Virtual Noon Report Three Shoulders in Three Weeks
- Slides: 24
Virtual Noon Report: Three Shoulders in Three Weeks AN EVIDENCE BASED APPROACH TO NON-TRAUMATIC SHOULDER COMPLAINTS KELSI MANLEY MD 3. 16. 2020 CHIEF FACILITATOR: KIM CHESTEEN MD
Three Shoulders in Three Weeks Last month, I spent three weeks rotating through various primary care clinics as a part of my Primary Care Track experience. This rotation’s emphasis was on Sports Medicine, and with the following three cases, I found myself revisiting the key history and exam maneuvers that assist in delineating shoulder complaints. We will review 3 cases related to 3 common, separate causes of shoulder pain. This is not an all encompassing shoulder talk, but rather meant to outline high-yield, bread-andbutter shoulder disease. Please click through in Presentation Mode and either silently with yourself or together aloud with your team, follow prompts for questions and/or exam maneuvers:
Case #1: HPI 72 yo M with HTN, obesity, otherwise healthy presents for evaluation of shoulder pain. Onset: ◦ 3 months ago, insidious onset Progression: ◦ Feels it is getting worse, no clear injury Quality: ◦ Dull, achy. Occasionally sharp. Radiation: Why is this question important & if he has radiating pain, what might you consider? ◦ No Radiation ◦ Radiating pain down the arm increases the likelihood of cervical pathology Severity: ◦ Was hoping to paint his garage this weekend, but no longer thinks he will be able to. Is retired. Location: ◦ Points to his lateral deltoid and posterior shoulder
Additional Questions: Shoulder Evaluation: Provoking Movements: Overhead activity Nocturnal Symptoms: Present * LR for Nocturnal OR Rest Symptoms Indicating Rotator Cuff Disease= 0. 125 ≠ NOT helpful Symptoms at Rest: Absent * Weakness: Unclear. He struggles to lift his arm, but can’t tell if it’s just because it hurts.
