Viral infections Dr Mohammad Arif Abid wartsverruca vulgaris
Viral infections Dr. Mohammad Arif Abid
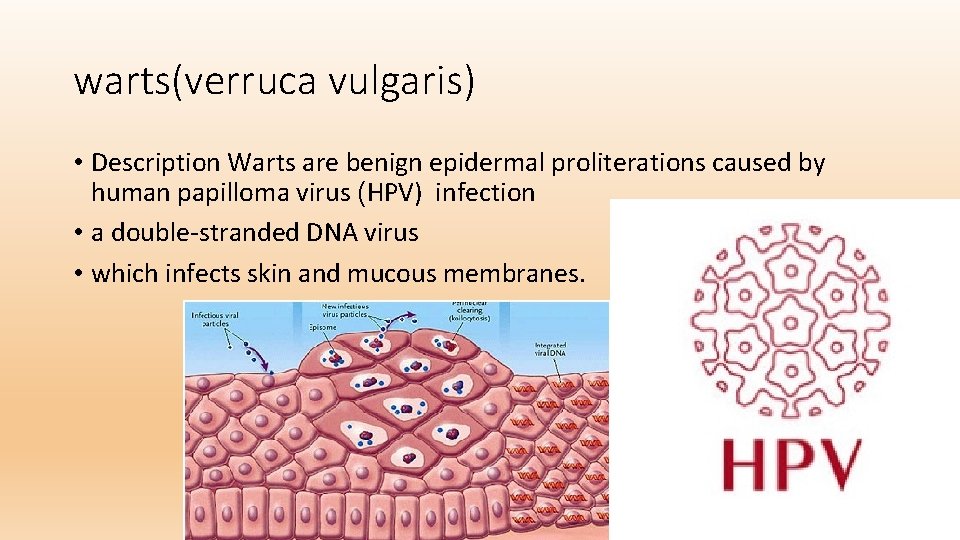
warts(verruca vulgaris) • Description Warts are benign epidermal proliterations caused by human papilloma virus (HPV) infection • a double-stranded DNA virus • which infects skin and mucous membranes.
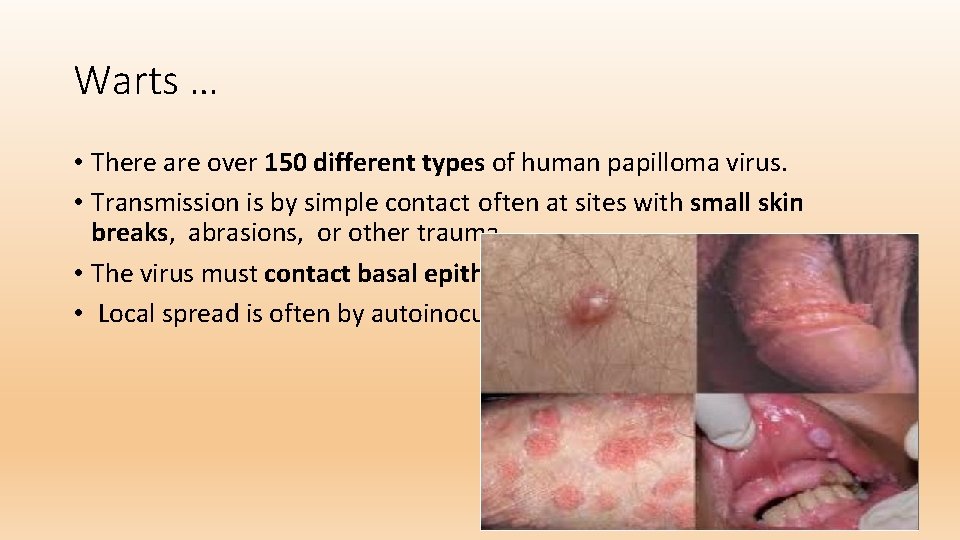
Warts … • There are over 150 different types of human papilloma virus. • Transmission is by simple contact often at sites with small skin breaks, abrasions, or other trauma • The virus must contact basal epithelial cells for infection to occur. • Local spread is often by autoinoculation.
History • The estimated incidence of infection is 10% in children and young adults. • The peak incidence is age 12 -16 years. • The incubation period is variable: 1 -6 months for common warts. .
