Vive Le PHM Revolution Andi Orlowski Deputy Director











- Slides: 30

Vive Le PHM Revolution! Andi Orlowski Deputy Director of Business Intelligence at Imperial Health Partners Senior Population Health Analytics Advisor to NHS England
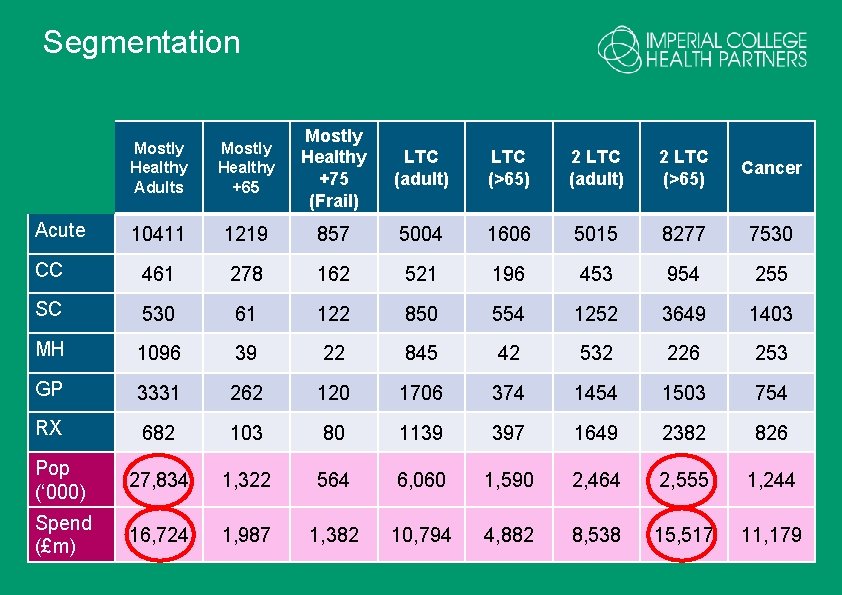
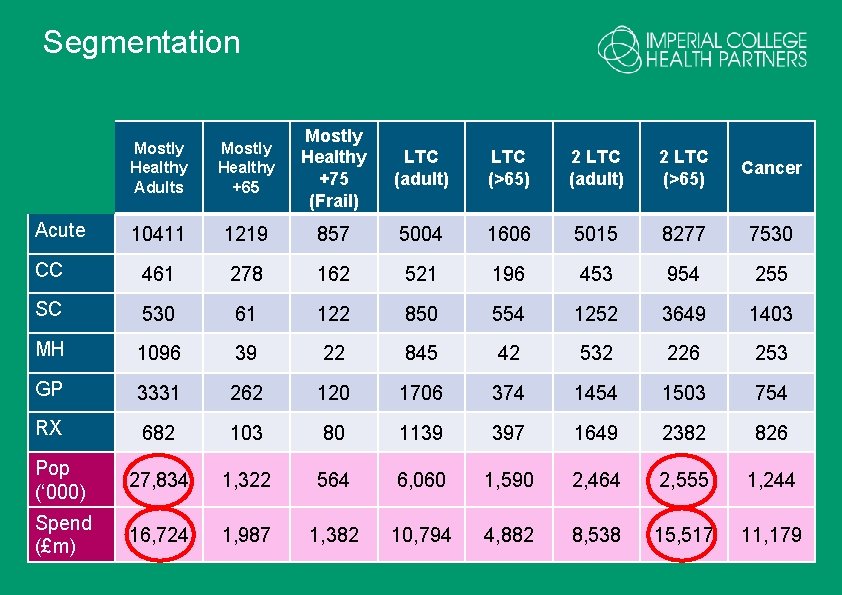
Segmentation Mostly Healthy Adults Mostly Healthy +65 Mostly Healthy +75 (Frail) LTC (adult) LTC (>65) 2 LTC (adult) 2 LTC (>65) Cancer 10411 1219 857 5004 1606 5015 8277 7530 CC 461 278 162 521 196 453 954 255 SC 530 61 122 850 554 1252 3649 1403 MH 1096 39 22 845 42 532 226 253 GP 3331 262 120 1706 374 1454 1503 754 RX 682 103 80 1139 397 1649 2382 826 Pop (‘ 000) 27, 834 1, 322 564 6, 060 1, 590 2, 464 2, 555 1, 244 Spend (£m) 16, 724 1, 987 1, 382 10, 794 4, 882 8, 538 15, 517 11, 179 Acute


