Viability assessment and its role in Revascularization Review
Viability assessment and its role in Revascularization Review of evidence Dr. Nithin P G Dr Nithin P G
Overview • Introduction • Viability assessment by various investigations • Comparisons • Clinical correlations • Benefits of viability assessment in clinical scenario • Conclusion Dr Nithin P G
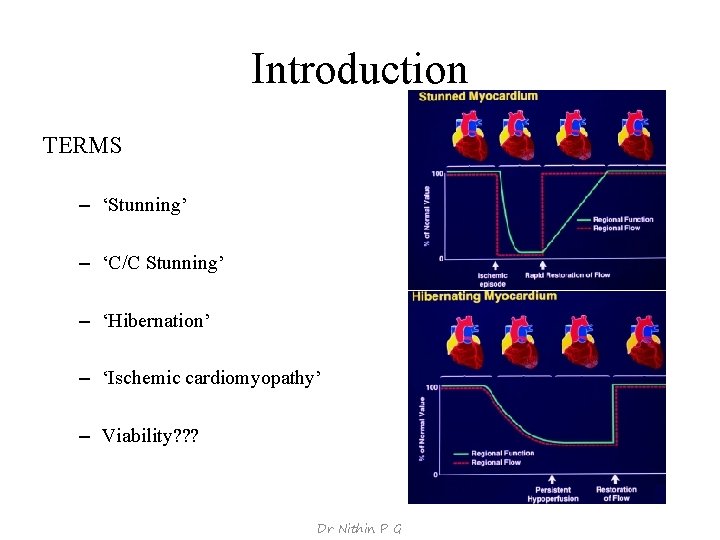
Introduction TERMS – ‘Stunning’ – ‘C/C Stunning’ – ‘Hibernation’ – ‘Ischemic cardiomyopathy’ – Viability? ? ? Dr Nithin P G
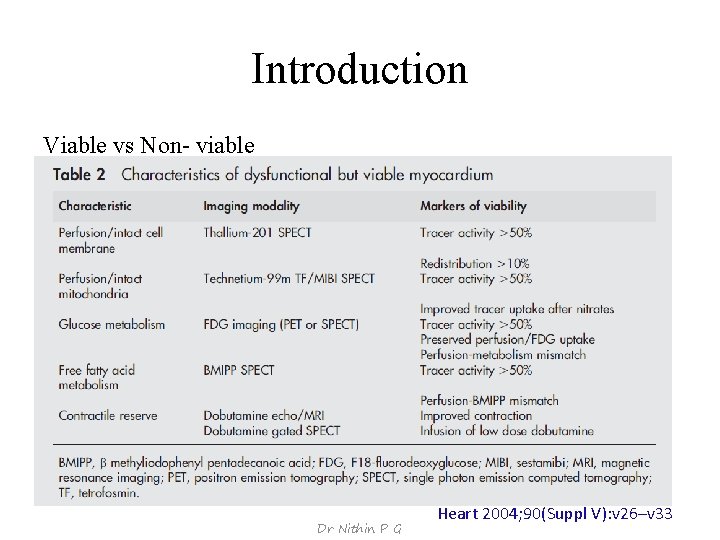
Introduction Viable vs Non- viable Dr Nithin P G Heart 2004; 90(Suppl V): v 26–v 33
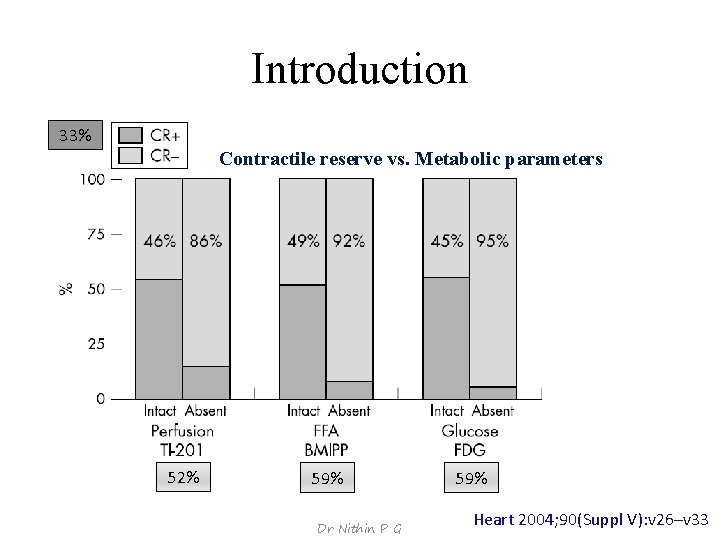
Introduction 33% Contractile reserve vs. Metabolic parameters 52% 59% Dr Nithin P G 59% Heart 2004; 90(Suppl V): v 26–v 33
![Introduction What to look for in viable tissues? [endpoints used in viability studies] – Introduction What to look for in viable tissues? [endpoints used in viability studies] –](http://slidetodoc.com/presentation_image_h2/74405f11233ae7d76a35d60dff7599c5/image-6.jpg)
Introduction What to look for in viable tissues? [endpoints used in viability studies] – Improvement in regional LV function (segments) – Improvement in global LV function (LVEF) – Improvement in symptoms (NYHA functional class) – Improvement in exercise capacity (metabolic equivalents) – Reverse LV remodeling (LV volumes) – Prevention of sudden death (ventricular arrhythmias) – Long-term prognosis (survival) Dr Nithin P G
![Introduction Pooled data-105 studies (n= 3, 003) [Nucl. Im. , DSE] 15, 045 dysfunctional Introduction Pooled data-105 studies (n= 3, 003) [Nucl. Im. , DSE] 15, 045 dysfunctional](http://slidetodoc.com/presentation_image_h2/74405f11233ae7d76a35d60dff7599c5/image-7.jpg)
Introduction Pooled data-105 studies (n= 3, 003) [Nucl. Im. , DSE] 15, 045 dysfunctional segments analyzed; 7, 941 (53%) – Segmental LV function showed improvement in function after revasc. [84% detected prior as viable] – LVEF Curr Probl Cardiol. 2001; 26: 142– 186 20%– 30% of LV viable to allow improvement in the LVEF Trials use criteria of >5% increase in EF J Nucl Med 2007; 48: 1135– 1146 – LV volumes ESV ≥ 140 m. L low improvement in LVEF post-revascularization [sens 68%; spec 65% to predict absence of global recovery] J Thorac Cardiovasc Surg 2004; 127: 385‐ 390 EDV 70% of patients with EDV 140 -180 ml & 35% with EDV>180 ml improved LVEF by 5% Eur Heart J 2000; 21: 125‐ 136 – Long-term prognosis (survival) Dr Nithin P G
