Vasopressors Inotropes and Shock Beatrice Wong Pharm D
Vasopressors, Inotropes, and Shock Beatrice Wong, Pharm. D, BCPS November 1, 2011
Objectives Define types of shock. Review pharmacology of vasoactive agents. Overview of management of the different types of shock. Discuss cases.
Shock �Physiologic state of impaired tissue perfusion and oxygen delivery �Cardinal signs • Hypotension (SBP <90 mm. Hg or >40 mm. Hg decrease from baseline) • Oliguria • Altered mental status • Metabolic acidosis • Cool, clammy skin
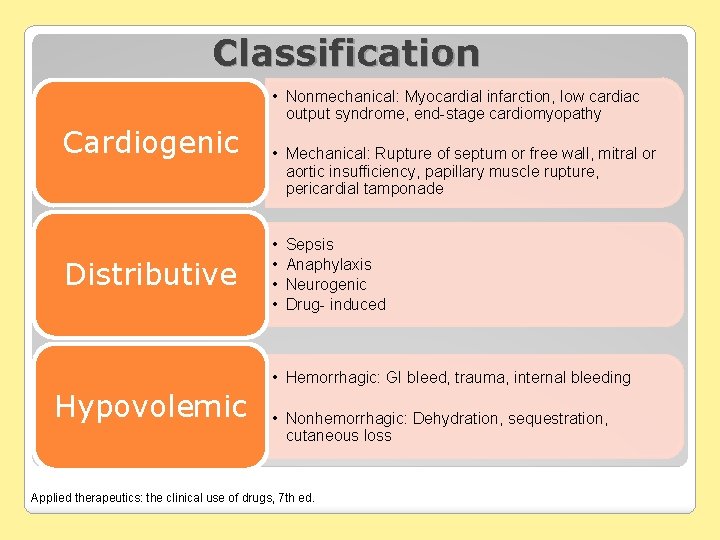
Classification • Nonmechanical: Myocardial infarction, low cardiac output syndrome, end-stage cardiomyopathy Cardiogenic Distributive • Mechanical: Rupture of septum or free wall, mitral or aortic insufficiency, papillary muscle rupture, pericardial tamponade • • Sepsis Anaphylaxis Neurogenic Drug- induced • Hemorrhagic: GI bleed, trauma, internal bleeding Hypovolemic • Nonhemorrhagic: Dehydration, sequestration, cutaneous loss Applied therapeutics: the clinical use of drugs, 7 th ed.
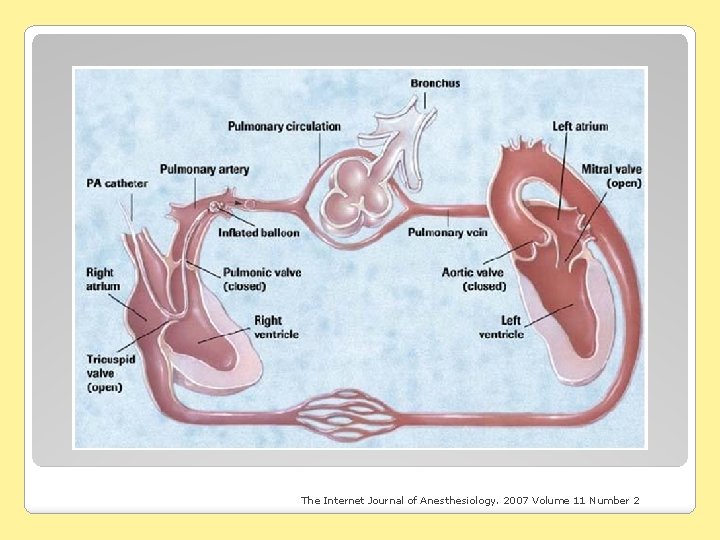
The Internet Journal of Anesthesiology. 2007 Volume 11 Number 2
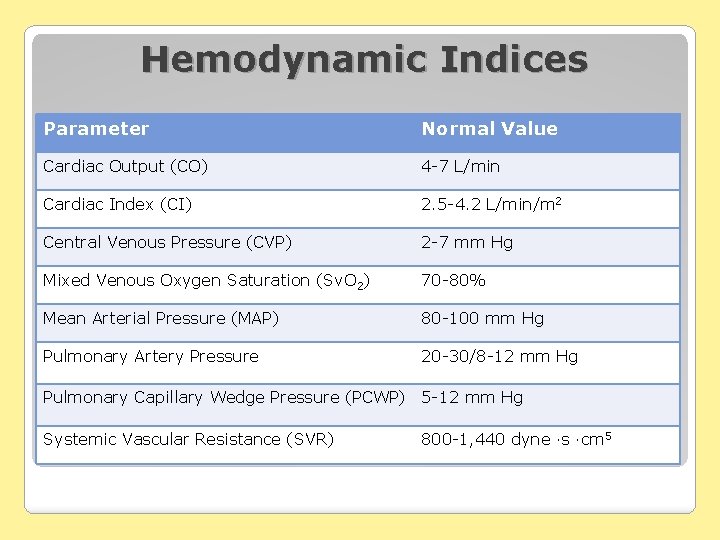
Hemodynamic Indices Parameter Normal Value Cardiac Output (CO) 4 -7 L/min Cardiac Index (CI) 2. 5 -4. 2 L/min/m 2 Central Venous Pressure (CVP) 2 -7 mm Hg Mixed Venous Oxygen Saturation (Sv. O 2) 70 -80% Mean Arterial Pressure (MAP) 80 -100 mm Hg Pulmonary Artery Pressure 20 -30/8 -12 mm Hg Pulmonary Capillary Wedge Pressure (PCWP) 5 -12 mm Hg Systemic Vascular Resistance (SVR) 800 -1, 440 dyne ∙s ∙cm 5