Impactibility modelling Predicts which high-risk patients are most likely to be responsive to the preventive care intervention being offered. Approaches to impactibiliy modelling include: - Ambulatory Care–Sensitive Conditions - Gap analysis - Excluding patients unlikely to respond* - Impactible moments - Risking risk/deteriorating patient
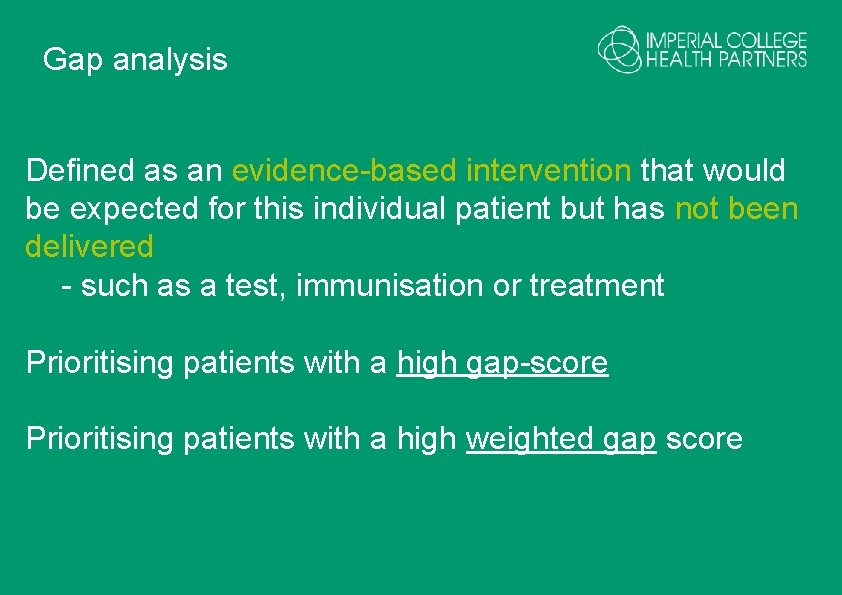
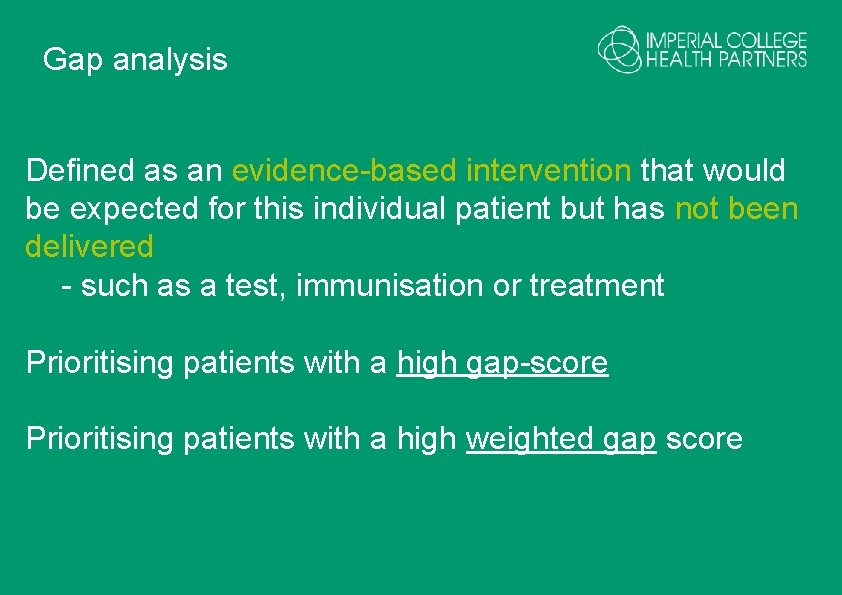
Gap analysis Defined as an evidence-based intervention that would be expected for this individual patient but has not been delivered - such as a test, immunisation or treatment Prioritising patients with a high gap-score Prioritising patients with a high weighted gap score
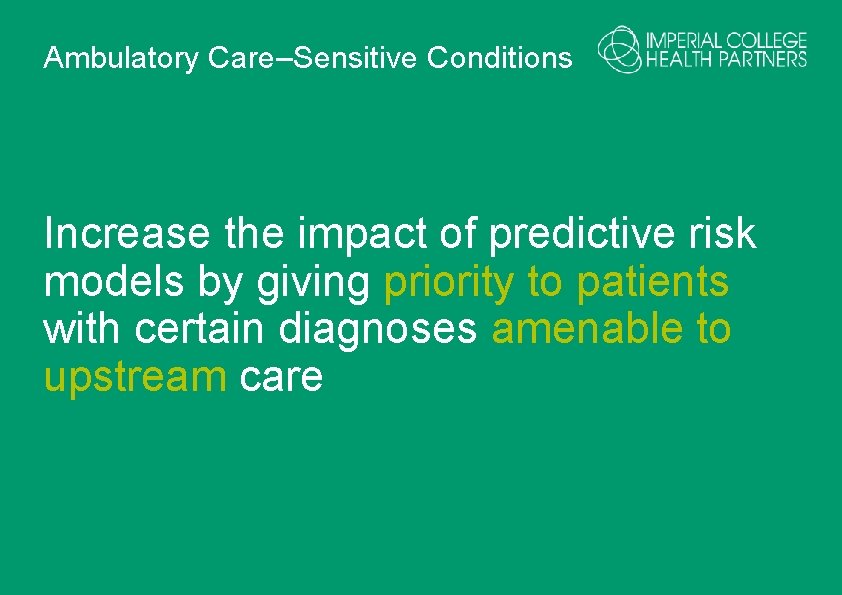
Ambulatory Care–Sensitive Conditions Increase the impact of predictive risk models by giving priority to patients with certain diagnoses amenable to upstream care
