Vermont Dental Hygienists Association OSHA Review 2015 Trisha












- Slides: 72

Vermont Dental Hygienists’ Association OSHA Review 2015 Trisha A. Cloutier, CDA, RDH, BS, MA trisha. cloutier@bristolcc. edu Bristol Community College, Fall River MA
Introduction • OSHA Occupational Safety and Health Administration www. osha. gov • OSAP Organization for Safety and Asepsis Procedures www. osap. org • CDC Centers for Disease Control www. cdc. gov
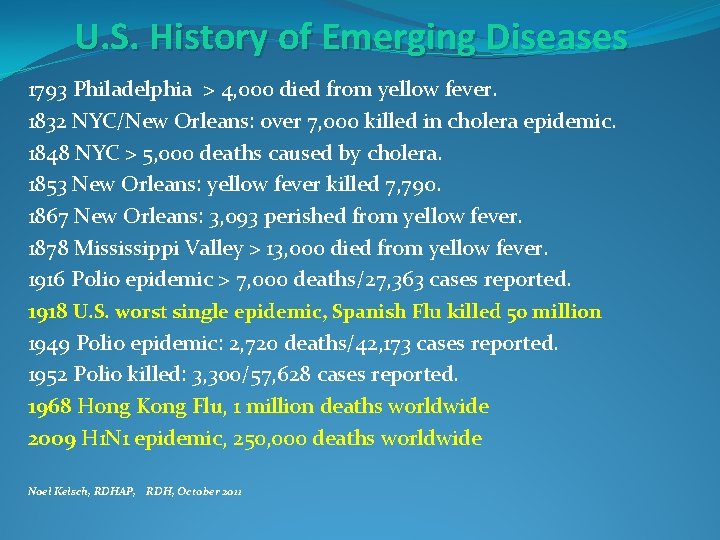
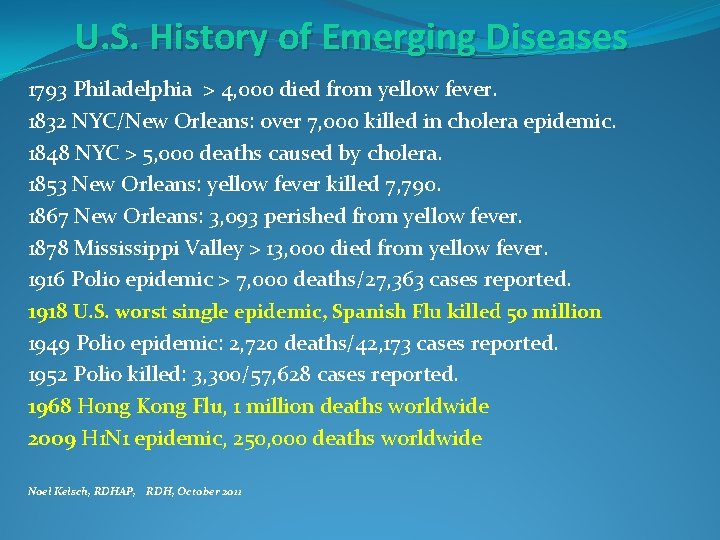
U. S. History of Emerging Diseases 1793 Philadelphia > 4, 000 died from yellow fever. 1832 NYC/New Orleans: over 7, 000 killed in cholera epidemic. 1848 NYC > 5, 000 deaths caused by cholera. 1853 New Orleans: yellow fever killed 7, 790. 1867 New Orleans: 3, 093 perished from yellow fever. 1878 Mississippi Valley > 13, 000 died from yellow fever. 1916 Polio epidemic > 7, 000 deaths/27, 363 cases reported. 1918 U. S. worst single epidemic, Spanish Flu killed 50 million 1949 Polio epidemic: 2, 720 deaths/42, 173 cases reported. 1952 Polio killed: 3, 300/57, 628 cases reported. 1968 Hong Kong Flu, 1 million deaths worldwide 2009 H 1 N 1 epidemic, 250, 000 deaths worldwide Noel Kelsch, RDHAP, RDH, October 2011
Evolutionary Biology “Microbes on Parade”, Reynolds Headliners “An Old Bug Has Learned Lethal New Tricks”, Ricks, Newsday, 2007 “Deadly Staph: Drug-resistant germ may kill more people then AIDS”, Stein, Washington Post, 2007
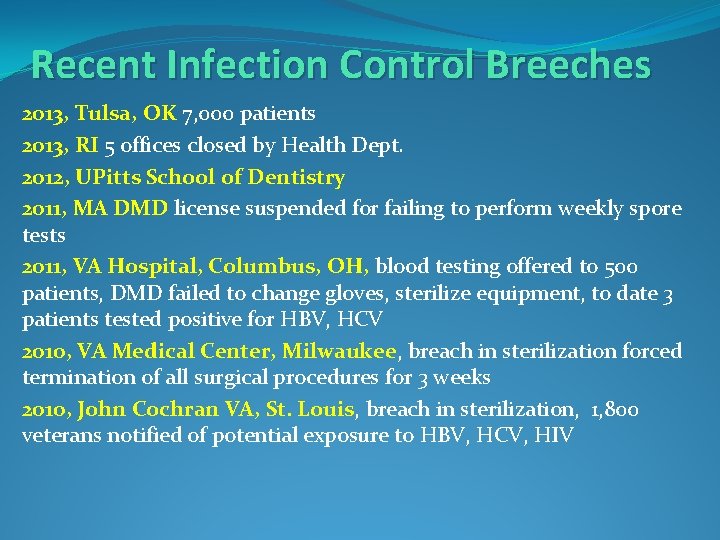
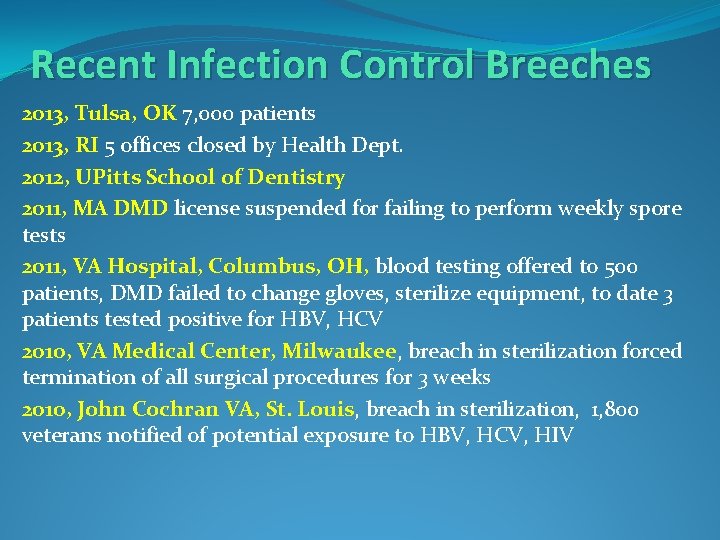
Recent Infection Control Breeches 2013, Tulsa, OK 7, 000 patients 2013, RI 5 offices closed by Health Dept. 2012, UPitts School of Dentistry 2011, MA DMD license suspended for failing to perform weekly spore tests 2011, VA Hospital, Columbus, OH, blood testing offered to 500 patients, DMD failed to change gloves, sterilize equipment, to date 3 patients tested positive for HBV, HCV 2010, VA Medical Center, Milwaukee, breach in sterilization forced termination of all surgical procedures for 3 weeks 2010, John Cochran VA, St. Louis, breach in sterilization, 1, 800 veterans notified of potential exposure to HBV, HCV, HIV
CDC defines Cross Contamination: “As the act of spreading bacteria and viruses from one surface to another. Blood-borne viruses can live on objects for up to a week. Spread can occur when surfaces are not disinfected immediately or if equipment is not cleaned and sterilized between patients. ”
Importance of Infection Prevention Pathogen Source Mode of transmission Portal of entry/exit Susceptible host

