VENOUS AND LYMPHATICS DISEASES DR USMAN QURESHI SURGICAL
















- Slides: 78
VENOUS AND LYMPHATICS DISEASES DR USMAN QURESHI SURGICAL UNIT-1 1
presentation outlines • Intoduction • Venous and lymphatic drainage of extermities. • Pathophysiology and Mx of specific venous diseases. . Varicose vein. Chronic venous insufficiency. Deep vein thrombosis • Diseases of lymphatic system. 2
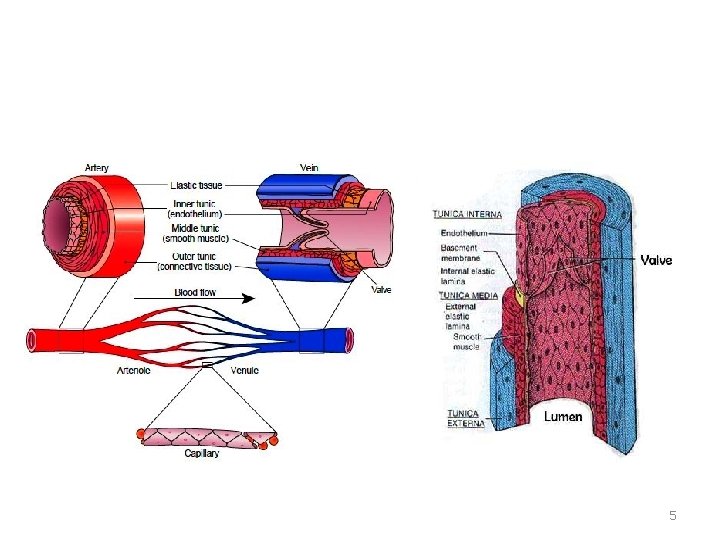
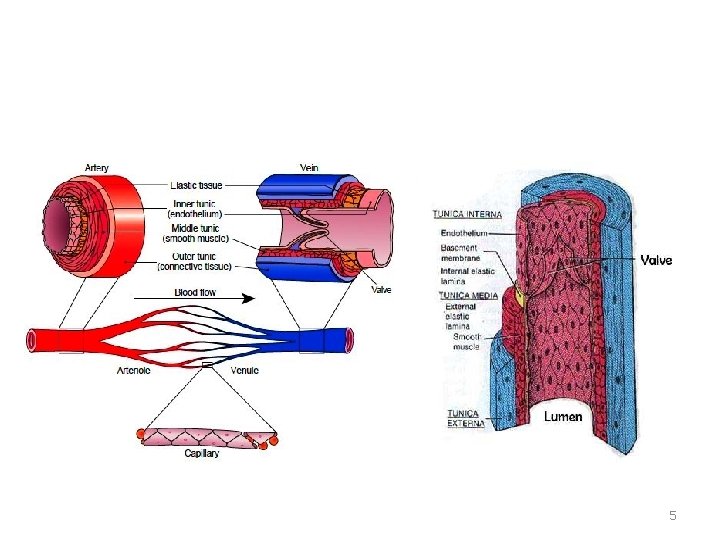
• Introduction VEINS • Huge capacitance vessels containing approximately 2/3 rd of all systemic blood. • Have larger diameters, larger lumina, and thinner, less wellorganized walls . • Low pressure and flow velocities. 3
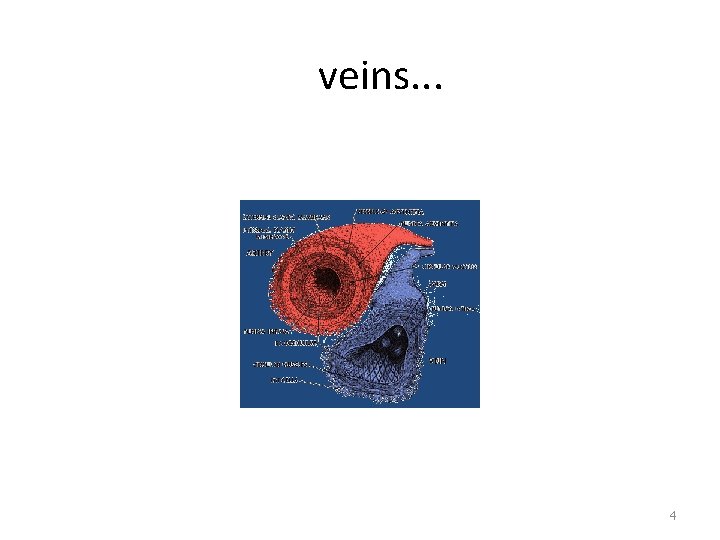
veins. . . 4
5
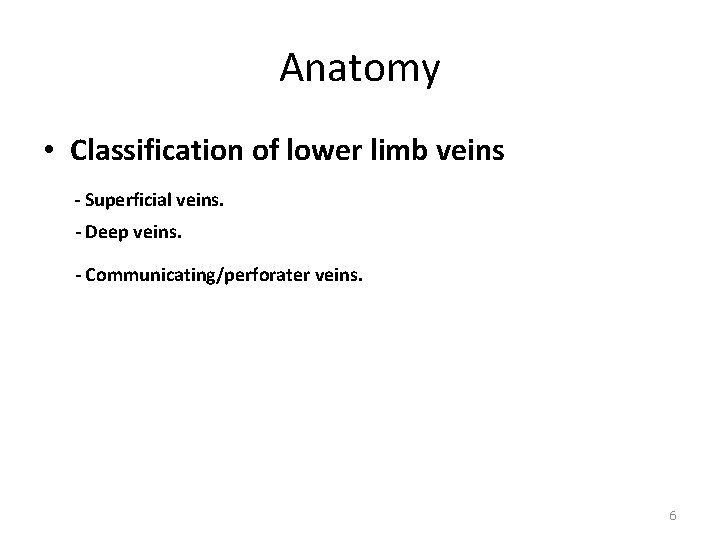
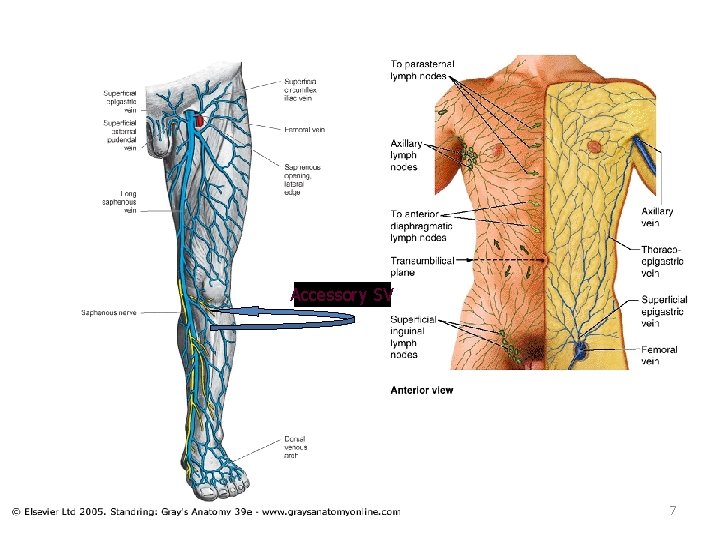
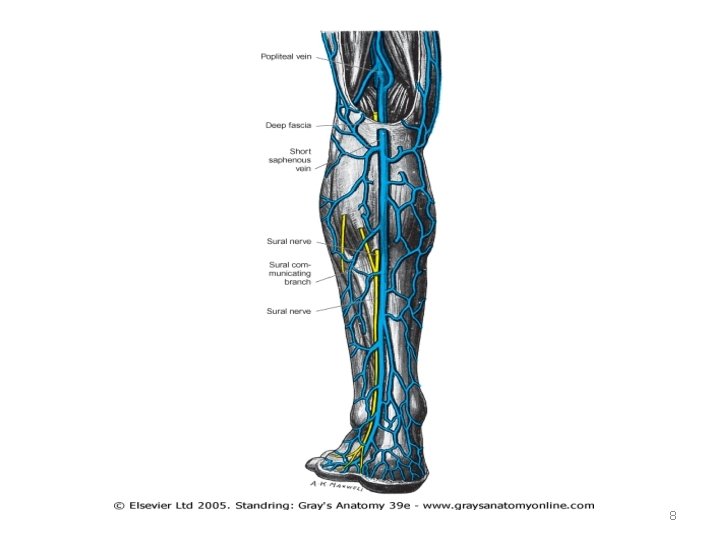
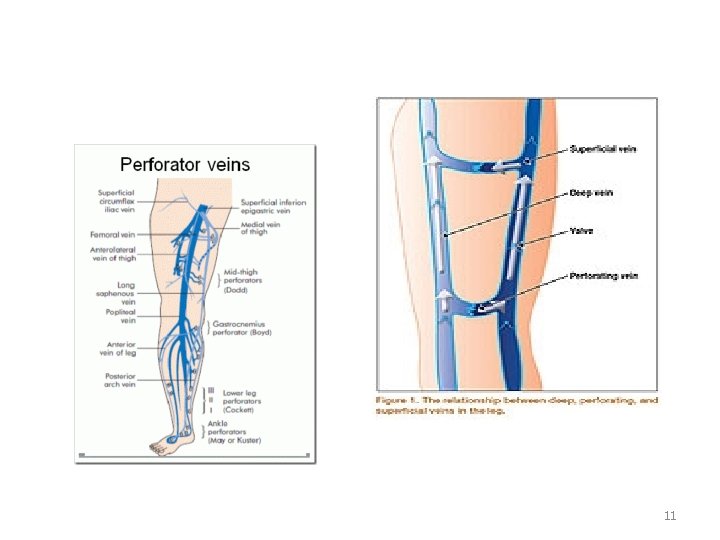
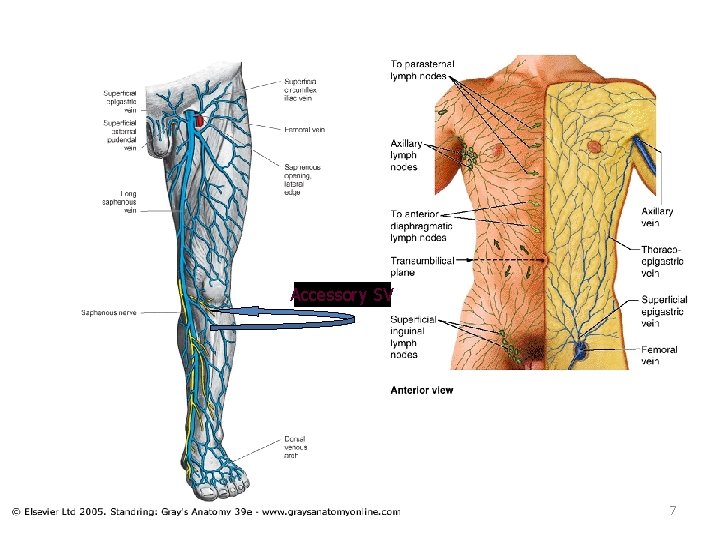
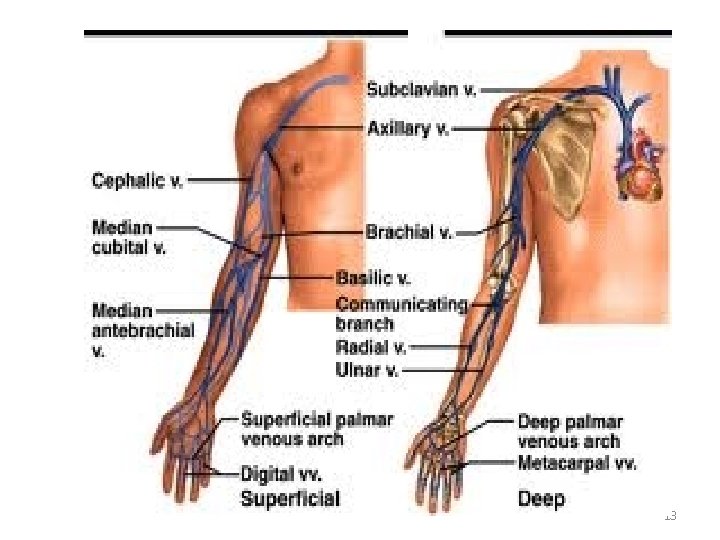
Anatomy • Classification of lower limb veins - Superficial veins. - Deep veins. - Communicating/perforater veins. 6
Accessory SV 7
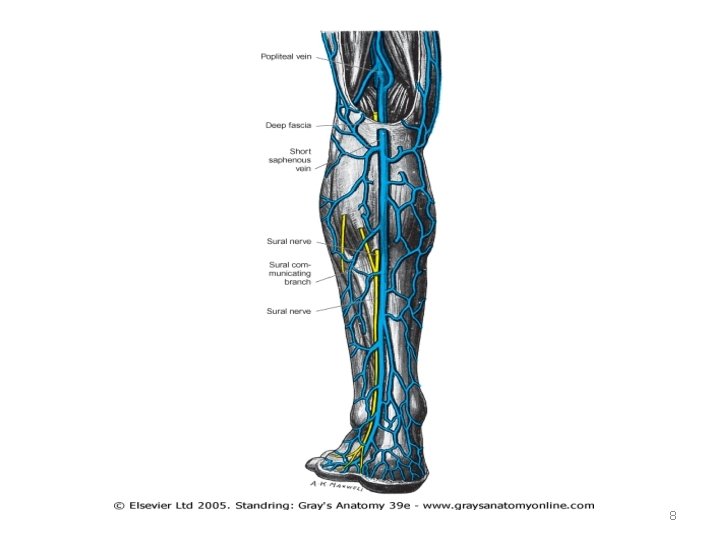
8

