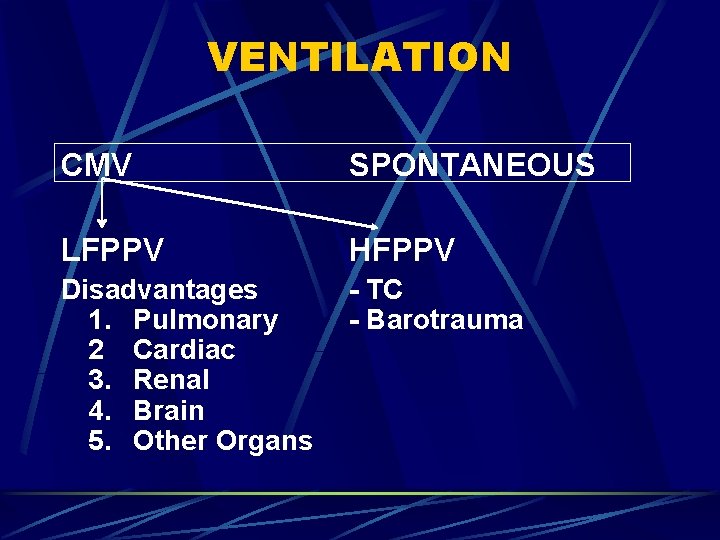
VENTILATION CMV SPONTANEOUS LFPPV HFPPV Disadvantages 1 Pulmonary

- Slides: 63
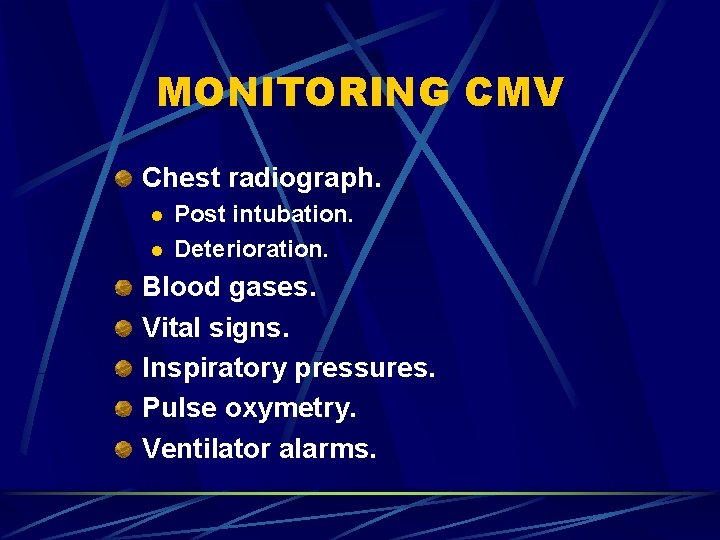
VENTILATION CMV SPONTANEOUS LFPPV HFPPV Disadvantages 1. Pulmonary 2 Cardiac 3. Renal 4. Brain 5. Other Organs - TC - Barotrauma
VENTILATION Prof. Mehdi Hasan Mumtaz
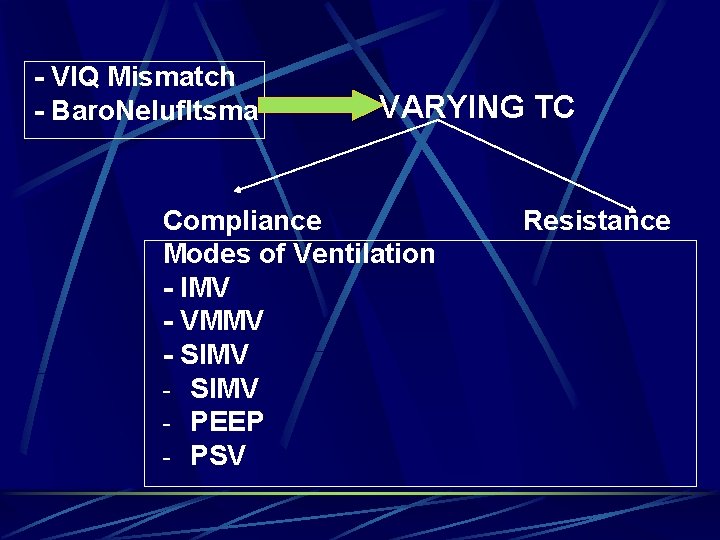
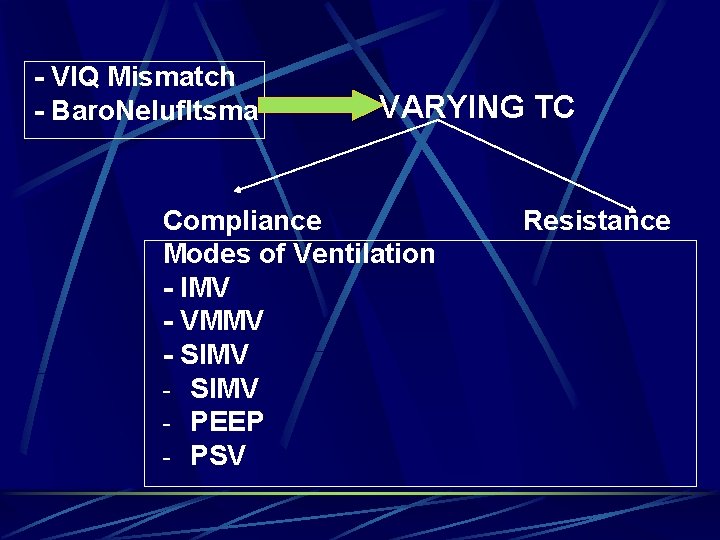
- VIQ Mismatch - Baro. Nelufltsma VARYING TC Compliance Modes of Ventilation - IMV - VMMV - SIMV - PEEP - PSV Resistance
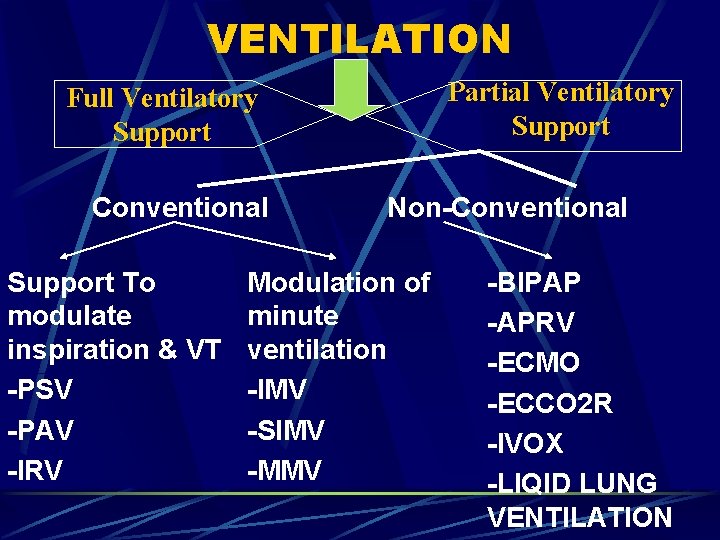
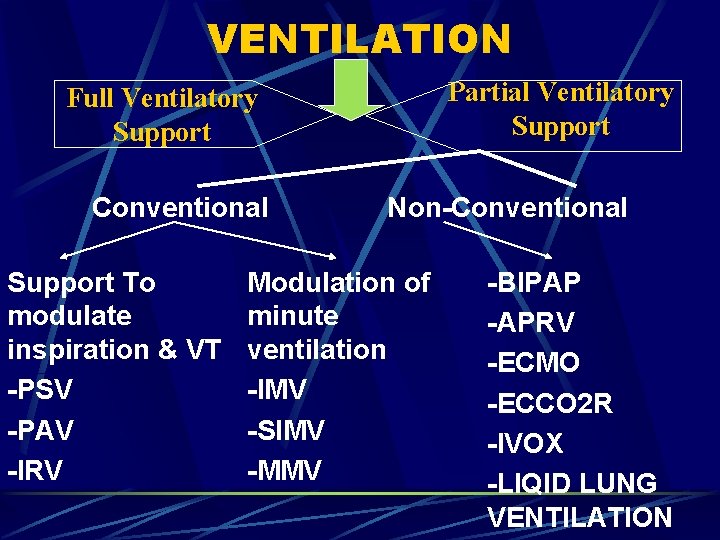
VENTILATION Partial Ventilatory Support Full Ventilatory Support Conventional Support To modulate inspiration & VT -PSV -PAV -IRV Non-Conventional Modulation of minute ventilation -IMV -SIMV -MMV -BIPAP -APRV -ECMO -ECCO 2 R -IVOX -LIQID LUNG VENTILATION
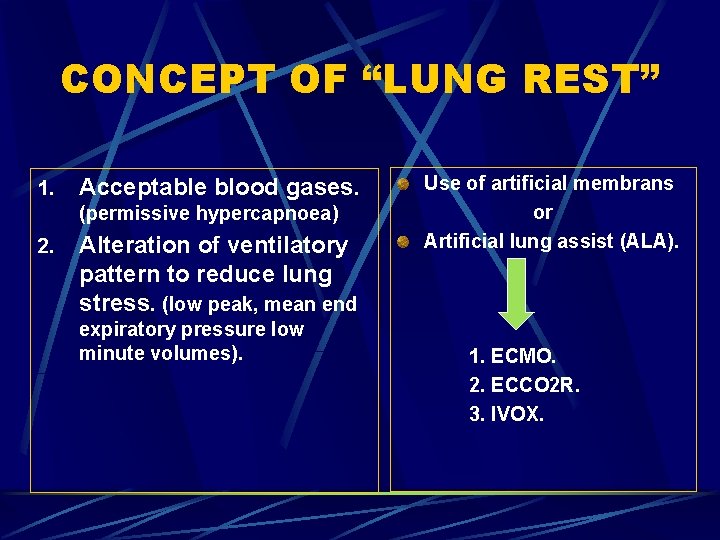
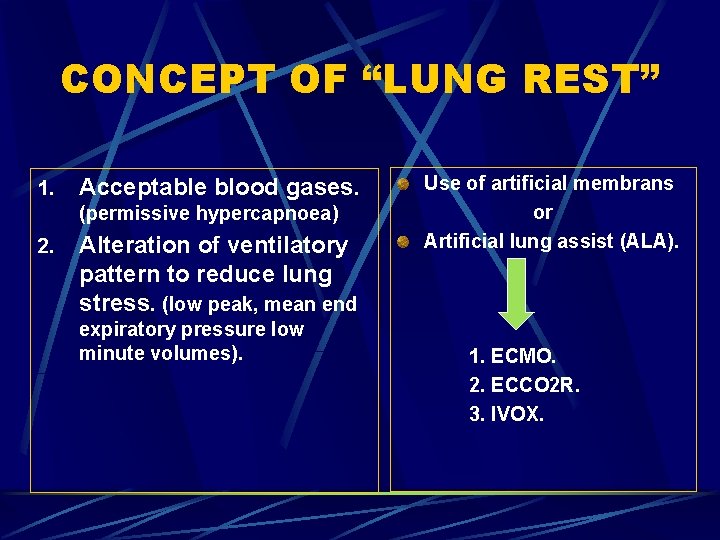
CONCEPT OF “LUNG REST” 1. Acceptable blood gases. (permissive hypercapnoea) 2. Alteration of ventilatory pattern to reduce lung stress. (low peak, mean end expiratory pressure low minute volumes). Use of artificial membrans or Artificial lung assist (ALA). 1. ECMO. 2. ECCO 2 R. 3. IVOX.
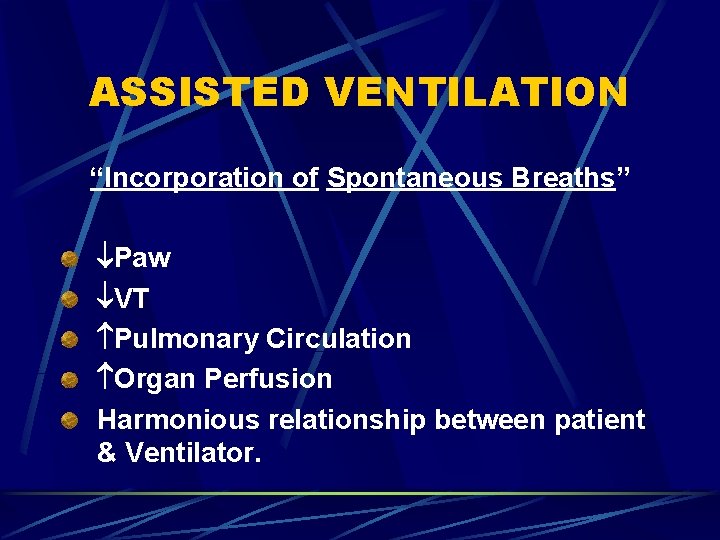
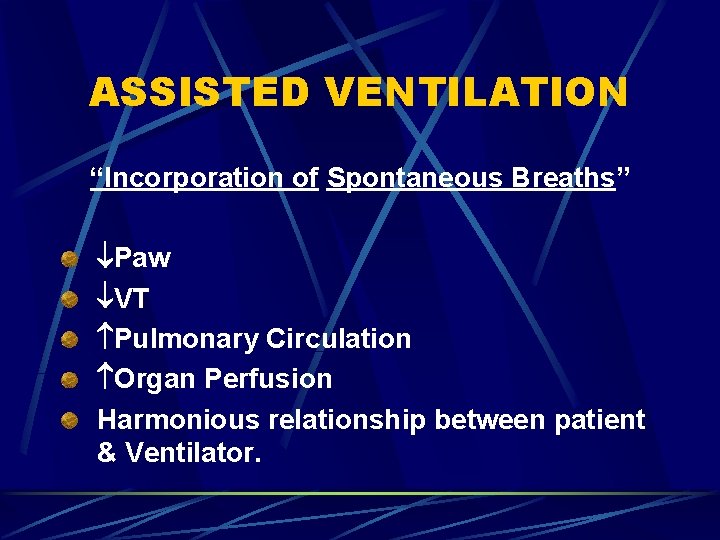
ASSISTED VENTILATION “Incorporation of Spontaneous Breaths” Paw VT Pulmonary Circulation Organ Perfusion Harmonious relationship between patient & Ventilator.
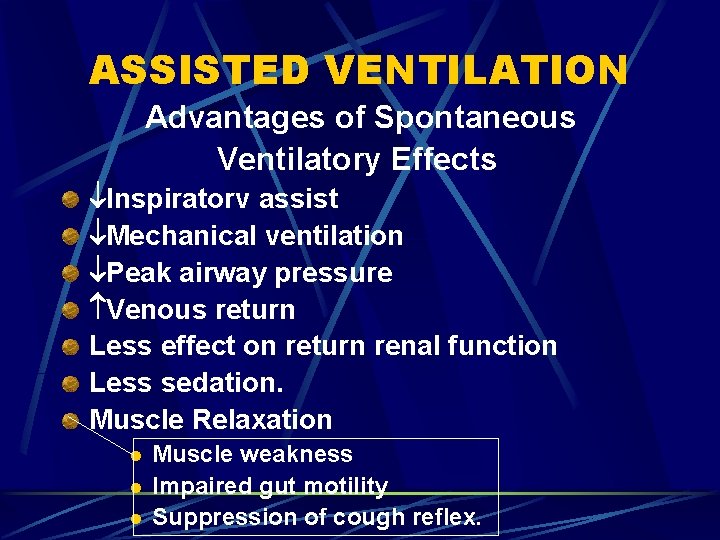
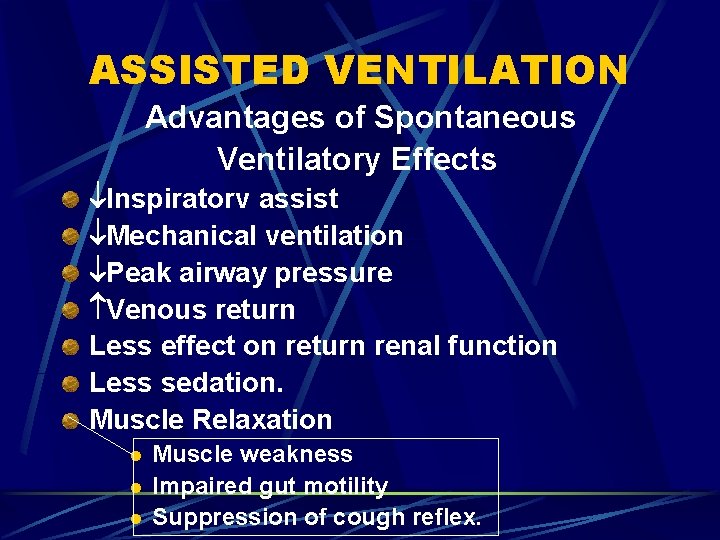
ASSISTED VENTILATION Advantages of Spontaneous Ventilatory Effects lnspiratorv assist Mechanical ventilation Peak airway pressure Venous return Less effect on return renal function Less sedation. Muscle Relaxation l l l Muscle weakness Impaired gut motility Suppression of cough reflex.
