VESTIBULAR DYSFUNCTION IN THE ACUTE CARE SETTING Alyssa
VESTIBULAR DYSFUNCTION IN THE ACUTE CARE SETTING Alyssa Babitt
Why it’s 1 important ◦ Over age 40, 1 in 3 have experienced symptoms related to a vestibular disorder ◦ Most patients see 4 -5 doctors before receiving a diagnosis ◦ 80% of fallers had symptoms of vestibular impairments ◦ Less than 4% of patients with vertigo will be tested for BPPV in the acute setting ◦ Increased medical costs
Our role in the acute ◦ Assist with differential diagnosis of dizziness ◦ Initiate treatment ◦ Recommend further work up or to another provider ◦ Facilitate transition to home safely 1, 2 setting
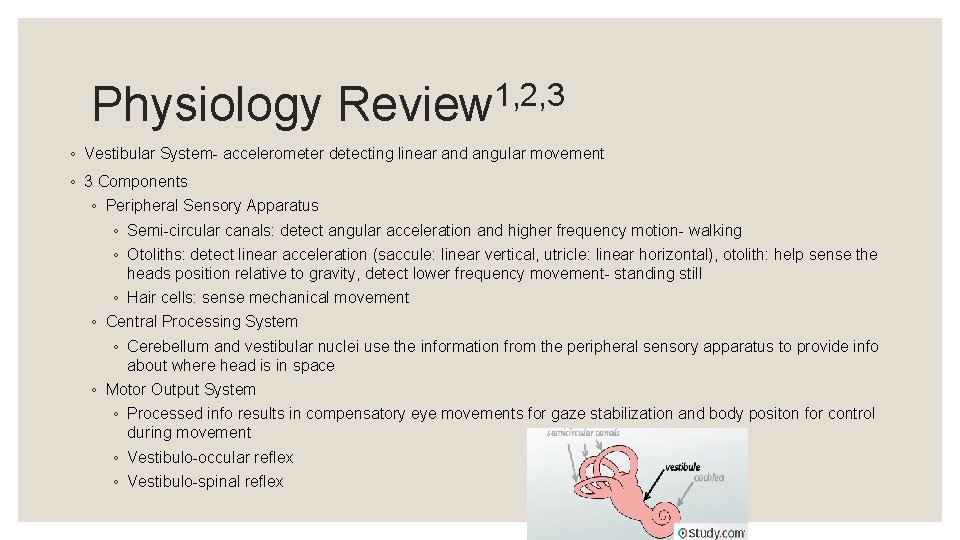
Physiology 1, 2, 3 Review ◦ Vestibular System- accelerometer detecting linear and angular movement ◦ 3 Components ◦ Peripheral Sensory Apparatus ◦ Semi-circular canals: detect angular acceleration and higher frequency motion- walking ◦ Otoliths: detect linear acceleration (saccule: linear vertical, utricle: linear horizontal), otolith: help sense the heads position relative to gravity, detect lower frequency movement- standing still ◦ Hair cells: sense mechanical movement ◦ Central Processing System ◦ Cerebellum and vestibular nuclei use the information from the peripheral sensory apparatus to provide info about where head is in space ◦ Motor Output System ◦ Processed info results in compensatory eye movements for gaze stabilization and body positon for control during movement ◦ Vestibulo-occular reflex ◦ Vestibulo-spinal reflex
Examination◦ ◦ ◦ ◦ ◦ 1, 2, 3 History Onset Continuous or intermittent Duration Intensity Provocative/alleviating factors PMH, Social History, Family History (BPPV) Medications Associated symptoms Tests and measures to date RED FLAGS? ? ◦ Numbness, tingling, weakness, slurred speech, poor coordination, tremors, progressive hearing loss, memory loss, cranial nerve dysfunction

Non-vestibular 2 Vestibular 2 ◦ Vertigo ◦ Associated with other signs/symptoms ◦ Hearing loss ◦ Aural pressure ◦ Otalgia ◦ Nausea/Vomiting ◦ Vision changes ◦ Nystagmus ◦ Oscillopsia ◦ Gradual onset of symptoms ◦ ◦ Presyncope, palpitations, disequilibrium, SOB Spontaneously Gradually worse over time Red Flags?
Differential 2 Diagnosis ◦ Benign Paroxysmal Positional Vertigo ◦ Vestibular Neuritis ◦ Labyrinthitis
2, 4 BPPV ◦ Otoliths become dislodged and move into one of the semicircular canals ◦ Interfere with normal fluid movement and sends false signals to the brain ◦ False information doesn't match with the other ear or eyes causing vertigo ◦ Two types ◦ Canalithiasis- crystals move freely ◦ Cupulolithiasis- crystals are stuck on the bundle of sensory nerves ◦ Findings ◦ ◦ ◦ Pt’s not dizzy if they aren’t moving Insidious onset or secondary to fall/hitting head Room spinning when they change positions that lasts <1 minute Postural instability May be nauseous
BPPV 4, 5 continued ◦ Diagnosis ◦ Positive Dix-Hallpike or Roll Test ◦ Looking for nystagmus ◦ Rotational nystagmus: posterior canal ◦ Lateral nystagmus: lateral canal ◦ Vertical nystagmus: superior canal ◦ Treatment ◦ Canalithiasis Canalith Repositioning Treatment ◦ Posterior: Epley’s ◦ Horizontal: Lempert’s ◦ Superior: Deep head hanging maneuver ◦ Cupulolithiasis Liberatory Maneuver
Vestibular Neuritis and Labyrinthitis 2 ◦ Vestibulocochlear nerve becomes inflamed and disrupts the way information would be interpreted by the brain ◦ Sudden onset of intense vertigo, nausea, vomiting ◦ No hearing loss with vestibular neuritis, hearing loss with labyrinthitis ◦ Dizzy at rest, worse with movement- nystagmus may be present at rest ◦ Gait disturbances ◦ Positive head thrust test and VOR ◦ Smooth pursuits normal ◦ Treat through habituation, balance exercises, and keep them moving!
Main Points ◦ Vertigo is very common in the acute setting and it’s our job as therapists to help diagnose ◦ Know signs and symptoms to look for and who to refer to if need be
References ◦ 1. Lammers K and Steinhorn G. Defining dizziness: an acute approach to vestibular dysfunction in the hospital setting. Combined Sections Meeting 2017. ◦ 2. Campeau M, Grove C, Smith B, and Van Heuklon N. Evaluating and treating patients with vestibular syndromes in acute settings. Combined Sections Meeting 2014. ◦ 3. Smith B. Vestibular Rehabilitation in Acute Care. GPTA and TPTA Meeting 2016. ◦ 4. Bhattacharyya N et al. Clinical practice guideline: benign paroxysmal positional vertigo. Otolaryngol Head Neck Surg. 139 (5 Suppl 4): S 47 -81, 2008. ◦ 5. Fife T. Benign paroxysmal positional vertigo in the acute care setting. Neurologic Clinics. 2017. 33(3); 601 -617.
- Slides: 12