VENTILATION OF THE LUNGS Minute respiratory volume is


- Slides: 20
VENTILATION OF THE LUNGS Minute respiratory volume is the total amount of air that moves into respiratory passages each minute n =tidal volume ×respiratory rate(RR). n =500× 12=6 L/ min. n
VENTILATION OF THE LUNGS Alveolar ventilation represents the volume of fresh gas that reaches the alveoli each minute (available for gas exchange), of each 500 ml inhaled tidal volume, 150 ml remain behind in the space which fills the conducting zone between the mouth and nose and respiratory bronchioles, where no exchange of gas takes place(anatomical dead space) n Alveolar ventilation =RR×(500150)=4. 2 L/min. n
Dead Space n It is the volume of air which does not undergo gas exchange with pulmonary capillaries.
Dead Space n n n Types of dead space: 1 -Anatomical dead space(conducting zone) 2 -Alveolar dead space(non functioning alveoli) due to absent or poor blood through pulmonary capillaries, these alveoli are considered as alveolar dead space. 3 -Alveolar dead space and anatomical dead space=physiological dead space. In healthy persons anatomical dead space =physiological dead space because all alveoli when ventilated well and perfused well with blood should function well.
Regional differences in ventilation n Ventilation increases slowly from top to bottom of the lung due to regional changes in the –ve ipp, it is less negative at the base than the apex because of the weight of the lung.
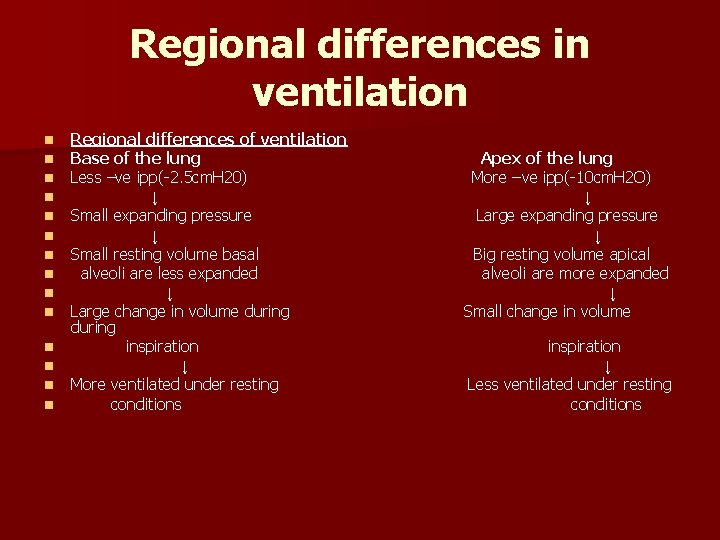
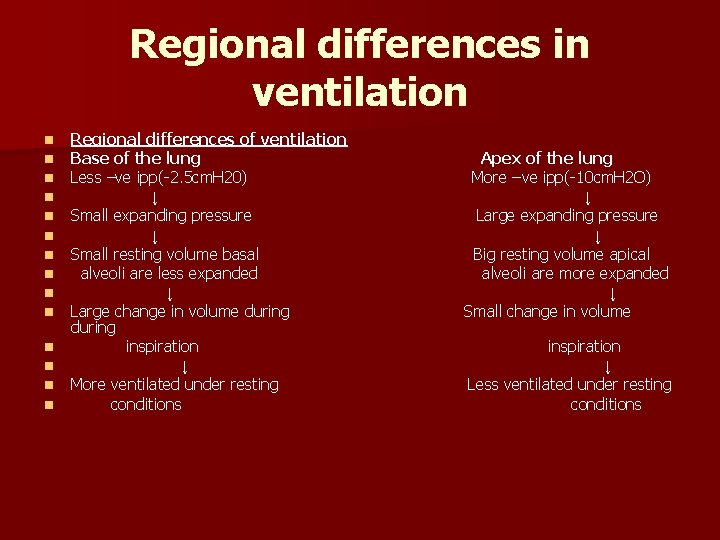
Regional differences in ventilation n n n Regional differences of ventilation Base of the lung Less –ve ipp(-2. 5 cm. H 20) ↓ Small expanding pressure ↓ Small resting volume basal alveoli are less expanded ↓ Large change in volume during inspiration ↓ More ventilated under resting conditions Apex of the lung More – ve ipp(-10 cm. H 2 O) ↓ Large expanding pressure ↓ Big resting volume apical alveoli are more expanded ↓ Small change in volume inspiration ↓ Less ventilated under resting conditions

DIFFUSION n After the alveoli are ventilated with fresh air, the next step in the respiratory process is the transfer of gas across the blood gas barrier (diffusion).
