Veterans Guide to Effective Chronic Pain Management Materials





- Slides: 22
Veteran's Guide to Effective Chronic Pain Management Materials Created By: Durham Interdisciplinary Pain Clinic (DIPC) of the Durham VA Health Care System Funding Provided By: VISN 6 Mid-Atlantic Research, Education and Clinic Center (MIRECC)

Goals for Today 1 Define pain (acute and chronic) 2 Basic ways to manage pain and improve function 3 Understand pain and its impact on your life 4 Tips to help you communicate with medical provider(s) 2

Define Pain 3
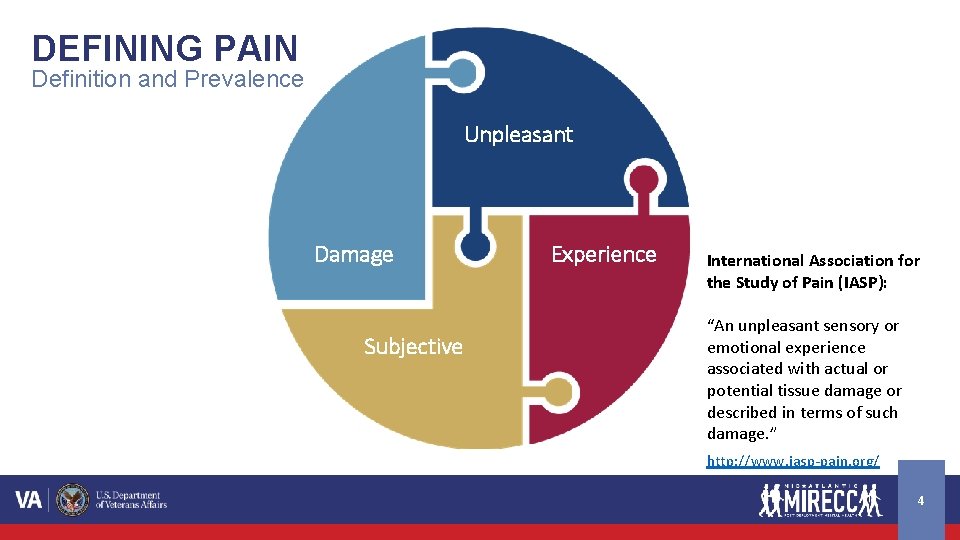
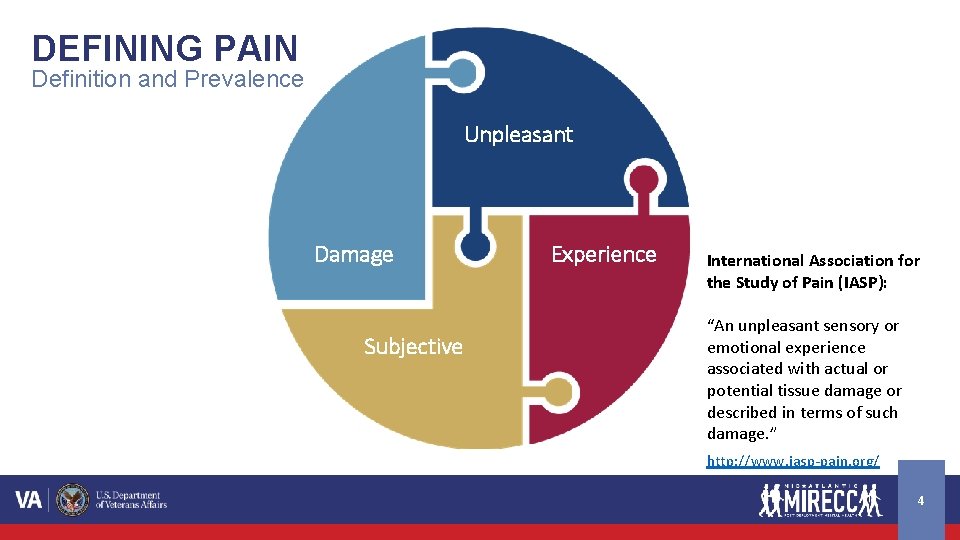
DEFINING PAIN Definition and Prevalence Unpleasant Damage Subjective Experience International Association for the Study of Pain (IASP): “An unpleasant sensory or emotional experience associated with actual or potential tissue damage or described in terms of such damage. ” http: //www. iasp-pain. org/ 4
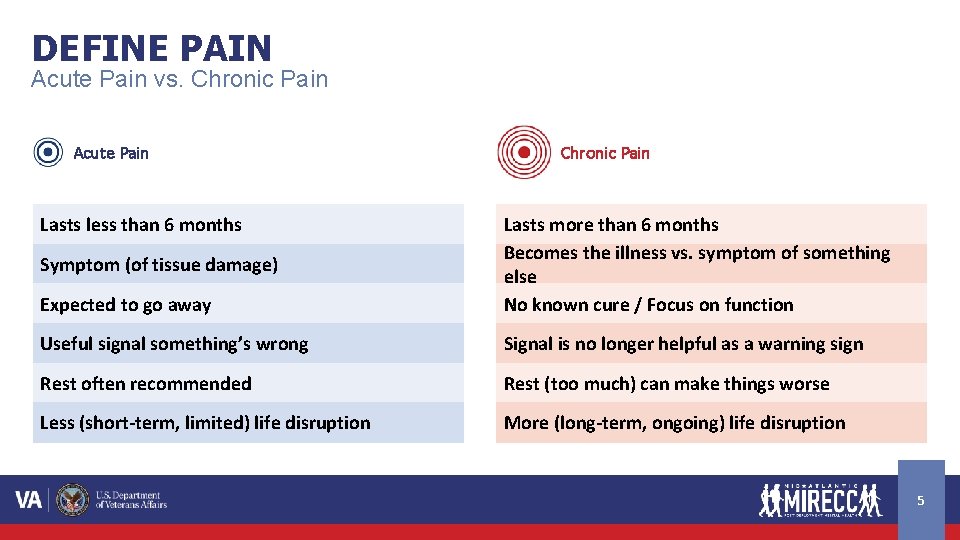
