Visual and Perceptual Deficits After a Neurological Event

- Slides: 61
Visual and Perceptual Deficits After a Neurological Event Stacy Krueger, OTR/L, C/NDT 2016
Why is Vision Important? • Vision plays a vital role in all activities of daily living • Visual deficits are often overlooked
Three Component Model of Vision • Visual Integrity • Visual Efficiency • Visual Information Processing
Visual Integrity • Visual Acuity, Refraction, and Eye Heath Visual Acuity (i. e. , 20/20) • Numerator- testing distance at which the subject recognizes stimulus • Denominator- Distance at which the letter being viewed could be identified by a patient with normal visual acuity
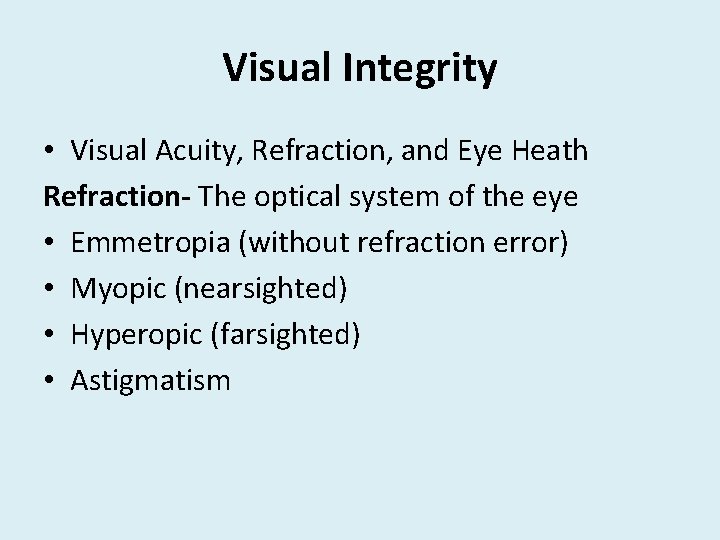
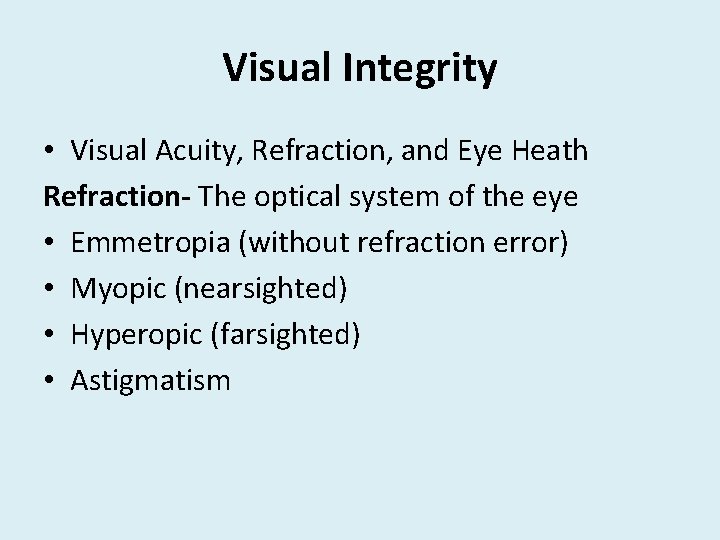
Visual Integrity • Visual Acuity, Refraction, and Eye Heath Refraction- The optical system of the eye • Emmetropia (without refraction error) • Myopic (nearsighted) • Hyperopic (farsighted) • Astigmatism