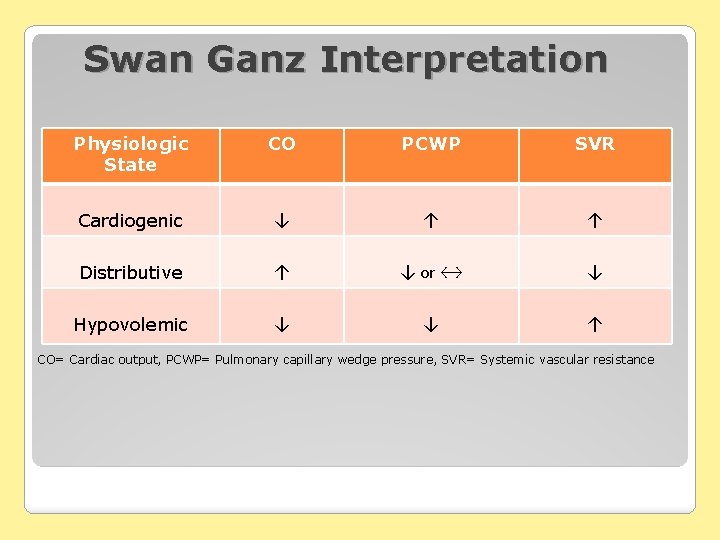
Swan Ganz Interpretation Physiologic State CO PCWP SVR Cardiogenic ↓ ↑ ↑ Distributive ↑ ↓ or ↔ ↓ Hypovolemic ↓ ↓ ↑ CO= Cardiac output, PCWP= Pulmonary capillary wedge pressure, SVR= Systemic vascular resistance
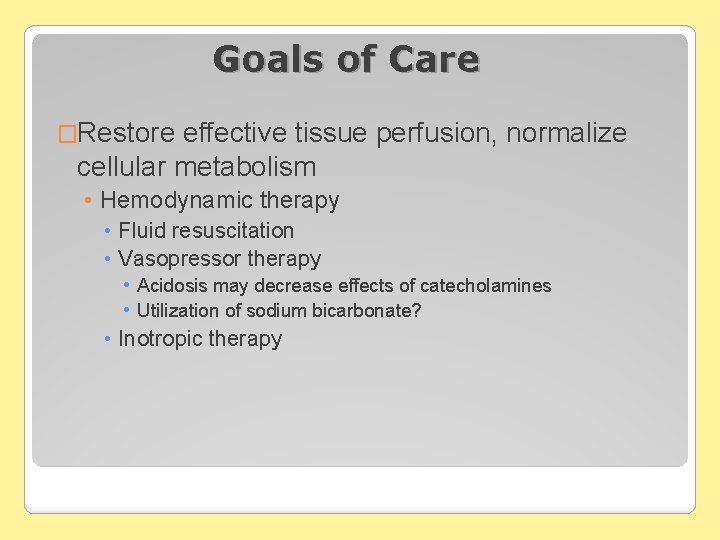
Goals of Care �Restore effective tissue perfusion, normalize cellular metabolism • Hemodynamic therapy • Fluid resuscitation • Vasopressor therapy • Acidosis may decrease effects of catecholamines • Utilization of sodium bicarbonate? • Inotropic therapy
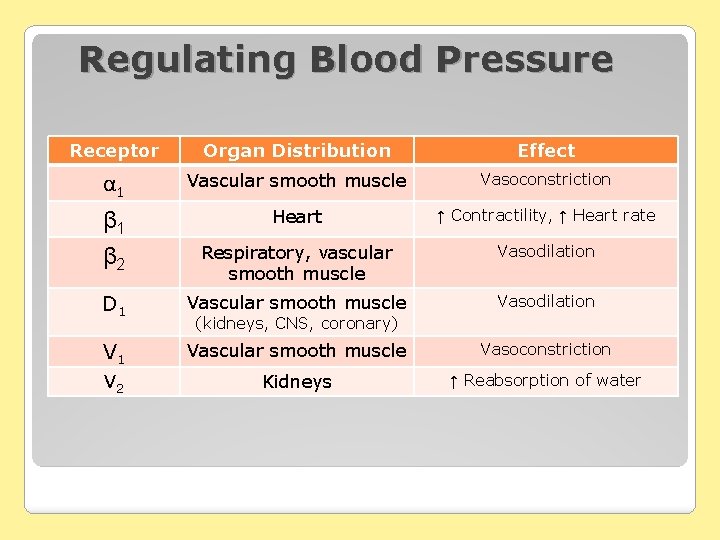
Regulating Blood Pressure Receptor Organ Distribution Effect α 1 Vascular smooth muscle Vasoconstriction β 1 β 2 Heart ↑ Contractility, ↑ Heart rate Respiratory, vascular smooth muscle Vasodilation D 1 Vascular smooth muscle Vasodilation V 1 Vascular smooth muscle Vasoconstriction V 2 Kidneys ↑ Reabsorption of water (kidneys, CNS, coronary)
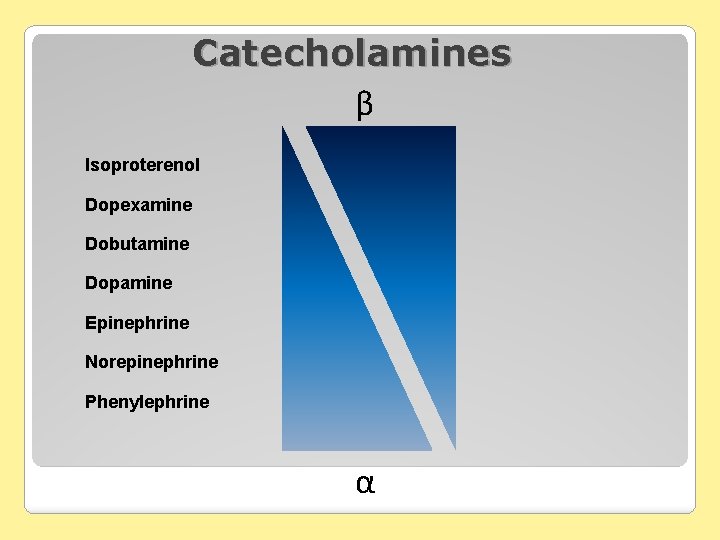
Catecholamines β Isoproterenol Dopexamine Dobutamine Dopamine Epinephrine Norepinephrine Phenylephrine α
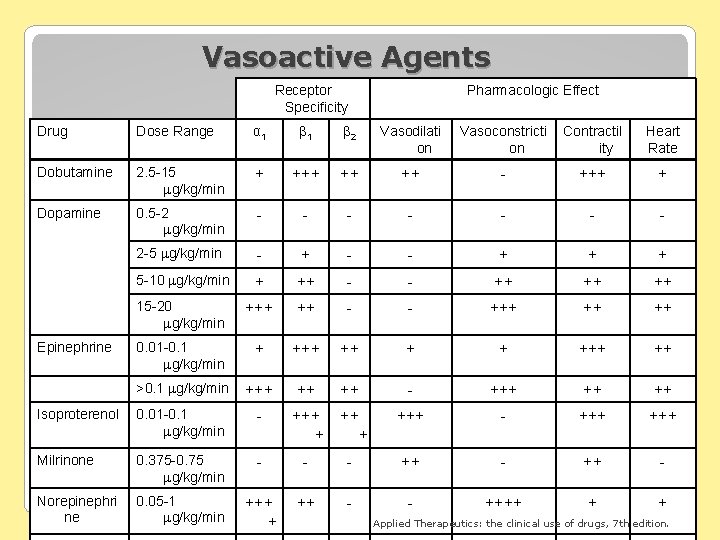
Vasoactive Agents Receptor Specificity Pharmacologic Effect Drug Dose Range α 1 β 2 Vasodilati on Vasoconstricti on Contractil ity Heart Rate Dobutamine 2. 5 -15 g/kg/min + ++ ++ - +++ + Dopamine 0. 5 -2 g/kg/min - - - - 2 -5 g/kg/min - + - - + + + 5 -10 g/kg/min + ++ - - ++ ++ ++ 15 -20 g/kg/min +++ ++ - - +++ ++ ++ 0. 01 -0. 1 g/kg/min + ++ + + ++ >0. 1 g/kg/min +++ ++ ++ - +++ ++ ++ Isoproterenol 0. 01 -0. 1 g/kg/min - +++ + +++ - +++ Milrinone 0. 375 -0. 75 g/kg/min - - - ++ - Norepinephri ne 0. 05 -1 g/kg/min +++ + ++ - - ++++ + + Epinephrine Applied Therapeutics: the clinical use of drugs, 7 th edition.