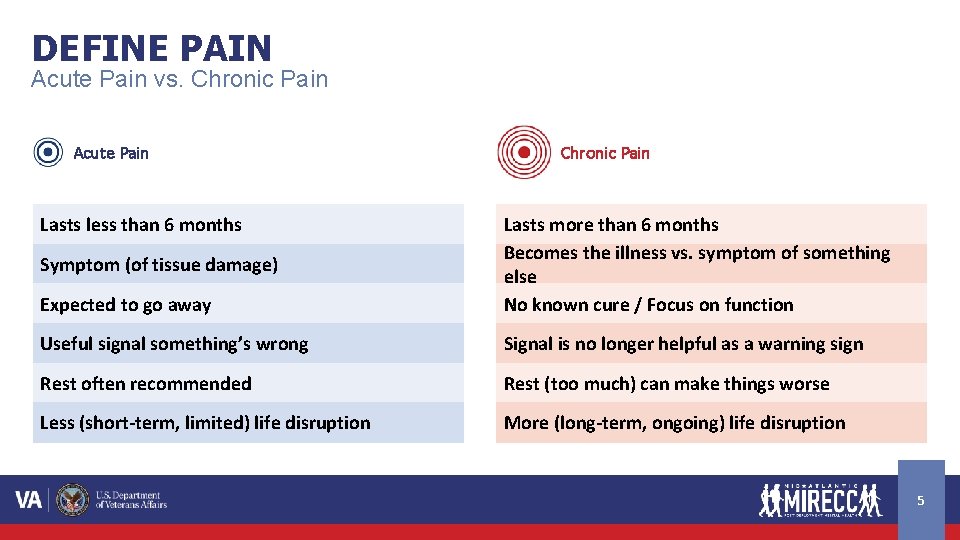
DEFINE PAIN Acute Pain vs. Chronic Pain Acute Pain Lasts less than 6 months Chronic Pain Expected to go away Lasts more than 6 months Becomes the illness vs. symptom of something else No known cure / Focus on function Useful signal something’s wrong Signal is no longer helpful as a warning sign Rest often recommended Rest (too much) can make things worse Less (short-term, limited) life disruption More (long-term, ongoing) life disruption Symptom (of tissue damage) 5
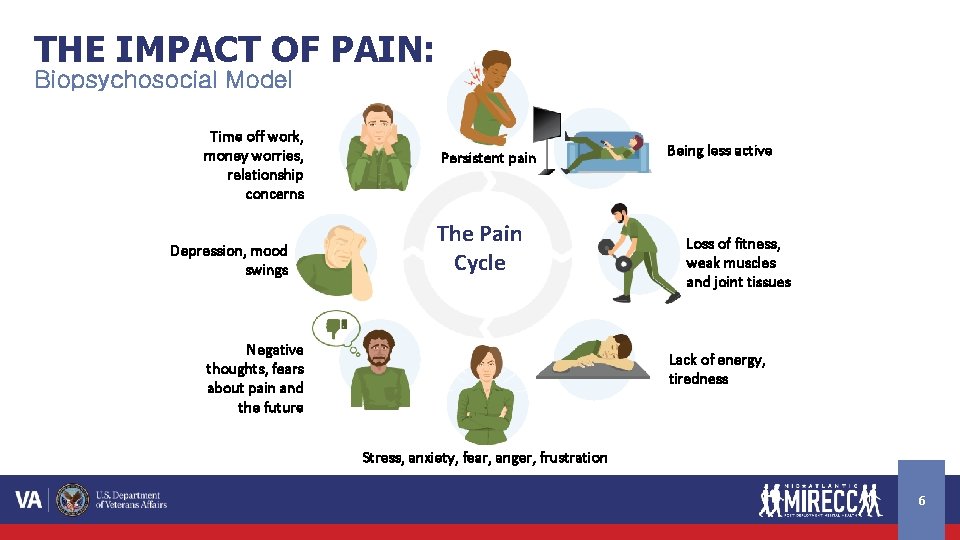
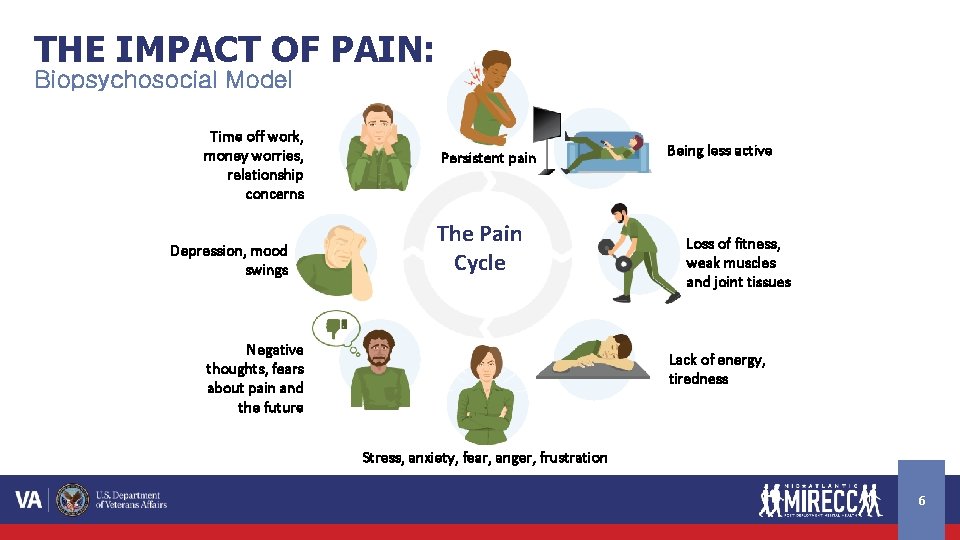
THE IMPACT OF PAIN: Biopsychosocial Model Time off work, money worries, relationship concerns Depression, mood swings Persistent pain The Pain Cycle Negative thoughts, fears about pain and the future Being less active Loss of fitness, weak muscles and joint tissues Lack of energy, tiredness Stress, anxiety, fear, anger, frustration 6