Refraction Errors
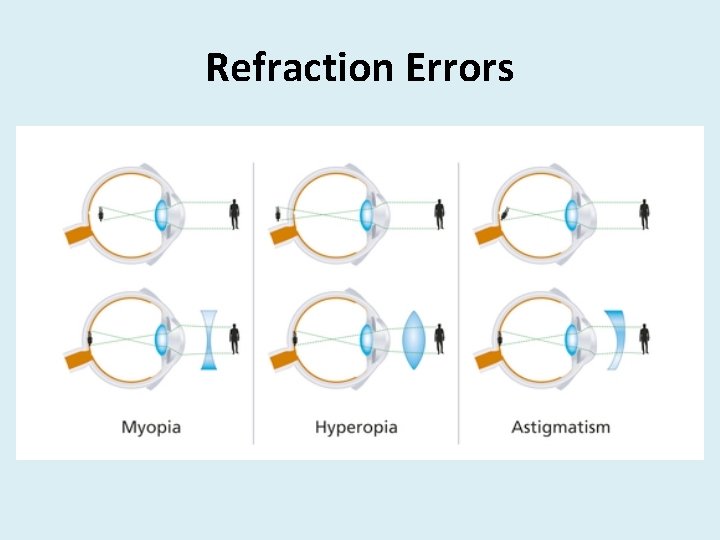
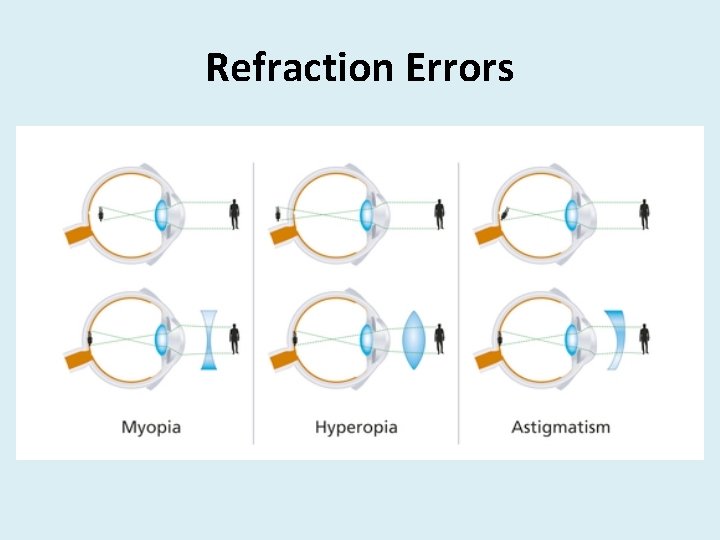
Visual Integrity • Visual Acuity, Refraction, and Eye Heath • Anterior segment, lens, posterior segment, visual pathway
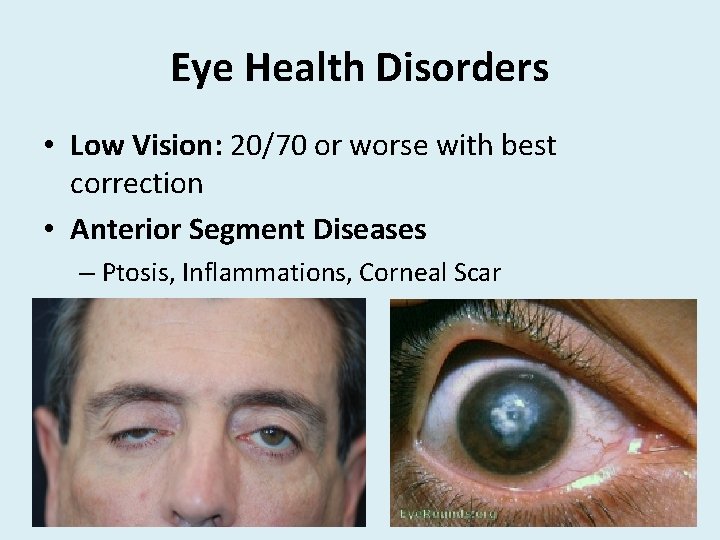
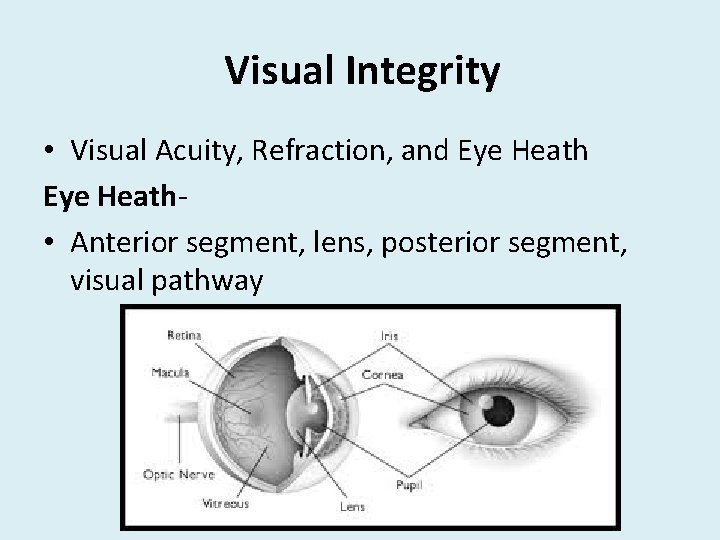
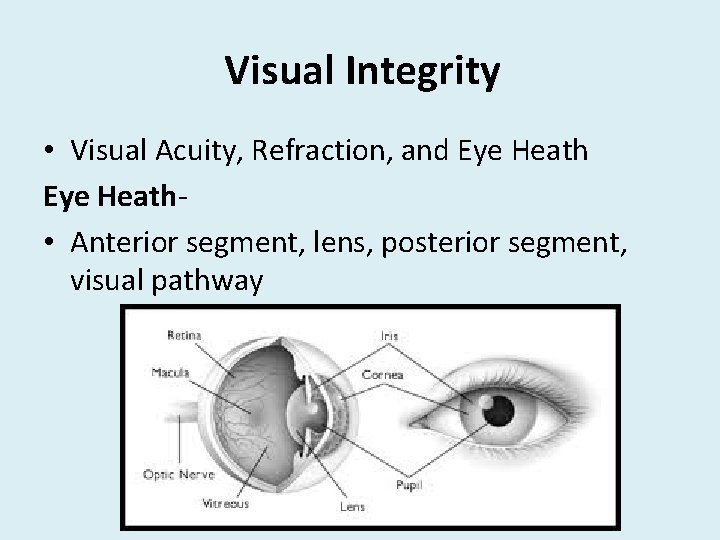
Eye Health Disorders • Low Vision: 20/70 or worse with best correction • Anterior Segment Diseases – Ptosis, Inflammations, Corneal Scar
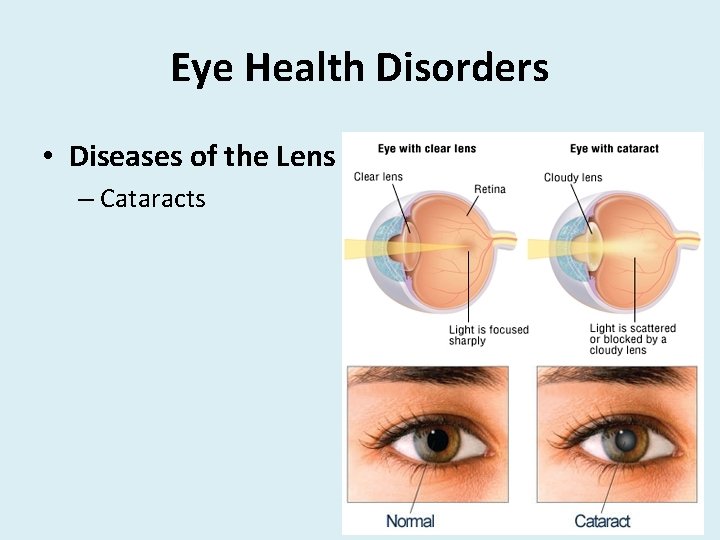
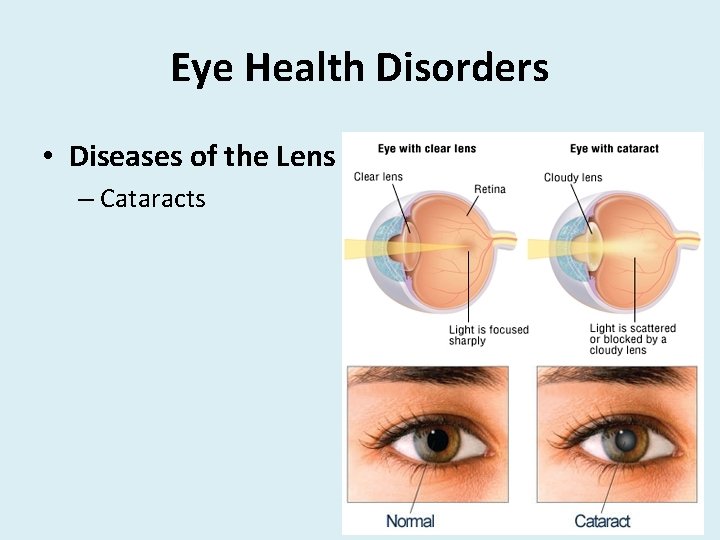
Eye Health Disorders • Diseases of the Lens – Cataracts
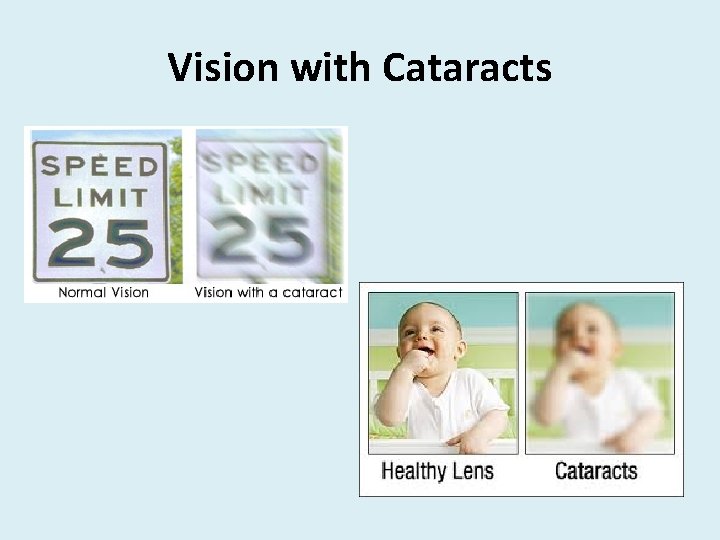
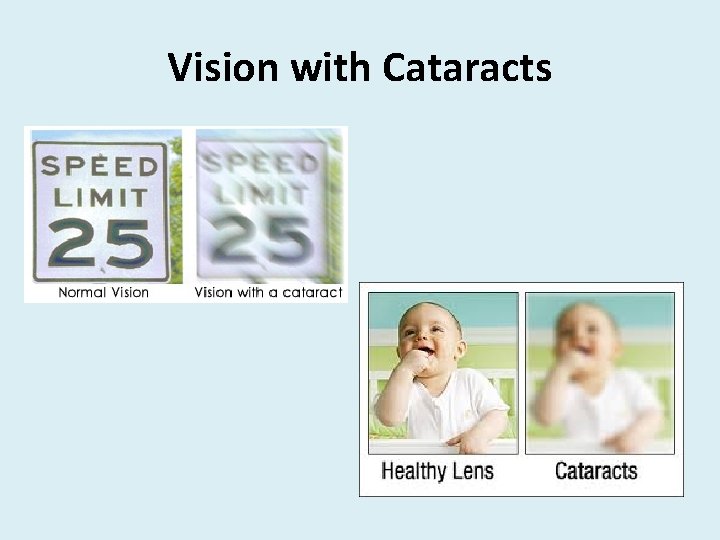
Vision with Cataracts
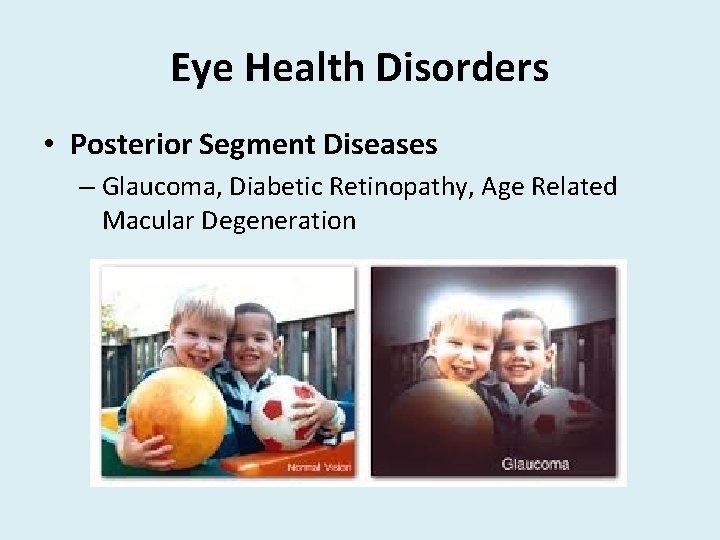
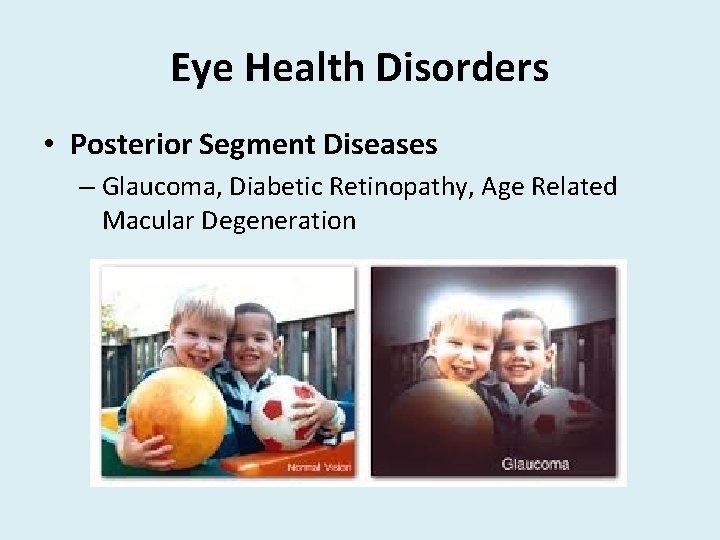
Eye Health Disorders • Posterior Segment Diseases – Glaucoma, Diabetic Retinopathy, Age Related Macular Degeneration
