Viewing MACRA Through a Medicaid Lens R Shawn






- Slides: 28
Viewing MACRA Through a Medicaid Lens R. Shawn Martin Senior Vice President, Advocacy, Practice Advancement, and Policy American Academy of Family Physicians
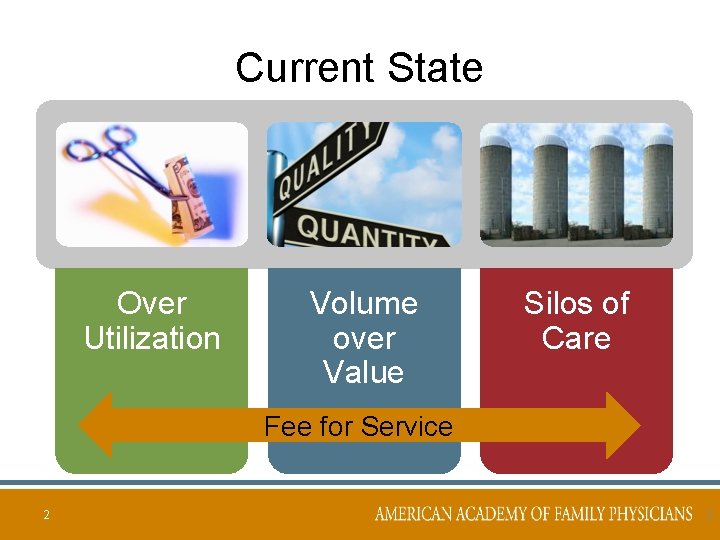
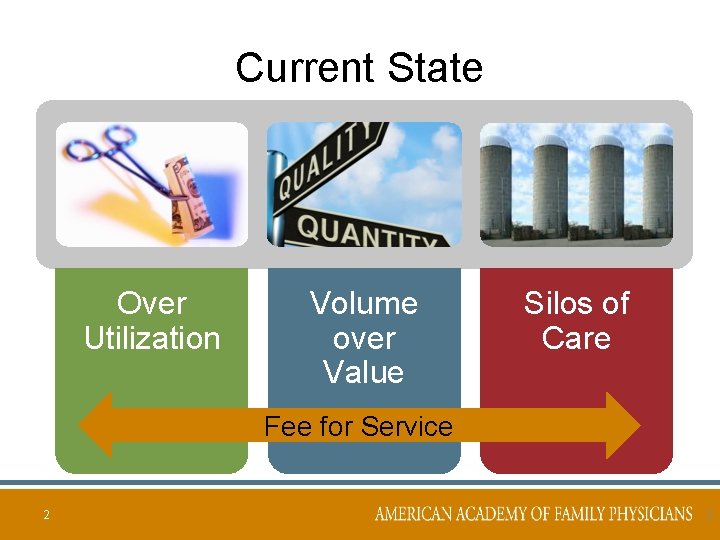
Current State Over Utilization Volume over Value Silos of Care Fee for Service 2 2
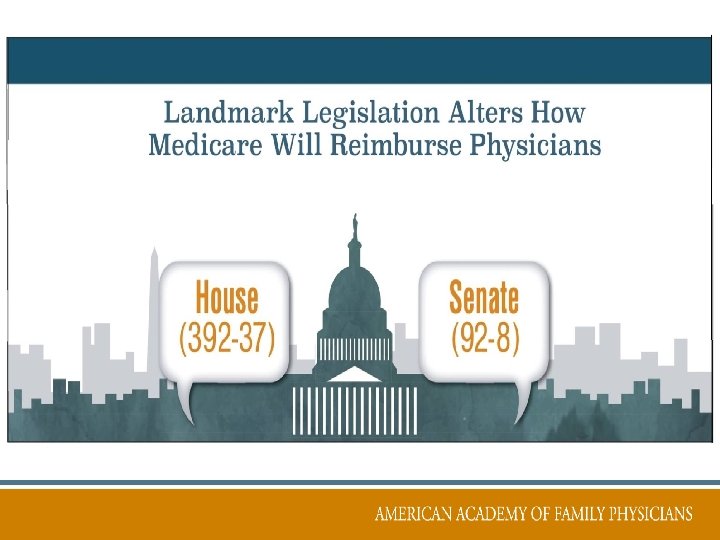

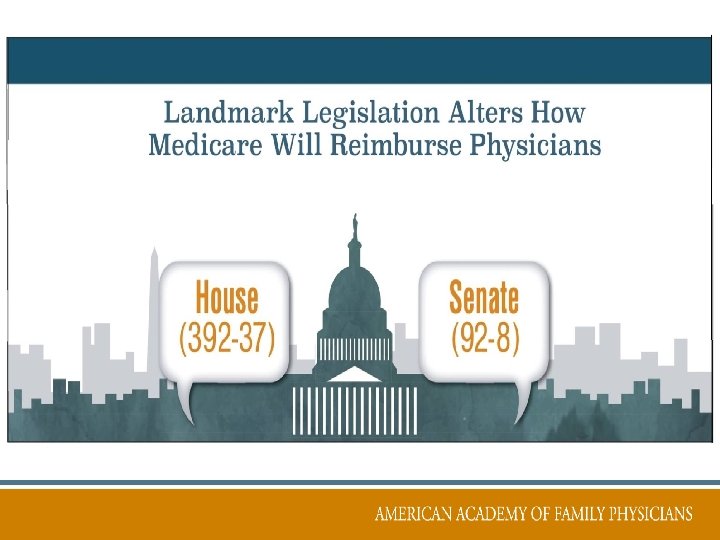
What Does MACRA Do? Merit-Based Incentive Payment System (MIPS) • Consolidates quality programs Advanced Alternative Payment Models (AAPM) • Potential for bonus payment for participation

Merit-Based Incentive Payment System (MIPS)

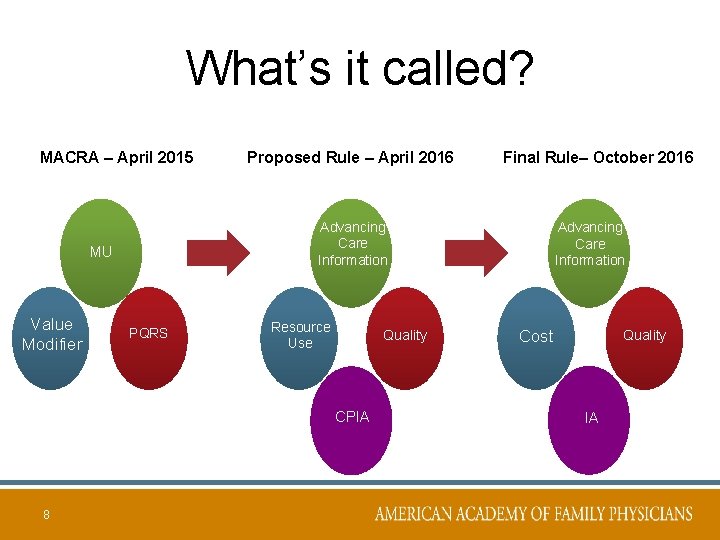
“Consolidates” PQRS VBPM Old Meaningful Use = Value-Based = Payment Modifier PQRS = New Advancing Care Information (ACI) MU Advancing Care Information Cost Quality Cost 7 Qualit y
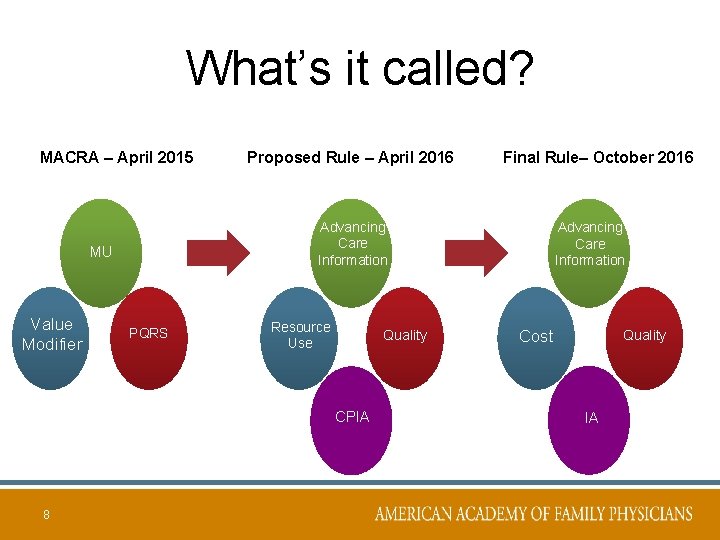
