Vertical Strabismus A and V Patterns Matthew D
Vertical Strabismus A and V Patterns Matthew D. Gearinger, MD Professor of Ophthalmology and Pediatrics Associate Chair for Education
Purpose To develop an evaluation and treatment plan for patients with vertical strabismus and A and V pattern strabismus.
Objectives • Summarize the surgical options for patients with congenital or acquired 4 th nerve palsies • Describe the characteristic eye movements in dissociated vertical deviation • List 3 clinical indications for the surgical correction of Brown syndrome • Devise an algorithm for the surgical treatment of A and V pattern strabismus
• Inferior Oblique Dysfunction • Overaction, Palsy • Superior Oblique Dysfunction • Overaction, Palsy, Brown Syndrome • Dissociated Vertical Deviation • Monocular Elevation Deficiency • Orbital Floor Fractures • A and V patterns

Inferior Oblique Overaction May be primary (usually with cong ET), or secondary (to SO palsy). Adducted eye over-elevates (causing RHT in L gaze, or LHT in R gaze). Can be associated with a V-pattern. Surgery by myotomy, recession, anterior transposition (if DVD).
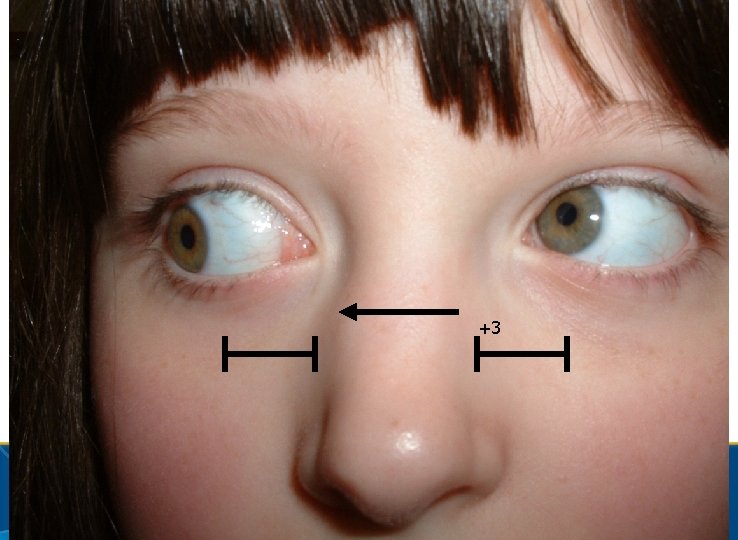
+3
Inferior Oblique Palsy Rare, from damage to inf division of CN III. Inablity to elevate in adduction (like Brown’s) But. . Negative forced duction, A-pattern, +SOOA Treat by ipsilateral SO weakening or contralateral SR recession.
• Inferior Oblique Dysfunction • Overaction, Palsy • Superior Oblique Dysfunction • Overaction, Palsy, Brown Syndrome • Dissociated Vertical Deviation • Monocular Elevation Deficiency • Orbital Floor Fractures • A and V patterns
Superior Oblique Overaction • Nearly always primary (rarely secondary to IO palsy). • Adducted eye over-depresses (RHo. T in L gaze, LHo. T in R gaze) • Associated with A-pattern • Manage by tenotomy (temporal or nasal), or spacer. • Risk of torsional/vertical diplopia post-op in fusing adult.
Which of the following is not a viable surgical treatment of superior oblique palsy? A. Superior oblique tuck B. Ipsilateral inferior oblique myotomy. C. Contralateral inferior oblique anterior transposition D. Contralateral inferior rectus recession E. Ipsilateral superior rectus recession
Superior Oblique Palsy Majority are congenital or traumatic; if acute with no suggestive history, r/o intracranial process. Congenital has large vertical fusion amplitudes and head position (tilt away from paretic muscle). Bilateral cases have large extorsion (>10 degrees, worse in downgaze), alternating HT’s in lateral gaze, ET in down.
Superior Oblique Palsy Surgical options include: • Ipsilateral SO tuck (if large torsion, HT) • Harada-Ito (if isolated torsion) • Ipsilateral IO weakening (if HT<15 D) • Contralateral IR Rec- allows adjustment. • Ipsilateral SR Rec- if tight from longstanding HT.