Viability assessment by different investigations Dr Nithin P G
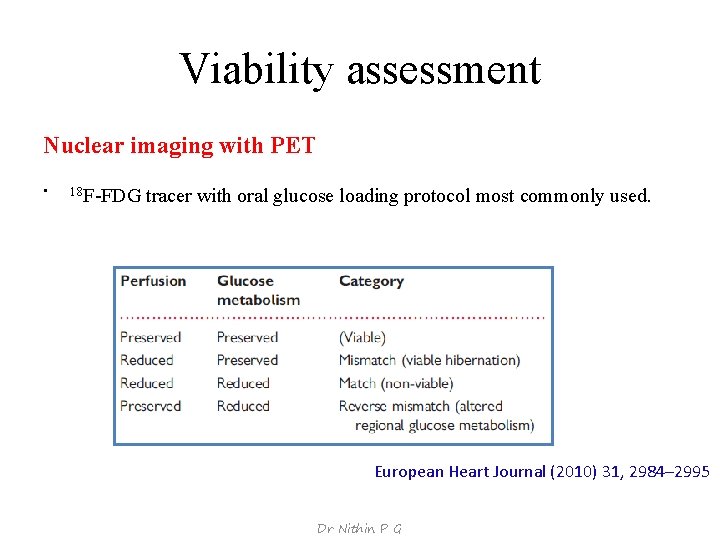
Viability assessment Nuclear imaging with PET • 18 F-FDG tracer with oral glucose loading protocol most commonly used. European Heart Journal (2010) 31, 2984– 2995 Dr Nithin P G
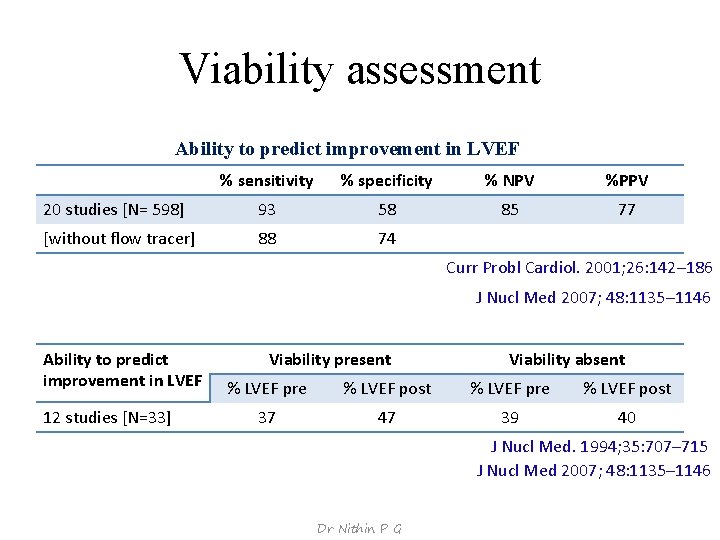
Viability assessment Ability to predict improvement in LVEF % sensitivity % specificity % NPV %PPV 20 studies [N= 598] 93 58 85 77 [without flow tracer] 88 74 Curr Probl Cardiol. 2001; 26: 142– 186 J Nucl Med 2007; 48: 1135– 1146 Ability to predict improvement in LVEF 12 studies [N=33] Viability present Viability absent % LVEF pre % LVEF post 37 47 39 40 J Nucl Med. 1994; 35: 707– 715 J Nucl Med 2007; 48: 1135– 1146 Dr Nithin P G
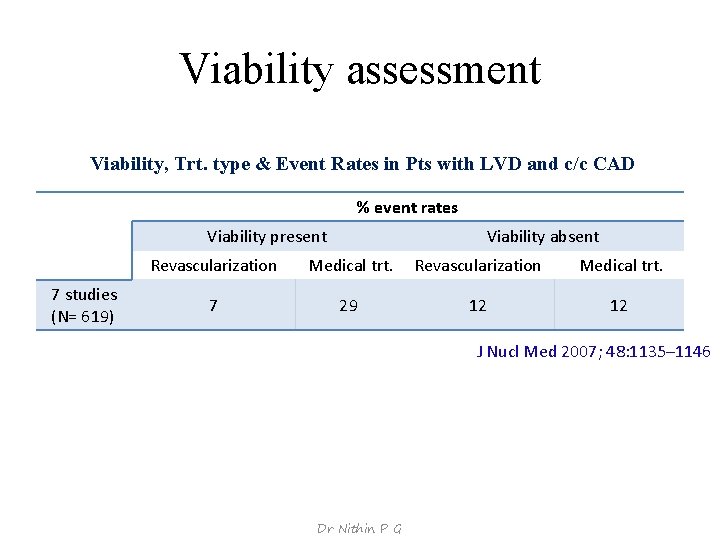
Viability assessment Viability, Trt. type & Event Rates in Pts with LVD and c/c CAD % event rates Viability present 7 studies (N= 619) Viability absent Revascularization Medical trt. 7 29 12 12 J Nucl Med 2007; 48: 1135– 1146 Dr Nithin P G

Viability assessment Nuclear imaging with SPECT • Tracers- 201 Tl-Chloride & 99 m. Tc-Labeled Agents [sestamibi] Viability assessment • Stress -Normal perfusion • Stress- defects with redistribution on delayed images • Delayed rest images or reinjection- fixed defect showing redistribution • Delayed rest images or reinjection- more than 50% tracer uptake Dr Nithin P G
![Viability assessment Ability to predict improvement in LVEF 201 Tl‐Chloride 33 trials[N=858] 99 m. Viability assessment Ability to predict improvement in LVEF 201 Tl‐Chloride 33 trials[N=858] 99 m.](http://slidetodoc.com/presentation_image_h2/74405f11233ae7d76a35d60dff7599c5/image-13.jpg)
Viability assessment Ability to predict improvement in LVEF 201 Tl‐Chloride 33 trials[N=858] 99 m. Tc‐Labeled Agents 20 trials[N=488] % sensitivity % specificity % NPV %PPV 87 55 81 64 81 66 77 71 Curr Probl Cardiol. 2001; 26: 142– 186 J Nucl Med 2007; 48: 1135– 1146 Ability to predict improvement in LVEF 201 Tl 5 trials [N=96] 99 m. Tc 4 trials [N=75] Viability present Viability absent % LVEF pre % LVEF post 30 38 29 31 47 53 Dr Nithin P G 40 39 J Nucl Med. 1994; 35: 707– 715 J Nucl Med 2007; 48: 1135– 1146