What’s it called? MACRA – April 2015 PQRS Resource Use Quality Advancing CPIA Care CPIA Information 8 Final Rule– October 2016 Advancing Care Information MU Value Modifier Proposed Rule – April 2016 Advancing Care Information Cost Quality IA
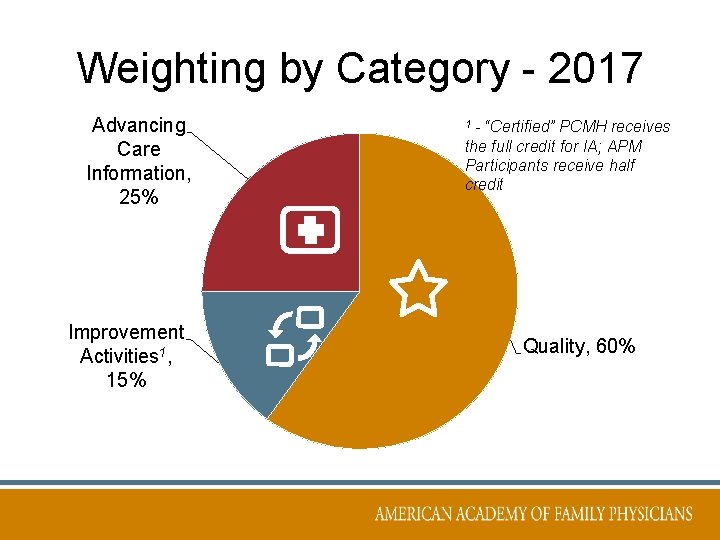
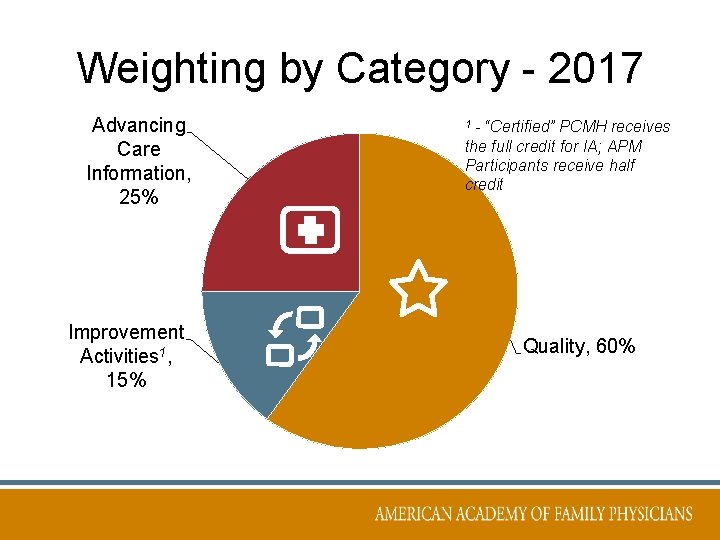
Weighting by Category - 2017 Advancing Care Information, 25% Improvement Activities 1, 15% - “Certified” PCMH receives the full credit for IA; APM Participants receive half credit 1 Quality, 60%
Advanced Alternative Payment Models (AAPMs)
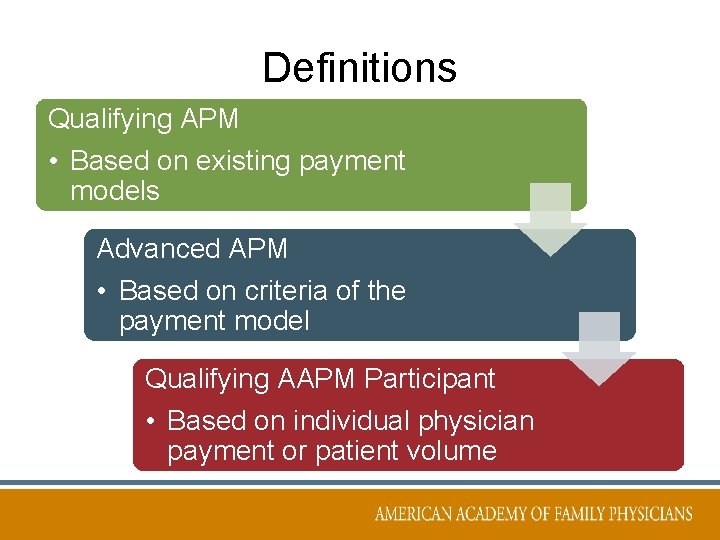
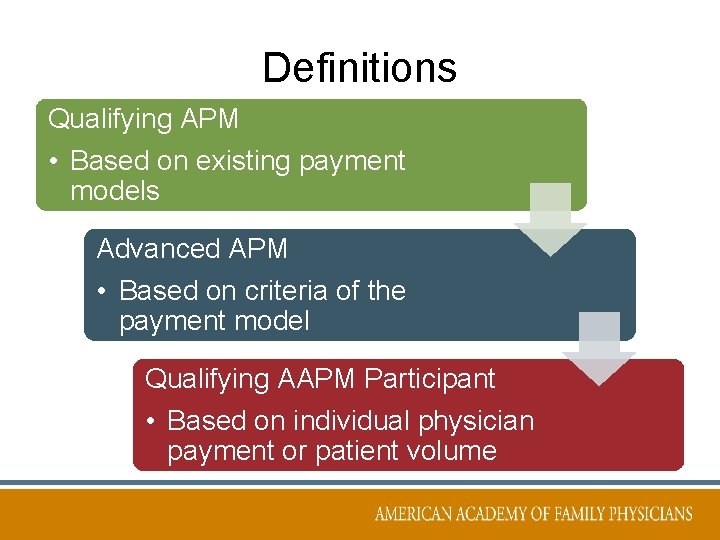
Definitions Qualifying APM • Based on existing payment models Advanced APM • Based on criteria of the payment model Qualifying AAPM Participant • Based on individual physician payment or patient volume
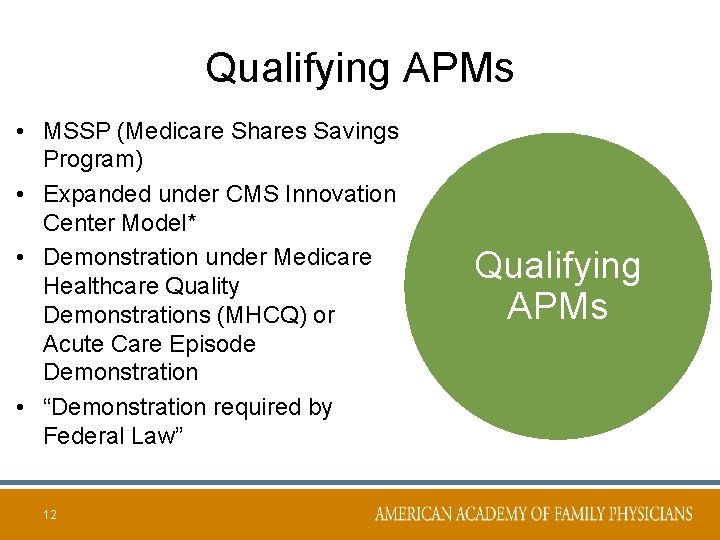
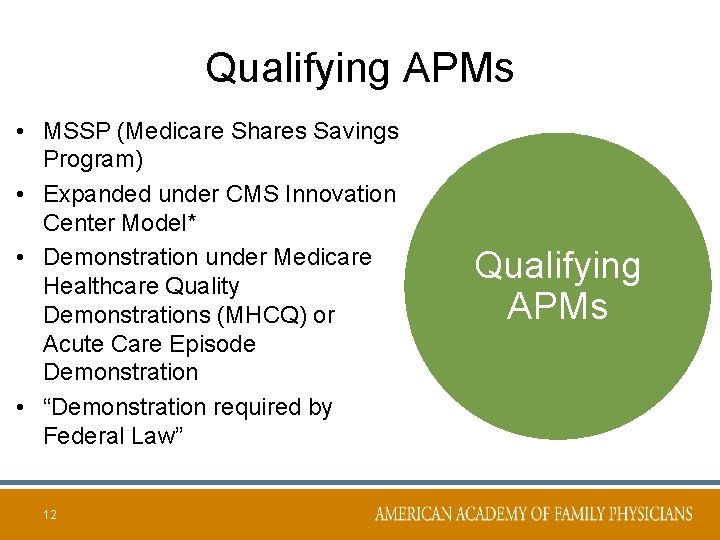
Qualifying APMs • MSSP (Medicare Shares Savings Program) • Expanded under CMS Innovation Center Model* • Demonstration under Medicare Healthcare Quality Demonstrations (MHCQ) or Acute Care Episode Demonstration • “Demonstration required by Federal Law” 12 Qualifying APMs