Which is characteristic of Brown’s syndrome? A. Hypertropia of affected eye in primary gaze. B. Treatment by Harada-Ito procedure. C. Face turn towards affected eye (e. g. R face turn for R Brown’s) D. Limitation of elevation in adduction with positive forced duction.
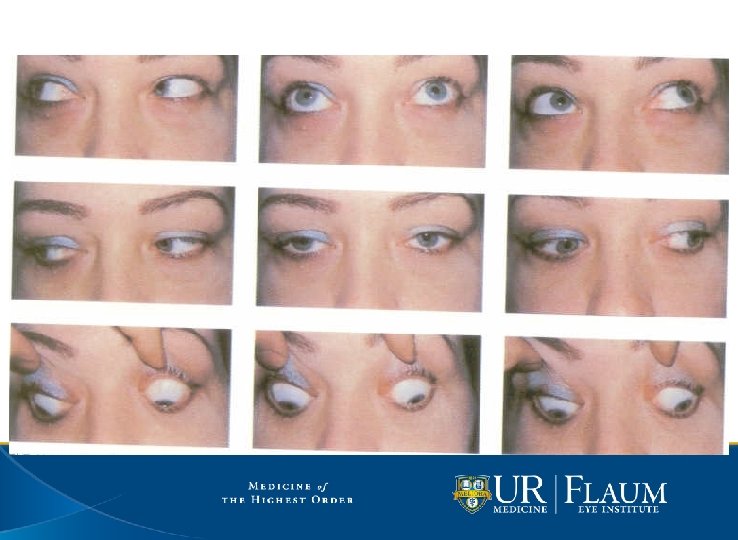
Brown’s Syndrome Inability to elevate in adduction secondary to superior oblique tendon/trochlea dysfunction. Can be primary or secondary to trauma or inflammatory conditions. Acquired forms are often intermittent and can resolved spontaneously. Often XT in upgaze (IO palsy doesn’t).
Brown’s Syndrome Chin-up, face turn away from Brown’s eye (face to left in R Brown’s). Severe cases have hypotropia in primary gaze and downshoot in adduction. Restriction on forced ductions enhanced by retropulsing, extorting and adducting.
Brown’s Syndrome If inflammatory, can inject steroid near trochlea. Observe if no AHP, hypo in primary. Surgery by tenotomy (temporal or nasal) +/- IO weakening, or SO spacer.

-3
• Inferior Oblique Dysfunction • Overaction, Palsy • Superior Oblique Dysfunction • Overaction, Palsy, Brown Syndrome • Dissociated Vertical Deviation • Monocular Elevation Deficiency • Orbital Floor Fractures • A and V patterns
