Vision 4 You How to measure tear film



- Slides: 41
Vision 4 You How to measure tear film Quality & Quantity the least INVASIVE way. Claes Feinbaum M. Sc. Ph. D. Professor Emeritus OPHTHALMOLOGY & OPTOMETRY BEN GURION UNIVERSITY OF THE NEGEV, ISRAEL
Introduction • The last three decades have seen the awareness of dry eye dis-ease (DED) rise considerably around the world. Through the mutual efforts of many organizations, much has been learned about the basis and impact of this disease in the continued attempt to improve clinical care for affected individuals.
TFOS DEWS II revised definition Dry eye is a multifactorial disease of the ocular surface charac-terized by a loss of homeostasis of the tear film, and accompanied by ocular symptoms, in which tear film instability and hyper-osmolarity, ocular surface inflammation and damage, and neuro-sensory abnormalities play etiological roles.
Ocular surface Is defined as comprising the structures of the eye and adnexa, including the cornea, conjunctiva, eyelids, eyelashes, tear film, main and accessory lacrimal glands, and the meibomian glands. Thus, the tears, both in terms of the individual components at the site of production, and as a film on the ocular surface, are included within the term “ocular surface

The Tear Film
Glycocalix The innermost layer of the tear film connects the glycocalyx of corneal epithelia with mucins secreted by goblet cells. This mucous layer is critical in adhering the tear film to the cornea. It connects the hydrophobic cells of the cornea with the hydrophilic aqueous layer of the tear film.
Typically tear film abnormalities associated With the corneal glycocalyx layer are localized to discrete areas of the cornea, whereas those associated with mucins are more diffuse. Common problems that disrupt the glycocalyx include corneal sequestrums, ulcerations, touch and mineralizations. For example, a corneal ulceration generates a dry spot that will retain debris and bacteria that would normally be cleared by an intact tear film.
Goblet cells Produce most of the mucins within the tear film, but some are derived from corneal epithelia. The act of blinking spreads these mucins across the corneal surface. Mucins are "sticky" hydrophilic carbohydrates that form a physical barrier to bacterial adherence. The initial stages of clearing bacteria from the ocular surface include mucins coating the invaders. Mucins are therefore critical in preventing bacterial infection of the eye.