9
PERFORATORS Types • Direct -GSV/LSV -small perforators • Indirect 10
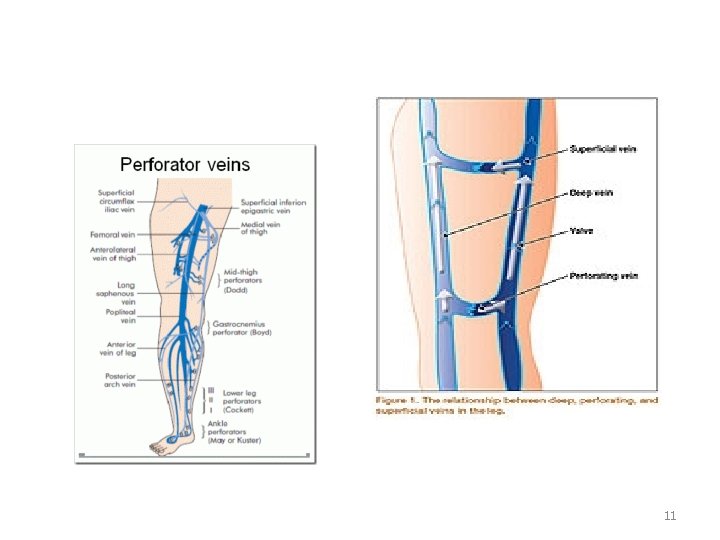
11

12
13
14
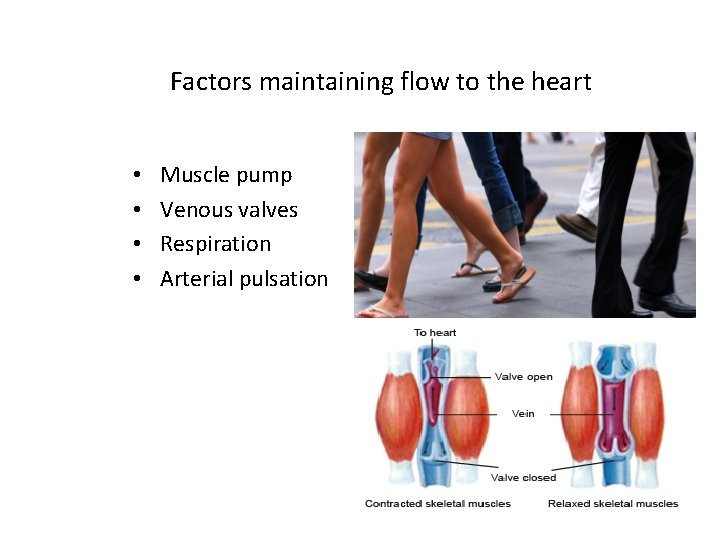
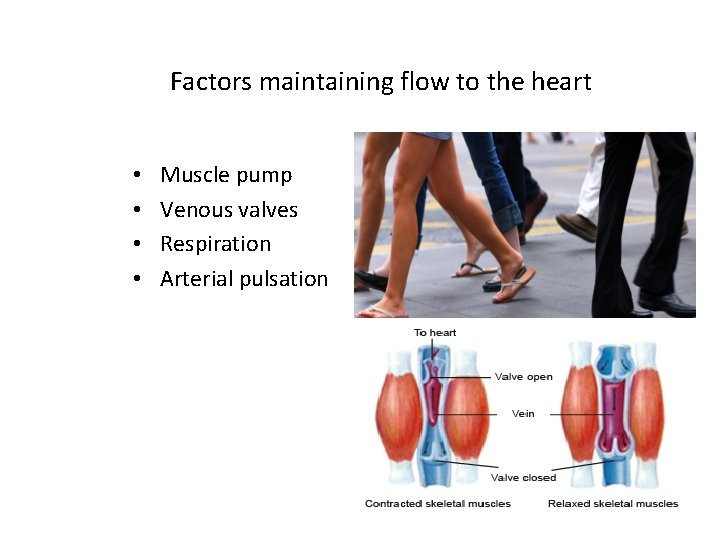
Factors maintaining flow to the heart • • Muscle pump Venous valves Respiration Arterial pulsation 15
Varicose Veins • Varicose veins are a common medical condition present in at least 10% of the general population. • VARICOSE VEINS ARE – DILATED – TORTUOUS AND – ELONGATED VEINS 16
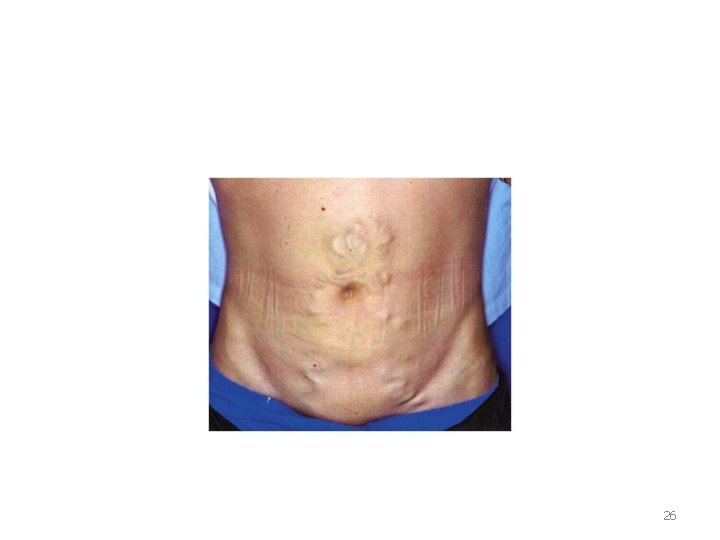
COMMON SITES OF VARICOSE VEINS • superficial venous system of lower limb • spermatic veins (VARICOCELE) • sites of porto-systemic anastomosis - OESOPHAGEAL VARICES -HAEMORRHOIDAL VARICES -AROUND UMBILICUS(CAPUT MEDUSAE) -BARE AREA OF LIVER -RETROPERITONEAL REGION 17
• varicose veins are menifestation of an underlying disease process not disease by itself. • Represent enlarged collaterals of saphenous venous system affected by disease called SUPERFICIAL VENOUS INSUFFICIENCY OF LOWER EXTREMITIES 18
Pathophysiology of Varicose Veins: 1 - Defects in the strength and characteristics of the venous wall 2 - Anatomic differences in the location of the superficial veins 3 - Intrinsic competence or incompetence of the valve system -saphenous vein and its tributaries/perforating veins 19
Pressure studies show that two sources of venous hypertension exist. 1 - hydrostatic pressure • Gravitational and is a result of venous blood coursing in a distal direction down linear axial venous segments • Weight of the blood column from the right atrium • Highest pressure is generated in ankle and foot. 2 - hydrodynamic pressure • Generated by force of muscular contraction in lower leg. 20

