Venous Thromboembolism Prophylaxis in Hospitalized Patients Robert Rubin
Venous Thromboembolism Prophylaxis in Hospitalized Patients Robert Rubin, MD, FACP Associate Program Director, Internal Medicine Residency Program Jewish Hospital, Mercy Health Cincinnati, Ohio
VTE, comprising pulmonary embolism and DVT, is a common clinical problem and is associated with substantial morbidity and mortality. Most hospitalized medical patients have at least 1 factor for VTE, and this is persistent for several weeks after discharge. 26% of patients with undiagnosed and untreated PE will have a subsequent fatal embolic event, whereas another 26% will have a nonfatal recurrent embolic event. Studies shows that between 5 and 10% of all in-hospital deaths are a direct result of PE While many epidemiologic studies report VTE rates, in the absence of prophylaxis, that range from 10 -80%, this radiates likely overestimated.
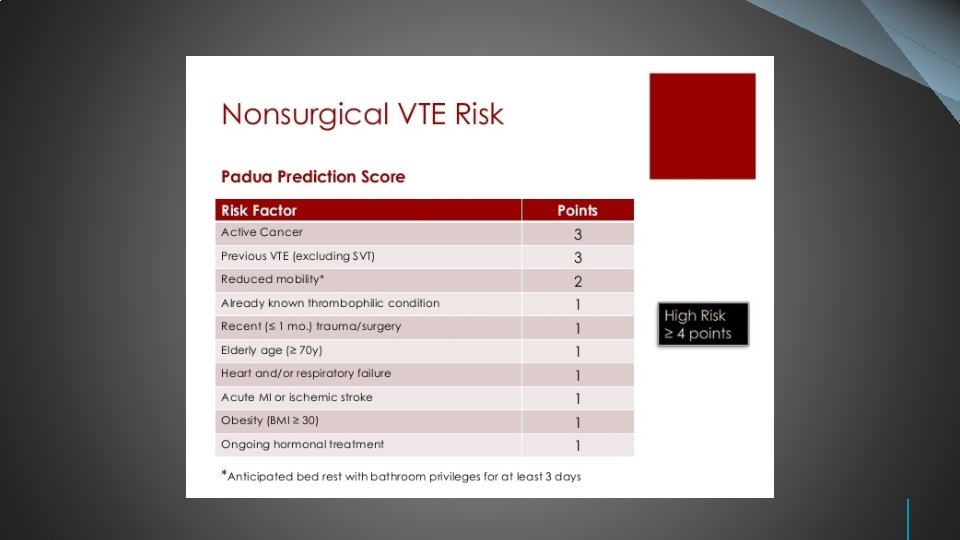
While thromboprophylaxis has been reported to reduce the risk of death in surgical patients, most studies and a meta-analysis haven’t been able to show a consistent benefit effect of thromboprophylaxis on mortality in hospitalized medical patients. ACP recommends assessment of the risk for thromboembolism and bleeding in medical (including stroke) patients prior to initiation of prophylaxis of the TEE Patients at highest risk of DVT include patients who are critically- ill, patients with cancer and stroke, and patients with multiple risk factors for VTE, including pregnancy, heart failure, myocardial infarction, old age (> 75 years), previous TTE, prolonged immobility, renal failure, obesity, and inherited or acquired hypercoagulable states.
Risk factors for bleeding with anticoagulant therapy: Female sex; older age; diabetes; hypertension; presence of cancer; acute or chronic alcoholism; liver disease; severe chronic kidney disease; peptic ulcer disease; anemia; poor treatment adherence; prior stroke or intracerebral hemorrhage; hasn’t soft bleeding lesions; bleeding disorders; and concomitant use of aspirin, NSAIDs, antibiotics, statins, fibroids, and steroids
Recommendation 2: ACP recommends pharmacologic prophylaxis with heparin or a related drugs for venous thromboembolism in medical ( including stroke ) patients unless that assessed risk for bleeding outweighs the likely benefits ( Grade: stronger recommendation, moderate–quality evidence). 10 trials ( N= 20717) evaluated medical patients without stroke. The results showed that compared with no heparin prophylaxis, heparin prophylaxis was not associated with a statistically significant reduced risk for mortality ( RR 0. 94); absolute reduction of PE- 4 events per 1000 patients treated, by increased risk for all bleeding events ( absolute increase 9 events per 1000 patients treated), although, it didn’t reach statistical significance. Heparin prophylaxis resulted in an absolute reduction of 2 fewer symptomatic DVTs per 1000 patients treated, although the difference wasn’t statistically significant. Recommended dosage of UFH: 5, 000 units every 8– 12 hours subcutaneously
Comparative effectiveness of LMWH vs UFH 9 trials ( n= 11650) that com pa red LM WH with UFH medi cal patient’s showed no sta tistically sign if icant difference in mortal ity ( RR 0. 9 1) a nd m ajor bleeding, although a nonsignificant dif f er ence favor ed LMWH for P E ( OR - 0. 6 7) Recommended dosages o f L MWH: - Enoxaparin ( Lovenox)- 40 mg su bcu taneously daily for 30 mg subcutaneously twice da ily - Dalteparin ( Fragmin)- 5000 u nits subcuta ne ously daily
Comparative effectiveness of mechanical devices versus no mechanical devices Evidence on clinical outcomes from randomized, controlled trials evaluating mechanical devices versus no mechanical devices is sparse. 3 trials included in the systematic review compared mechanical devices with no mechanical devices, but one large trial ( n= 2518 ) included 232 of the 247 deaths reported. Included patients with acute stroke and compared thigh- length graduated compression stockings with no stockings. The results showed no statistically significant difference in the risk for mortality ( RR-1. 11), symptomatic DVT, or PE. However, risk for lower extremity skin damage statistically significantly increased among the patients treated with compression stockings ( RR-4. 02; absolute increase– 39 events per 1000 patients treated) The 2 other studies showed no differences in the rates of PE or mortality. Recommendation 3: ACP recommended against the use of mechanical prophylaxis with graduated compression stockings for prevention of DVT ( Grade: stronger recommendation, moderate–quality evidence).