De-prioritise/excluding patients with • stable characteristics (e. g. expensive, longterm drug) • extremely high risk e. g. in the top strata • characteristics (psychosis, language barrier) • NOT a recommended technique but useful to compare • or use this method to help address inequalities

Impactable moments • (e. g. post discharge from hospital) Rising risk score • (rate of change of risk score) Patient Activation Measure • e. g. how ready people are for healthcare
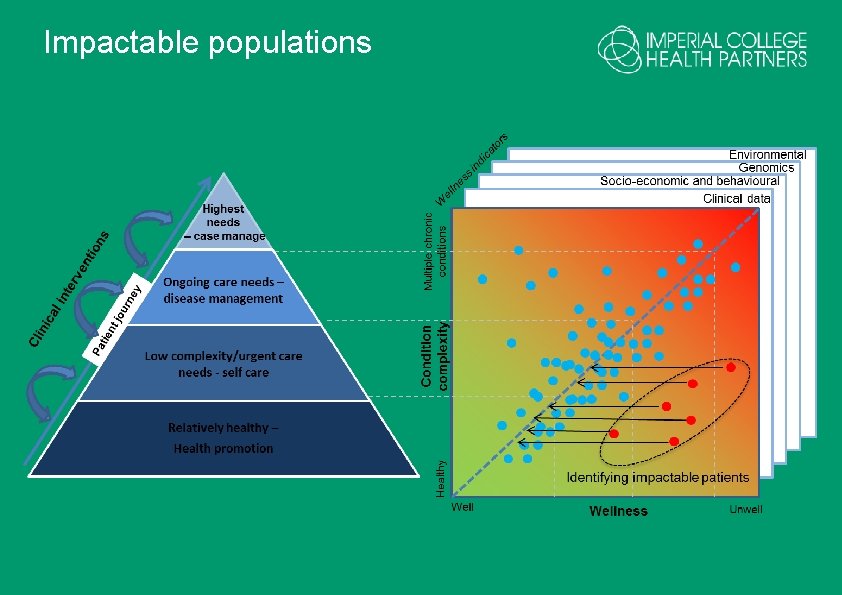
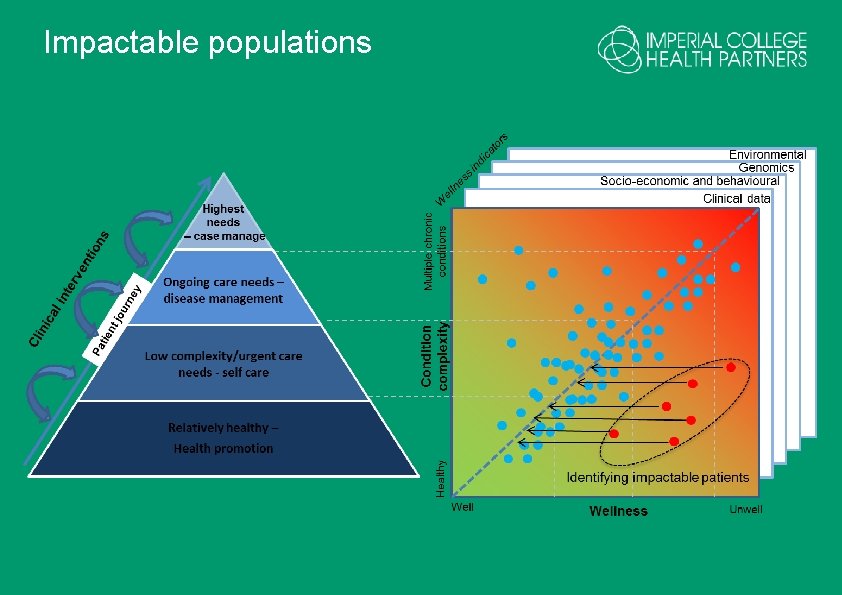
Impactable populations

Impactibility
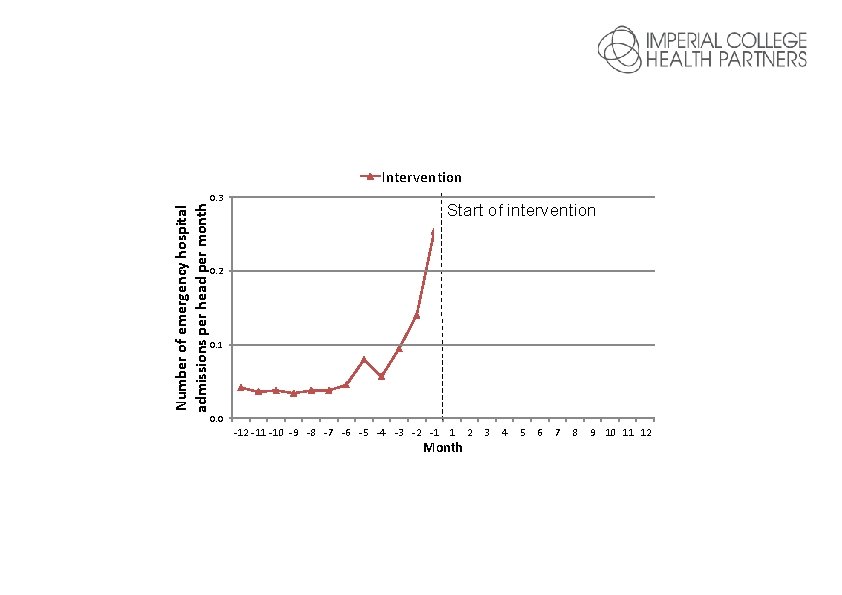
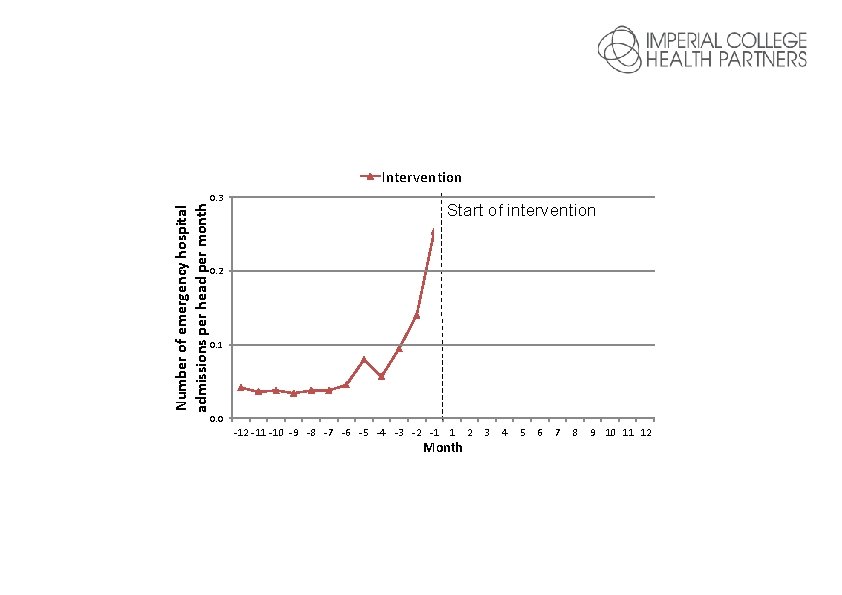
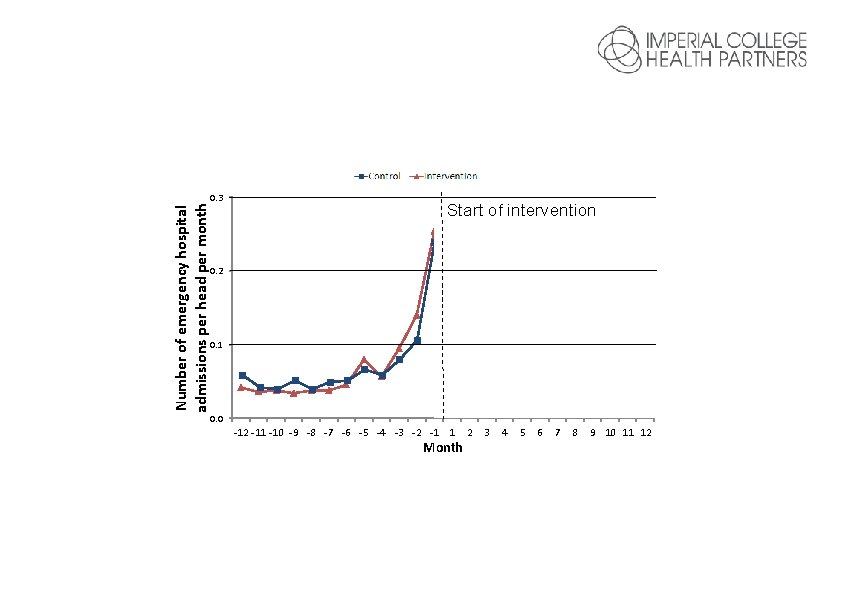
Number of emergency hospital admissions per head per month Intervention 0. 3 Start of intervention 0. 2 0. 1 0. 0 -12 -11 -10 -9 -8 -7 -6 -5 -4 -3 -2 -1 1 Month 2 3 4 5 6 7 8 9 10 11 12
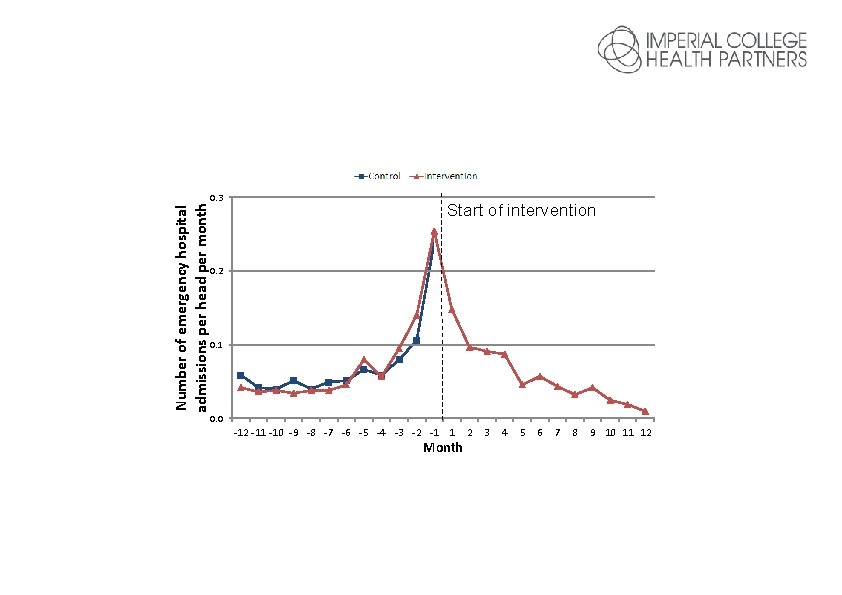