Quiz Yourself: List the most (5) most common categories of MSK shoulder pain presenting to the ambulatory office? 1. Rotator Cuff Disorder 2. Glenohumeral Disorder 3. Acromioclavicular Disease 4. Referred Cervical Pain 5. Biceps Tendinopathy
Quiz Yourself: For Each Category, List Common Causes of Shoulder Pain: 1. Rotator Cuff Disease: ◦ ◦ Impingement Syndrome Rotator Cuff Tendonitis Subacromial Bursitis Partial or Full Thickness Tendon Tear 2. Glenohumeral Pathology: ◦ Adhesive Capsulitis ◦ Glenohumeral Arthritis * 3. Acromioclavicular Disease Top 3 have similar presentation and treatment strategy Very rare, nonweight-bearing joint ◦ AC Joint Separation/Injury ◦ AC Joint Arthritis
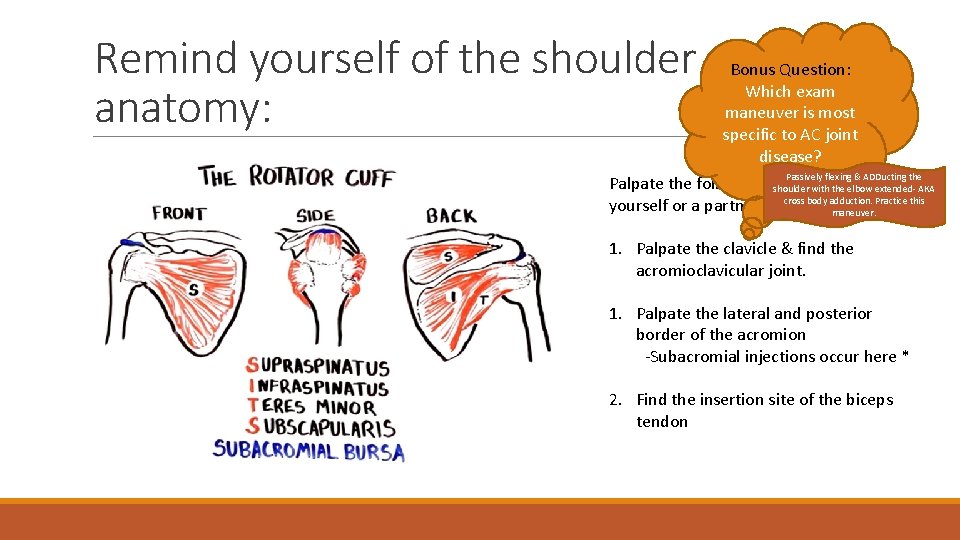
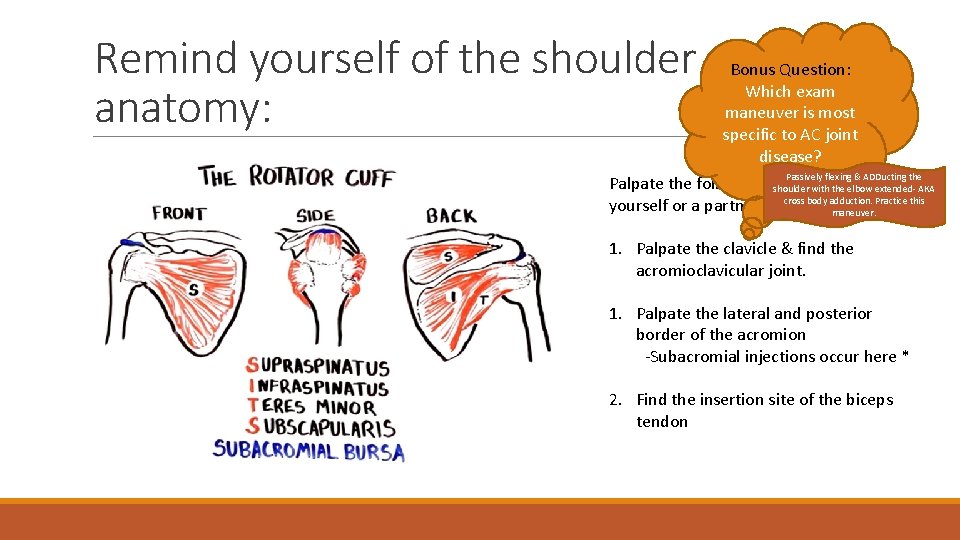
Remind yourself of the shoulder anatomy: Bonus Question: Which exam maneuver is most specific to AC joint disease? Passively flexing & ADDucting the Palpate the following structures shoulder with the on elbow extended- AKA cross body adduction. Practice this yourself or a partner: maneuver. 1. Palpate the clavicle & find the acromioclavicular joint. 1. Palpate the lateral and posterior border of the acromion -Subacromial injections occur here * 2. Find the insertion site of the biceps tendon
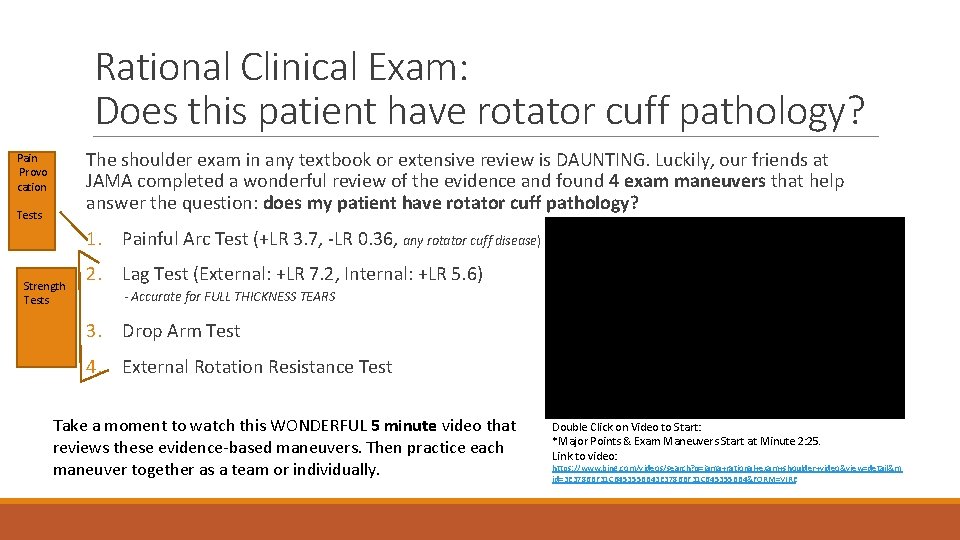
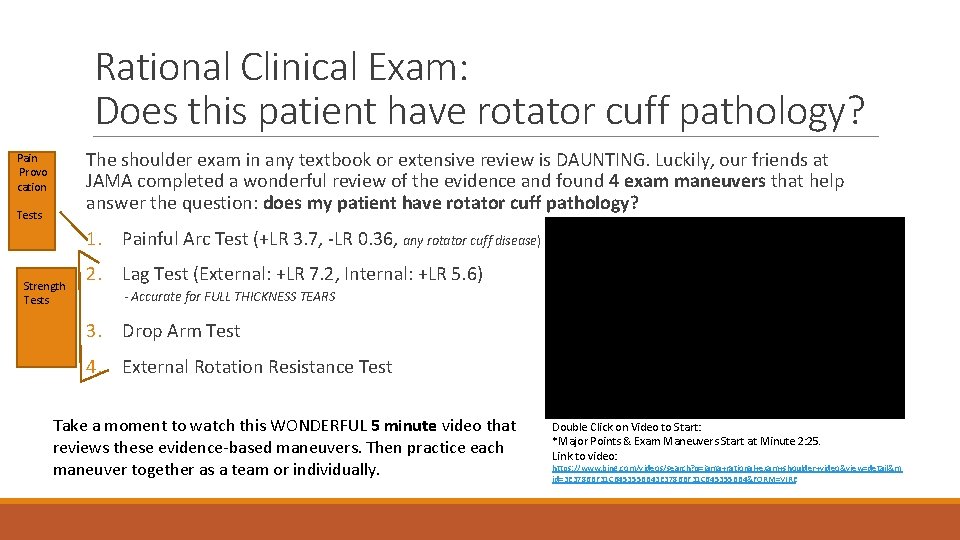
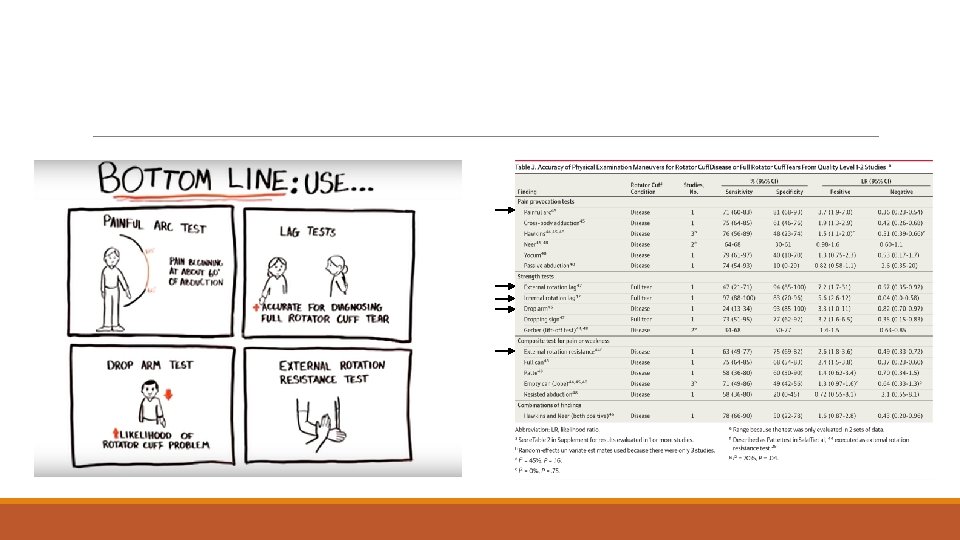
Rational Clinical Exam: Does this patient have rotator cuff pathology? The shoulder exam in any textbook or extensive review is DAUNTING. Luckily, our friends at JAMA completed a wonderful review of the evidence and found 4 exam maneuvers that help answer the question: does my patient have rotator cuff pathology? Pain Provo cation Tests 1. Painful Arc Test (+LR 3. 