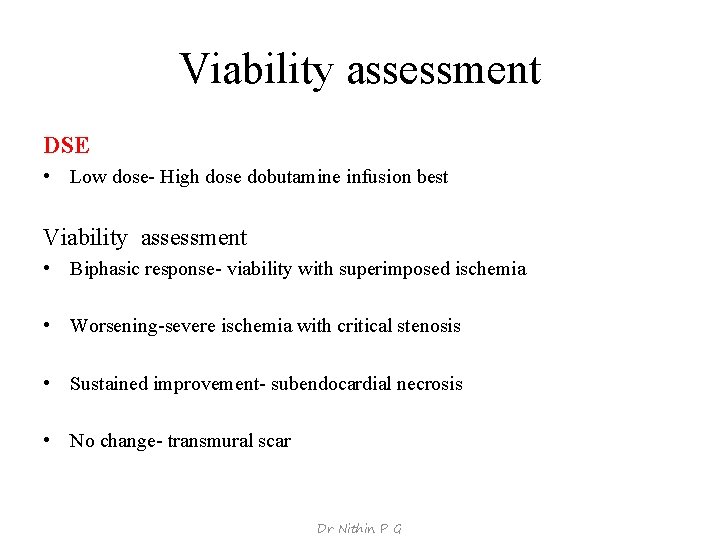
Viability assessment DSE • Low dose- High dose dobutamine infusion best Viability assessment • Biphasic response- viability with superimposed ischemia • Worsening-severe ischemia with critical stenosis • Sustained improvement- subendocardial necrosis • No change- transmural scar Dr Nithin P G
![Viability assessment Ability to predict improvement in LVEF 32 studies [N= 1090] % sensitivity Viability assessment Ability to predict improvement in LVEF 32 studies [N= 1090] % sensitivity](http://slidetodoc.com/presentation_image_h2/74405f11233ae7d76a35d60dff7599c5/image-15.jpg)
Viability assessment Ability to predict improvement in LVEF 32 studies [N= 1090] % sensitivity % specificity % NPV %PPV 81 80 85 77 Curr Probl Cardiol. 2001; 26: 142– 186 J Nucl Med 2007; 48: 1135– 1146 Ability to predict improvement in LVEF 8 studies [N=254] Viability present Viability absent % LVEF pre % LVEF post 35 43 35 36 J Nucl Med. 1994; 35: 707– 715 J Nucl Med 2007; 48: 1135– 1146 Dr Nithin P G
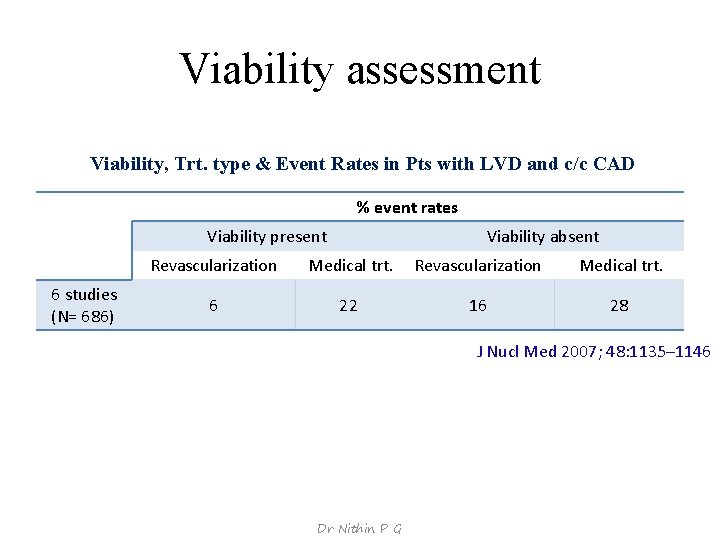
Viability assessment Viability, Trt. type & Event Rates in Pts with LVD and c/c CAD % event rates Viability present 6 studies (N= 686) Viability absent Revascularization Medical trt. 6 22 16 28 J Nucl Med 2007; 48: 1135– 1146 Dr Nithin P G
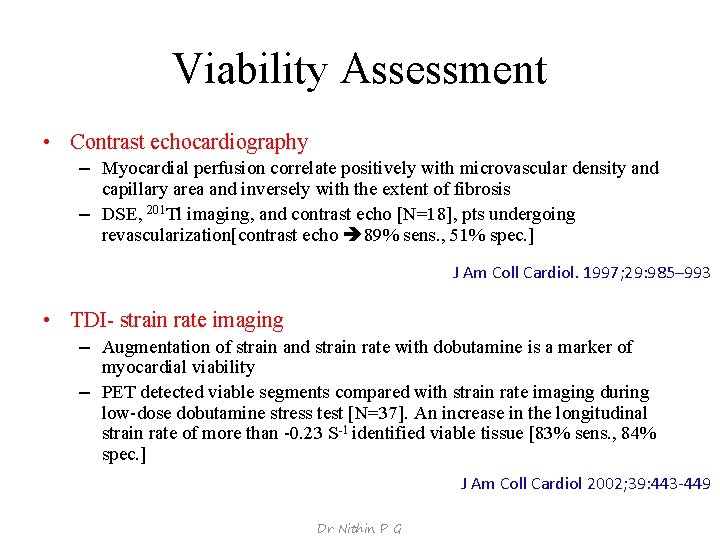
Viability Assessment • Contrast echocardiography – Myocardial perfusion correlate positively with microvascular density and capillary area and inversely with the extent of fibrosis – DSE, 201 Tl imaging, and contrast echo [N=18], pts undergoing revascularization[contrast echo 89% sens. , 51% spec. ] J Am Coll Cardiol. 1997; 29: 985– 993 • TDI- strain rate imaging – Augmentation of strain and strain rate with dobutamine is a marker of myocardial viability – PET detected viable segments compared with strain rate imaging during low-dose dobutamine stress test [N=37]. An increase in the longitudinal strain rate of more than -0. 23 S-1 identified viable tissue [83% sens. , 84% spec. ] J Am Coll Cardiol 2002; 39: 443‐ 449 Dr Nithin P G