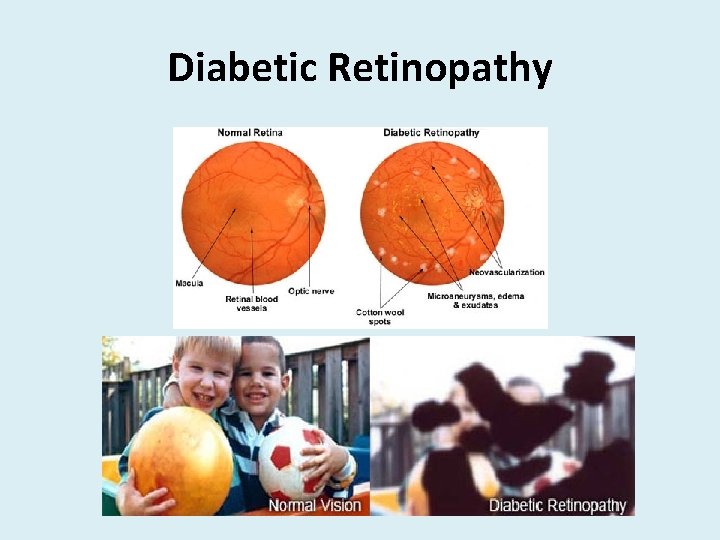
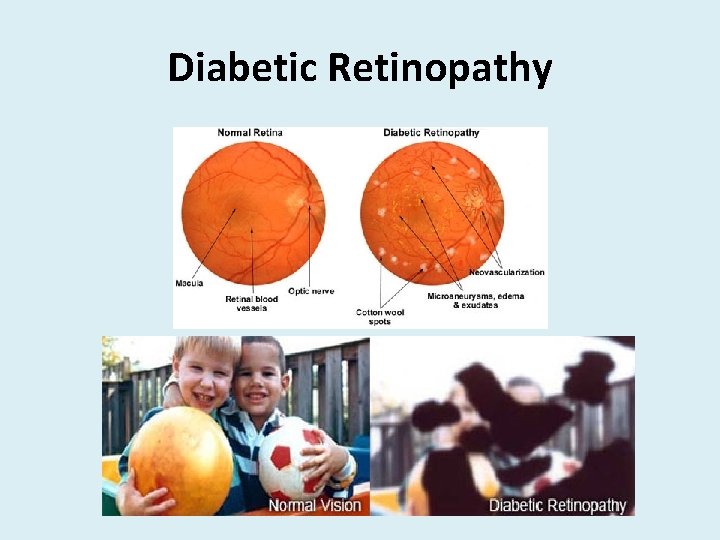
Diabetic Retinopathy
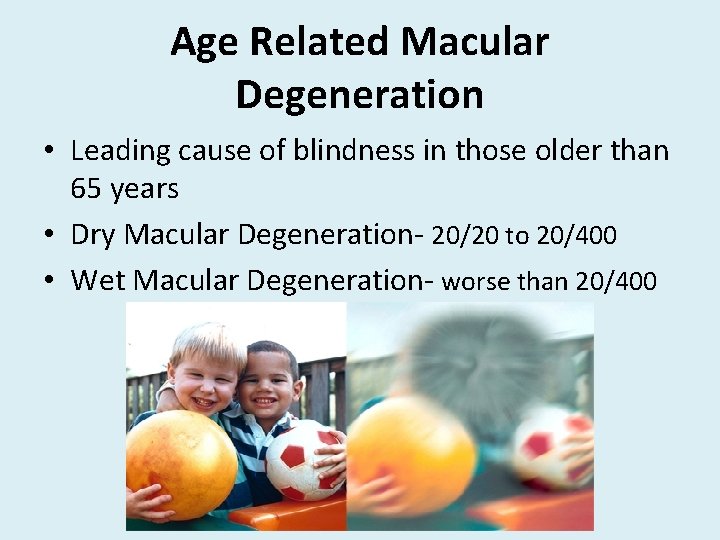
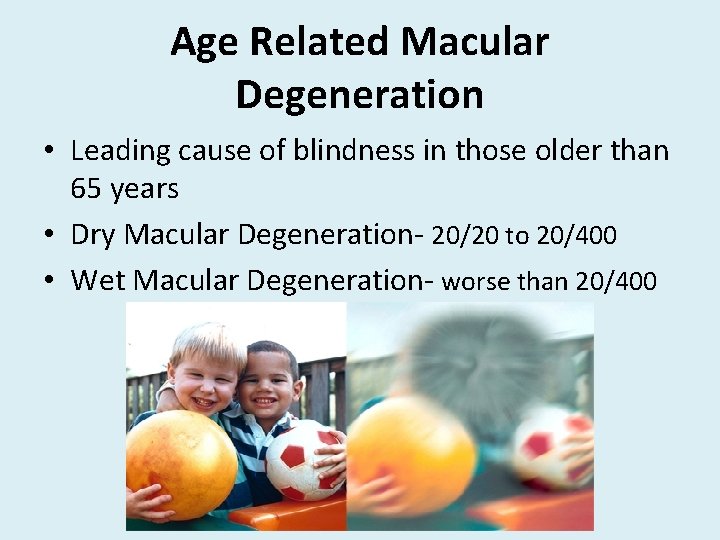
Age Related Macular Degeneration • Leading cause of blindness in those older than 65 years • Dry Macular Degeneration- 20/20 to 20/400 • Wet Macular Degeneration- worse than 20/400
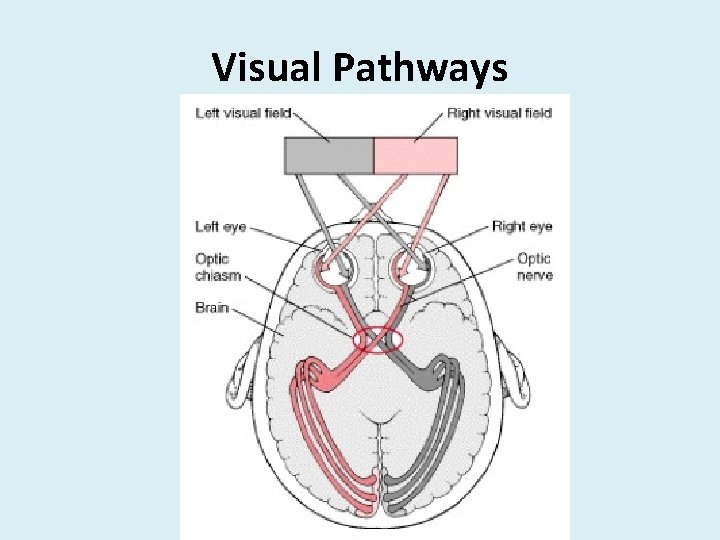
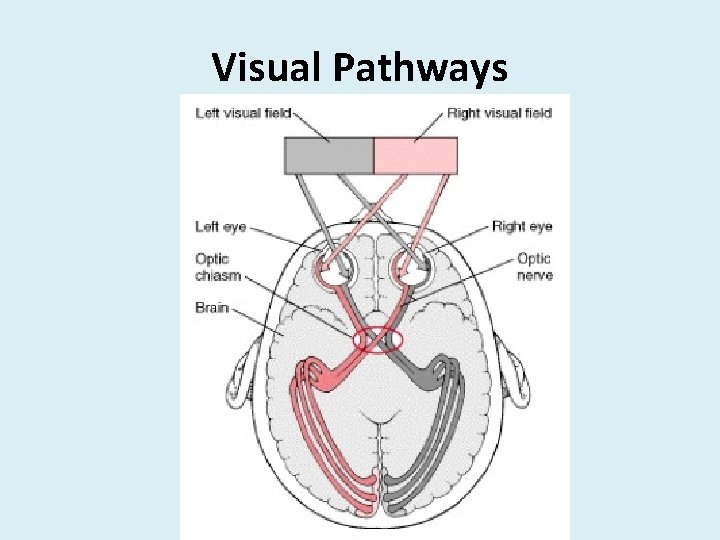
Visual Pathways
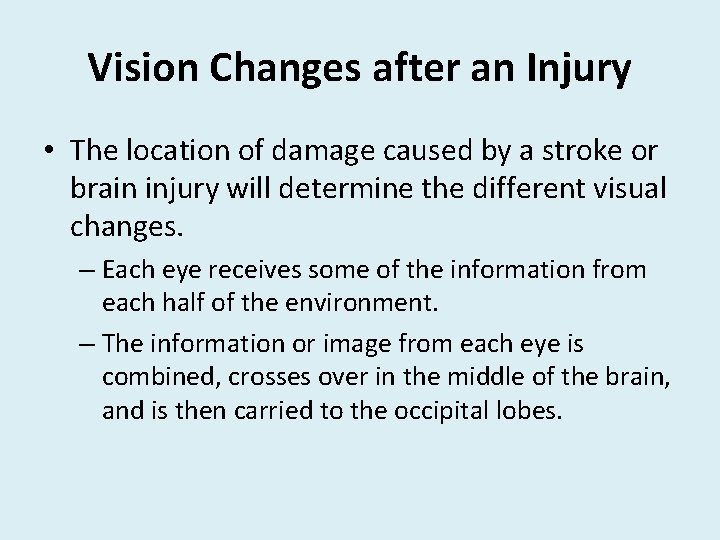
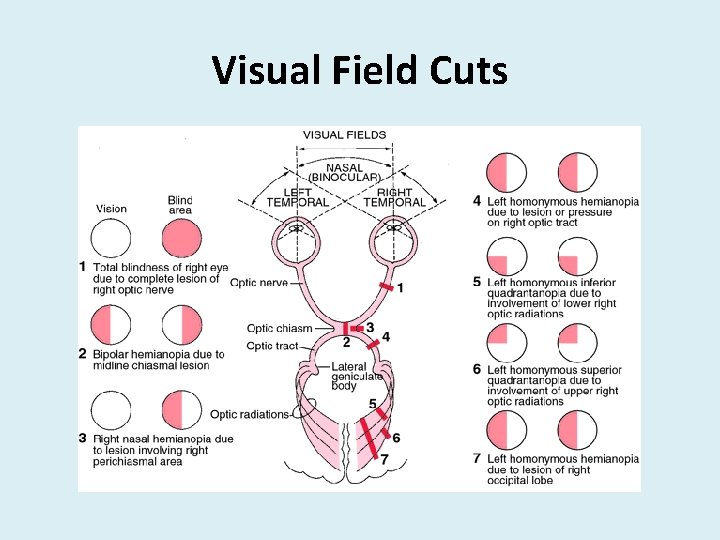
Vision Changes after an Injury • The location of damage caused by a stroke or brain injury will determine the different visual changes. – Each eye receives some of the information from each half of the environment. – The information or image from each eye is combined, crosses over in the middle of the brain, and is then carried to the occipital lobes.