causes Primary l Congenital abnormality, most common cause. • Secondary l Factors that raises intra-abdominal pressure or raises pressure in superficial/deep venous system. Pregnancy. Abdominal/pelvic mass l Ascites l obesity l constipation l thrombosis of leg veins l long periods of time standing • 21
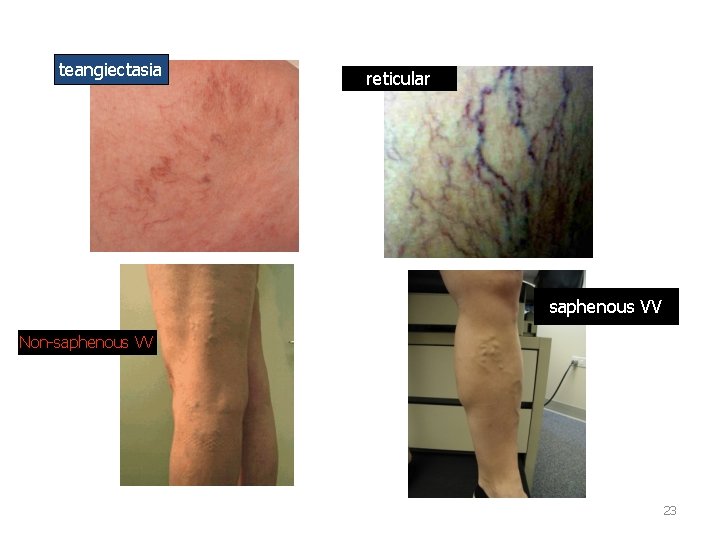
clinical features: • Dilated and tortuous veins, telangiectasias and fine reticular varicosities. • Pain, heaviness, tiredness of legs • Itching, dermatitis, hyperpigmentation • Thrombophlebitis, lipodermatosclerosis, skin ulceration, bleeding, blood lipodermatosclerosis, clots • All increase with dependency, resolve with leg elevation or compression 22
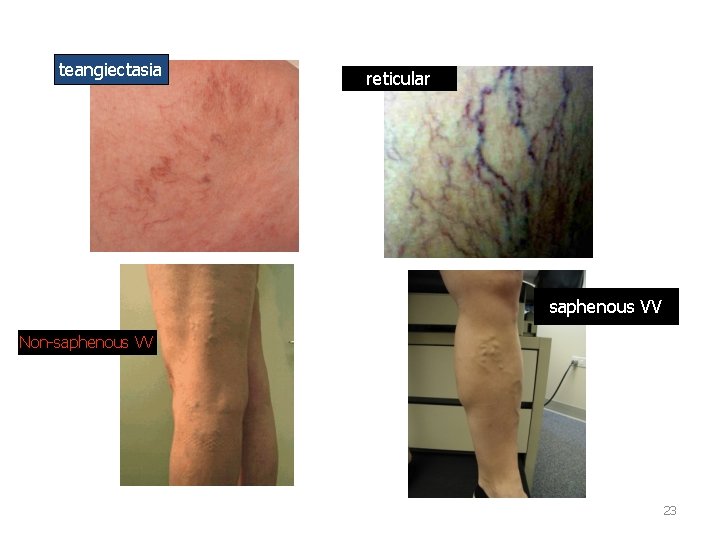
teangiectasia reticular saphenous VV Non-saphenous VV 23

*Image via Bing 24

*Image via Bing 25
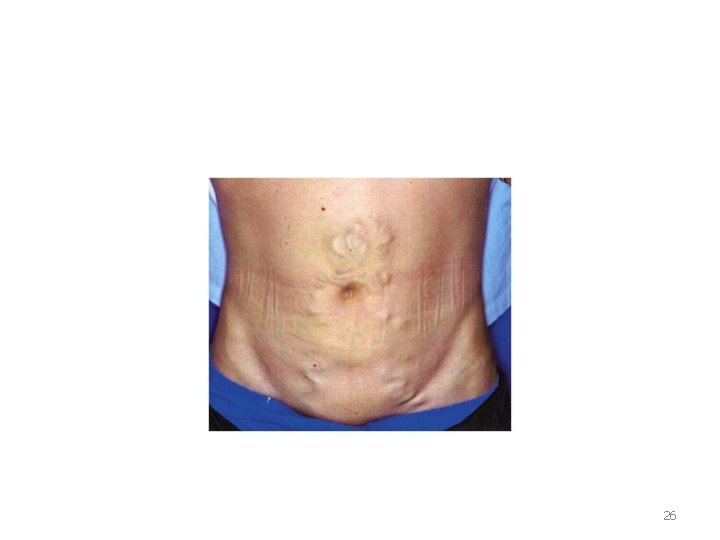
26

clinical evaluation • • Position-standing Examine from all sides Inspection of the vein Site and extent Skin overlying the varices and medial 1/3 rd of lower leg. Cough impulse Inspection of lower anterior abdominal wall 27
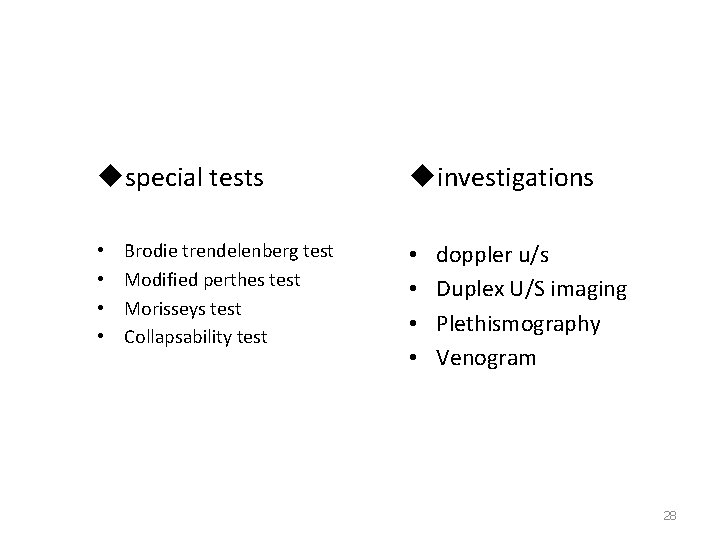
uspecial tests • • Brodie trendelenberg test Modified perthes test Morisseys test Collapsability test uinvestigations • • doppler u/s Duplex U/S imaging Plethismography Venogram 28