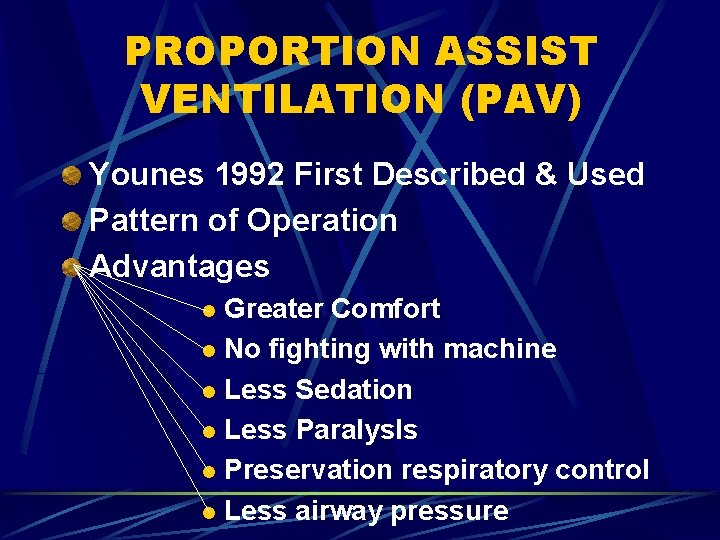
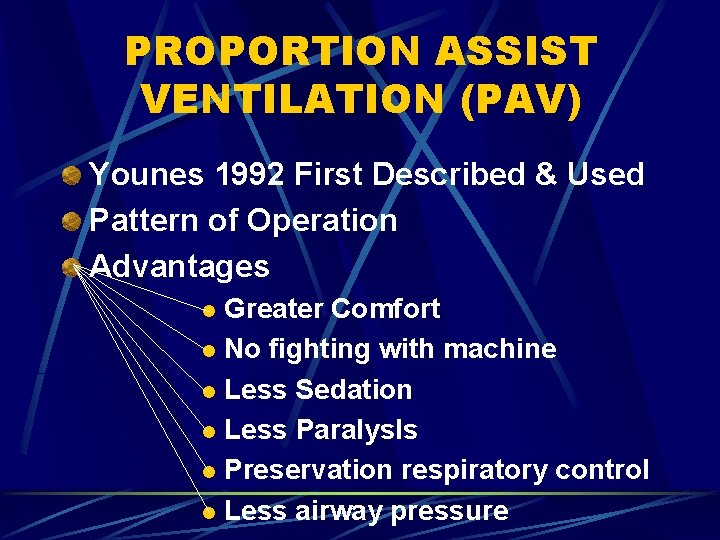
PROPORTION ASSIST VENTILATION (PAV) Younes 1992 First Described & Used Pattern of Operation Advantages Greater Comfort l No fighting with machine l Less Sedation l Less Paralys. Is l Preservation respiratory control l Less airway pressure l
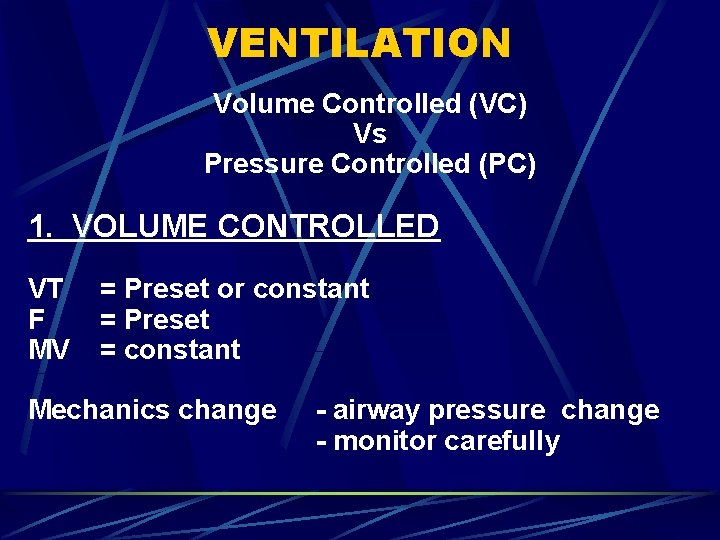
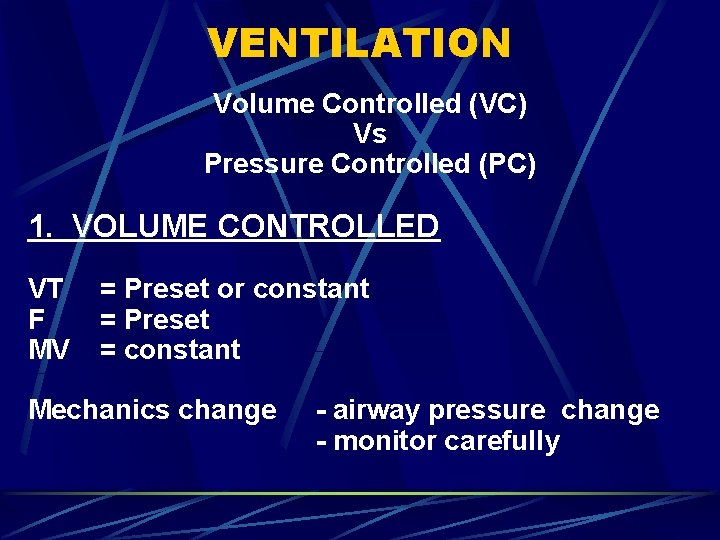
VENTILATION Volume Controlled (VC) Vs Pressure Controlled (PC) 1. VOLUME CONTROLLED VT F MV = Preset or constant = Preset = constant Mechanics change - airway pressure change - monitor carefully
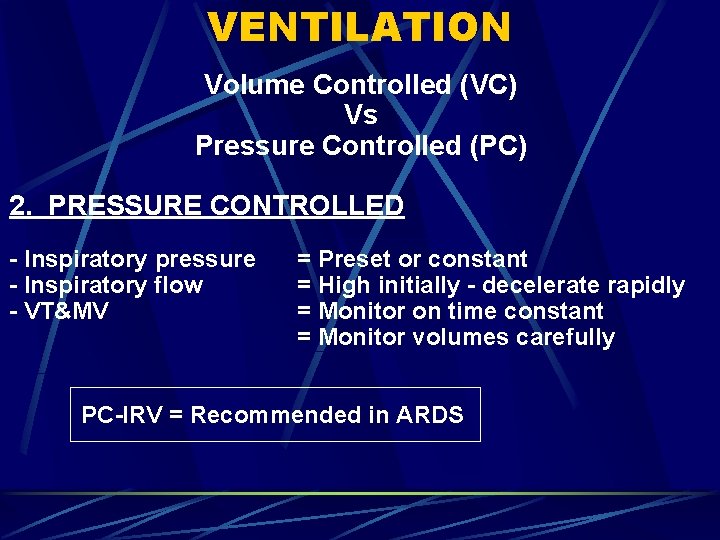
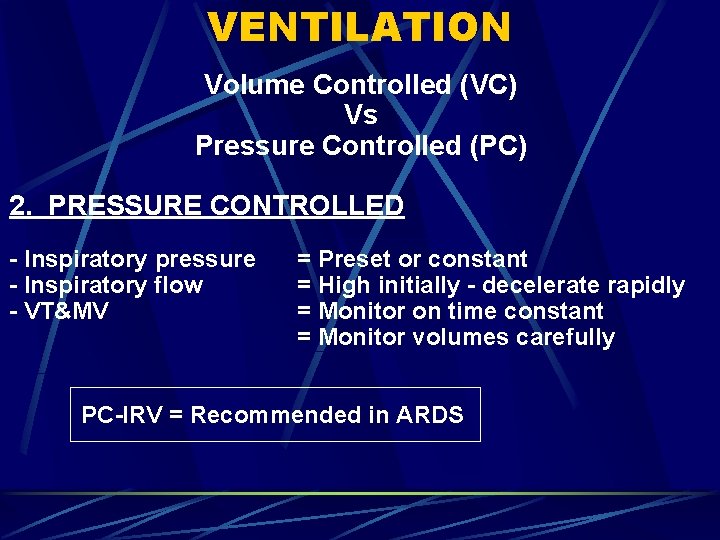
VENTILATION Volume Controlled (VC) Vs Pressure Controlled (PC) 2. PRESSURE CONTROLLED - lnspiratory pressure - Inspiratory flow - VT&MV = Preset or constant = High initially - decelerate rapidly = Monitor on time constant = Monitor volumes carefully PC-IRV = Recommended in ARDS
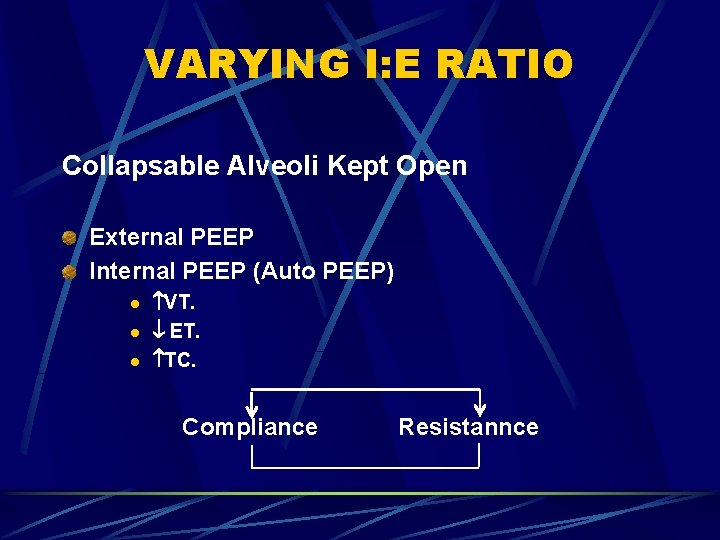
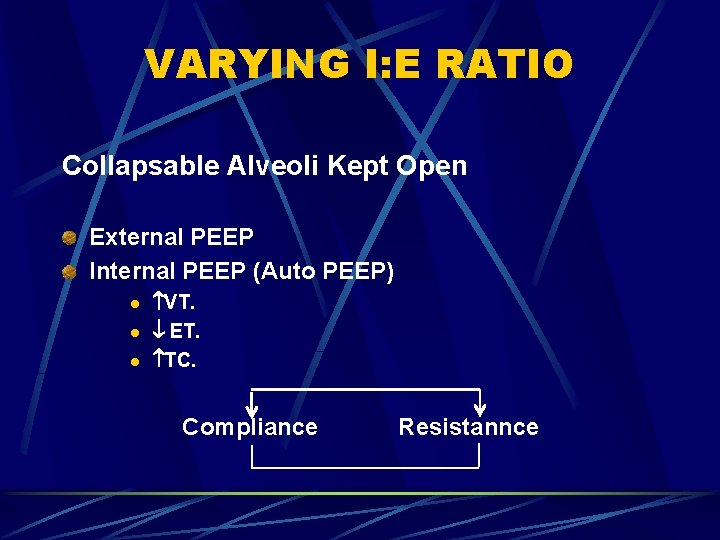
VARYING I: E RATIO Collapsable Alveoli Kept Open External PEEP Internal PEEP (Auto PEEP) l l l VT. ET. TC. Compliance Resistannce
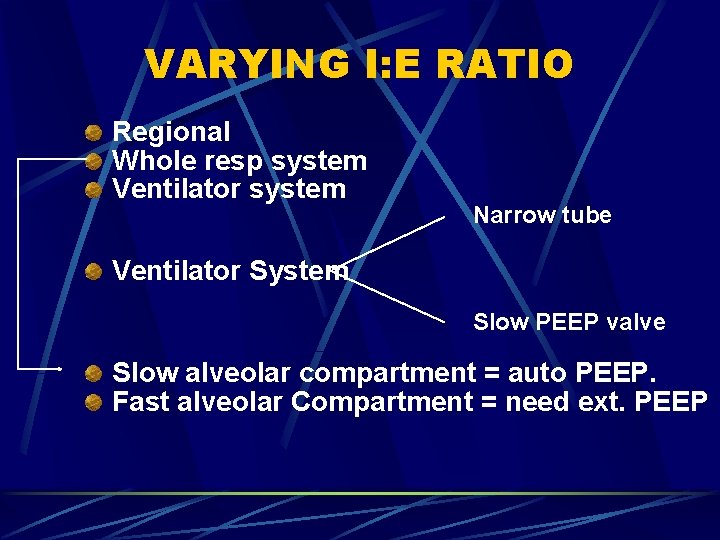
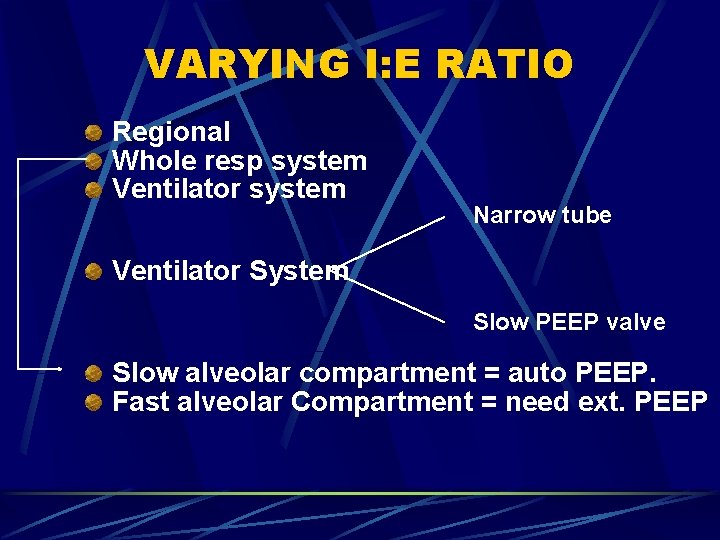
VARYING I: E RATIO Regional Whole resp system Ventilator system Narrow tube Ventilator System Slow PEEP valve Slow alveolar compartment = auto PEEP. Fast alveolar Compartment = need ext. PEEP
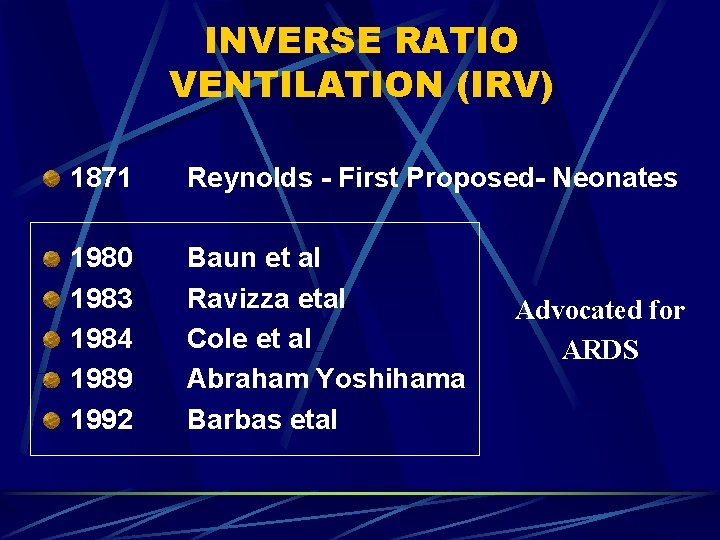
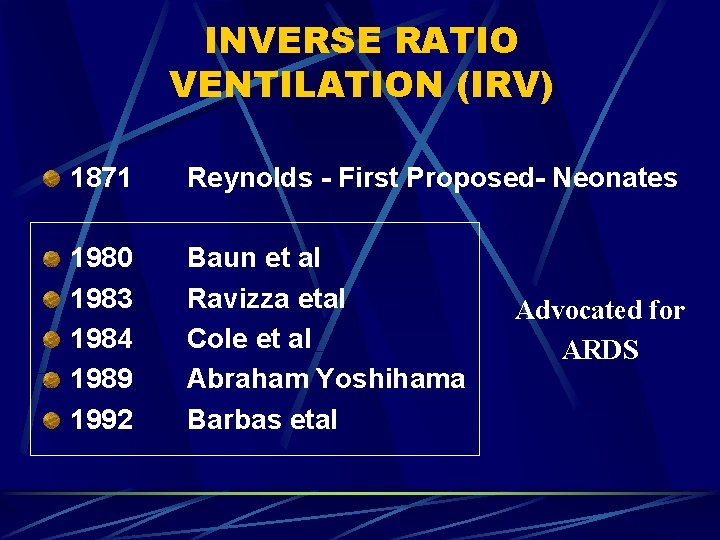
INVERSE RATIO VENTILATION (IRV) 1871 Reynolds - First Proposed- Neonates 1980 1983 1984 1989 1992 Baun et al Ravizza etal Cole et al Abraham Yoshihama Barbas etal Advocated for ARDS
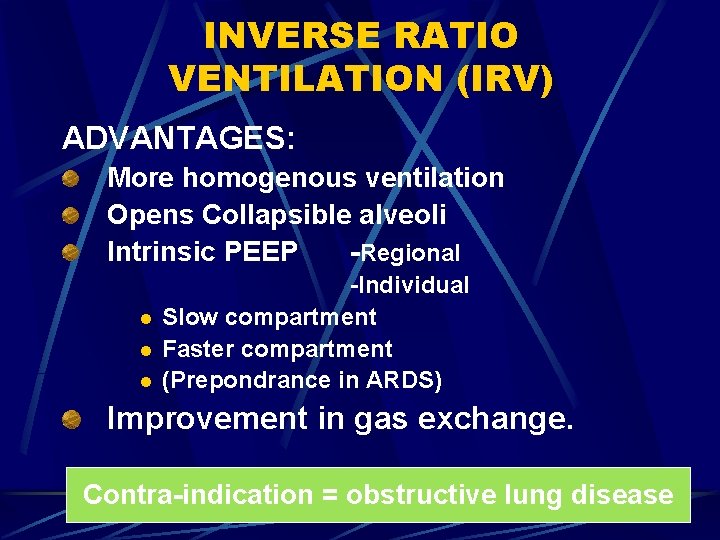
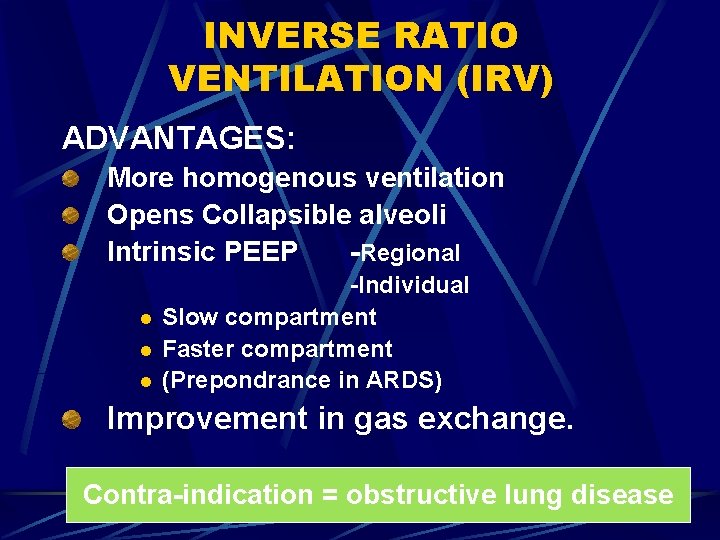
INVERSE RATIO VENTILATION (IRV) ADVANTAGES: More homogenous ventilation Opens Co. IIapsible alveoli Intrinsic PEEP -Regional l -Individual Slow compartment Faster compartment (Prepondrance in ARDS) Improvement in gas exchange. Contra-indication = obstructive lung disease
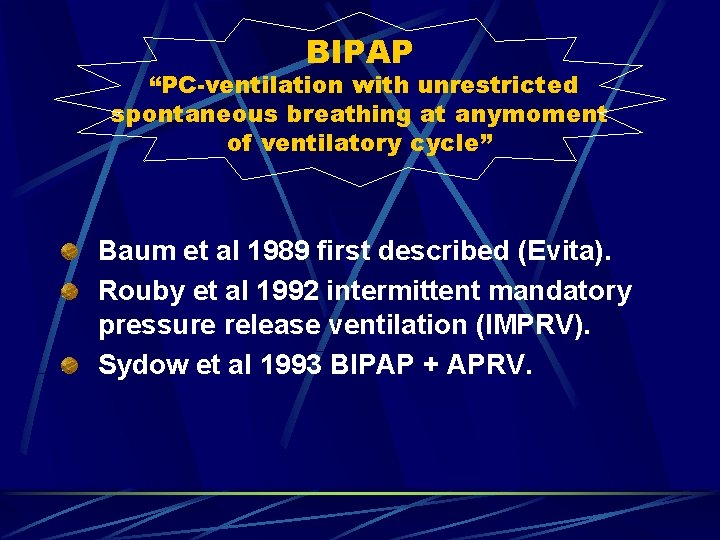
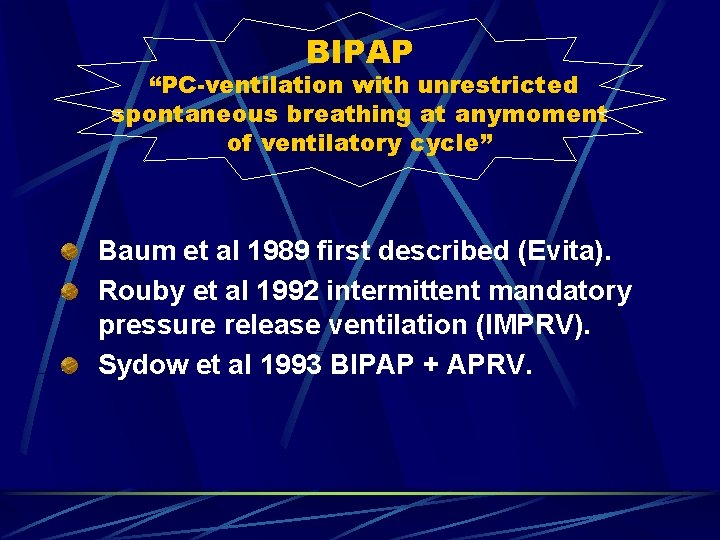
BIPAP “PC-ventilation with unrestricted spontaneous breathing at anymoment of ventilatory cycle” Baum et al 1989 first described (Evita). Rouby et al 1992 intermittent mandatory pressure release ventilation (IMPRV). Sydow et al 1993 BIPAP + APRV.