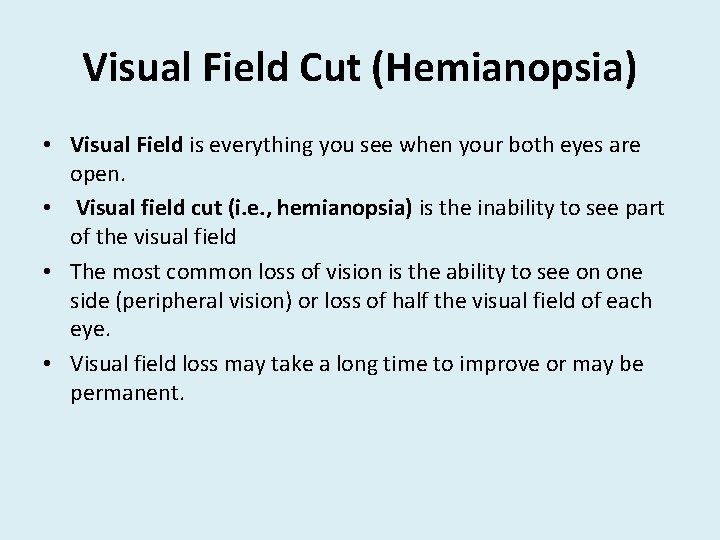
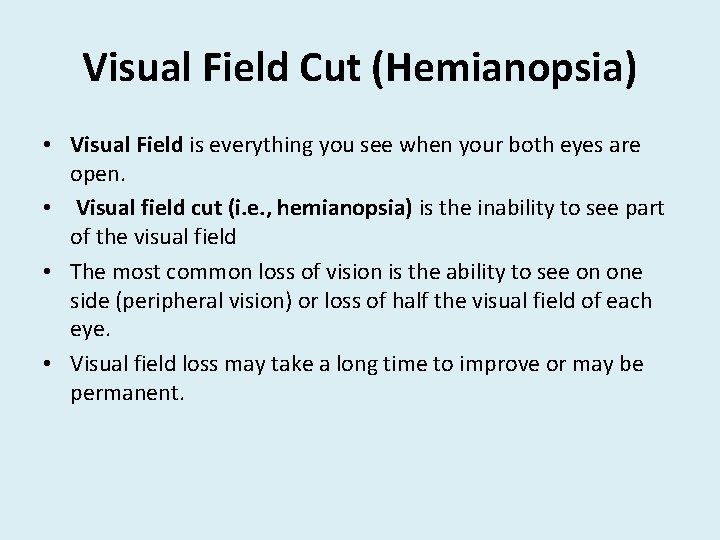
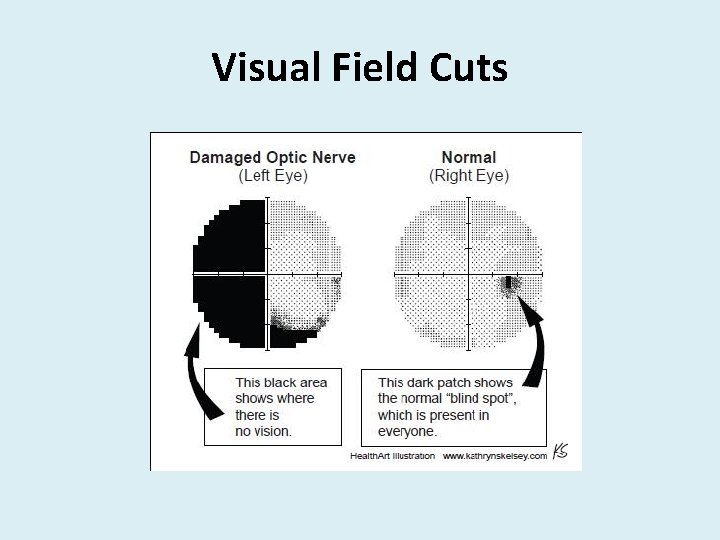
Visual Field Cut (Hemianopsia) • Visual Field is everything you see when your both eyes are open. • Visual field cut (i. e. , hemianopsia) is the inability to see part of the visual field • The most common loss of vision is the ability to see on one side (peripheral vision) or loss of half the visual field of each eye. • Visual field loss may take a long time to improve or may be permanent.
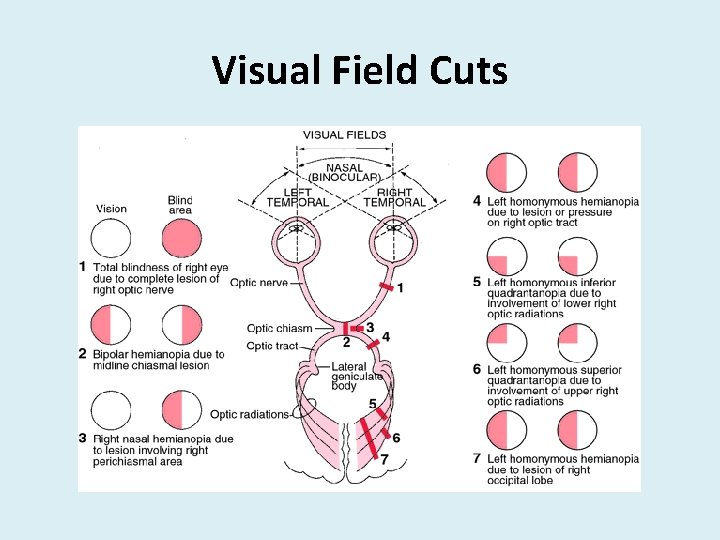
Visual Field Cuts
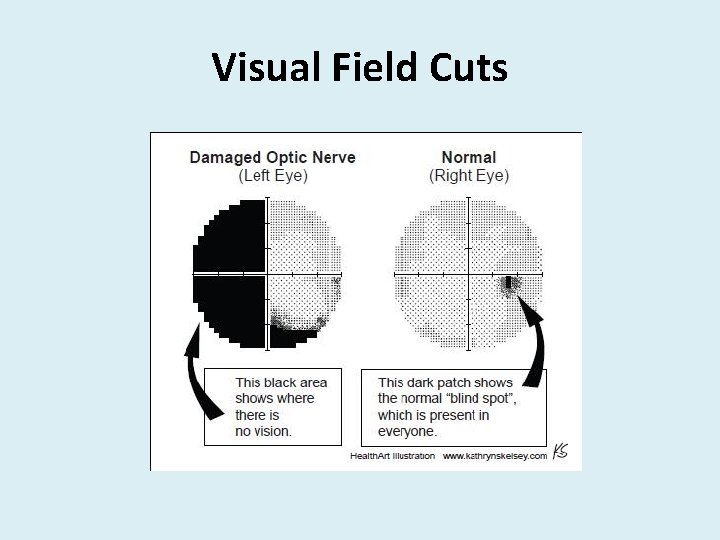
Visual Field Cuts
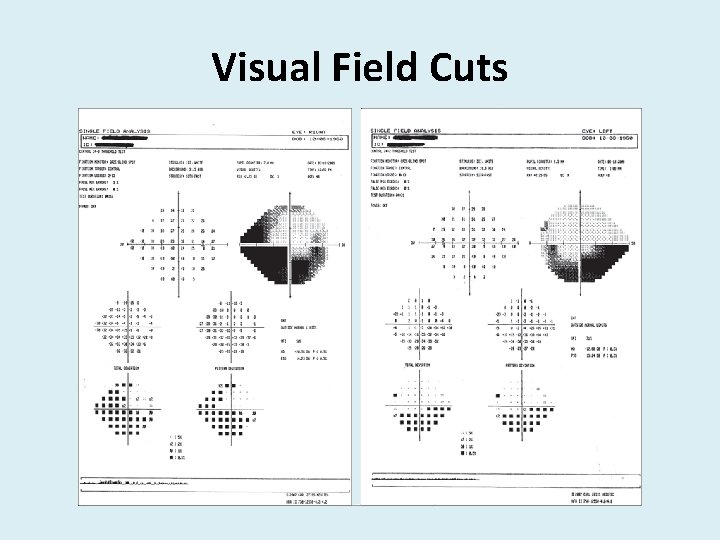
Visual Field Cuts
Visual Efficiency • Effectiveness of the Visual System to clearly, efficiently, and comfortably allow someone to gather visual information – Accommodation (i. e. , focusing) – Binocular Vision (i. e. , eye muscles and teaming) – Eye Movements (i. e. , tracking)
Accommodation Disorders • Insufficiencies – Lens hardens, neuromuscular pathway problems • Excess – Muscles can not relax • Symptoms: – Blurred Vision – Headaches – Eyestrain – Avoidance of reading or other close work
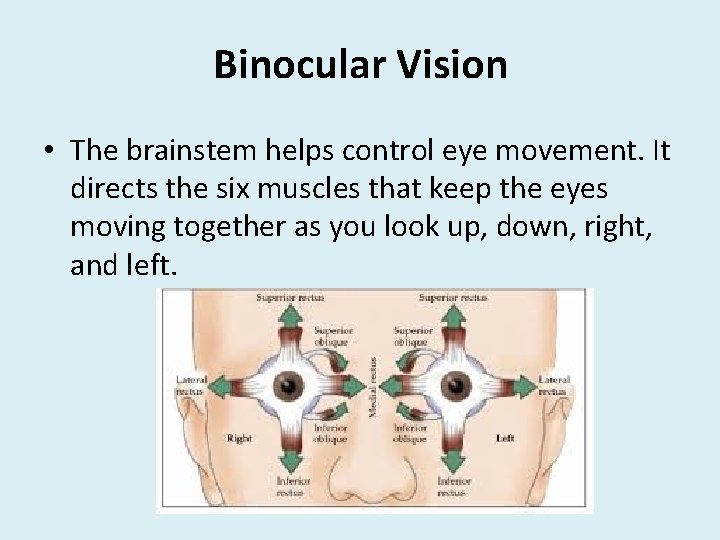
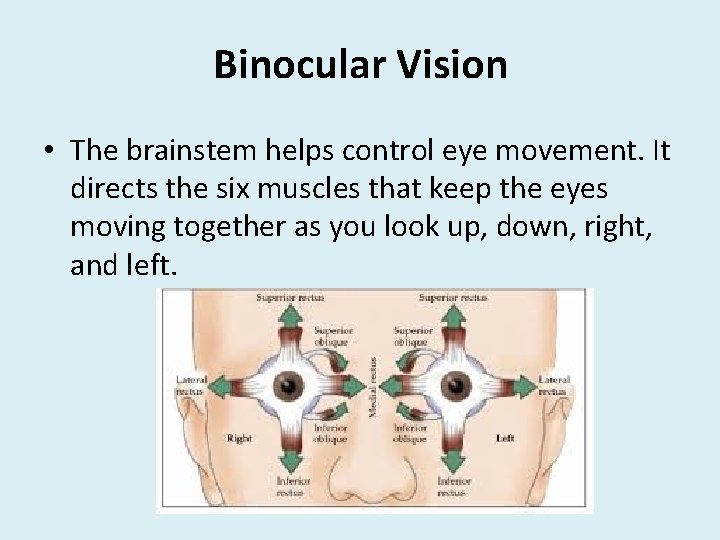
Binocular Vision • The brainstem helps control eye movement. It directs the six muscles that keep the eyes moving together as you look up, down, right, and left.
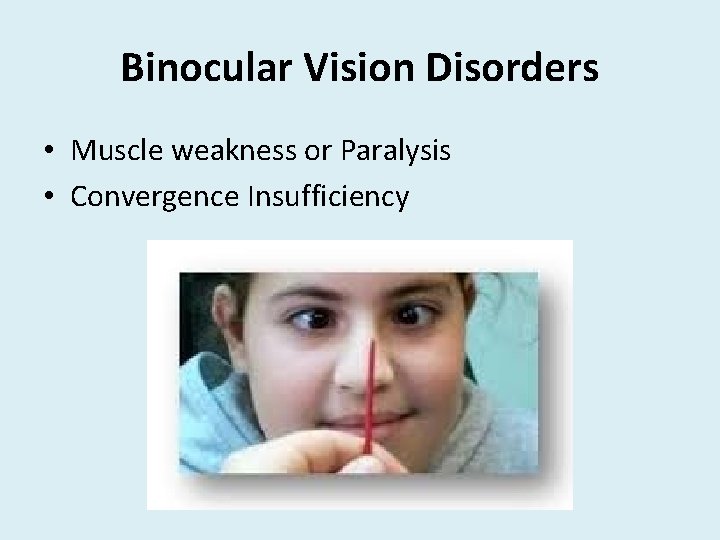
Binocular Vision Disorders • Muscle weakness or Paralysis • Convergence Insufficiency
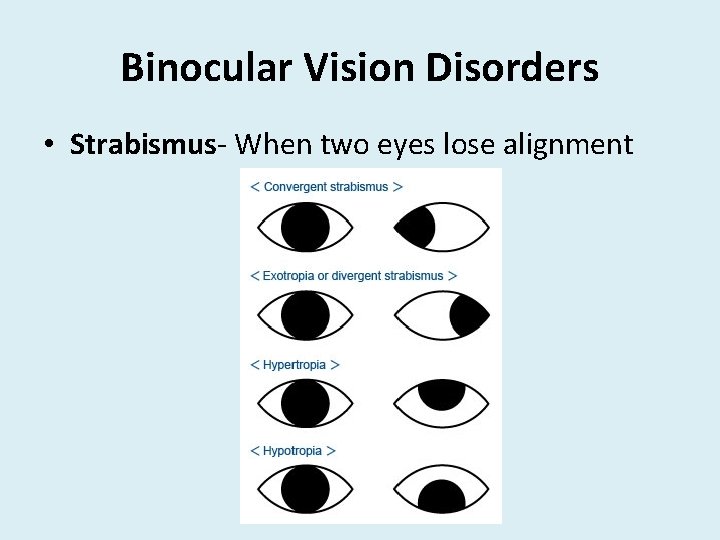
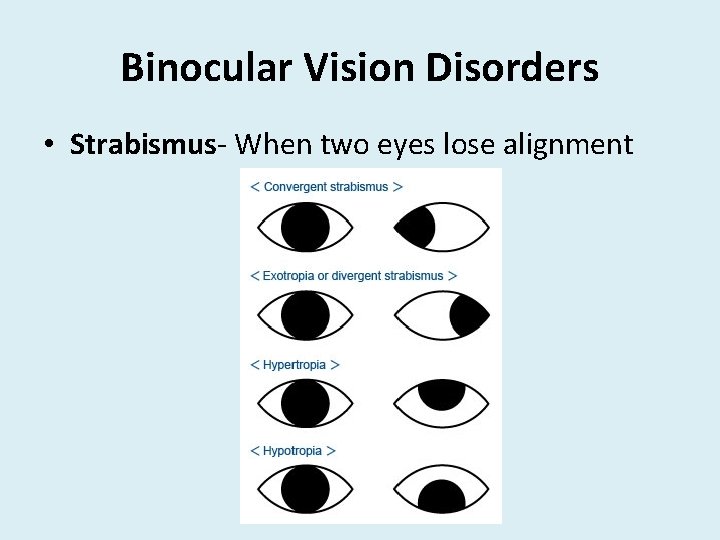
Binocular Vision Disorders • Strabismus- When two eyes lose alignment
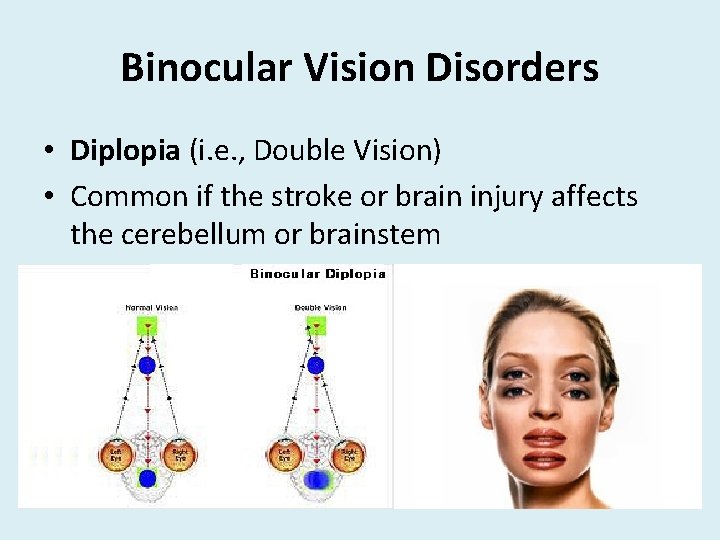