History of Public Health • • Phase 1 (1849 -1900) Elimination /control of diseases Phase 2 (1880 -1930) Prevention born with immunization Phase 3 (1930 -1975) More complex medical treatment Phase 4 (1975 - present) Age of technology but limited availability to all members of public

1. Take Action to Stay Healthy • Personnel Health Elements • Immunization • Work Restrictions • Hand Hygiene • Contact Dermatitis and Latex Allergy • Hand Maintenance
Personnel Health Elements 1. 2. 3. 4. 5. Good nutrition Sleep Exercise Meditation /prayer Vaccinate
Ten Great Public Health Achievements United States, 1900 -1999 Vaccination Motor-vehicle safety Safer workplaces Control of infectious diseases Decline in deaths from coronary heart disease and stroke 6. Safer and healthier foods 7. Healthier mothers and babies 8. Family planning 9. Fluoridation of drinking water 10. Recognition of tobacco use as a health hazard 1. 2. 3. 4. 5.

Immunization “Healthcare Personal Vaccination Recommendations” www. immunize. org HBV Influenza MMR Varicella (chicken pox) TDAP MCV 4 TRAVEL
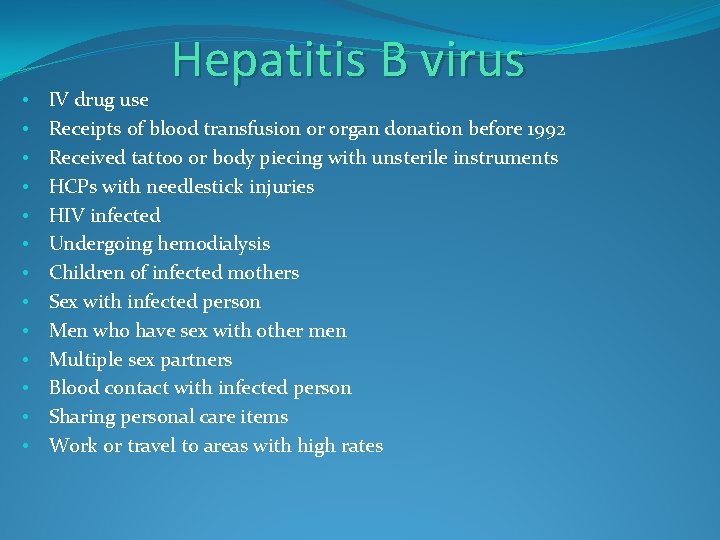
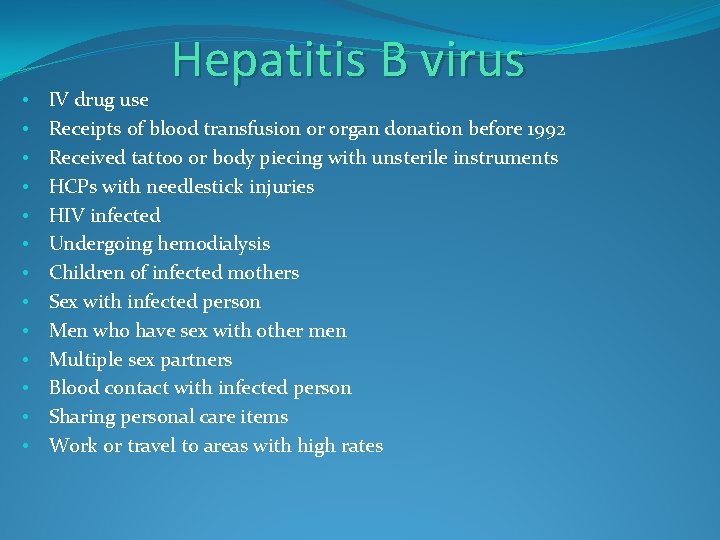
• • • • Hepatitis B virus IV drug use Receipts of blood transfusion or organ donation before 1992 Received tattoo or body piecing with unsterile instruments HCPs with needlestick injuries HIV infected Undergoing hemodialysis Children of infected mothers Sex with infected person Men who have sex with other men Multiple sex partners Blood contact with infected person Sharing personal care items Work or travel to areas with high rates
Hepatitis B • Immunization for DHCP 3 doses, 1, 1 mos. , 1, 6 mos. • Employer required to offer • May decline, Sign form • Booster • MMWR, 2012
Influzena • Who? ALL ADULTS • Why? Flu viruses spread like wildfire, difficult to avoid particularly in dental/medical offices • When? Every year -According to CDC, flu season typically ramps up during December /January, peaks February -About 2 weeks to develop immunity
MMR measles, mumps, rubella • Increase in US and other countries • Adult born after 1956 recmd one dose, unless had all 3 diseases • Not advised for pregnant women • Association between Autistic Spectrum Disorder (ASD) and MMR vaccine? • Systematic Review found 12 epidemiological studies which provided NO evidence of association between ASD and MMR vaccine

Varicella (Chickenpox) Who? 13 years of age and older who never had chickenpox • Healthcare professionals • • • People who care for/around others with weakened immune systems Teachers Child care workers Residents/staff in nursing homes/residential settings College students Inmates/staff of correctional institutions Military personnel Non-pregnant women of child-bearing age Adolescents/adults living with children International travelers When? two doses, at least 28 days apart