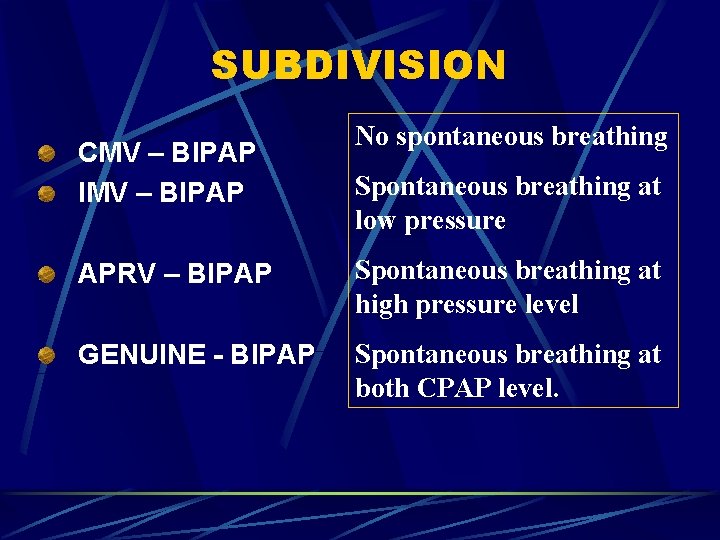
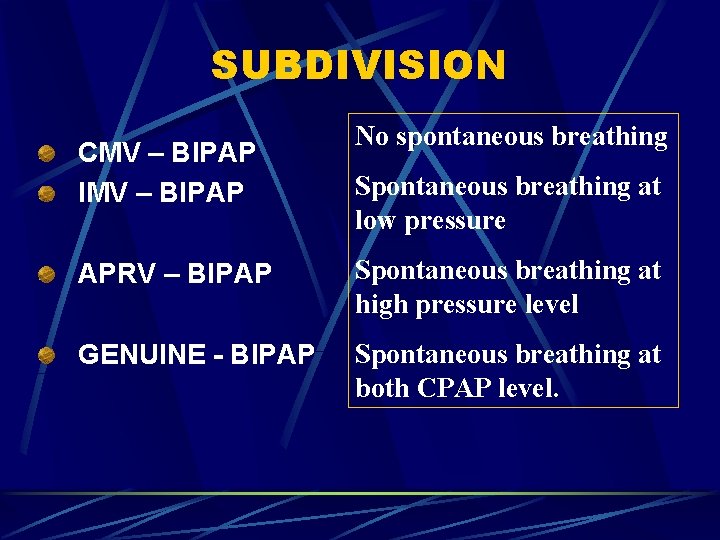
SUBDIVISION CMV – BIPAP IMV – BIPAP No spontaneous breathing Spontaneous breathing at low pressure APRV – BIPAP Spontaneous breathing at high pressure level GENUINE - BIPAP Spontaneous breathing at both CPAP level.
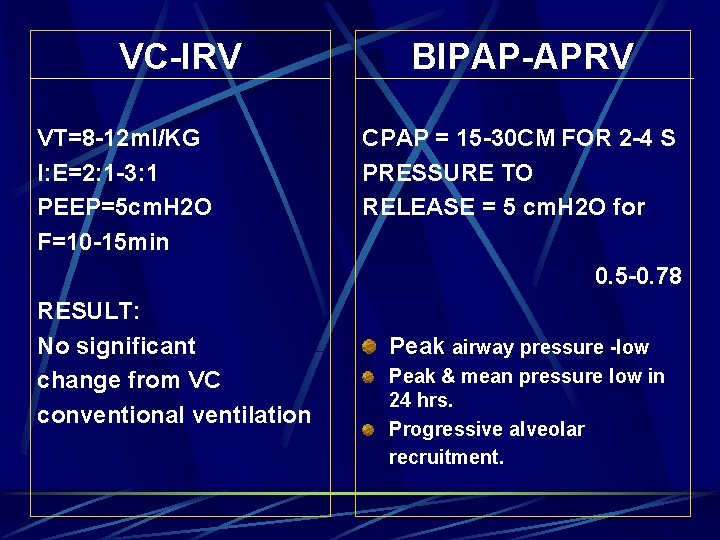
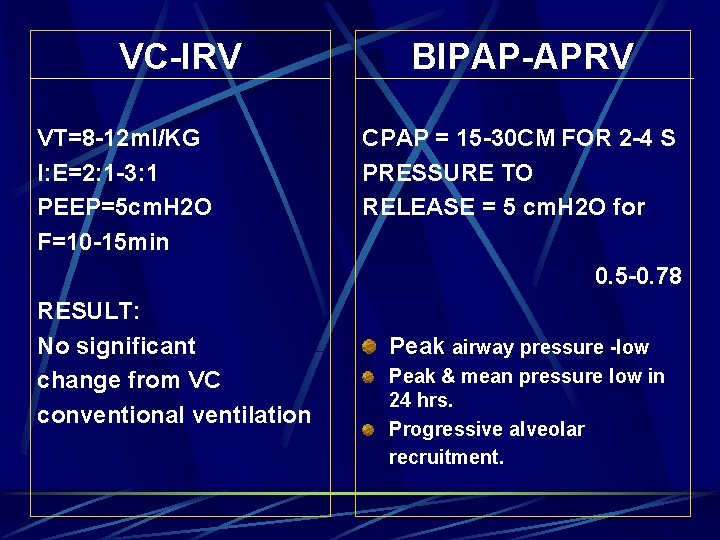
VC-IRV VT=8 -12 ml/KG I: E=2: 1 -3: 1 PEEP=5 cm. H 2 O F=10 -15 min BIPAP-APRV CPAP = 15 -30 CM FOR 2 -4 S PRESSURE TO RELEASE = 5 cm. H 2 O for 0. 5 -0. 78 RESULT: No significant change from VC conventional ventilation Peak airway pressure -low Peak & mean pressure low in 24 hrs. Progressive alveolar recruitment.
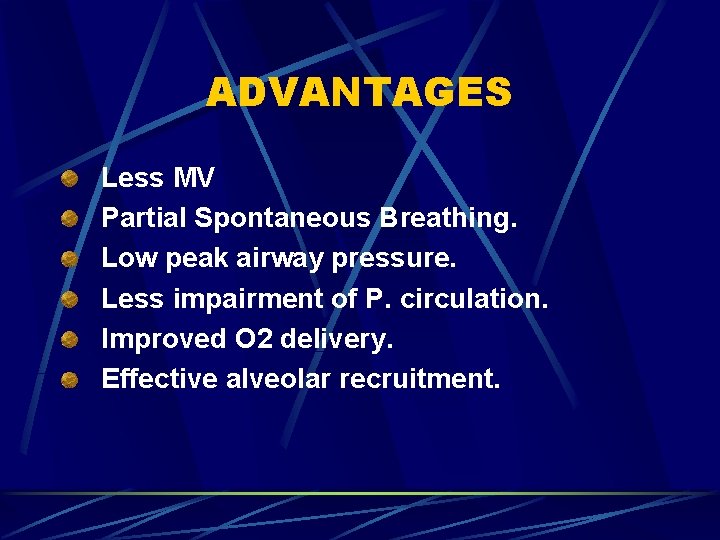
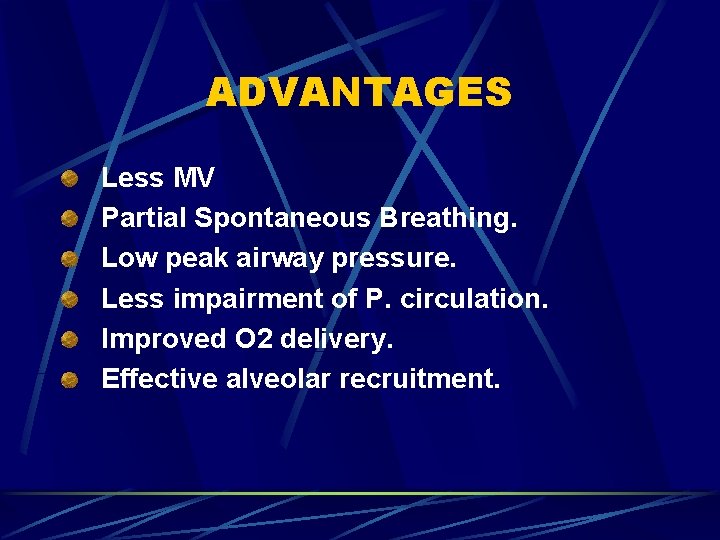
ADVANTAGES Less MV Partial Spontaneous Breathing. Low peak airway pressure. Less impairment of P. circulation. Improved O 2 delivery. Effective alveolar recruitment.
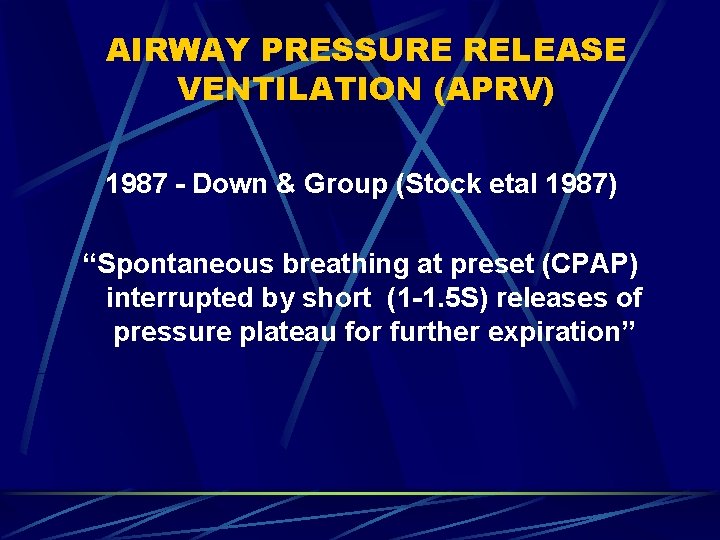
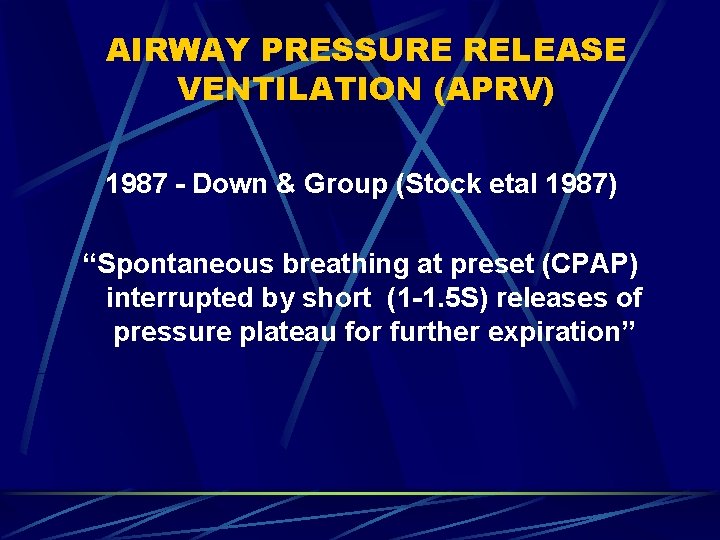
AIRWAY PRESSURE RELEASE VENTILATION (APRV) 1987 - Down & Group (Stock etal 1987) “Spontaneous breathing at preset (CPAP) interrupted by short (1 -1. 5 S) releases of pressure plateau for further expiration”
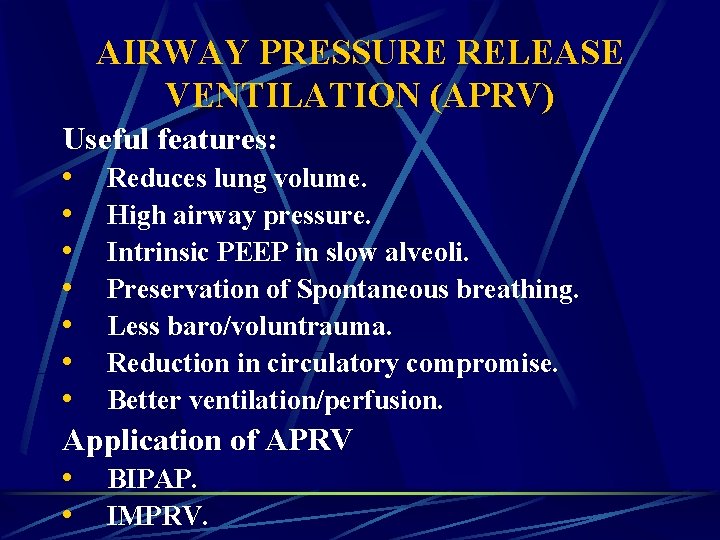
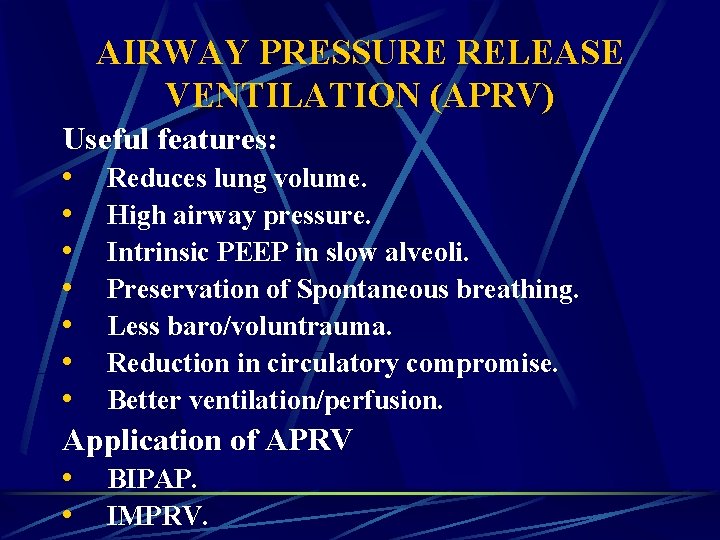
AIRWAY PRESSURE RELEASE VENTILATION (APRV) Useful features: • Reduces lung volume. • High airway pressure. • Intrinsic PEEP in slow alveoli. • Preservation of Spontaneous breathing. • Less baro/voluntrauma. • Reduction in circulatory compromise. • Better ventilation/perfusion. Application of APRV • BIPAP. • IMPRV.