29
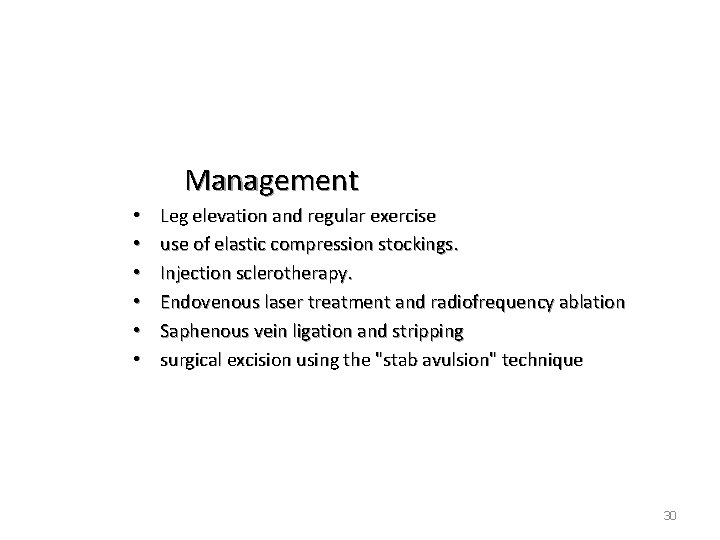
Management • • • Leg elevation and regular exercise use of elastic compression stockings. Injection sclerotherapy. Endovenous laser treatment and radiofrequency ablation Saphenous vein ligation and stripping surgical excision using the "stab avulsion" technique 30
Chronic venous insufficiency The presence of varicose veins and valvular incompetence can lead to a condition called chronic venous insufficiency. • Major and costly medical problem, affecting an estimated 600, 000 people in the United States. • Carry significant negative physical, financial, and psychologic implications. 31
The signs and symptoms of CVI can be attributed : Ø venous reflux Ø venous obstruction Ø calf muscle pump dysfunction Ø loss of venous wall elasticity Ø combination of these factors symptoms- leg fatigue, discomfort, and heaviness. Signs - varicose veins, pigmentation, lipodermatosclerosis, and venous ulceration, impaired wound healing. 32
VARICOSE ULCER • Most common site– medial aspect of ankle & lower 1/3 rd of leg • characteristic features: – Superficial – Vertically oval – Painless – Irregular, Ragged , Sloping edges – Pink base , Unhealthy granulations – Never penetrate deep fascia 33

*Image via Bing 34

35
Evaluation of Venous Insufficiency • • • Ambulatory venuos pressure Venous recovery time Venous filling index Muscle pump ejection fraction Residual volume fraction • Venous Duplex Ultrasound 36
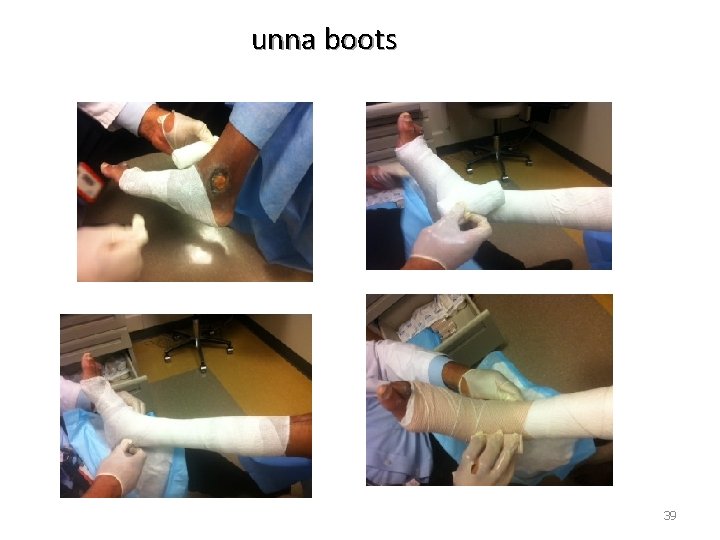
RX of Chronic Venous Insufficiency u. Non-operative Compression Therapy • • Elastic compression stockings Paste gauze boots (Unna's boots) Multilayer elastic wraps or dressings Pneumatic compression devices 37

38
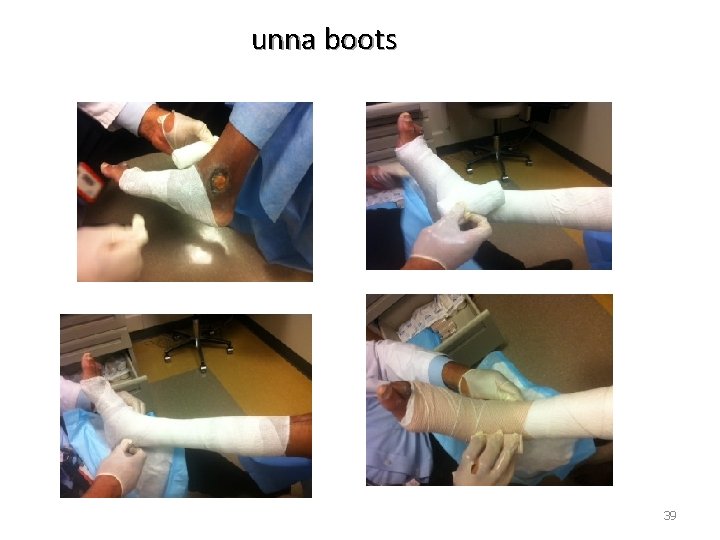
unna boots 39
Surgical Treatment of Chronic Venous Insufficiency Perforator Vein Ligation - subfascial endoscopic perforator vein surgery /SEPS Venous Reconstruction • Repair of existing valves • Transplant of venous segments from the arm • Transposition of an incompetent vein onto an adjacent competent vein. 40
VENOUS THROMBOEMBOLISM THROMBUS -->A blood clot that forms in the lumen of a blood vessel. • Remain important preventable sources of morbidity and mortality • Incidence -DVT 5 and 9 per 10, 000 person-years in the general population -VTE approximately 14 per 10, 000 person-years. 41