Binocular Vision Disorders • Diplopia (i. e. , Double Vision) • Common if the stroke or brain injury affects the cerebellum or brainstem
Eye Movements • Fixation • Saccades- (i. e. , scanning) • Pursuits (i. e. , tracking)
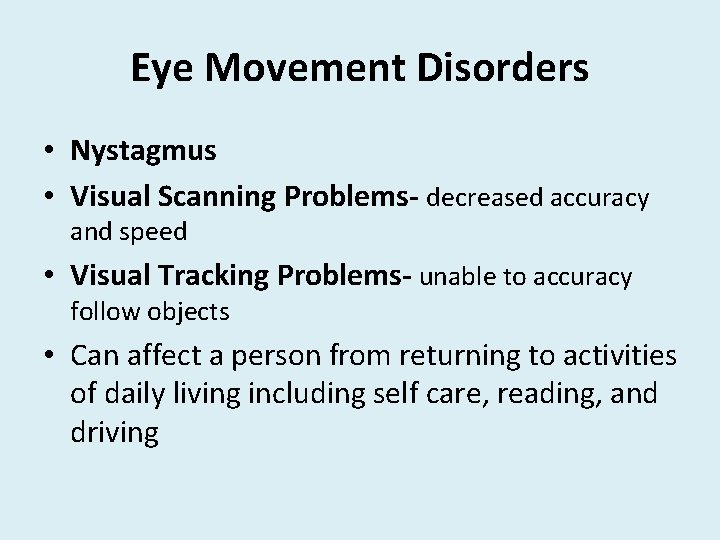
Eye Movement Disorders • Nystagmus • Visual Scanning Problems- decreased accuracy and speed • Visual Tracking Problems- unable to accuracy follow objects • Can affect a person from returning to activities of daily living including self care, reading, and driving
Visual Information Processing • This is where the true "seeing" takes place. • Taking in and organizing visual information from the environment • Integrating this visual information • Making a motor response
Visual Information Processing Visual spatial skills • Used to interact the environment • Develop directional awareness • Develop good motor coordination and balance
Visual Spatial Dysfunction • • Lack of coordination and balance Clumsy, falls Tendency to work with one side of the body Reversing letters and numbers
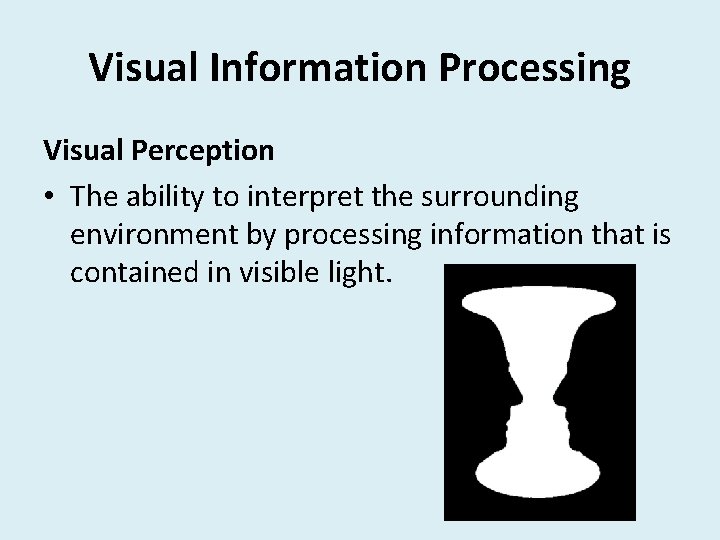
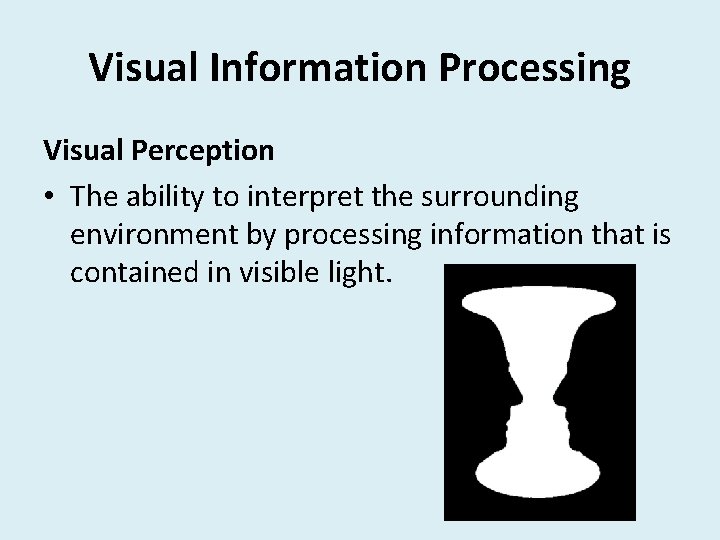
Visual Information Processing Visual Perception • The ability to interpret the surrounding environment by processing information that is contained in visible light.
Visual Perception • Visual Discrimination- size, shape, orientation • Figure Ground- attending to a form while maintaining awareness of background • Visual Closure- determine final picture without all the pieces • Visual Memory- recognize and recall visually presented information
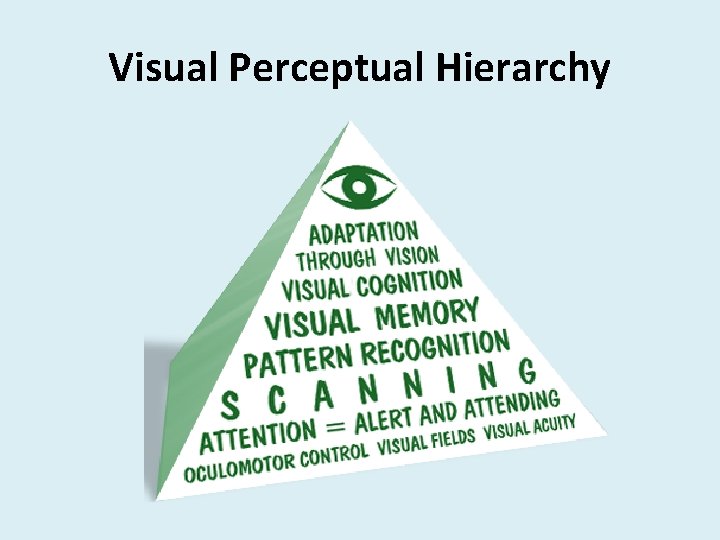
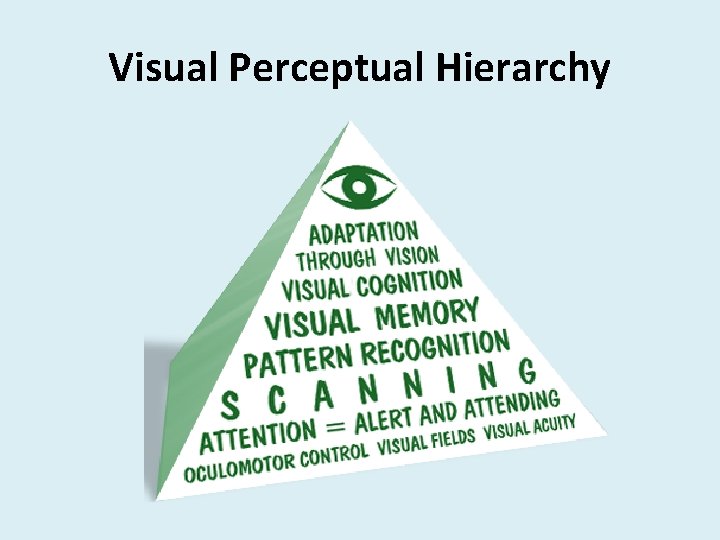
Visual Perceptual Hierarchy
Visual Processing Deficits Common Visual Processing Deficits include: – Visual inattention – Visual neglect – Decreased speed of visual and cognitive processing