TDAP (Tetanus, Diphtheria, Pertussis) Who? ALL ADULTS • Tetanus bacterial infection-causes lockjaw, kills about 1 out of 5 • Pertussis (Whopping Cough) bacterial infection causes violent coughing, vomiting, and even sleep apnea in adults Kills infants, First case in years, coming to US, Shot not effective to this strain attributed to over prescription of antibiotics • Cold-like symptoms • Persistent hacking cough for weeks • Children/elderly-more serious or even fatal When? Get Tdap vaccine ASAP if not received Tetanus booster shot every 10 years
MCV 4 Meningococcal disease Bacterial infection of the covering of the brain and spinal cord, can be life-threatening. Who? • College students in dorms at most risk • Military recruit • Adults with damaged/no spleen • Traveling or residing in countries where common
Work Restrictions Illness or infection that can be transmitted to patients and/or staff members • Polices: • Written: (based on CDC guidelines) • http: //www. cdc. gov//Diseases. Conditions/ • Personal physician • Training of Staff

Hand Hygiene CLEAN HANDS SAVE LIVES Protect patients, protect yourself • • Candida Staphylococcus RSV Influenza Klebsiella Pseudomonas Enterococcus www. cdc. gov/handhygiene

Hand Hygiene • Nonantimicrobial • Antiseptic • Alcohol-based
To remove all transient bacteria and as many residential bacteria as possible. Performed at beginning and end of day Remove jewelry, clean nails, hands, forearms with antimicrobial agent Wet hands and wrist under cool running water Dispense antimicrobial agent to cover hands and wrist Begin with finger tips, working down each finger, keeping hands above elbow level to prevent contaminated water from running onto clean fingers for 30 seconds Rinse with cool water. Repeat for 2 minutes: Wet hand, wrist with water Dispense Antimicrobial agent Clean fingers, hands, wrist Rinse under cool water Dry thoroughly by gently patting hand, wrist with paper towels
Contact Dermatitis and Latex Allergy • Irritant Contact Dermatitis • Allergic Contact Dermatitis • Seek expert medical advice
Hand maintenance • • • Moisturizing hands Lotions/Cremes Paraffin wax Petroleum based Water based
2. Avoid Contact with Blood and Other Body Fluids • Bloodborne Pathogens • Standard Precautions • Administrative Controls • Engineering Controls • Personal Protective Equipment (PPE) • Work Practices Controls • Exposure Prevention and Post exposure Management
Bloodborne Pathogens • Disease spread through blood and other body excretions: • Hepatitis B virus (HBV) • Hepatitis C virus (HCV) • Human immunodeficiency virus (HIV) • Transmission • Percutaneous injury • Contact of mucous membrane with blood • Contact of broken skin with blood • Bites • Eyes