Which is characteristic of DVD? A. Deviation consists of elevation, abduction, and extorsion. B. Refixation causes fellow eye to become hypotropic C. Commonly associated with superior oblique overaction D. Surgery consists of transposing MR/LR to SR.
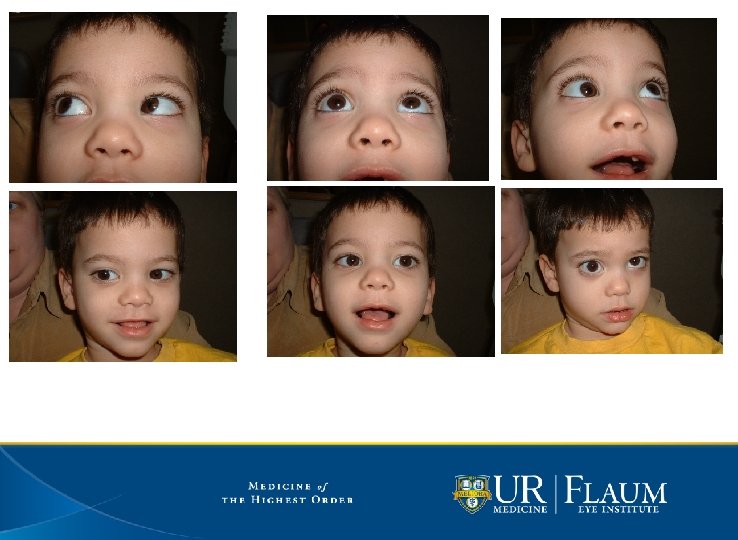
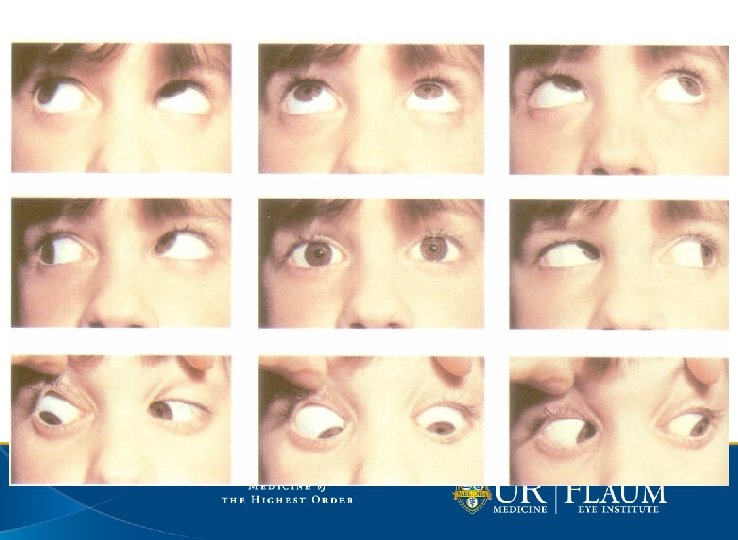
Dissociated Vertical Deviation Common following early-onset strabismus. Deviated (covered) eye elevates, abducts, extorts. When DVD eye takes up fixation, fellow eye does not become hypotropic (violating Hering’s law) Treat by SR Rec/Faden, IO AT.
• Inferior Oblique Dysfunction • Overaction, Palsy • Superior Oblique Dysfunction • Overaction, Palsy, Brown Syndrome • Dissociated Vertical Deviation • Monocular Elevation Deficiency • Orbital Floor Fractures • A and V patterns
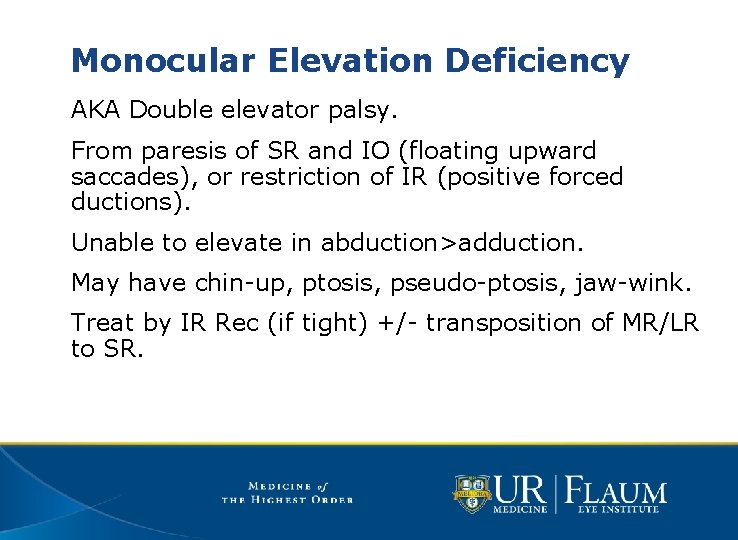
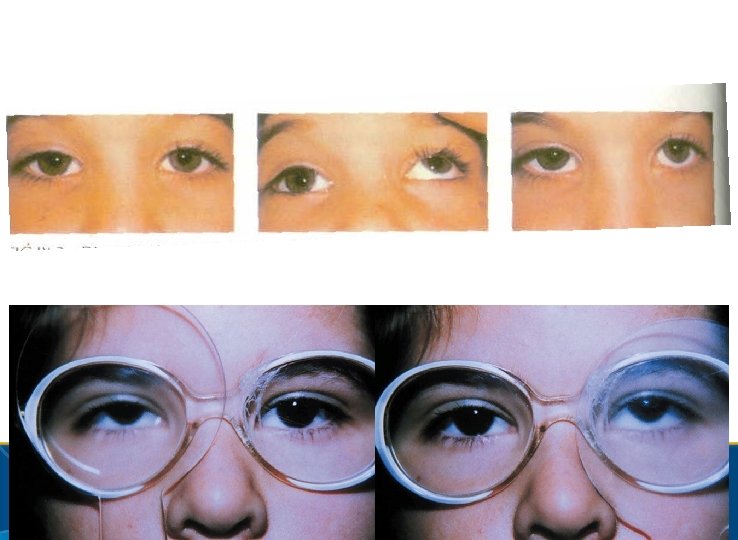
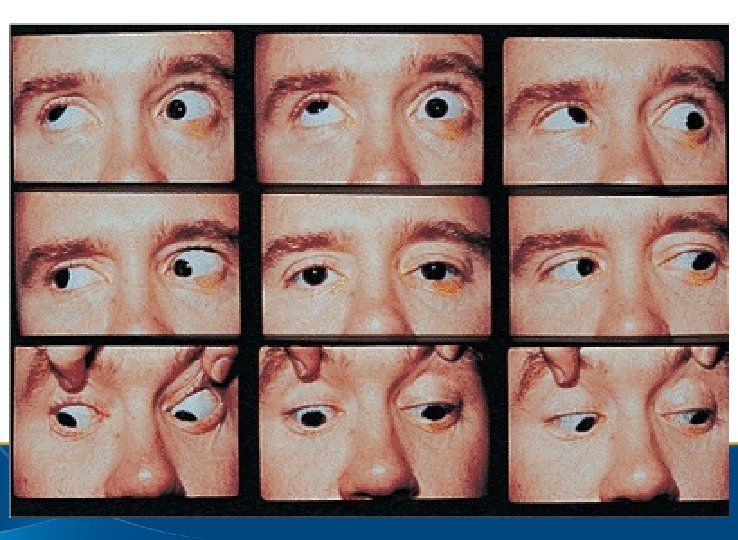
Monocular Elevation Deficiency AKA Double elevator palsy. From paresis of SR and IO (floating upward saccades), or restriction of IR (positive forced ductions). Unable to elevate in abduction>adduction. May have chin-up, ptosis, pseudo-ptosis, jaw-wink. Treat by IR Rec (if tight) +/- transposition of MR/LR to SR.