7, -LR 0. 36, any rotator cuff disease) Strength Tests 2. Lag Test (External: +LR 7. 2, Internal: +LR 5. 6) - Accurate for FULL THICKNESS TEARS 3. Drop Arm Test 4. External Rotation Resistance Test Take a moment to watch this WONDERFUL 5 minute video that reviews these evidence-based maneuvers. Then practice each maneuver together as a team or individually. Double Click on Video to Start: *Major Points & Exam Maneuvers Start at Minute 2: 25. Link to video: https: //www. bing. com/videos/search? q=jama+rational+exam+shoulder+video&view=detail&m id=3 E 3786 BF 31 C 645355 BB 4&FORM=VIRE
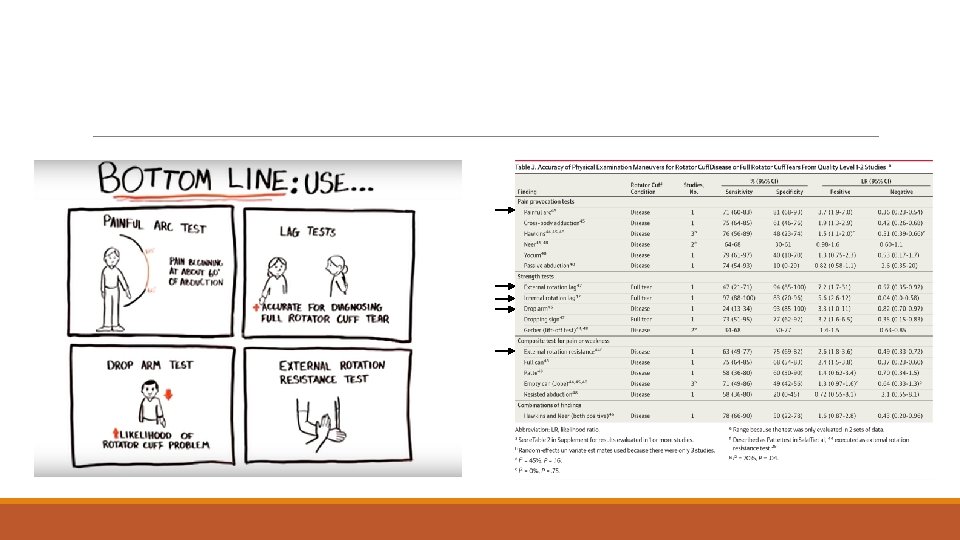
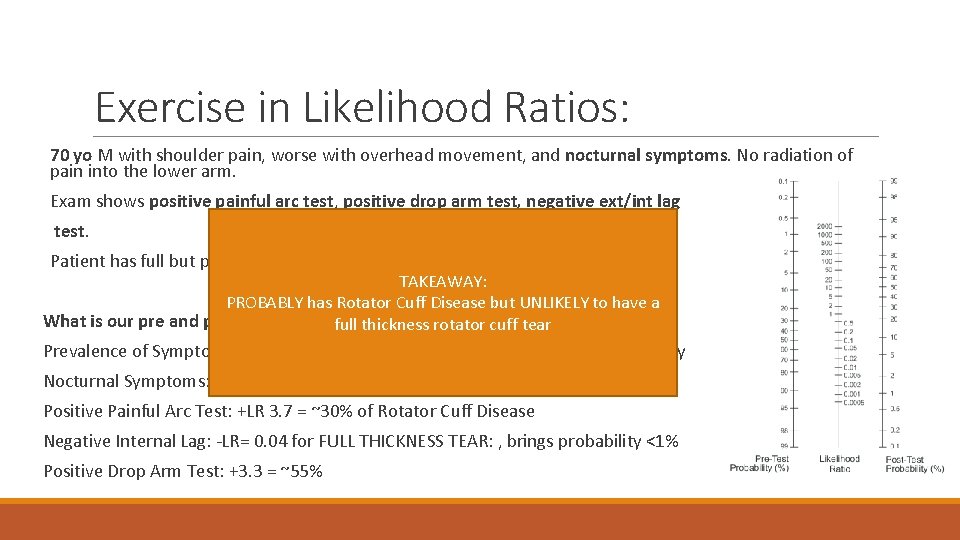
Exercise in Likelihood Ratios: 70 yo M with shoulder pain, worse with overhead movement, and nocturnal symptoms. No radiation of pain into the lower arm. Exam shows positive painful arc test, positive drop arm test, negative ext/int lag test. Patient has full but painful passive ROM. TAKEAWAY: PROBABLY has Rotator Cuff Disease but UNLIKELY to have a What is our pre and post test probability of rotator cuff disease? full thickness rotator cuff tear Prevalence of Symptomatic Rotator Cuff Disease > 70 yo: 15% = pre-test probability Nocturnal Symptoms: does not alter our probability = 15% Positive Painful Arc Test: +LR 3. 7 = ~30% of Rotator Cuff Disease Negative Internal Lag: -LR= 0. 04 for FULL THICKNESS TEAR: , brings probability <1% Positive Drop Arm Test: +3. 3 = ~55%
CASE #2: 65 yo M with DM, hypothyroidism presenting with 3 months of severe shoulder pain, reduced range of motion Onset: ◦ 3 months ago, fairly rapid onset Progression: ◦ Feels it is getting worse, no clear injury Quality: ◦ Sharp, catching. Very stiff. Radiation: ◦ No radiation of pain Severity: ◦ Unable to perform household tasks, combing his hair is difficult Location: ◦ ‘All around’ the joint