Infectious Disease Update • Tuberculosis • Human Immunodeficiency Virus (HIV) • Hepatitis C

Tuberculosis (TB) Bacterial infection caused by Mycobacterium tuberculosis 2014 9, 412 new cases in US, decrease of 2. 2% from 2013 • Attacks lungs… • Lives in people • Mode of transmission - Airborne • HCP require TB Skin test upon hire www. cdc. gov/mmwr March 2015
• Patients w/ HIV (weak immune system) • IV drug users • Residents/employees of shared habitation settings • Healthcare professionals • Immigrants • Medically underserved

Latent tuberculosis (Non infectious) • • No symptoms Remain inactive, but alive, can become active but may not Active tuberculosis (Infectious) • • • Affects lungs Coughing often only indication of infection Cough lasting three or more weeks Bloody sputum Weight loss (greater than 10 lbs) Fatigue/excessive tiredness, fever, night sweats, chills, loss of appetite, pain when breathing or coughing
Diagnosis • Physical exam/clinical • • symptoms Chest radiograph Diagnostic microbiological tests/sputum culture Patients w/ active TB should be treated in hospital Must have negative test to treat
Human Immunodeficiency Virus (HIV) 1980 – ID first case, “AIDS” 1983 – Discovery of AIDS 1981 -2012: Total estimated U. S. cases: 1, 218, 400 Total estimated deaths: 658, 507 • HIV - CDC: > than 1 million in US currently infected • 1 in 8 not diagnosed, let alone reported • Minority Americans represent 78% of new cases • Women represent 20% of new cases • Approx. 300 children born with virus in US per year www. cdc. gov/hiv/statistics/surveillance
Only 57 documented (130 possible) occupational infections in the healthcare professions in US • 48 from needle sticks • 8 from splashes to face • 1 unknown • Low risk Why worry? • No cure – fatal • No vaccine • Strains resistant • Therapy expensive Ora. Sure Technologies presents Ora. Quick ® First FDA-approved oral swab in-home test for HIV Molanari, 2011
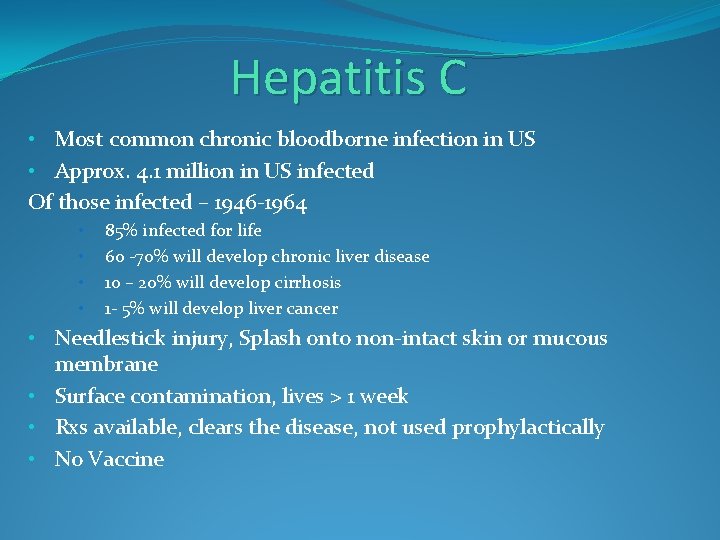
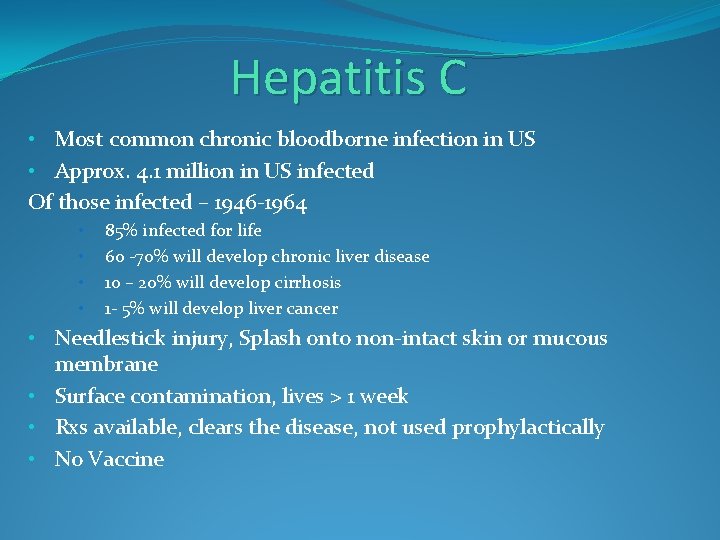
Hepatitis C • Most common chronic bloodborne infection in US • Approx. 4. 1 million in US infected Of those infected – 1946 -1964 • • 85% infected for life 60 -70% will develop chronic liver disease 10 – 20% will develop cirrhosis 1 - 5% will develop liver cancer • Needlestick injury, Splash onto non-intact skin or mucous membrane • Surface contamination, lives > 1 week • Rxs available, clears the disease, not used prophylactically • No Vaccine
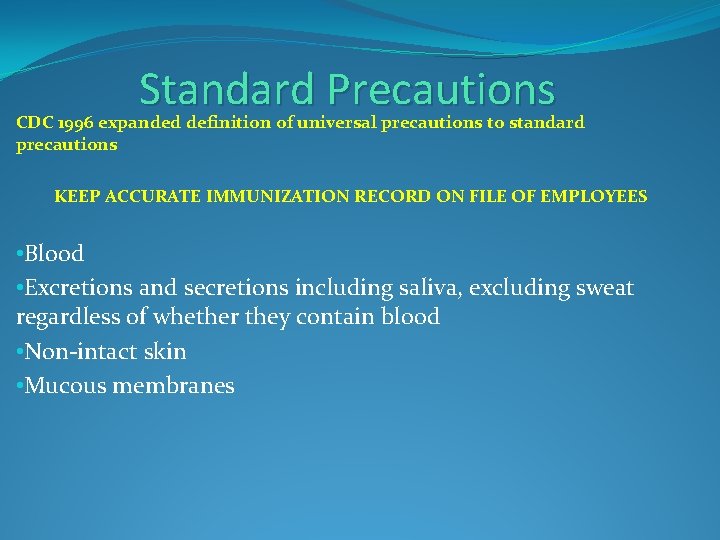
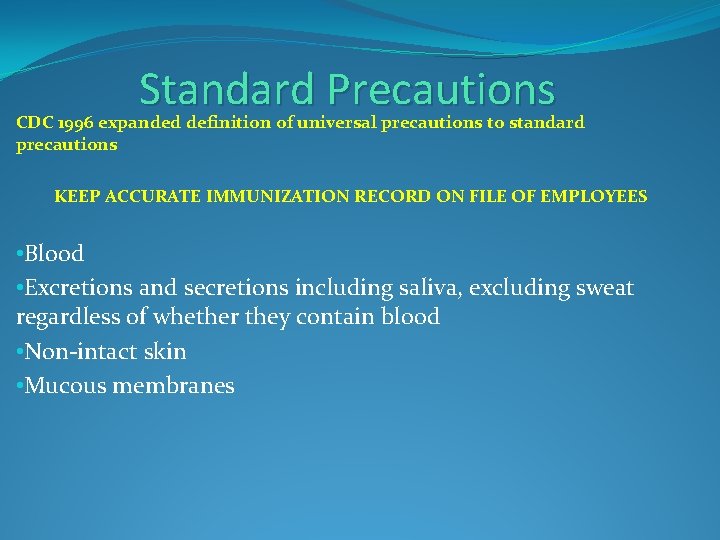
Standard Precautions CDC 1996 expanded definition of universal precautions to standard precautions KEEP ACCURATE IMMUNIZATION RECORD ON FILE OF EMPLOYEES • Blood • Excretions and secretions including saliva, excluding sweat regardless of whether they contain blood • Non-intact skin • Mucous membranes
