Verifying NG Tube Placement in the Neonate According
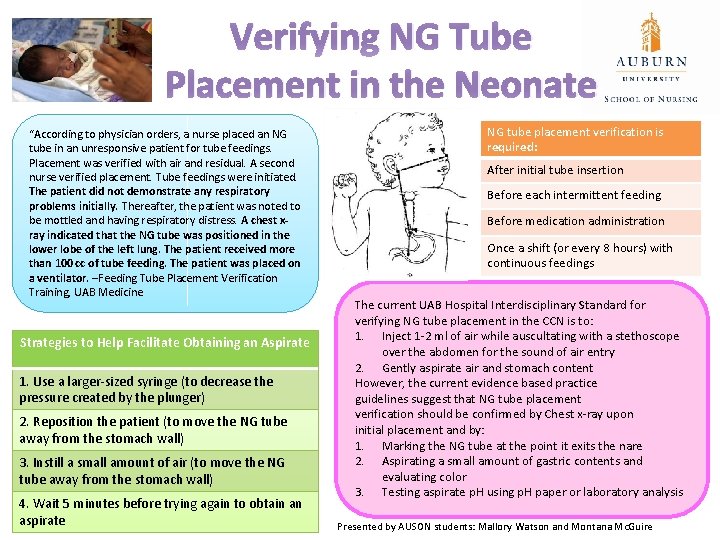
Verifying NG Tube Placement in the Neonate “According to physician orders, a nurse placed an NG tube in an unresponsive patient for tube feedings. Placement was verified with air and residual. A second nurse verified placement. Tube feedings were initiated. The patient did not demonstrate any respiratory problems initially. Thereafter, the patient was noted to be mottled and having respiratory distress. A chest xray indicated that the NG tube was positioned in the lower lobe of the left lung. The patient received more than 100 cc of tube feeding. The patient was placed on a ventilator. –Feeding Tube Placement Verification Training, UAB Medicine Strategies to Help Facilitate Obtaining an Aspirate 1. Use a larger-sized syringe (to decrease the pressure created by the plunger) 2. Reposition the patient (to move the NG tube away from the stomach wall) 3. Instill a small amount of air (to move the NG tube away from the stomach wall) 4. Wait 5 minutes before trying again to obtain an aspirate NG tube placement verification is required: After initial tube insertion Before each intermittent feeding Before medication administration Once a shift (or every 8 hours) with continuous feedings The current UAB Hospital Interdisciplinary Standard for verifying NG tube placement in the CCN is to: 1. Inject 1 -2 ml of air while auscultating with a stethoscope over the abdomen for the sound of air entry 2. Gently aspirate air and stomach content However, the current evidence based practice guidelines suggest that NG tube placement verification should be confirmed by Chest x-ray upon initial placement and by: 1. Marking the NG tube at the point it exits the nare 2. Aspirating a small amount of gastric contents and evaluating color 3. Testing aspirate p. H using p. H paper or laboratory analysis Presented by AUSON students: Mallory Watson and Montana Mc. Guire
- Slides: 1