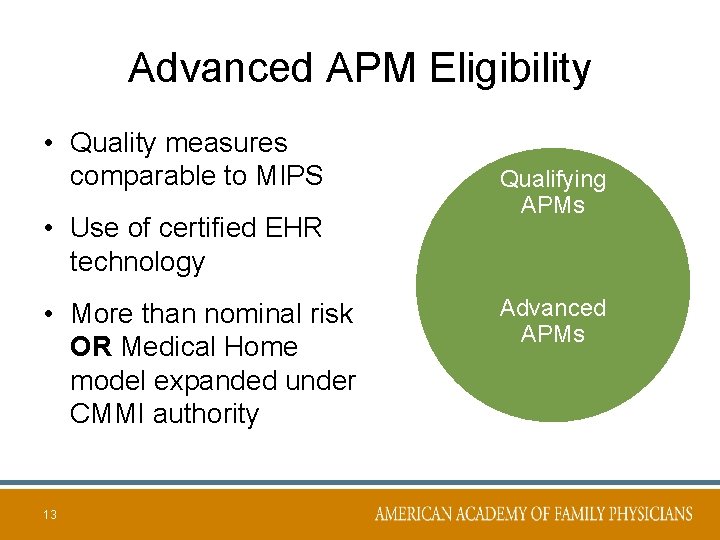
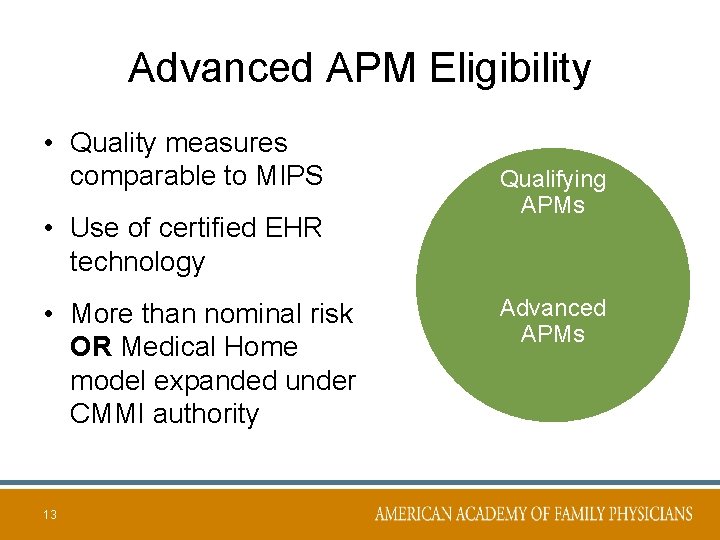
Advanced APM Eligibility • Quality measures comparable to MIPS • Use of certified EHR technology • More than nominal risk OR Medical Home model expanded under CMMI authority 13 Qualifying APMs Advanced APMs
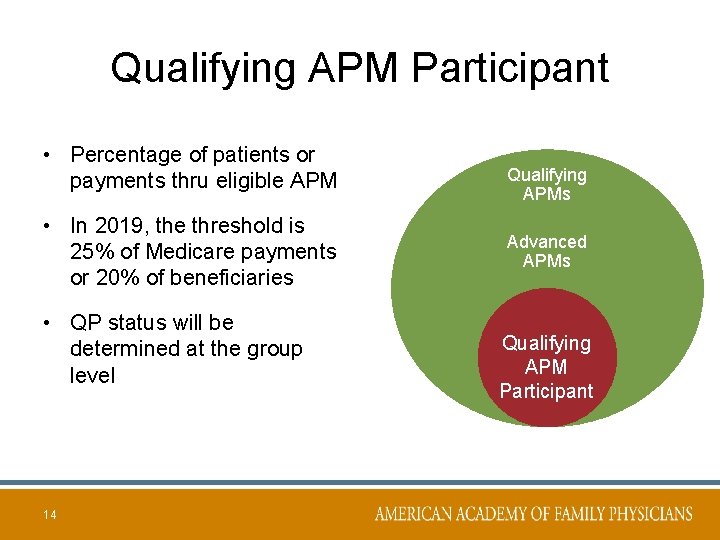
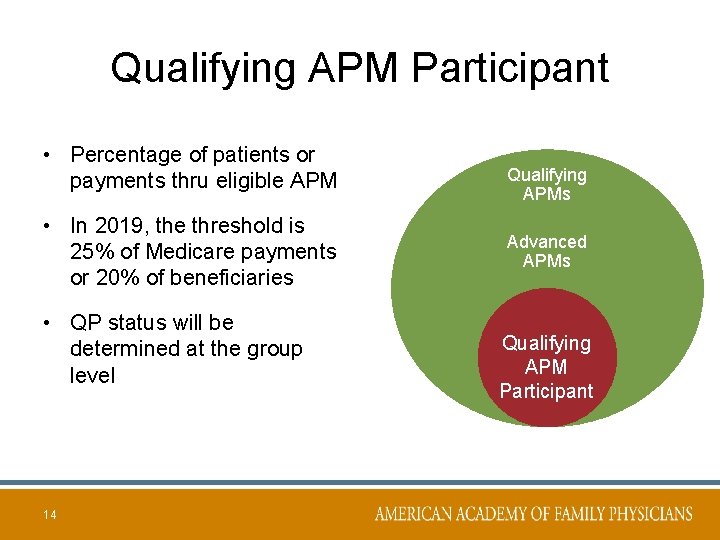
Qualifying APM Participant • Percentage of patients or payments thru eligible APM • In 2019, the threshold is 25% of Medicare payments or 20% of beneficiaries • QP status will be determined at the group level 14 Qualifying APMs Advanced APMs Qualifying APM Participant
Key Concerns • • Administrative complexity Lack of alignment Availability & affordability of staff Poor data or no data • And let us not forget – EMRs
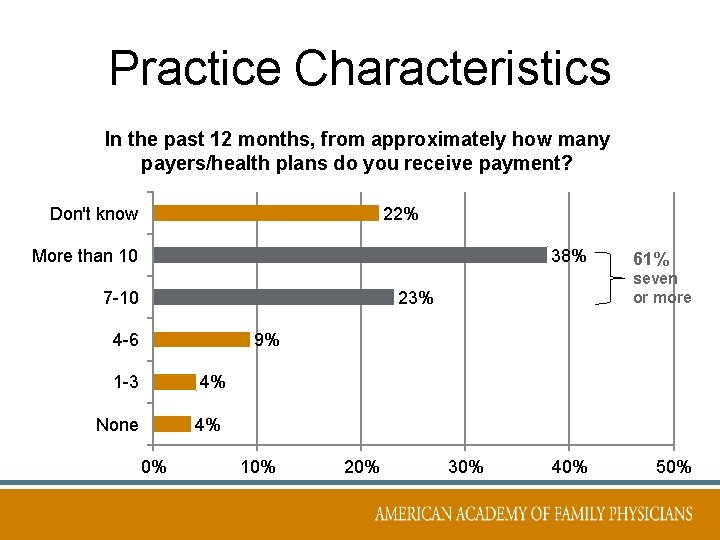
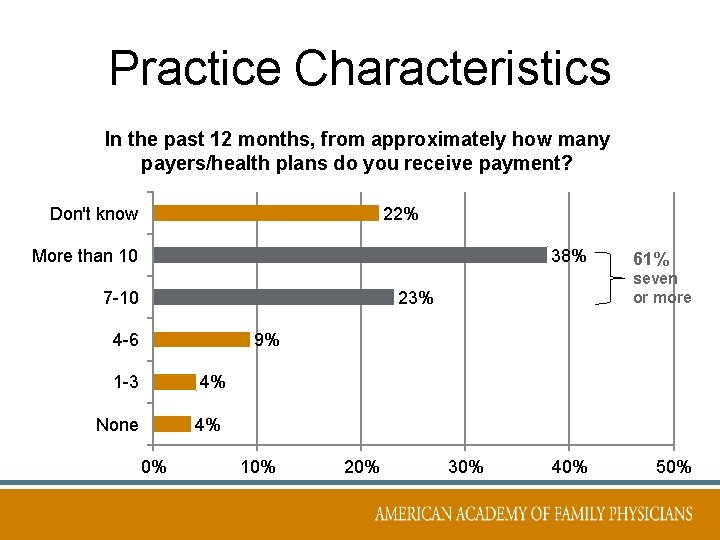