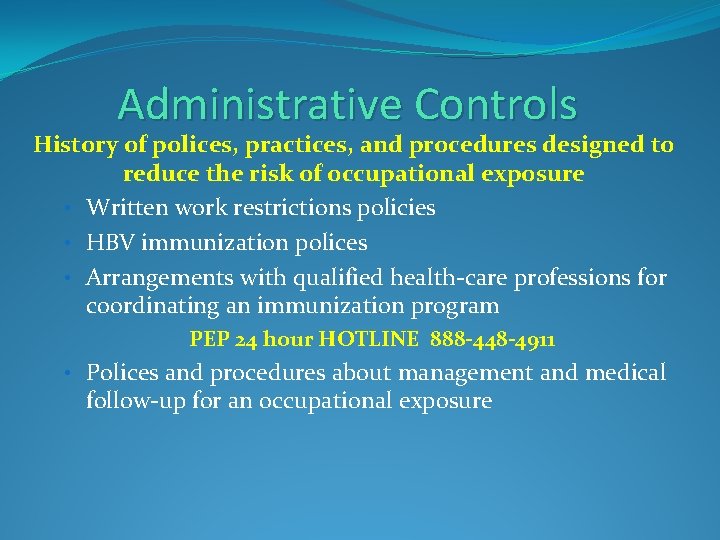
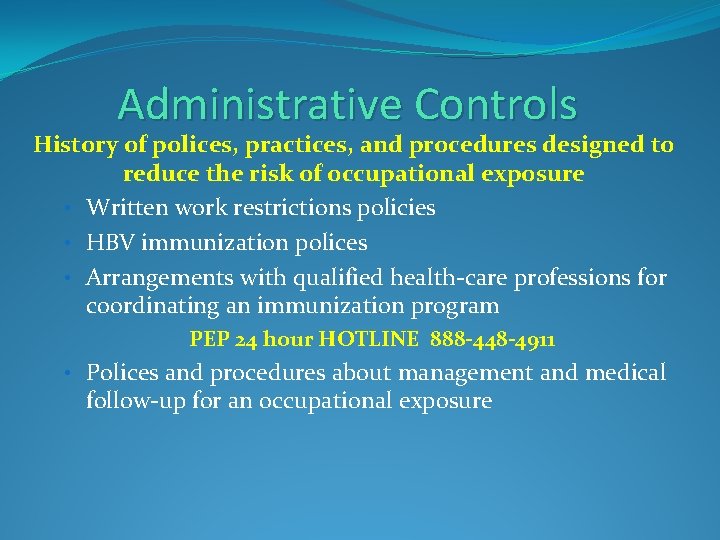
Administrative Controls History of polices, practices, and procedures designed to reduce the risk of occupational exposure • Written work restrictions policies • HBV immunization polices • Arrangements with qualified health-care professions for coordinating an immunization program PEP 24 hour HOTLINE 888 -448 -4911 • Polices and procedures about management and medical follow-up for an occupational exposure
Wash needlesticks and cuts with soap and water Flush splashes to the nose, mouth, or skin with water Irrigate eyes with clean water, saline, or sterile irrigants Do NOT apply caustic agents or inject antiseptics or disinfectants into the wound • Report the incident • Immediately seek medical treatment. • •
Written Certification Employer shall verify that each affected employee has received and understood the required training through a written certification that contains the name of each employee trained, the date(s) of training, and the subject of the certification. Hazard Communication-OSHA’s Hazard Communication Standard is based on the concept that employees have both the need and the “right to know “ the hazards and identities the chemicals they are exposed to when working. www. osha. gov/SLTC/dentistry/index. html

Engineering Controls to reduce/eliminate hazards to prevent exposure • Examples include: • Safety devices • Retractable scalpels • Self-sheathing needles • Anesthetic syringes and needles with engineered safety features • Sharps disposal containers • Cassettes • PPE • HVE
Personal Protective Equipment (PPE) All DHCP in direct patient contact will wear the appropriate PPE appropriate for the tasks performed • • Gloves Face masks Protective eyewear Clothing
Face masks CDC 2003 Guidelines for Infection Control in Dental Health Care Settings “Wear a surgical mask and eye protection with solid side shields or a face shield to protect mucous membranes of the eyes, nose, and mouth during procedures likely to generate splashing or spattering of blood and other body fluids. ”
Face masks-specific features Does not come into contact with nostrils or lips Has high bacterial filtration efficiency (BFE) rate (95%) Fits snugly around entire periphery Does not cause fogging of eyewear Made of a fabric that does not irritate skin or induce an allergic reaction • Comprised of material that does not collapse when worn or wet • Easy to put on and remove • Change for every patient (60 mins) • • •