Number of emergency hospital admissions per head per month Intervention 0. 3 Start of intervention 0. 2 0. 1 0. 0 -12 -11 -10 -9 -8 -7 -6 -5 -4 -3 -2 -1 1 Month 2 3 4 5 6 7 8 9 10 11 12
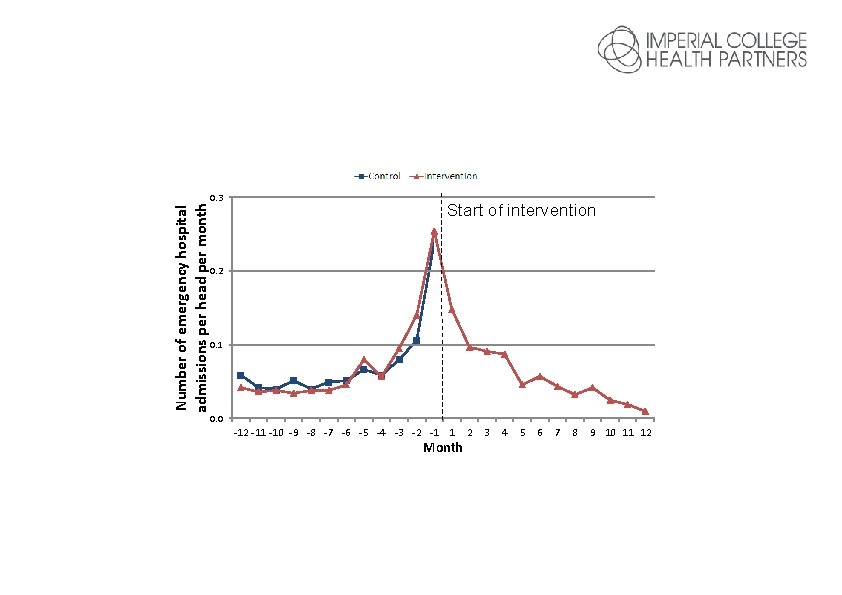
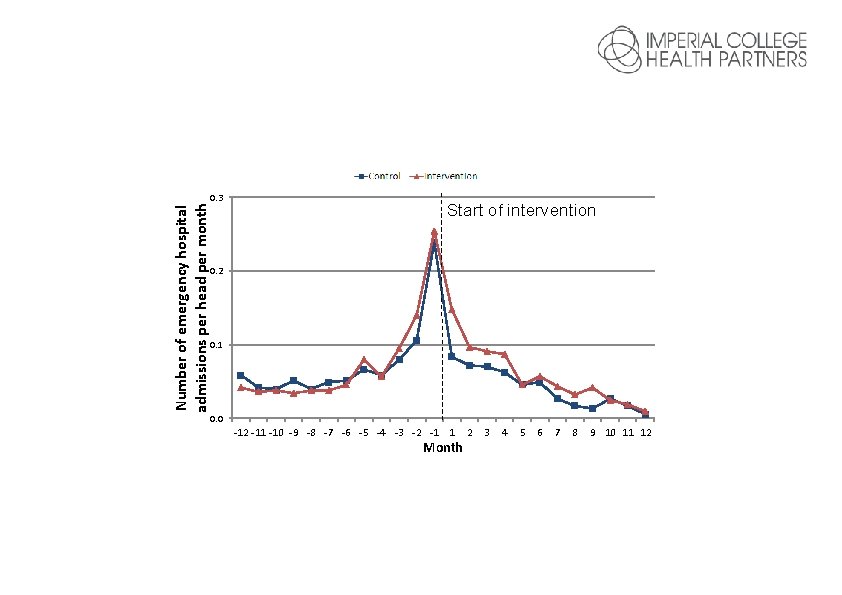
Number of emergency hospital admissions per head per month Intervention 0. 3 Start of intervention 0. 2 0. 1 0. 0 -12 -11 -10 -9 -8 -7 -6 -5 -4 -3 -2 -1 1 Month 2 3 4 5 6 7 8 9 10 11 12
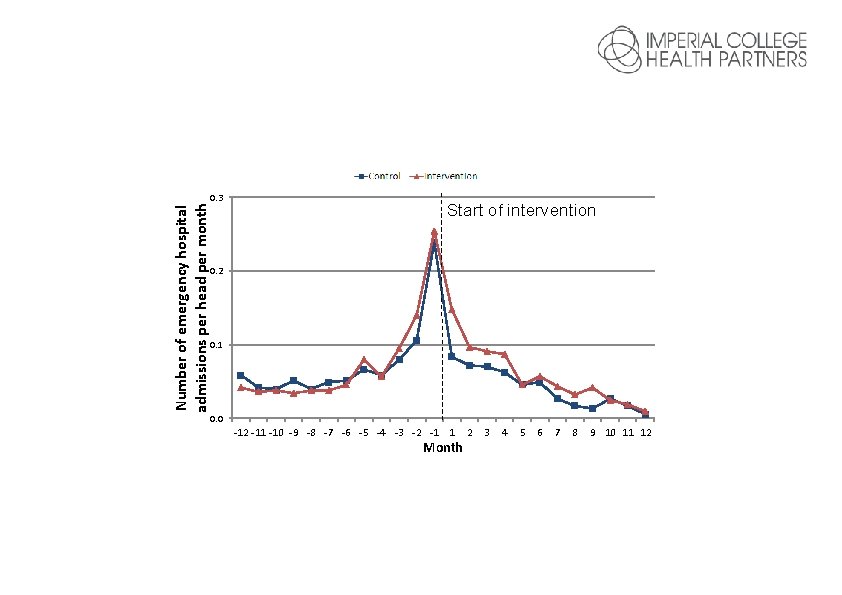
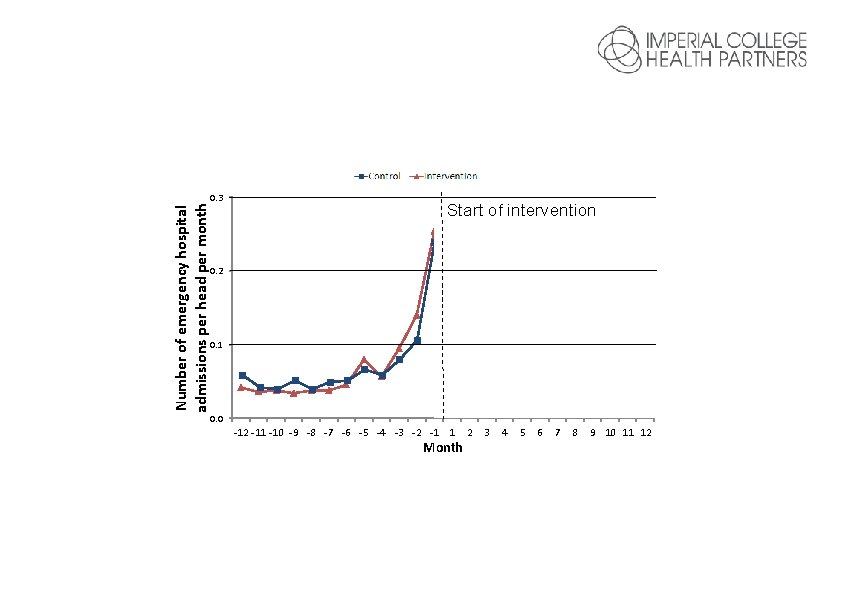
Number of emergency hospital admissions per head per month Control 0. 3 Intervention Start of intervention 0. 2 0. 1 0. 0 -12 -11 -10 -9 -8 -7 -6 -5 -4 -3 -2 -1 1 Month 2 3 4 5 6 7 8 9 10 11 12

The importance of using PHM to Improve value
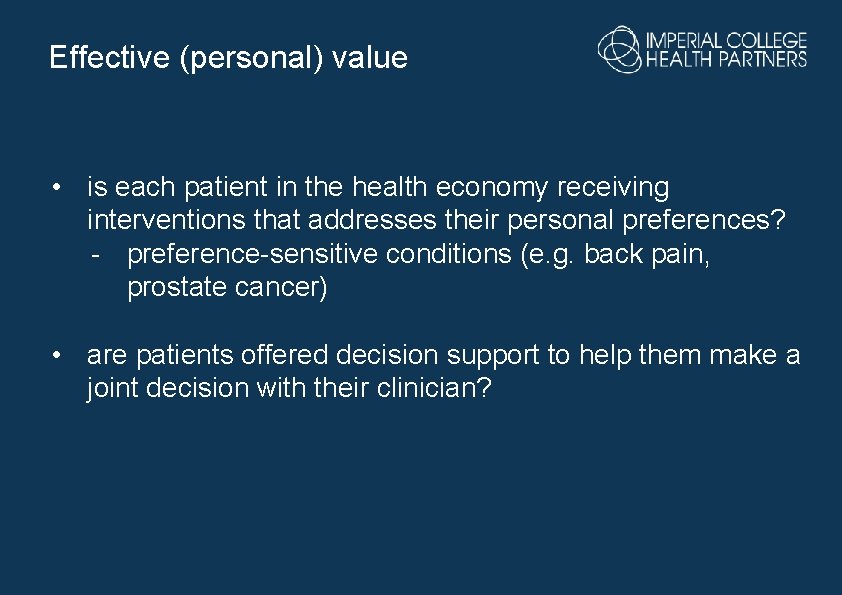