Visual Inattention • The inability to perceive a stimulus in a visual field when a similar stimulus is presented and perceived simultaneously in the same visual field • Most evident when searching for visual detail when array is complex and random
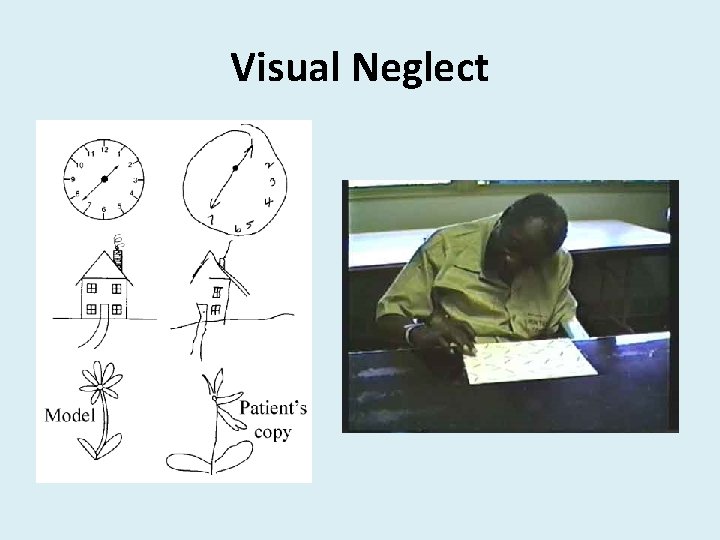
Visual Neglect • Most severe form of visual inattention • Hemispatial neglect is a deficit in attention to and awareness of one side of space is observed. It is the inability of a person to process and perceive stimuli on one side of the body or environment • A person with left neglect may – – hold their head or eyes to the right may not look at you if you stand to their left may not be able to locate items on the left may run into objects on their left side
Visual Neglect Presentation of a person with left neglect may include: – hold their head or eyes to the right – may not look at you if you stand to their left – may not be able to locate items on the left – may run into objects on their left side
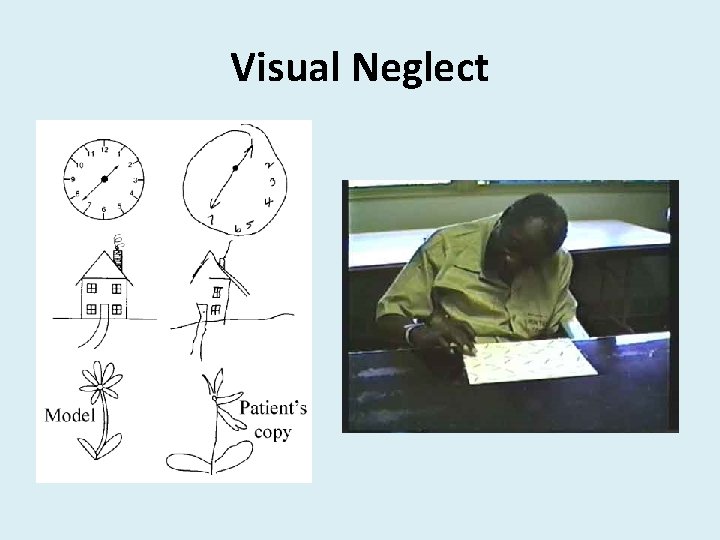
Visual Neglect

Speed of Visual Processing • People who sustain a neurological event often have decreased speed of visual processing • Functional scanning and processing speed is necessary for returning to competitive employment, school activities, and driving
Visual Motor Coordination • Ability to integrate visual information processing skills with: – Fine motor coordination – Visual motor integration
Visual Motor Dysfunction • Common symptoms with visual motor dysfunction: – Fumbling objects – Overshooting and undershooting – Difficulty writing – Slowed reaction times
What Can We Do? • Assessment for and identify potential visual deficits • Direct your patient to the appropriate professional • Create functional goals for Visual Deficits • Provide treatment activities to retrain visual skills and/or teach ways to help compensate for vision deficits