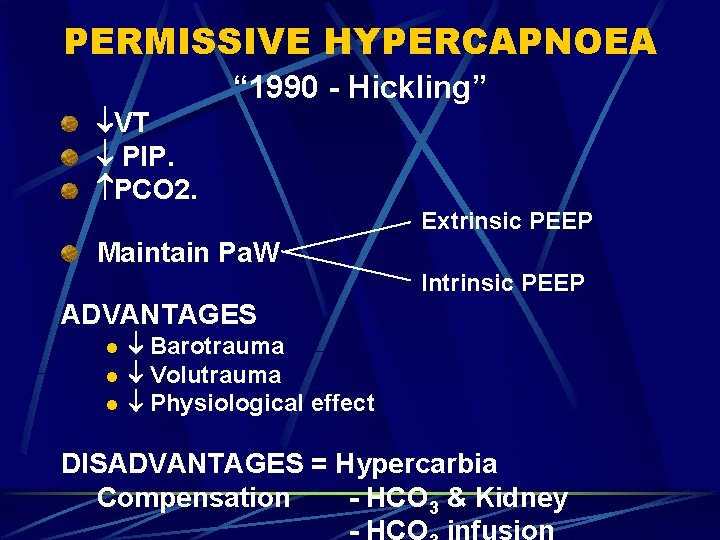
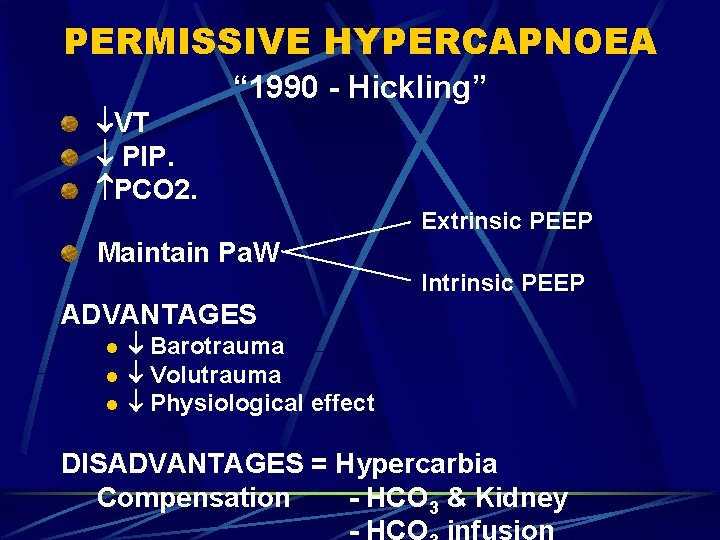
PERMISSIVE HYPERCAPNOEA VT PIP. PCO 2. “ 1990 - Hickling” Extrinsic PEEP Maintain Pa. W Intrinsic PEEP ADVANTAGES l l l Barotrauma Volutrauma Physiological effect DISADVANTAGES = Hypercarbia Compensation - HCO 3 & Kidney

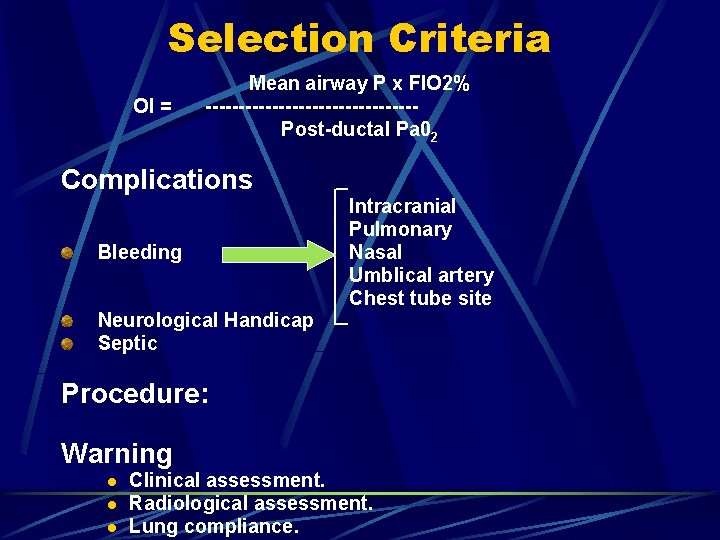
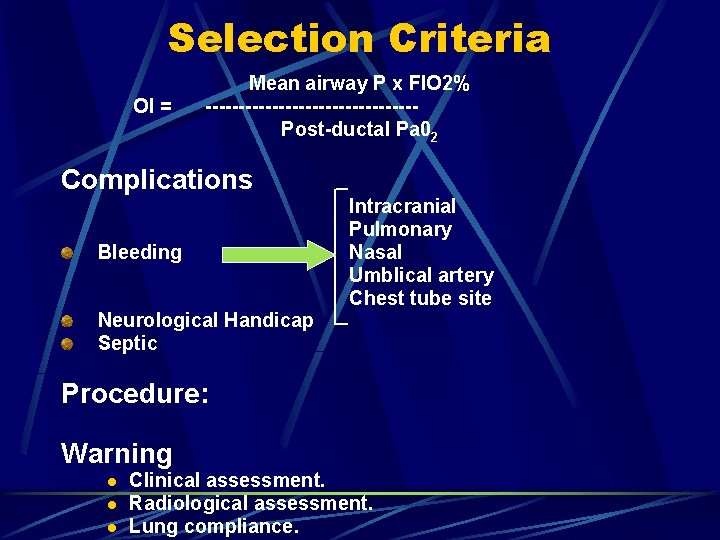
Selection Criteria OI = Mean airway P x FIO 2% ----------------Post-ductal Pa 02 Complications Bleeding Intracranial Pulmonary Nasal Umb. Iica. I artery Chest tube site Neurologica. I Handicap Septic Procedure: Warning l l l Clinical assessment. Radiological assessment. Lung compliance.
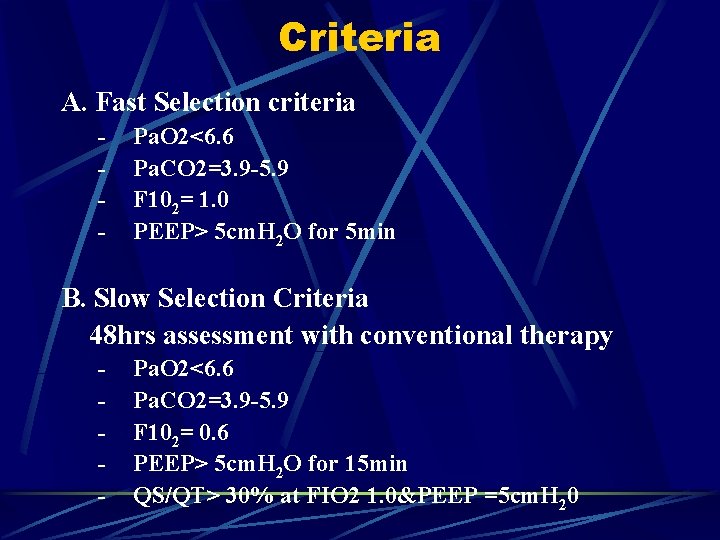
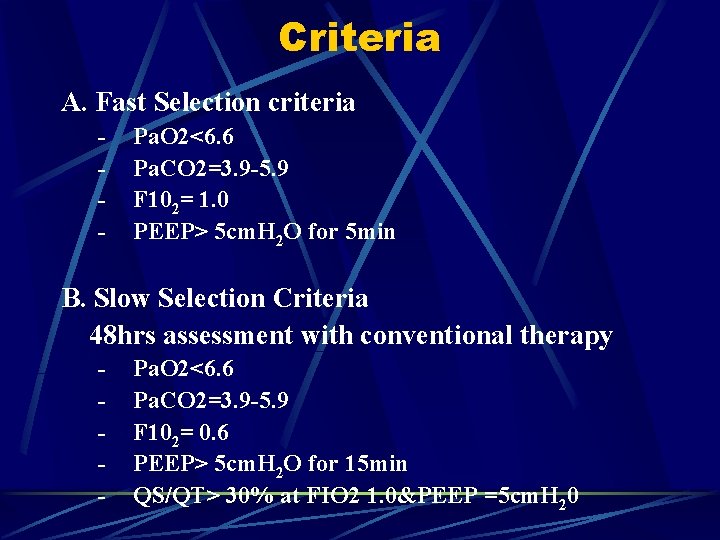
Criteria A. Fast Selection criteria - Pa. O 2<6. 6 Pa. CO 2=3. 9 -5. 9 F 102= 1. 0 PEEP> 5 cm. H 2 O for 5 min B. Slow Selection Criteria 48 hrs assessment with conventional therapy - Pa. O 2<6. 6 Pa. CO 2=3. 9 -5. 9 F 102= 0. 6 PEEP> 5 cm. H 2 O for 15 min QS/QT> 30% at FIO 2 1. 0&PEEP =5 cm. H 20
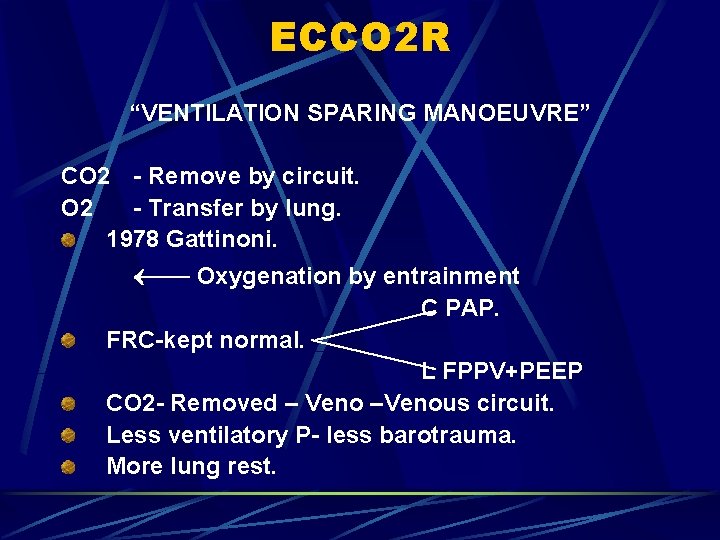
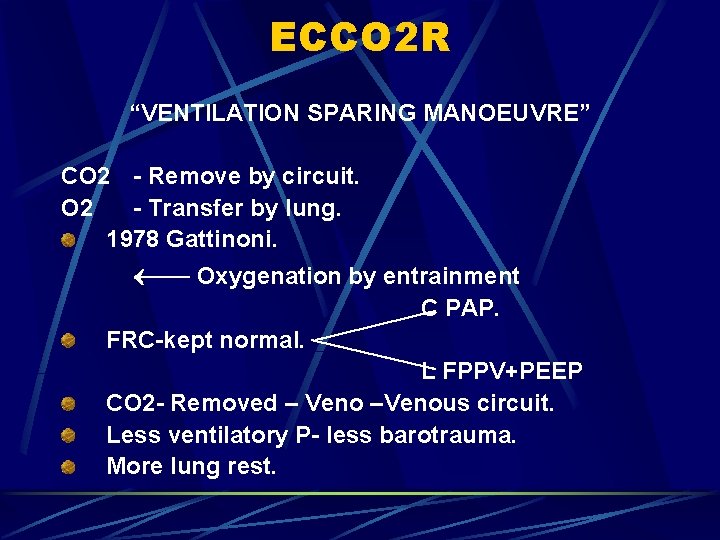
ECCO 2 R “VENTILATION SPARING MANOEUVRE” CO 2 - Remove by circuit. O 2 - Transfer by lung. 1978 Gattinoni. Oxygenation by entrainment C PAP. FRC-kept normal. L FPPV+PEEP CO 2 - Removed – Veno –Venous circuit. Less ventilatory P- less barotrauma. More lung rest.
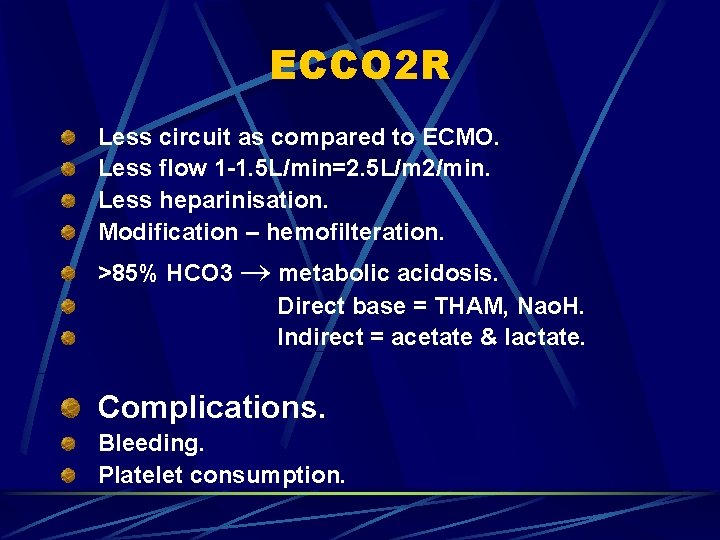
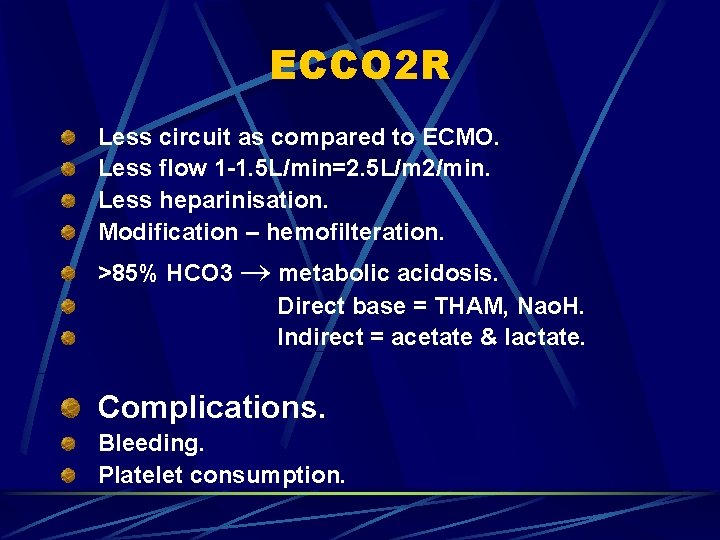
ECCO 2 R Less circuit as compared to ECMO. Less flow 1 -1. 5 L/min=2. 5 L/m 2/min. Less heparinisation. Modification – hemofilteration. >85% HCO 3 metabolic acidosis. Direct base = THAM, Nao. H. Indirect = acetate & lactate. Complications. Bleeding. Platelet consumption.
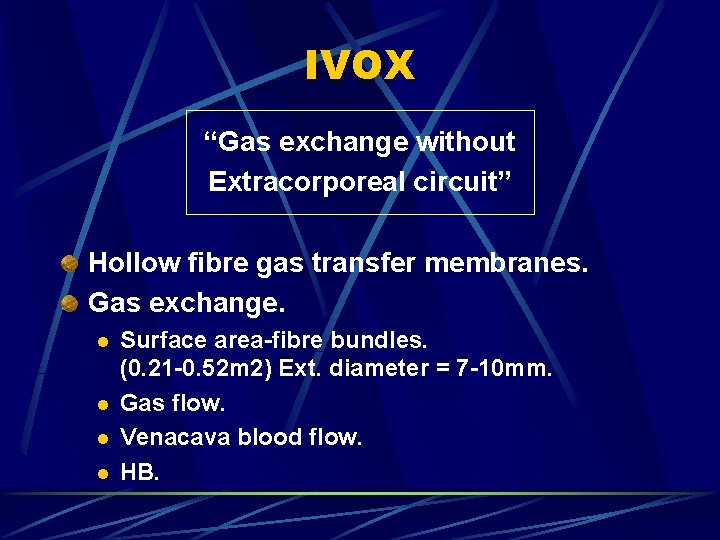
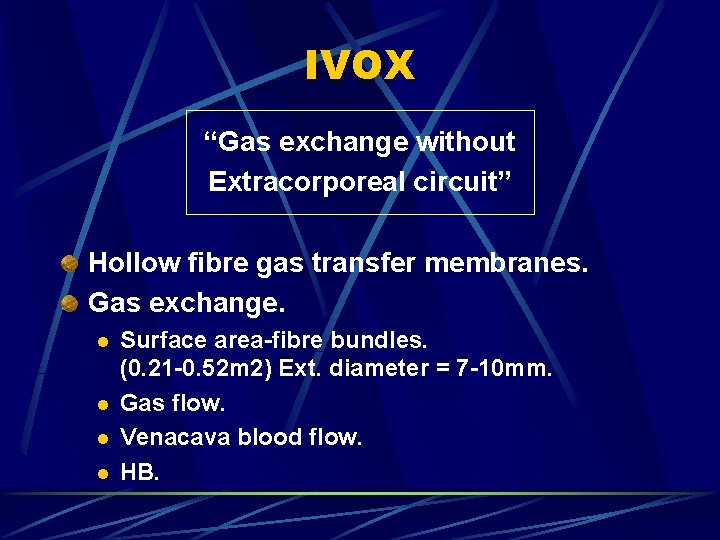
IVOX “Gas exchange without Extracorporeal circuit” Hollow fibre gas transfer membranes. Gas exchange. l l Surface area-fibre bundles. (0. 21 -0. 52 m 2) Ext. diameter = 7 -10 mm. Gas flow. Venacava blood flow. HB.