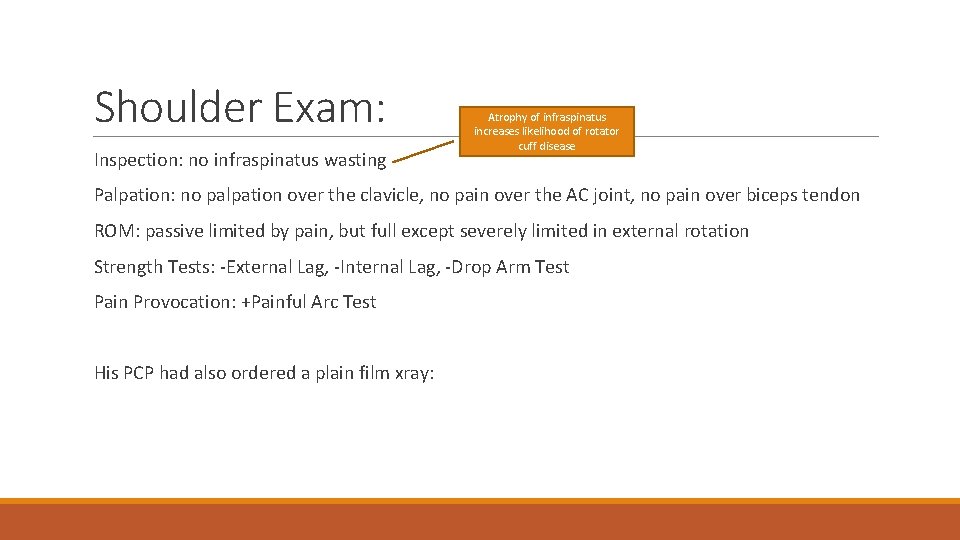
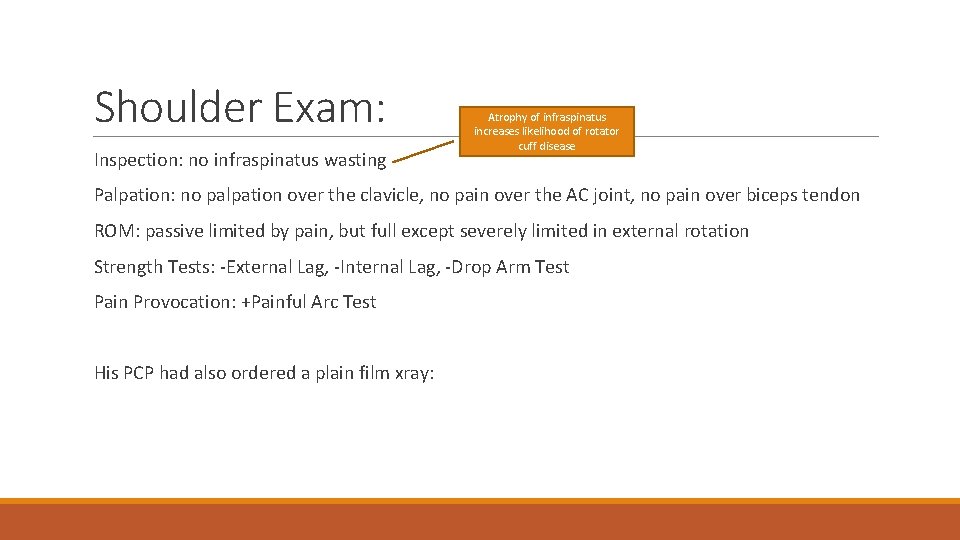
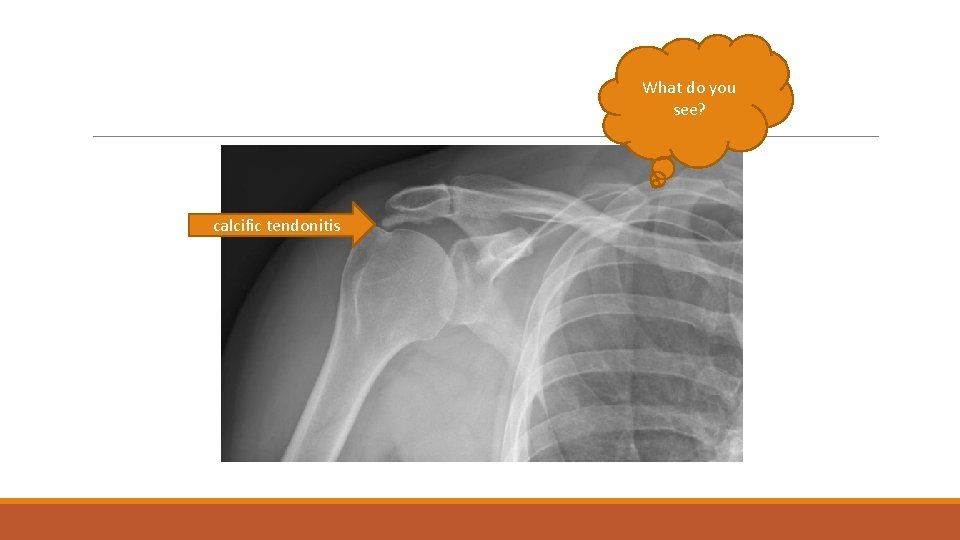
Shoulder Exam: Inspection: no infraspinatus wasting Atrophy of infraspinatus increases likelihood of rotator cuff disease Palpation: no palpation over the clavicle, no pain over the AC joint, no pain over biceps tendon ROM: passive limited by pain, but full except severely limited in external rotation Strength Tests: -External Lag, -Internal Lag, -Drop Arm Test Pain Provocation: +Painful Arc Test His PCP had also ordered a plain film xray:
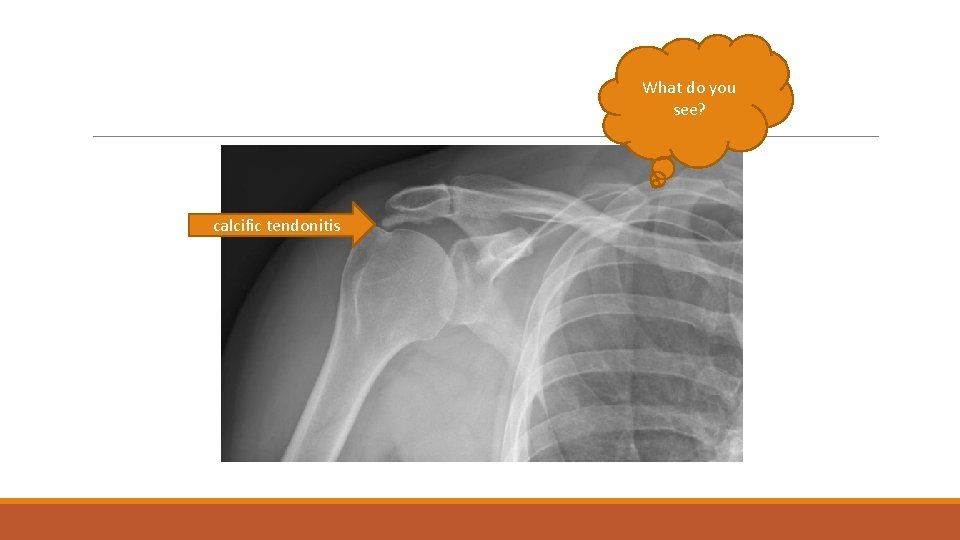
What do you see? calcific tendonitis
Quiz Yourself How can you counsel this patient about his chances of improvement if he does nothing, or just does home exercises/PT and ibuprofen? • 50% of calcific tendinopathy resolves within 3 months spontaneously or w/ conservative therapy • 20% more (for total of 70% *math*) will improve within 1 year • 30% of patients either don’t get better or have recurrence of pain That can be a LONG year, if you’re in significant pain. What additional therapies have modest evidence to support their use? • Subacromial Steroid Injection in PCP office reliably provides acute pain relief and increased adherence with exercises • Extracorpreal Shockwave Therapy: Acoustic breakup of calcific deposits. Good evidence for improvement in the short term, less robust data but appears to also improve outcomes at up to 1 year. • Needling: Sports Medicine at OHSU performs. Using US, insert needle into deposit, and ‘suck out’ the calcium. Takes 20 minutes. Systematic Review showed 55% of those who failed conservative treatment had pain improvement.