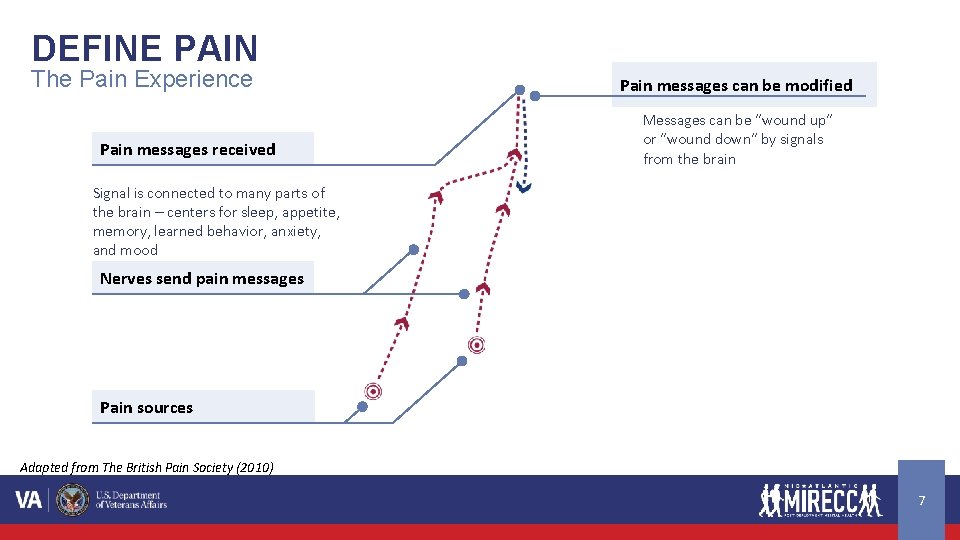
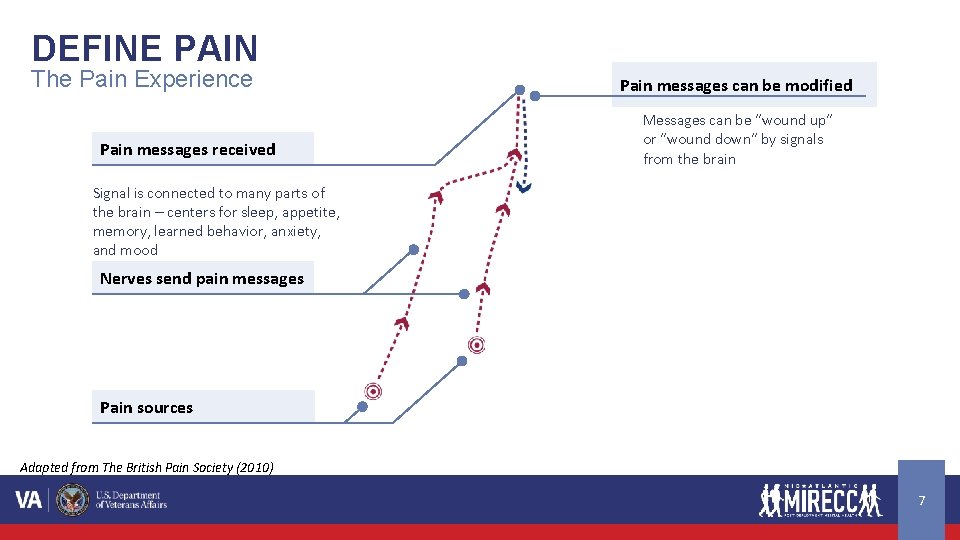
DEFINE PAIN The Pain Experience Pain messages received Pain messages can be modified Messages can be “wound up” or “wound down” by signals from the brain Signal is connected to many parts of the brain – centers for sleep, appetite, memory, learned behavior, anxiety, and mood Nerves send pain messages Pain sources Adapted from The British Pain Society (2010) 7
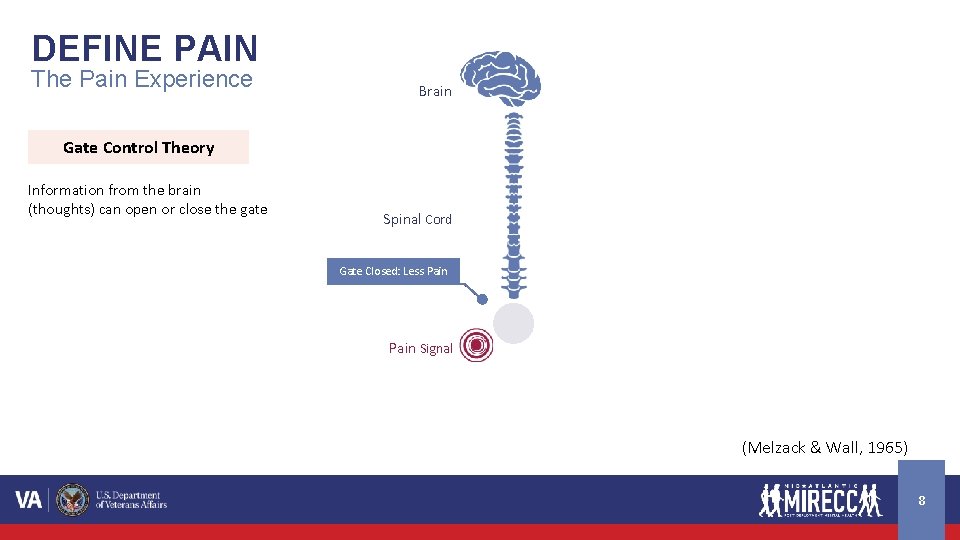
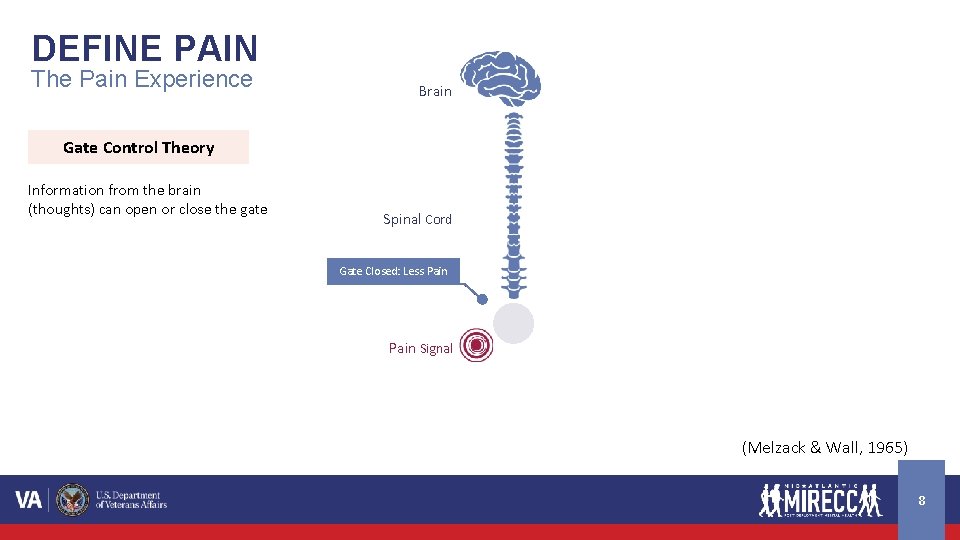
DEFINE PAIN The Pain Experience Brain Gate Control Theory Information from the brain (thoughts) can open or close the gate Spinal Cord Closed: More Less Pain Gate Open: Pain Signal (Melzack & Wall, 1965) 8
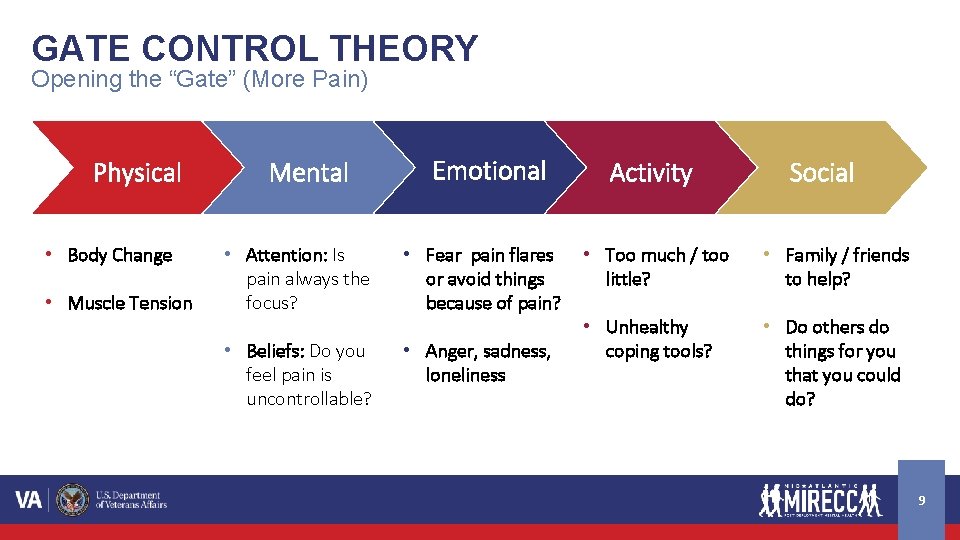
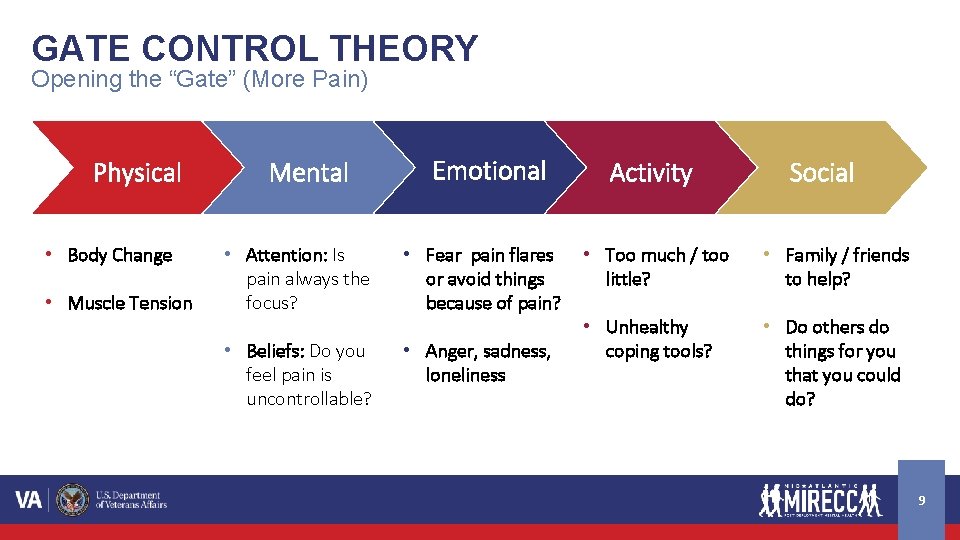