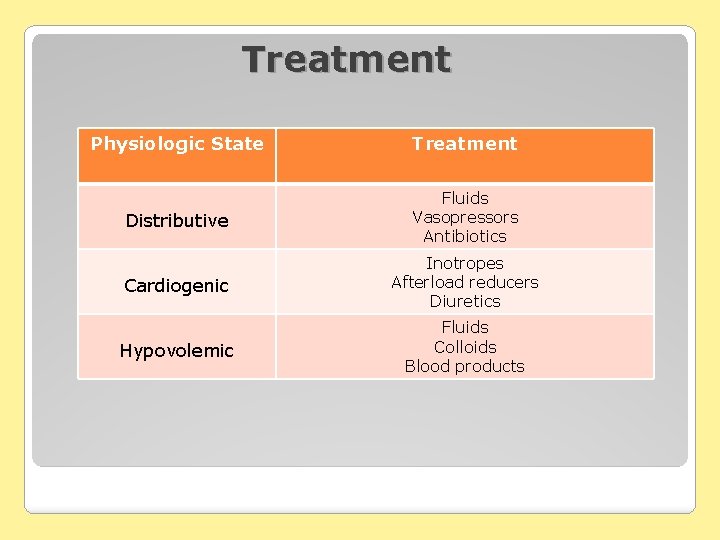
Treatment Physiologic State Treatment Distributive Fluids Vasopressors Antibiotics Cardiogenic Inotropes Afterload reducers Diuretics Hypovolemic Fluids Colloids Blood products
Vasoactive Agents Vasopressors Inotropes Vasodilators
Vasopressor Agents �Catecholamines • Dopamine • Epinephrine • Norepinephrine (Levophed®) • Phenylephrine (Neosynephrine®) DOPAMINE NOREPI EPINEPHRINE Miscellaneous • Vasopressin agents
Vasoactive Therapy Adverse Effects • Arrhythmias • Direct effect of beta-1 stimulation • ↑ oxygen demand by the heart • Regional Hypoperfusion • Possible organ hypoperfusion at the expense of restoring central BP (e. g. kidney, gastrointestinal) • Endocrine Effects • Hyperglycemia • Tissue Damage and Extravastation • Tachyphylaxis may occur with prolonged use
Dopamine Most common first MOA: dose-related line catecholamine receptor activity • DA, beta-1, alpha-1 • ↑ BP via ↑ myocardial contractility and vasoconstriction Dosing • 0. 5 – 20 mcg/kg/min Considerations DA: 0. 5 -3 mcg/kg/min Beta-1: 3 -10 mcg/kg/min Alpha-1: > 10 mcg/kg/min • Dose response is highly variable • “Renal” dosing: Low-dose dopamine should not be used to prevent renal failure • Tachydysrhythmias are common
Epinephrine More often used for inotropic effects in patients with ↓ CO/CI and ↓SVR MOA: dose-dependent hemodynamic effect Dosing – split dosing effect • 0. 01 -0. 1 mcg/kg/min (β 1, β 2 effects predominate) • > 0. 1 -1 mcg/kg/min (α 1 effects predominate) Considerations • Metabolic derangements