Practice Characteristics In the past 12 months, from approximately how many payers/health plans do you receive payment? Don't know 22% More than 10 38% 7 -10 seven or more 23% 4 -6 61% 9% 1 -3 4% None 4% 0% 10% 20% 30% 40% 50%
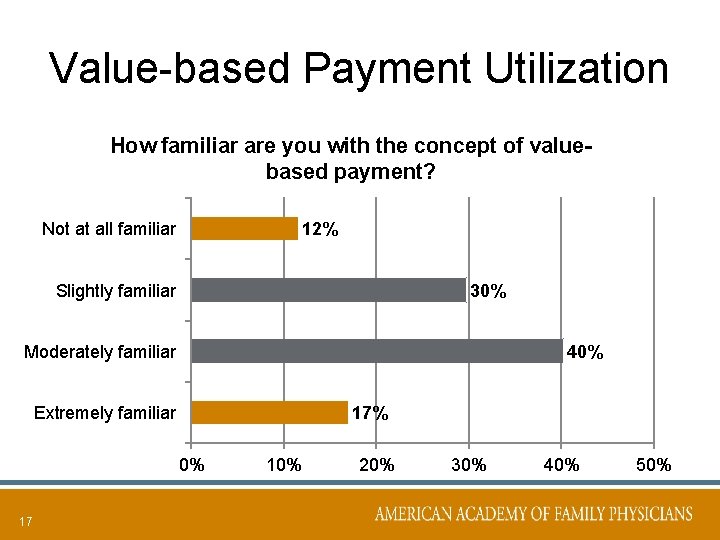
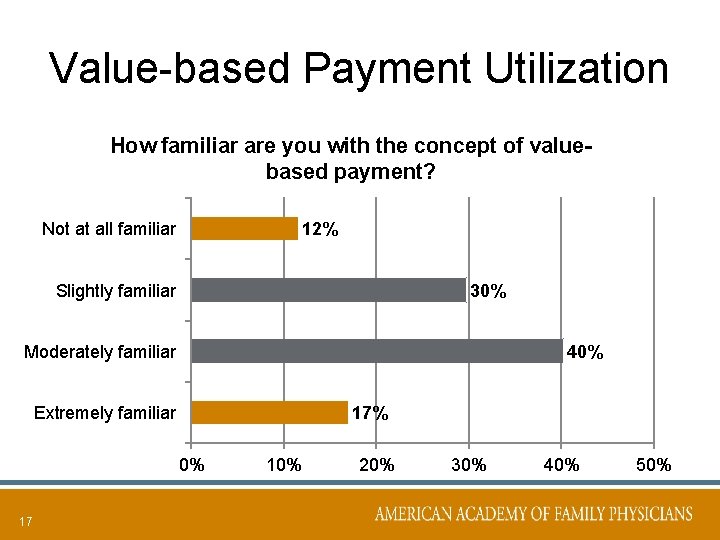
Value-based Payment Utilization How familiar are you with the concept of valuebased payment? Not at all familiar 12% Slightly familiar 30% Moderately familiar 40% Extremely familiar 17% 0% 17 10% 20% 30% 40% 50%
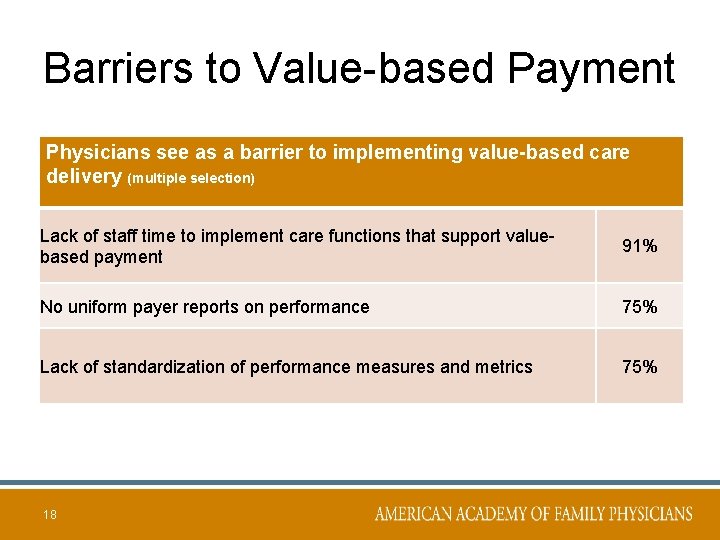
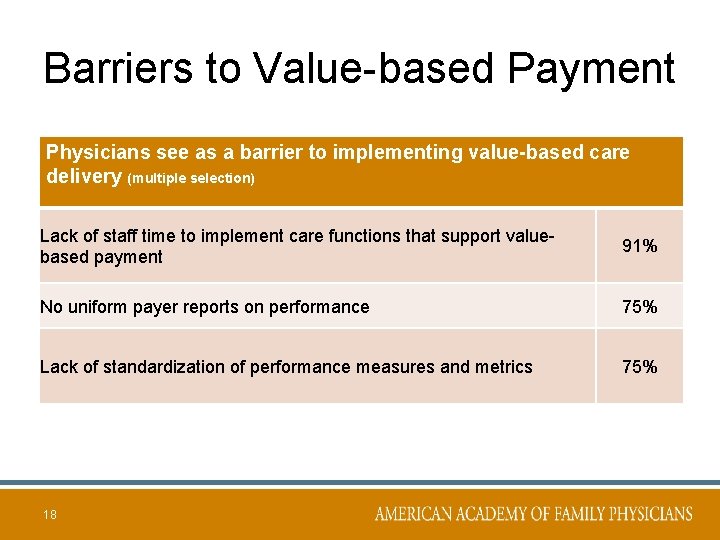
Barriers to Value-based Payment Physicians see as a barrier to implementing value-based care delivery (multiple selection) Lack of staff time to implement care functions that support valuebased payment 91% No uniform payer reports on performance 75% Lack of standardization of performance measures and metrics 75% 18