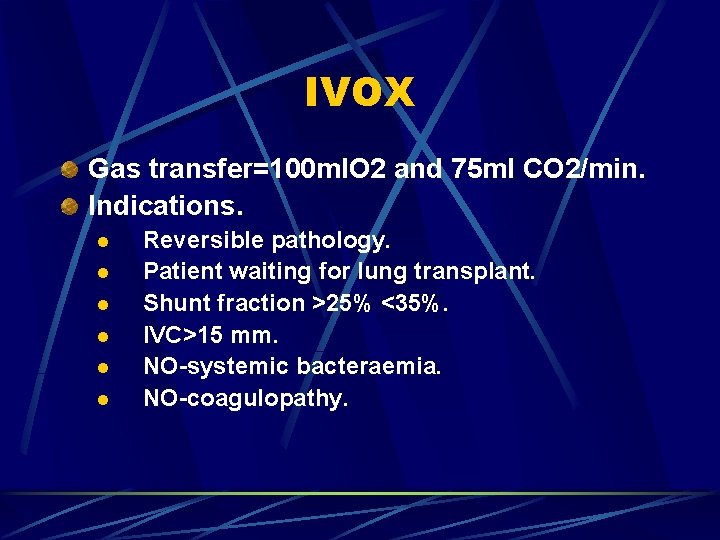
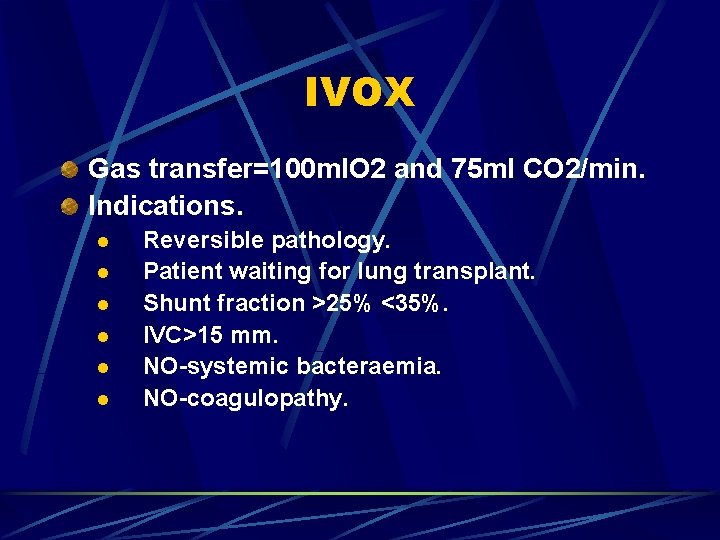
IVOX Gas transfer=100 m. IO 2 and 75 ml CO 2/min. Indications. l l l Reversible pathology. Patient waiting for lung transplant. Shunt fraction >25% <35%. IVC>15 mm. NO-systemic bacteraemia. NO-coagulopathy.
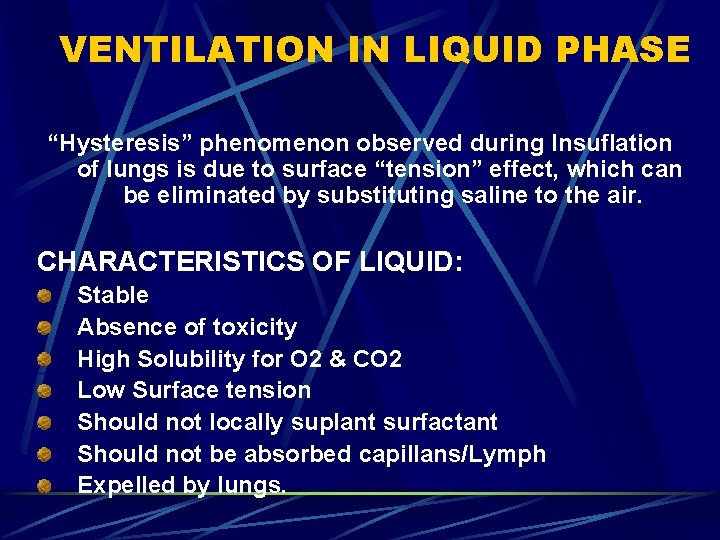
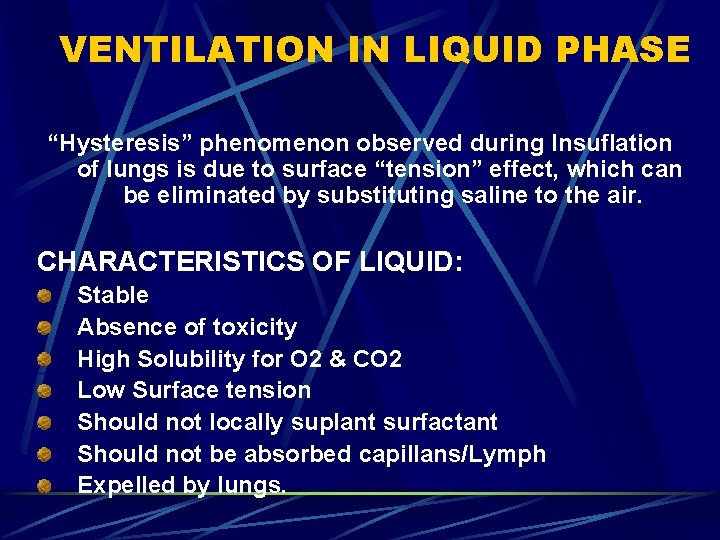
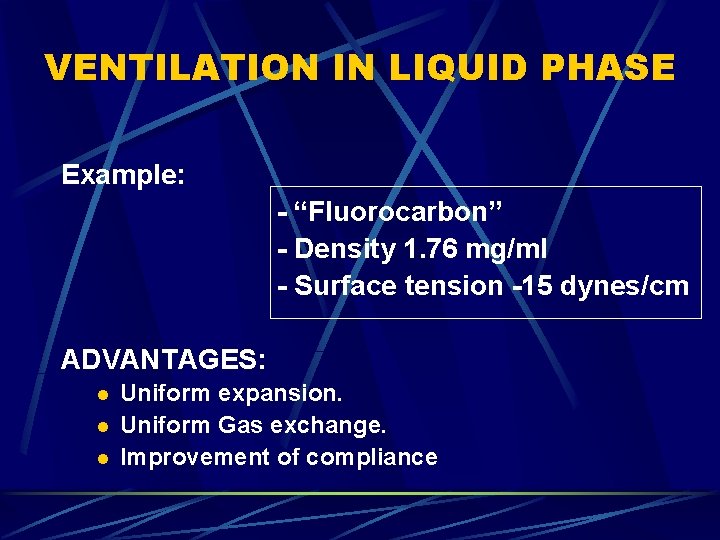
VENTILATION IN LIQUID PHASE “Hysteresis” phenomenon observed during Insuflation of lungs is due to surface “tension” effect, which can be eliminated by substituting saline to the air. CHARACTERISTICS OF LIQUID: Stable Absence of toxicity High Solubility for O 2 & CO 2 Low Surface tension Should not locally suplant surfactant Should not be absorbed capillans/Lymph Expelled by lungs.
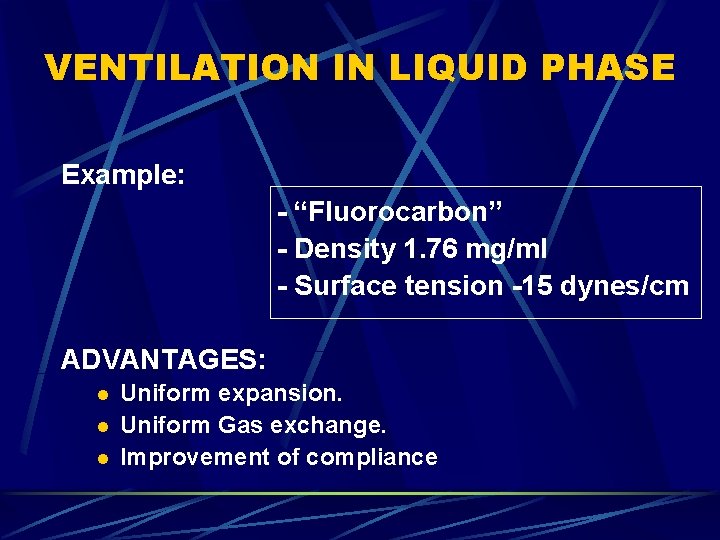
VENTILATION IN LIQUID PHASE Example: - “Fluorocarbon” - Density 1. 76 mg/ml - Surface tension -15 dynes/cm ADVANTAGES: l l l Uniform expansion. Uniform Gas exchange. Improvement of compliance
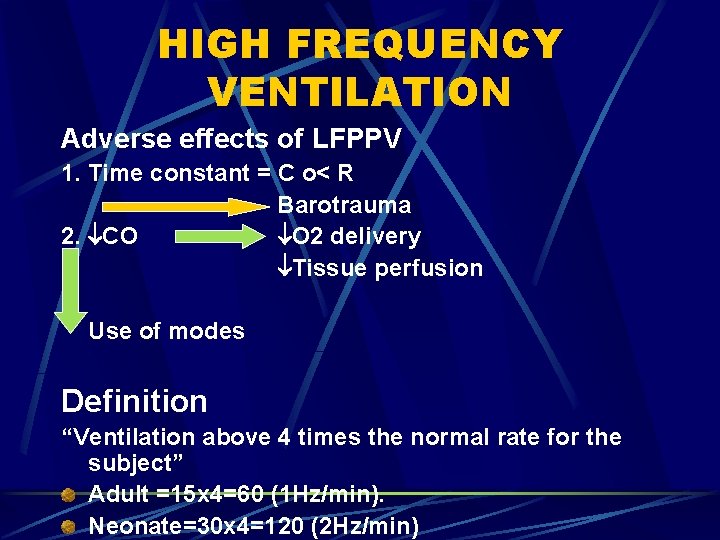
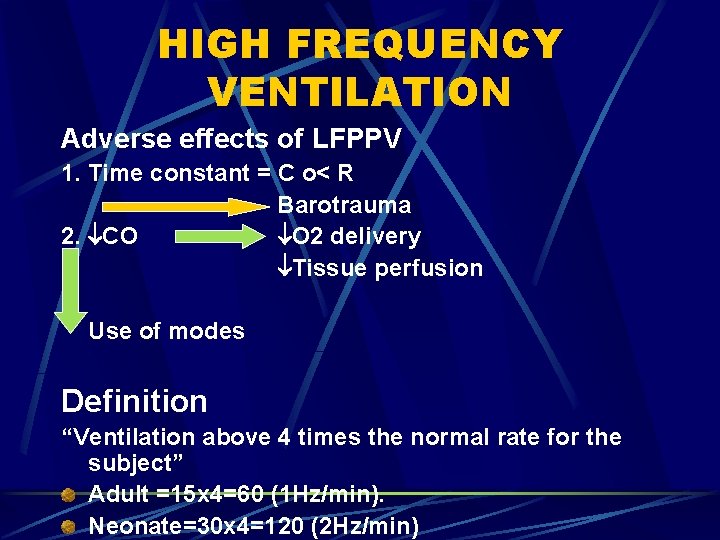
HIGH FREQUENCY VENTILATION Adverse effects of LFPPV 1. Time constant = C o< R Barotrauma 2. CO O 2 delivery Tissue perfusion Use of modes Definition “Ventilation above 4 times the normal rate for the subject” Adult =15 x 4=60 (1 Hz/min). Neonate=30 x 4=120 (2 Hz/min)
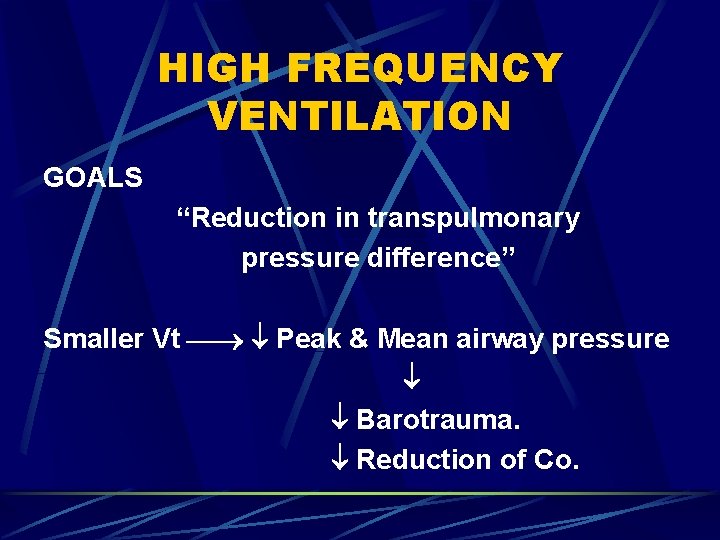
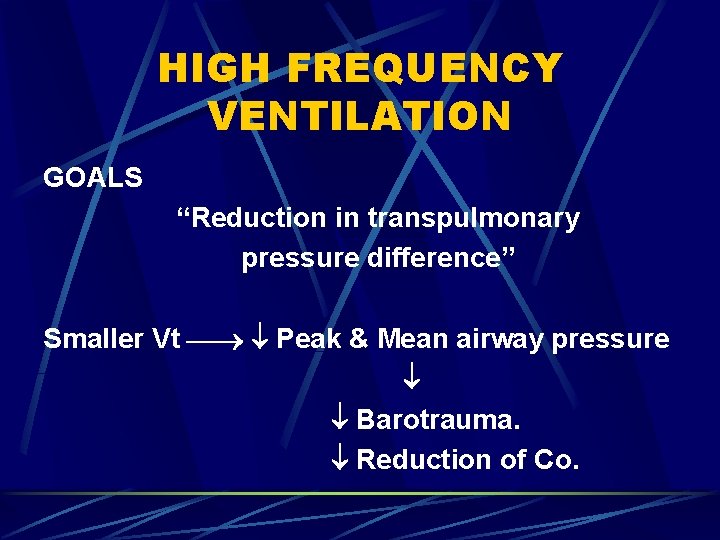
HIGH FREQUENCY VENTILATION GOALS “Reduction in transpulmonary pressure difference” Smaller Vt Peak & Mean airway pressure Barotrauma. Reduction of Co.