Norepinephrine Vasoconstriction HR effect predominates over CO or • Improved regional perfusion than higher dose dopamine MOA: alpha >>> beta effects Dosing • 0. 01 – 1 mcg/kg/min Considerations • Splanchnic perfusion
Phenylephrine Selective alpha agonist producing ↑SVR • May decrease HR, CO and cause coronary constriction MOA: alpha-1 mediated vasoconstriction Dosing • 0. 5 – 5 mcg/kg/min Considerations • Useful in pts with significant tachycardia
Vasopressin Renal Actions • Antidiuretic hormone (ADH), concentrates urine by increasing the flow of water from the collecting ducts into the renal medulla Vascular Actions • Direct action on vascular smooth muscle (V 1 receptor) • Increases vascular resistance in the mesenteric beds, reducing portal venous flow • Increases vascular reactivity to catecholamines • Coronary artery vasoconstriction has been reported especially at high doses (>0. 1 u/min may need nitroglycerin gtt)
Vasopressin Dosing • 0. 01 -0. 1 u/min • 0. 04 units/min in sepsis (not titrated) Onset: immediate t 1/2: 10 -20 mins Titration • 0. 01 -0. 02 units/min q 30 minutes Monitoring • Decreased cardiac output • Peripheral vasoconstriction and ischemia
Vasopressin Advantages • Long half-life • Works independently of adrenergic receptors • Works in acidotic patients • Doesn’t appear to elevate PA pressures Disadvantages • Decreased mesenteric perfusion
Inotropes Dopamine Dobutamine Epinephrine Isoproterenol (Isuprel®) Milrinone (Primacor®)