GATE CONTROL THEORY Opening the “Gate” (More Pain) Physical • Body Change • Muscle Tension Mental Emotional • Attention: Is pain always the focus? • Fear pain flares or avoid things because of pain? • Beliefs: Do you feel pain is uncontrollable? • Anger, sadness, loneliness Activity Social • Too much / too little? • Family / friends to help? • Unhealthy coping tools? • Do others do things for you that you could do? 9
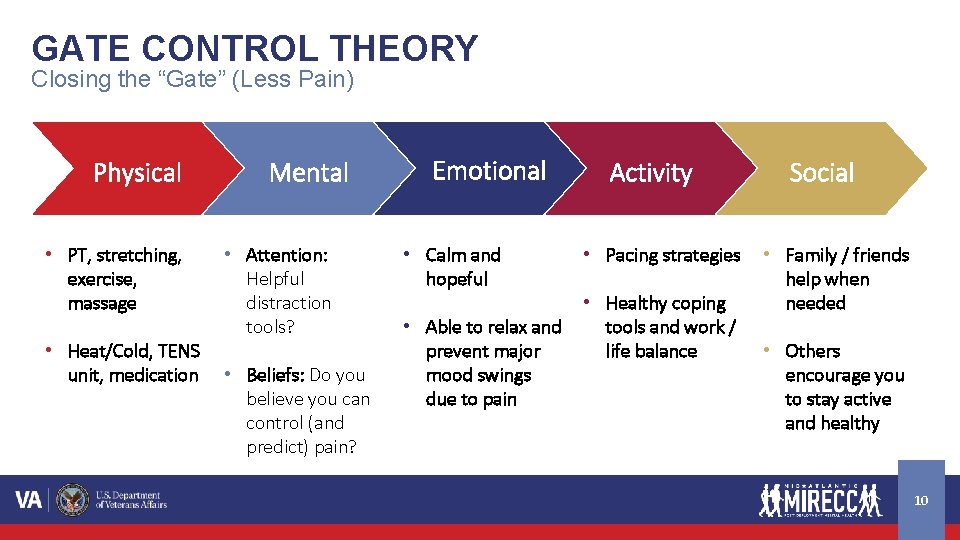
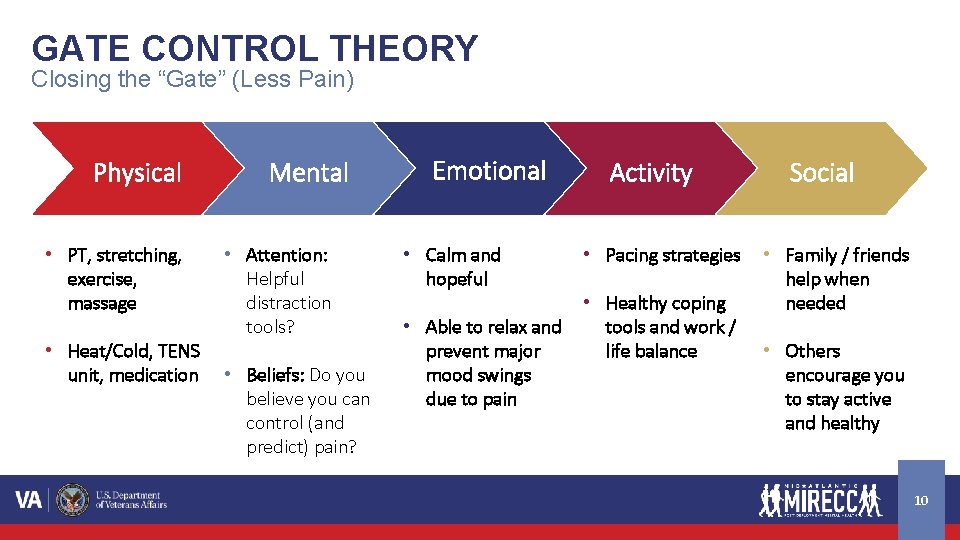
GATE CONTROL THEORY Closing the “Gate” (Less Pain) Physical • PT, stretching, exercise, massage • Heat/Cold, TENS unit, medication Mental • Attention: Helpful distraction tools? • Beliefs: Do you believe you can control (and predict) pain? Emotional • Calm and hopeful • Able to relax and prevent major mood swings due to pain Activity • Pacing strategies • Healthy coping tools and work / life balance Social • Family / friends help when needed • Others encourage you to stay active and healthy 10
Manage Pain 11
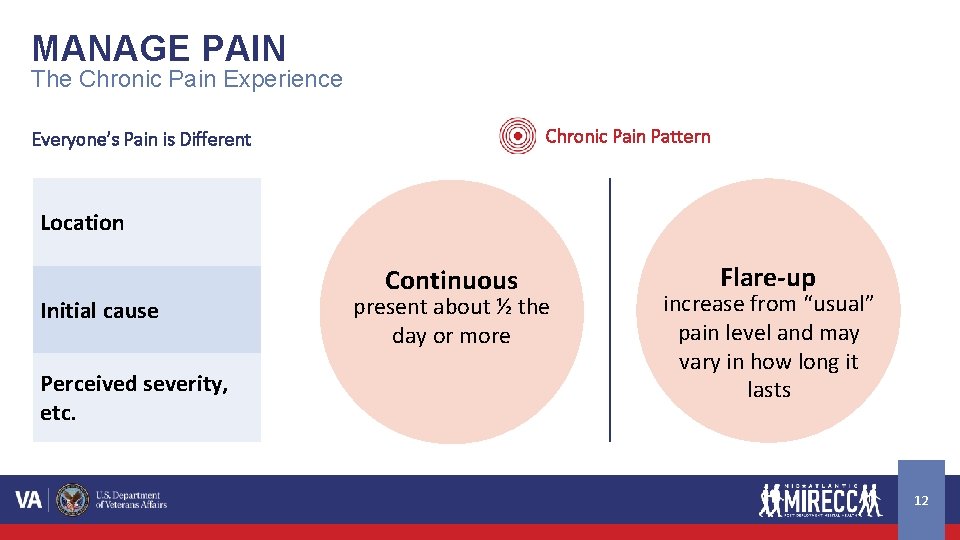
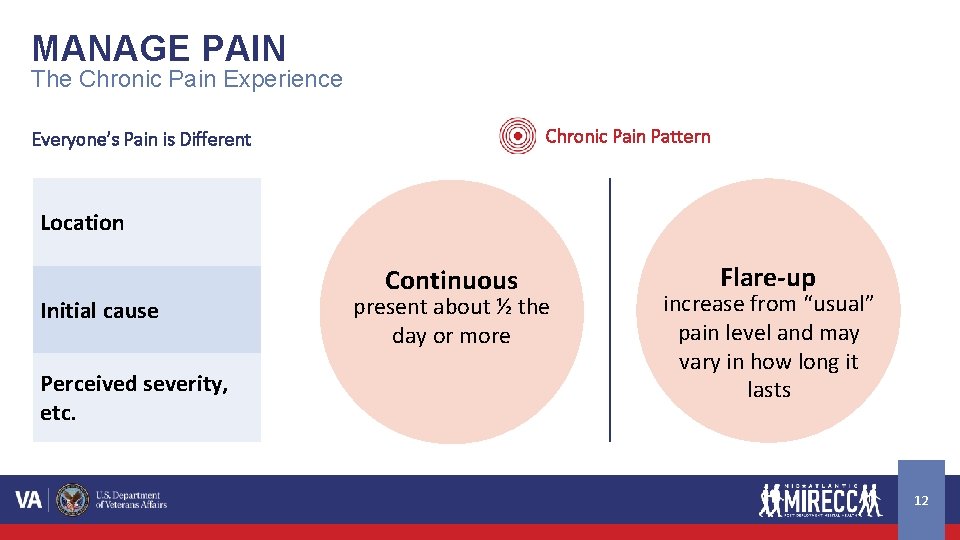