• Inferior Oblique Dysfunction • Overaction, Palsy • Superior Oblique Dysfunction • Overaction, Palsy, Brown Syndrome • Dissociated Vertical Deviation • Monocular Elevation Deficiency • Orbital Floor Fractures • A and V patterns
Orbital Floor Fractures Enophthalmos, vertical diplopia, hypesthesia of cheek. Eye may be hypotropic in upgaze (IR restriction) and hypertropic in downgaze (paresis). Repair fracture/release IR if early enophthalmos, painful diplopia with entrapment.
Orbital Floor Fractures If paretic pattern (HT on affected side, worse in downgaze), IR Res, +/-SR Rec. If restricted pattern (Ho. T on affected side, worse in upgaze), IR Rec. • Likely will “flip” to HT in down, and will need contralateral IR Faden.
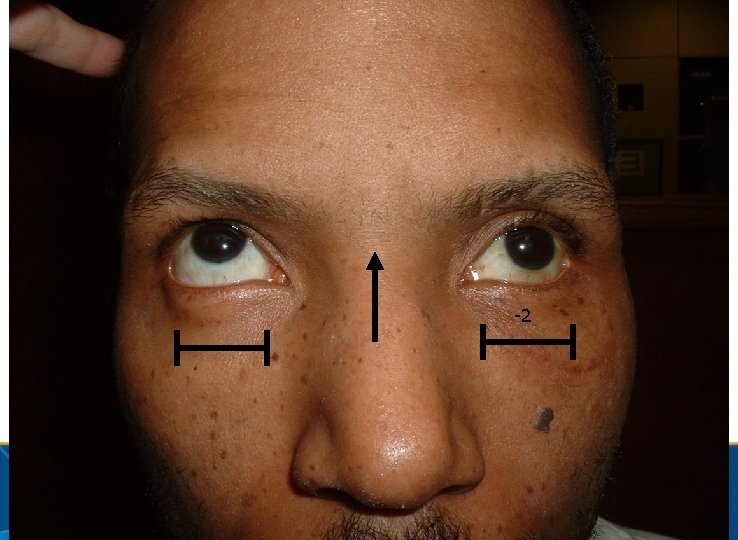
-2
• Inferior Oblique Dysfunction • Overaction, Palsy • Superior Oblique Dysfunction • Overaction, Palsy, Brown Syndrome • Dissociated Vertical Deviation • Monocular Elevation Deficiency • Orbital Floor Fractures • A and V patterns
Which is not correct? A. V-pattern XT can be associated with inferior oblique overaction. B. Craniofacial syndromes are associated with vertically incomitant horizontal strabismus C. A-pattern ET can be treated with bilateral medial rectus recessions, infraplaced. D. Abnormal insertions of the vertical recti can cause A or V patterns.