Dobutamine Cardiogenic MOA shock, heart failure • Selective beta-2 agonist, ↑CO and HR Dosing • 1 -20 mcg/kg/min • Dose > 10 mcg/kg/min rarely used Considerations • Dose-related tachyarrhythmias • ↑ m. VO 2 – caution in ischemia, CAD pts
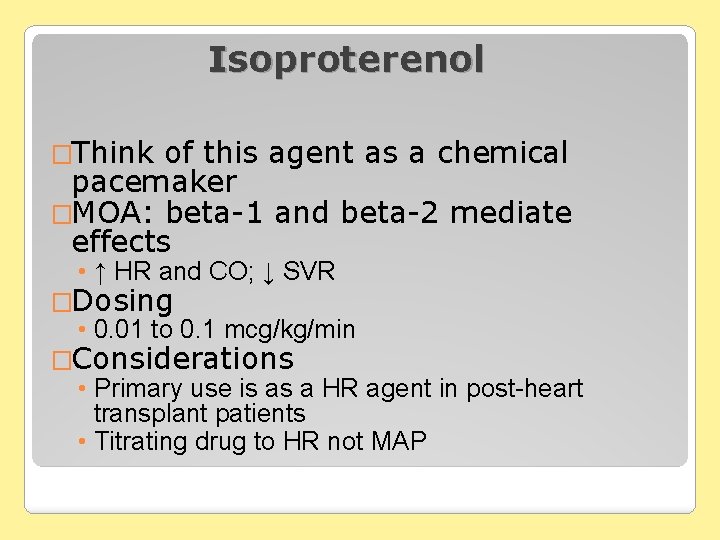
Isoproterenol �Think of this agent as a chemical pacemaker �MOA: beta-1 and beta-2 mediate effects • ↑ HR and CO; ↓ SVR �Dosing • 0. 01 to 0. 1 mcg/kg/min �Considerations • Primary use is as a HR agent in post-heart transplant patients • Titrating drug to HR not MAP
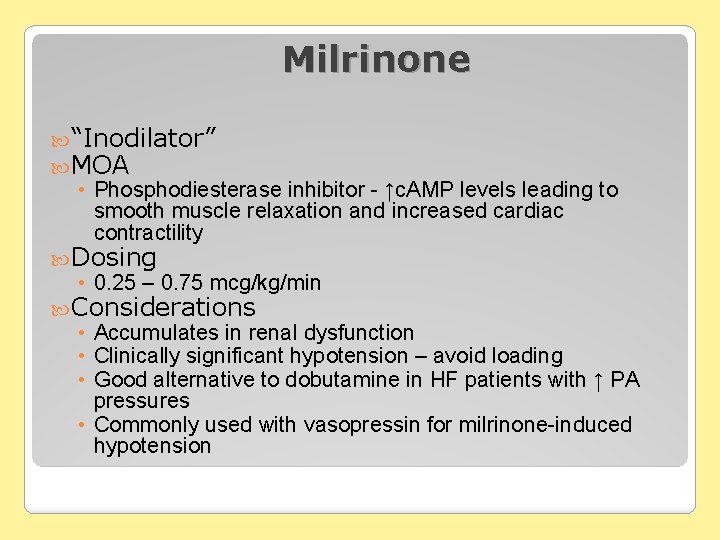
Milrinone “Inodilator” MOA • Phosphodiesterase inhibitor - ↑c. AMP levels leading to smooth muscle relaxation and increased cardiac contractility Dosing • 0. 25 – 0. 75 mcg/kg/min Considerations • Accumulates in renal dysfunction • Clinically significant hypotension – avoid loading • Good alternative to dobutamine in HF patients with ↑ PA pressures • Commonly used with vasopressin for milrinone-induced hypotension
Vasodilators Sodium Nitroprusside (Nipride®) Nitroglycerin Nesiritide (Natrecor®)
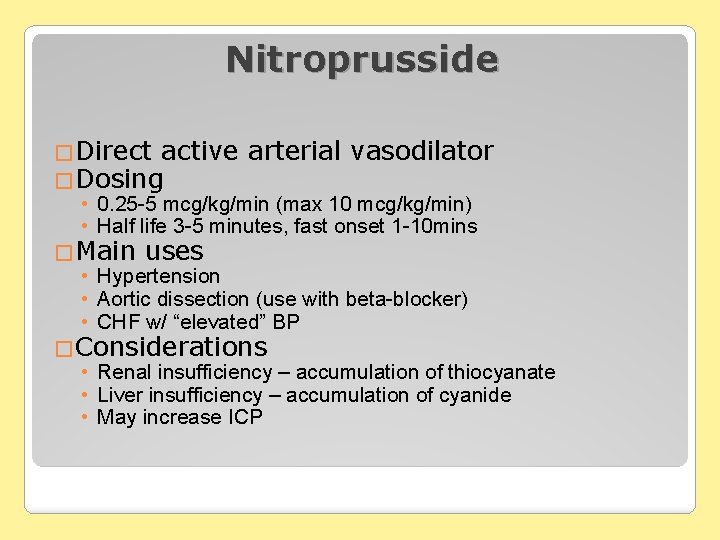
Nitroprusside �Direct active arterial vasodilator �Dosing • 0. 25 -5 mcg/kg/min (max 10 mcg/kg/min) • Half life 3 -5 minutes, fast onset 1 -10 mins �Main uses • Hypertension • Aortic dissection (use with beta-blocker) • CHF w/ “elevated” BP �Considerations • Renal insufficiency – accumulation of thiocyanate • Liver insufficiency – accumulation of cyanide • May increase ICP
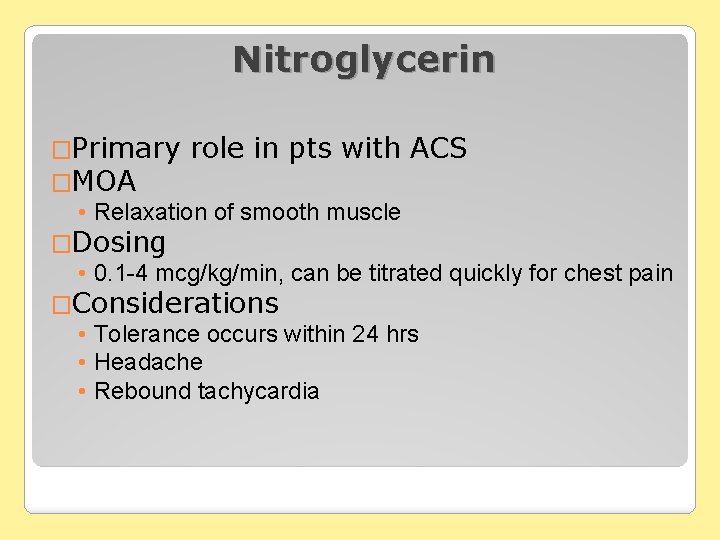