MANAGE PAIN The Chronic Pain Experience Chronic Pain Pattern Everyone’s Pain is Different Location Initial cause Perceived severity, etc. Continuous present about ½ the day or more Flare-up increase from “usual” pain level and may vary in how long it lasts 12
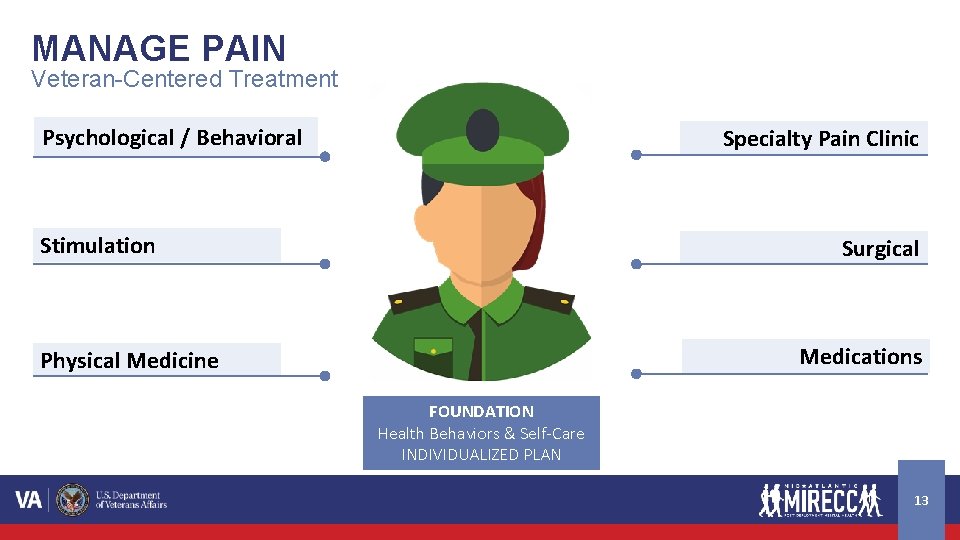
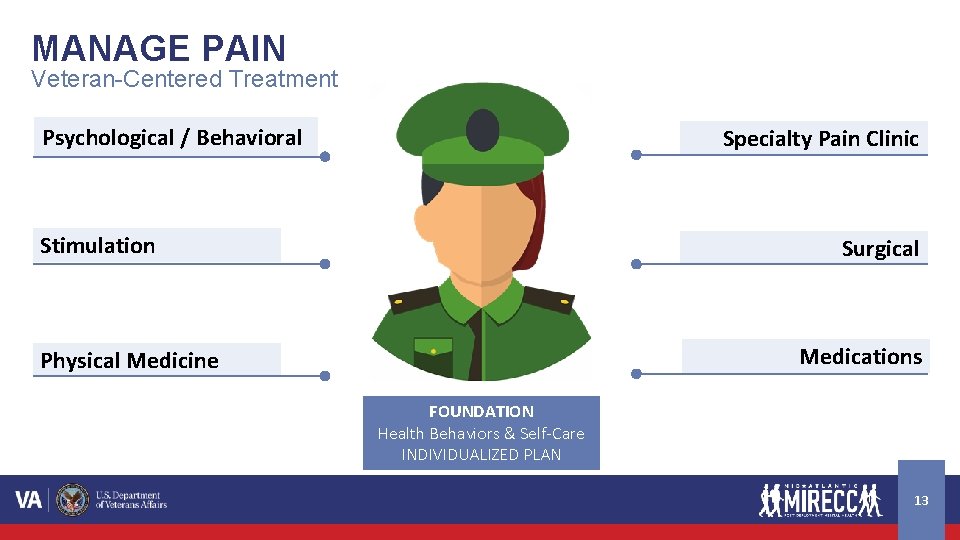
MANAGE PAIN Veteran-Centered Treatment Psychological / Behavioral Specialty Pain Clinic Stimulation Surgical Medications Physical Medicine FOUNDATION Health Behaviors & Self-Care INDIVIDUALIZED PLAN 13
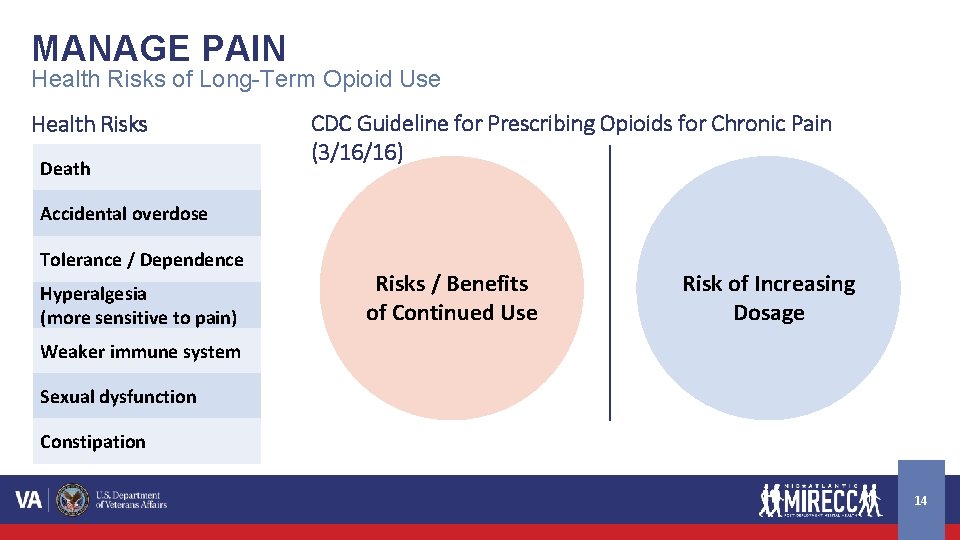
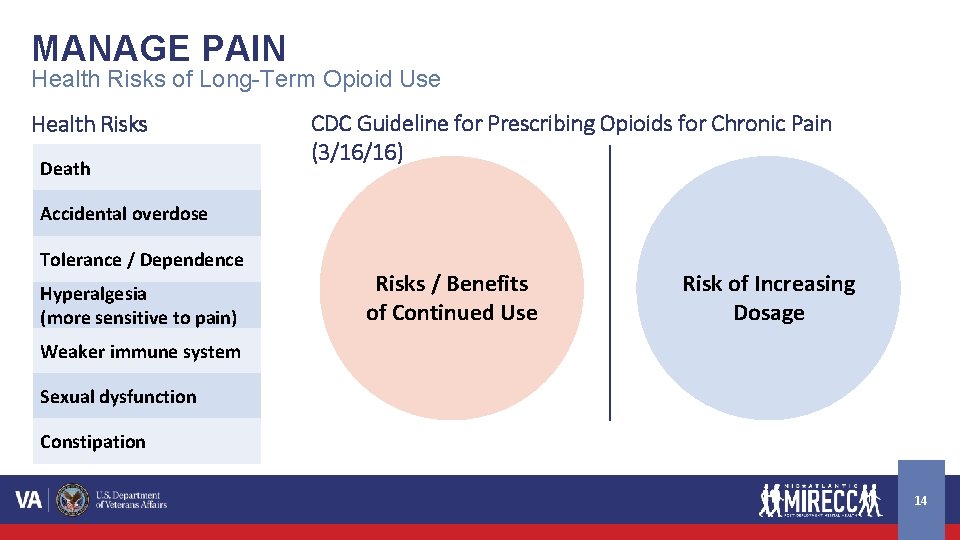
MANAGE PAIN Health Risks of Long-Term Opioid Use Health Risks Death CDC Guideline for Prescribing Opioids for Chronic Pain (3/16/16) Accidental overdose Tolerance / Dependence Hyperalgesia (more sensitive to pain) Risks / Benefits of Continued Use Risk of Increasing Dosage Weaker immune system Sexual dysfunction Constipation 14