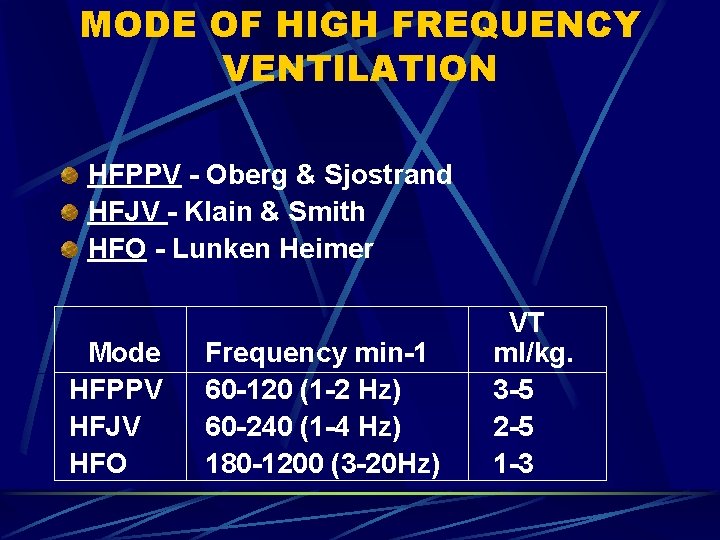
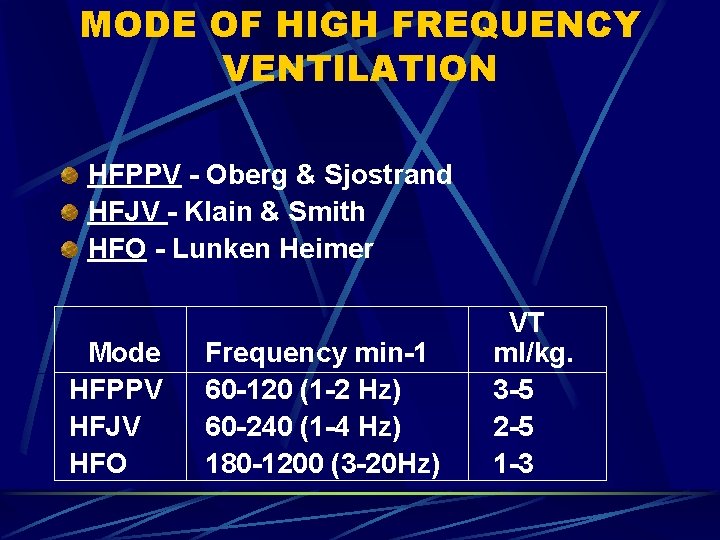
MODE OF HIGH FREQUENCY VENTILATION HFPPV - Oberg & Sjostrand HFJV - Klain & Smith HFO - Lunken Heimer Mode HFPPV HFJV HFO Frequency min-1 60 -120 (1 -2 Hz) 60 -240 (1 -4 Hz) 180 -1200 (3 -20 Hz) VT ml/kg. 3 -5 2 -5 1 -3
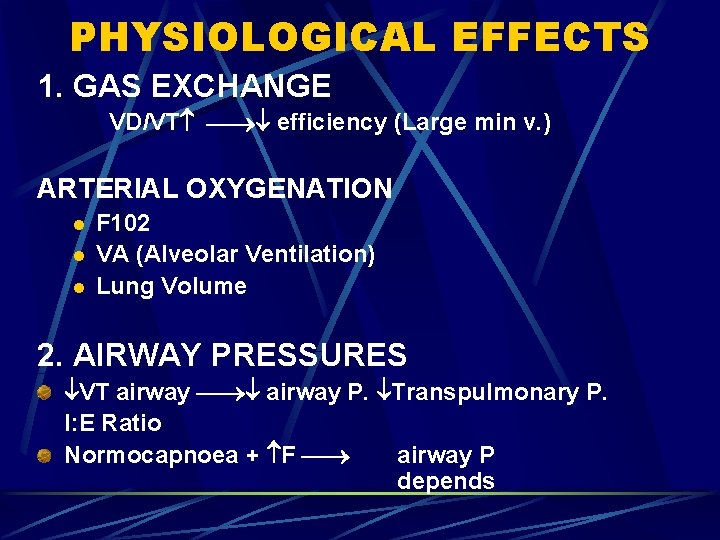
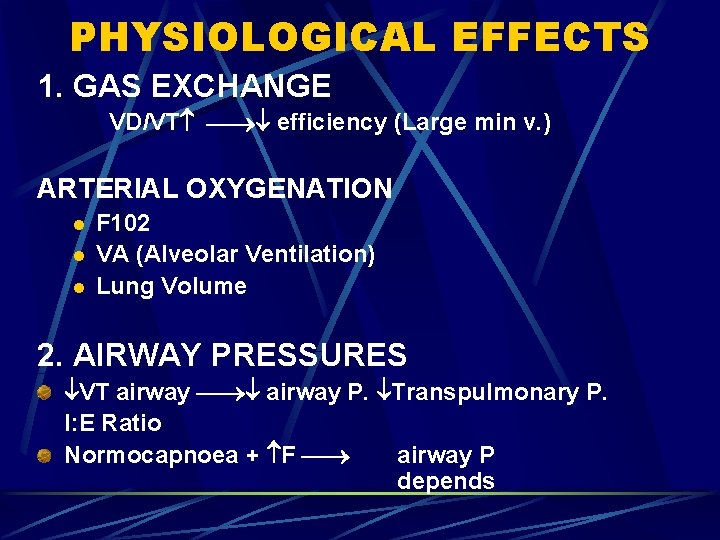
PHYSIOLOGICAL EFFECTS 1. GAS EXCHANGE VD/VT efficiency (Large min v. ) ARTERIAL OXYGENATION l l l F 102 VA (Alveolar Ventilation) Lung Volume 2. AIRWAY PRESSURES VT airway P. Transpulmonary P. I: E Ratio Normocapnoea + F airway P depends
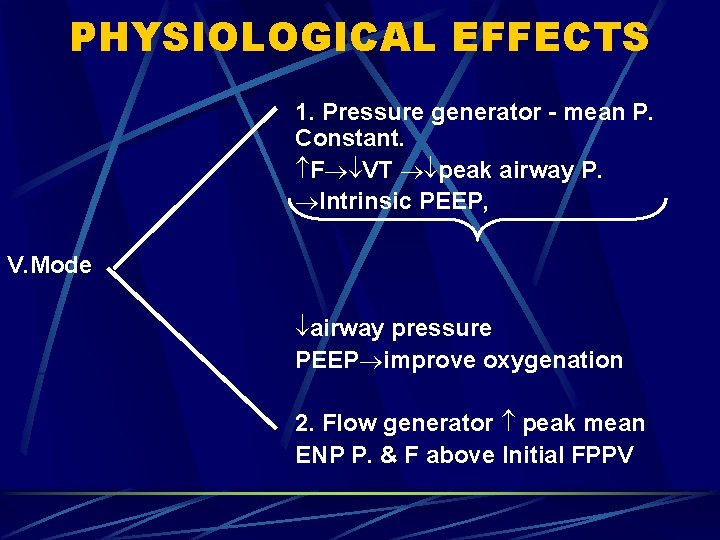
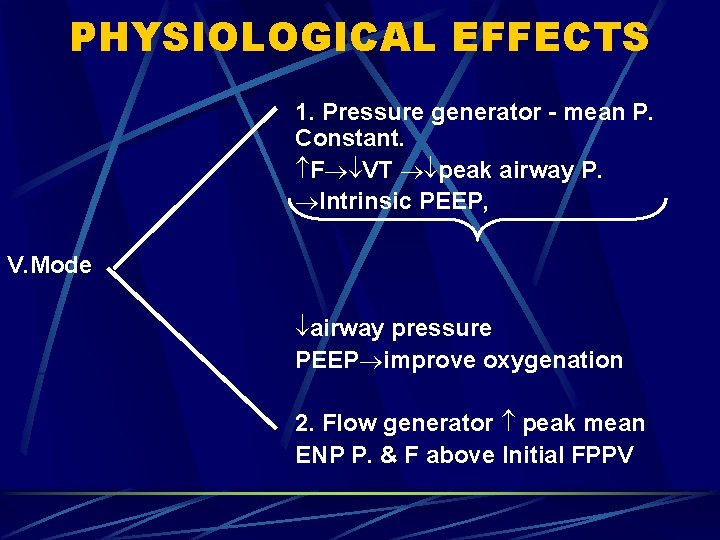
PHYSIOLOGICAL EFFECTS 1. Pressure generator - mean P. Constant. F VT peak airway P. Intrinsic PEEP, V. Mode airway pressure PEEP improve oxygenation 2. Flow generator peak mean ENP P. & F above Initial FPPV
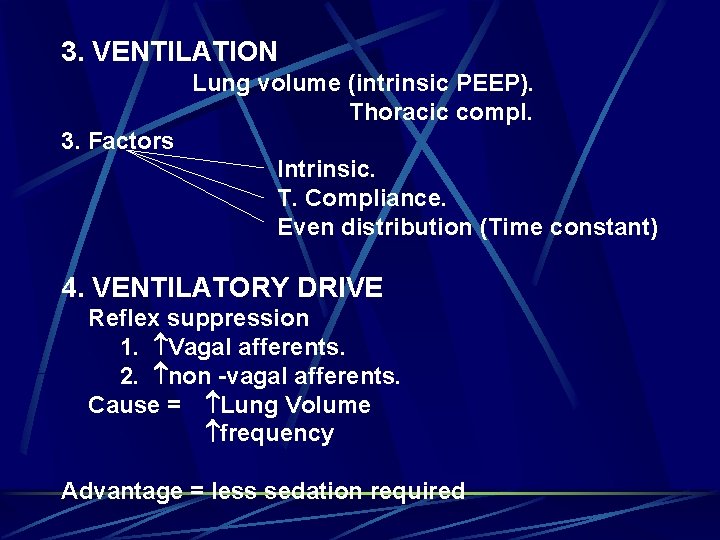
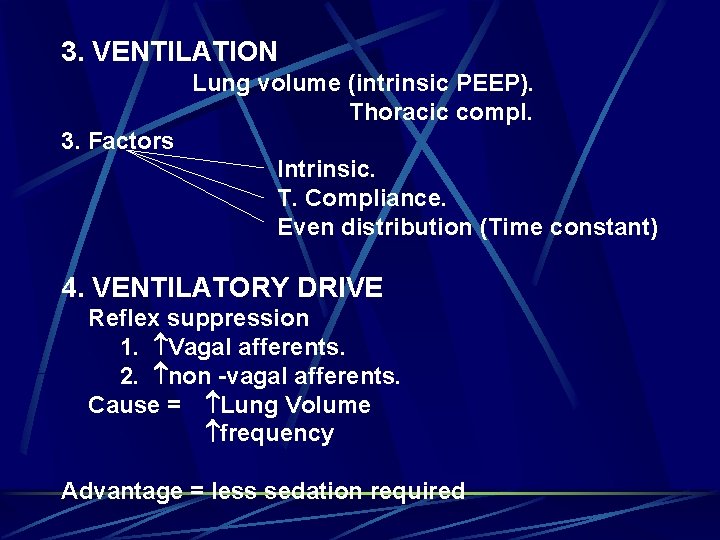
3. VENTILATION Lung volume (intrinsic PEEP). Thoracic compl. 3. Factors Intrinsic. T. Compliance. Even distribution (Time constant) 4. VENTILATORY DRIVE Reflex suppression 1. Vagal afferents. 2. non -vagal afferents. Cause = Lung Volume frequency Advantage = less sedation required
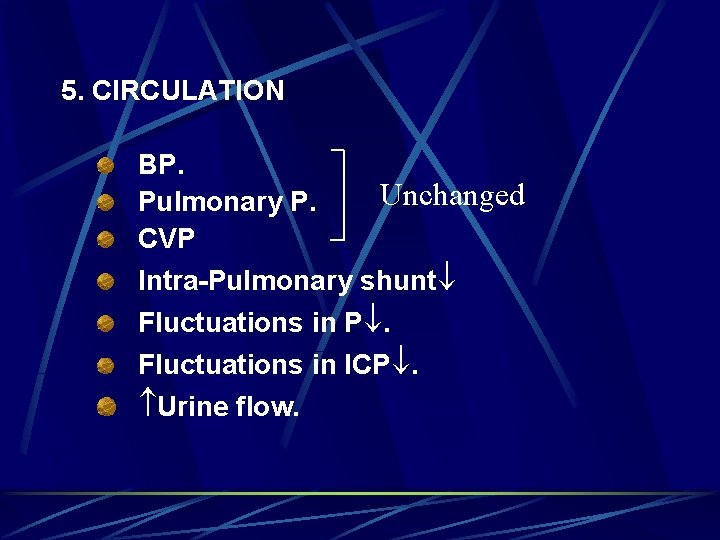
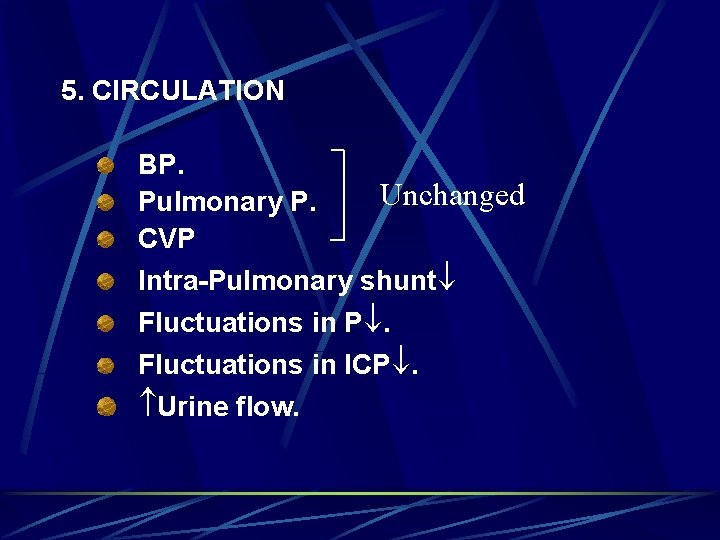
5. CIRCULATION BP. Unchanged Pulmonary P. CVP Intra-Pulmonary shunt Fluctuations in P. Fluctuations in ICP. Urine flow.
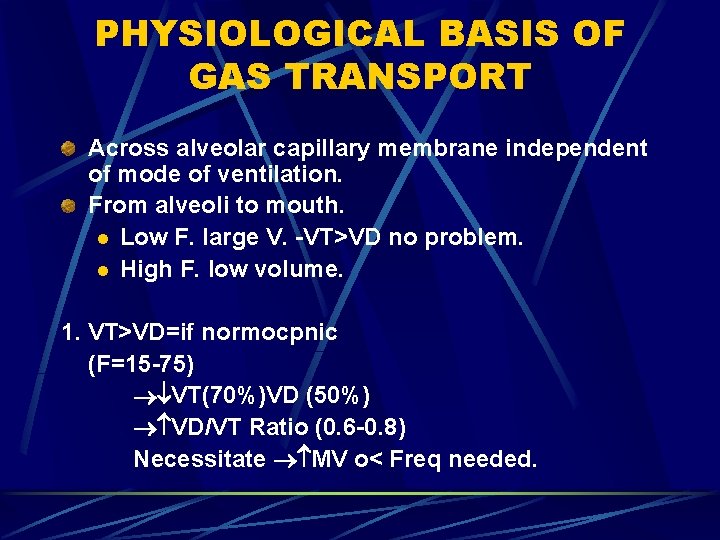
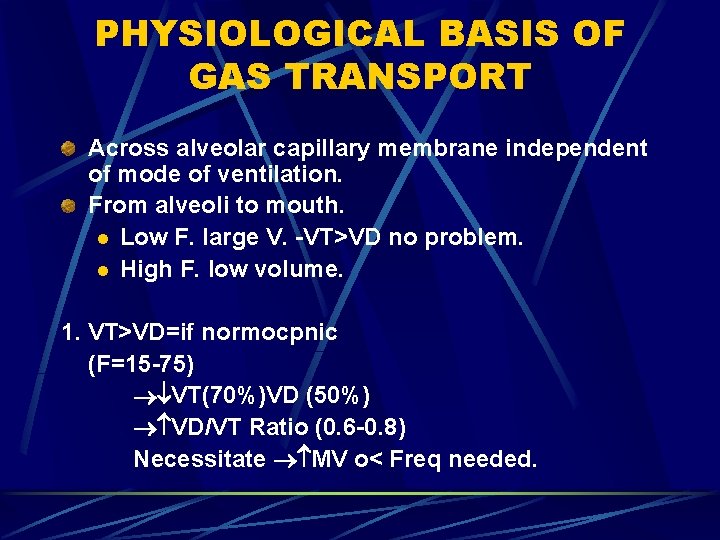
PHYSIOLOGICAL BASIS OF GAS TRANSPORT Across alveolar capillary membrane independent of mode of ventilation. From alveoli to mouth. l Low F. large V. -VT>VD no problem. l High F. low volume. 1. VT>VD=if normocpnic (F=15 -75) VT(70%)VD (50%) VD/VT Ratio (0. 6 -0. 8) Necessitate MV o< Freq needed.
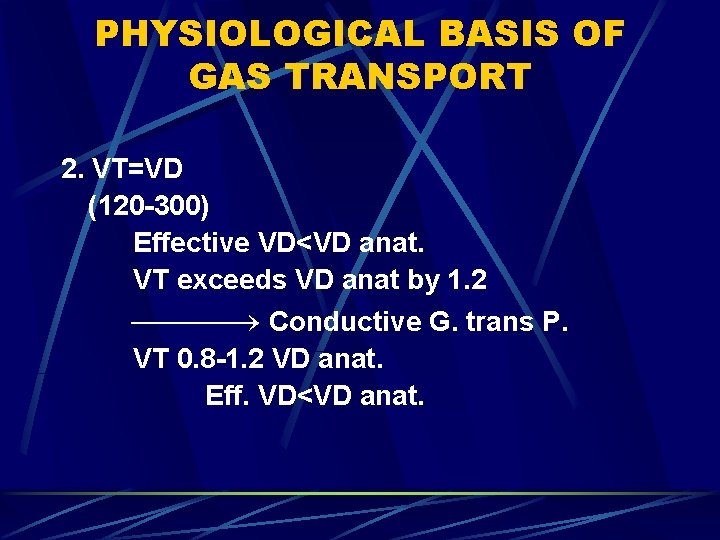
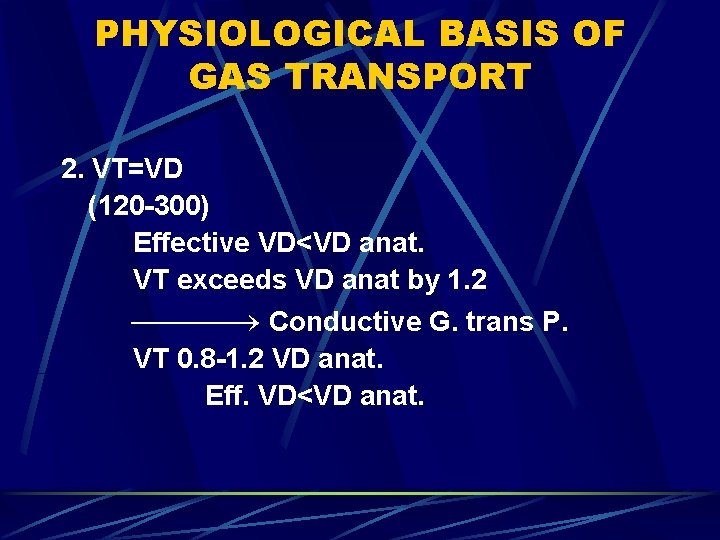
PHYSIOLOGICAL BASIS OF GAS TRANSPORT 2. VT=VD (120 -300) Effective VD<VD anat. VT exceeds VD anat by 1. 2 Conductive G. trans P. VT 0. 8 -1. 2 VD anat. Eff. VD<VD anat.