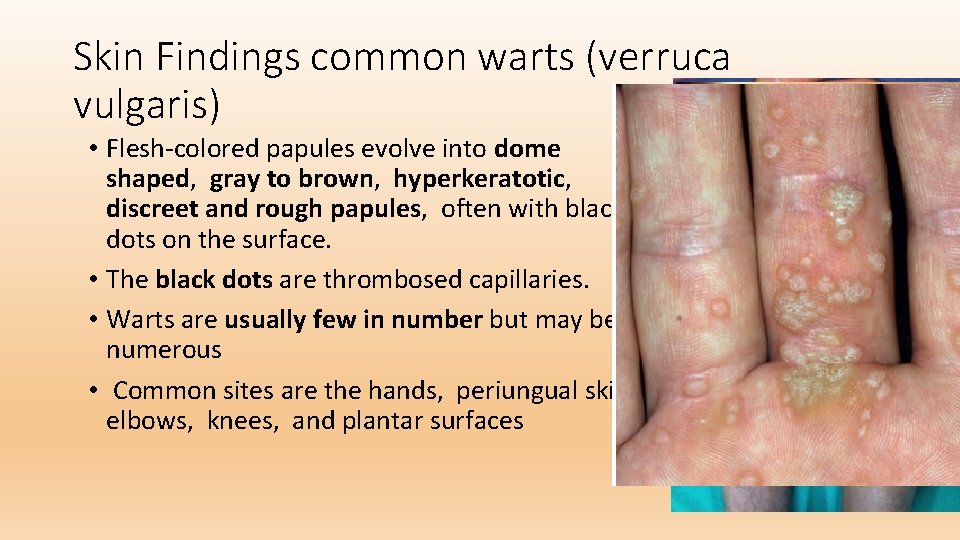
Skin Findings common warts (verruca vulgaris) • Flesh-colored papules evolve into dome shaped, gray to brown, hyperkeratotic, discreet and rough papules, often with black dots on the surface. • The black dots are thrombosed capillaries. • Warts are usually few in number but may be numerous • Common sites are the hands, periungual skin, elbows, knees, and plantar surfaces
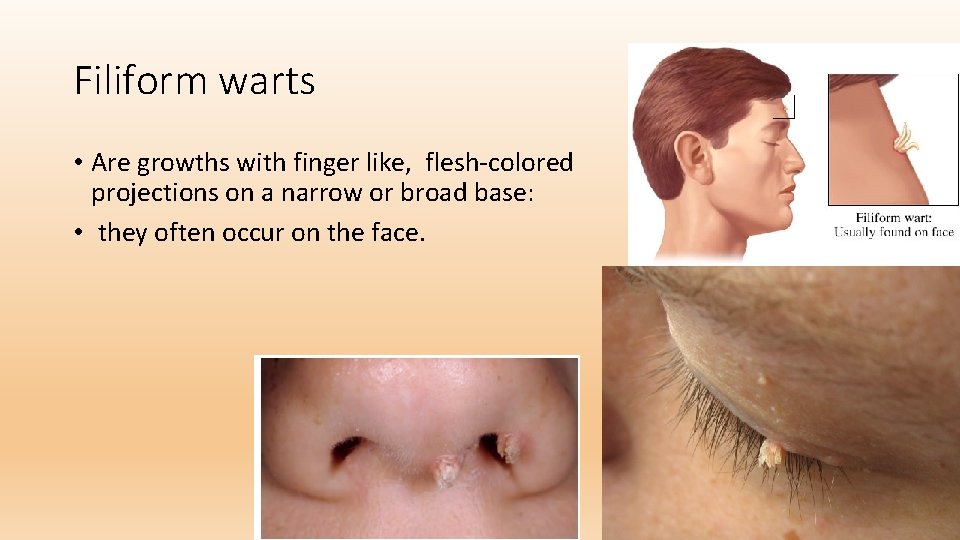
Filiform warts • Are growths with finger like, flesh-colored projections on a narrow or broad base: • they often occur on the face.
Treatment • Multiple treatments are available for warts. • No single treatment is consistently highly effective. • topical salicylic acid preparations(15 -40%) are applied once the a day • The preparations may be occluded with tape to increase penetration. The duration of treatment is often lengthy (8 -12 weeks). • Cure rate with salicylic acid preparations is 75% compared with 48% with placebo.

Treatment • Vinegar soak • Imoquimd 5% • Liquid nitrogen + 17% salicylic acid • Laser therapy • Currete filiform wart
Flat Warts Description • Flat warts are benign cutaneous hyperproliferation due to infection human papilloma virus. • Common subtypes are types 3 and 10.
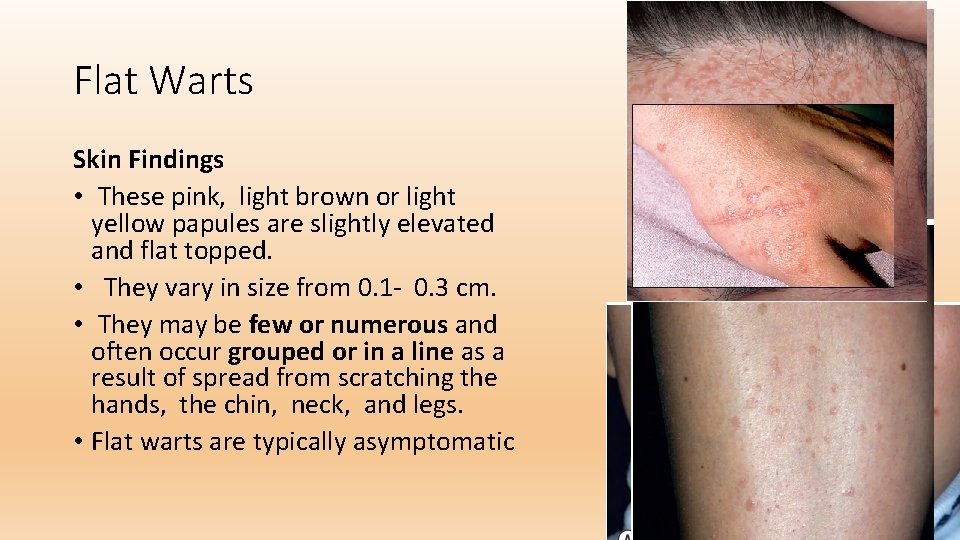
Flat Warts Skin Findings • These pink, light brown or light yellow papules are slightly elevated and flat topped. • They vary in size from 0. 1 - 0. 3 cm. • They may be few or numerous and often occur grouped or in a line as a result of spread from scratching the hands, the chin, neck, and legs. • Flat warts are typically asymptomatic
Flat Warts Treatment • If sparse numbers of lesions, a salicylic acid preparation may be applied daily directly to each lesion • This treatment is limited by irritation. • Applied Imiquimod 5% cream frequency affected skin at night • Tretinoin cream 0. 025%, 0. 05%, or 0. 1% • 5 fluorouracil 3 -5 weeks 2 times/day

Planter Warts Description • plantar warts are caused by human papilloma virus infection on the plantar foot. • Warts frequently occur at points of maximal pressure, such as over the heads of the metatarsal bones, the heels or the toes. • A cluster of many warts is referred to as a"mosaic wart".
