Violence against Women Domestic Abuse and Sexual Violence
Violence against Women, Domestic Abuse and Sexual Violence (Wales) Act 2015 “Ask & Act” Group 2 training 1
Housekeeping • • Toilets Breaks Mobile phones Taking care of yourself and each other 2
Ground rules • Confidentiality • Do you need support? • Respect Any others? 3
Violence against Women, Domestic Abuse and Sexual Violence (Wales) Act 2015 What does the Act do? The Violence against Women, Domestic Abuse and Sexual Violence (Wales) Act 2015 centres on the PREVENTION of these issues, the PROTECTION of victims and SUPPORT for those affected by these issues. This is a unique and ground-breaking piece of legislation. 4
Objectives – What are these sessions about? 1. How to recognise the signs and symptoms of violence against women, domestic abuse and sexual violence; 2. Understand the purpose of and demonstrate an ability to undertake targeted enquiry; 3. Demonstrate knowledge around data protection and the duty of confidentiality; 4. Understand the purpose of risk identification in relation to some forms of violence against women, domestic abuse and sexual violence; 5. Be able to implement the targeted enquiry care pathway. 5
The language we are using: • • • Abuse; Domestic abuse; Gender-based Violence; Sexual Violence; Violence against women; Victim/survivor; Client/service user; Ask; Act. 6
Benefits of “Ask and Act” • Increased identification of those experiencing violence against women, domestic abuse and sexual violence by using targeted enquiry; • Increased referrals to specialist services for those identified; • An improved culture across the Welsh Public Service where identification of violence against Women, domestic abuse and sexual violence is an accepted area of business and where disclosure is supported, accepted and facilitated. Earlier identification ensures support services are available at the earliest opportunity, rather than just at the point of crisis! 7
Targeted enquiry – why? • • Victims want to be asked Early intervention can reduce impacts – including death Helps to reduce stigma and isolation Signals service as somewhere that help can be gained Child protection Good clinical practice Silence is not neutral 8
Group activity: • Get into groups to respond to two questions: • What might be some of the barriers for professionals to make a targeted enquiry about VAWDASV? • What might be some of the barriers for service users/clients/patients to make a disclosure about VAWDASV? 9
Survivors said they want… • • To be treated with dignity and respect; To be believed; To be given help to get themselves and their children safe; For professionals to know that abuse is universal; is more than physical assaults; is about power and control and affects the whole family and how hard it is to disclose. 10
How might you encourage disclosure? Think about… • • Indicators The environment/creating a supportive environment What the client may be feeling What barriers the worker may create 11
Build rapport • • Use the person’s name where possible Be polite and sympathetic Use active listening Agree with them to encourage talking Do not tell them what to do Let them know they are doing the right thing by telling you Let them know you are taking them seriously Do not act shocked or appear as if you do not believe them 12