The Blepharitis Patient • The chronic blepharitis patient that has attempted numerous unsuccessful treatment regimens and has visited numerous eye doctors looking for some relief. Interestingly, the cause of their chronic blepharitis might be secondary to Demodex infestation.
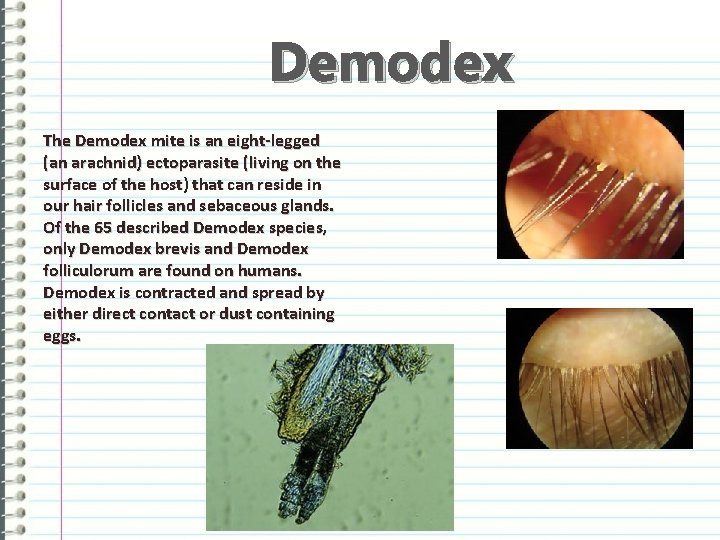
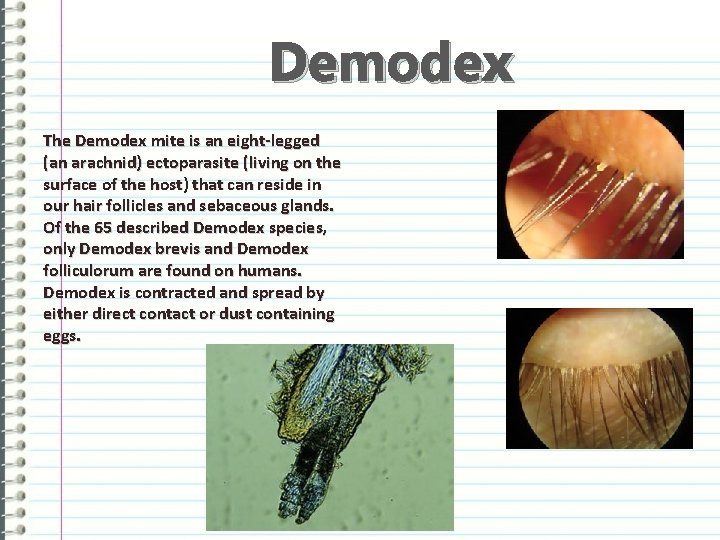
Demodex The Demodex mite is an eight-legged (an arachnid) ectoparasite (living on the surface of the host) that can reside in our hair follicles and sebaceous glands. Of the 65 described Demodex species, only Demodex brevis and Demodex folliculorum are found on humans. Demodex is contracted and spread by either direct contact or dust containing eggs.
DES or KCS Dry eye syndrome (DES) is one of the most frequently encountered ocular morbidities. Twenty-five percent of patients who visit ophthalmic clinics report symptoms of dry eye, making it a growing public health problem and one of the most common conditions seen by eye care practitioners. The prevalence of DES is estimated to be 7. 4% to 33. 7% depending on which study is cited, how the disease is diagnosed, and which population is surveyed.
What is the impact of dry eye syndrome? More than three million American women over the age of 50 have moderate to severe dry eyes, while more than 1. 5 million American men over the age of 50 are similarly afflicted. This condition is fairly benign and easily treated with artificial tears, however. Many contact lens wearers experience dry eyes at some point with many discontinuing or limiting lens wear. Dry eye is a significant finding in patients having undergone refractive surgery, especially LASIK.
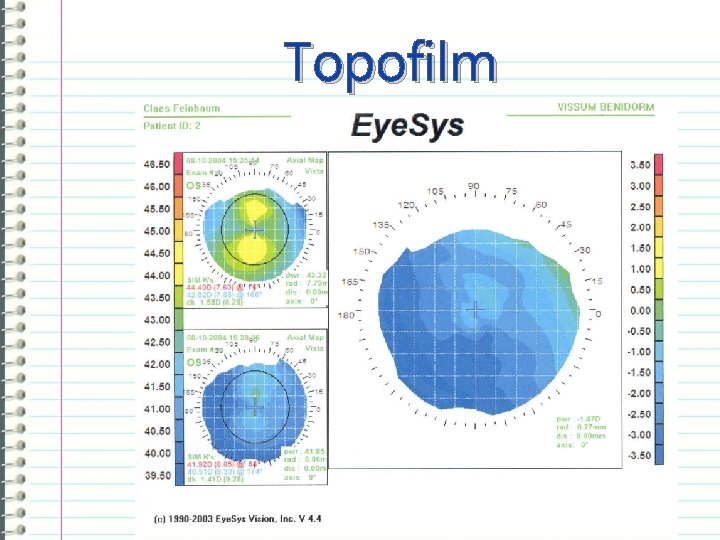
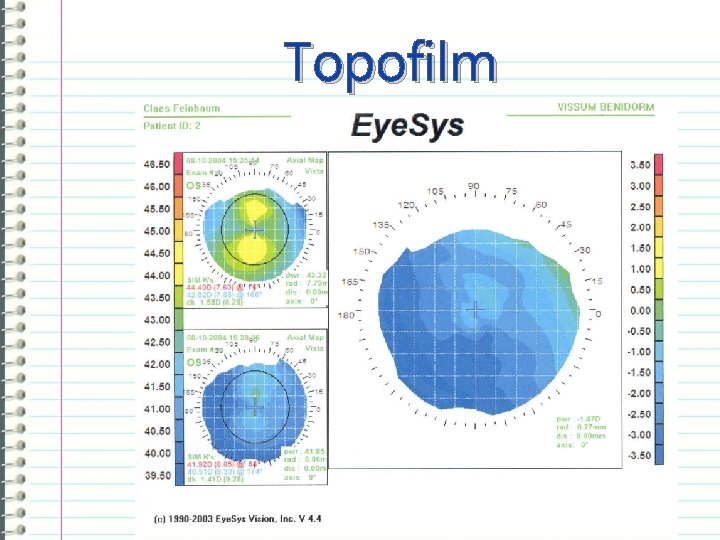
Topofilm
TEAR FILM STABILITY TESTS
Normal tear film is continuously available. Blinking maintains the tear film continuity. However if you keep your eyes open long enough, without blinking, the tear film will start breaking up. Your eye will feel uncomfortable forcing you to blink. In patients with dry eyes the tear film is unstable, and breaks up faster. Therefore the tear break up time in patients who have dry eyes is shorter.
