Vasopressors and Inotropes Critical Care Lecture Series Objectives
Vasopressors and Inotropes Critical Care Lecture Series
Objectives ICU n n n What are the different classes of shock and give examples of each. Discuss how to investigate and the management principles behind each of the causes of shock. What are the different crystalloids and colloids available for resuscitation? Have knowledge of the mechanism of action of commonly used vasopressors and inotropes, including dopamine, dobutamine, milnerone, levophed, phenylephrine, epinephrine, vasopressin Discuss adverse events associated with the above agents.
Is My Patient in Shock? ICU n Definition of shock n Inadequate end organ perfusion leading to inadequate oxygen delivery n N. B. a patient in shock does not have to be hypotensive
ICU
Treatment of Shock ICU n Basic Resuscitation: ABCDE’s A: Airway establishment n B: Breathing: control WOB n C(a): Circulation Optimization n C(b): Control O 2 consumption n D: Delivery of O 2 adequately n E Extraction of O 2 n

Fluid resuscitation ICU Very important…. n Therapy with least detrimental effects n Fluid therapy may be beneficial in any type of shock n n Even cardiogenic shock/pulmonary edema
Fluid Resusitation ICU n Must “test the patient” n n Must always look for the effect of treatment n n Give volume and look for response/improvement Always start with NS of RL ? Need blood Re-evaluate patient after fluid If no improvement, and no adverse effects, repeat If adverse effect, needs inotropes/vasopressor if still in shock Too much: pulmonary edema (O 2 sats)
ICU A: Airway establishment Indications for intubation: 1. Failure of oxygenation or ventilation 2. Failure to protect airway 3. Condition present or procedure needed that will require intubation “shock” is an indication for intubation Hypotension common after intubation
B: Breathing: control WOB ICU Respiratory muscles are significant consumers of oxygen n Control will allow better O 2 delivery to other tissues n Sedation after intubation n
C(a): Circulation Optimization ICU Most causes of shock require some volume re-expansion – even cardiogenic shock - Starling curve n Crystalloid as good as colloid n Vasopressors ineffective if hypovolemic n n “double edged sword”
C(b): Control O 2 consumption ICU Reduce hyper-adrenergic state n Analgesia/sedation/muscle relaxation n temperature n
ICU D: Delivery of O 2 adequately Follow sats (keep > 92%) n ? Transfusion (Hbg >80 -100) n Lactate n Smv. O 2 n
E: Extraction of O 2 ICU O 2 must get from lungs to Hbg to tissues n O 2 extraction important in some types of shock n n Cyanide, Met. Hbg, SEPSIS