Assessing for Visual Deficits • Clinical Observation – Look at functional vision during ADL completion – Bump into objects during ambulation – Overshoot/Undershoot when reaching for items – Miss items unilaterally – Squinting when looking at targets
Assessing for Visual Deficits • Interview – Does the patient report any visual changes? • Blurry or fuzzy vision • Visual Fatigue • Visual Fluctuations • Missing items
Assessing for Visual Deficits • Screening – Complete simple oculomotor screening • Fixation • Saccades • Pursuits • Convergence
Assessing for Visual Deficits • Screening • Complete screening for visual tracking, attention, and neglect – Letter Cancellation – Shape Cancellation – Line Bisection – Draw Clock
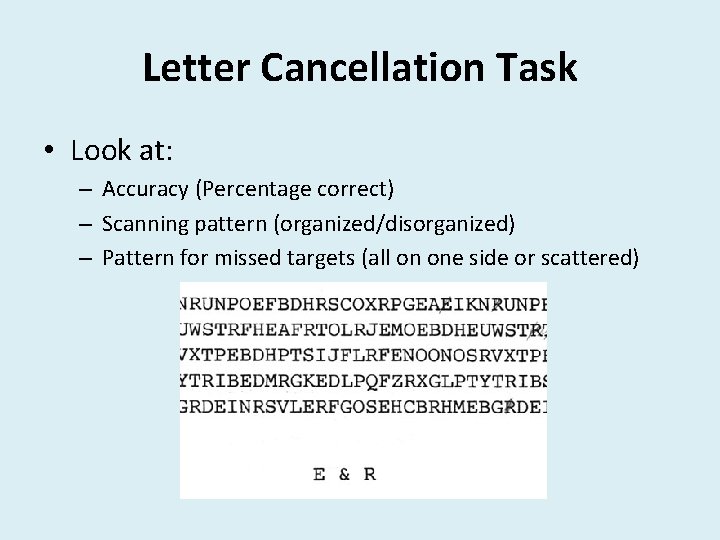
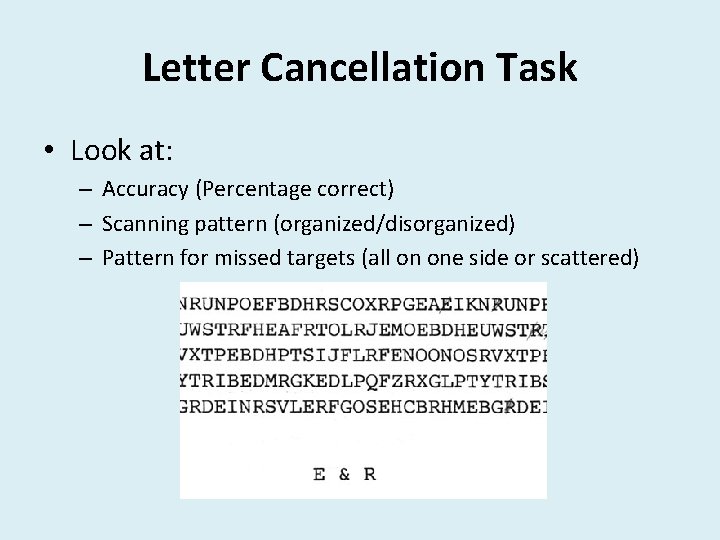
Letter Cancellation Task • Look at: – Accuracy (Percentage correct) – Scanning pattern (organized/disorganized) – Pattern for missed targets (all on one side or scattered)
Assessing for Visual Deficits • Complete standardized assessments • Visual Perception – Motor Free Visual Perceptual Test (MVPT) • Speed of Visual Processing – Trail Making Part A and Part B • Visual Motor Coordination – Dynavision D 2
Dynavision D 2 • The Dynavision D 2 Visuomotor Training System has proven effective for use in visual, cognitive, and physical rehabilitation. • The programmable options standard with Dynavision D 2 software will enable the clinician to facilitate individualized treatment for clients of different ages, abilities, and conditions. • Performance data is quantitative and objective ensuring accuracy for initial evaluation and progress monitoring.