Quiz Yourself What percent of patients who do conservative therapy, ECSW, and Needling will continue to have symptoms? • 10 % will require surgical evaluation after failing PT, subacromial injection, needling, ECSW therapy You picked up on severely limited passive external rotation on exam. What concomitant condition does this suggest? • Adhesive Capsulitis Which of his medical problems predispose him to adhesive capsulitis? • Strong relationship with DM. Also associated to a lesser extent with thyroid disease, pts on anti-retrovirals, strokes, and Pakinson’s What is the reported lifetime prevalence of frozen shoulder in patients with diabetes? • Upwards of 20%. In Type I DM, as high as 59 -76%!! What could you do to test the hypothesis that this patient also has glenohumeral disease, or frozen shoulder (adhesive capsulitis)? • Injection Test : inject the subacromial space with lidocaine +/- steroid, if passive ROM is still limited, increases likelihood of frozen shoulder
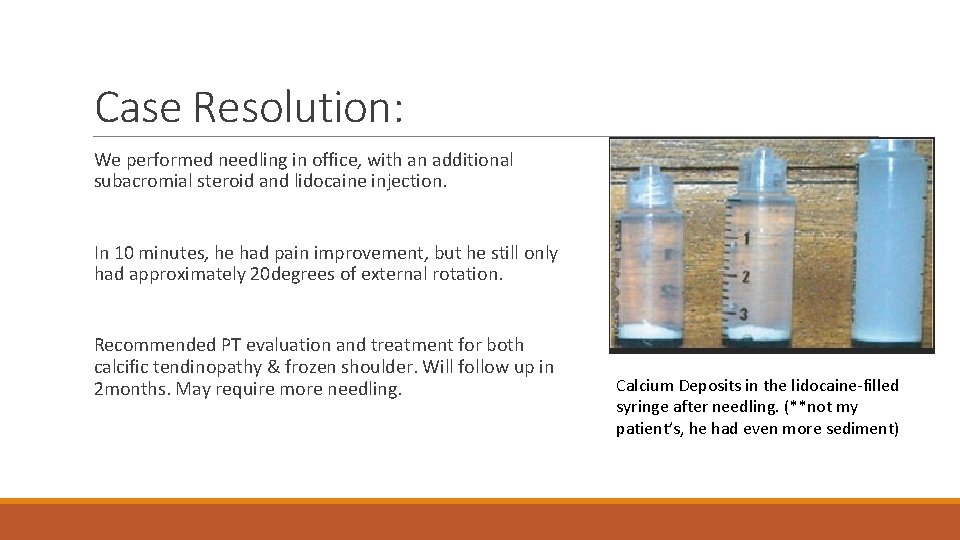
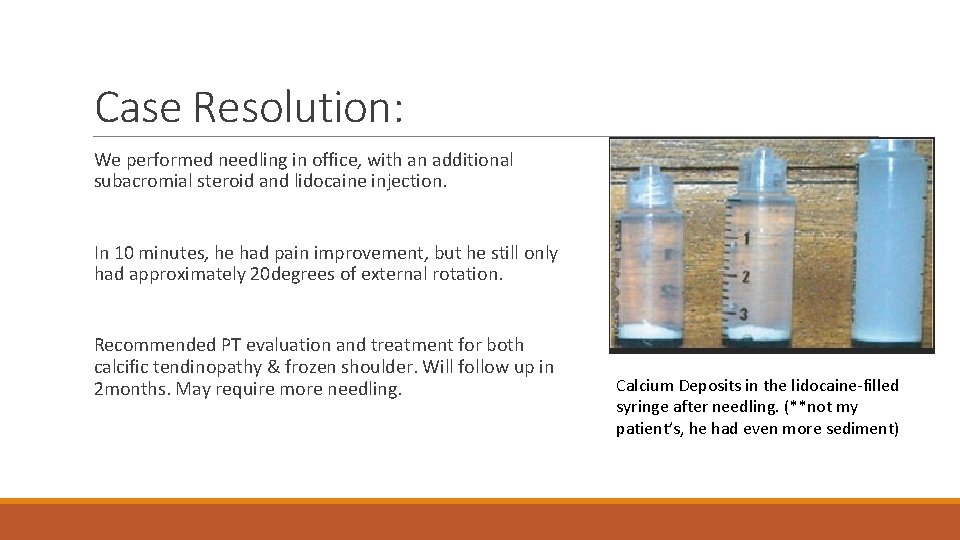
Case Resolution: We performed needling in office, with an additional subacromial steroid and lidocaine injection. In 10 minutes, he had pain improvement, but he still only had approximately 20 degrees of external rotation. Recommended PT evaluation and treatment for both calcific tendinopathy & frozen shoulder. Will follow up in 2 months. May require more needling. Calcium Deposits in the lidocaine-filled syringe after needling. (**not my patient’s, he had even more sediment)
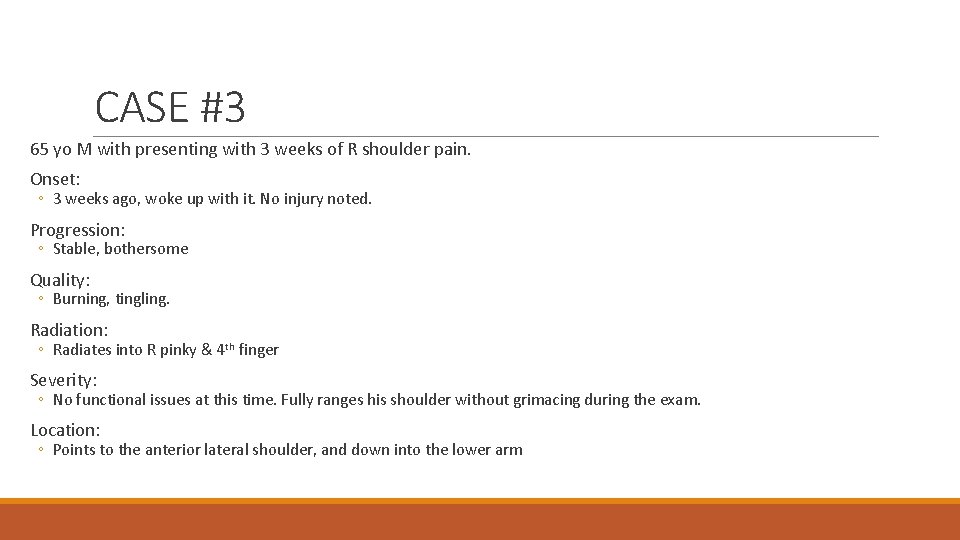
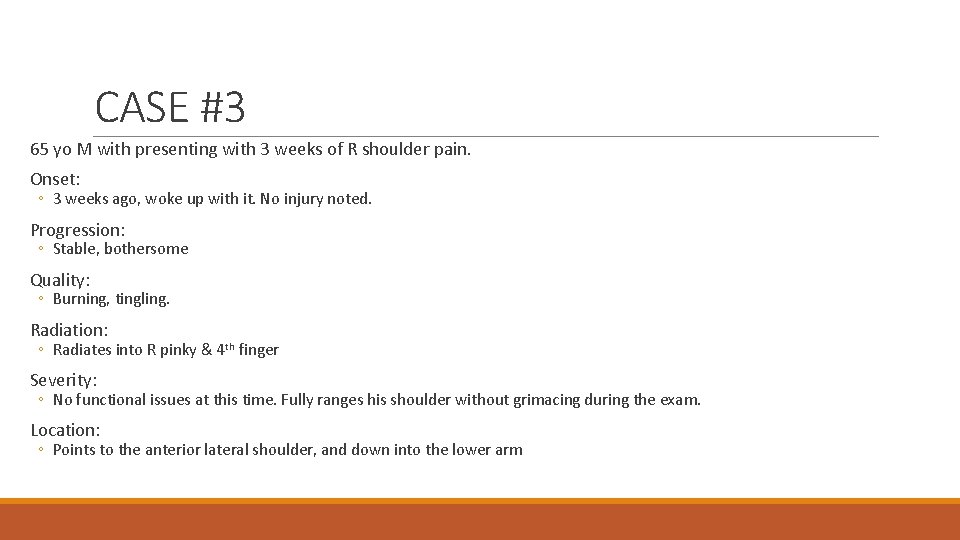