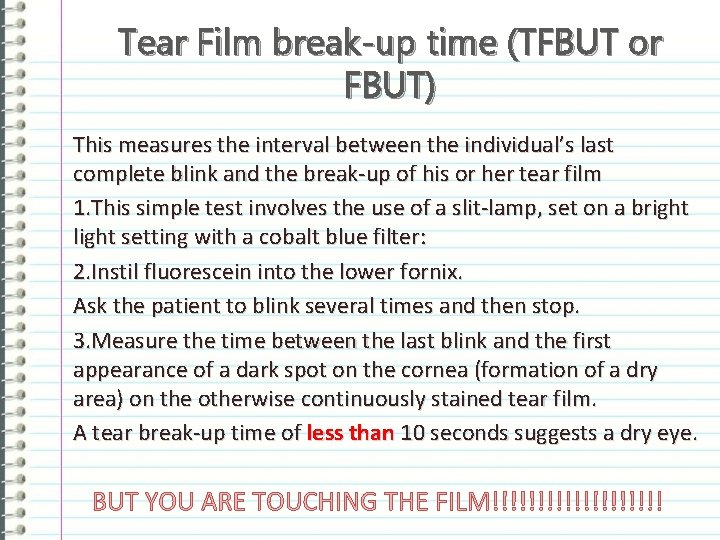
Tear Film break-up time (TFBUT or FBUT) This measures the interval between the individual’s last complete blink and the break-up of his or her tear film 1. This simple test involves the use of a slit-lamp, set on a bright light setting with a cobalt blue filter: 2. Instil fluorescein into the lower fornix. Ask the patient to blink several times and then stop. 3. Measure the time between the last blink and the first appearance of a dark spot on the cornea (formation of a dry area) on the otherwise continuously stained tear film. A tear break-up time of less than 10 seconds suggests a dry eye. BUT YOU ARE TOUCHING THE FILM!!!!!!!!!!