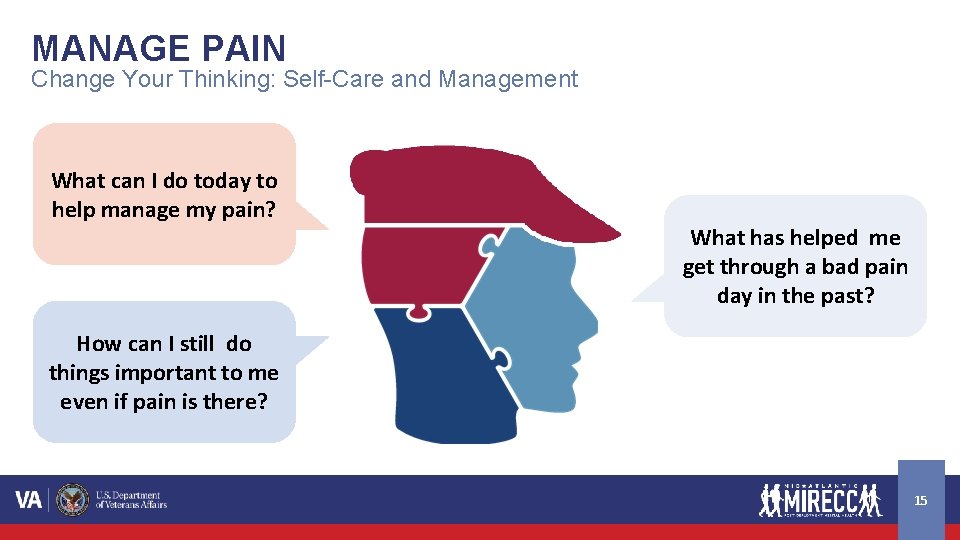
MANAGE PAIN Change Your Thinking: Self-Care and Management What can I do today to help manage my pain? What has helped me get through a bad pain day in the past? How can I still do things important to me even if pain is there? 15
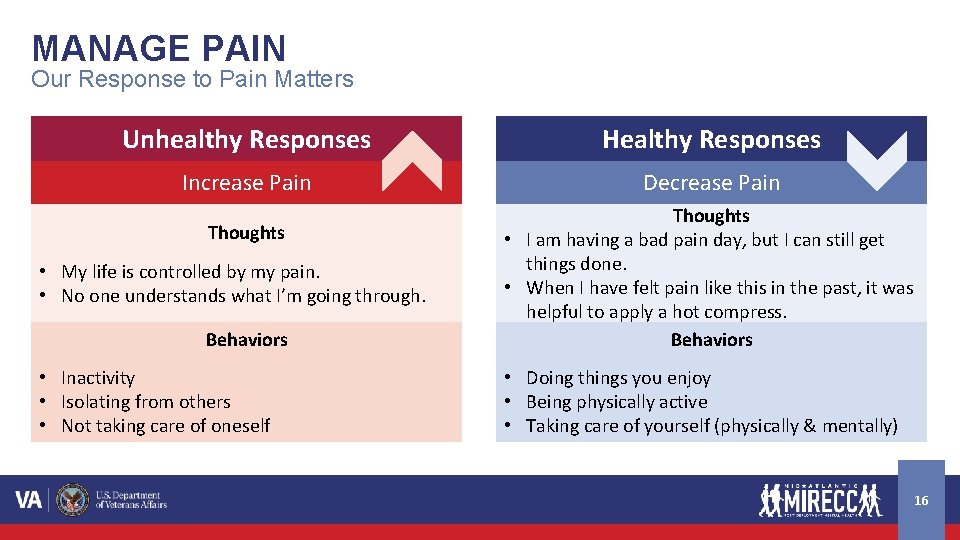
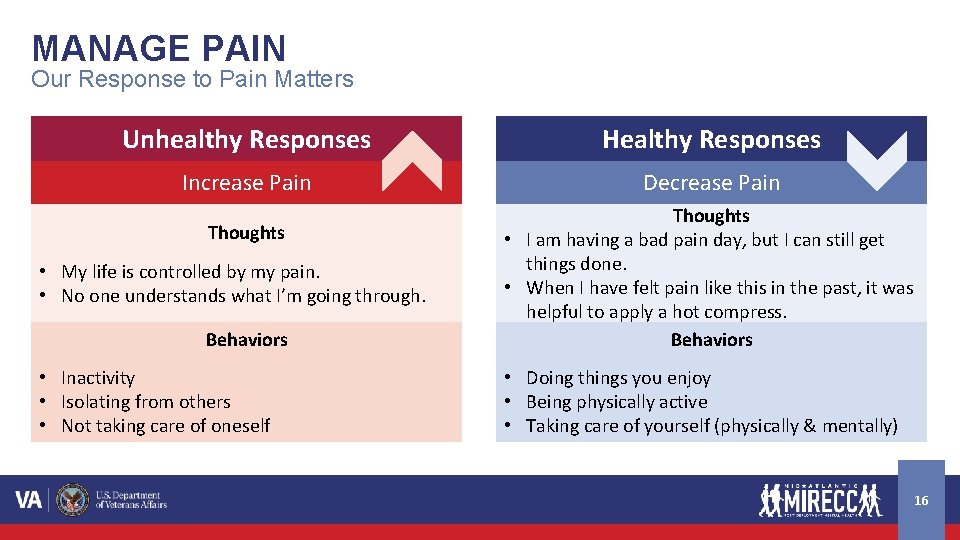
MANAGE PAIN Our Response to Pain Matters Unhealthy Responses Healthy Responses Increase Pain Decrease Pain Thoughts • My life is controlled by my pain. • No one understands what I’m going through. Behaviors • Inactivity • Isolating from others • Not taking care of oneself Thoughts • I am having a bad pain day, but I can still get things done. • When I have felt pain like this in the past, it was helpful to apply a hot compress. Behaviors • Doing things you enjoy • Being physically active • Taking care of yourself (physically & mentally) 16