Nitroglycerin �Primary role in pts with ACS �MOA • Relaxation of smooth muscle �Dosing • 0. 1 -4 mcg/kg/min, can be titrated quickly for chest pain �Considerations • Tolerance occurs within 24 hrs • Headache • Rebound tachycardia
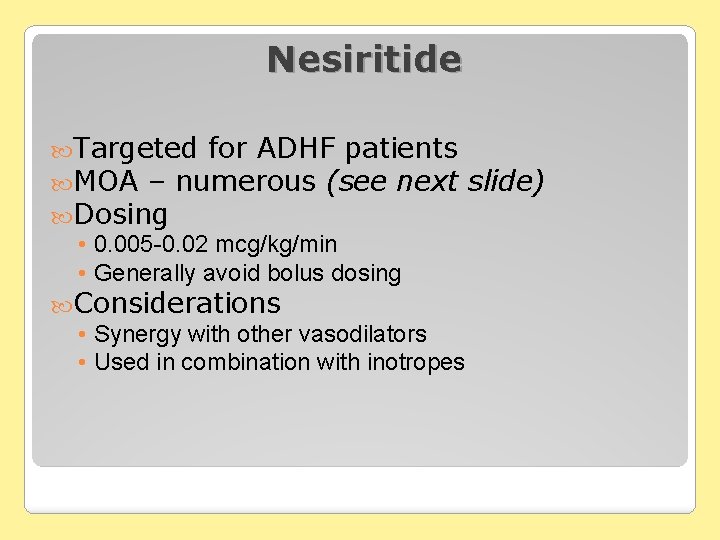
Nesiritide Targeted for ADHF patients MOA – numerous (see next slide) Dosing • 0. 005 -0. 02 mcg/kg/min • Generally avoid bolus dosing Considerations • Synergy with other vasodilators • Used in combination with inotropes
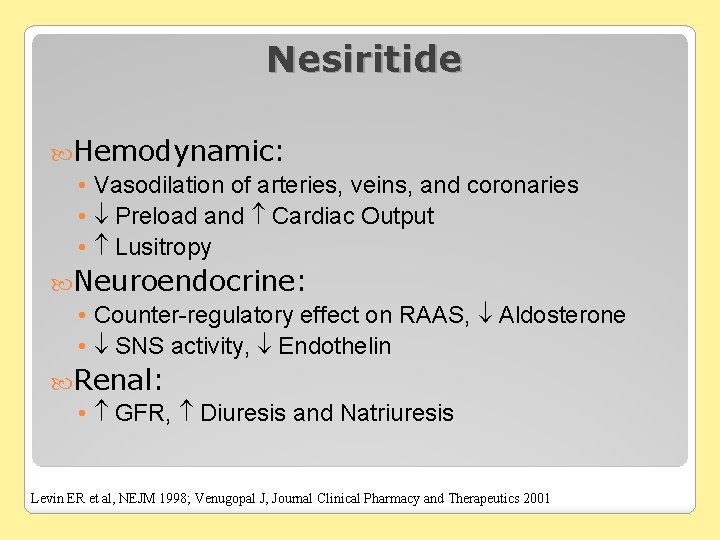
Nesiritide Hemodynamic: • Vasodilation of arteries, veins, and coronaries • Preload and Cardiac Output • Lusitropy Neuroendocrine: • Counter-regulatory effect on RAAS, Aldosterone • SNS activity, Endothelin Renal: • GFR, Diuresis and Natriuresis Levin ER et al, NEJM 1998; Venugopal J, Journal Clinical Pharmacy and Therapeutics 2001
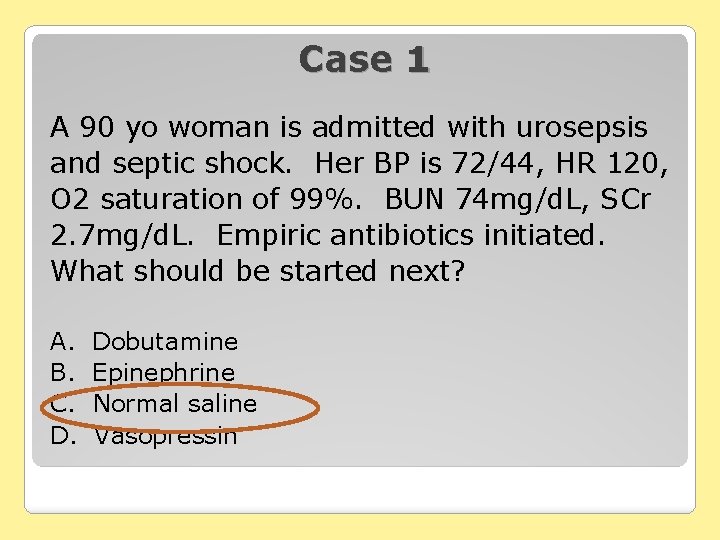
Case 1 A 90 yo woman is admitted with urosepsis and septic shock. Her BP is 72/44, HR 120, O 2 saturation of 99%. BUN 74 mg/d. L, SCr 2. 7 mg/d. L. Empiric antibiotics initiated. What should be started next? A. B. C. D. Dobutamine Epinephrine Normal saline Vasopressin
Case 1 continued Patient’s CVP ↑ to 8 mm. Hg. MAP ↓ to 50 s. Besides continuing fluid resuscitation, what agent would you like to start? Dobutamine B. Milrinone C. Dopamine D. Epinephrine A.
Which agent to choose in sepsis?
CATS Study Randomized, N= double-blind study in France 330 patients with septic shock Epinephrine vs Dobutamine + Norepinephrine Primary outcome= 28 day mortality Lancet 2007; 370: 676 -84.