In the F B U T test the presence of fluorescein in the tears may stimulate reflex tearing and may also result in changes to the tear film properties. To overcome these potential limitations,
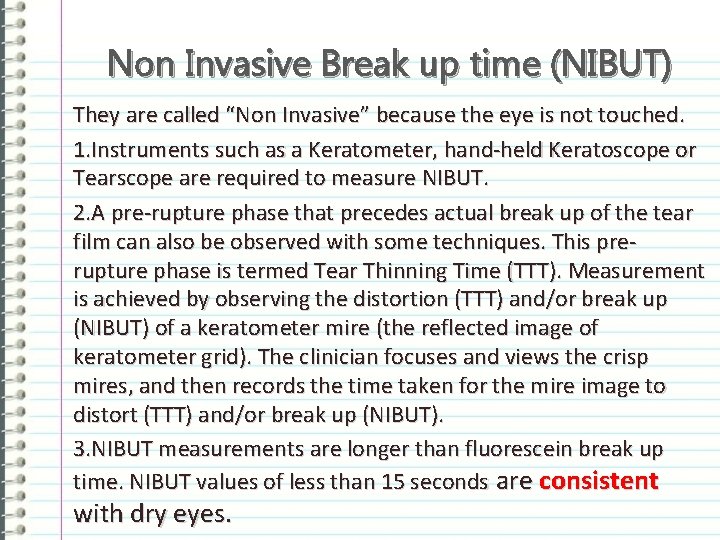
Non Invasive Break up time (NIBUT) They are called “Non Invasive” because the eye is not touched. 1. Instruments such as a Keratometer, hand-held Keratoscope or Tearscope are required to measure NIBUT. 2. A pre-rupture phase that precedes actual break up of the tear film can also be observed with some techniques. This prerupture phase is termed Tear Thinning Time (TTT). Measurement is achieved by observing the distortion (TTT) and/or break up (NIBUT) of a keratometer mire (the reflected image of keratometer grid). The clinician focuses and views the crisp mires, and then records the time taken for the mire image to distort (TTT) and/or break up (NIBUT). 3. NIBUT measurements are longer than fluorescein break up time. NIBUT values of less than 15 seconds are consistent with dry eyes.
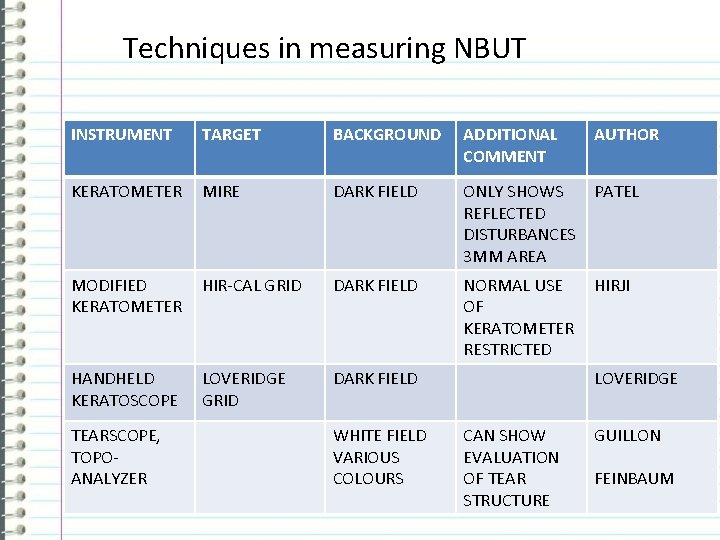
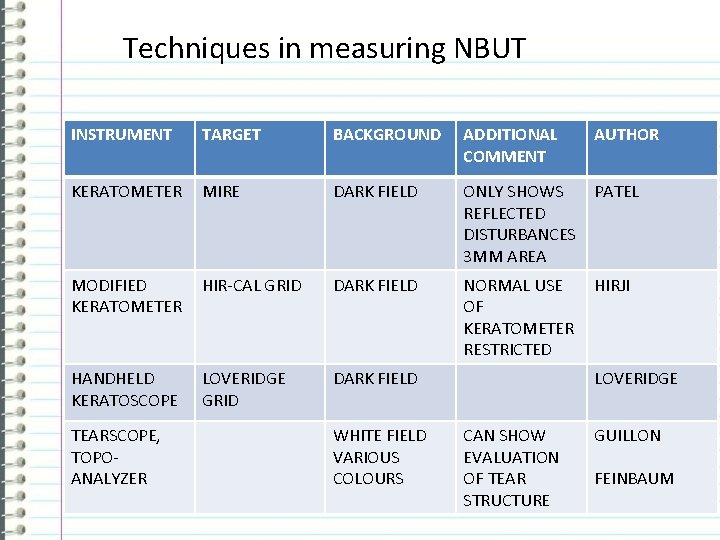
Techniques in measuring NBUT INSTRUMENT TARGET BACKGROUND ADDITIONAL COMMENT KERATOMETER MIRE DARK FIELD ONLY SHOWS PATEL REFLECTED DISTURBANCES 3 MM AREA MODIFIED KERATOMETER HIR-CAL GRID DARK FIELD