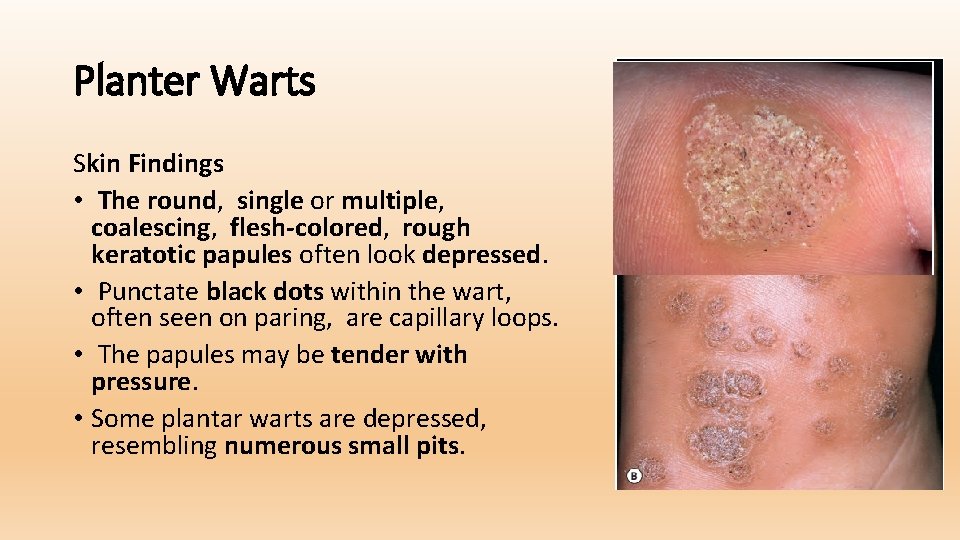
Planter Warts Skin Findings • The round, single or multiple, coalescing, flesh-colored, rough keratotic papules often look depressed. • Punctate black dots within the wart, often seen on paring, are capillary loops. • The papules may be tender with pressure. • Some plantar warts are depressed, resembling numerous small pits.
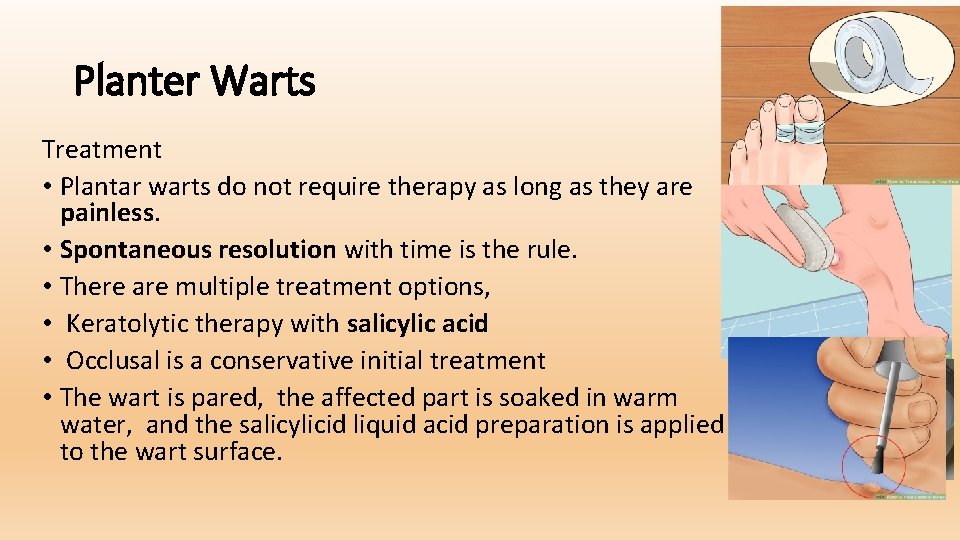
Planter Warts Treatment • Plantar warts do not require therapy as long as they are painless. • Spontaneous resolution with time is the rule. • There are multiple treatment options, • Keratolytic therapy with salicylic acid • Occlusal is a conservative initial treatment • The wart is pared, the affected part is soaked in warm water, and the salicylicid liquid acid preparation is applied to the wart surface.