• • • Protective Clothing Must be properly cleaned, laundered, repaired, disposed of at no cost to employees Must be removed when leaving the treatment area or upon visible contamination Cleaned by a professional service or cleaned in-house Must not be taken home Consider disposable gowns
Work Practices Controls Behavior based. Changing the way someone performs a task, to remove or lessen the exposure, as opposed to the use of a physical device, such as an engineering control.
Handling Emergencies • Eye injury, quick action can prevent a permanent disability • Emergency eyewashes should be placed in ALL hazardous areas • First-aid instructions should be posted close to potential danger spots • Employees must know where closest eyewash station is and how to get there with restricted vision
Amalgam/Mercury protocol Amalgam Separator Installation and Maintenance Requirements www. mercvt. org/dental/amalgsepreq. htm • Vermont - January 2007 Dental offices must install amalgam separator • List of approved amalgam separators • Environmental Assistance Office at 800 -974 -9559
Safety Data Sheets (formerly known MSDSs) June 1, 2015, Hazard Communication Standard will require new SDSs to be in uniformat, include section numbers, headings, associated info…etc. www. osha. gov/Publications/Haz. Comm_Quick. Card_Safety. Data. html Employee training www. osha. gov/Publications/OSHA 3636. pdf
Control of Nitrous Oxide in Dental Operatories • System maintenance • Ventilation • Work Practices www. cdc. gov/niosh/docs/hazardcontrol/hc 3. html
Exposure Prevention and Postexposure Management Exposure Determination OSHA states - tasks in dental office be evaluated/classified by categories of tasks Category I: that involve exposure to blood, body fluids, tissues Category II: that involve no exposure to blood, body fluids, tissues, but may require performing unplanned Category I tasks Category III: that involve no exposure to blood, body fluids, tissues
3. Make Objects Safe for Use • Classification of Patient-Care Items • Environmental Surfaces • Instrument Processing • Sterilization Monitoring

Classification of Patient-Care Items • Critical Penetrates soft tissue, contacts bone, enters bloodstream Dental Hygiene instruments, dental burs, needles • Semicritical Contacts mucous membranes, nonintact skin, does not penetrate soft tissue, contact bone, or enter bloodstream Dental mirror, impression trays, *handpieces • Noncritical Contacts intact skin Radiograph head, blood pressure cuff
Environmental Surfaces • Many products available • Consider surface barriers for difficult to clean areas • Evaluate properties of surface cleaners and disinfectants before purchase • Surface cleaning can remove > 95% surface debris • Certain products useful both cleaners and disinfects • Surface wipes reduce aerosolized chemicals • Choices: no single available product is the only one to use