Barriers to Value-based Payment Physicians see as a barrier to accepting more financial risk value-based payment (multiple selection). Lack of resources to report, validate, and use data 81% Unpredictability of revenue stream 81% Administrative complexity and cost needed to understand financial risk 19 80%
EMR’s & IT Systems Must Work for & With Everyone
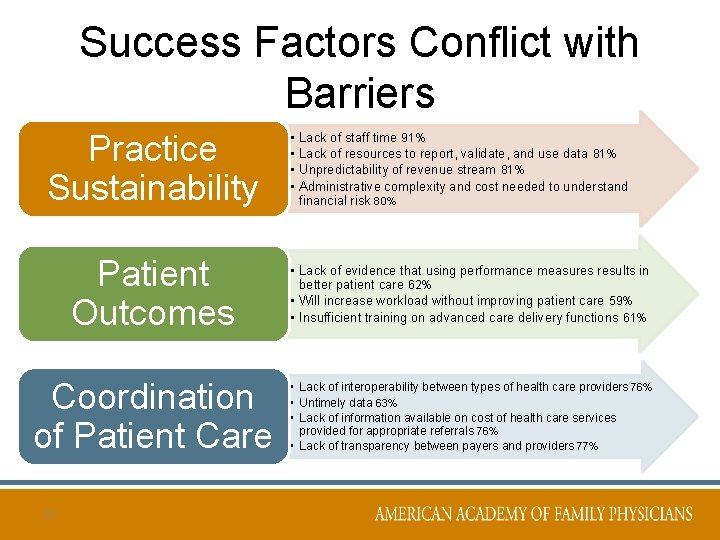
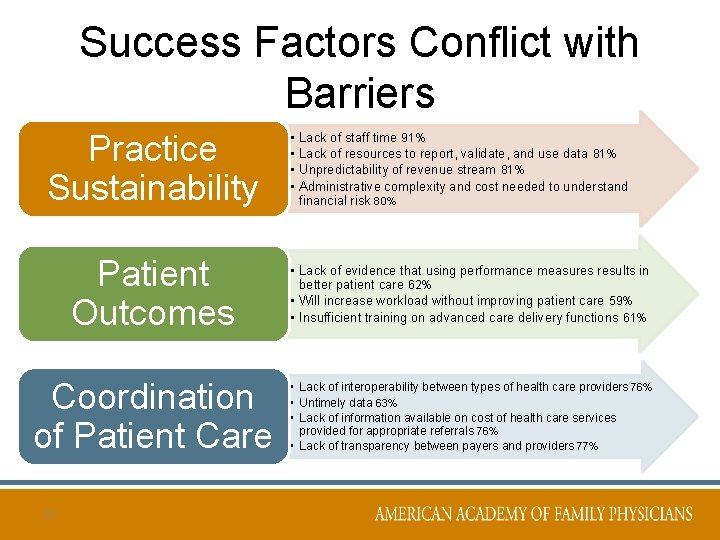
Success Factors Conflict with Barriers Practice Sustainability • • Lack of staff time 91% Lack of resources to report, validate, and use data 81% Unpredictability of revenue stream 81% Administrative complexity and cost needed to understand financial risk 80% Patient Outcomes • Lack of evidence that using performance measures results in better patient care 62% • Will increase workload without improving patient care 59% • Insufficient training on advanced care delivery functions 61% Coordination of Patient Care • Lack of interoperability between types of health care providers 76% • Untimely data 63% • Lack of information available on cost of health care services provided for appropriate referrals 76% • Lack of transparency between payers and providers 77% 21