Effective (personal) value • is each patient in the health economy receiving interventions that addresses their personal preferences? - preference-sensitive conditions (e. g. back pain, prostate cancer) • are patients offered decision support to help them make a joint decision with their clinician?
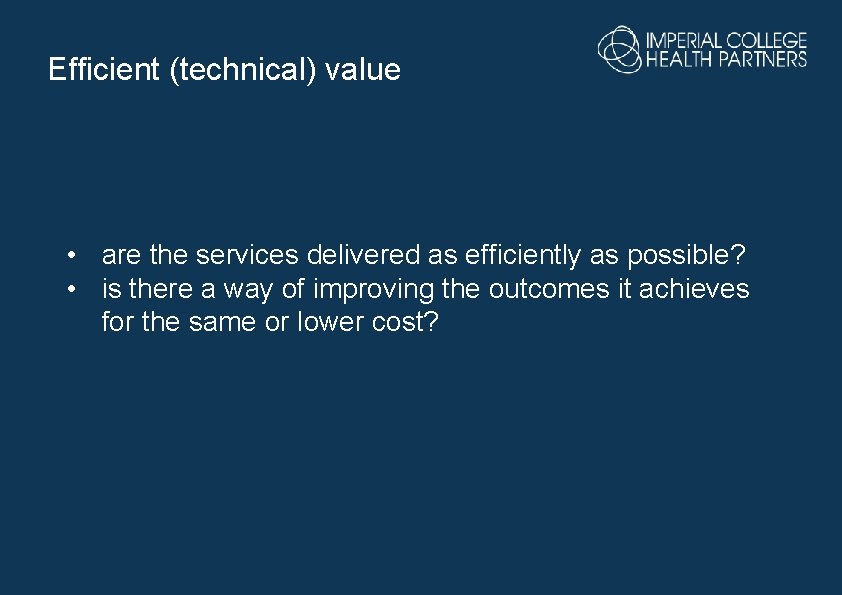
Efficient (technical) value • are the services delivered as efficiently as possible? • is there a way of improving the outcomes it achieves for the same or lower cost?
Population (allocative) value • is the health economy investing in the right mix of services to address the needs of its population? - between services - within services
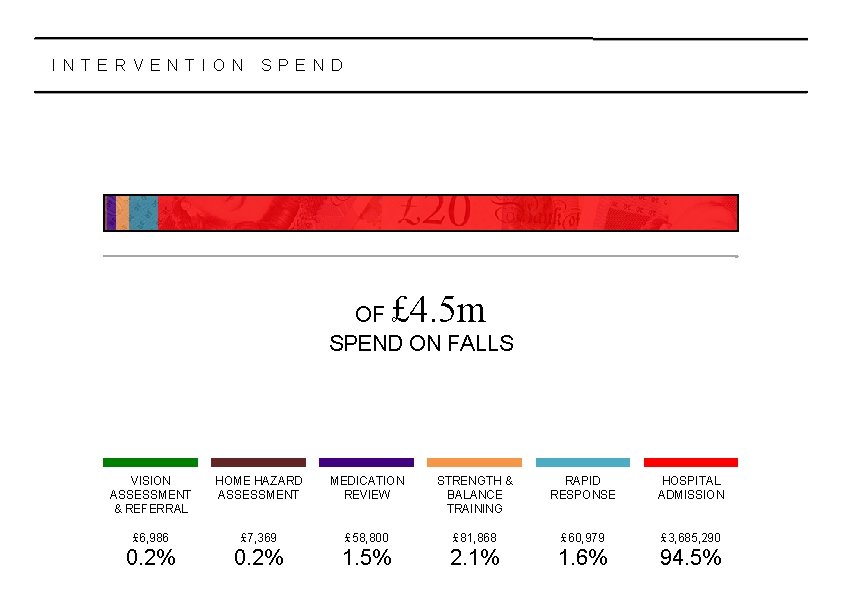
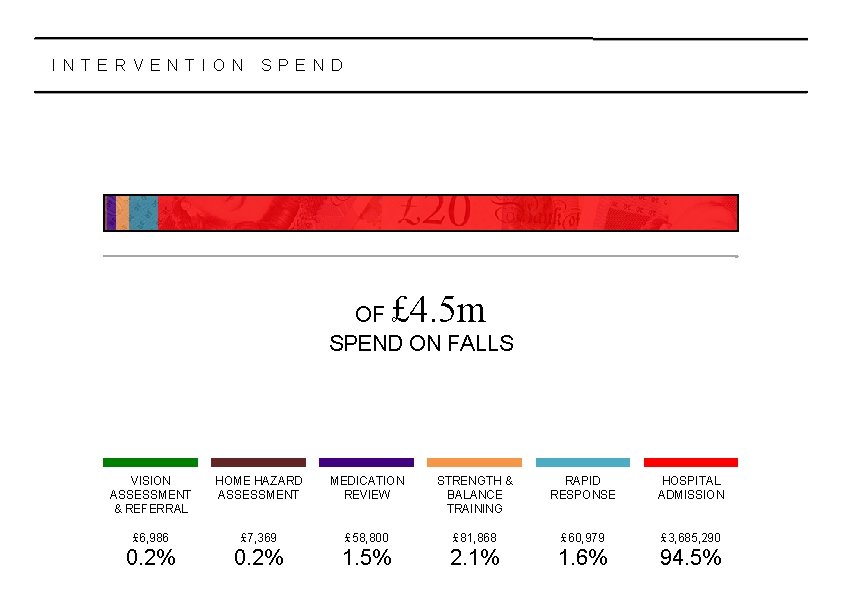
I N T E R V E N T I O N S P E N D £ 4. 5 m OF SPEND ON FALLS VISION ASSESSMENT & REFERRAL HOME HAZARD ASSESSMENT MEDICATION REVIEW STRENGTH & BALANCE TRAINING RAPID RESPONSE HOSPITAL ADMISSION £ 6, 986 £ 7, 369 £ 58, 800 £ 81, 868 £ 60, 979 £ 3, 685, 290 0. 2% 1. 5% 2. 1% 1. 6% 94. 5%