Instrument Processing • Dental handpieces considered a semicritical item, should always be heat-sterilized between uses • Ultrasonic use • Holding “baths”, transport, reduce drying • No scrubbing!!! • Protective eyewear must be worn for all clean-up procedures
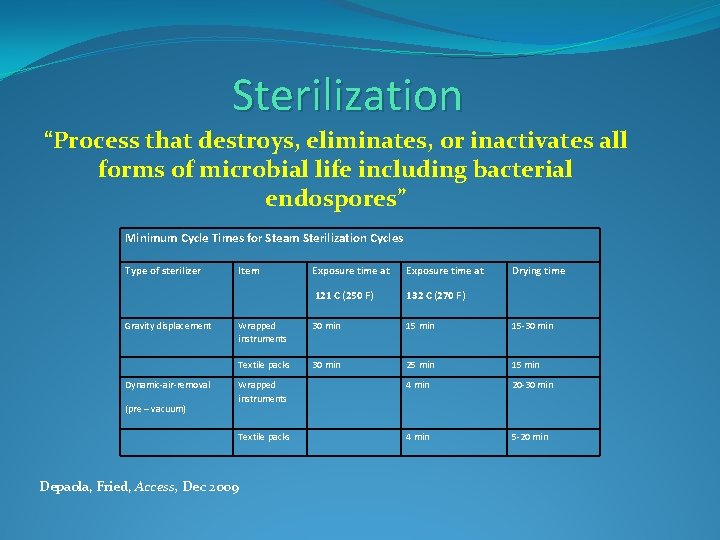
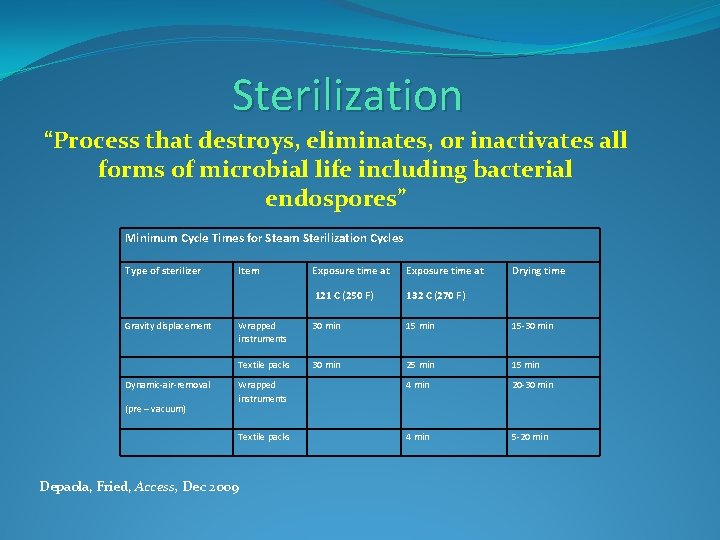
Sterilization “Process that destroys, eliminates, or inactivates all forms of microbial life including bacterial endospores” Minimum Cycle Times for Steam Sterilization Cycles Type of sterilizer Gravity displacement Dynamic-air-removal (pre – vacuum) Item Exposure time at 121 C (250 F) 132 C (270 F) Wrapped instruments 30 min 15 -30 min Textile packs 30 min 25 min 15 min Wrapped instruments 4 min 20 -30 min Textile packs 4 min 5 -20 min Depaola, Fried, Access, Dec 2009 Drying time
Sterilization Monitoring Autoclave Bags Indicator Tape Heat indicators Biological Monitoring
• • • Improper timing Wrong temperature Incorrect sterilization method for item Unit malfunction Improper packaging Overloading Inappropriate operation Incorrect maintenance of sterilizer Inadequate cleaning of instruments Temperature exceeding temperature-pressure relationship Ineffective or nonexistent monitoring process
www. crosstex. com • Con. Firm Mail-in with results www. hufriedy. com Has Class 4 internal/external multi-variable indicators when ALL criteria are met: • Time • Temperature • Steam
Remember: • Store cool, dry place. Heat/moisture can compromise indicator, adhesion, materials. • Companies have instructions, videos to help you. • Do not overload. Most units load vertically. If load horizontally, make sure do not touch so maximum amount of exposure. • Training must occur for every staff member. • Do not remove until processed/dry. • Shelf life is considered “event related”, check each bag for compromise before use. • Label date, cycle load, sterilizer-write on plastic side not paper
4. Limit Contamination • Environmental Infection Control • Medical Waste • Dental Unit Waterlines • Boil Water Advisory
Environmental Infection Control US Environmental Protection Agency (EPA) www. epa. gov/epahome/state. htm Vermont Department of Environmental Conservation (VDEC) www. anr. state. vt. us/dec/ead/index. htm Risk of inspection, reporting , disgruntled worker/patient
Medical Waste • Check your Local Authority • Needles, blood soaked gauze, infectious waste (teeth) must be placed in closable, leakproof containers built to contain all contents during handling, storing, transporting or shipping and be appropriately labeled and color-coded.