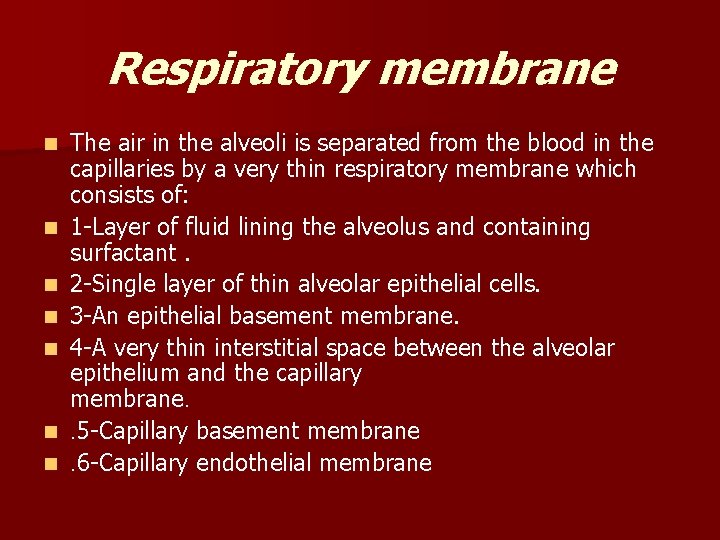
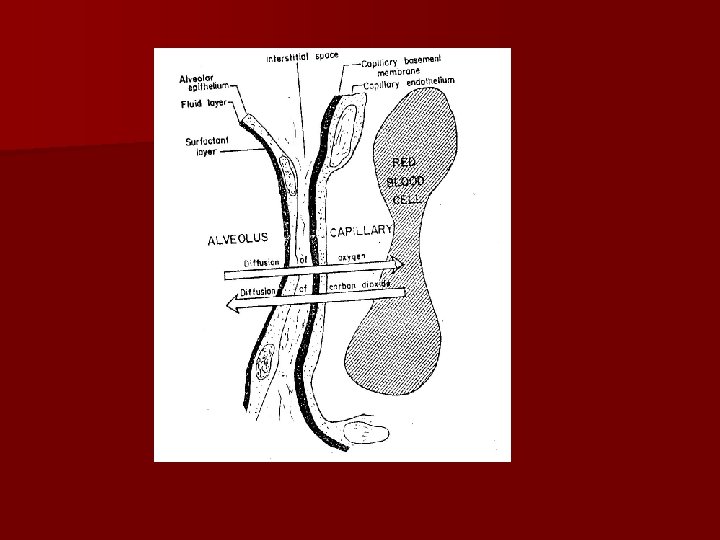
Respiratory membrane n n n n The air in the alveoli is separated from the blood in the capillaries by a very thin respiratory membrane which consists of: 1 -Layer of fluid lining the alveolus and containing surfactant. 2 -Single layer of thin alveolar epithelial cells. 3 -An epithelial basement membrane. 4 -A very thin interstitial space between the alveolar epithelium and the capillary membrane. . 5 -Capillary basement membrane. 6 -Capillary endothelial membrane
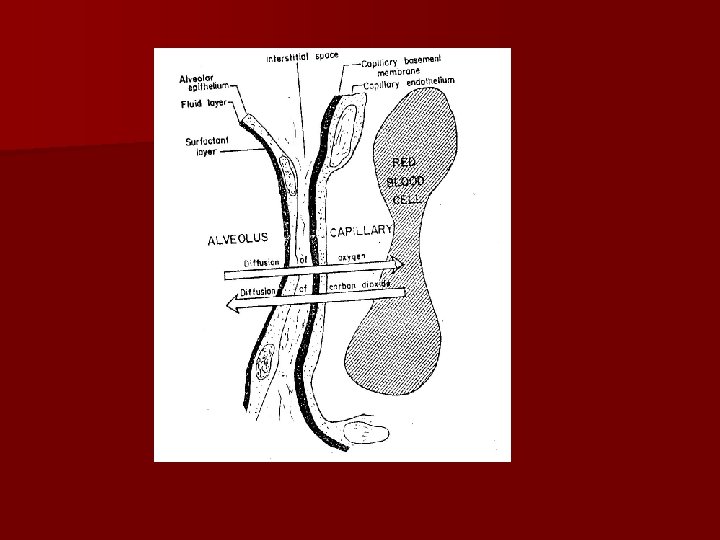
Respiratory membrane n n n Factors affecting the rate of gas diffusion through respiratory membrane 1 -Thickness of the membrane. 2 -Surface area of the membrane. 3 -The diffusion coefficient of the gas in the substance of the membrane depends on its solubility in the membrane and inversely on the square root of its molecular weight, the net result is that the diffusion rate of CO 2 through a tissue sheet is about 20 times that of O 2. 4 -Pressure gradient.