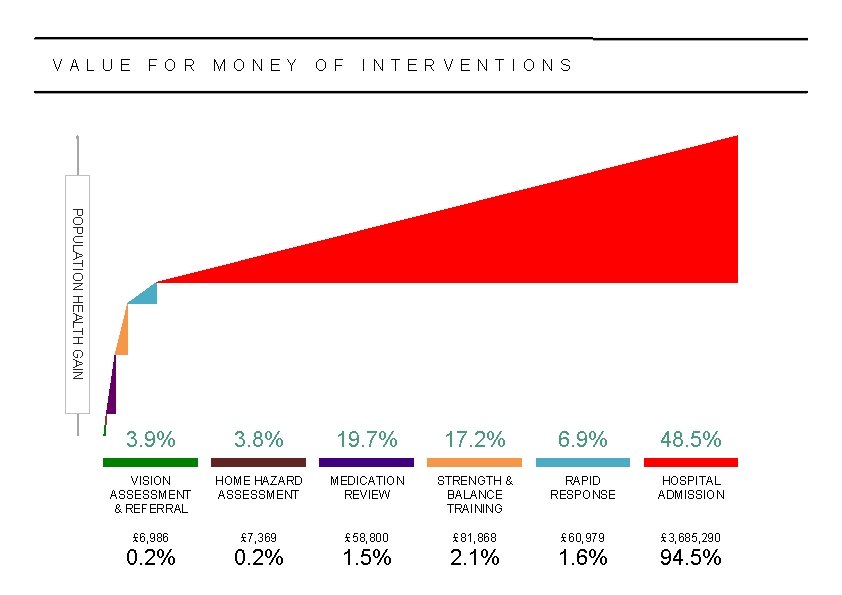
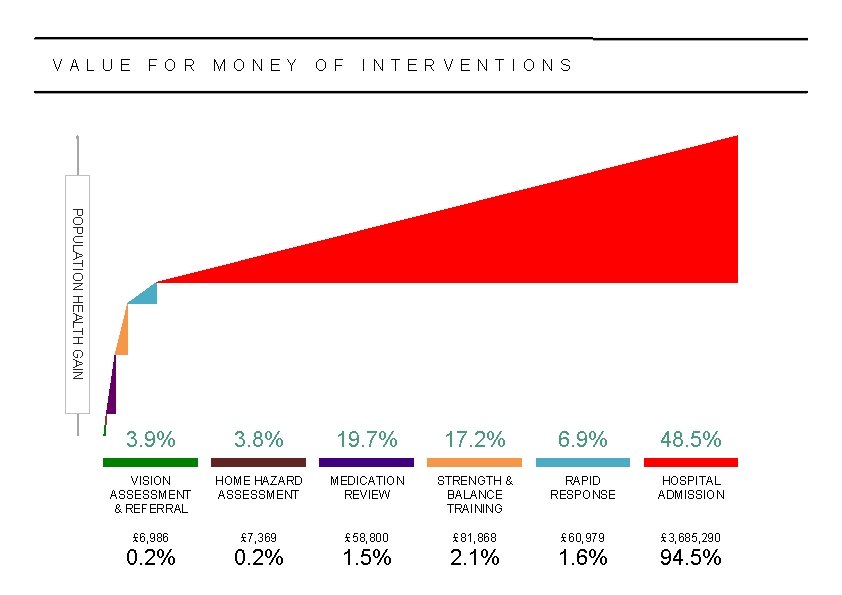
V A L U E F O R M O N E Y O F I N T E R V E N T I O N S POPULATION HEALTH GAIN 3. 9% 3. 8% 19. 7% 17. 2% 6. 9% 48. 5% VISION ASSESSMENT & REFERRAL HOME HAZARD ASSESSMENT MEDICATION REVIEW STRENGTH & BALANCE TRAINING RAPID RESPONSE HOSPITAL ADMISSION £ 6, 986 £ 7, 369 £ 58, 800 £ 81, 868 £ 60, 979 £ 3, 685, 290 0. 2% 1. 5% 2. 1% 1. 6% 94. 5%

H O W F A R D O E S A P O U N D G O VISION ASSESSMENT & REFERRAL 14 HOURS HOME HAZARD ASSESSMENT 13 HOURS MEDICATION REVIEW 8 HOURS 24 MINS STRENGTH & BALANCE TRAINING 5 HOURS 18 MINS RAPID RESPONSE 2 HOURS 48 MINS HOSPITAL ADMISSION 18 MINS This chart tells us how much ‘quality-adjusted life time’ we get from every intervention for every pound spent.