Dental Unit Waterlines • Flush air, water, suction lines for two minutes each at the beginning of day and for 20 to 30 seconds between patients. Flush the air/water syringe into the sink to remove debris and stagnant water from lines. • Flush lines using cleaning agents Garland, Dimensions, Sept. 2012, The Battle against Biofilms
Boil Water Advisory Once an advisory has been issued follow local guidelines http: //emergency. cdc. gov/disasters/floods/cleanupwater. asp http: //www. cdc. gov/healthywater/emergency/flood/standing. html http: //emergency. cdc. gov/disasters/mold/reenter. asp
Special Considerations • Dental Radiology • Parenteral Medications • Oral Surgery • Biopsy Specimen • Extracted Teeth • Dental Laboratory
Dental Radiology • Use PPE and maintain asepsis when exposing, processing radiographs • Use heat tolerant or disposable intraoral devices • Use FDA cleared barriers for digital radiography sensors
Parenteral Medications Drugs that are given by injection or used in an IV • Single Dose vials: Preferred and use whenever possible • Multi-Dose vials: Clean access diaphragm with 70% alcohol before inserting device into vial Use sterile device to access multi-dose vial Keep multi-dose away from immediate patient treatment area to prevent inadvertent contamination by spray or splatter
Oral Surgery • Perform surgical hand asepsis using antimicrobial product before donning sterile surgeon's gloves • Use sterile saline/sterile water as coolant/irrigants when performing surgical procedures
Biopsy Specimen • During transport, place biopsy specimens in sturdy, leak-proof container with Biohazard symbol • If biopsy specimen container is visibly contaminated, clean, disinfect outside of a container or place in an impervious bag labeled with Biohazard symbol
Extracted Teeth • Extracted teeth are infectious, considered regulated medical waste • Do not incinerate extracted teeth containing amalgam Mercury vapor • Teeth transported to educational institutions/laboratories are to be cleaned, disinfected, placed in leak proof container, labeled with biohazard label • Patient has right to their extracted teeth OSHA regulations no longer apply once teeth are extracted Teeth need to be cleaned, disinfected before given to patient
Dental Laboratory • Clean, disinfect, label with biohazard symbol on ALL laboratory cases sent offsite • Use PPE when handling items received in laboratory • Clean, disinfect, rinse ALL items before handled in laboratory • Use approved disinfection procedures for products as recommended by manufacturer • Clean/heat sterilize items used in mouth (metal impression trays, etc)
Program Evaluation • Review YOUR Infection Control Program • Conduct a Work Practice Observation on Wearing PPE • Conduct a Work Practice Observation on Using Alcohol Hand Rub (gel)/ Handwashing • Review Immunization Records • Screen/Evaluate New Safety Devices • Review Occupational Exposures • HIPAA
 Cdha jobs
Cdha jobs Vermont dental hygiene association
Vermont dental hygiene association Vermont association of criminal defense lawyers
Vermont association of criminal defense lawyers Trisha eardley
Trisha eardley Dr pachiano
Dr pachiano Trisha patel orlando
Trisha patel orlando Trisha carroll
Trisha carroll Trisha paul
Trisha paul Dr trisha pachiano
Dr trisha pachiano Trisha paul
Trisha paul Iso awareness training for employees
Iso awareness training for employees Management review iso 9001 version 2015 muster
Management review iso 9001 version 2015 muster Becker cpa review 2015
Becker cpa review 2015 Maine dental hygiene association
Maine dental hygiene association Astdd
Astdd Montana dental association
Montana dental association Dtabc
Dtabc Definition of dental composite
Definition of dental composite Rule 4500
Rule 4500 Augusta is the capital of what state
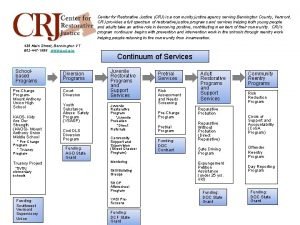
Augusta is the capital of what state Crj bennington vt
Crj bennington vt American marten vermont
American marten vermont Romeo and juliet law vermont
Romeo and juliet law vermont Vermont sheep and goat
Vermont sheep and goat Vermont department of health
Vermont department of health Child development clinic vermont
Child development clinic vermont Medical examiner vs coroner
Medical examiner vs coroner Vermont doh
Vermont doh Central vermont railroad
Central vermont railroad Vermont sheep and goat
Vermont sheep and goat Hans kastensmith
Hans kastensmith Vermont drought monitor
Vermont drought monitor Vermont yankee v nrdc
Vermont yankee v nrdc Vermont yankee nuclear power corp. v. nrdc
Vermont yankee nuclear power corp. v. nrdc Vermont pbis
Vermont pbis Ahec vermont
Ahec vermont Does green mountain care cover dental
Does green mountain care cover dental Vermont blueprint for health
Vermont blueprint for health Kellar
Kellar Vt ems protocols
Vt ems protocols What two sites did the narrator go back to see at devon
What two sites did the narrator go back to see at devon Chapter review motion part a vocabulary review answer key
Chapter review motion part a vocabulary review answer key Writ of certiorari ap gov example
Writ of certiorari ap gov example Nader amin-salehi
Nader amin-salehi Systematic review definition
Systematic review definition Narrative review vs systematic review
Narrative review vs systematic review Osha hot work standard 1910
Osha hot work standard 1910 Osha 29 cfr 1910
Osha 29 cfr 1910 Cal osha fire extinguisher training
Cal osha fire extinguisher training Osha z tables
Osha z tables 29 cfr 1910 subpart z
29 cfr 1910 subpart z Power tools safety training ppt
Power tools safety training ppt Theories of accidents osha
Theories of accidents osha Objectives of occupational health
Objectives of occupational health 29 cfr 1926 subpart m
29 cfr 1926 subpart m 1926 subpart v
1926 subpart v Double-cleated ladder
Double-cleated ladder Osha telecommunications standards
Osha telecommunications standards What are the three phases of site characterization
What are the three phases of site characterization Espacios confinados osha
Espacios confinados osha Cfr
Cfr Osha safety pyramid
Osha safety pyramid Osha 300 puerto rico
Osha 300 puerto rico Osha 1910 forklift
Osha 1910 forklift Osha 1910-134
Osha 1910-134 Part 1926 subpart j of osha standards
Part 1926 subpart j of osha standards Osha form 33
Osha form 33 1910 134
1910 134 29cfr1926.1101
29cfr1926.1101 Osha history
Osha history State 3 objectives of osha 1994 act 514
State 3 objectives of osha 1994 act 514 Www osha gov
Www osha gov Osha heat work/rest chart
Osha heat work/rest chart