Dynavision D 2 https: //www. youtube. com/watch? v=Kz. M-z. FSR 1 Vg
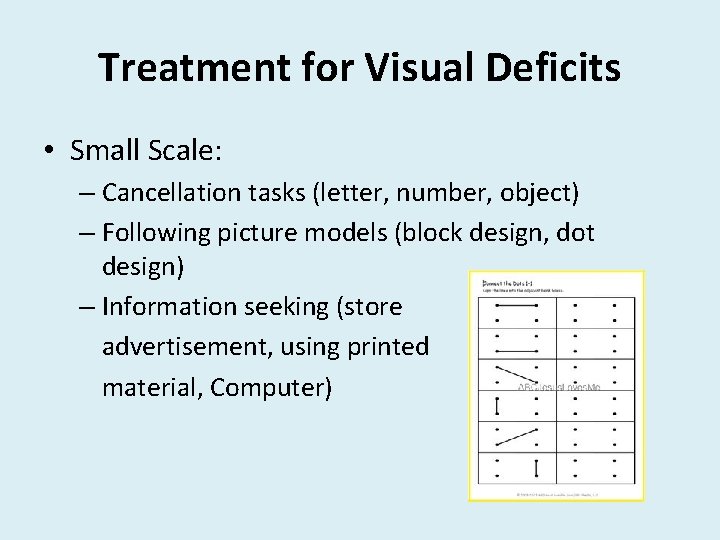
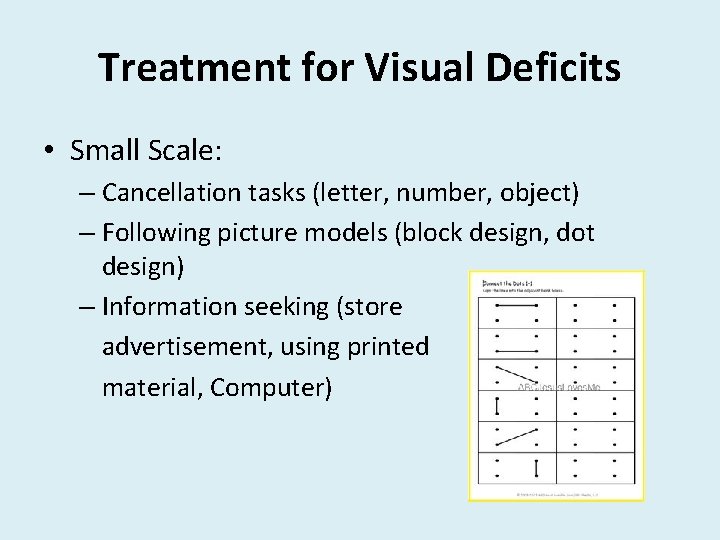
Treatment for Visual Deficits • Small Scale: – Cancellation tasks (letter, number, object) – Following picture models (block design, dot design) – Information seeking (store advertisement, using printed material, Computer)
Treatment for Visual Deficits • Medium Scale: – Matching and sorting activities – Locate target objects (Cards on table, target positions/pieces on game board)
Treatment for Visual Deficits • Large Scale: – Dynavision D 2 activities – Visual Scanning during ambulation (i. e. , Scavenger hunt) – Kinect – Wii – Active Passenger Tasks
Case Study “Mary” • Complaint of blurred vision and difficulty with computer usage at work. • Went to the eye doctor who sent her for additional testing due to concerns of Stroke in December
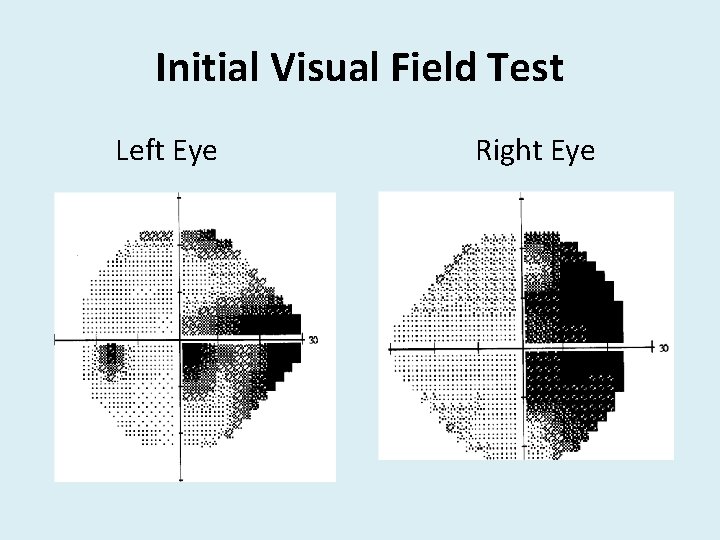
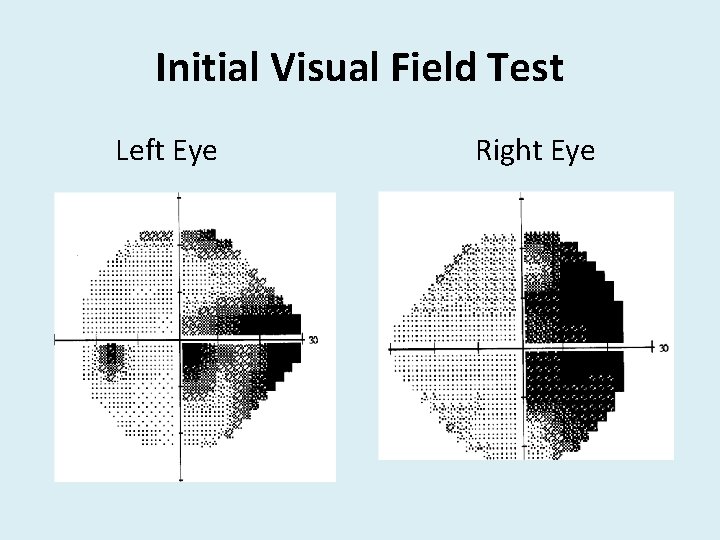
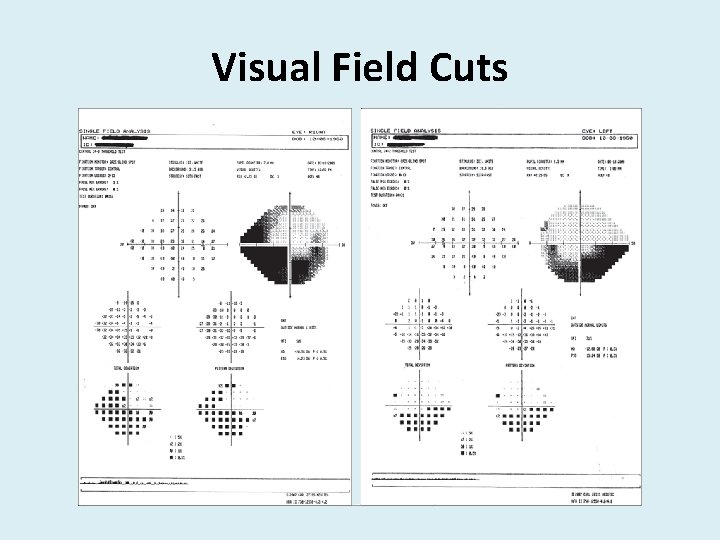
Initial Visual Field Test Left Eye Right Eye
Evaluation • Patient is unable to complete daily activities due to visual deficits (i. e. , working, driving, cooking) • Evaluation results include – Impaired visual scanning, processing, perception – Unable to read standard print or complete computer work – Dynavison D 2 60 -second trial Score: 50 Average Reaction Time 1. 20 seconds – Intact UE and LE skills
Treatment • Recommend Skilled OT 3 x/week which tapered to 2 x/week as patient progressed • Completed 44 treatment session prior to discharge • Treatment included: – Training for functional visual scanning patterns – Activities to improve perceptual skills – Information seeking using printed material and computer tasks – Dynavision D 2 to improve visual motor coordination and speed of visual processing
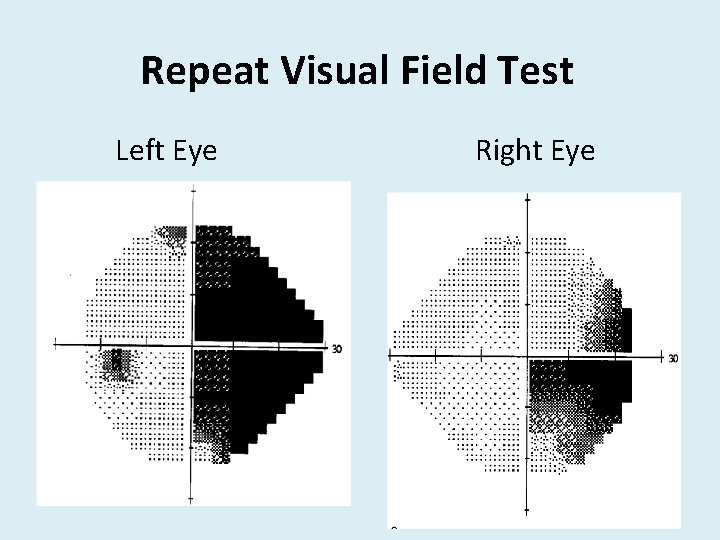
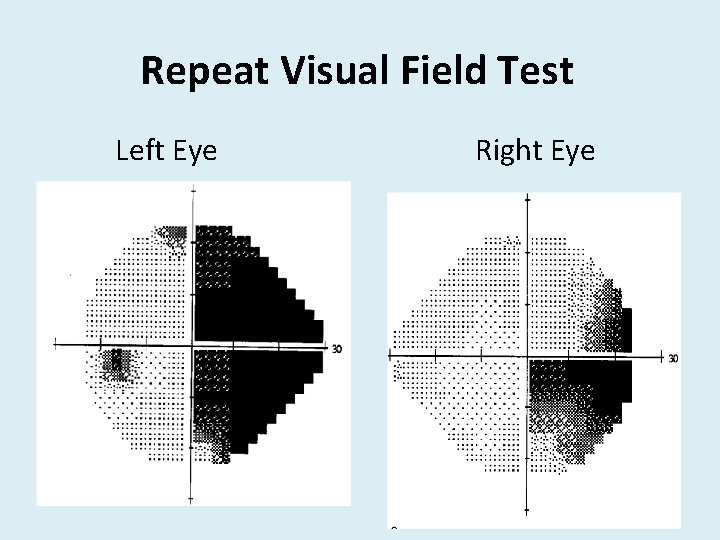
Repeat Visual Field Test Left Eye Right Eye
Discharge • Mary did have some continued visual deficits, however was able to compensate well enough to return to independent living and driving. • Discharge Dynavision D 2 60 second trial Score: 78 Average Reaction Time: 0. 77 seconds
? s n o i t Ques
References • Ciuffreda KJ, Suchoff IB, Marrone MA, Ahmann E. , Oculomotor rehabilitation in traumatic brain-injured patients. J Behavioral Optom 1996; 7: 31 -38 • Scheiman M, Gallaway MF. , Vision Therapy to Treat Binocular Vision Disorders After Acquired Brain Injury: Factors Affecting Prognosis. In: Suchoff I, Ciuffreda, KJ, Kapoor N, ed. Visual and Vestibular Consequences of Acquired Brain Injury. Santa Ana: Optometric Extension Program; 2001 • Suter, P. , Harvey L. , Vision Rehabilitation: Multidisciplinary Care of the Patient Following Brain Injury, CRC Press, New York, 2011 • Schlageter K, Shaw R. , Vision Therapy. OT Week, July 11, 1991. • Warren, M. L. (1993). “A Hierarchical Model for Evaluation and Treatment of Visual Perception Dysfunction in Adult Acquired Brain Injury” Parts 1 and 2, American J of Occupational Therapy, 47: 42 -66