Respiratory membrane n n Diffusion capacity of respiratory membrane= p. gradient×surface area ×solubility ---------------------Thickness× √M. W n PAO 2=100 mm. Hg PVO 2=40 mm. Hg PVCO 2=46 mm. Hg PACO 2=40 mm. Hg
PULMONARY CIRCULATION n The blood supply of the lung is derived from 2 sources: n 1 -Bronchial vessels, coming from the aorta, supply the bronchial tree and the parietal pleura. n 2 -Pulmonary artery.

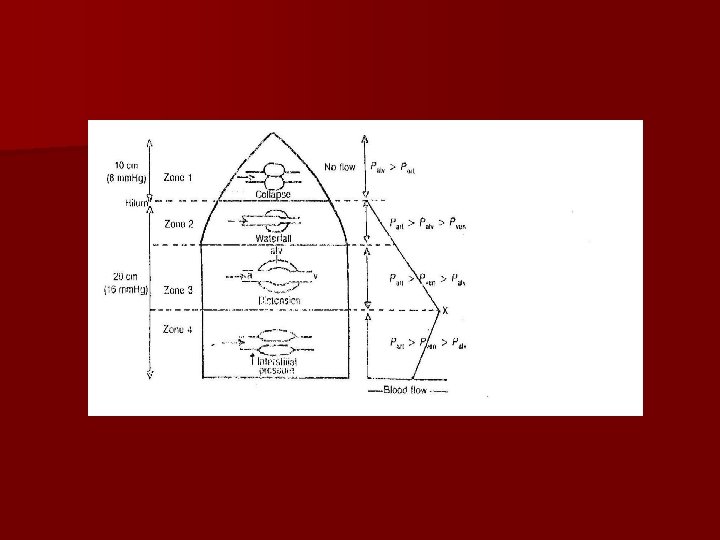
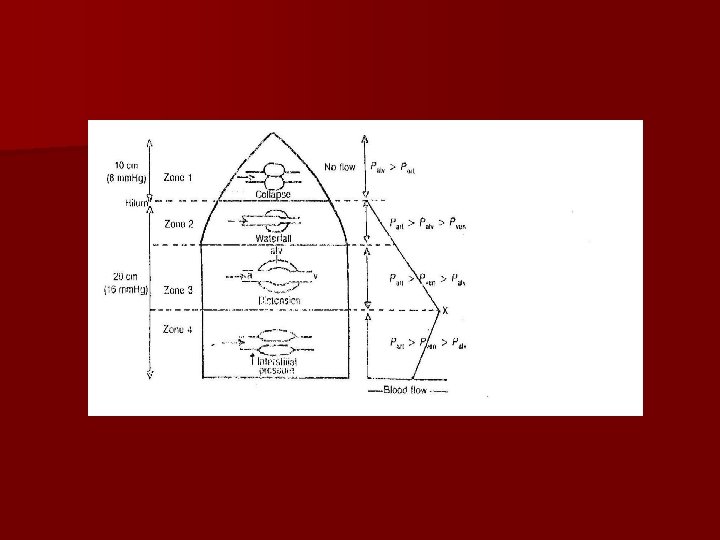
Distribution of blood flow n Like ventilation it is found that inequality of blood flow exists within the human lung as well. In the upright lung, blood flow decreases almost linearly from the bottom to the top reaching very low values at the apex.
Causes of regional distribution of blood flow n 2 -The difference in pressure between the arterial and venous ends of lung capillaries drives blood through them. But blood only flows when the hydrostatic pressure keeps capillaries open. n 3 -Alveolar air pressure
Causes of regional distribution of blood flow 1 -The hydrostatic pressure is determined by the distance of any region of the lung above the base. n In the normal upright, the lowest point in the lungs is about 30 cm below the highest point, this represents a 23 mm. Hg pressure difference, about 15 mm. Hg of which is above the heart and 8 below, the pulmonary arterial pressures in the upper portion of the lung of a standing person are about 15 mm. Hg less than the pulmonary arterial pressure at the level of the heart and the pressure in the lowest portion of the lungs is about 8 mm. Hg greater. n
Perfusion zones of the vertical lung n 1 -Zone I: Palv > Part > Pven (no flow, collapse) n 2 -Zone 2: Part > Palv > Pven. (water fall) n 3 -Zone 3: Part > P ven > Palv. (distension) n 4 -Zone 4: Part > P ven > Palv (interstitial pressure)
Regulation of pulmonary blood flow n -Alveolar hypoxia produces hypoxic pulmonary vasoconstriction(shifting the blood to well ventilated region)