Targeted interventions
Clinical considerations Three major clinical complications of diabetes were identified by Nottinghamshire ICS as being of particular interest: • Amputations • Vision loss • Chronic kidney disease
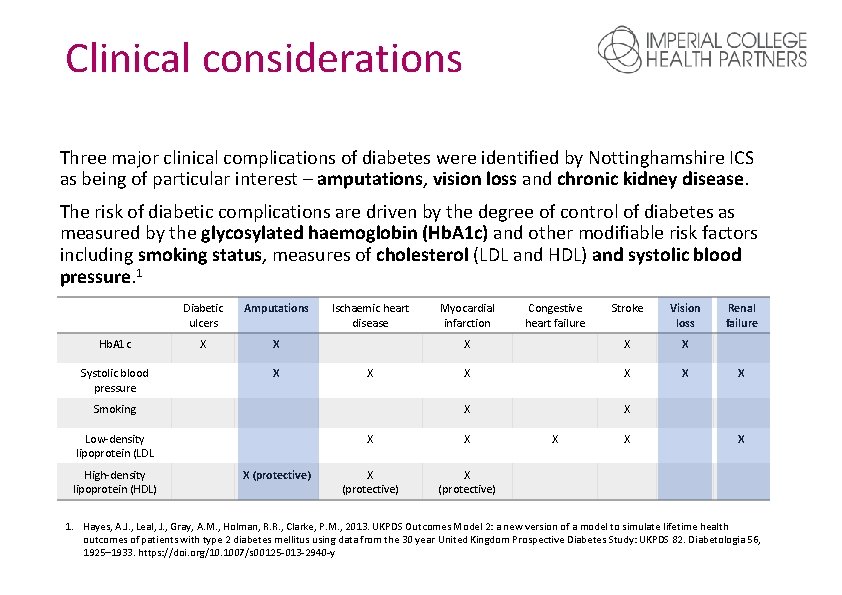
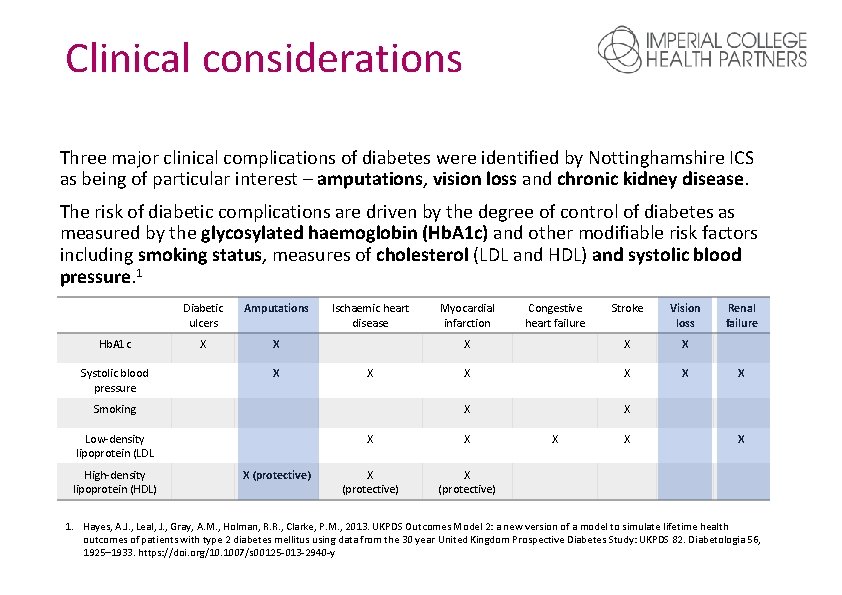
Clinical considerations Three major clinical complications of diabetes were identified by Nottinghamshire ICS as being of particular interest – amputations, vision loss and chronic kidney disease. The risk of diabetic complications are driven by the degree of control of diabetes as measured by the glycosylated haemoglobin (Hb. A 1 c) and other modifiable risk factors including smoking status, measures of cholesterol (LDL and HDL) and systolic blood pressure. 1 Hb. A 1 c Systolic blood pressure Diabetic ulcers Amputations X X X Ischaemic heart disease X Smoking Low-density lipoprotein (LDL High-density lipoprotein (HDL) X (protective) Myocardial infarction Stroke Vision loss X X X (protective) Congestive heart failure X X Renal failure X X 1. Hayes, A. J. , Leal, J. , Gray, A. M. , Holman, R. R. , Clarke, P. M. , 2013. UKPDS Outcomes Model 2: a new version of a model to simulate lifetime health outcomes of patients with type 2 diabetes mellitus using data from the 30 year United Kingdom Prospective Diabetes Study: UKPDS 82. Diabetologia 56, 1925– 1933. https: //doi. org/10. 1007/s 00125 -013 -2940 -y
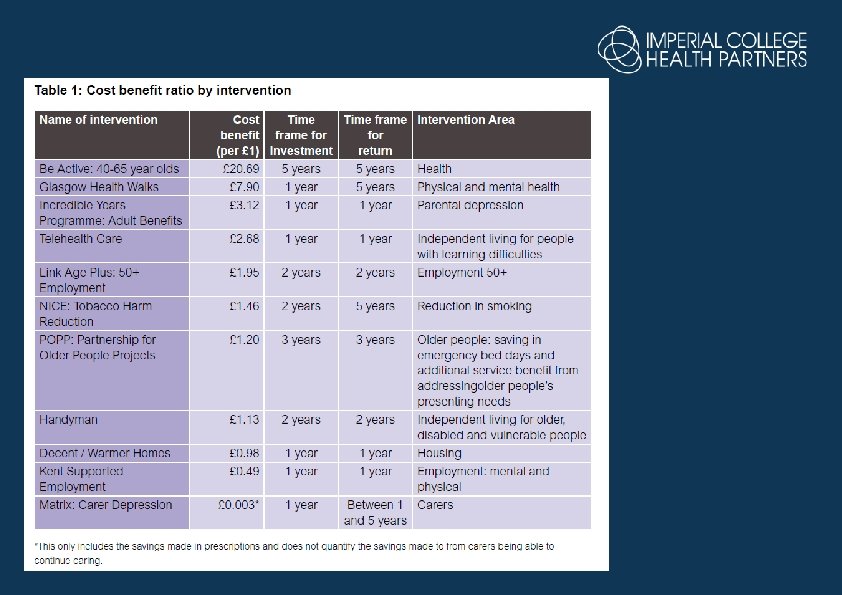
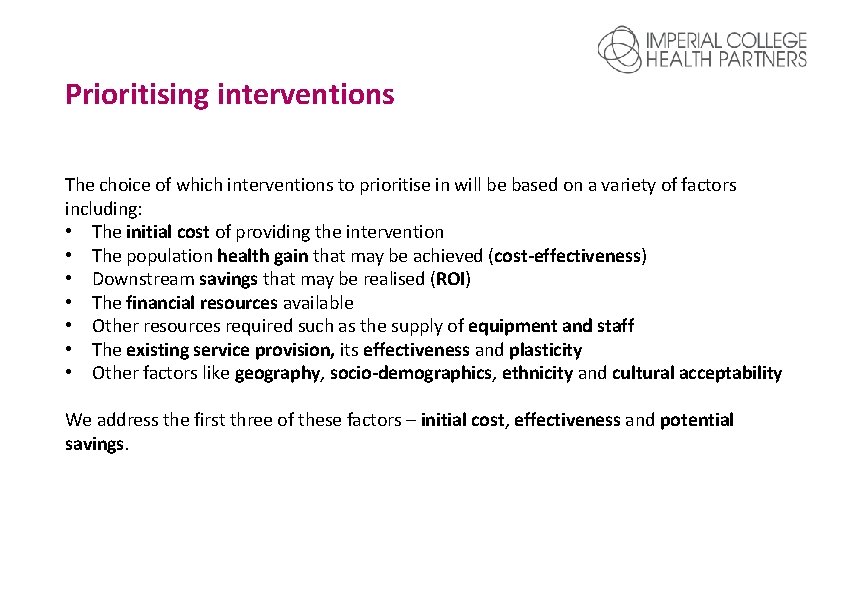
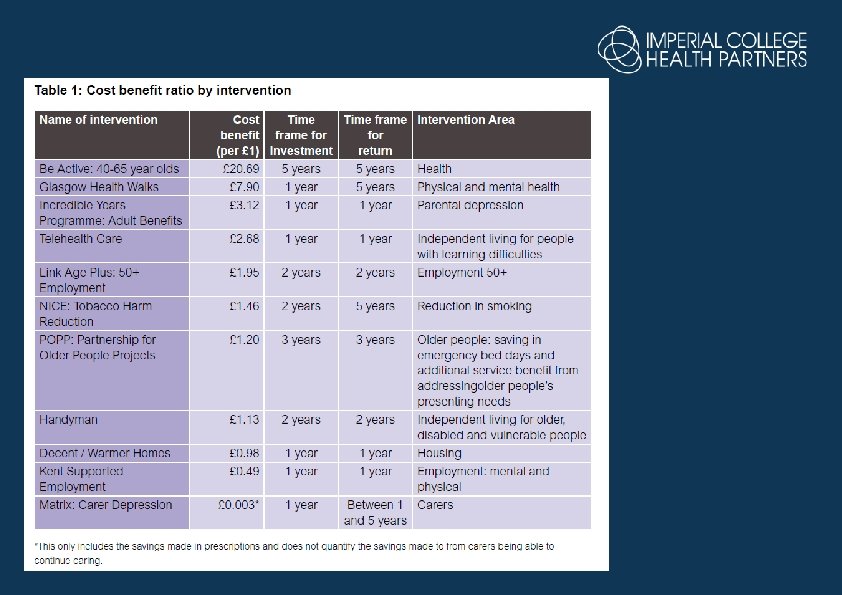
Prioritising interventions The choice of which interventions to prioritise in will be based on a variety of factors including: • The initial cost of providing the intervention • The population health gain that may be achieved (cost-effectiveness) • Downstream savings that may be realised (ROI) • The financial resources available • Other resources required such as the supply of equipment and staff • The existing service provision, its effectiveness and plasticity • Other factors like geography, socio-demographics, ethnicity and cultural acceptability We address the first three of these factors – initial cost, effectiveness and potential savings.