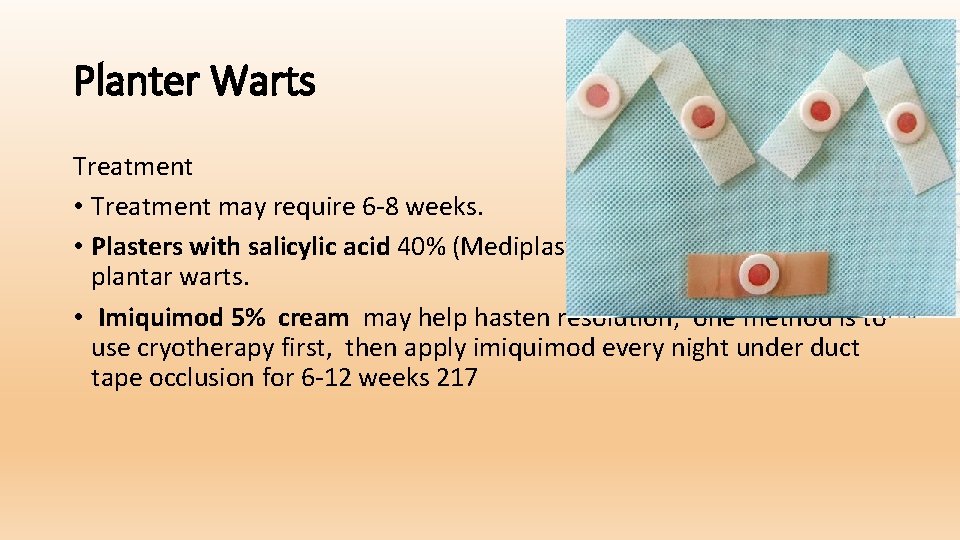
Planter Warts Treatment • Treatment may require 6 -8 weeks. • Plasters with salicylic acid 40% (Mediplast) are useful in treating plantar warts. • Imiquimod 5% cream may help hasten resolution; one method is to use cryotherapy first, then apply imiquimod every night under duct tape occlusion for 6 -12 weeks 217
Planter Warts • cryosurgery with liquid nitrogen, • Vinegar soak a piece • Carbon. • Electrodesiccation/curettage is sometimes used,
Molluscum Contagiosum • Description • Molluscum contagiosum is a localized, limited viral infection of the skin, • it is spread on the skin by autoinoculation and is transmitted to others by skin to skin contact • The cause of infection is a DNA virus of the pox virus family.

Molluscum Contagiosum • History • Molluscum contagiosum may occur at any age, • Numerous lesions and case of spread are notable in atopic patients • Most lesions are asymptomatic, although tenderness and itching can occur and are usually associated with mild local inflammation • lesions are transmitted by close contact.
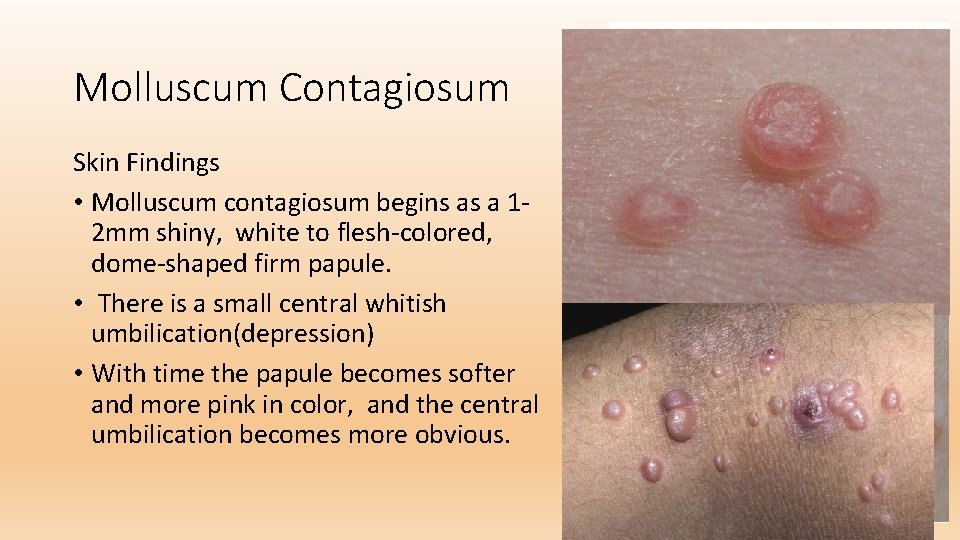
Molluscum Contagiosum Skin Findings • Molluscum contagiosum begins as a 12 mm shiny, white to flesh-colored, dome-shaped firm papule. • There is a small central whitish umbilication(depression) • With time the papule becomes softer and more pink in color, and the central umbilication becomes more obvious.