VTE. . . • DVT of the lower extremity usually begins in the deep veins of the calf around the valve cusps or within the soleal plexus. • Rarely arise primarily in the ileofemoral system as a result of direct vessel . wall injury, as seen with hip surgery or catheter-induced DVT 42
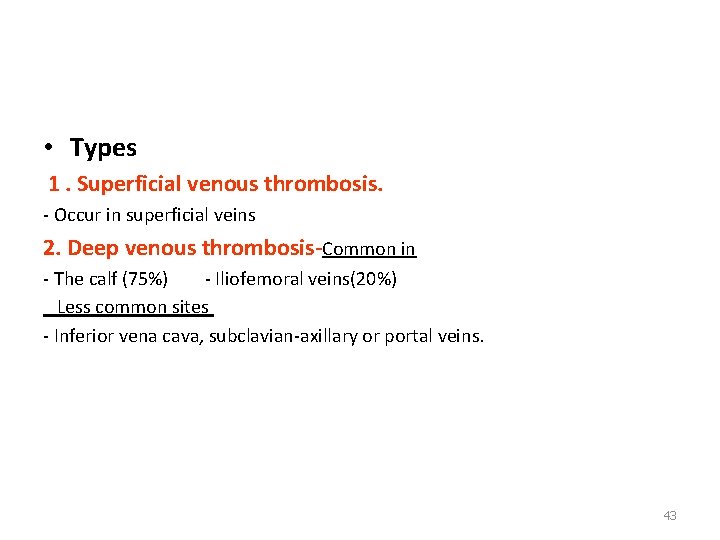
• Types 1. Superficial venous thrombosis. - Occur in superficial veins 2. Deep venous thrombosis-Common in - The calf (75%) - Iliofemoral veins(20%) Less common sites - Inferior vena cava, subclavian-axillary or portal veins. 43
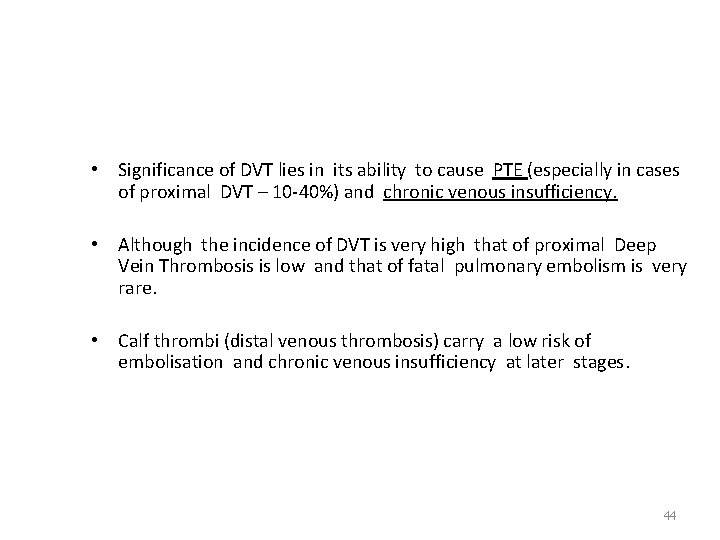
• Significance of DVT lies in its ability to cause PTE (especially in cases of proximal DVT – 10 -40%) and chronic venous insufficiency. • Although the incidence of DVT is very high that of proximal Deep Vein Thrombosis is low and that of fatal pulmonary embolism is very rare. • Calf thrombi (distal venous thrombosis) carry a low risk of embolisation and chronic venous insufficiency at later stages. 44
Rudolph Virchow 1821 -1902 45
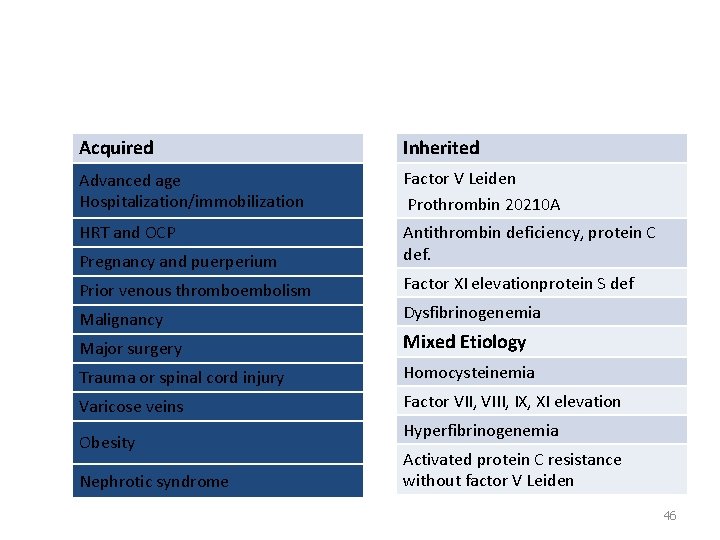
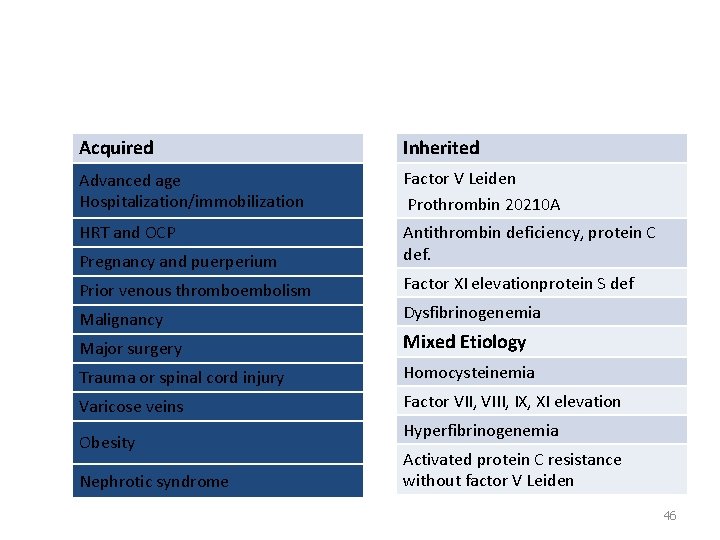
Risk Factors for Venous Thromboembolism Acquired Inherited Advanced age Hospitalization/immobilization Factor V Leiden Prothrombin 20210 A HRT and OCP Antithrombin deficiency, protein C def. Pregnancy and puerperium Prior venous thromboembolism Malignancy Factor XI elevationprotein S def Dysfibrinogenemia Major surgery Mixed Etiology Trauma or spinal cord injury Homocysteinemia Varicose veins Factor VII, VIII, IX, XI elevation Obesity Nephrotic syndrome Hyperfibrinogenemia Activated protein C resistance without factor V Leiden 46
Diagnosis • • High index of suspision History and physical examination-40% pain, swelling , immobility Homans sign Moses sign phlegmasia alba dolens phlegmasia cerulea dolens 47