Key indicators? • In your department/area of work what would you identify as the key indicators? 13
Key indicators (NICE, 2014) • • • Depression, anxiety, sleep disorders; Suicidal tendencies or self-harming; Alcohol or other substance misuse; Unexplained reproductive symptoms, including pelvic pain and sexual dysfunction; Adverse pregnancy outcomes, i. e. multiple unintended pregnancies or terminations, miscarriage, pre-term labour and stillbirth; Frequent bladder or kidney infections; Vaginal bleeding or sexually transmitted infections; Chronic pain (unexplained); Traumatic injury, particularly if repeated with vague or implausible explanations; 14
Key indicators (NICE, 2014) • Repeated health consultations with no clear diagnosis; • Appointments missed or frequently rescheduled; • Intrusive “other person” in consultations, this can be partner, parent, grandparent or an adult child (abuse of the older person); • Partner or other person’s behaviour: aggressive, overly dominant, doesn’t let their partner / family member speak for themselves. 15
Key indicators Social Services Depression, anxiety, sleep issues; Suicidal tendencies or self-harming; Alcohol or other substance misuse; Chronic pain (unexplained); Cancelled or frequently not attending appointments • Not wanting to meet at house • Not being able to meet anywhere public • • • Never allowed alone, partner or family member present • Reluctance to speak of personal matters • Always seeming afraid or nervous • Children known to Social Services • Traumatic injury, particularly if repeated with vague or implausible explanations • Physical injuries 16
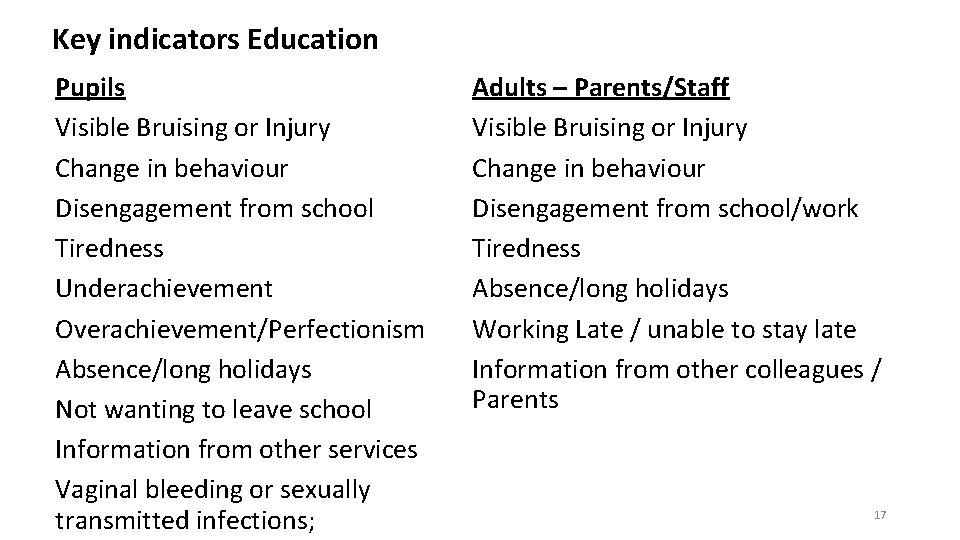
Key indicators Education Pupils Visible Bruising or Injury Change in behaviour Disengagement from school Tiredness Underachievement Overachievement/Perfectionism Absence/long holidays Not wanting to leave school Information from other services Vaginal bleeding or sexually transmitted infections; Adults – Parents/Staff Visible Bruising or Injury Change in behaviour Disengagement from school/work Tiredness Absence/long holidays Working Late / unable to stay late Information from other colleagues / Parents 17
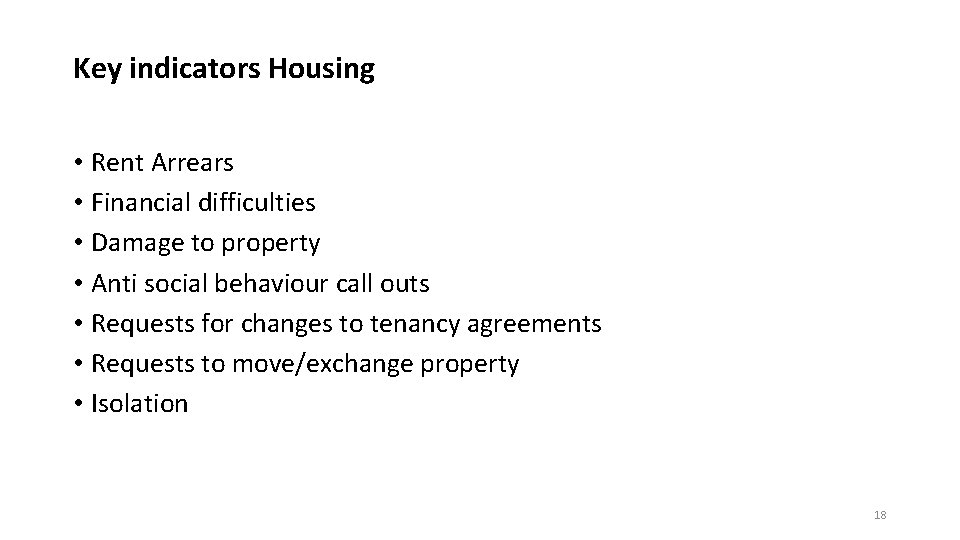
Key indicators Housing • Rent Arrears • Financial difficulties • Damage to property • Anti social behaviour call outs • Requests for changes to tenancy agreements • Requests to move/exchange property • Isolation 18
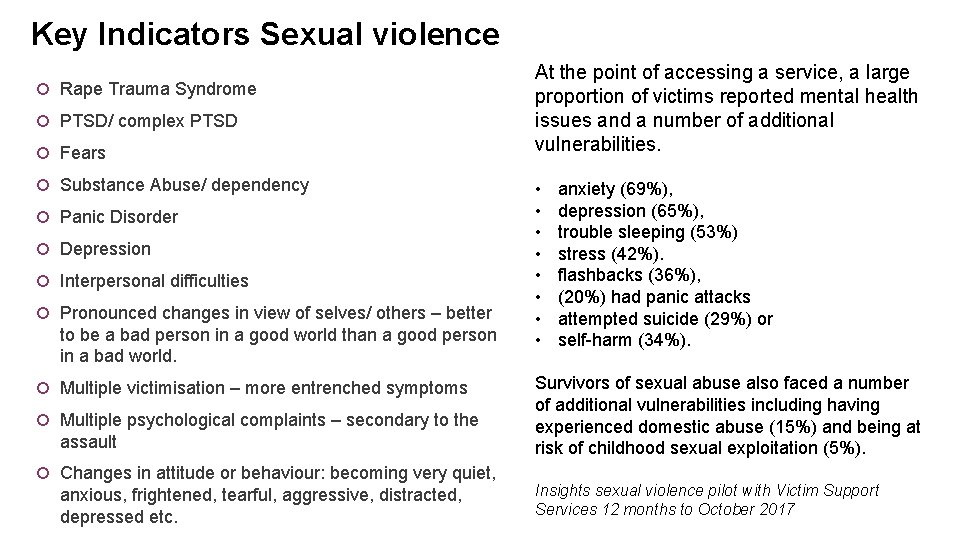
Key Indicators Sexual violence Rape Trauma Syndrome PTSD/ complex PTSD Fears Substance Abuse/ dependency Panic Disorder Depression Interpersonal difficulties Pronounced changes in view of selves/ others – better to be a bad person in a good world than a good person in a bad world. Multiple victimisation – more entrenched symptoms Multiple psychological complaints – secondary to the assault Changes in attitude or behaviour: becoming very quiet, anxious, frightened, tearful, aggressive, distracted, depressed etc. At the point of accessing a service, a large proportion of victims reported mental health issues and a number of additional vulnerabilities. • • anxiety (69%), depression (65%), trouble sleeping (53%) stress (42%). flashbacks (36%), (20%) had panic attacks attempted suicide (29%) or self-harm (34%). Survivors of sexual abuse also faced a number of additional vulnerabilities including having experienced domestic abuse (15%) and being at risk of childhood sexual exploitation (5%). Insights sexual violence pilot with Victim Support Services 12 months to October 2017