MANAGE PAIN Self-Care Strategies Stress (Manage Stress) • Relaxation: meditation, prayer, reading a book • Staying active: walking, social activities, volunteering Sleep (Improve Sleep) • Consistent wake time and rise time • Bed only for sleeping • No alcohol / caffeine close to bedtime Healthy Weight (Eat Healthier) • Limit sugary drinks and alcohol • Add more fruits / vegetables / water • Eat at restaurants less often • Use CPAP if prescribed 17

Understand Pain 18
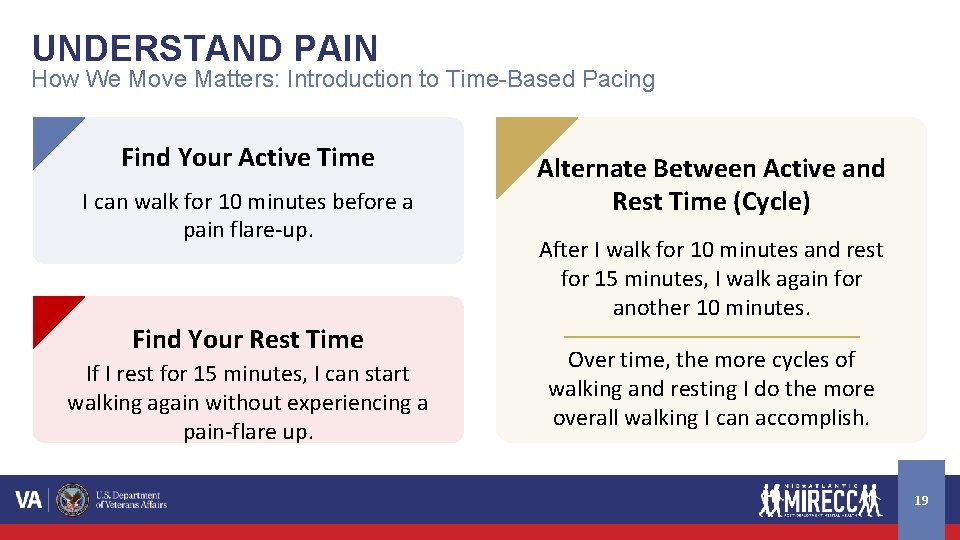
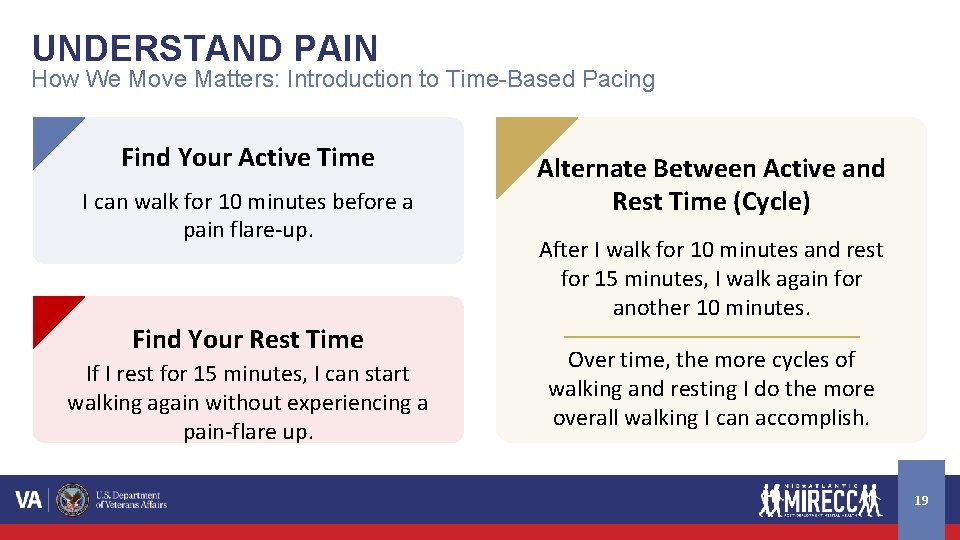
UNDERSTAND PAIN How We Move Matters: Introduction to Time-Based Pacing Find Your Active Time I can walk for 10 minutes before a pain flare-up. Find Your Rest Time If I rest for 15 minutes, I can start walking again without experiencing a pain-flare up. Alternate Between Active and Rest Time (Cycle) After I walk for 10 minutes and rest for 15 minutes, I walk again for another 10 minutes. Over time, the more cycles of walking and resting I do the more overall walking I can accomplish. 19