ICU ABCDE’s: Summary n A: Airway establishment: 02, bi. Pap, ETT n B: Breathing: control WOB: Sedation, analgesia n C(a): Circulation Optimization: fluids, inotropes, pressors n C(b): Control O 2 consumption: sedation, temp control, seizure control n D: Delivery of O 2 adequately: Hbg, fluid, pressor, inotropes n E: Extraction of O 2: R/O cyanide, met. Hbg, sepsis
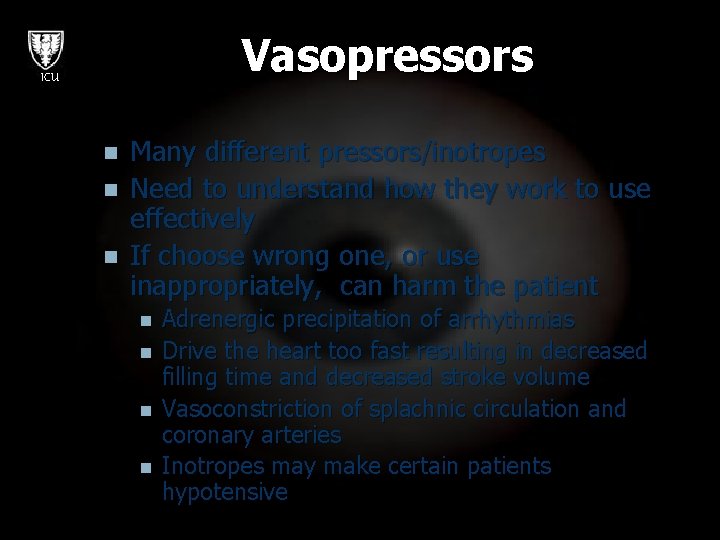
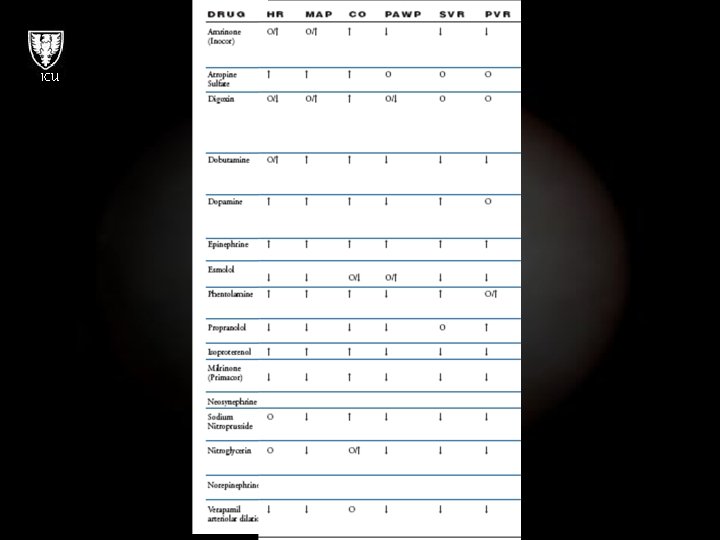
Vasopressors ICU n n n Many different pressors/inotropes Need to understand how they work to use effectively If choose wrong one, or use inappropriately, can harm the patient n n Adrenergic precipitation of arrhythmias Drive the heart too fast resulting in decreased filling time and decreased stroke volume Vasoconstriction of splachnic circulation and coronary arteries Inotropes may make certain patients hypotensive
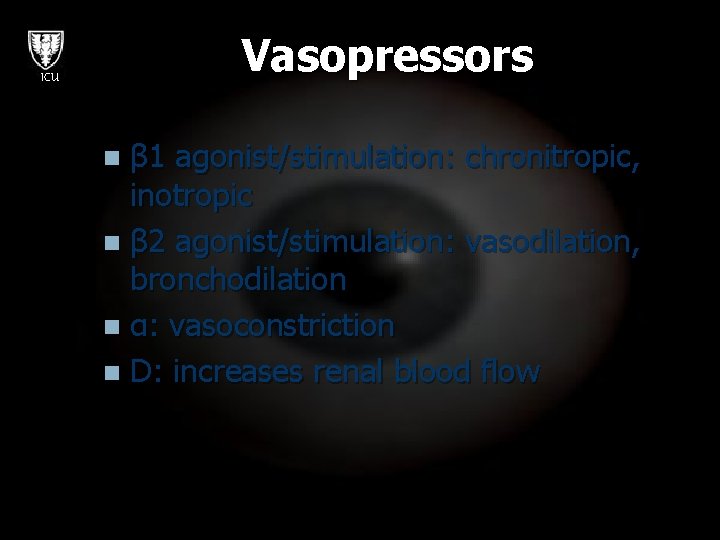
Vasopressors ICU β 1 agonist/stimulation: chronitropic, inotropic n β 2 agonist/stimulation: vasodilation, bronchodilation n α: vasoconstriction n D: increases renal blood flow n
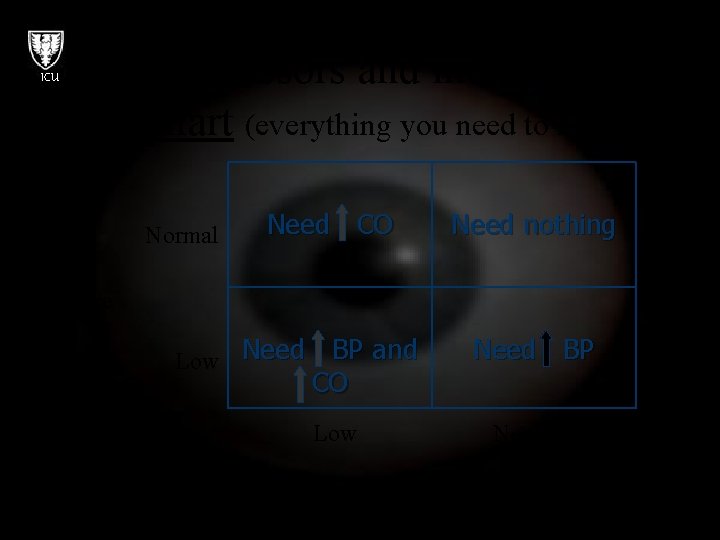
ICU Vasopressors and inotropes: the chart (everything you need to know) Normal Need CO Need nothing Blood pressure Low Need BP and CO Low Need BP Normal Cardiac Output
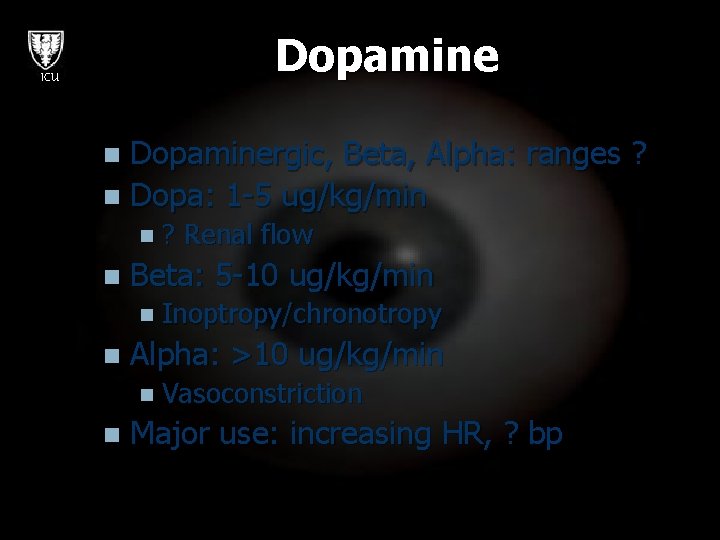
Dopamine ICU Dopaminergic, Beta, Alpha: ranges ? n Dopa: 1 -5 ug/kg/min n n? n Renal flow Beta: 5 -10 ug/kg/min n Inoptropy/chronotropy n Alpha: >10 ug/kg/min n Vasoconstriction n Major use: increasing HR, ? bp