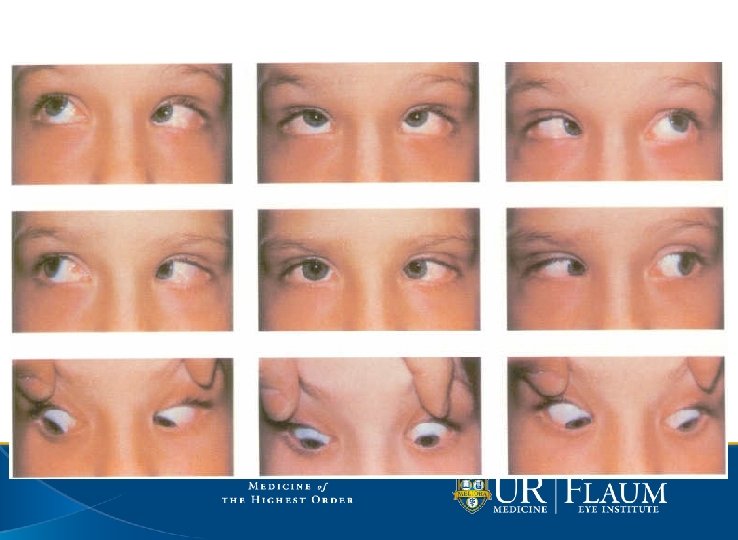
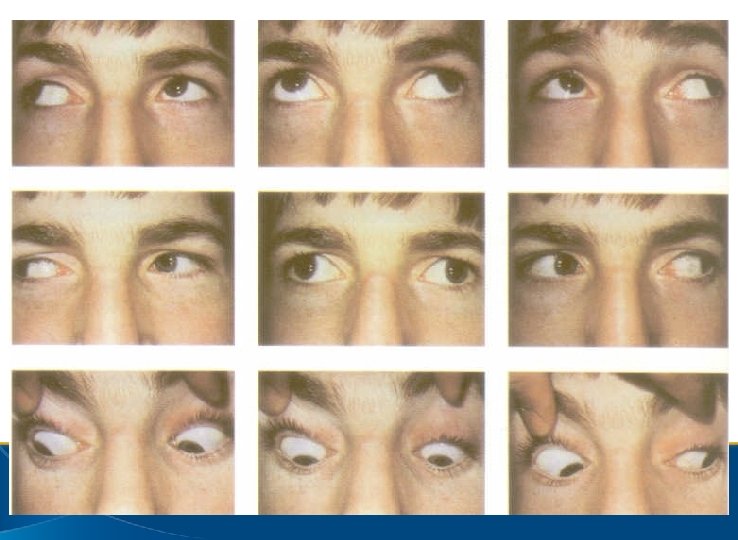
A and V Patterns Vertically incomitant horizontal strabismus. V pattern is more divergent in upgaze (more convergent in downgaze), and associated with IOOA. A pattern is more convergent in upgaze (more divergent in downgaze), and associated with SOOA. Can have A or V pattern ET or XT. Also, Y, l, X or diamond patterns.
A and V Patterns About 20% of strab cases. A pattern significant if 10 D difference in up and down, V pattern if 15 D difference. Usually from oblique dysfunction. Can be MR/LR dysfunction- LROA in up/ MROA in down causes V pattern. Can be SR/IR dysfunction- lack of tertiary adduction (V with SR, A with IR)
A and V Patterns Can also be seen in craniofacial syndromes • Apert and Crouzon syndromes typically have large V patterns. • Thought to be secondary to orbital extorsion. • Correct strabismus after skull/face surgery.