48

phlegmasia alba dolens phlegmasia cerulea dolens 49
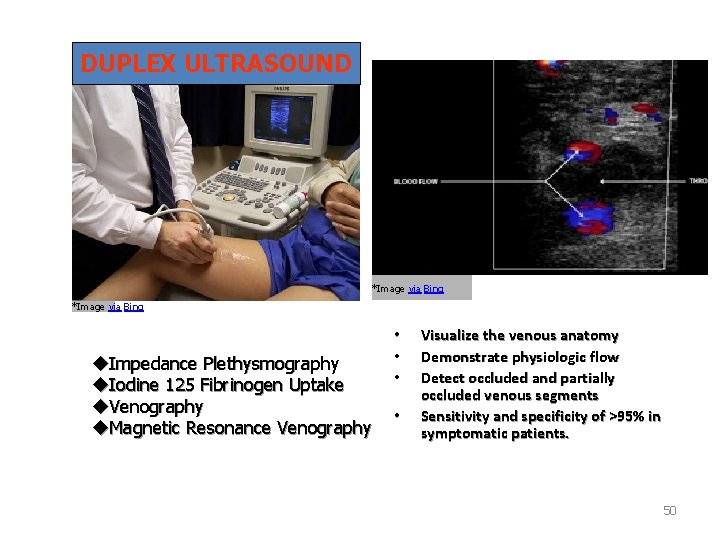
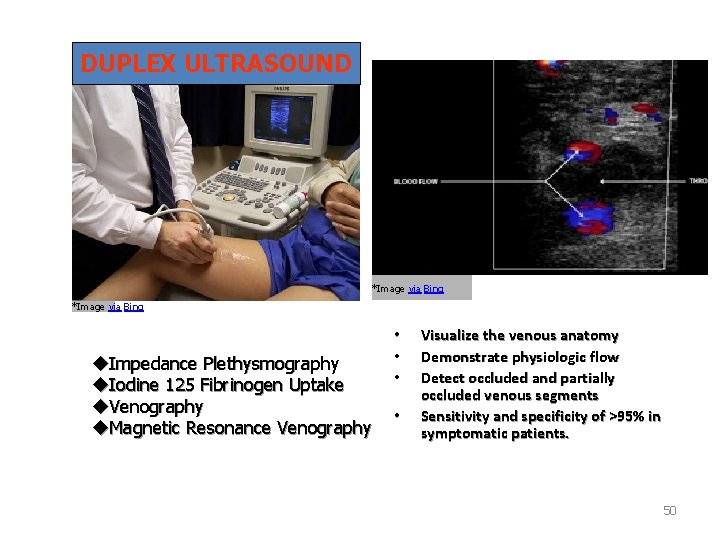
DUPLEX ULTRASOUND *Image via Bing u. Impedance Plethysmography u. Iodine 125 Fibrinogen Uptake u. Venography u. Magnetic Resonance Venography • • Visualize the venous anatomy Demonstrate physiologic flow Detect occluded and partially occluded venous segments Sensitivity and specificity of >95% in symptomatic patients. 50
Suggestive of lower exremity DVT: • • • Lack of spontaneous flow Inability to compress the vein Absence of color filling of the lumen by color flow DUS Loss of respiratory flow variation Venous distention. 51
PULMONARY EMBOLISM • PE is one of the most common causes of sudden death in hospitalized patients. u Dislodgement and embolizition of thrombi -pulmonary arterial circulation u Through a patent foramen ovale or atrial septal defect • Lower Extremities: 65% to 90% • Pelvic venous system • Renal venous system • Upper Extremity • Right Heart 52
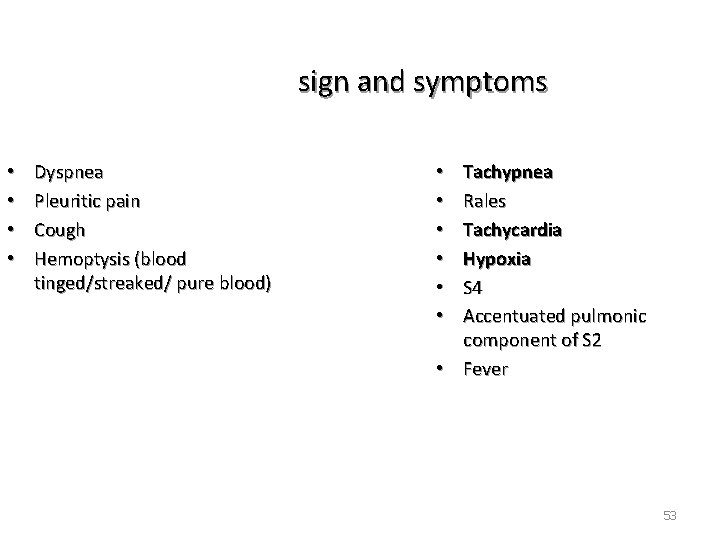
sign and symptoms • • Dyspnea Pleuritic pain Cough Hemoptysis (blood tinged/streaked/ pure blood) Tachypnea Rales Tachycardia Hypoxia S 4 Accentuated pulmonic component of S 2 • Fever • • • 53
54
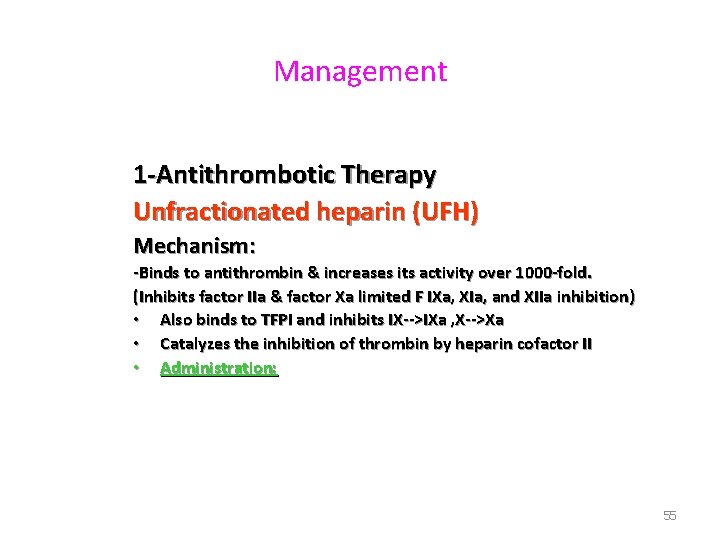
Management 1 -Antithrombotic Therapy Unfractionated heparin (UFH) Mechanism: -Binds to antithrombin & increases its activity over 1000 -fold. (Inhibits factor IIa & factor Xa limited F IXa, XIa, and XIIa inhibition) • Also binds to TFPI and inhibits IX-->IXa , X-->Xa • Catalyzes the inhibition of thrombin by heparin cofactor II • Administration: 55
Low molecular weight heparins (LMWHs) • • Derived from the depolymerization of porcine UFH. Bind to antithrombin and inhibit Fxa>FII Increased bioavailability (>90% after SC injection) Longer half-lives(4 to 6 hours), more predictable elimination rates. Weight-based once- or twice-daily SC injections No monitoring is needed. The more recent studies demonstrate a decrease in thrombotic complications, bleeding, HIT and mortality with LMWHs. 56
Vitamin K antagonists • Include warfarin and other coumarin derivatives • mainstay of long-term antithrombotic therapy in patients with VTE. • Warfarin inhibits the -carboxylation of vitamin K–dependent procoagulants (factors II, VII, IX, X) and anticoagulants (proteins C and S), which results in the formation of less functional proteins 57
• Warfarin usually requires several days to achieve its full effect • The steady-state concentration of warfarin is usually not reached for 4 to 5 days • May be started on the same day as the initial parenteral anticoagulant, usually at doses ranging from 5 to 10 mg. • The therapeutic target INR range is usually 2. 0 to 3. 0. • Complication-bleeding 58
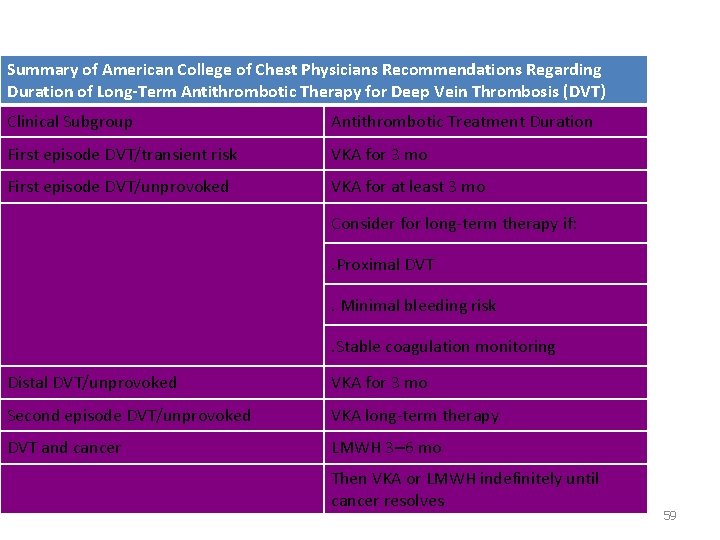
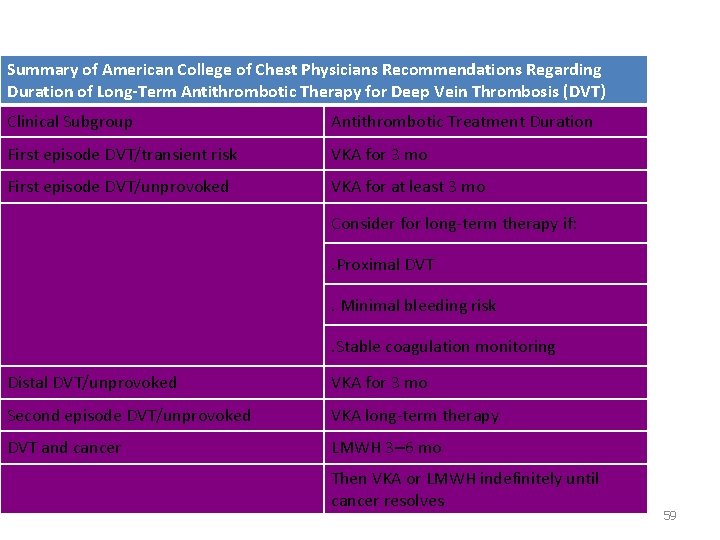
Summary of American College of Chest Physicians Recommendations Regarding Duration of Long-Term Antithrombotic Therapy for Deep Vein Thrombosis (DVT) Clinical Subgroup Antithrombotic Treatment Duration First episode DVT/transient risk VKA for 3 mo First episode DVT/unprovoked VKA for at least 3 mo Consider for long-term therapy if: . Proximal DVT. Minimal bleeding risk. Stable coagulation monitoring Distal DVT/unprovoked VKA for 3 mo Second episode DVT/unprovoked VKA long-term therapy DVT and cancer LMWH 3– 6 mo Then VKA or LMWH indefinitely until cancer resolves 59
Systemic and Catheter-Directed Thrombolysis • • • Streptokinase, urokinase, alteplase (recombinant tpa), reteplase For Patients with extensive proximal DVT. Reduce acute symptoms more rapidly than anticoagulation alone. Decrease the development of post-thrombotic syndrome. Improved valve preservation and quality of life. Minimize bleeding complications and increase efficacy. Convert plasminogen to plasmin, which leads to the degradation of fibrin. 60