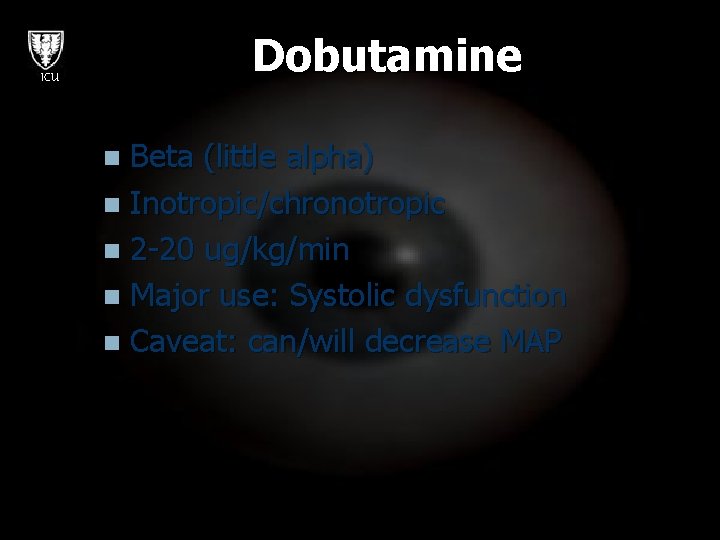
Dobutamine ICU Beta (little alpha) n Inotropic/chronotropic n 2 -20 ug/kg/min n Major use: Systolic dysfunction n Caveat: can/will decrease MAP n
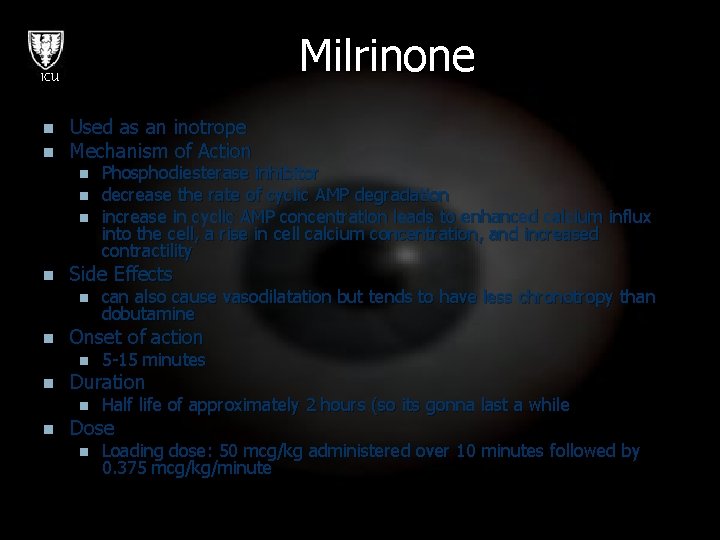
Milrinone ICU n n Used as an inotrope Mechanism of Action n n Side Effects n n 5 -15 minutes Duration n n can also cause vasodilatation but tends to have less chronotropy than dobutamine Onset of action n n Phosphodiesterase inhibitor decrease the rate of cyclic AMP degradation increase in cyclic AMP concentration leads to enhanced calcium influx into the cell, a rise in cell calcium concentration, and increased contractility Half life of approximately 2 hours (so its gonna last a while Dose n Loading dose: 50 mcg/kg administered over 10 minutes followed by 0. 375 mcg/kg/minute
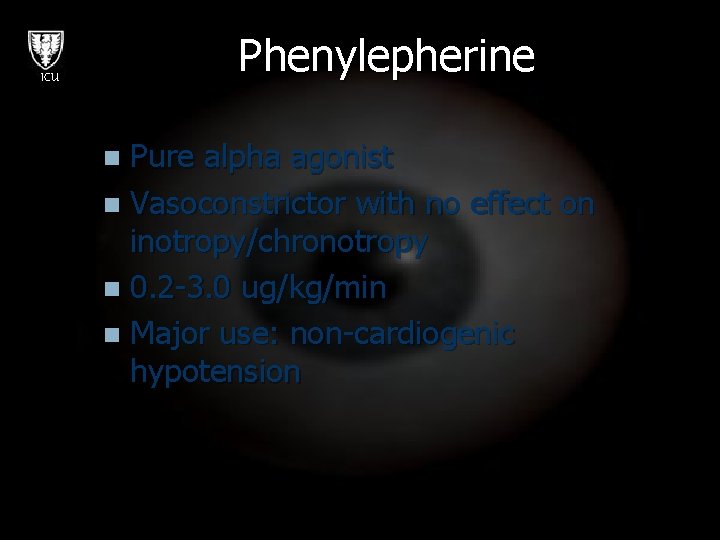
Phenylepherine ICU Pure alpha agonist n Vasoconstrictor with no effect on inotropy/chronotropy n 0. 2 -3. 0 ug/kg/min n Major use: non-cardiogenic hypotension n
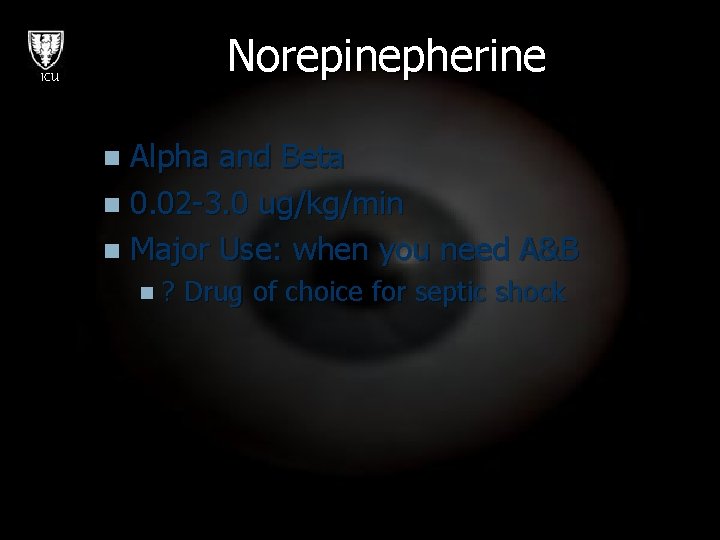
Norepinepherine ICU Alpha and Beta n 0. 02 -3. 0 ug/kg/min n Major Use: when you need A&B n n? Drug of choice for septic shock
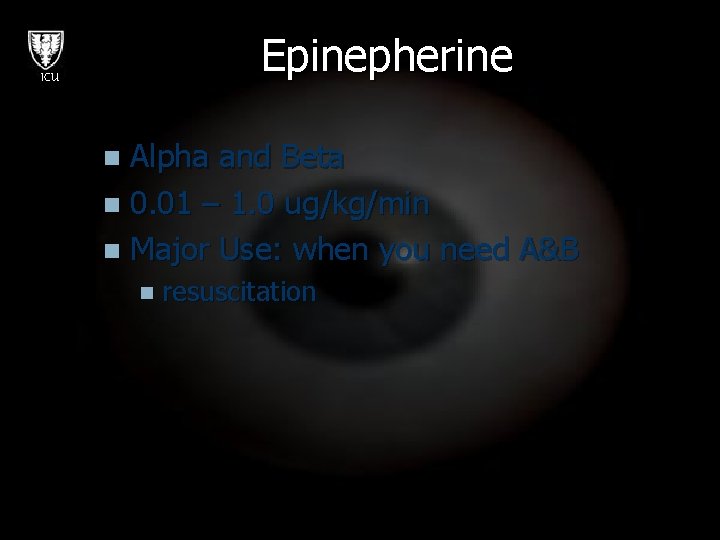
Epinepherine ICU Alpha and Beta n 0. 01 – 1. 0 ug/kg/min n Major Use: when you need A&B n n resuscitation
