Venous Cannulation Learning Resource Aim and Learning Outcomes
- Slides: 35
Venous Cannulation Learning Resource • • Aim and Learning Outcomes Overview – what do you need to do NDHB Learning Handout BD Interactive Learning Module Resource Articles Self Test Competency Assessment Tool Version 1 – February 2009
Aim: To provide registered nurses with the knowledge and skills to safely perform venous cannulation Learning Outcomes On completion of the readings and practice session the nurse will be able to: – Describe rationale for selection of cannulation device – Discuss criteria for vein selection – Demonstrate selection of veins – Discuss potential complication, causes and nursing actions – Demonstrate safe cannulation technique Version 1 – February 2009
Overview What do you need to do? • • Discuss with your manager and educator – is this right for you right now? Read through the training handout Work through the “Interactive learning module – produced by BD Medical - Medical Surgical Systems Read the resource articles Complete the Self Test Book in for a practise and training session with your Venous Cannulation Link nurse Develop expertise by performing cannulation supported by your Link nurse or a credentialed peer Be signed off as competent, using the competency assessment Tool CHECKLIST – PRINT AND TAKE TO YOUR TRAINING SESSION Version 1 – February 2009
BD Interactive Learning Module Click here • • Scroll down Double click on “Interactive Inservice Module Click “next” at bottom to go to next slide Note: video may take a minute to load – be patient Version 1 – February 2009
Resource Articles • Hadaway, L. C. , & Millam, D. A. (2003). On the road to successful I. V. starts. Nursing 2003, 33 (1), 1 -14. • Ingram, P. , & Lavery, I. (2007). Peripheral intravenous cannulation: safe insertion and removal technique. Nursing Standard, 22 (1), 44 -48. • Lavery, I. , & Ingram, P. (2005). Venepuncture: best practice. Nursing Standard. 19, (49) 55 -65. • Lavery, I. , & Ingram, P. (2006). Prevention of infrection in peripheral intravenous devices. Nursing Standard. 20, (49) 49 -56. • Scales, K. (2005). Vascular access: a guide to peripheral venous cannulation. Nursing Standard, 19 (49), 48 -52. Version 1 – February 2009
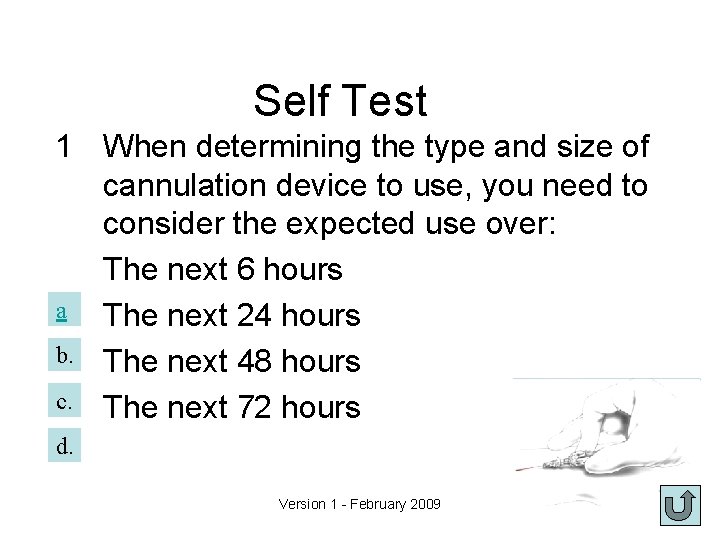
Self Test 1 When determining the type and size of cannulation device to use, you need to consider the expected use over: The next 6 hours a The next 24 hours b. The next 48 hours c. The next 72 hours d. Version 1 - February 2009
• No, when determining size, consider the fluid type expected to be used over the next 72 hours. This may prevent an additional venepuncture. Always use the smallest needle/cannula that you can to reduce the risk of phlebitis Version 1 - February 2009
• Yes! When determining size, consider the fluid type expected to be used over the next 72 hours. This may prevent an additional venepuncture. Always use the smallest needle/cannula that you can to reduce the risk of phlebitis Version 1 - February 2009
2 For an adult patient going to surgery, who may require blood, your best choice of cannula size would be: a. b. c. d. 22 g 24 g 20 g 18 g Version 1 - February 2009
• No, an 18 g is recommended for surgical patients and for blood administration (Although blood can be given through smaller catheters, it flows better through a larger lumen). Version 1 - February 2009
• Yes! • An 18 g is recommended for surgical patients and for blood administration (Although blood can be given through smaller catheters, it flows better through a larger lumen). Version 1 - February 2009
3 Veins below a previous IV insertion site should be avoided for: a. b. c. d. 12 hours 24 hours 48 hours 72 hours Version 1 - February 2009
No, veins below a previous IV insertion sites should be avoided for 72 hours Version 1 - February 2009
Yes! Veins below a previous IV insertion site should be avoided for 72 hours Version 1 - February 2009
4 A vein should be at least ______of the diameter of the cannula to be used. a. b. c. d. the same diameter twice the diameter three times the diameter as large as possible Version 1 - February 2009
No, the vein should be twice the diameter of the cannula to be used. First determine the size of cannula required, and then choose the vein. Version 1 - February 2009