NORMAL USE HIRJI OF KERATOMETER RESTRICTED HANDHELD KERATOSCOPE LOVERIDGE GRID DARK FIELD TEARSCOPE, TOPOANALYZER WHITE FIELD VARIOUS COLOURS AUTHOR LOVERIDGE CAN SHOW EVALUATION OF TEAR STRUCTURE GUILLON FEINBAUM
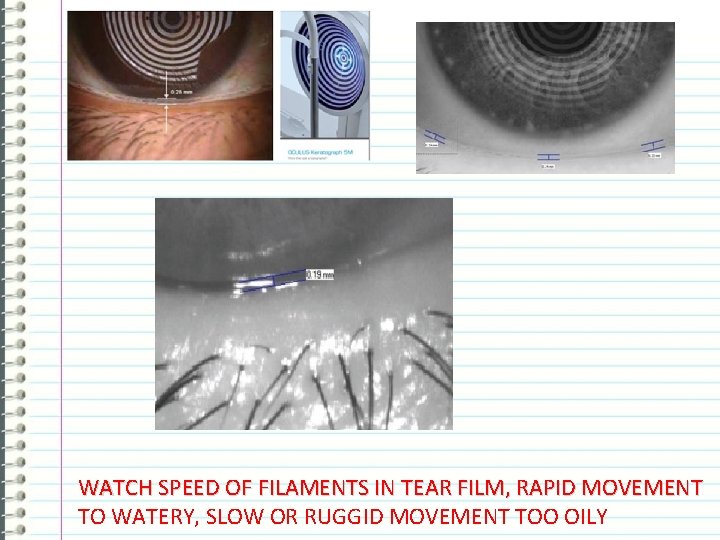
Tear Prism Height & Speed of filaments.

Routine A clinical routine to incorporate the measurement of the tear film prism height: • Immediately below the pupil centre • 5 mm nasally • 5 mm temporally Try to avod fluorescein!
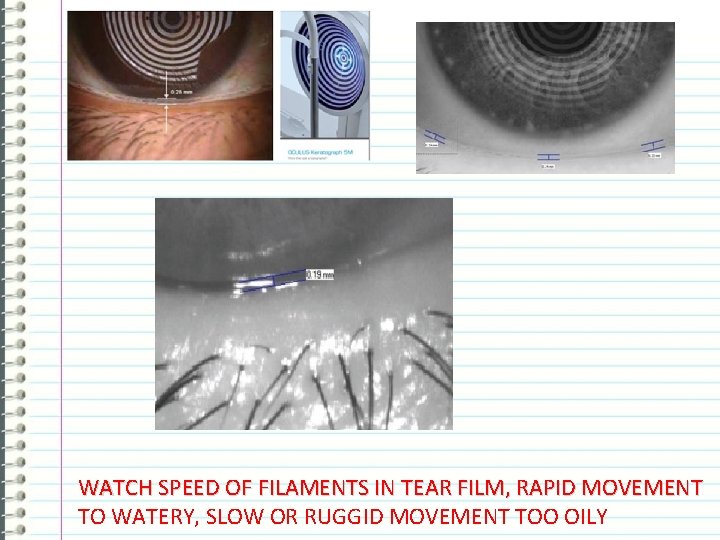
WATCH SPEED OF FILAMENTS IN TEAR FILM, RAPID MOVEMENT TO WATERY, SLOW OR RUGGID MOVEMENT TOO OILY
TEAR VOLUME TESTS
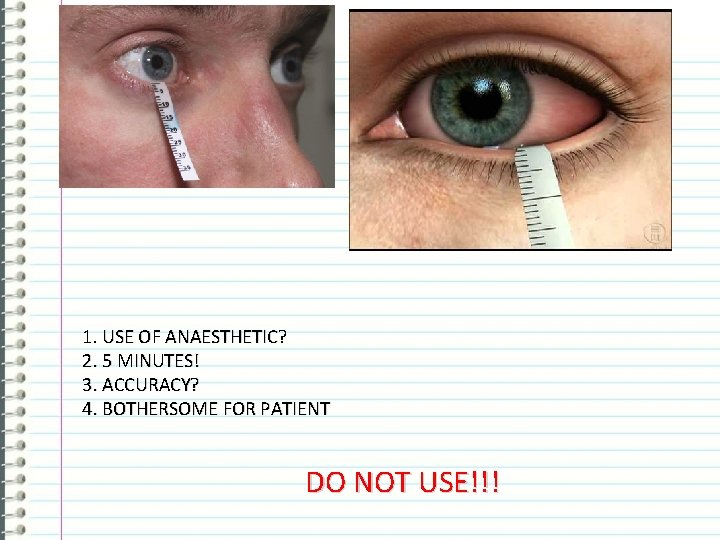
Schirmer test 1. Instil a drop of local anaesthetic into the eye, (optional). 2. Prepare a filter paper (5 mm x 35 mm with folded end). 3. Gently dry the eye. 4. Apply the filter paper with the folded end hooked onto the lower lid margin at the junction between the middle and outer third (take care not to touch the cornea). 5. Tell patient to keep their eye open and blink normally. 6. Measure the amount of wetting after 5 minutes: 13 -15 mm wetting rules out a dry eye; 6 -10 mm is borderline and less than 6 mm indicates dry eye. 7. The filter paper strips can cause reflex tearing and may require the use of anaesthetic agents. However, they still provide a measurable clinical indication of dry eye.