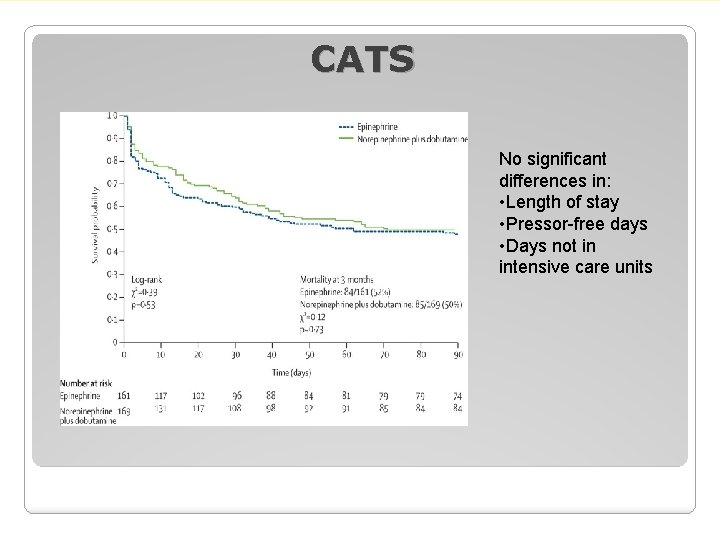
CATS No significant differences in: • Length of stay • Pressor-free days • Days not in intensive care units
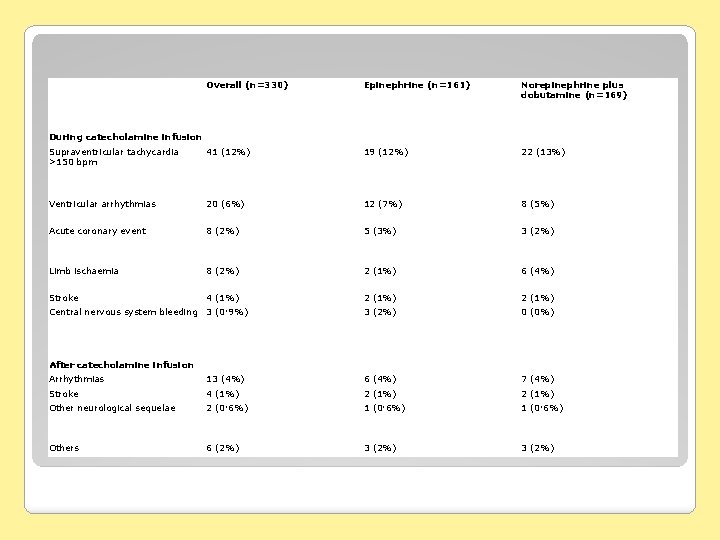
Overall (n=330) Epinephrine (n=161) Norepinephrine plus dobutamine (n=169) Supraventricular tachycardia >150 bpm 41 (12%) 19 (12%) 22 (13%) Ventricular arrhythmias 20 (6%) 12 (7%) 8 (5%) Acute coronary event 8 (2%) 5 (3%) 3 (2%) Limb ischaemia 8 (2%) 2 (1%) 6 (4%) Stroke 4 (1%) 2 (1%) 3 (2%) 0 (0%) During catecholamine infusion Central nervous system bleeding 3 (0· 9%) After catecholamine infusion Arrhythmias 13 (4%) 6 (4%) 7 (4%) Stroke 4 (1%) 2 (1%) Other neurological sequelae 2 (0· 6%) 1 (0· 6%) Others 6 (2%) 3 (2%)
VASST Study Randomized, double-blind trial N=778 pts with septic shock receiving Norepinephrine Vasopressin 0. 01 -0. 03 units/min vs Norepi 5 -15 mcg/min in addition to open label vasopressors Primary outcome=28 day mortality NEJM 2008; 358: 877 -87.
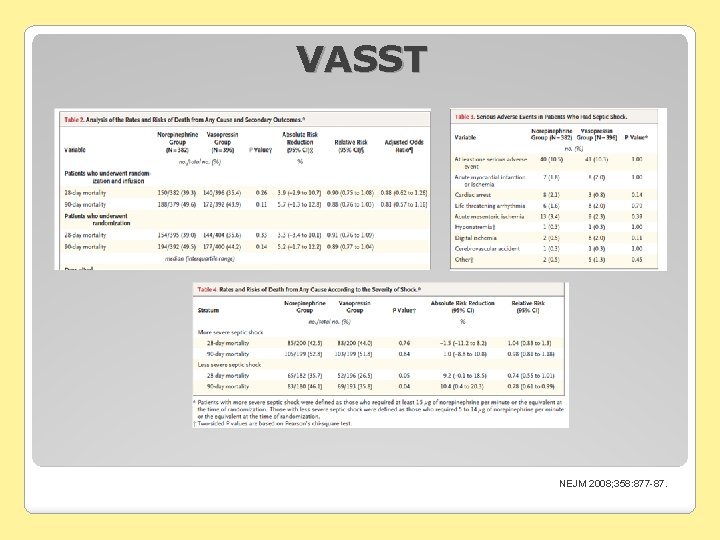
VASST NEJM 2008; 358: 877 -87.
SOAP II Randomized, N=1679 double-blind trial pts with shock Dopamine vs Norepinephrine as first-line vasopressor Primary outcome=28 day mortality NEJM 2010; 362: 779 -89.
SOAP II Cause of shock Sepsis 60% Cardiogenic source 16% Hypovolemia 16% Other 6% NEJM 2010; 362: 779 -89.
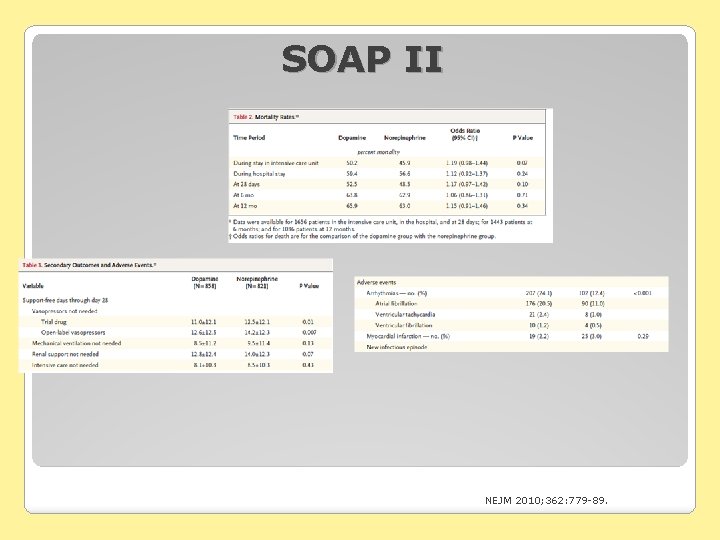
SOAP II NEJM 2010; 362: 779 -89.