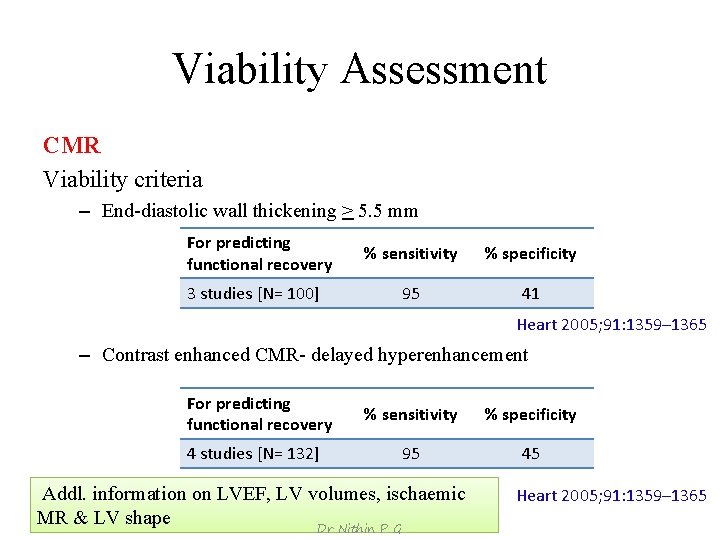
Viability Assessment CMR Viability criteria – End-diastolic wall thickening > 5. 5 mm For predicting functional recovery 3 studies [N= 100] % sensitivity % specificity 95 41 Heart 2005; 91: 1359– 1365 – Contrast enhanced CMR- delayed hyperenhancement For predicting functional recovery 4 studies [N= 132] % sensitivity % specificity 95 45 Addl. information on LVEF, LV volumes, ischaemic MR & LV shape Dr Nithin P G Heart 2005; 91: 1359– 1365
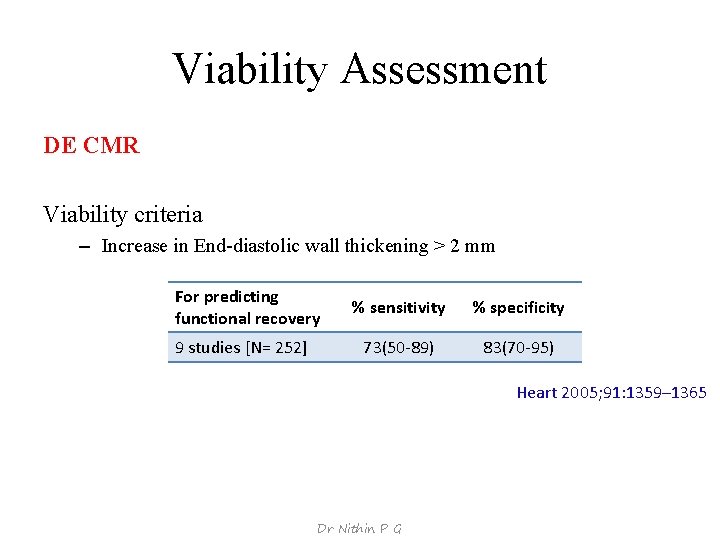
Viability Assessment DE CMR Viability criteria – Increase in End-diastolic wall thickening > 2 mm For predicting functional recovery 9 studies [N= 252] % sensitivity % specificity 73(50‐ 89) 83(70‐ 95) Heart 2005; 91: 1359– 1365 Dr Nithin P G
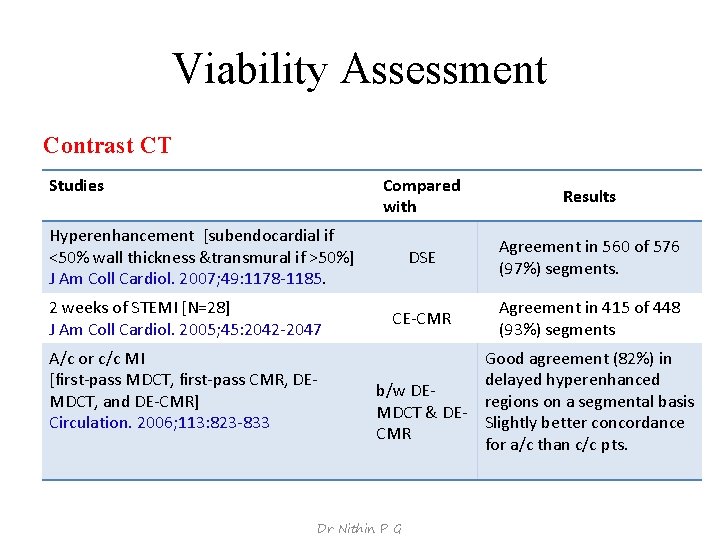
Viability Assessment Contrast CT Studies Compared with Results DSE Agreement in 560 of 576 (97%) segments. CE‐CMR Agreement in 415 of 448 (93%) segments Hyperenhancement [subendocardial if <50% wall thickness &transmural if >50%] J Am Coll Cardiol. 2007; 49: 1178‐ 1185. 2 weeks of STEMI [N=28] J Am Coll Cardiol. 2005; 45: 2042‐ 2047 A/c or c/c MI [first‐pass MDCT, first‐pass CMR, DE‐ MDCT, and DE‐CMR] Circulation. 2006; 113: 823‐ 833 Good agreement (82%) in delayed hyperenhanced b/w DE‐ regions on a segmental basis MDCT & DE‐ Slightly better concordance CMR for a/c than c/c pts. Dr Nithin P G
Comparison b/w different investigations Dr Nithin P G
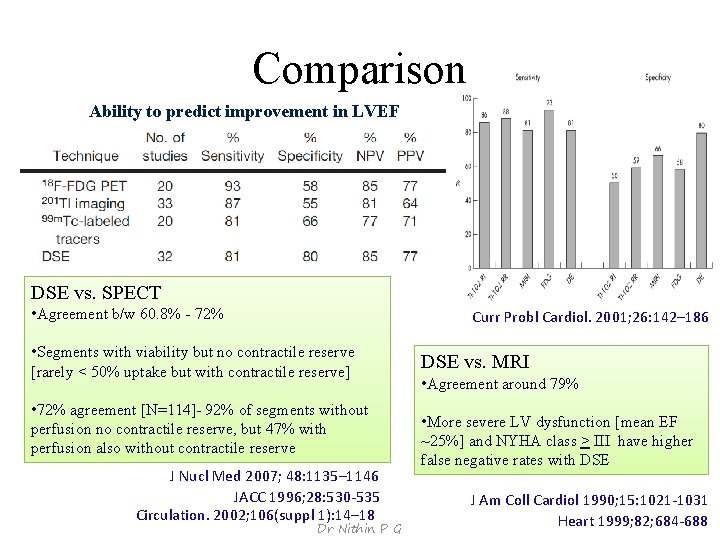
Comparison Ability to predict improvement in LVEF DSE vs. SPECT • Agreement b/w 60. 8% - 72% Curr Probl Cardiol. 2001; 26: 142– 186 • Segments with viability but no contractile reserve [rarely < 50% uptake but with contractile reserve] • 72% agreement [N=114]- 92% of segments without perfusion no contractile reserve, but 47% with perfusion also without contractile reserve J Nucl Med 2007; 48: 1135– 1146 JACC 1996; 28: 530‐ 535 Circulation. 2002; 106(suppl 1): 14– 18 Dr Nithin P G DSE vs. MRI • Agreement around 79% • More severe LV dysfunction [mean EF ~25%] and NYHA class > III have higher false negative rates with DSE J Am Coll Cardiol 1990; 15: 1021‐ 1031 Heart 1999; 82; 684‐ 688