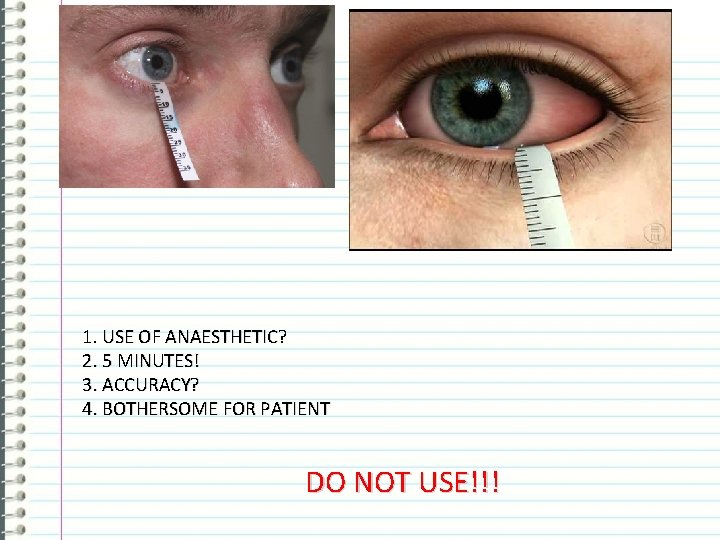
1. USE OF ANAESTHETIC? 2. 5 MINUTES! 3. ACCURACY? 4. BOTHERSOME FOR PATIENT DO NOT USE!!!
The LACRYMETER™ by ECCG GROUP Ltd
The Lacrymeter A paper strip impregnated with phenol red dye. Phenol red is p. H sensitive and changes from yellow to red when wetted by tears. On the other end a sensitive p. H dye is used.
Pretest Examining the patient performing the Lacryp. Hmeter™ test does not require any anaesthetic. If patient is using any kind of eye drop, the patient must not instill drops 1 hour before the examination. However, if the patient is wearing contact lenses, these can be worn during performance of test.
Instruction for use 1. Place the 3 mm hook over the lower eyelid approximately 5 mm from the lateral canthus when the eyelid is pulled out slightly, release the eyelid and start a stop clock and ask patient to look straight ahead and blink as normal. 2. Each eye is individually tested with open eyes and normal blinking for 30 seconds. 3. Remove the strip gently. Pull the lower eyelid down before removing the thread and patient will not have any discomfort. 4. Measure the entire length of where the strip has changed color from yellow to red including the fold.