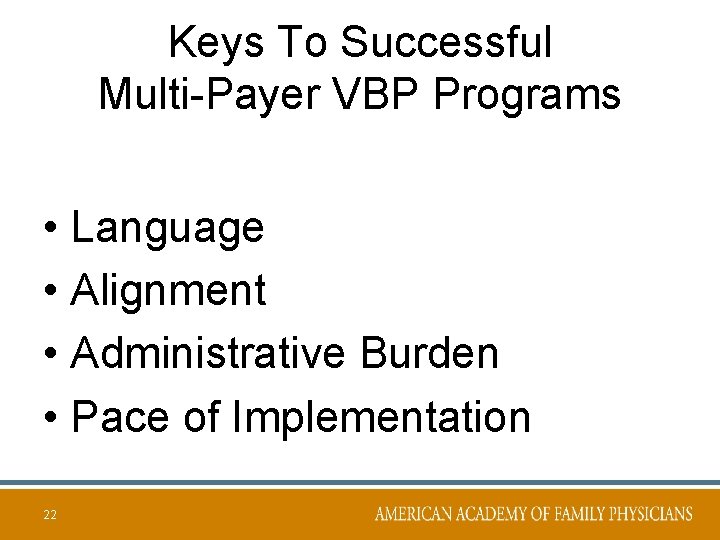
Keys To Successful Multi-Payer VBP Programs • Language • Alignment • Administrative Burden • Pace of Implementation 22
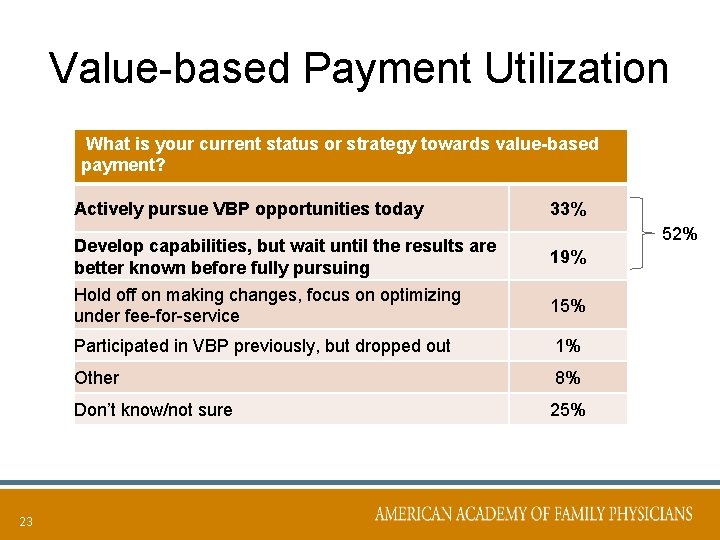
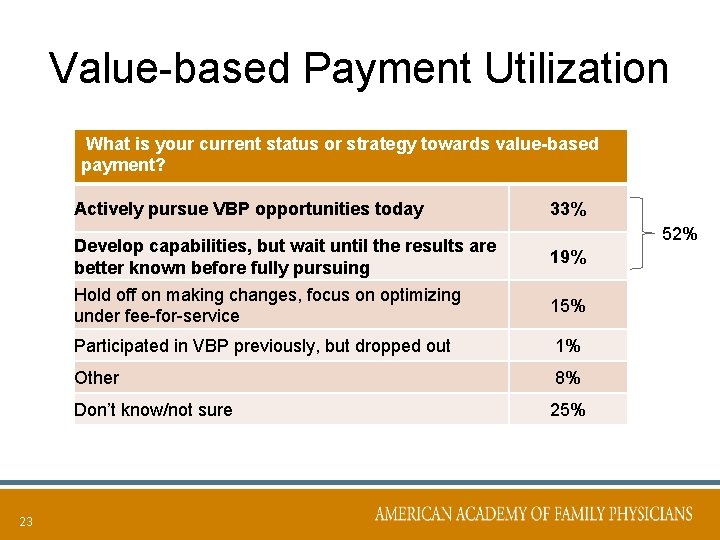
Value-based Payment Utilization What is your current status or strategy towards value-based payment? Actively pursue VBP opportunities today Develop capabilities, but wait until the results are better known before fully pursuing Hold off on making changes, focus on optimizing under fee-for-service 23 33% 52% 19% 15% Participated in VBP previously, but dropped out 1% Other 8% Don’t know/not sure 25%
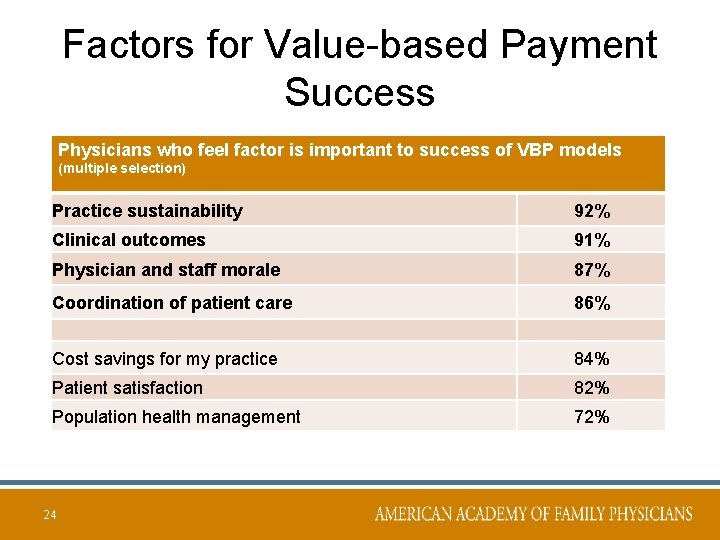
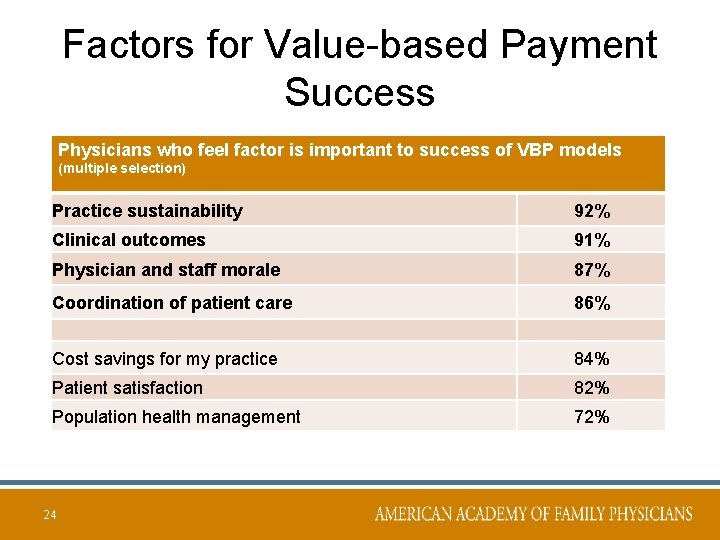
Factors for Value-based Payment Success Physicians who feel factor is important to success of VBP models (multiple selection) Practice sustainability 92% Clinical outcomes 91% Physician and staff morale 87% Coordination of patient care 86% Cost savings for my practice 84% Patient satisfaction 82% Population health management 72% 24