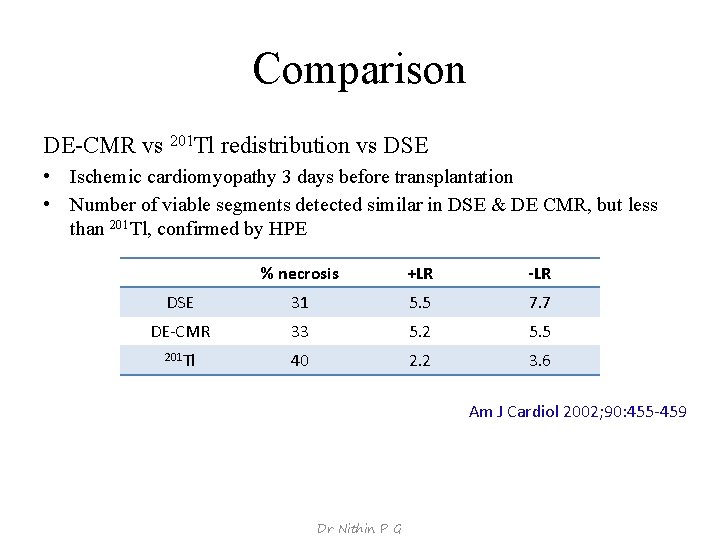
Comparison DE-CMR vs 201 Tl redistribution vs DSE • Ischemic cardiomyopathy 3 days before transplantation • Number of viable segments detected similar in DSE & DE CMR, but less than 201 Tl, confirmed by HPE % necrosis +LR -LR DSE 31 5. 5 7. 7 DE‐CMR 33 5. 2 5. 5 201 Tl 40 2. 2 3. 6 Am J Cardiol 2002; 90: 455‐ 459 Dr Nithin P G
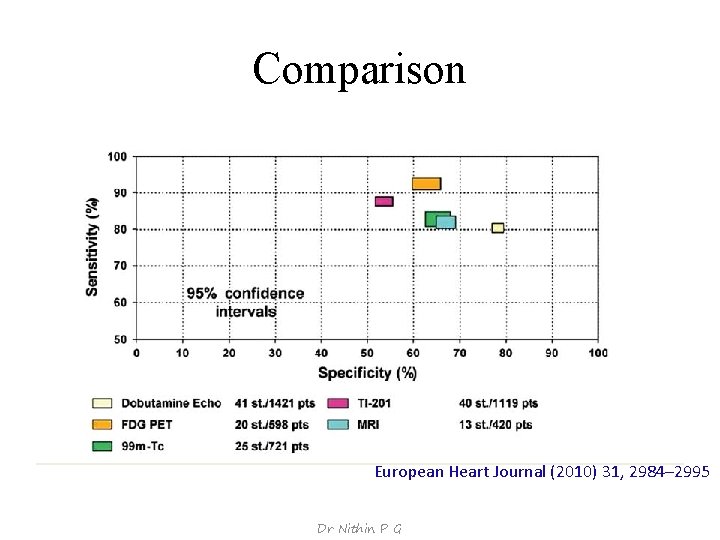
Comparison European Heart Journal (2010) 31, 2984– 2995 Dr Nithin P G
Clinical correlation Dr Nithin P G
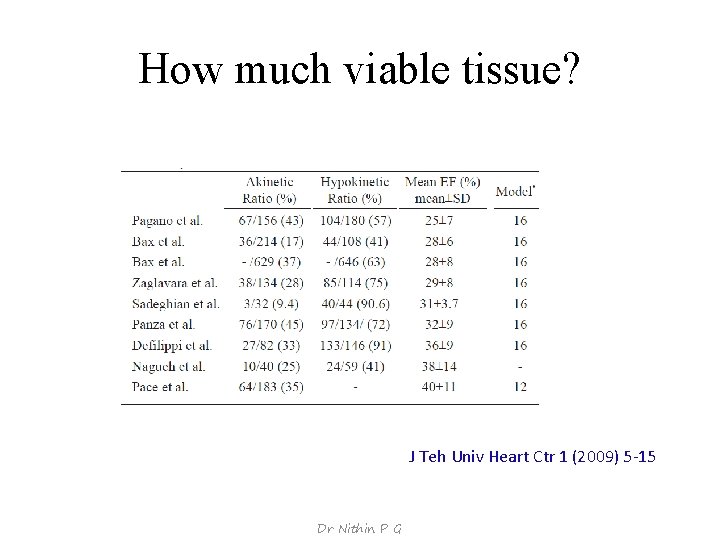
How much viable tissue? J Teh Univ Heart Ctr 1 (2009) 5‐ 15 Dr Nithin P G
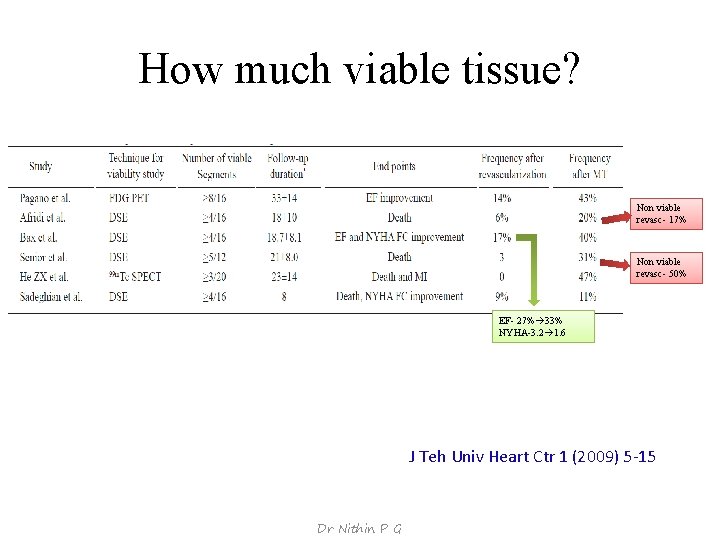
How much viable tissue? Non viable revasc- 17% Non viable revasc- 50% EF- 27% 33% NYHA-3. 2 1. 6 J Teh Univ Heart Ctr 1 (2009) 5‐ 15 Dr Nithin P G
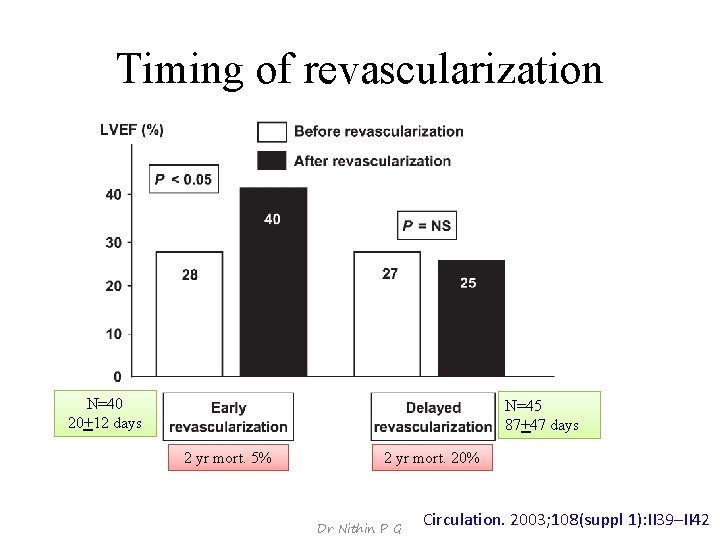
Timing of revascularization N=40 20+12 days N=45 87+47 days 2 yr mort. 5% 2 yr mort. 20% Dr Nithin P G Circulation. 2003; 108(suppl 1): II 39–II 42
![Viability and coronary circulation Study [N=41] previous Q wave infarction and SV‐CAD [compared viability Viability and coronary circulation Study [N=41] previous Q wave infarction and SV‐CAD [compared viability](http://slidetodoc.com/presentation_image_h2/74405f11233ae7d76a35d60dff7599c5/image-29.jpg)
Viability and coronary circulation Study [N=41] previous Q wave infarction and SV‐CAD [compared viability with angiographic variables, including the degree of patency & collateralization]. Imaging 201 Tl SPECT Rev Port Cardiol 1996; 15: 313‐ 320 [N=64]CAD & LV dysfunction [whether coronary patency could help in assessing viability] Angiology 2007; 58: 550‐ 555 • No association b/w TIMI grade and reversibility • Collateral circulation associated with viability, but absence did not exclude viability. PET Patent arteries more likely to be viable Akinetic segments by occluded arteries (56 vs. 23, 72%) Dyskinetic segments non‐viable (86%) and supplied by occluded arteries (77%). DSE 18 (38. 3%) viable 29 (61. 7%) non‐viable significant coronary collateral circulation in viable [66. 7% (12 patients)] and non viable [20. 7% (6 patients]. Good coronary collaterals sens. (75%) & spec. (65. 7%) Clin Cardiol 2003; 26: 60‐ 66 [N=47] total occlusion. good coronary collaterals had a high sensitivity (75%) and specificity (65. 7%) as well as high positive predictive (75%) and negative predictive values (79%) Findings Dr Nithin P G