Lacrymeter™ Functional Mode Yellow (acidic) color on removal from wrapper and before contact with tears Changes to red (basic) indicating the volume of tears soaked up over the time of contact Borderline If change of color of thread less than 10 mm, the tear quantity must be considered to be low. And the eye must be suspected to being dry. For p. H. Compare with supplied scale of p. H. Indicating acidic or basic tears. A p. H meter provides a value as to how acidic or alkaline a liquid is. The basic principle of the p. H meter is to measure the concentration of hydrogen ions. Acids dissolve in water forming positively charged hydrogen ions (H+).
The Lacryp. H© Test one eye at a time. Gently touch eye temporally for 2 -4 seconds with the p. H end of strip p. H stands for power of hydrogen, which is a measurement of the hydrogen ion concentration in the body. The total p. H scale ranges from 1 to 14, with 7 considered to be neutral. A p. H less than 7 is said to be acidic and solutions with a p. H greater than 7 are basic or alkaline.
More on p. H The mean p. H values of 40 eyes from 20 healthy volunteers was 7. 50 (SD ± 0. 23), which corresponded well with those measured by the micro p. H-meter. CONCLUSIONS. The method described was useful in measuring the p. H of the precorneal tear film of humans with minimal invasion. Depleted mucous: Yes. Indirectly because the mucous level is down. Meibomian gland dysfuntion: Yes. Indirectly because the evaporation goes up
Treat p. H • If tears too alcidic - give tear substitute that is basic in p. H • If tears too basic - give tear substituted that is alcidic in p. H.
STAIN TESTS
Rose Bengal Test The dye has been shown to be toxic to corneal epithelium at routine concentrations. Stinging DO NOT USE!!!!
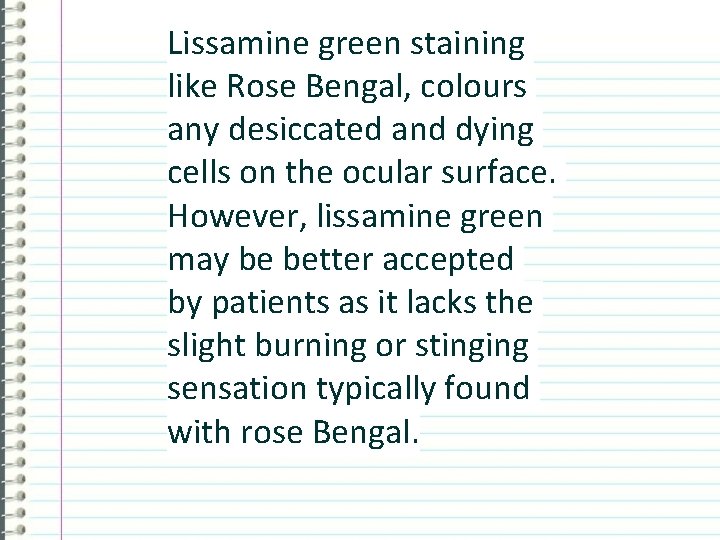
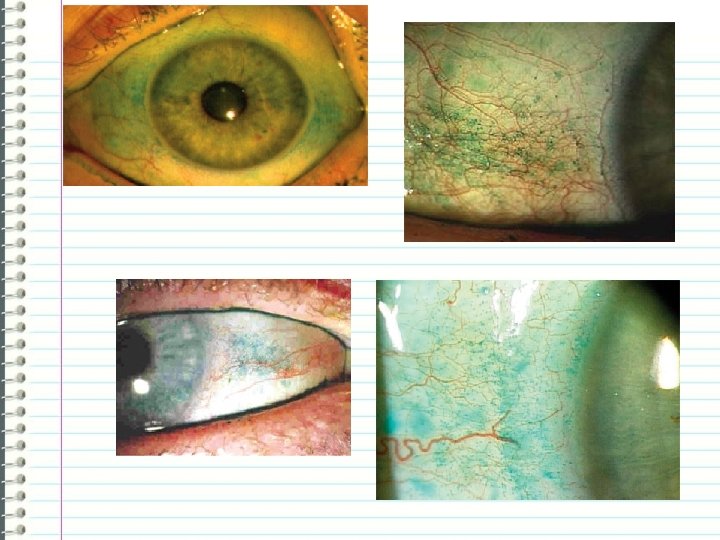
Lissamine Green
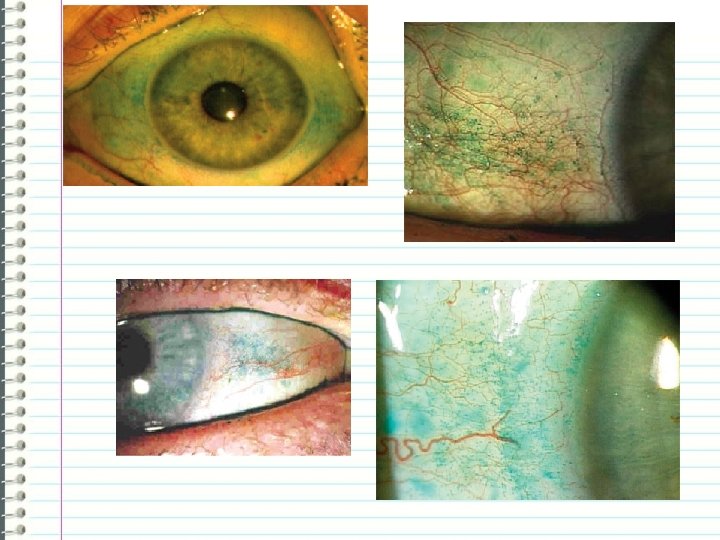
Lissamine green staining like Rose Bengal, colours any desiccated and dying cells on the ocular surface. However, lissamine green may be better accepted by patients as it lacks the slight burning or stinging sensation typically found with rose Bengal.

HYPEROSMOLARITY TEST
Tearlab Osmolarity System The disposable probe, touched onto the lower tear meniscus at the lid margin, collects a nanolitre sample of tears, which is analysed within seconds to provide the clinician with an osmolarity reading. Normal values lie around 304 m. Osm/kg while values over 320 m. Osm/kg indicate dry eye. (Mainly used in research). TOO EXPENSIVE! HOW LONG WILL IT BE AVAILABLE? ? ?