Special Considerations Low risk group patients: early ambulation with or without mechanical methods of thromboprophylaxis. Fondaparinux is used as an alternative to heparin for patient with heparin induced thrombocytopenia Patients, who have at least 1 risk factor for VTE ( moderate to high risk) and do not have an increased risk of bleeding, use pharmacologic thromboprophylaxis rather than mechanical methods or no prophylaxis. ( Grade 1 B) For most patients hospitalized with an acute medical illness with multiple recent factors for VTE, many experts administer more aggressive prophylaxis in the form of increased intensity of a pharmacologic agent 3 times at day UFH, twice daily enoxaparin) or the addition of a mechanical device. For patient with renal failure (creatinine clearance < 30 ml/min) or for those in whom cost is an issue, unfractionated heparin is a reasonable alternative.
Special Considerations For most patients hospitalized with an acute medical illness who have risk factors for DVT and who are at high risk of bleeding or in whom anticoagulation is contraindicated (eg, gastrointestinal or intracranial hemorrhage), mechanical methods of VTE prevention are suggested over no prophylaxis ( Grade 2 C). Among this methods, compression boots as the most common form of mechanical prophylaxis used. Transition to a pharmacologic agent should occur as soon as the bleeding reason becomes acceptably low all has been reversed.

Policy Implications ACP does not support the application of performance measures in medical (including stroke) patients that promotes universal venous thromboembolism prophylaxis regardless of risk
Q u e s t i o n 1 T h e p a t i e n t i s a 4 0 y e a r o l d m a l e w h o w a s a d m i t t e d t o t h e h o s p i t a l w i t h c h e s t p a i n. H e h a s a h i s t o r y o f m i l d d y s l i p i d e m i a a n d h e a r t b u r n. B P 1 2 5 / 8 0 m m H g. L a b w o r k i s n o r m a l. C a r d i a c e n z y m e s n e g a t i v e f o r a c u t e M I. E K G w a s n o r m a l. T h e p a t i e n t i s s c h e d u l e d f o r t r e a d m i l l c a r d i a c s t r e s s t e s t a n d 2 D E c h o. W h a t i s t h e b e s t a p p r o a c h f o r V T E p r o p h y l a x i s ? A. B. C. D. Enoxaparin 40 mg subcutaneously daily Heparin 5, 000 U subcutaneously every 8 hours. Anti-thrombotic pneumatic boots (SCD) No prophylaxis needed. The Power of Power. Point | thepopp. com 1 2
ANSWER: A. Enoxaparin 40 mg subcutaneously daily B. Heparin 5, 000 U subcutaneously every 8 hours. C. Anti-thrombotic pneumatic boots (SCD) D. No prophylaxis needed. 1 3
Q u e s t i o n 2 M s. G i s a 7 5 y e a r o l d f e m a l e a d m i t t e d t o t h e h o s p i t a l w i t h r i g h t s i d e d l o w e r l o b e p n e u m o n i a. S h e h a s a h i s t o r y o f i n s u l i n d e p e n d e n t D M t y p e 2 , m i l d o b e s i t y ( B M I 3 2 ) , C K D s t a g e 4 , a n d c h r o n i c d i a s t o l i c h e a r t f a i l u r e. H e r l a b s a r e c o n s i s t e n t w i t h W B C – 1 4 , 0 0 0 , H b – 1 0 , H c t – 3 0 , B u n – 3 0 , s e r u m c r e a t i n e 2. 6. H e r w e i g h t i s 6 8 k g. W h a t i s t h e b e s t a p p r o a c h f o r V T E p r o p h y l a x i s ? A. B. C. D. Enoxaparin 40 mg subcutaneously daily Heparin 5, 000 U subcutaneously every 8 hours. Anti-thrombotic pneumatic boots (SCD) No prophylaxis needed. The Power of Power. Point | thepopp. com 1 4
ANSWER: A. Enoxaparin 40 mg subcutaneously daily B. Heparin 5, 000 U subcutaneously every 8 hours. C. Anti-thrombotic pneumatic boots (SCD). D. No prophylaxis needed. 1 5
- Slides: 15