Benefits of Viability Assessment Dr Nithin P G
Meta-analysis J Am Coll Cardiol 2002; 39: 1151– 8 • Late survival with revasc. vs. medical therapy after myocardial viability testing in pts with severe CAD & LV dysfunction • 24 studies Thallium, PET & DSE • N= 3, 088 (2, 228 men), EF 32+8%, followed for 25+10 months Dr Nithin P G
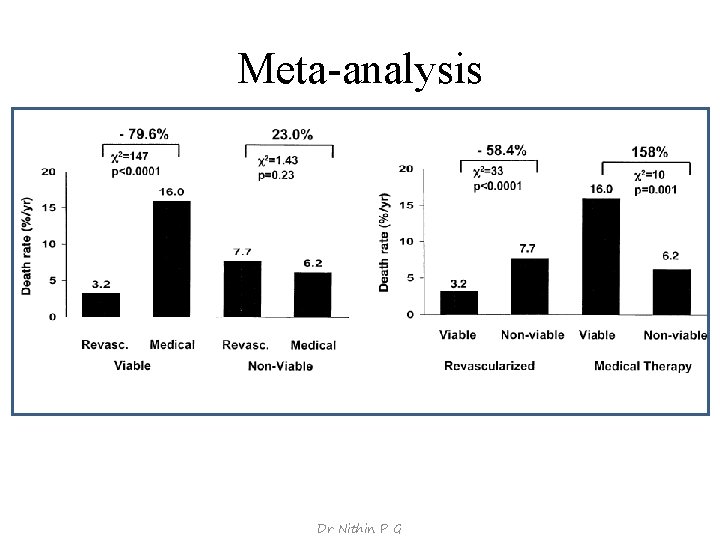
Meta-analysis Dr Nithin P G
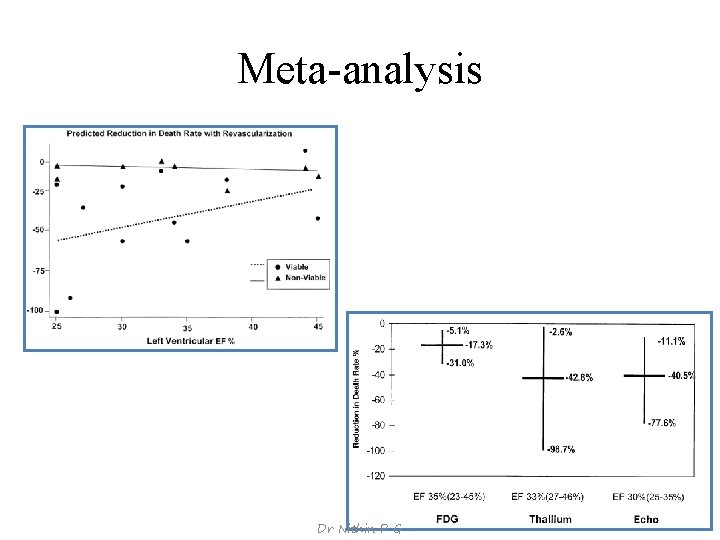
Meta-analysis Dr Nithin P G
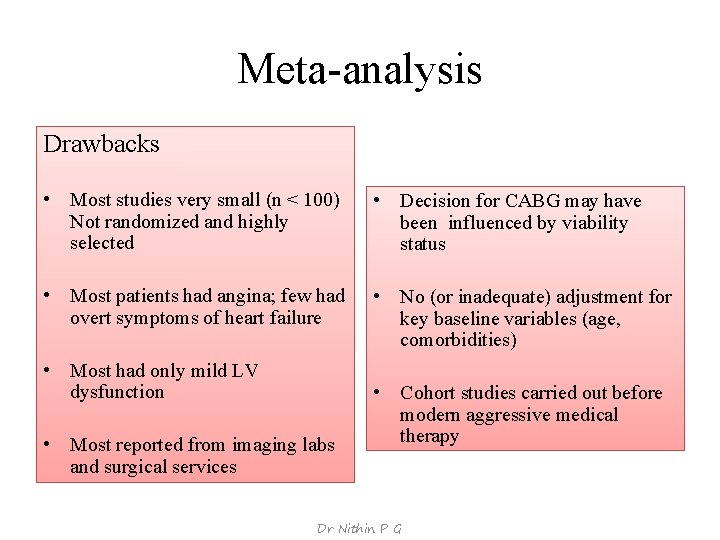
Meta-analysis Drawbacks • Most studies very small (n < 100) Not randomized and highly selected • Decision for CABG may have been influenced by viability status • Most patients had angina; few had overt symptoms of heart failure • No (or inadequate) adjustment for key baseline variables (age, comorbidities) • Most had only mild LV dysfunction • Most reported from imaging labs and surgical services • Cohort studies carried out before modern aggressive medical therapy Dr Nithin P G
![PARR 2 • [N=430]; EF ≤ 35% considered for revascularization, transplant, or HF work‐ PARR 2 • [N=430]; EF ≤ 35% considered for revascularization, transplant, or HF work‐](http://slidetodoc.com/presentation_image_h2/74405f11233ae7d76a35d60dff7599c5/image-35.jpg)
PARR 2 • [N=430]; EF ≤ 35% considered for revascularization, transplant, or HF work‐ up with high suspicion of CAD. • Randomized patients to a PET‐guided therapy or “standard care” (no PET). • Imaging physicians issued a therapy recommendation based on PET findings and treating physicians then made a decision regarding revascularization. • Patients in the standard care arm had no PET, but could have another viability test, which was performed in 138 of 209 (66%) patients. • Primary outcome: composite of cardiac death, myocardial infarction, or recurrent cardiac hospitalization within 1 year. J Am Coll Cardiol 2007; 50: 2002‐ 2012 Dr Nithin P G
![PARR 2 Hazard ratio 0. 78 [95% CI –(0. 58 to 1. 1)] [p= PARR 2 Hazard ratio 0. 78 [95% CI –(0. 58 to 1. 1)] [p=](http://slidetodoc.com/presentation_image_h2/74405f11233ae7d76a35d60dff7599c5/image-36.jpg)