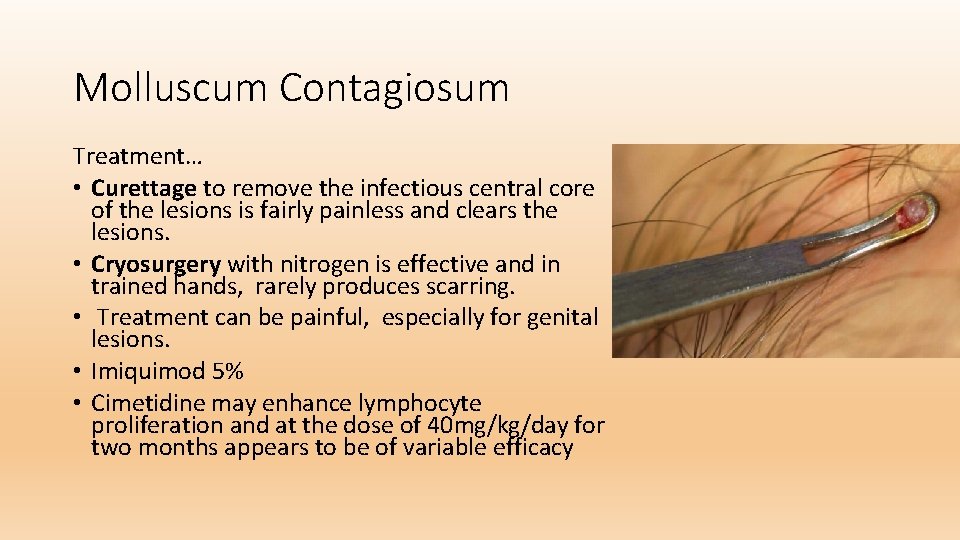
Molluscum Contagiosum Treatment… • Curettage to remove the infectious central core of the lesions is fairly painless and clears the lesions. • Cryosurgery with nitrogen is effective and in trained hands, rarely produces scarring. • Treatment can be painful, especially for genital lesions. • Imiquimod 5% • Cimetidine may enhance lymphocyte proliferation and at the dose of 40 mg/kg/day for two months appears to be of variable efficacy
Herpes Simplex(Cold Sores, Fever Blisters) Description • Herpes simplex virus is a double stranded DNA virus with two different virus types(types 1 and 2) • Can be distinguished in the laboratory • Type 1 is generally associated with vesicular ulcerative oral infections • Type 2 with genital infections. • Type 1 genital infections and type 2 oral infections are becoming more common, possibly as a result of increased incidence of oral-genital sexual contact
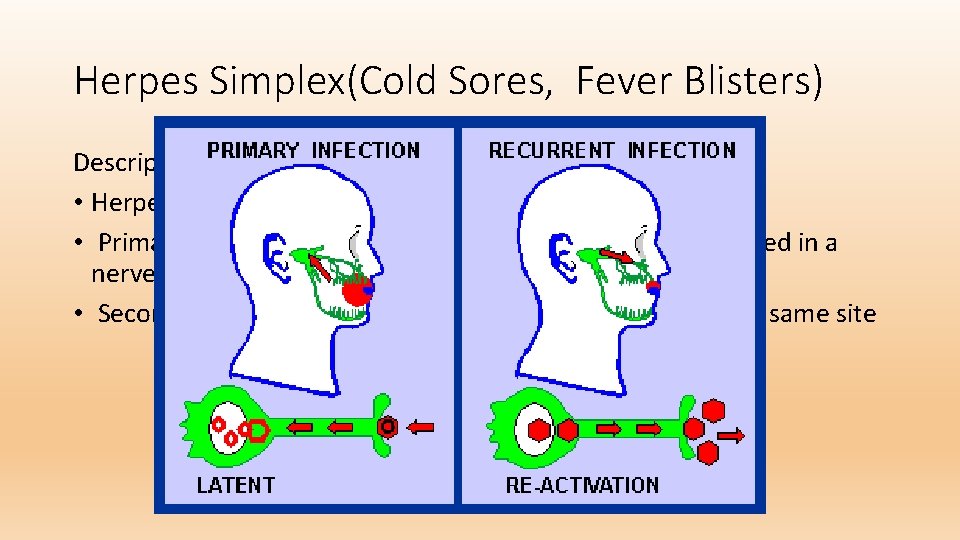
Herpes Simplex(Cold Sores, Fever Blisters) Description • Herpes simplex virus infections have two phases: • Primary infection, after which the virus becomes established in a nerve ganglion • Secondary phase, characterized by recurrent disease at the same site
Herpes Simplex(Cold Sores, Fever Blisters) Primary Infection • The majority of primary infections are asymptomatic and can be detected only by an elevated immunoglobulin G antibody titer
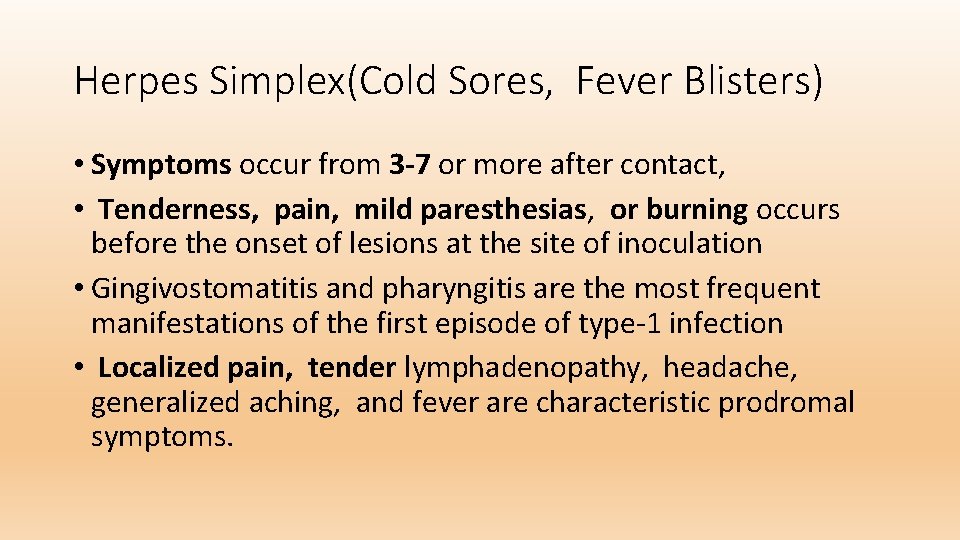
Herpes Simplex(Cold Sores, Fever Blisters) • Symptoms occur from 3 -7 or more after contact, • Tenderness, pain, mild paresthesias, or burning occurs before the onset of lesions at the site of inoculation • Gingivostomatitis and pharyngitis are the most frequent manifestations of the first episode of type-1 infection • Localized pain, tender lymphadenopathy, headache, generalized aching, and fever are characteristic prodromal symptoms.
