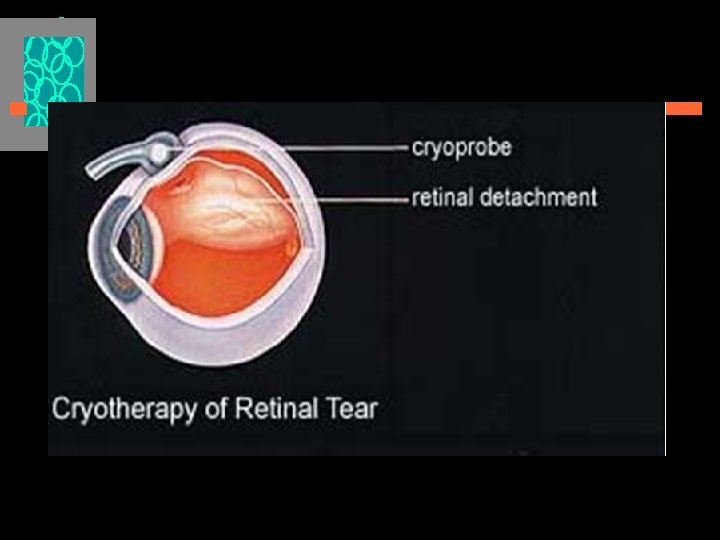
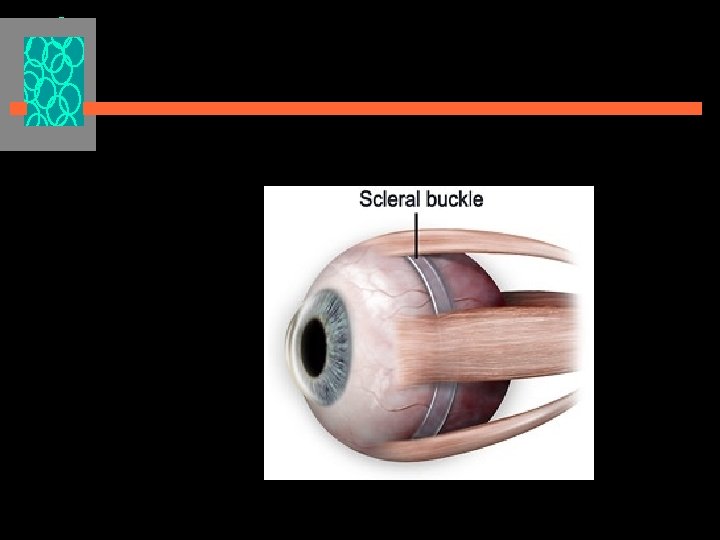
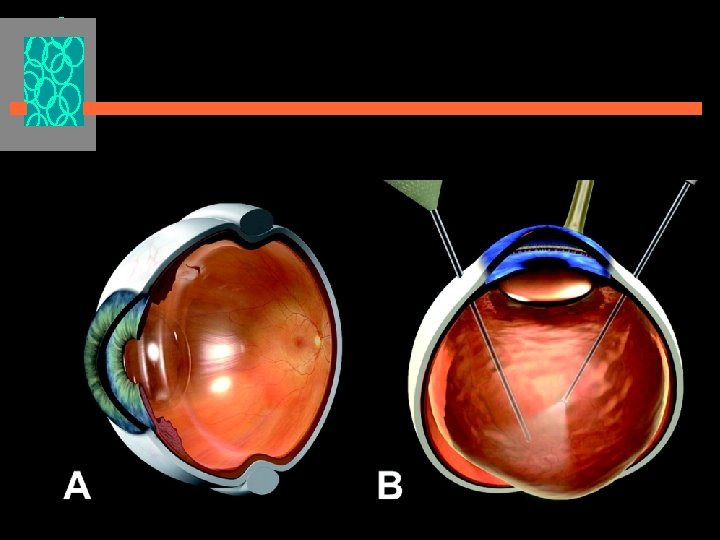
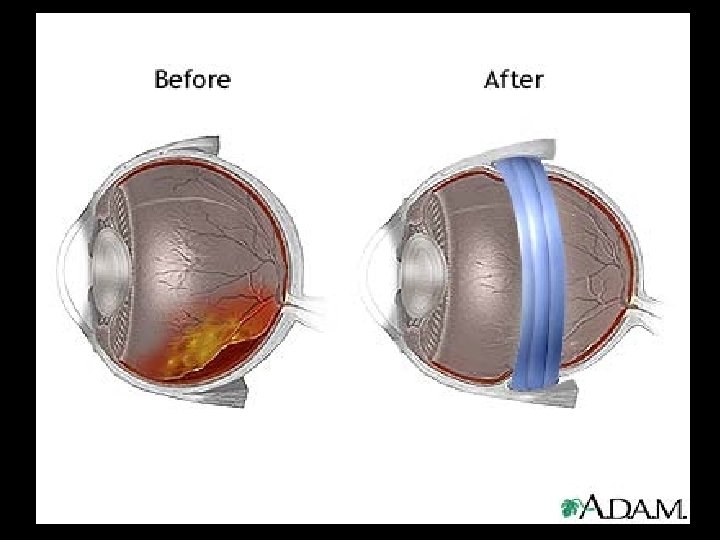
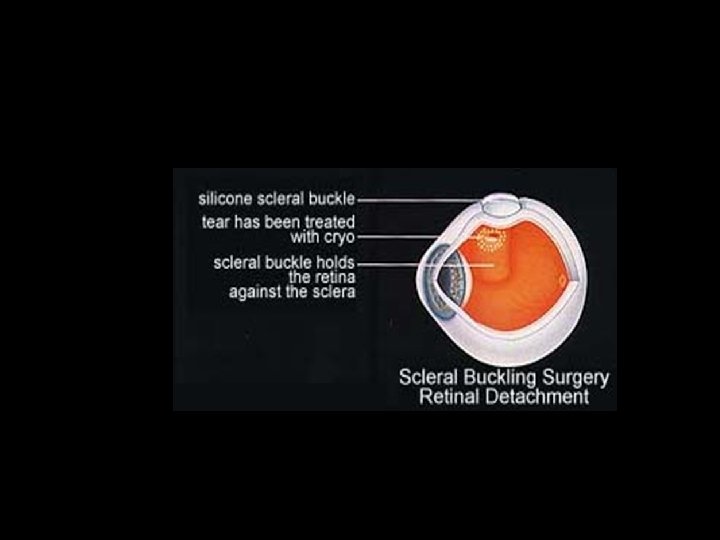
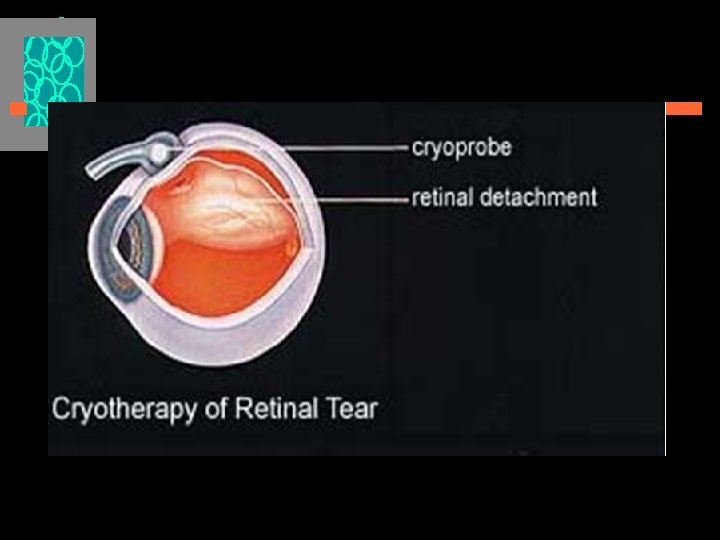
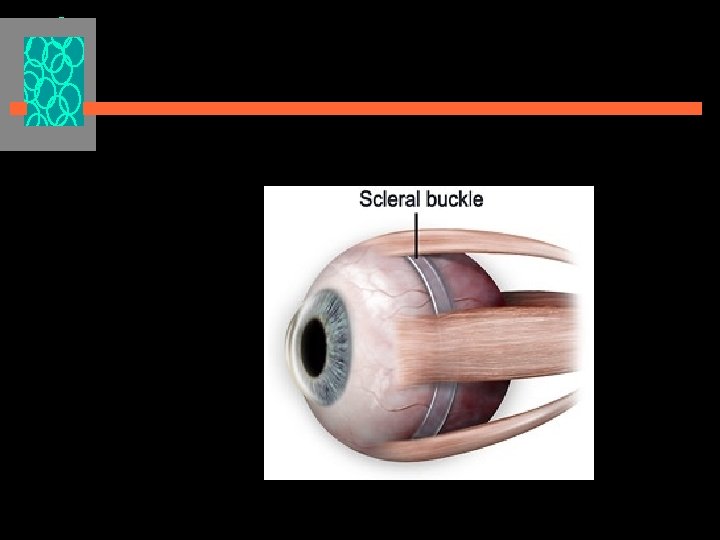
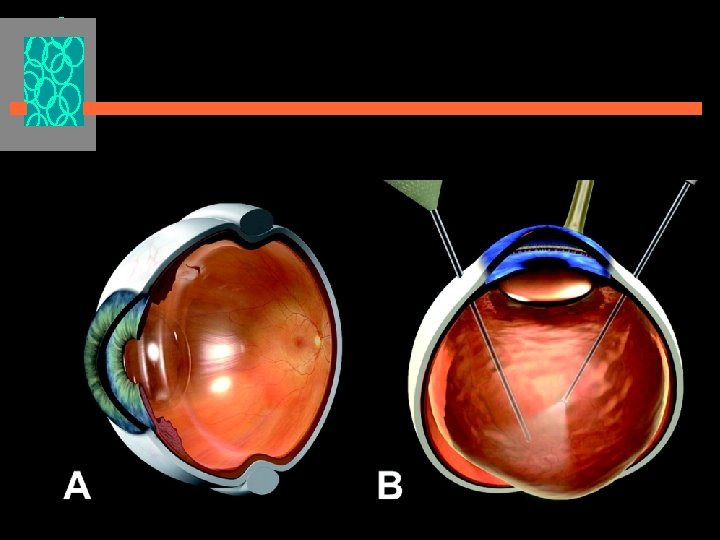
Principles of management u Identify & Seal the break u Drain the SRF (subretinal fluid)-if required u Apply temponade – External temponade/ scleral buckling IDe – Internal temponade A
Prophylaxis of RRD u Photocoagulation of the risky lesions with laser u So patients with risk factors should be referred to an ophthalmologist
Announcements u HW Three common causes of exudative retinal detachment