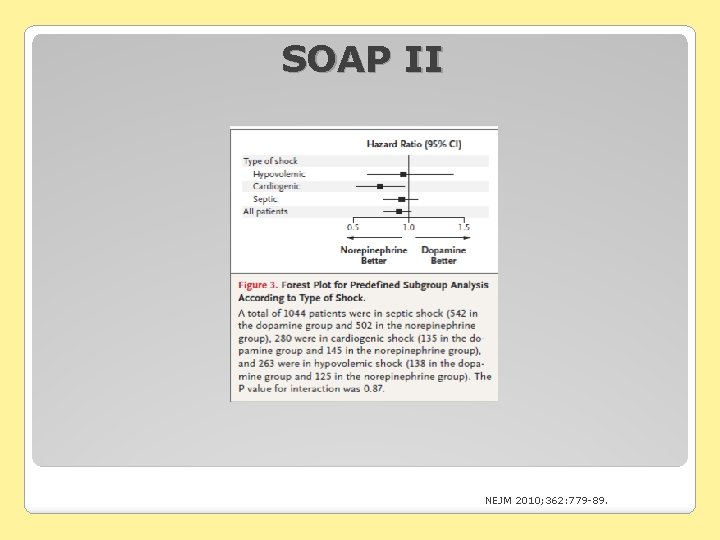
SOAP II NEJM 2010; 362: 779 -89.
Agent of Choice in Sepsis Surviving Sepsis Guidelines • No high quality evidence to recommend one catecholamine over another. • Dopamine or Norepinephrine as 1 st line • Norepinephrine is more potent. • Dopamine may be more useful in patients with compromised systolic function. • Epinephrine suggested as first alternative in septic shock poorly responsive to 1 st line tx (grade 2 B) • Vasopressin may be added to Norepinephrine. Crit Care Med 2008; 36: 296 -327.
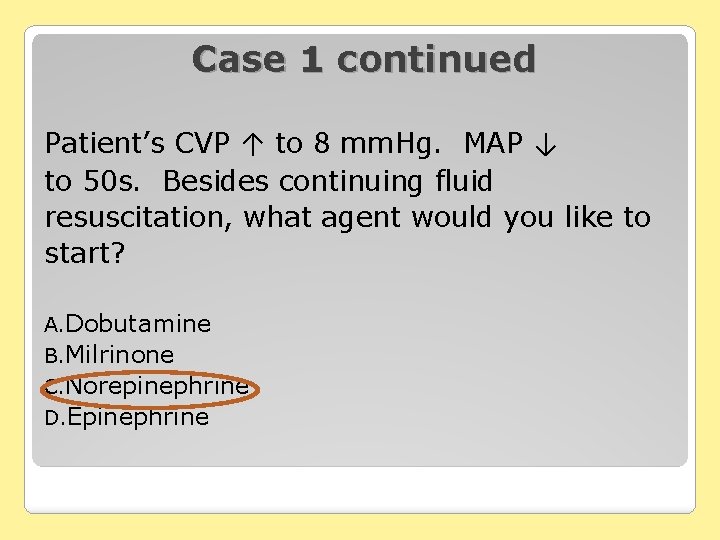
Case 1 continued Patient’s CVP ↑ to 8 mm. Hg. MAP ↓ to 50 s. Besides continuing fluid resuscitation, what agent would you like to start? A. Dobutamine B. Milrinone C. Norepinephrine D. Epinephrine
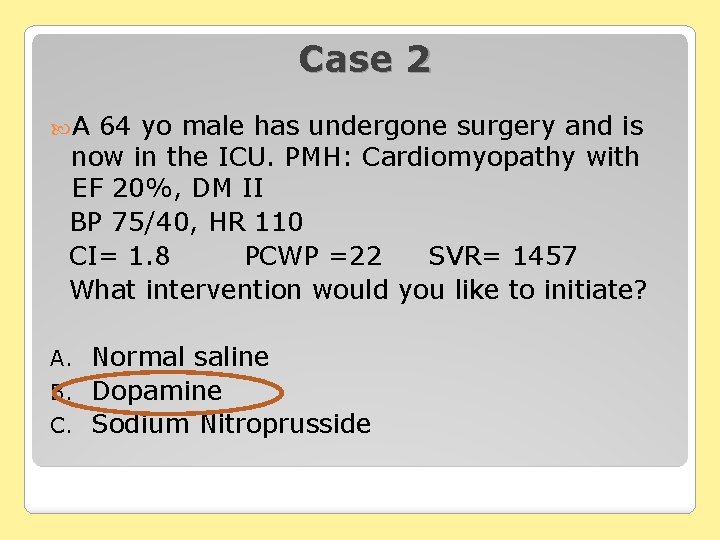
Case 2 A 64 yo male has undergone surgery and is now in the ICU. PMH: Cardiomyopathy with EF 20%, DM II BP 75/40, HR 110 CI= 1. 8 PCWP =22 SVR= 1457 What intervention would you like to initiate? Normal saline B. Dopamine C. Sodium Nitroprusside A.
Questions
- Slides: 47