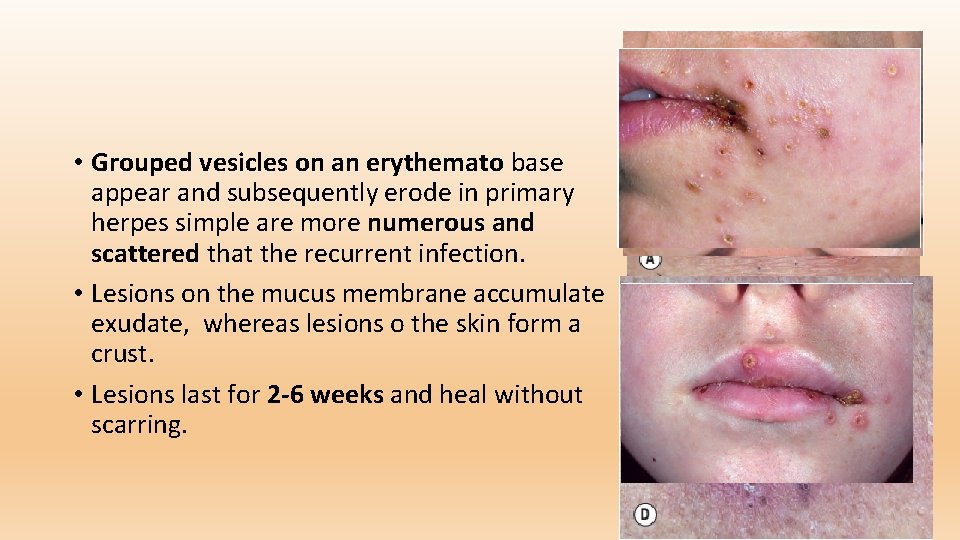
• Grouped vesicles on an erythemato base appear and subsequently erode in primary herpes simple are more numerous and scattered that the recurrent infection. • Lesions on the mucus membrane accumulate exudate, whereas lesions o the skin form a crust. • Lesions last for 2 -6 weeks and heal without scarring.
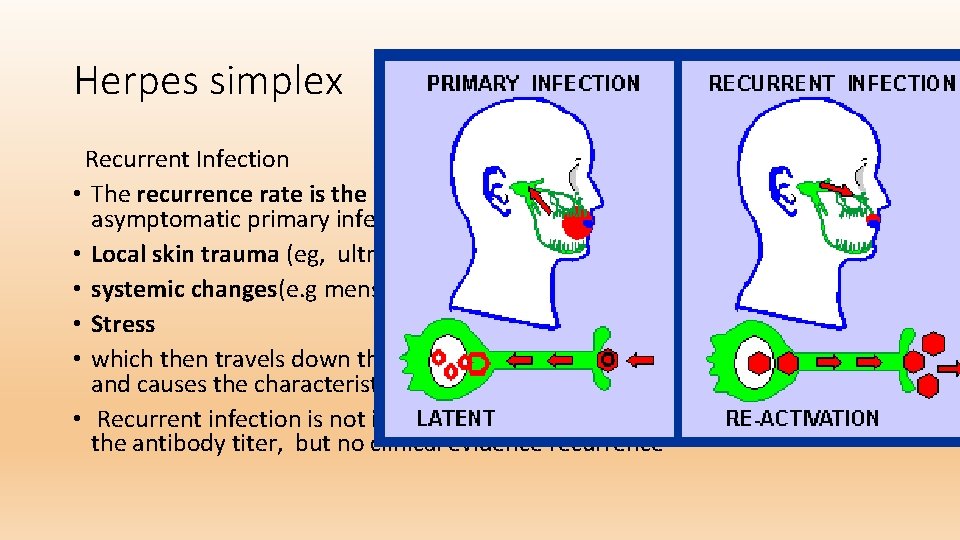
Herpes simplex Recurrent Infection • The recurrence rate is the same as for patients who had a symptomatic or asymptomatic primary infection. • Local skin trauma (eg, ultraviolet light exposure, chapping, abrasion) • systemic changes(e. g menses, fatigue, fever) reactivate the virus, ) • Stress • which then travels down the peripheral nerves to the site of initial infection and causes the characteristic focal, recurrent infection • Recurrent infection is not inevitable In many individuals, there is a rise in the antibody titer, but no clinical evidence recurrence
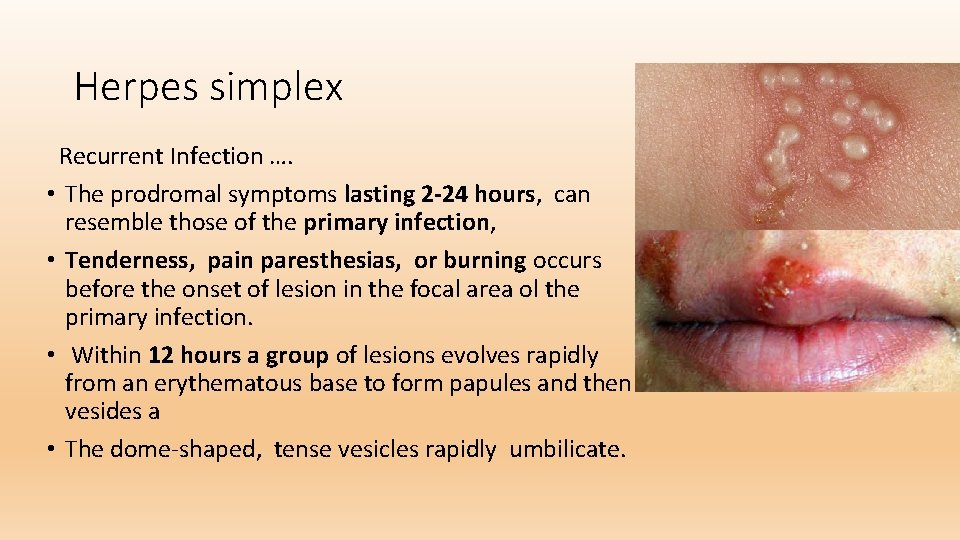
Herpes simplex Recurrent Infection …. • The prodromal symptoms lasting 2 -24 hours, can resemble those of the primary infection, • Tenderness, pain paresthesias, or burning occurs before the onset of lesion in the focal area ol the primary infection. • Within 12 hours a group of lesions evolves rapidly from an erythematous base to form papules and then vesides a • The dome-shaped, tense vesicles rapidly umbilicate.
Herpes simplex. . Treatment • Topical Agents • These can be used for relief of pain When applied frequently tetracaine cream 1. 8% reduces the healing time of recurrent herpes labialis lesions by about 2 days • Penciclovir cream reduces a duration of herpes labialis by about half day.