CASE #3 65 yo M with presenting with 3 weeks of R shoulder pain. Onset: ◦ 3 weeks ago, woke up with it. No injury noted. Progression: ◦ Stable, bothersome Quality: ◦ Burning, tingling. Radiation: ◦ Radiates into R pinky & 4 th finger Severity: ◦ No functional issues at this time. Fully ranges his shoulder without grimacing during the exam. Location: ◦ Points to the anterior lateral shoulder, and down into the lower arm
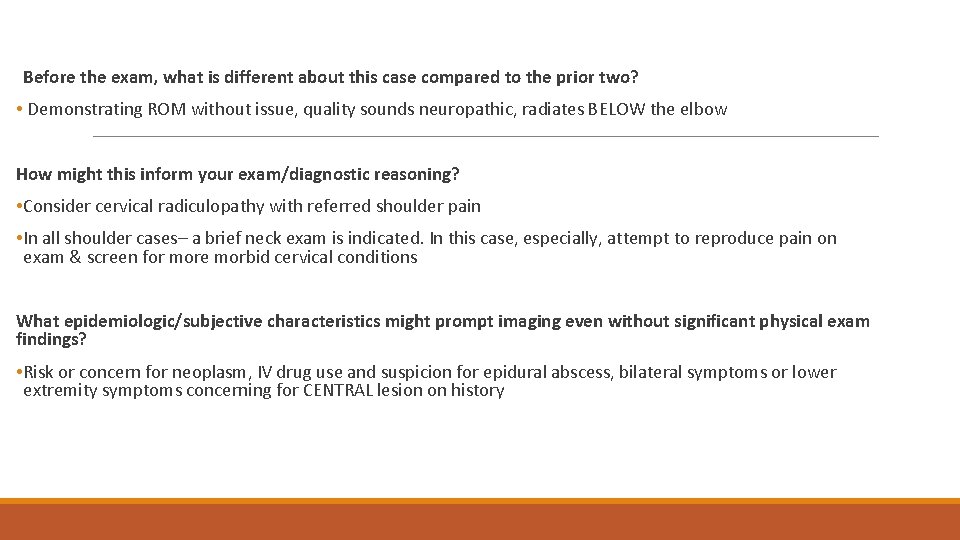
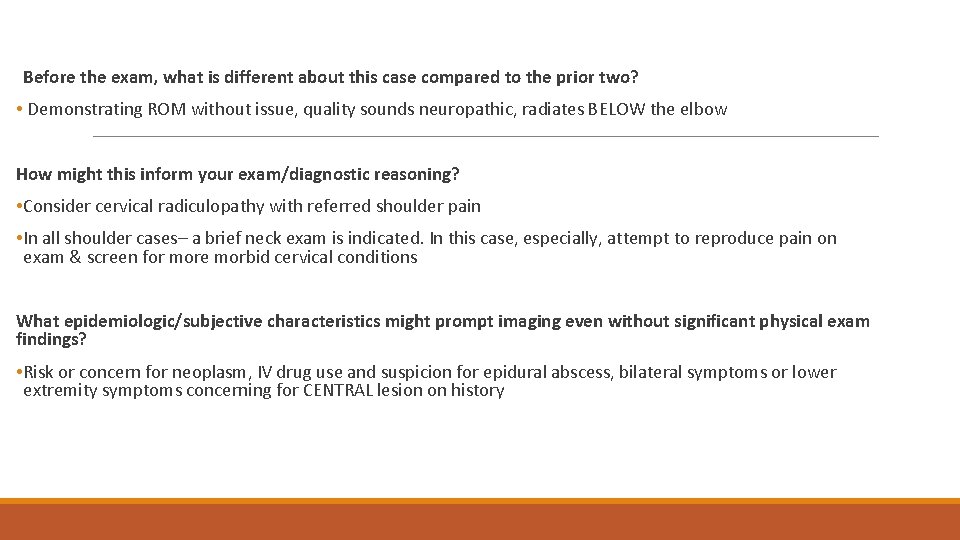
Before the exam, what is different about this case compared to the prior two? • Demonstrating ROM without issue, quality sounds neuropathic, radiates BELOW the elbow How might this inform your exam/diagnostic reasoning? • Consider cervical radiculopathy with referred shoulder pain • In all shoulder cases– a brief neck exam is indicated. In this case, especially, attempt to reproduce pain on exam & screen for more morbid cervical conditions What epidemiologic/subjective characteristics might prompt imaging even without significant physical exam findings? • Risk or concern for neoplasm, IV drug use and suspicion for epidural abscess, bilateral symptoms or lower extremity symptoms concerning for CENTRAL lesion on history
Physical Exam: Inspection: no infraspinatus wasting Palpation: no palpation over the clavicle, no pain over the AC joint, no pain over biceps tendon. No pain over cervical spine in the midline or paraspinal muscles Shoulder ROM: Full active and passive ROM without pain Strength Tests: -External Lag, -Internal Lag, -Drop Arm Test Pain Provocation: -Painful Arc Test
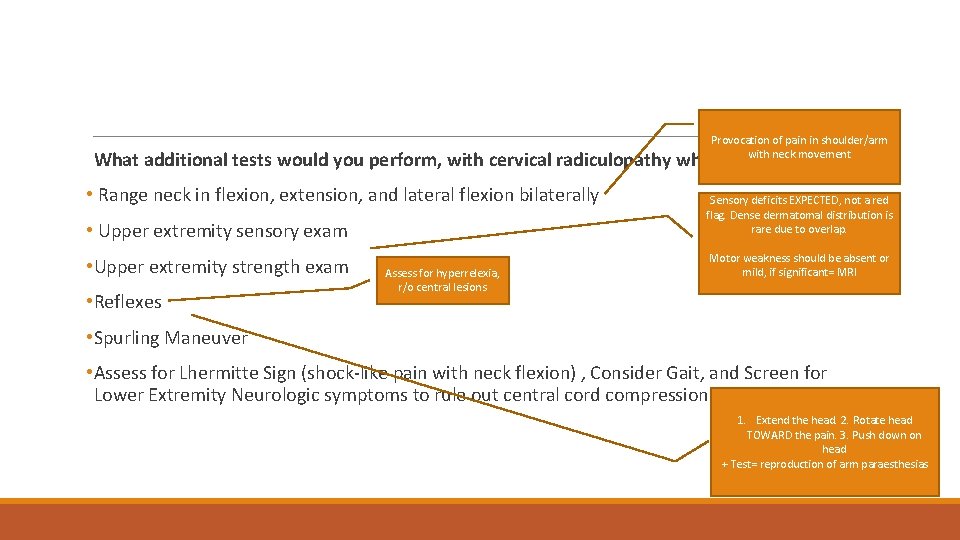
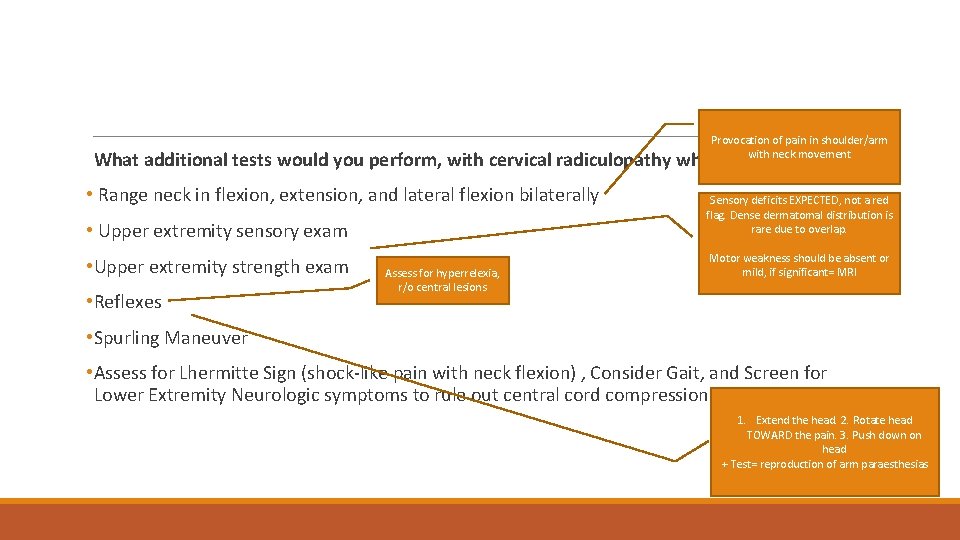
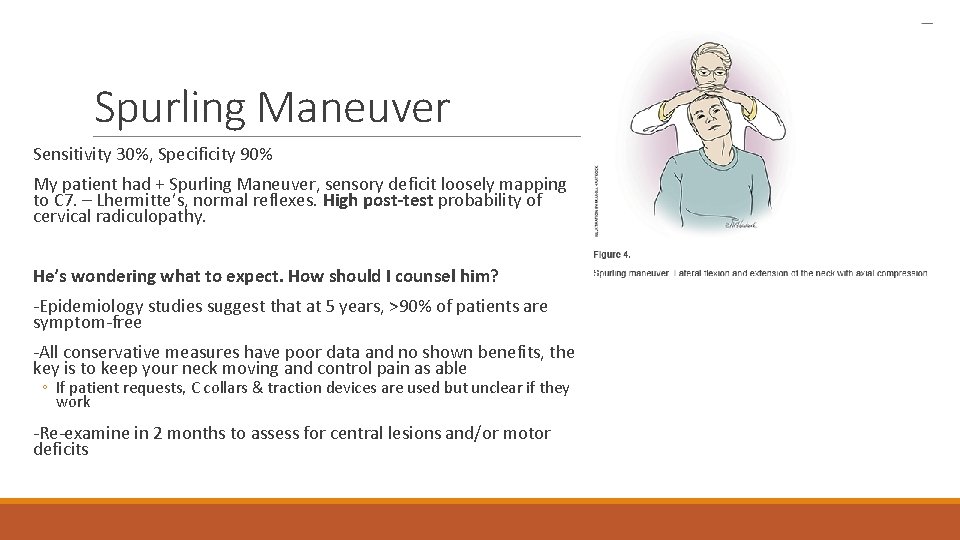