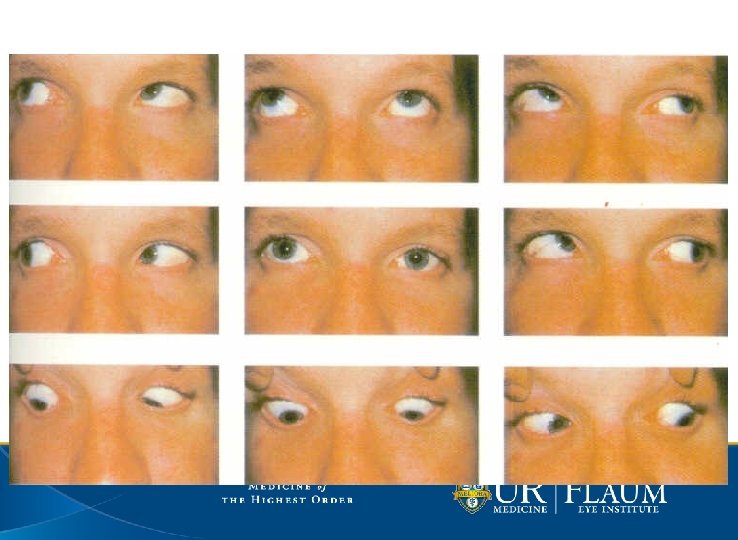
A and V Patterns When looking at gaze pictures: • What is alignment in primary (ET/XT)? • Is there over-elevation/depression in adduction? • Is there more divergence/convergence in up or down gaze? • Then name it: • A/V pattern ET/XT with/without SO/IO OA.
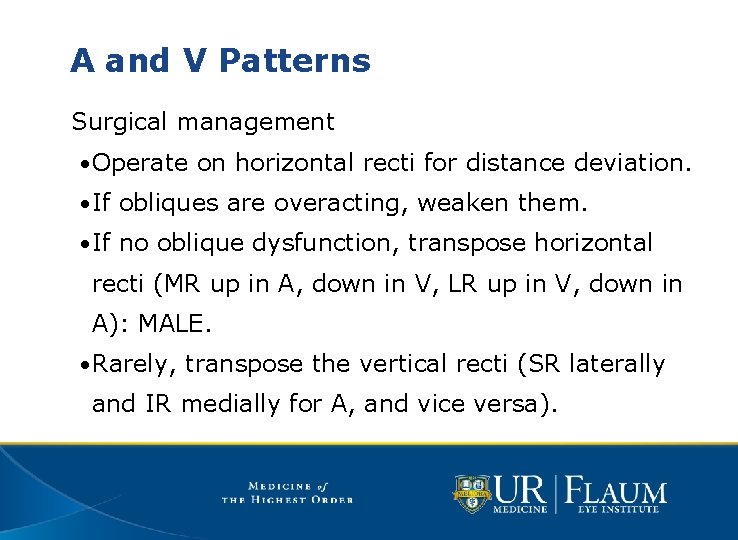
A and V Patterns Surgical management • Operate on horizontal recti for distance deviation. • If obliques are overacting, weaken them. • If no oblique dysfunction, transpose horizontal recti (MR up in A, down in V, LR up in V, down in A): MALE. • Rarely, transpose the vertical recti (SR laterally and IR medially for A, and vice versa).
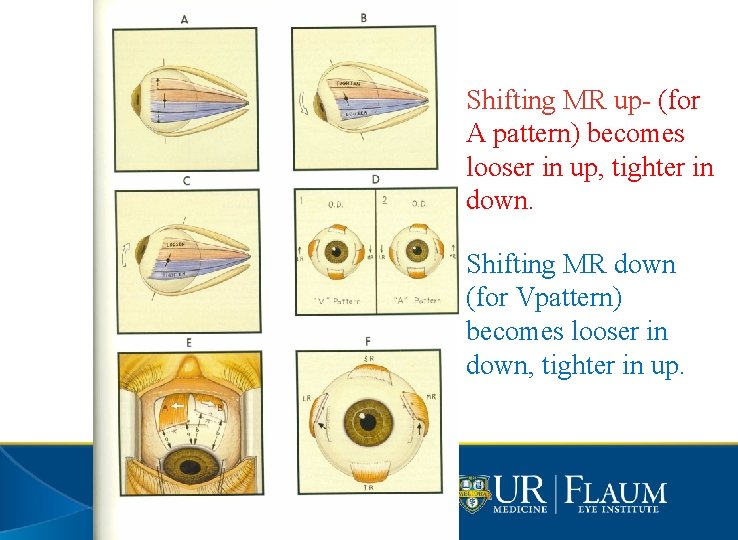
Shifting MR up- (for A pattern) becomes looser in up, tighter in down. Shifting MR down (for Vpattern) becomes looser in down, tighter in up.