Video clip…. • How to ask and respond…. https: //www. youtube. com/watch? v=_u. Ew. Ng 0 p. FAI 20
Questions that work • • • How… Do you ever… Has anyone… Has your partner… I can see… We know that… In pairs – think about questions you might ask…. now think of a follow-up question. 21
Responding to disclosures • • • Thank you for telling me I believe you What you have described is not uncommon You are not to blame for the violence or abuse Your safety and wellbeing is my priority You have the right to be safe and get support You have the right to feel the way you do and to talk about it You are the expert on what you need There is help available For many survivors, just having someone listen to them, is all they need. 22
Do not behave like the abuser. • • This means do not: Judge Deny Blame Disbelieve Tell them what to do Act without client knowledge (and preferably, do not act without consent) 23
Identify risk: 1. 2. 3. 4. What do we mean by risk? Why is it important to identify risk? Based on the brief video clip – what are some important questions to ask? What are some of the most significant risk factors associated with cases of serious harm or death in relation to domestic abuse? 24
Additional resources available: YOU ARE NOT EXPECTED TO DO RISK ASSESSMENTS – ASK FOR SUPPORT AND ADVICE. • Refer to an IDVA (add local details) • Refer to Welsh Women’s Aid / local specialists (handout with local information) • Refer to Safeguarding Lead • Ensure they have the national helpline (give out cards/pamphlets) • Key issues for survivors + safety, housing, money & children – you might need to link into other agencies (refer to handout). Not expecting you to be experts…. group 3 25
Gathering & Sharing Information Legislation • Data Protection Act (2018) - Prevention and detection of a crime and/or the apprehension or prosecution of offenders & General Data Protection Regulation (GDPR) • Human Rights Act (1998) – e. g. Right to life, right to be free from torture or inhuman or degrading treatment – Articles 2 & 3 • Children’s Act (1989)- disclosure to CYPS or the Police for the exercise of functions under the Children Act – Schedules 2 & 3, DPA • Crime & Disorder Act (1998) – prevention and detection of crime • Common Law Duty to act.
National Helplines • Live Fear Free Helpline: 0808 8010 800 (professionals can also call the helpline for advice) • Survivors Trust • Men’s Advice Line: 0808 801 0327 • Broken Rainbow: 0300 999 5428 • Forced Marriage Unit Helpline: 020 7008 0151 • National NSPCC FGM Helpline: 0800 028 3550 • For abusers: Respect: 0808 802 4040 27
Local Referral Pathway (handout) 28
Key messages: • ASK consistently and ACT confidently; • Get as much information as you can about what services and support are available; • Seek help and support from colleagues, Safeguarding Leads, VAWDASV Leads, workplace champions, specialist sector – there is a lot of support; • Leaving is very dangerous so ensure expert advice is accessed. 29

Diolch yn fawr - Thank you 30
- Slides: 30