PARR 2 Hazard ratio 0. 78 [95% CI –(0. 58 to 1. 1)] [p= 0. 15] Dr Nithin P G
![PARR 2 Hazard ratio 0. 62 [95% CI- (0. 42 to 0. 93)][p=0. 019] PARR 2 Hazard ratio 0. 62 [95% CI- (0. 42 to 0. 93)][p=0. 019]](http://slidetodoc.com/presentation_image_h2/74405f11233ae7d76a35d60dff7599c5/image-37.jpg)
PARR 2 Hazard ratio 0. 62 [95% CI- (0. 42 to 0. 93)][p=0. 019] Dr Nithin P G
![HEART Trial • RCT [N=800] symptomatic HF, EF ≤ 35%, and evidence of substantial HEART Trial • RCT [N=800] symptomatic HF, EF ≤ 35%, and evidence of substantial](http://slidetodoc.com/presentation_image_h2/74405f11233ae7d76a35d60dff7599c5/image-38.jpg)
HEART Trial • RCT [N=800] symptomatic HF, EF ≤ 35%, and evidence of substantial myocardial viability to conservative vs. CAG with the intention of revascularization. • Stopped early -138 pts enrolled, 69 randomized to revascularization, but only 45 underwent a procedure. Eur J Heart Fail 2011; 13: 227‐ 33 Dr Nithin P G
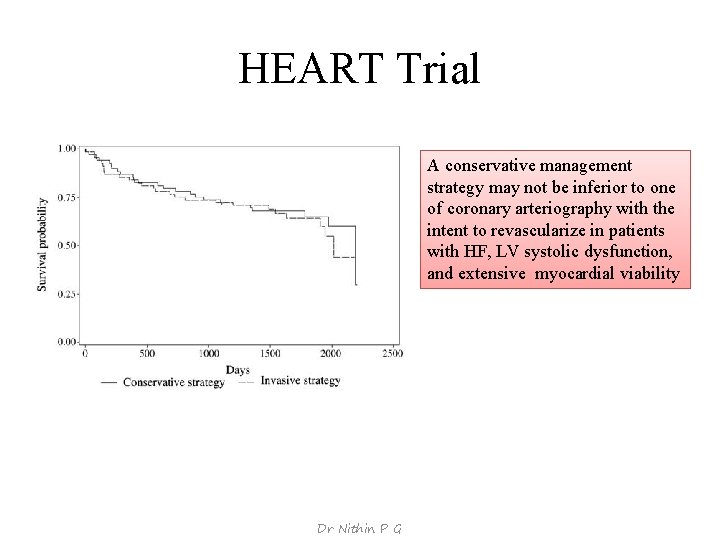
HEART Trial A conservative management strategy may not be inferior to one of coronary arteriography with the intent to revascularize in patients with HF, LV systolic dysfunction, and extensive myocardial viability Dr Nithin P G
N Engl J Med 2011; 364: 1617‐ 25 • The first prospective randomized trial testing the hypothesis that CABG improves survival in patients with ischemic LV dysfunction [EF-26. 7%± 8. 6] compared to outcome with aggressive medical therapy • Myocardial viability identifies patients with CAD and LV dysfunction who have the greatest survival benefit with CABG compared to aggressive medical therapy Dr Nithin P G
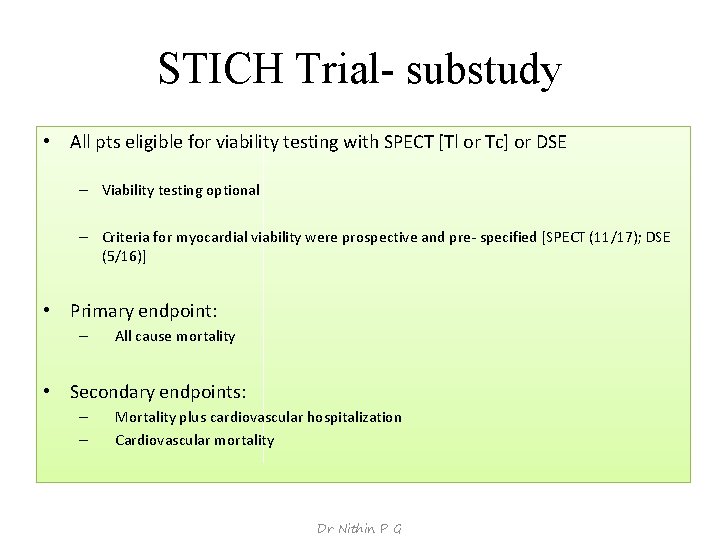
STICH Trial- substudy • All pts eligible for viability testing with SPECT [Tl or Tc] or DSE – Viability testing optional – Criteria for myocardial viability were prospective and pre‐ specified [SPECT (11/17); DSE (5/16)] • Primary endpoint: – All cause mortality • Secondary endpoints: – – Mortality plus cardiovascular hospitalization Cardiovascular mortality Dr Nithin P G
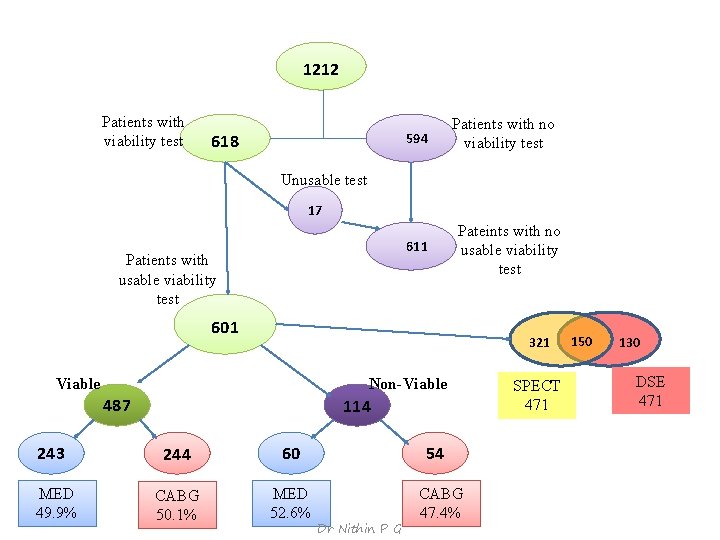