Herpes simplex. . Treatment Oral Antiviral Agents • Therapy is initiated at the first sign or symptom. • Therapy is most effective when administered within 48 hours of the onset of signs and symptoms. • Valacyclovir For initial episodes, 1 g is given twice a day for 7 -10 days. • Famciclovir For initial episode: 250 mg three times a day for 7 -10 days. • Acyclovir For initial episodes, 400 mg three times a day for 7 -10 days • Suppressive therapy indicate for more than 6 episodes/ year
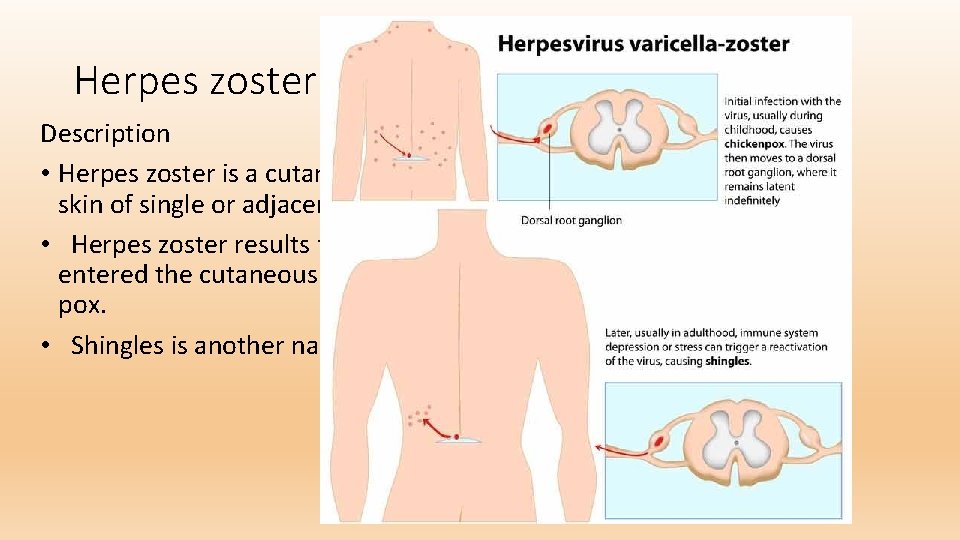
Herpes zoster(Shingles) Description • Herpes zoster is a cutaneous viral infection generally involving the skin of single or adjacent dermatomes. • Herpes zoster results from the reactivation of varicella virus that entered the cutaneous nerves during an earlier episode of chicken pox. • Shingles is another name for herpes zoster.
Herpes zoster(Shingles) History • This condition occurs during the lifetime of 10 -20% of all people. • People of all ages may be afflicted; the incidence increases with age. • Patients with zoster are not more likely to have an unknown underlying malignancy. • Zoster may be the earliest clinical sign of the development of the acquired immunodeficiency syndrome in high-risk individuals.
Herpes zoster(Shingles) Skin Findings • Pre eruptive tenderness or hyperesthesia throughout the dermatome is a useful predictive sign. • Pain, itching, or burning, generally localized to the dermatome, may precede the eruption by 4 or 5 days. • Although generally limited to the skin of a single dermatome, the eruption may involve one or two adjacent dermatomes.