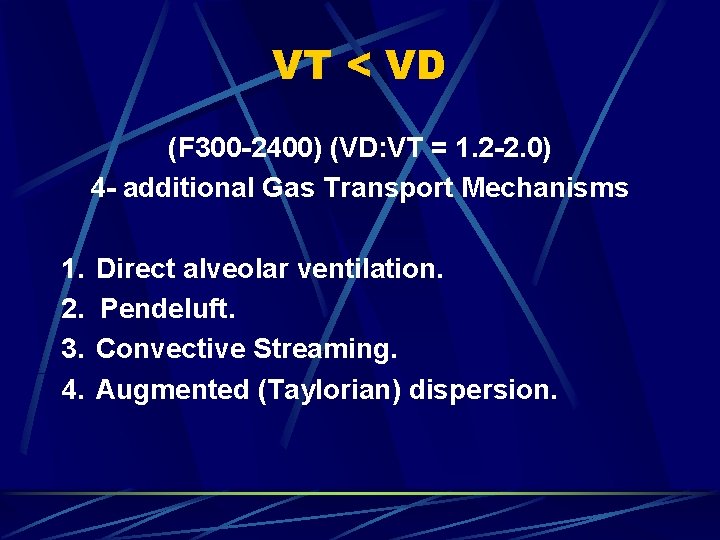
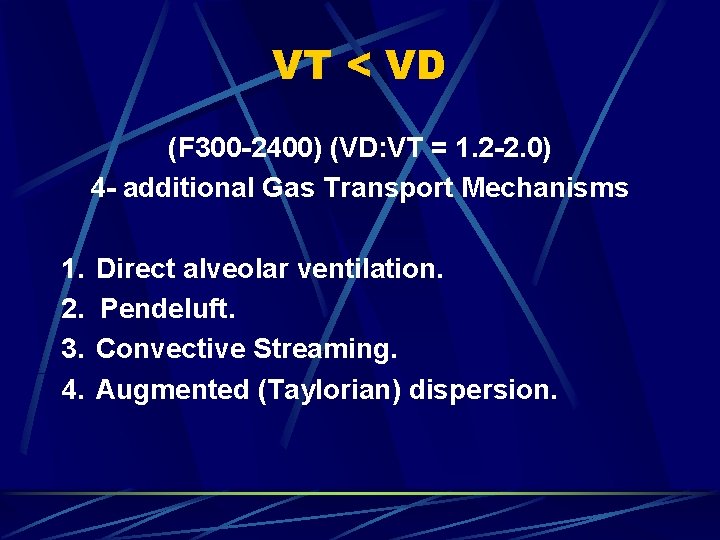
VT < VD (F 300 -2400) (VD: VT = 1. 2 -2. 0) 4 - additional Gas Transport Mechanisms 1. Direct alveolar ventilation. 2. Pendeluft. 3. Convective Streaming. 4. Augmented (Taylorian) dispersion.
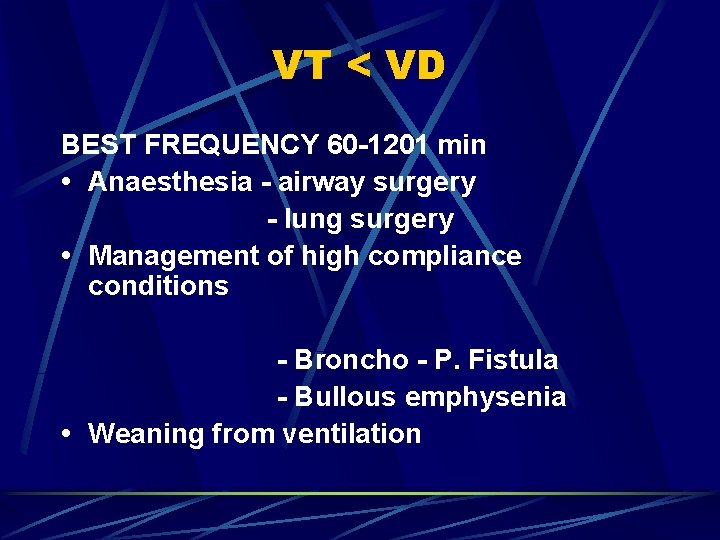
VT < VD BEST FREQUENCY 60 -1201 min • Anaesthesia - airway surgery - lung surgery • Management of high compliance conditions - Broncho - P. Fistula - Bullous emphysenia • Weaning from ventilation
CLINICAL APPLICATIONS 1. ANAESTHESIA a. Surgery on Conducting airways & Lungs b. Laryngoscopy, microsurgery, Laser surgery on larynx c. Tracheal resection & tracheostomy d. Bronchoscopy. 2. RESUSCITATION Percutaneous Trannstracheal Jet Ventilation with 100% O 2. - Direct delivery of 02 below cords. - Intrinsic PEEP. - Pulsatile Expired gas flow prevent aspiration.
CLINICAL APPLICATIONS 3. ICU Broncho-pleural fistula. 4. OTHER ADVANTAGES - Weaning - Endobronchial Sunction
DIFFERENTIAL LUNG V WHOLE – L. V. LOBAR – V. WHY DLV - NEEDED? Variable Time Constant l TC = R o< C l
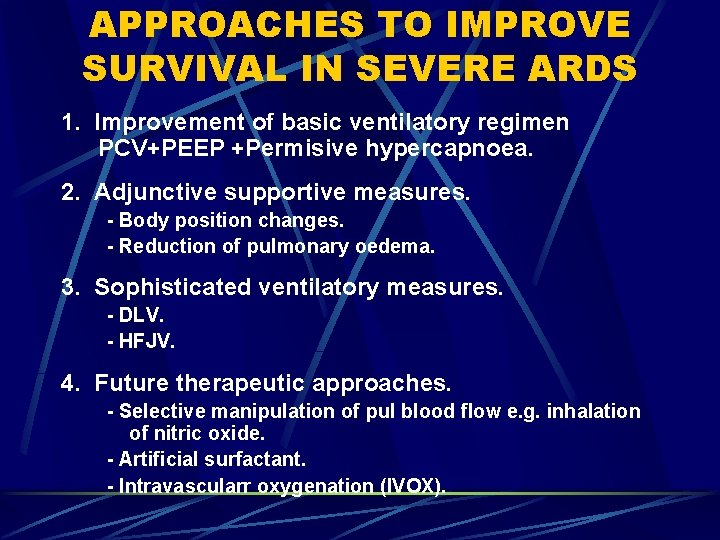
APPROACHES TO IMPROVE SURVIVAL IN SEVERE ARDS 1. Improvement of basic ventilatory regimen PCV+PEEP +Permisive hypercapnoea. 2. Adjunctive supportive measures. - Body position changes. - Reduction of pulmonary oedema. 3. Sophisticated ventilatory measures. - DLV. - HFJV. 4. Future therapeutic approaches. - Selective manipulation of pul blood flow e. g. inhalation of nitric oxide. - Artificial surfactant. - Intravascularr oxygenation (IVOX).
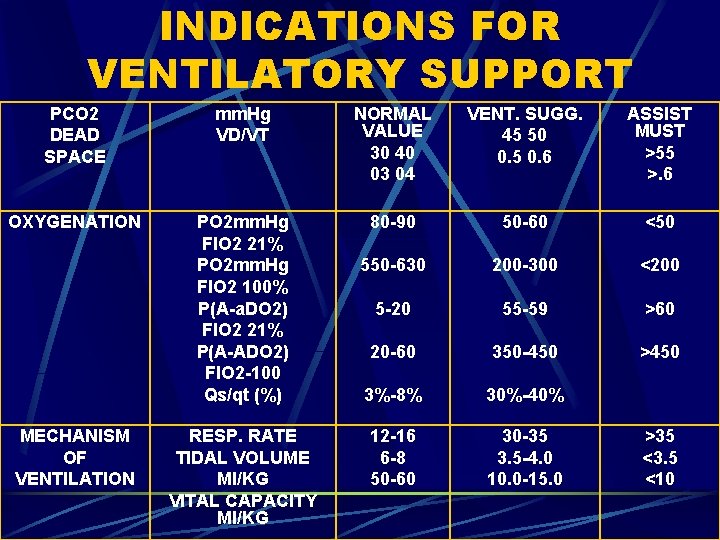
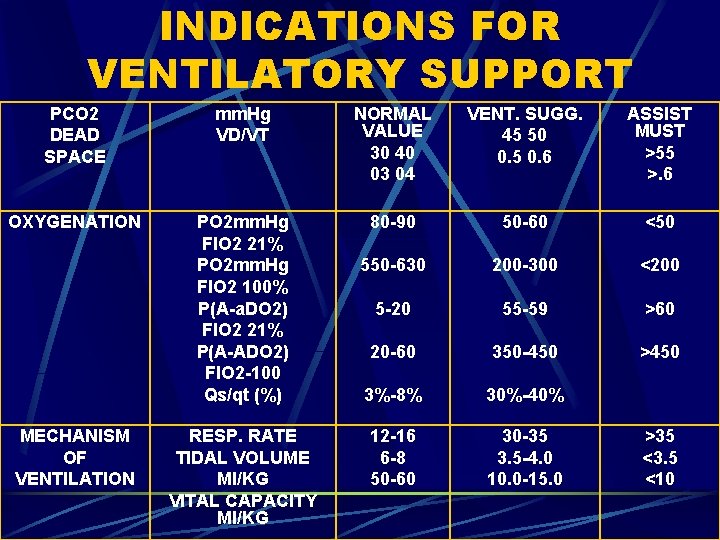
INDICATIONS FOR VENTILATORY SUPPORT PCO 2 DEAD SPACE mm. Hg VD/VT NORMAL VALUE 30 40 03 04 VENT. SUGG. 45 50 0. 5 0. 6 ASSIST MUST >55 >. 6 OXYGENATION PO 2 mm. Hg FIO 2 21% PO 2 mm. Hg FIO 2 100% P(A-a. DO 2) FIO 2 21% P(A-ADO 2) FIO 2 -100 Qs/qt (%) 80 -90 50 -60 <50 550 -630 200 -300 <200 5 -20 55 -59 >60 20 -60 350 -450 >450 3%-8% 30%-40% 12 -16 6 -8 50 -60 30 -35 3. 5 -4. 0 10. 0 -15. 0 MECHANISM OF VENTILATION RESP. RATE TIDAL VOLUME MI/KG VITAL CAPACITY MI/KG >35 <3. 5 <10
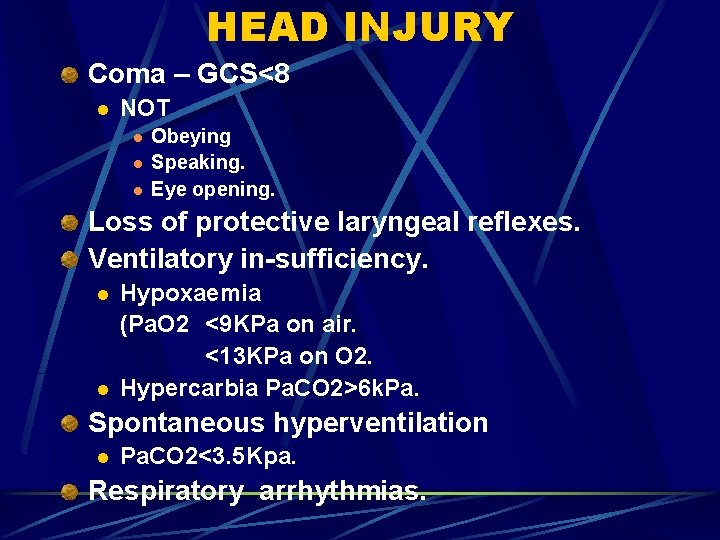
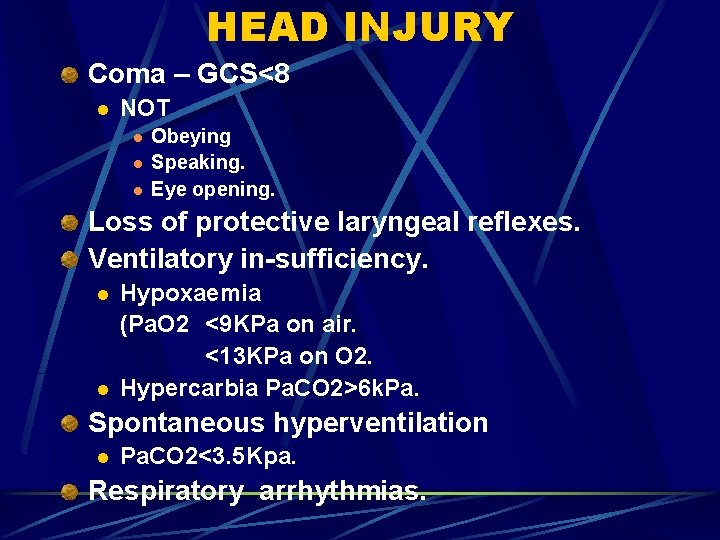
HEAD INJURY Coma – GCS<8 l NOT l l l Obeying Speaking. Eye opening. Loss of protective laryngeal reflexes. Ventilatory in-sufficiency. l l Hypoxaemia (Pa. O 2 <9 KPa on air. <13 KPa on O 2. Hypercarbia Pa. CO 2>6 k. Pa. Spontaneous hyperventilation l Pa. CO 2<3. 5 Kpa. Respiratory arrhythmias.
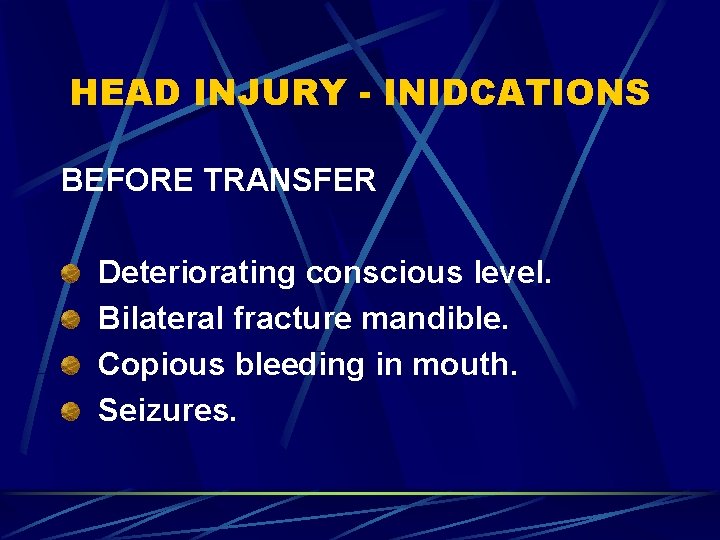
HEAD INJURY - INIDCATIONS BEFORE TRANSFER Deteriorating conscious level. Bilateral fracture mandible. Copious bleeding in mouth. Seizures.
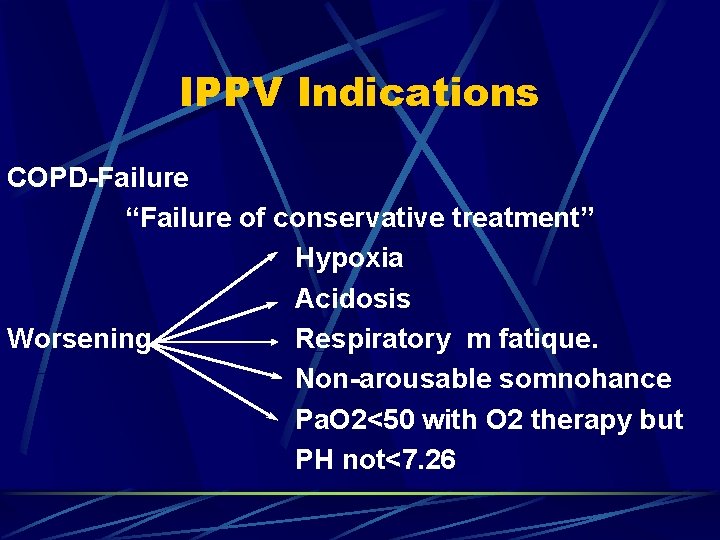
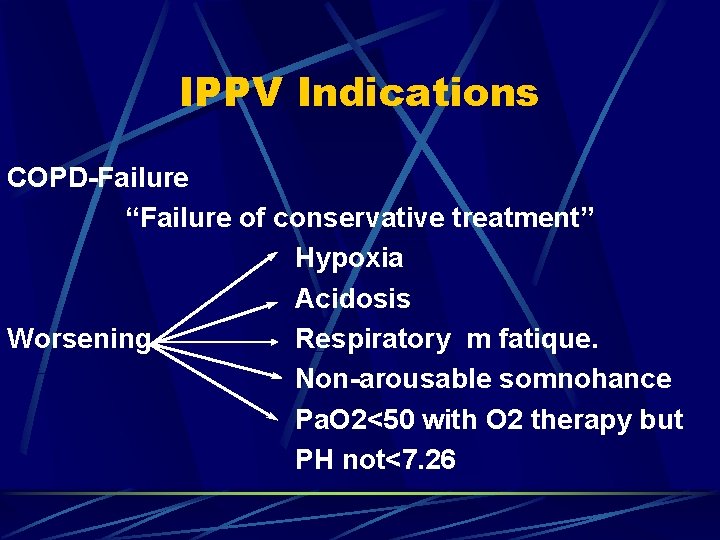
IPPV Indications COPD-Failure “Failure of conservative treatment” Hypoxia Acidosis Worsening Respiratory m fatique. Non-arousable somnohance Pa. O 2<50 with O 2 therapy but PH not<7. 26
CMV INITIATION Mode of ventilation. Inflation volume. Respiratory rate. Inspired O 2 level.