Communicate Effectively 20
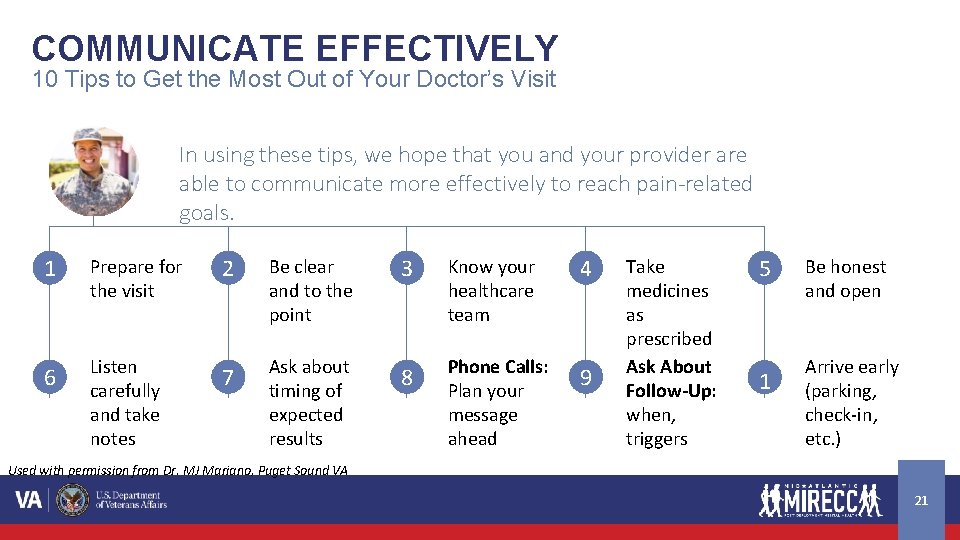
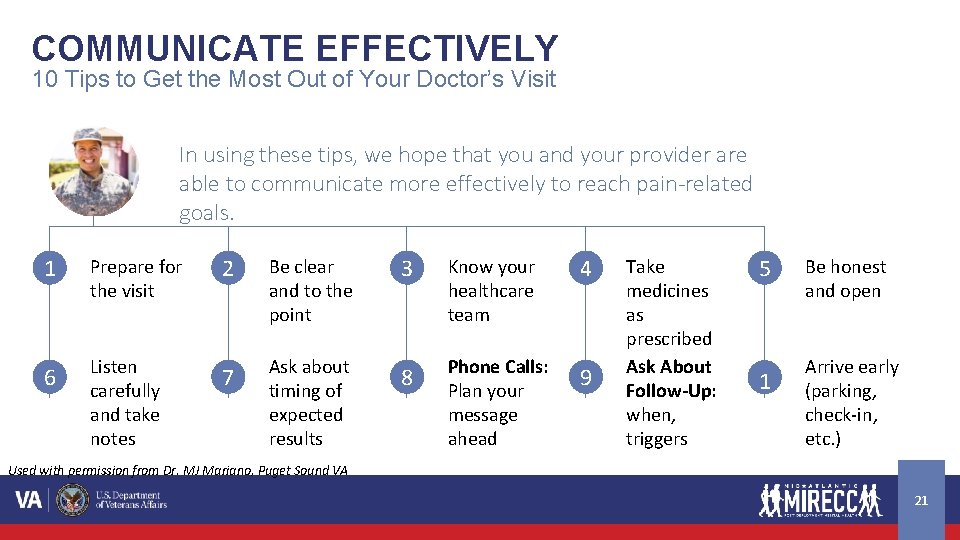
COMMUNICATE EFFECTIVELY 10 Tips to Get the Most Out of Your Doctor’s Visit In using these tips, we hope that you and your provider are able to communicate more effectively to reach pain-related goals. 1 Prepare for the visit 2 Be clear and to the point 3 Know your healthcare team 4 6 Listen carefully and take notes 7 Ask about timing of expected results 8 Phone Calls: Plan your message ahead 9 Take medicines as prescribed Ask About Follow-Up: when, triggers 5 1 0 Be honest and open Arrive early (parking, check-in, etc. ) Used with permission from Dr. MJ Mariano, Puget Sound VA 21
Today's Summary We can live better with pain if we do a few things: 1 Understand our pain better 2 Be an active part of our own pain management 3 Team up with providers and communicate well 22