Partnering for Success Comprehensive Primary Care Initiative State Innovation Models Accountable Care Organizations Comprehensive Primary Care Plus Program Accountable Care Organizations Insurance Industry Transformation Projects 25
26
R. Shawn Martin Senior Vice President Advocacy, Practice Advancement, & Policy smartin@aafp. org @rshawnm

 Macra plastic surgeon
Macra plastic surgeon Macra proposed rule
Macra proposed rule Macra for dummies
Macra for dummies Converging lens is concave or convex
Converging lens is concave or convex Thin lens equation
Thin lens equation Nearsightedness
Nearsightedness Fresnel lens vs convex lens
Fresnel lens vs convex lens Thank you for viewing my presentation
Thank you for viewing my presentation Making quick glances to the roadway
Making quick glances to the roadway Bryanna and charles are in a dancing competition
Bryanna and charles are in a dancing competition Wide reading critical film viewing
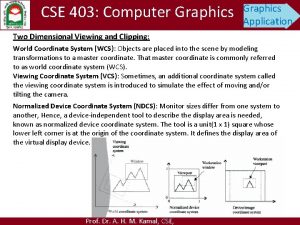
Wide reading critical film viewing What is window and viewport in computer graphics
What is window and viewport in computer graphics Steps in viewing
Steps in viewing Viewing angel
Viewing angel Viewing pipeline
Viewing pipeline Eccentric viewing techniques occupational therapy
Eccentric viewing techniques occupational therapy Exterior clipping
Exterior clipping Viewing pipeline in computer graphics
Viewing pipeline in computer graphics Contoh viewing 3d
Contoh viewing 3d Tyoes of claims
Tyoes of claims Define viewing in computer graphics
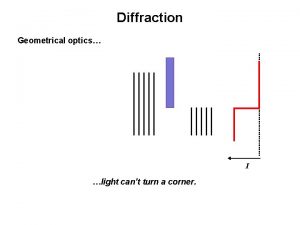
Define viewing in computer graphics Slit diffraction
Slit diffraction What process occurs
What process occurs Viewing coordinate sering juga disebut
Viewing coordinate sering juga disebut What is full section
What is full section Introduction to computer graphics - ppt
Introduction to computer graphics - ppt Shawn ralston
Shawn ralston Al shawn jeffery
Al shawn jeffery Shawn merdinger
Shawn merdinger