2 -Inferior Vena Caval Filters Indications: --Recurrent DVT. --significant propagation of the original thrombus or proximal DVT at a new site. --PE despite adequate anticoagulation therapy. --patients with pulmonary hypertension who experience recurrent PE. --CI/Cxs of anticoagulation therapy in the presence of an acute proximal DVT. -- ? prophylaxis against PE in patients receiving catheter-directed thrombolysis & in high-risk pts without established DVT or PE. Ø CXs-wound hematoma, migration of the device into the pulmonary artery, caval occlusion due to trapping of a large embolus. Ø Continue antithrombotic medication 61
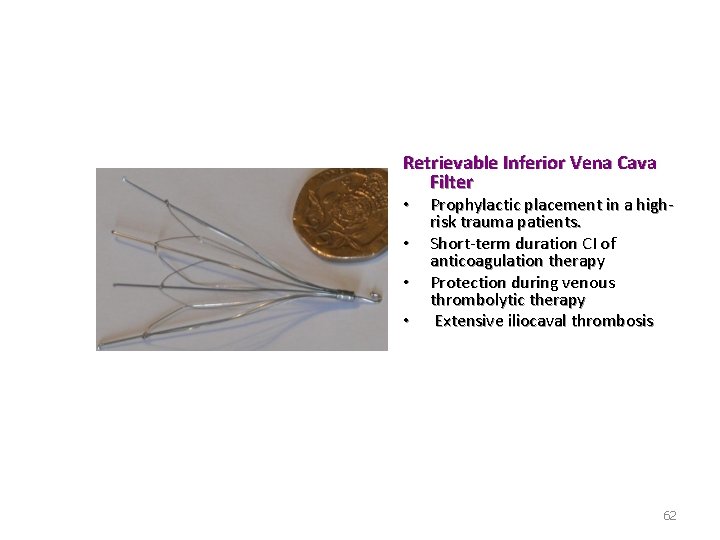
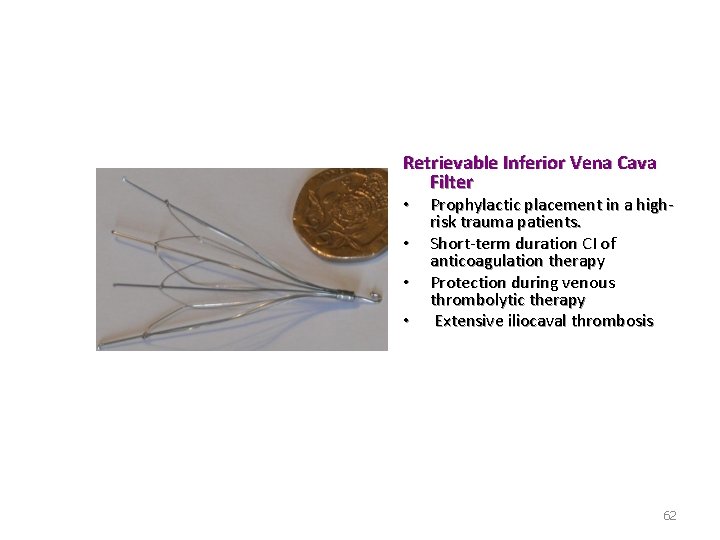
Retrievable Inferior Vena Cava Filter • • Prophylactic placement in a highrisk trauma patients. Short-term duration CI of anticoagulation therapy Protection during venous thrombolytic therapy Extensive iliocaval thrombosis 62
3 -Operative Venous Thrombectomy • • • In pts with acute iliofemoral DVT, surgical therapy is generally reserved for pts who worsen with anticoagulation therapy & those with phlegmasia cerulea dolens and impending venous gangrene Continue Heparin and warfarin administered postoperatively. Emergency pulmonary embolectomy for acute PE for whom thrombolysis has failed or who have contraindications to thrombolytics. 63
Venous Thromboembolism Prophylaxis in General Surgery • Patients who undergo major operative procedures without thromboprophylaxis have a significant incidence of perioperative DVT (15 to 40%). • The incidence is even higher with major trauma (40 to 80%), hip and knee replacement surgery (40 to 60%), and spinal cord injury (60 to 80%). • pharmacologic agents/mechanica methods. 64
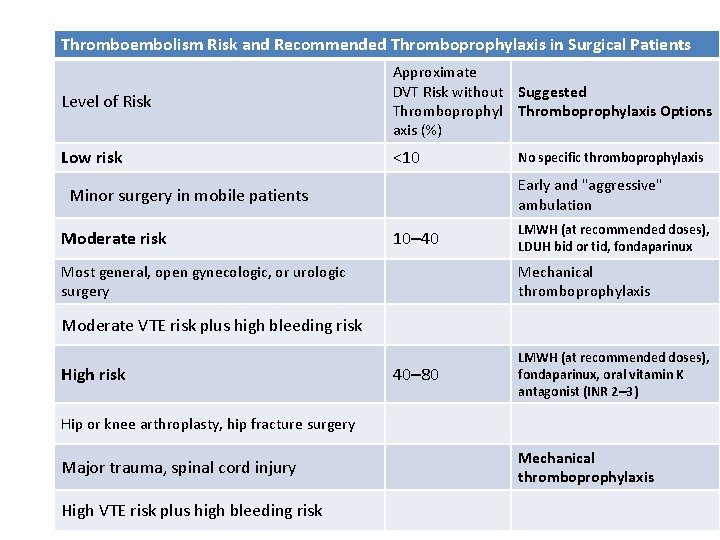
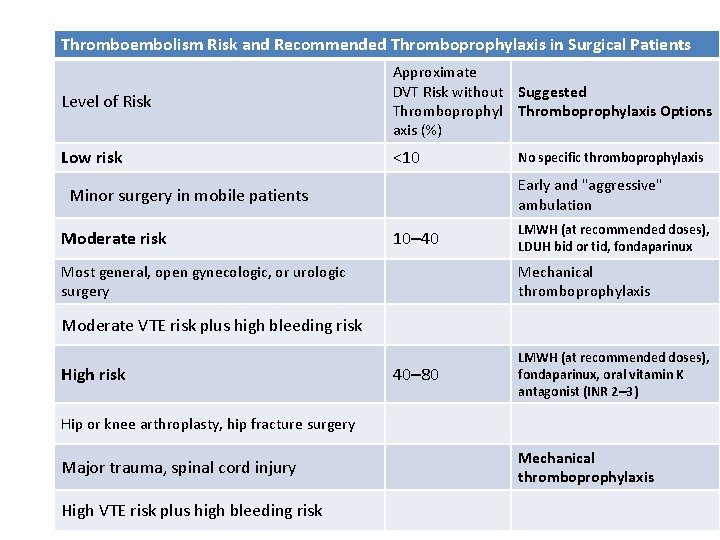
Thromboembolism Risk and Recommended Thromboprophylaxis in Surgical Patients Level of Risk Approximate DVT Risk without Suggested Thromboprophylaxis Options axis (%) Low risk <10 Early and "aggressive" ambulation Minor surgery in mobile patients Moderate risk No specific thromboprophylaxis 10– 40 Most general, open gynecologic, or urologic surgery LMWH (at recommended doses), LDUH bid or tid, fondaparinux Mechanical thromboprophylaxis Moderate VTE risk plus high bleeding risk High risk 40– 80 LMWH (at recommended doses), fondaparinux, oral vitamin K antagonist (INR 2– 3) Hip or knee arthroplasty, hip fracture surgery Major trauma, spinal cord injury High VTE risk plus high bleeding risk Mechanical thromboprophylaxis 65
LYMPHATIC DISEASE 66
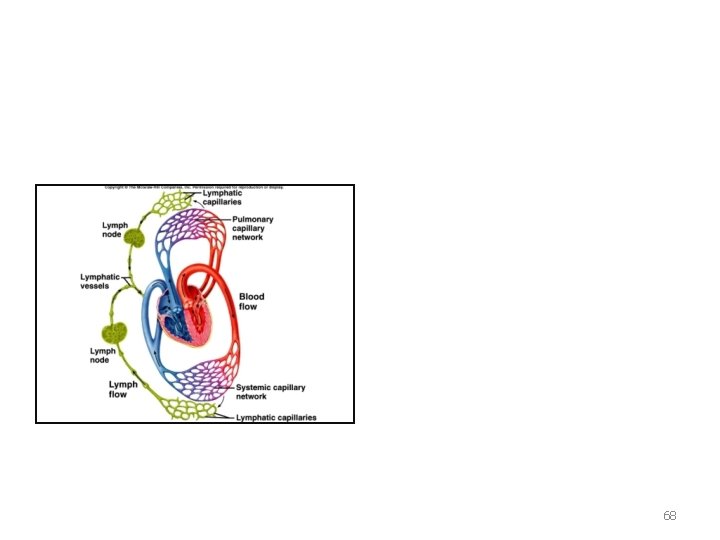
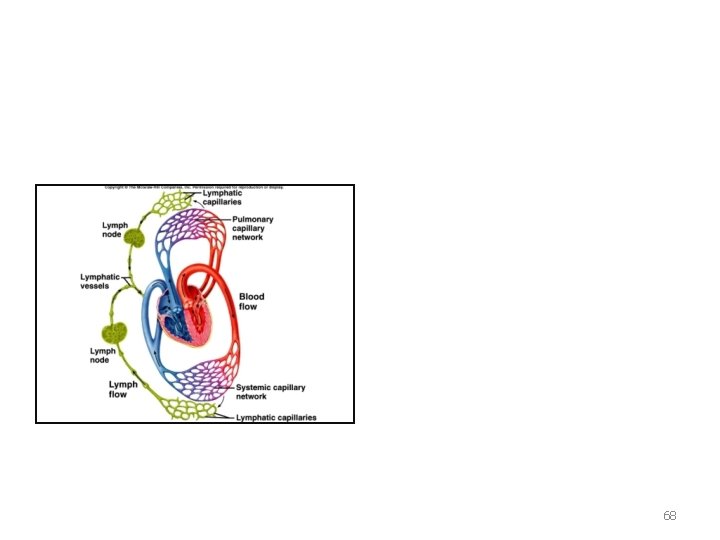
• Lymph • • • Colorless fluid and protein that has been squeezed out of the blood. Similar in composition to blood plasma. Flow rate. . . Lymphatic system includes : • Lymph Organs • Lymph Vessels • Lymph Tissues FUNCTION. . . 67
68
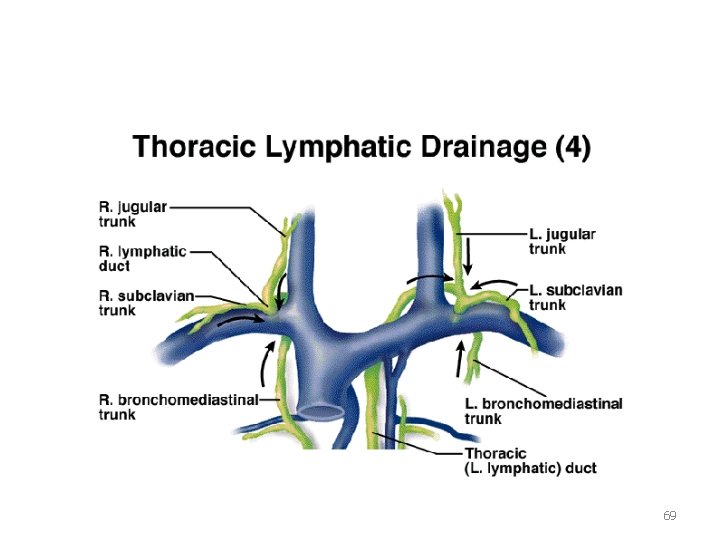
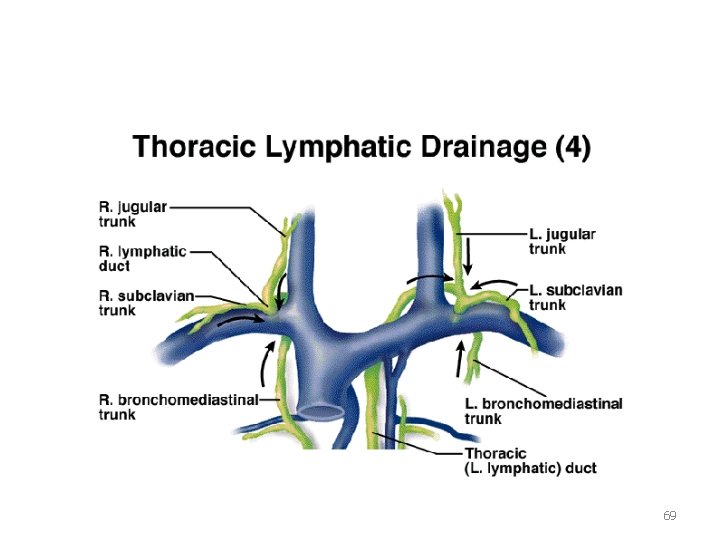
69
Lymphedema • Extremity swelling that results from a reduction in lymphatic transport, with resultant pooling of lymph within the interstitial space. • caused by anatomic problems such as lymphatic hypoplasia, functional insufficiency, or absence of lymphatic valves. 70
lymphedema. . . • Primary lymphedema - congenital lymphedema-milroys ds -lymphedema praecox - Lymphedema tarda • Secondary lymphedema -Axillary node dissection. - Radiation therapy, trauma, infection, malignancy, filariasis 71
GRADING OF LYMPHEDEMA • GRADE 1_ Decreases with limb elevation • GRADE 2 _ Does not decrease completely with limb elevation • GRADE 3 _ Develops secondary skin changes venous and lymphatic. . . 72
Lymphedema. . . Clinical Diagnosis History and physical examination. • Heaviness and fatigue in the affected extremity. • In the LE swelling involves the dorsum of the foot, and the toes have a squared-off appearance. • Hyperkeratosis of the skin, fluid weeps from lymph-filled vesicles. • Recurrent cellulitis. • Radiologic Diagnosis • Duplex Ultrasound • Lymphoscintigraphy • Lymphangiography 73