1212 Patients with viability test 618 594 Patients with no viability test Unusable test 17 611 Patients with usable viability test Pateints with no usable viability test 601 321 Viable Non-Viable 487 243 MED 49. 9% 114 244 60 CABG 50. 1% MED 52. 6% 54 Dr Nithin P G CABG 47. 4% SPECT 471 150 130 DSE 471
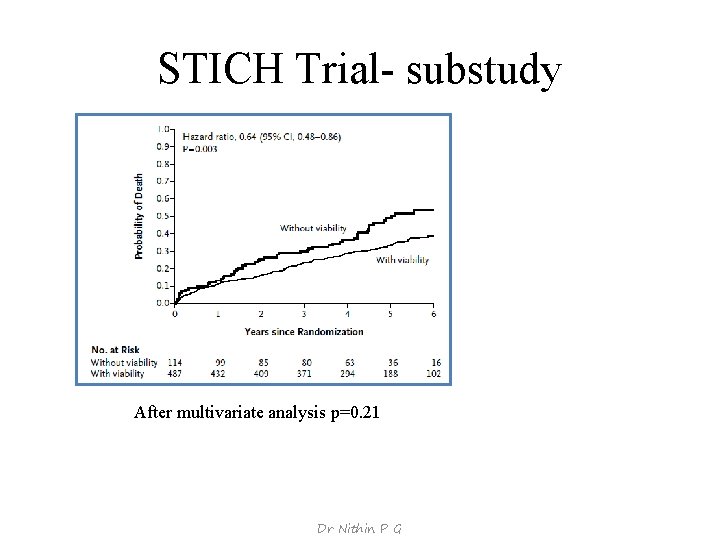
STICH Trial- substudy After multivariate analysis p=0. 21 Dr Nithin P G
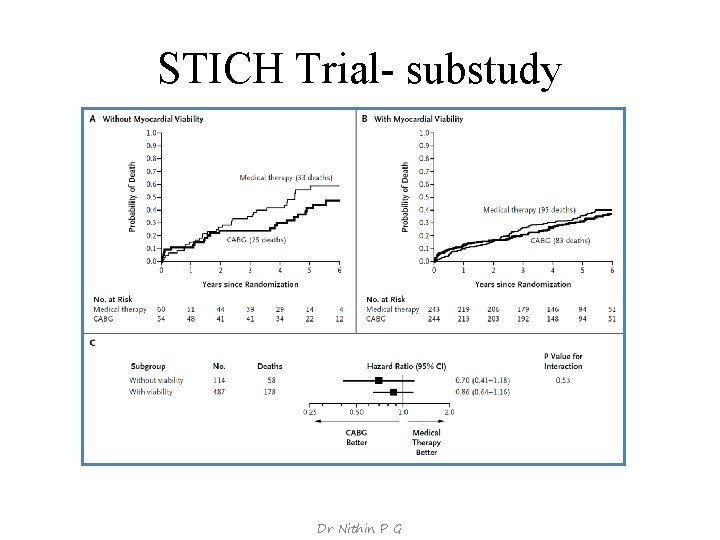
STICH Trial- substudy Dr Nithin P G
STICH Trial- substudy • Substudy of a major trial • Viability study according to the judgement of physician • Small number of non viable group for comparison • Sx influenced by timing and results of viability test • Two types of viability tests‐SPECT & DSE • Better medical therapy available • Combined procedure [CABG + SVR] done probably not optimum In patients with CAD and LV dysfunction, assessment of myocardial viability does not identify patients who will have the greatest survival benefit from adding CABG to aggressive medical therapy Dr Nithin P G
Conclusions Dr Nithin P G
Conclusions • Limitations in study design and test inaccuracies ‐prevented the detection of a true interaction b/w viability & benefit of revascularization • Advances in medical therapy markedly reduced the added benefit of revascularization • The critical information may not lie in the presence but rather in the absence of viability. • The benefit of CABG may only be related to revascularization of potentially ischemic segments. • The greatest benefit of CABG may be limited to those patients with more advanced forms of the disease[those with relatively small amount of viable myocardium] Dr Nithin P G
Conclusions • Currently available evidence does not support the use of viability testing as the arbitrator in the decision making process regarding revascularization in ischemic cardiomyopathy • Ischemic cardiomyopathy [heterogeneous population] multiple factors play important prognostic role. Viability alone cannot provide an unequivocal answer • Prospective trials demystify the emphasis previously placed – without appropriate evidence‐‐ in the significance of myocardial viability • These observations urge physicians to consider the multiplicity of factors involved in the decision making process in this complex population of patients. Dr Nithin P G
Thank you Dr Nithin P G
- Slides: 49