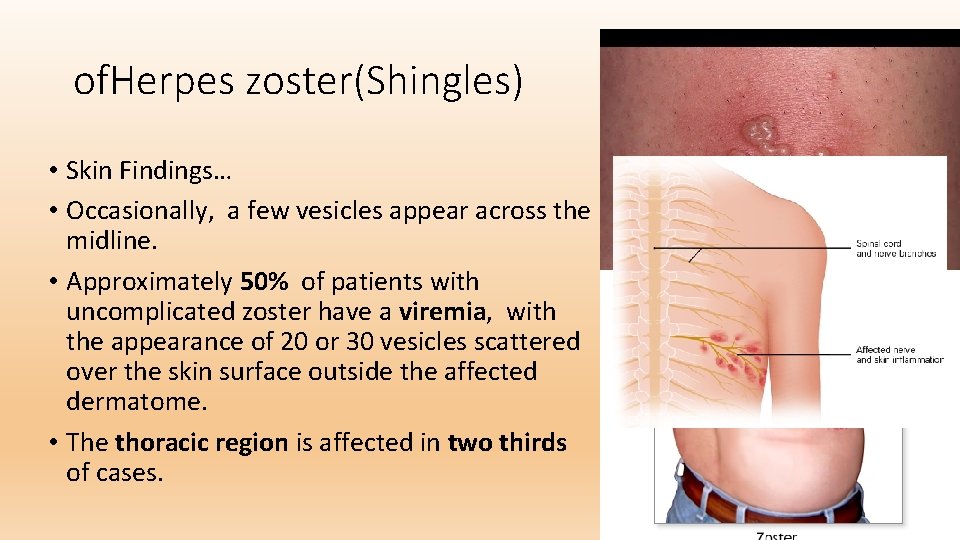
of. Herpes zoster(Shingles) • Skin Findings… • Occasionally, a few vesicles appear across the midline. • Approximately 50% of patients with uncomplicated zoster have a viremia, with the appearance of 20 or 30 vesicles scattered over the skin surface outside the affected dermatome. • The thoracic region is affected in two thirds of cases.
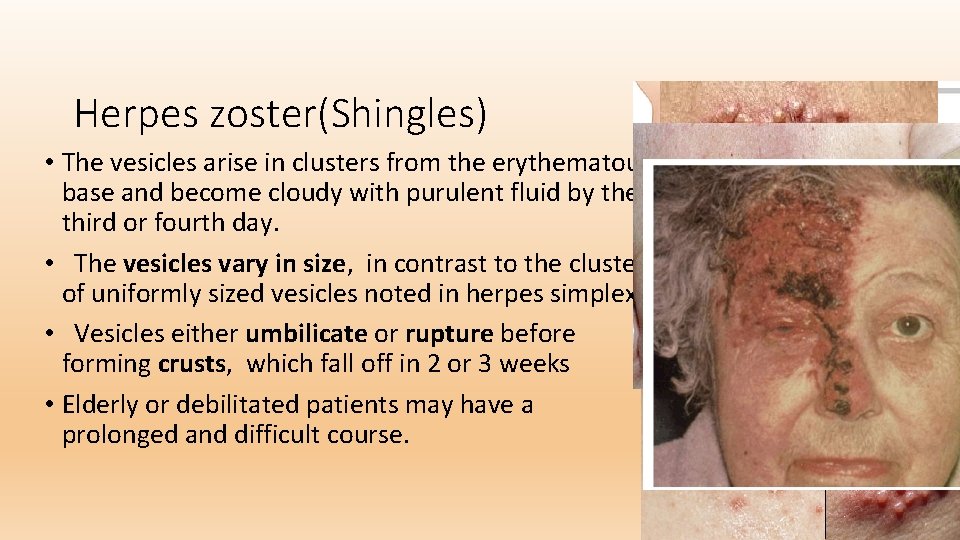
Herpes zoster(Shingles) • The vesicles arise in clusters from the erythematous base and become cloudy with purulent fluid by the third or fourth day. • The vesicles vary in size, in contrast to the cluster of uniformly sized vesicles noted in herpes simplex. • Vesicles either umbilicate or rupture before forming crusts, which fall off in 2 or 3 weeks • Elderly or debilitated patients may have a prolonged and difficult course.
Herpes zoster(Shingles) Post-Herpetic Neuralgia • Post-herpetic neuralgia is pain that persists more than 30 days after the rash. • The incidence and duration of pain increase with age. • Pain can persist in a dermatome for months or years after lesions have disappeared • The pain is often severe, intractable, and exhausting. • The majority of patients under 30 years age experience no pain. • By age 40 risk of prolonged pain lasting longer than 1 month increases to 33%. • By age 70, the risk increases to 74%.

Herpes zoster(Shingles) • Treatment • Suppression of Inflammation, Pain, and Infection • Topical therapy is tried. • Cool tap water can be used in a wet dressing With oral steroids, there is a decrease of acute pain and a quicker rash resolution but no effect on post-herpetic neuralgia,
Herpes zoster(Shingles) • Treatment is most effective when started within the first 48 hours of infection. • It is reasonable to use antiviral therapy in the patient seeking medical treatment more than 48 hours after the vesicles appear if the lesions are not completely crusted. • The recommended oral dosage for adults is a 7 -10 -day course of : • acyclovir 800 mg five times a day • valacyclovir Waltrex) 1000 mg three times a day • famciclovir(Famvir) 500 mg three times a day.
Any question?

Thank you
- Slides: 39