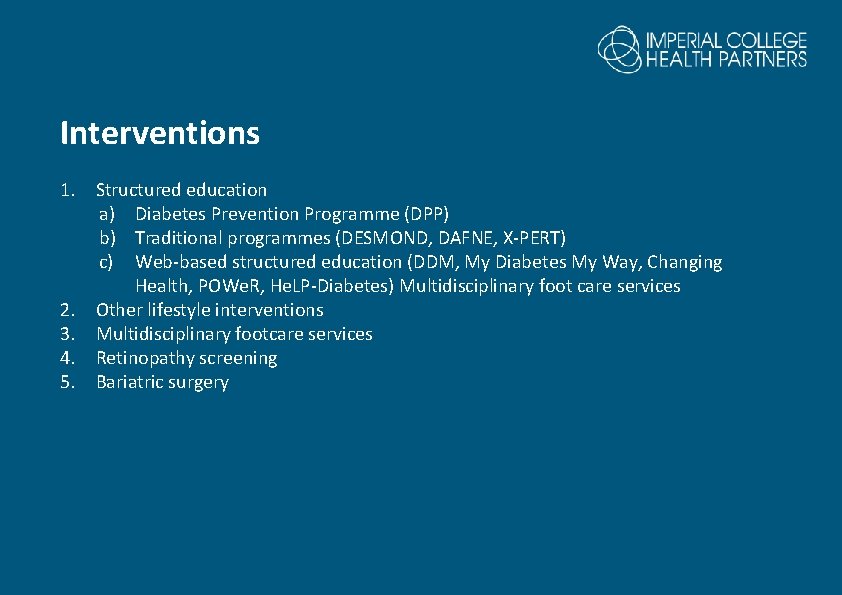
Interventions 1. Structured education a) Diabetes Prevention Programme (DPP) b) Traditional programmes (DESMOND, DAFNE, X-PERT) c) Web-based structured education (DDM, My Diabetes My Way, Changing Health, POWe. R, He. LP-Diabetes) Multidisciplinary foot care services 2. Other lifestyle interventions 3. Multidisciplinary footcare services 4. Retinopathy screening 5. Bariatric surgery

Thank you @andrzeio Andi. orlowski@imperialcollegehealthpartners. com ea@imperialcollegehealthpartners. com @ldn_ichp linkedin/imperialcollegehealthpartners
 Dan orlowski
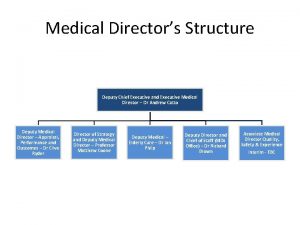
Dan orlowski Deputy medical director
Deputy medical director Daniel orlowski
Daniel orlowski Phm hai
Phm hai Phm sax
Phm sax Proccom phm pertamina
Proccom phm pertamina Phm 142
Phm 142 David elizalde
David elizalde Indirect characterization quote
Indirect characterization quote Confused deputy
Confused deputy Deputy head of division
Deputy head of division Daniel stephens md
Daniel stephens md Deputy stowers
Deputy stowers Roger lukoff
Roger lukoff The deputy incident commander will be replacing
The deputy incident commander will be replacing Stephen deputy md
Stephen deputy md Manifesto for head girl
Manifesto for head girl Deputy jody hull
Deputy jody hull Deputy manager wikipedia
Deputy manager wikipedia Onondaga county sheriff civil division
Onondaga county sheriff civil division How could the french revolution been avoided
How could the french revolution been avoided Definition of third agricultural revolution
Definition of third agricultural revolution Russian revolution vs french revolution
Russian revolution vs french revolution Cara pecahan senilai
Cara pecahan senilai @estehsegerdipagihari:http://work4unity.in/haicantik.html
@estehsegerdipagihari:http://work4unity.in/haicantik.html Langinkosken lukio
Langinkosken lukio Andi instruction example
Andi instruction example Fpb 51 dan 81
Fpb 51 dan 81 Andi kivinukk
Andi kivinukk Andi kushermanto
Andi kushermanto Apa yang dimaksud dengan da'watul afrad
Apa yang dimaksud dengan da'watul afrad