Provocation of pain in shoulder/arm with neck movement What additional tests would you perform, with cervical radiculopathy what might you expect? • Range neck in flexion, extension, and lateral flexion bilaterally • Upper extremity sensory exam Sensory deficits EXPECTED, not a red flag. Dense dermatomal distribution is rare due to overlap. • Upper extremity strength exam Motor weakness should be absent or mild, if significant= MRI • Reflexes Assess for hyperrelexia, r/o central lesions • Spurling Maneuver • Assess for Lhermitte Sign (shock-like pain with neck flexion) , Consider Gait, and Screen for Lower Extremity Neurologic symptoms to rule out central cord compression 1. Extend the head. 2. Rotate head TOWARD the pain. 3. Push down on head + Test= reproduction of arm paraesthesias
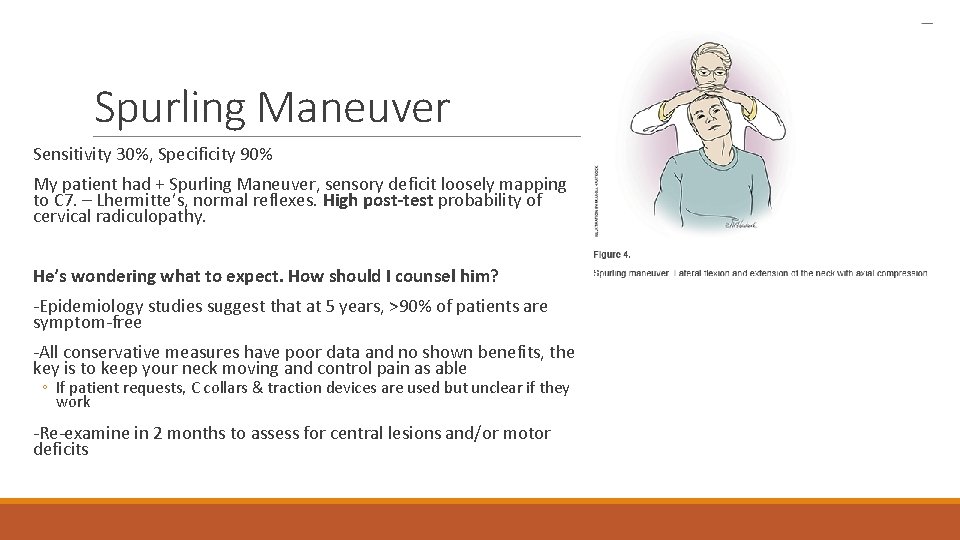
Spurling Maneuver Sensitivity 30%, Specificity 90% My patient had + Spurling Maneuver, sensory deficit loosely mapping to C 7. – Lhermitte’s, normal reflexes. High post-test probability of cervical radiculopathy. He’s wondering what to expect. How should I counsel him? -Epidemiology studies suggest that at 5 years, >90% of patients are symptom-free -All conservative measures have poor data and no shown benefits, the key is to keep your neck moving and control pain as able ◦ If patient requests, C collars & traction devices are used but unclear if they work -Re-examine in 2 months to assess for central lesions and/or motor deficits
Quick Hit Trivia: Name 5 Indications for Subacromial Steroid Injection: • Impingement Syndrome * • Rotator cuff tendonitis * *after failure of conservative therapy OR to improve PT engagement • Subacromial Bursitis • Diagnostic Evaluation if uncertainty about etiology of pain • Pain relief to perform accurate passive ROM to rule out adhesive capsulitis Describe the common presenting complaint of a patient with biceps tendinopathy: • Pain with