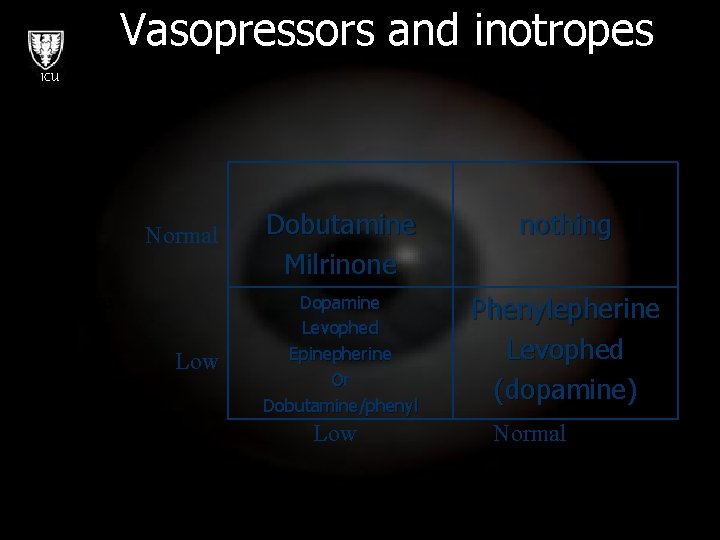
Vasopressors and inotropes ICU Normal Dobutamine Milrinone nothing Low Dopamine Levophed Epinepherine Or Dobutamine/phenyl Phenylepherine Levophed (dopamine) Blood pressure Low Normal Cardiac Output
ICU
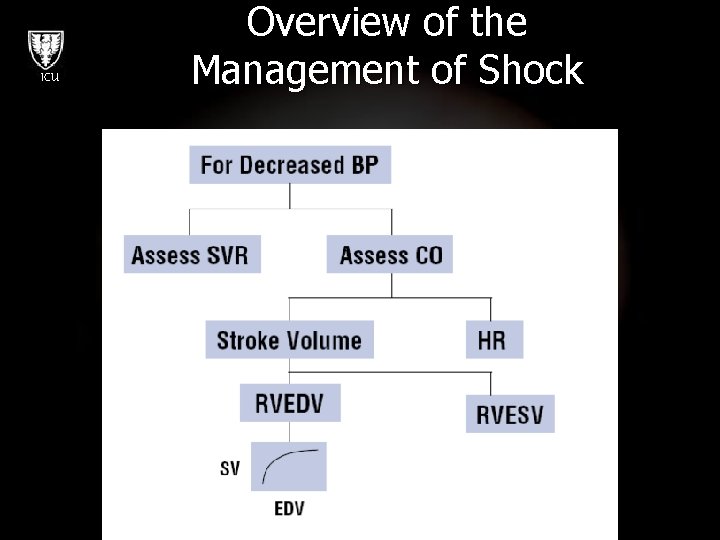
ICU Overview of the Management of Shock
Case Study ICU 65 yo male presents to ED n Complaining of cough and feeling very unwell n HR 120, BP 100/60, RR 30, temp 39 n Is this patient in shock? n What investigations n What treatment would you start? n
Case Study ICU The patient’s BP drops to 90/50, what would you do now? n Would you start pressors? Which one? n
Case Study ICU n The patient is on 0. 8 ug/kg/min of levophed through a femoral line. Why might the patient not be responding to the vasopressors? What measurement would be helpful in improving this man’s MAP?
Case Study ICU n The patient has been resuscitated, now has a BP of 110/90. HR 65. His JVP is 12. His lactate continues to rise however. He is also anuric. Is this patient in shock? What is your management now?
Summary ICU n n Shock can be the consequence of decreased SVR, decreased CO or both. Management of shock should be tailored to the physiologic state of the patient. Drugs are available to augment SVR, HR, afterload and contractility. Remember to optimize preload and consider the oxygen carrying capacity of the blood.
- Slides: 31