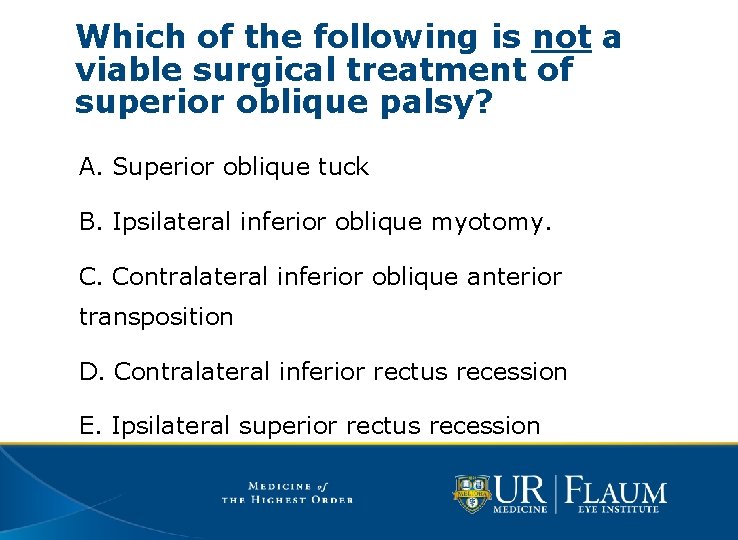
Which of the following is not a viable surgical treatment of superior oblique palsy? A. Superior oblique tuck B. Ipsilateral inferior oblique myotomy. C. Contralateral inferior oblique anterior transposition D. Contralateral inferior rectus recession E. Ipsilateral superior rectus recession
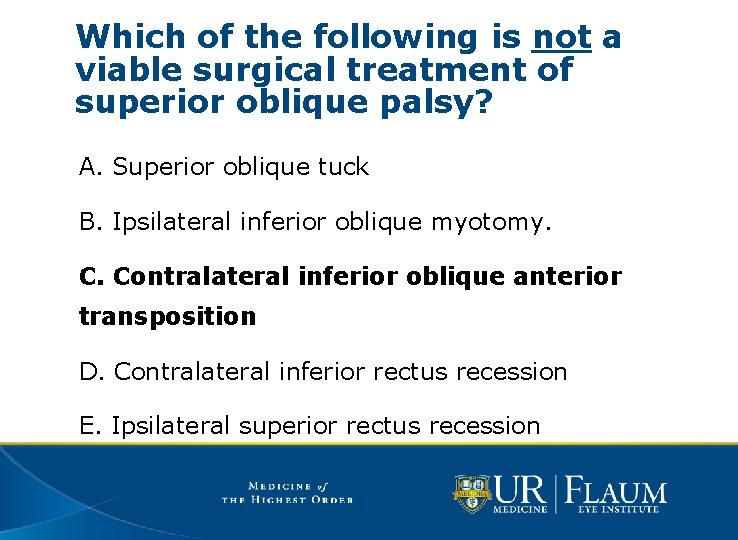
Which of the following is not a viable surgical treatment of superior oblique palsy? A. Superior oblique tuck B. Ipsilateral inferior oblique myotomy. C. Contralateral inferior oblique anterior transposition D. Contralateral inferior rectus recession E. Ipsilateral superior rectus recession
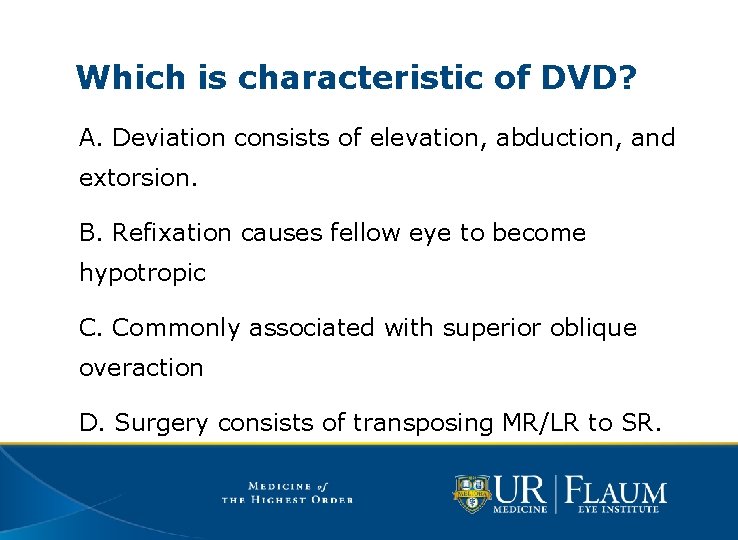
Which is characteristic of DVD? A. Deviation consists of elevation, abduction, and extorsion. B. Refixation causes fellow eye to become hypotropic C. Commonly associated with superior oblique overaction D. Surgery consists of transposing MR/LR to SR.
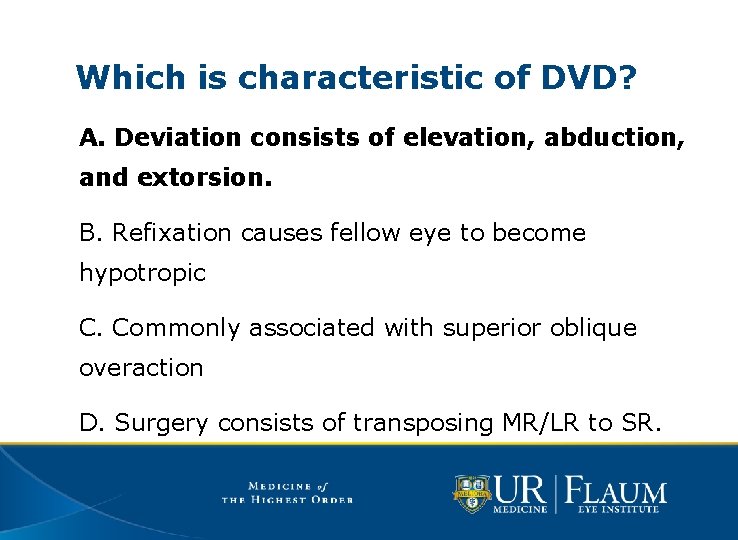
Which is characteristic of DVD? A. Deviation consists of elevation, abduction, and extorsion. B. Refixation causes fellow eye to become hypotropic C. Commonly associated with superior oblique overaction D. Surgery consists of transposing MR/LR to SR.
Which is characteristic of Brown’s syndrome? A. Hypertropia of affected eye in primary gaze. B. Treatment by Harada-Ito procedure. C. Face turn towards affected eye (e. g. R face turn for R Brown’s) D. Limitation of elevation in adduction with positive forced duction.
Which is characteristic of Brown’s syndrome? A. Hypertropia of affected eye in primary gaze. B. Treatment by Harada-Ito procedure. C. Face turn towards affected eye (e. g. R face turn for R Brown’s) D. Limitation of elevation in adduction with positive forced duction.
Which is not correct? A. V-pattern XT can be associated with inferior oblique overaction. B. Craniofacial syndromes are associated with vertically incomitant horizontal strabismus C. A-pattern ET can be treated with bilateral medial rectus recessions, infraplaced. D. Abnormal insertions of the vertical recti can cause A or V patterns.
Which is not correct? A. V-pattern XT can be associated with inferior oblique overaction. B. Craniofacial syndromes are associated with vertically incomitant horizontal strabismus C. A-pattern ET can be treated with bilateral medial rectus recessions, infraplaced. D. Abnormal insertions of the vertical recti can cause A or V patterns.
51
- Slides: 51