carrying a load with a flexed elbow Name indications for Orthopedic Referral in patients with shoulder pain: • Suspected Rotator Cuff Tear w/ Weakness • Rotator Cuff Disease w/o Tear that fails SIX-NINE MONTHS of conservative therapy • Adhesive Capsulitis that fails conservative therapy
Take Home Points: • In patients with shoulder complaints, try to characterize into 5 main categories: rotator cuff disease, glenohumeral disease, cervical radiculopathy referred pain, AC joint disease, biceps tendinopathy • There are evidence-based ways of delineating between the above categories. The best shoulder exam includes targeted inspection for infraspinatus wasting, palpation of the AC joint and biceps tendon, passive ROM to assess the glenohumeral joint, and FOUR exam maneuvers for rotator cuff disease + brief neck exam. • Most conditions benefit from targeted conservative therapies. The main finding that warrants early cross-sectional imaging is objective weakness. • Convince yourself with each patient that they do NOT have cervical spinal disease, and if they do rule out central lesions with a careful physical exam.
References 1. JAMA. Rational Clinical Exam of the Shoulder. 2. AAFP. The Painful Shoulder: Part I. 3. Ultrasound-guided percutaneous irrigation in rotator cuff calcific tendinopathy: what is the evidence? A systematic review with proposals for future reporting. AULanza E, Banfi G, Serafini G, Lacelli F, Orlandi D, Bandirali M, Sardanelli F, Sconfienza LM. Eur Radiol 2015. 4. AAFP. 2016. Nonoperative Management of Cervical Radiculopathy. MARC A. CHILDRESS, MD, Fairfax Family Practice Primary Care Sports Medicine Fellowship, Fairfax, Virginia. BLAIR A. BECKER, MD, Group Health Family Medicine Residency, Seattle, Washington.