Yes! The vein should be twice the diameter of the cannula to be used. First determine the size of cannula required, and then choose the vein. Version 1 - February 2009
5 When choosing a vein to cannulate, avoid: a. Joints, straight veins, areas of skin inflammation b. Joints, distal veins, arms with an artreriovenous shunt c. Joints, areas of skin inflammation, veins below previous IV insertion sites, arms with an artreriovenous shunt d. Distal veins, straight veins, hand veins Version 1 - February 2009
• No, straight, distal veins are recommended. Hand veins, being distal, can be used if they are large enough to accommodate the cannula required. Version 1 - February 2009
Yes! AVOID – – – Veins below a previous IV site (for 72 hours). Veins below a phlebotic area. Areas of skin inflammation, bruising. Joints. Arms affected by mastectomy, arteriovenous shunt. Anterior aspect of forearm. Version 1 - February 2009
6. Tourniquets should be placed _____above the intended insertion site. a. 2 cm b. as close as possible c. 5 cm d. 10 -15 cm Version 1 - February 2009
• No, apply the tourniquet 10 - 15 cm above intended insertion site. Apply snugly to trap venous blood, without occluding the pulse. Version 1 - February 2009
Yes! Apply the tourniquet 10 - 15 cm above intended insertion site. Apply snugly to trap venous blood, without occluding the pulse. Version 1 - February 2009
7 The BD cannula should be inserted through the skin at an angle of_______. a. b. c. d. 5 -10º 15 -30º 45º 90º Version 1 - February 2009
No, insert over the needle cannula at 1530° angle with bevel up. As soon as flash back of blood observed, lower the angle to skin level. Version 1 - February 2009
Yes! Insert over the needle cannula at 15 -30° angle with bevel up. As soon as flash back of blood observed, lower the angle to skin level. Version 1 - February 2009
8 Potential causes of phlebitis include: 1. tourniquet applied incorrectly 2. puncturing the back of vein 3. site not changed regularly (72 -96 hr) 4. vein too small for cannula a. b. c. d. 1 and 2 2 and 3 1 and 3 3 and 4 Version 1 - February 2009
No, Phlebitis Potential Causes • Needle/cannula size inappropriate Nursing Action • Use large cannula/needle for caustic medication. Choose vein twice the diameter of • Site not changed regularly cannula/needle. • Peripheral IV sites should be changed every 72 -96 hours. DO NOT wait for redness to appear, by then it is too late. Version 1 - February 2009
Yes! Phlebitis Potential Causes • Needle/cannula size inappropriate Nursing Action • Use large cannula/needle for caustic medication. Choose vein twice the diameter of • Site not changed regularly cannula/needle. • Peripheral IV sites should be changed every 72 -96 hours. DO NOT wait for redness to appear, by then it is too late. Version 1 - February 2009
9 Nursing actions that can reduce the potential for extravasation (tissuing) include: a. b. c. d. Stablising the cannula well NOT placing over a joint Entering the vein at 15 -30º All of the above Version 1 - February 2009
Yes Potential Causes • Needle/Cannula dislodged from vein • Vein doesn’t seal around cannula/needle Nursing Action • Don’t place over a joint. • Stabilise cannula well. • Observe regularly for oedema, coolness, tenderness. • Enter vein at 15 -30° angle to reduce cutting of vein wall fibres. Version 1 - February 2009
10 Peripheral IV site and dressing should be changed every: a. b. c. d. 24 – 48 hours 72 – 96 hours 5 – 7 days only when redness appears Version 1 - February 2009
No, Change IV site and dressing Q 72 - 96 hours. Observe site 8 hourly, change dressing as needed. Change IV site at first sign of redness, inflammation even if less than 72 hours. Version 1 - February 2009
Yes! Change IV site and dressing Q 72 - 96 hours. Observe site 8 hourly, change dressing as needed. Change IV site at first sign of redness, inflammation even if less than 72 hours. Version 1 - February 2009
The end • Have you read the resource articles? • Have you read through the BD interactive learning module? • Have you booked into a practice session? • Print off check list • Fill in • Take with you to your practice session Version 1 - February 2009