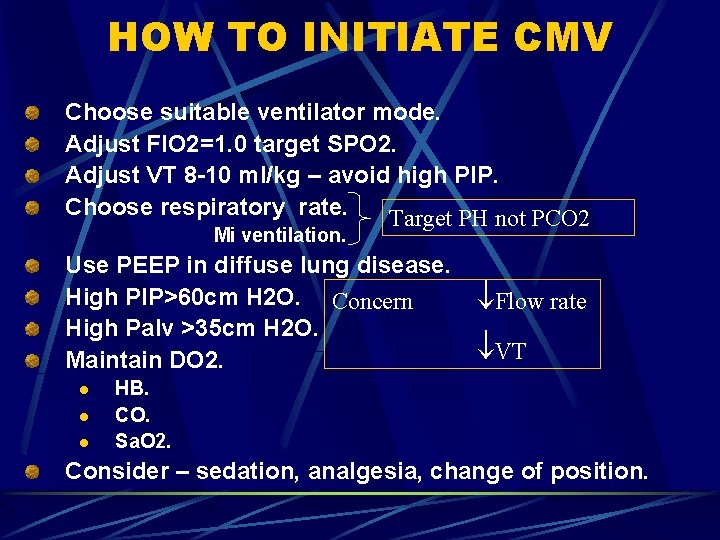
HOW TO INITIATE CMV Choose suitable ventilator mode. Adjust FIO 2=1. 0 target SPO 2. Adjust VT 8 -10 ml/kg – avoid high PIP. Choose respiratory rate. Target PH not PCO 2 Mi ventilation. Use PEEP in diffuse lung disease. High PIP>60 cm H 2 O. Concern High Palv >35 cm H 2 O. Maintain DO 2. l l l Flow rate VT HB. CO. Sa. O 2. Consider – sedation, analgesia, change of position.
GOALS Ensure-optimum O 2 delivery. Effective & appropriate ventilation. Decrease work of breathing.
PEEP Improve oxygenation. Improve gas exchange. l l Recruiting atelactasis. Recrutig non-functioning alveoli. Improve compliance. Improve FRC. Decrease shunt fraction. Decreases pulmonary oedema.
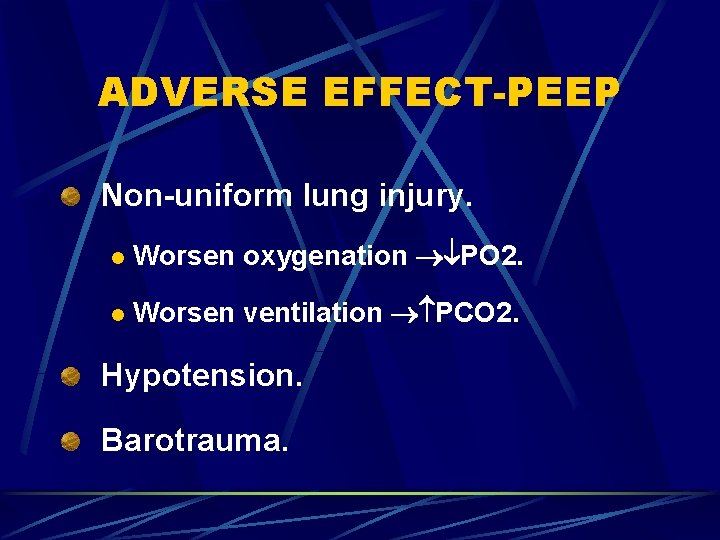
ADVERSE EFFECT-PEEP Non-uniform lung injury. l Worsen oxygenation PO 2. l Worsen ventilation PCO 2. Hypotension. Barotrauma.
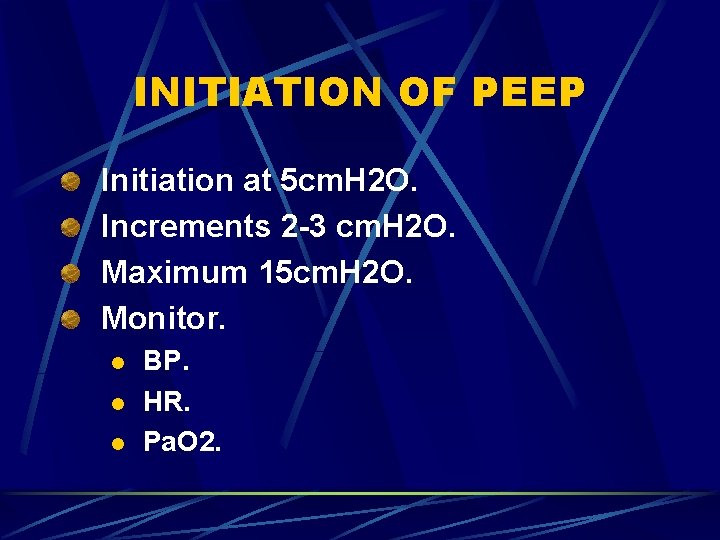
INITIATION OF PEEP Initiation at 5 cm. H 2 O. Increments 2 -3 cm. H 2 O. Maximum 15 cm. H 2 O. Monitor. l l l BP. HR. Pa. O 2.
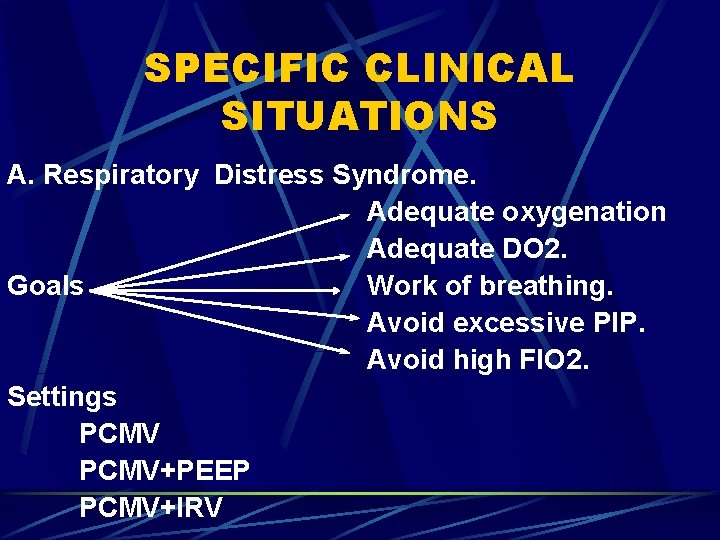
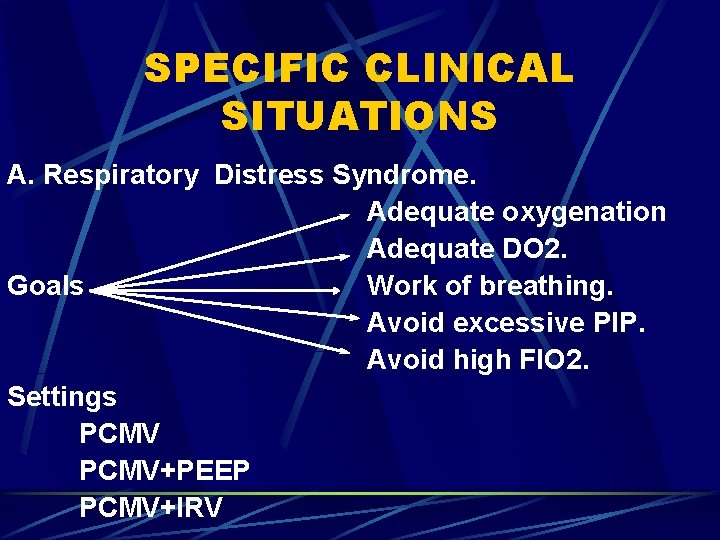
SPECIFIC CLINICAL SITUATIONS A. Respiratory Distress Syndrome. Adequate oxygenation Adequate DO 2. Goals Work of breathing. Avoid excessive PIP. Avoid high FIO 2. Settings PCMV+PEEP PCMV+IRV
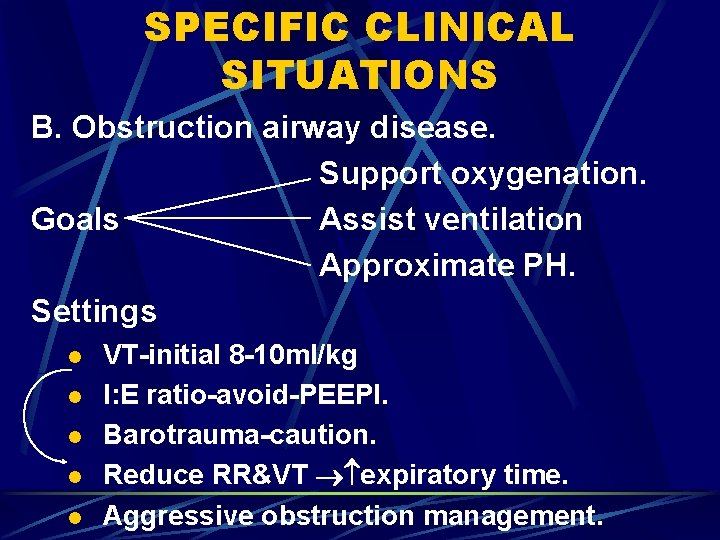
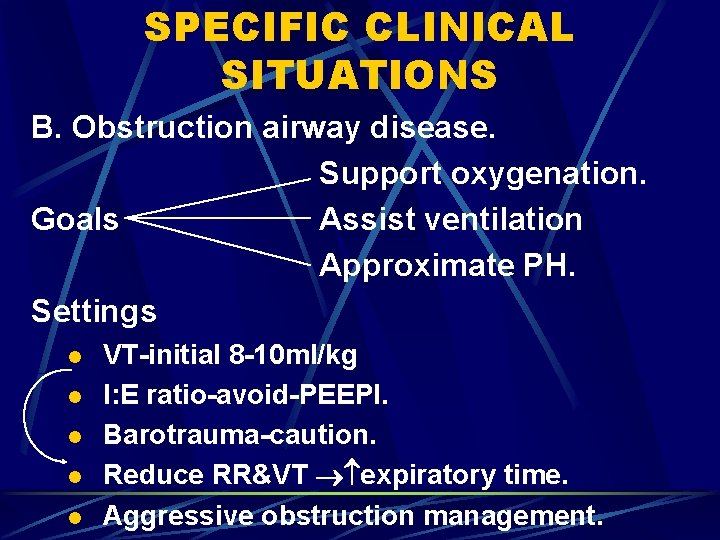
SPECIFIC CLINICAL SITUATIONS B. Obstruction airway disease. Support oxygenation. Goals Assist ventilation Approximate PH. Settings l l l VT-initial 8 -10 ml/kg I: E ratio-avoid-PEEPI. Barotrauma-caution. Reduce RR&VT expiratory time. Aggressive obstruction management.
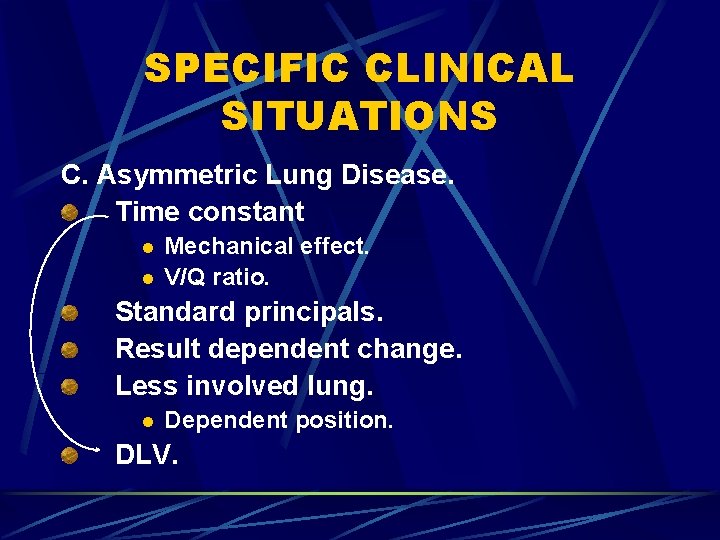
SPECIFIC CLINICAL SITUATIONS C. Asymmetric Lung Disease. Time constant l l Mechanical effect. V/Q ratio. Standard principals. Result dependent change. Less involved lung. l Dependent position. DLV.
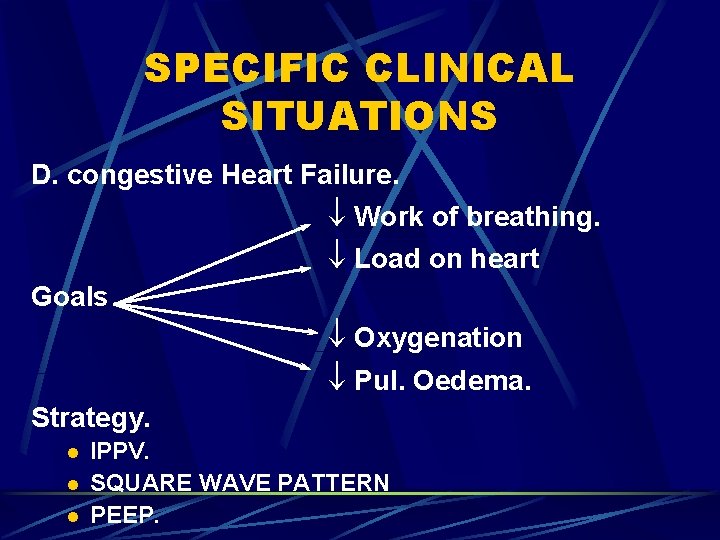
SPECIFIC CLINICAL SITUATIONS D. congestive Heart Failure. Work of breathing. Load on heart Goals Oxygenation Pul. Oedema. Strategy. l l l IPPV. SQUARE WAVE PATTERN PEEP.
SPECIFIC CLINICAL SITUATIONS E. Myocardial Ischaemia. Work of breathing. Goals DO 2 Strategy l As for CHF
SPECIFIC CLINICAL SITUATIONS F. Neuromuscular disease. “Intact respiratory drive” Higher VT: l l Avoid air hunger. Dyspnea sensation. 10 -12 ml/kg Ventilate - Normal PH.
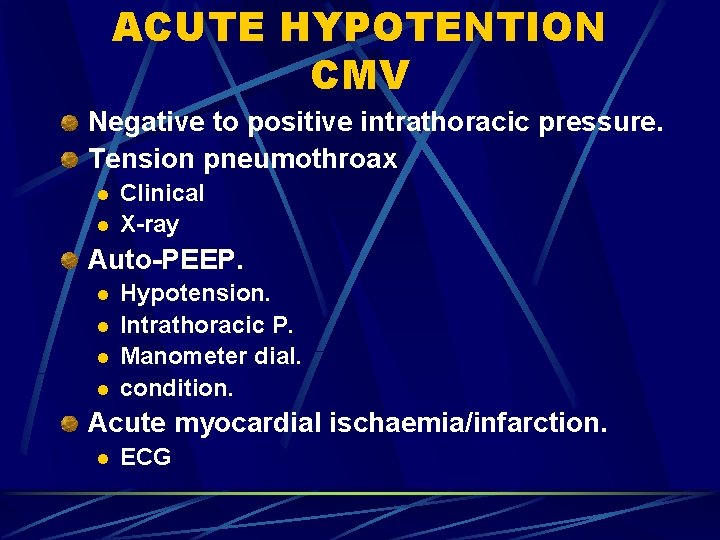
MONITORING CMV Chest radiograph. l l Post intubation. Deterioration. Blood gases. Vital signs. Inspiratory pressures. Pulse oxymetry. Ventilator alarms.
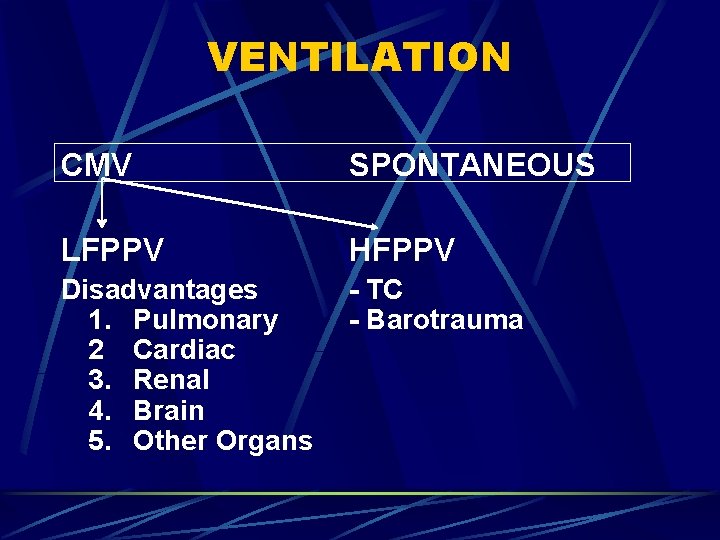
ACUTE HYPOTENTION CMV Negative to positive intrathoracic pressure. Tension pneumothroax l l Clinical X-ray Auto-PEEP. l l Hypotension. Intrathoracic P. Manometer dial. condition. Acute myocardial ischaemia/infarction. l ECG