74

75

76
management Conservative • • Bedrest and Leg Elevation Graded compression stockings Sequential External Pneumatic Compression Lymphatic Massage surgery • l l • Reconstructive -lympho-venous anastomosis - lymphatic transposition omental flap operations enteromesentric bridge procedures Excision of extra tissue (Debulking) 77
Thanks 78
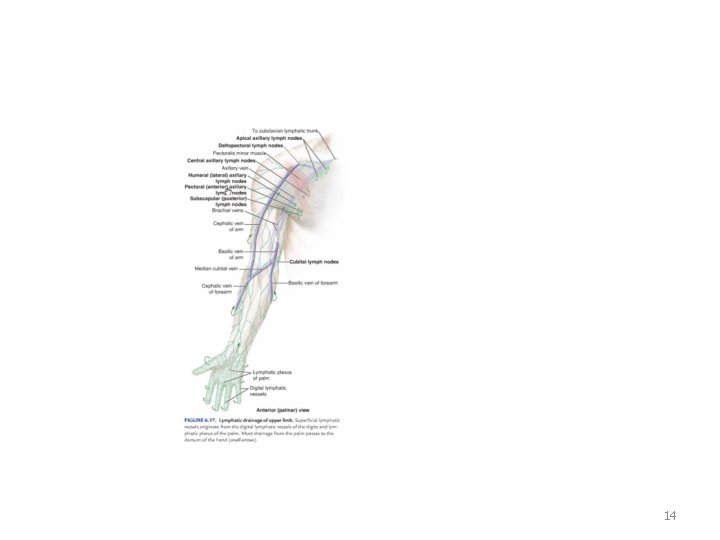
 Lymph nodes scapula
Lymph nodes scapula Brachial vein
Brachial vein Efferent lymphatics
Efferent lymphatics Angela qureshi
Angela qureshi 10 principles of family medicine
10 principles of family medicine Samina qureshi md
Samina qureshi md Dr riaz qureshi
Dr riaz qureshi Moin qureshi gatech
Moin qureshi gatech Dr riaz qureshi
Dr riaz qureshi Birthdates
Birthdates Drg usman sumantri
Drg usman sumantri Usman niazi
Usman niazi Nabila usman
Nabila usman Dr kauser usman clinic address
Dr kauser usman clinic address Bnfo
Bnfo Njit machine learning
Njit machine learning Usman roshan
Usman roshan Usman nawaz missing
Usman nawaz missing Iodine functions
Iodine functions Dr.kauser usman
Dr.kauser usman Usman mahboob
Usman mahboob Cs 675 njit
Cs 675 njit Doctor usman ghani
Doctor usman ghani Usman roshan
Usman roshan Usman roshan
Usman roshan Pengertian wawasan nusantara menurut prof wan usman
Pengertian wawasan nusantara menurut prof wan usman Dr kauser usman
Dr kauser usman Dr kauser usman clinic address
Dr kauser usman clinic address Group
Group Usman roshan
Usman roshan Usman roshan
Usman roshan Lesser saphenous vein
Lesser saphenous vein Precapillary sphincter
Precapillary sphincter Hunter perforator
Hunter perforator How to measure the jvp
How to measure the jvp Internal thoracic vein
Internal thoracic vein Lifestyle modern
Lifestyle modern Venn diagram of communicable and non-communicable diseases
Venn diagram of communicable and non-communicable diseases Section 19-3 diseases caused by bacteria and viruses
Section 19-3 diseases caused by bacteria and viruses Retention hyperkeratosis dermnet
Retention hyperkeratosis dermnet Chapter 6 musculoskeletal system diseases and disorders
Chapter 6 musculoskeletal system diseases and disorders Chapter 24 sexually transmitted diseases and hiv/aids
Chapter 24 sexually transmitted diseases and hiv/aids Chapter 22 genetics and genetically linked diseases
Chapter 22 genetics and genetically linked diseases Chapter 21 mental health diseases and disorders
Chapter 21 mental health diseases and disorders Chapter 17 reproductive system diseases and disorders
Chapter 17 reproductive system diseases and disorders Chapter 15 nervous system diseases and disorders
Chapter 15 nervous system diseases and disorders Onychomycosis milady
Onychomycosis milady Chapter 8 skin disorders and diseases
Chapter 8 skin disorders and diseases 10 nail diseases and disorders
10 nail diseases and disorders Certain infectious and parasitic diseases
Certain infectious and parasitic diseases Cardiovascular system diseases and disorders chapter 8
Cardiovascular system diseases and disorders chapter 8 Pulp pathosis
Pulp pathosis Milady chapter 8 skin disorders and diseases
Milady chapter 8 skin disorders and diseases Venn diagram of communicable and non-communicable diseases
Venn diagram of communicable and non-communicable diseases Purulent diseases of lungs and pleura
Purulent diseases of lungs and pleura Tronsmo plant pathology and plant diseases download
Tronsmo plant pathology and plant diseases download Tronsmo plant pathology and plant diseases download
Tronsmo plant pathology and plant diseases download Albugo eye
Albugo eye Venn diagram of communicable and non-communicable diseases
Venn diagram of communicable and non-communicable diseases Vitamins functions
Vitamins functions Myths and fallacies about non communicable diseases
Myths and fallacies about non communicable diseases 10 diseases of lymphatic system
10 diseases of lymphatic system Surgical team roles and responsibilities
Surgical team roles and responsibilities Wellspan surgical and rehab hospital
Wellspan surgical and rehab hospital Difference between medical and surgical asepsis
Difference between medical and surgical asepsis Anastomosis around elbow joint
Anastomosis around elbow joint Tapvd
Tapvd Dural arterial supply
Dural arterial supply Five layers of scalp
Five layers of scalp Pituitary gland nerve supply
Pituitary gland nerve supply Venous guttering foot
Venous guttering foot Lower border of heart
Lower border of heart Nose venous drainage
Nose venous drainage Venous tracing
Venous tracing Dural venous sinuses
Dural venous sinuses Arterial blood vs venous blood
Arterial blood vs venous blood Relations of ascending colon
Relations of ascending colon Constrictive pericarditis cvp waveform
Constrictive pericarditis cvp waveform Superior oblique tendon
Superior oblique tendon