 Claes feinbaum
Claes feinbaum Symbolic probability rules
Symbolic probability rules Wedge film journal bearing
Wedge film journal bearing Is measure for measure a comedy
Is measure for measure a comedy What weather instrument measures air temperature
What weather instrument measures air temperature If you don't measure it you can't manage it
If you don't measure it you can't manage it If you can’t measure it, you can’t manage it
If you can’t measure it, you can’t manage it If you cant measure it you can't manage it
If you cant measure it you can't manage it What you can't measure you can't manage
What you can't measure you can't manage You cant manage what you dont measure
You cant manage what you dont measure Structured light
Structured light Lisa cannada md
Lisa cannada md What is a tear stream
What is a tear stream Draft a circular letter announcing change in premises
Draft a circular letter announcing change in premises Past participle notes
Past participle notes Palettes and tear-off menus
Palettes and tear-off menus Periclitoral laceration during delivery
Periclitoral laceration during delivery Patriotic tear
Patriotic tear Bayonet charge tone
Bayonet charge tone Tear drop of india
Tear drop of india Tear drop of india
Tear drop of india Tear drop of india
Tear drop of india Foosh injury
Foosh injury Whats a husband stitch
Whats a husband stitch Tear drop of india
Tear drop of india Perineal tear classification rcog
Perineal tear classification rcog Palettes and tear-off menus
Palettes and tear-off menus Torn paper drawing
Torn paper drawing J shaped muscular sac
J shaped muscular sac Horseshoe tear
Horseshoe tear Digestion types
Digestion types Mash, grind, mix and tear food.
Mash, grind, mix and tear food. Epiphora
Epiphora Gluteus medius tear
Gluteus medius tear Diagnose ascites
Diagnose ascites Heat for meniscus tear
Heat for meniscus tear Homographs examples tear
Homographs examples tear Does software wear & tear by decomposition ?
Does software wear & tear by decomposition ? Knee lateral joint line
Knee lateral joint line Elements of wimp interface in hci
Elements of wimp interface in hci Mallory wiess tear
Mallory wiess tear Iad wondzorg
Iad wondzorg